Abstract
Rationale
Coronavirus (COVID-19) disproportionately affects people of color (e.g., Black and Latinx individuals) in the U.S., increasing their morbidity and mortality relative to White people. Despite this greater threat to their well-being, the mental health impact of COVID-19 on people of color remains poorly understood. Perseverative cognition (PC; i.e., excessive worry and/or rumination), is a common psychological response to such threats that independently associates with poor mental and physical health.
Objective
To examine patterns of PC across race/ethnicity when the COVID-19 pandemic began.
Methods
This study surveyed 6,514 respondents from the NORC AmeriSpeak panel, a probability-based representative national sample of U.S. adults between 3/18/20-4/18/20. We employed traditional statistical analyses and natural language processing of open-ended data to examine pandemic-related worries.
Results
Weighted regression analyses with relevant covariates revealed group differences across specific domains of COVID-related worry. Relative to White respondents, Hispanic/Latino respondents reported more worries about social disarray, meeting basic needs, experiencing economic impacts, obtaining healthcare, and contracting COVID-19. Black respondents reported more worry about economic impacts relative to Whites. Additional group differences in worry emerged in open-ended data: Black respondents perseverated about death from COVID-19, whereas Hispanic/Latino respondents reported concerns about COVID-19 spread, and people refusing to uphold mitigation mandates. In contrast, White respondents expressed worry over compromised immune systems and economic collapse.
Conclusions
Results identify significant group differences in COVID-19 related PC, suggesting that people of color faced greater threat to mental well-being at the onset of the pandemic, and may be at greater risk for downstream PC-related physical health consequences.
Keywords: Perseverative cognition, COVID, People of color, Worry, Mental health, SARS-CoV-2, Novel coronavirus
The COVID-19 pandemic has had a profound, yet disparate, negative impact on public health and well-being (Centers for Disease Control, 2021; Nicola et al., 2020). Compared to White Americans, people of color (e.g., Black and Hispanic/Latino Americans) have experienced more deleterious health outcomes due to COVID-19 (Centers for Disease Control, 2021; Garg et al., 2020; Kandil et al., 2020; Mackey et al., 2021) -- both Black and Hispanic/Latino individuals are at least two times more likely to die from COVID-19 relative to White individuals when adjusting for age (Centers for Disease Control, 2021). Such health disparities are not new, as some marginalized racial groups experience greater morbidity and mortality from the leading causes of death, including cardiovascular disease and cancer (Virani et al., 2020). During the pandemic, racial/ethnic disparities have also been found in sleep patterns (Yip et al., 2021, 2022; cf. Hisler and Twenge, 2021), economic outcomes (Couch et al., 2020), and among households with healthcare workers or workers who could not work from home (Selden and Berdahl, 2020). For example, people of color have borne the economic-brunt of COVID-19 despite representing a relatively large percentage of essential workers who continued working during the pandemic (Kantamneni, 2020). To put this in context, people of color are at higher risk for contracting COVID-19, perhaps due to ongoing work obligations and living arrangements (Selden and Berdahl, 2020), to struggle financially throughout the pandemic (Couch et al., 2020), and for those who contract COVID-19, to experience worse prognoses relative to their White counterparts (Kandil et al., 2020).
Disparities in these pandemic-related socioeconomic and health impacts may be associated with individuals’ mental health (Holman et al., 2020; Czeisler et al., 2020; Ettman et al., 2020). Perseverative cognition (PC), defined as excessive worry and/or rumination (Brosschot et al., 2006), is a key aspect of mental health and well-being. The PC Hypothesis (Brosschot et al., 2006) proposes that excessive perseveration can negatively affect both psychological and physiological well-being and is often characteristic of those who perceive their environment as less safe or threatening (Brosschot et al., 2006, 2018; Verkuil et al., 2010). Thus, PC is thought to be an important mechanism linking stress (e.g., pandemic-related threats) with negative health outcomes (Verkuil et al., 2010). Research has shown that general PC tendencies are linked with poorer mental health outcomes (e.g., emotion regulation, trait anxiety; Williams et al., 2017). Moreover, a meta-analysis found that PC negatively affects cardiovascular, autonomic, and endocrine nervous systems, providing compelling evidence linking PC with health outcomes and stress vulnerability (Ottaviani et al., 2016). Thus, research aimed at understanding racial/ethnic differences in PC at the onset of the COVID-19 pandemic is warranted, as such differences might contribute to or perpetuate identified disparities in COVID-19 and other health outcomes.
The COVID-19 pandemic has been unique in that it constitutes a collective trauma in which the exposures have been multiple and multi-faceted. For example, job loss because of business closings in the community could coincide with high sickness or death counts in one's community. Other individuals may have kept their jobs but were unable to get access to basic household items due to panic buying as the pandemic set in. Some individuals with specialized healthcare needs may have forgone standard health care visits because of fear or after losing their job-related health insurance. Furthermore, racial and ethnic disparities across these circumstances may be associated with PC in specific domains. For example, individuals who lost wages or employment during the pandemic may be particularly worried about the economic impact of the pandemic on their lives. It is also likely that among Black and Hispanic/Latino individuals, who are at greater risk of contracting and dying from COVID-19 (Centers for Disease Control, 2021), health-related worry may be particularly elevated relative to Whites (who often benefit from better health coverage and easier access to health facilities). Thus, understanding how people of color differ from their White counterparts on global worry, in addition to the specific worries embedded therein, is indeed warranted.
Given that direct and media-based exposures to collective traumas are cross-sectionally and longitudinally associated with poor psychological outcomes (see Holman et al., 2020; Thompson et al., 2019 for an overview), including worry, understanding how PC manifested among people of color relative to White individuals at the onset of the pandemic is critical for addressing community-specific mental health needs. In the current study, we examined these differences in a large, probability-based nationally representative sample of Americans. We had three aims: a) to examine whether people of color experienced more PC than their White counterparts (even when controlling for relevant covariates) and whether people of color differed from White individuals on specific domains of PC, b) ascertain the most prominent domains of PC within each race/ethnicity group, and c) explore PC topics by race/ethnicity among responses to an open-ended question about what concerned respondents the most about the COVID-19 pandemic.
1. Method
1.1. Design, sample, and data collection
Respondents were drawn from the NORC AmeriSpeak Panel, a probability-based survey research panel of 35,000 U.S. households who were selected at random from across the U.S. to create a representative panel of U.S. households. The AmeriSpeak Panel is the only probability panel in the U.S. that uses address-based sampling of respondents for the panel who subsequently participate in AmeriSpeak surveys online. Unlike typical Internet panels that allow people who already have Internet access to choose to opt in, no one can volunteer for the AmeriSpeak panel.
As part of a large, national study of early mental health responses to the COVID-19 pandemic, NORC drew our sample from the AmeriSpeak panel using sample stratification to assure representativeness with respect to age, gender, race/ethnicity, and education. The survey was fielded to a sample of 11,139 panelists between March 18, 2020 (five days after the United States President's declaration of a national emergency) and April 18, 2020. Participants received an email stating that the survey was available; they completed the survey anonymously online. Surveys are confidential, self-administered, and accessible at any time for a designated period; participants can complete it only once. Most respondents (86.4%) completed the survey within the first three days of data collection. Almost 44% completed the survey on a computer, about 54% completed it on a smartphone, and the remainder completed it on a tablet (or did not provide a response). NORC compensates AmeriSpeak panelists with points worth a cash equivalent (in this case $4). The survey was completed by 6,514 panelists (58.5% completion rate).
Participants were provided informed consent when they joined the NORC panel and were informed that their identities would remain confidential. All procedures for this study were approved by the Institutional Review Board at University of California, Irvine.
1.2. Measures
1.2.1. Perseverative cognition
Respondents completed a 10-item index of COVID-related worries adapted from measures used in prior research (Holman et al., 2008). Items measured prior-week global worry about COVID-19 affecting both participants and their loved ones (α = 0.91). Items were assessed on a 1 (never) to 5 (all the time) Likert-type scale. These 10-items were designed to cluster into 5 COVID-specific worry domains (each measured by two items) encompassing concerns around (1) being able to buy food, household supplies, and medications (α = 0.82), (2) not having enough money to pay bills (α = 0.80), (3) being unable to get healthcare (α = 0.87), (4) experiencing civil unrest in one's community (α = 0.90), and (5) getting sick or dying from COVID-19 (α = 0.80). A factor analysis of all 10 items revealed a 5-factor solution in which each of the two items that measured each domain loaded strongly on the appropriate factor (all factor loadings above 0.65). We also examined the measure for scale invariance across racial/ethnic groups and found that factor loadings do not substantively differ across racial/ethnic groups (see supplement for details).
Respondents were also asked “If you are worried about the Coronavirus outbreak, what is causing you the most concern?” and were provided with an open-ended text box in which to type their answers. There was no word limit, and they were encouraged to write as much or as little as they pleased.
1.2.2. Race and ethnicity
Upon entry to the AmeriSpeak panel, respondents provided their race and ethnicity. Categories include White, Black, Hispanic/Latino, Asian/Pacific Islander (Asian/PI), Multi-racial, and Other, which was comprised of Indigenous peoples and respondents who selected “Other” but did not provide more details about their race or ethnicity.
1.2.3. Covariates
Several covariates known to be associated with mental health outcomes in the context of large-scale traumatic events in past work (Holman et al., 2020; Garfin et al., 2020; Thompson et al., 2019) were included in the adjusted models. These covariates included demographic variables such as respondent age, gender, education, and region of residence. Models also included respondents’ pre-pandemic health status as collected by NORC upon enrollment into the AmeriSpeak panel 12–18 months before the pandemic began. Specifically, participants reported whether a doctor had ever diagnosed them with several physical and mental health ailments. Prior mental health diagnoses were coded as 0 (no prior mental health diagnosis) or 1 (prior anxiety, depression, or any other emotional, nervous, or psychiatric diagnosis). Prior physical health diagnoses were coded as a count of eight possible prior diagnoses (i.e., high cholesterol, hypertension, diabetes/high blood sugar, heart disease, stroke, cancer, lung disease, and other diagnoses; range 0–8).
Covariates also included relevant exposures to the COVID-19 pandemic.
Personal exposure. Respondents indicated their personal exposure to COVID-19 by responding to a checklist of experiences consisting of five items (had symptoms, were unable to get tested for the coronavirus, had contact with a COVID-19 positive person, was under quarantine, was diagnosed with COVID-19). The count ranged from 0 to 5.
Community exposure. Respondents indicated whether their community: had been ordered to “shelter in place”, experienced food shortages in local markets, closed educational institutions, canceled religious services, cancelled sports events, and closed restaurants. The count ranged from 0 to 6.
Work exposure. Respondents indicated whether their job required in-person interaction and whether they worked in an essential service role (e.g., grocery store, healthcare). Responses across these two items were collapsed and coded dichotomously to reflect whether a respondent was an essential worker (1) or not (0).
Secondary stressors. Respondents indicated their experiences with secondary stressors on a checklist including waiting in long lines for basic necessities, being asked to work or study remotely, losing wages, losing employment, cancelling travel plans, lacking access to healthcare, and having difficulty finding childcare. The count ranged from 0 to 7.
Media exposure. Respondents indicated their average daily hours of media exposure to COVID-related news in the past week (see Holman et al., 2020) on television, radio and print news; online news sources; and social media platforms. Response options ranged from 0 to 11 or more. Responses across these three media types were summed to create a composite variable ranging from 0 to 33.
Conflicting information exposure. Respondents were asked how often in the past week they were exposed to conflicting information across the news media, government officials, social media, and friends and family. Across these four items, response options ranged from 1 (Never) to 5 (All the time). A composite variable was created by averaging responses across these items (α = 0.68).
1.3. Analytic strategy
Differences in perseverative cognition (global worry) among racial and ethnic minority groups relative to White respondents were examined by conducting a series of ordinary least squares (OLS) regression analyses. All planned analyses met the assumptions of OLS regression. In the first analysis we assessed the raw mean differences in perseverative cognition between White respondents (reference group) and all other race/ethnicity categories, respectively. We followed up with an additional OLS model to determine whether controlling for covariates altered the mean differences. A series of additional multivariable OLS regressions were then used to examine whether people of color reported experiencing the five specific worries (basic necessities, economic impacts, healthcare access, social disarray, and sickness/death from COVID-19) differently than White respondents. From these latter models, we computed adjusted predicted mean worry values for each racial/ethnic group and plotted them descriptively to ascertain which worries were the most prominent within each race/ethnicity category. All OLS regression analyses were standardized and subsequently, each b represents the effect size (in standard deviation units) for the mean differences we report. Additionally, results were weighted to reflect the U.S. population and conducted in Stata 16.1 (College Station, TX).
An examination of missing data revealed that complete data were available for ∼98% of the sample (n = 6366). Further examination of the missingness revealed no specific pattern of missingness; a test of whether the data were missing completely at random (MCAR) across variables revealed that this was indeed the case (Little's MCAR test: χ 2 = 17.99, df = 360, p = 1.00 ns). Thus, we employed full information maximum likelihood estimation to estimate missing values, retain the full sample in each analysis, and derive unbiased regression estimates.
The content of the open-ended worry prompt was processed by first stemming each word such that each was altered to reflect its word stem (e.g., “analyzed” and “analyzing” became “analyz”). Responses were then tokenized into unigrams (i.e., single words) and bigrams (e.g., adjacent words pairs) to extract prevalent themes. An example of how bigrams are derived is as follows: the sentence “I wish I could fly” would be broken into the following word-pairs: I wish, wish I, I could, could fly. Next, stop words, or commonly used words that do not convey information about content (e.g., the, and), were removed from the corpus. Prevalent unigrams were identified by counting commonly expressed words by race/ethnicity. For deriving important bigrams, each was assigned an importance weight using the term frequency-inverse document frequency (tf-idf), a common metric that weighs less commonly used words and phrases in the English language more heavily than more commonly used words and phrases. All open-ended content was analyzed using the tidytext package (Silge and Robinson, 2016) in R software (R Core Team, 2021). Data from this study are under embargo through March 31st, 2023; after this date, the data will be available on the Open Science Framework.
2. Results
Weighted sample demographics (as well as descriptive statistics for all model variables) are contained in Table 1 . Fifty-two percent of the sample self-identified as female. Across the sample, 63.6% identified as White, 11.8% as Black, 16% as Hispanic/Latino, 3.4% as Asian/Pacific Islander (Asian/PI), 3.5% as Multi-racial, and 1.7% as Other. At least 91% of respondents had a high school diploma or above, and percentages were relatively equal across age ranges of the respondents. As such, our sample closely matched the census benchmarks across all demographic categories with the exception that we had slightly lower proportion of Asian/Pacific Islanders than is seen in the national population. Respondents on average reported experiencing more than four community-based COVID-related exposures (e.g., shelter in place), engaging over 7 hr of daily COVID-related media coverage in the prior week, and reported experiencing each of the different types of worries at least sometimes.
Table 1.
Weighted descriptive statistics for all model variables. Sample size varies across variables due to missing data.
| % | M | SD | Range | |
|---|---|---|---|---|
| Race/ethnicity | ||||
| White | 63.6 | |||
| Black | 11.8 | |||
| Hispanic | 16.0 | |||
| Asian | 3.4 | |||
| Multiracial | 3.5 | |||
| Other | 1.7 | |||
| Gender | ||||
| Man | 48.0 | |||
| Woman | 52.0 | |||
| Age | ||||
| 18-29 | 20.3 | |||
| 30-44 | 25.6 | |||
| 45-59 | 24.6 | |||
| 60+ | 29.5 | |||
| Education | ||||
| No HS diploma | 9.9 | |||
| HS graduate | 28.5 | |||
| Some college | 28.0 | |||
| BA or higher | 33.6 | |||
| Region | ||||
| Northeast | 17.3 | |||
| Midwest | 21.0 | |||
| South | 37.6 | |||
| West | 24.1 | |||
| Prior mental health diagnosis | .17 | .38 | 0–1 | |
| Prior physical health | 1.03 | 1.22 | 0–8 | |
| Personal COVID-19 exposure | .12 | .41 | 0–5 | |
| Community exposure | 4.87 | 1.53 | 0–6 | |
| Work exposure | .29 | .45 | 0–1 | |
| Secondary stressors | 1.36 | 1.21 | 0–7 | |
| Media exposure | 7.14 | 6.97 | 0–33 | |
| Conflicting information exposure | 2.90 | .83 | 1–5 | |
| Global worry | 2.59 | .93 | 1–5 | |
| Basic necessities | 2.60 | 1.07 | 1–5 | |
| Economic | 2.68 | 1.22 | 1–5 | |
| Healthcare access | 2.65 | 1.18 | 1–5 | |
| Social disarray | 2.53 | 1.06 | 1–5 | |
| Sickness/death from COVID-19 | 2.51 | 1.06 | 1–5 | |
2.1. Quantitative analyses
People of color reported significantly higher global worry than White respondents in the weighted unadjusted model (see Table 2 ). However, after the inclusion of relevant covariates, these group differences were somewhat attenuated, especially among Black respondents who on average were no longer significantly different from White individuals.
Table 2.
Standardized unadjusted and adjusted ordinary least squares regression analyses examining the racial/ethnic differences in global worry (N = 6,514).
| Variables | Unadjusted |
Adjusted |
||
|---|---|---|---|---|
| B | 95% CI | B | 95% CI | |
| Race/ethnicity (White = 0) | ||||
| Black | .07** | [.02,.12] | -.01 | [-.05,.04] |
| Hispanic/Latino | .16*** | [.12,.21] | .07** | [.03,.11] |
| Multi-racial | .06*** | [.03,.09] | .03* | [.01,.06] |
| Asian/PI | .05*** | [.02,.08] | .05** | [.01,.08] |
| Other | .02* | [.001,.05] | .01 | [-.01,.04] |
Note: CI = confidence interval; *p < .05, **p < .01, ***p < .001.
Adjusted model includes several covariates: demographics (age, gender, education, U.S. region), mental and physical health collected 12–18 months before the pandemic, COVID-related direct exposure, community exposures (e.g., school and business closures), secondary stressors (e.g., job loss, health care restrictions), hours of COVID-related media use, and exposure to conflicting information.
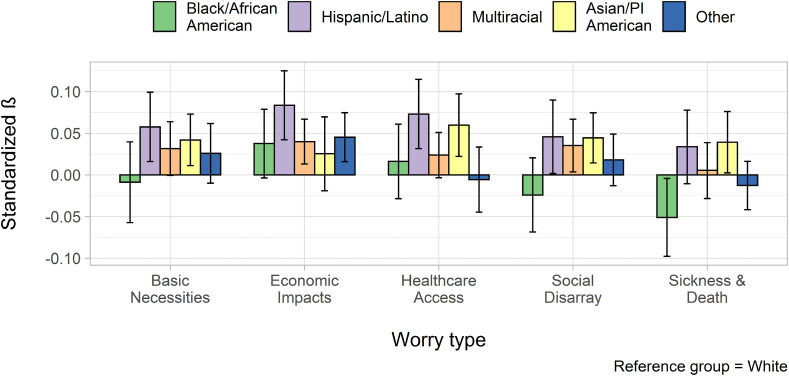
We then evaluated whether people of color differed from White individuals on the quantitative measure's subcategories of worry (see Fig. 1 ).
Fig. 1.
Standardized regression coefficients and confidence intervals representing the differences between people of color and White respondents across five domains of worry. All models adjusted for covariates: Demographics (age, gender, education, U.S. region), prior mental and physical health collected 12–18 months before the pandemic, COVID-related direct exposure, secondary stressors (e.g., job loss, health care restrictions), hours of COVID-related media use, and exposure to conflicting information. Note: Asian/PI = Asian/Pacific Islander. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
2.1.1. Basic necessities
Controlling for covariates, Hispanic/Latino (b = 0.05, SE = 0.02, p = .007) and Asian/PI respondents (b = 0.04, SE = 0.01, p = .008) reported significantly more worry about accessing basic necessities than did White respondents. That is, Hispanic/Latino and Asian/PI respondents were more worried about being able to access basic necessities than were White people.
2.1.2. Economic impacts
Respondents in the Hispanic/Latino (b = 0.08, SE = 0.02, p < .001), Multiracial (b = 0.04, SE = 0.01, p = .004), and “Other” (b = 0.04, SE = 0.01, p = .003) categories expressed significantly more worry about economic impacts than did White respondents. That is, respondents from Hispanic/Latino, Multiracial, and “Other” racial/ethnic backgrounds were more worried about the economic impacts of the pandemic than were White respondents.
2.1.3. Healthcare access
Hispanic/Latino (b = 0.07, SE = 0.02, p = .001) and Asian/PI respondents (b = 0.05, SE = 0.01, p = .002) reported significantly more worry about healthcare access than did White respondents. That is, Hispanic/Latino and Asian/PI respondents were more worried about accessing healthcare than were White respondents.
2.1.4. Social disarray
Hispanic/Latino (b = 0.04, SE = 0.02, p = .04), Multiracial (b = 0.03, SE = 0.01, p = .03), and Asian/PI respondents (b = 0.04, SE = 0.01, p = .004) reported significantly more worry about social disarray than did White respondents. That is, respondents from Hispanic/Latino, Multiracial, and Asian/PI racial/ethnic backgrounds were more worried about social disarray than were White respondents.
2.1.5. Sickness and death from COVID-19
Even though people of color were at greater risk of sickness and death from COVID-19, only Asian/PI respondents reported more worry about getting sick or dying from COVID-19 than did White respondents (b = 0.03, SE = 0.01, p = .03). Unexpectedly, in the quantitative data, Black respondents reported significantly less worry about sickness and death from COVID-19 relative to their White counterparts (b = −0.05, SE = 0.02, p = .03) as the pandemic was just starting to spread across the U.S.
2.1.6. Prominent worries within minority group
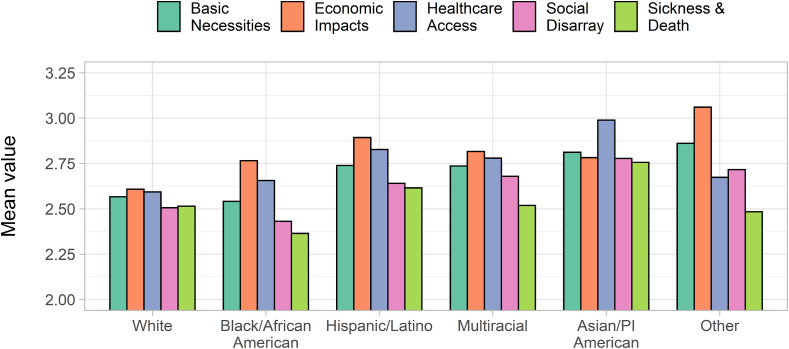
Predicted mean levels of specific worries within each race/ethnicity revealed additional patterning in the worries most prominent within each group (Fig. 2 ). For example, among Black and Hispanic/Latino respondents, economic impacts and healthcare access were the top worries, consistent with studies documenting greater economic impacts for people of color (Kantamneni, 2020). For Asian/PI respondents, healthcare access was the top worry. Among respondents categorized as Other, worries related to economic impacts and access to basic necessities were the most prominent.
Fig. 2.
Predicted mean values of worry across five worry domains by race/ethnicity group. All models adjusted for covariates: Demographics (age, gender, education, U.S. region), mental and physical health collected 12–18 months before the pandemic, COVID-related direct exposure, community exposures (e.g., school and business closures), secondary stressors (e.g., job loss, health care restrictions), hours of COVID-related media use, and exposure to conflicting information. Note: Asian/PI = Asian/Pacific Islander.
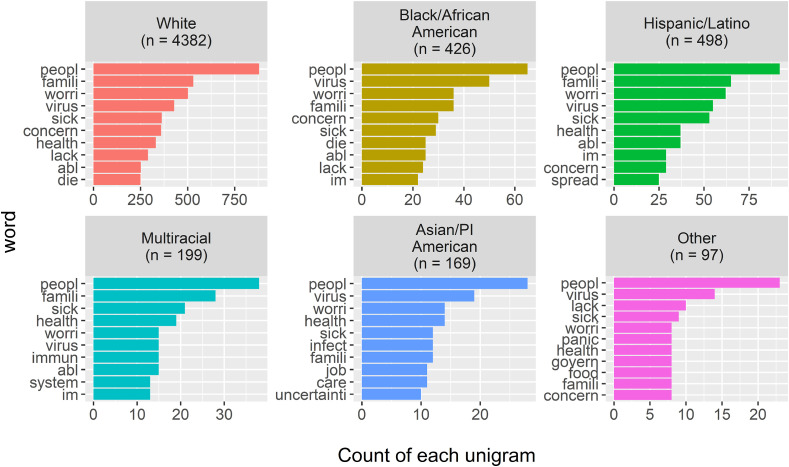
2.2. Open-ended worries by race/ethnicity
In all, 88.6% of respondents wrote a response to this open open-ended item. Controlling for covariates, Black respondents were less likely than Whites to respond to the prompt (OR = 0.53, SE = 0.09, p = .001). No other groups differed from White respondents in the likelihood of responding.
On average, respondents wrote ∼15 words (SD = 13.65; Range: 1–57 words). Relative to White respondents, Black and Asian/PI respondents wrote fewer words (b Black = −2.19, SE = 0.68, p = .001; b Asian/PI = −3.03, SE = 0.99, p = .002).
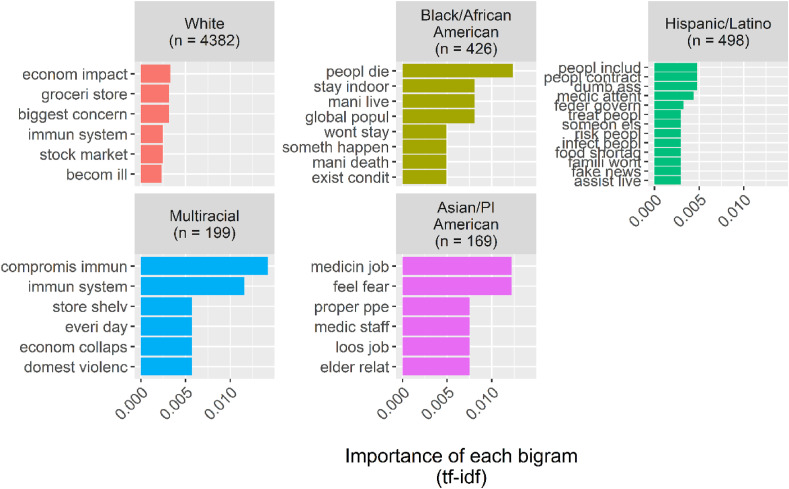
Next, we evaluated worry prompt content by race/ethnicity. We found important areas of incongruence among quantitatively and qualitatively measured PC (see Fig. 3, Fig. 4 ). For example, in contrast to the economic worries reported above, Black respondents expressed concerns around adherence to mitigation efforts (e.g., “stay indoor”) and COVID-related mortality (e.g., “people die”, “mani lives”, and “exist conditions”), and Hispanic/Latino respondents focused on concerns about the virality of COVID-19 (e.g., “spread” and “infect people”) in the open-ended data. Hispanic/Latino respondents also expressed concerns around food shortages (e.g., “food shortage”), in keeping with their PC around obtaining basic necessities.
Fig. 3.
Top 10 most frequent words in COVID-related concerns by race/ethnicity.
Fig. 4.
Top bigrams of COVID-related concerns by race/ethnicity.
Among Asian/PI respondents, for whom health care access was a prominent worry, we found congruence in their open-ended responses as evidenced by themes related to properly staffed hospitals and access to personal protective equipment. Additionally, their responses included marked expression of COVID-related fear.
Multiracial/ethnic respondents’ open-ended responses mirrored their worries (measured quantitatively); they expressed health-related concerns (e.g., “compromis immune”), access to basic necessities concerns (e.g., “store shelves”), and economic concerns (e.g., “economic collaps”).
Among White respondents, concerns expressed in the prompt were also consistent with quantitatively measured worries (i.e., both a focus on health and marked economic concerns). They also expressed concerns around panic buying at grocery stores (e.g., “groceri store”)
3. Discussion
The goal of the current study was to investigate whether COVID-19 pandemic-related PC – specifically worry – differed as a function of race/ethnicity. Using a mixed methods approach, we found that this was indeed the case. Unadjusted regression results showed that all people of color in our sample exhibited higher pandemic-related PC compared with White individuals. These data are consistent with prior reports on mental well-being and COVID-19 among marginalized individuals in the U.S. (Novacek et al., 2020). For example, in a sample of over 10,000 online respondents, fear of COVID-19 was higher for Asian and Hispanic/Latino individuals, and women, and this fear was associated with anxiety and depressive symptoms (Fitzpatrick et al., 2020) – both of which have been associated with PC (Verkuil et al., 2010; Williams et al., 2017). Moreover, anxiety increased more than 20% over the initial month of the pandemic among Black individuals, an increase that was linked to COVID-19 mortality (Jacobs and Burch, 2021). However, in the present study, the difference in worry between Black and White respondents was attenuated, especially when adjusting for age. Black respondents between ages 37 and 44 years of age reported the highest PC related to COVID. When age was not considered as a covariate, PC related to COVID remained significantly elevated for Black compared to White respondents. This suggests that the significant difference between White and Black respondents is driven by high PC in the Black 37–44 age group and may not be present among Black people across the lifespan.
We also found that PC was domain-specific for respondents of color. In the quantitative analyses, relative to White respondents, people of color expressed more worry about acquiring basic necessities, economic impacts, access to healthcare, and social disarray resulting from the pandemic. We also examined the most prominent worries within race/ethnicity groups, finding that all pandemic-related concerns were not experienced equally. Patterning within groups provided insight into domains of PC most salient for members of each racial/ethnic group. Although the most prominent concerns revolved around economic impacts and access to healthcare, this examination also made it clear that worry about sickness and death was the least prominent worry among respondents of color. Given the detrimental psychophysiological nature of PC (Ottaviani et al., 2016; Verkuil et al., 2010; Williams et al., 2017), these findings suggest that to mitigate the harm caused by the pandemic in communities of color, we need to tailor pandemic-related communications and interventions for different racial/ethnic groups so that they adequately target the concerns experienced in these communities.
Furthermore, while these data revealed that people of color exhibited higher mean levels of PC in quantitative data (relative to Whites), open-ended responses to a question about what worried respondents the most provided additional context into PC and in some cases was incongruent with group-specific means across worry domains. This suggests that pandemic-related PC may be multifaceted among people of color. For example, Black and Hispanic/Latino respondents reported higher quantitative PC related to economic impacts during the pandemic, yet qualitative responses highlighted concerns around adherence to mitigation efforts and mortality. Similarly, Hispanic/Latino respondents reported concerns about the virality of the coronavirus. Although not evident among Asian/PI and Multiracial respondents, inconsistencies between quantitative and qualitative data highlight the complex nature of PC in people of color relative to White individuals at the start of the COVID-19 pandemic. Future research on PC should consider employing a multimethodological approach when attempting to understand meaningful differences in psychological phenomena like PC, as inconsistencies across methods might lead to additional community-specific insights.
3.1. Strengths and limitations
We acknowledge some limitations of this work. First, our quantitative measure of pandemic-related worry was not exhaustive of all the respondents' possible worries. Although we believe we captured respondents’ general concerns, respondents were likely to have other worries on their minds, as evidenced by the open-ended responses in our survey. We further note that the effect sizes of our findings are relatively small, but nonetheless significant. Given the robust associations found between perseverative cognition and physical health in prior research (Ottaviani et al., 2016), the potential health implications for people of color dealing with an already deadly pandemic are substantial. Thus, small effect sizes still reveal meaningful differences (relative to Whites) when applied to the millions of people who comprise these minority groups.
Finally, not all respondents answered the open-ended item about their COVID-19 pandemic-related worries, as just over 11% of the sample did not respond. This could be because the standard survey items measuring worries accurately captured non-responders’ concerns. Alternatively, respondents may have been hesitant because they were uncomfortable sharing any additional information. Thus, we may have missed important information from these individuals as it relates to the potential differences between quantitative and qualitative data. Additionally, we used “rough” automated natural language processing (NLP) techniques to understand the qualitative data we collected; there are more sophisticated techniques for automatically extracting topical content from text data (e.g., topic modeling) however the short length of the responses to this prompt could render these techniques less effective.
Despite these limitations, our study has several strengths. For example, we utilized a probability-based sample drawn from a panel of 35,000 U.S. households who were selected at random from across the United States. The rigorous sampling and weighting procedures ensured that our results were representative of the population under study and provided confidence in our assertions about the domain-specific impact of the COVID-19 pandemic on respondents' PC. We also used a mixed-method approach, employing NLP analyses of open-ended text data, to triangulate on PC at the beginning of the pandemic. The inclusion of this open-ended item provided respondents the opportunity to share more and thus enrich our understanding of other domains of PC relevant at the onset of the pandemic. Such data driven approaches in novel contexts help to bolster the scientific community's ability to fully understand the psychological phenomena under study. The analyses we conducted also included several relevant covariates known to be associated with PC in collective trauma contexts; although not the focus of this paper, including these covariates offers clues about potential mechanisms that put people of color at increased risk of PC.
To date, people of color continue to have higher morbidity and mortality from COVID-19 compared with White individuals (Centers for Disease Control, 2021; Kandil et al., 2020). As mentioned, such health disparities are not new. The current results identify racial/ethnic differences in early pandemic-related PC that may ultimately play an important role in perpetuating these disparities and serve as a potential mechanism for poorer mental and physical health outcomes. For example, autonomic dysregulation at rest, marked by lower parasympathetic activity, is linked with both PC and maladaptive regulation of the immune (Thayer and Sternberg, 2006) and inflammatory (Williams et al., 2019) systems. It thus stands to reason that greater PC at the beginning of the pandemic might have left people of color particularly susceptible to complications and death from COVID-19. The risk associated with heightened early pandemic-related PC would likely be especially problematic for essential workers, many of whom are people of color who were at high risk for exposure to COVID-19 every day. Given our data and the detrimental nature of PC, it is critical for clinical settings and public health measures to consider racial and ethnic differences in PC related to the disease itself, and how such PC might negatively contribute to health and recovery.
Pandemics and other public health emergencies are likely to occur in the future; our data suggest that communities of color may have a more diverse array of concerns that need to be addressed to limit the harm done by such events. Priorities should include (but not be limited to) access to health care, testing and personal protective equipment, as well as other resources (e.g., economic support, basic necessities) to promote survival and minimize exposure and death risk. Making such resources readily available might decrease PC and in so doing, improve mental and physical well-being (see Ottaviani et al., 2016; Williams et al., 2017). As future threats like the COVID-19 pandemic arise, it is crucial that a more robust public health response be executed to deliver key resources to communities of color so that they can survive amidst a public health emergency at a rate similar to their White counterparts.
A recent example of this is the issue of COVID-19 “vaccine hesitancy”, especially in communities of color where individuals may be “waiting to see” whether the vaccine is effective (Kaiser Family Foundation, 2021). People of color may also have preferences about how and where to get vaccinated that were not well understood or addressed in the COVID-19 vaccine roll-out (see Fisher et al., 2021). Examining vaccine-related PC is an important step for future research to better understand the barriers that may be limiting vaccination uptake in communities of color. With that information, public health officials could tailor communications to address vaccine-related concerns, and hopefully encourage confidence in the safety and efficacy of the vaccine, while simultaneously making the vaccine more accessible (e.g., mobile vaccine clinics); such efforts would directly combat race-related concerns often observed in medicine (Vince, 2020; Yancy, 2020). Indeed, cultural mistrust and vaccine hesitancy among the Black community persist in part due to historical contexts such as the Tuskegee experiment. Therefore, efforts at decreasing vaccine hesitancy must consider cultural collective traumas experienced by people of color that are linked to the medical establishment.
Future studies also need to address the attacks on Asian/PIs, who continue to be victims of racialized violence resulting from conflicting information and the spread of disinformation about the origins of COVID-19. These unfortunate incidents are in line with worries of “social disarray” indicated by Asian/PI respondents at the onset of the pandemic in the current study (see Wu et al., 2021). In fact, hearing about or witnessing these incidents is associated with poorer sleep quality and shorter sleep duration, thereby contributing to health risks, in Asian Americans during the pandemic (Yip et al., 2022). Pandemic-related PC might be even more complex among Asian/PI people today compared to the onset of the pandemic given the continued rise of these incidents. This notion is supported in a recent study showing Asian and Black individuals to have higher levels of COVID-related perceived racial bias compared to both AIAN and Hispanic/Latino individuals (Fisher et al., 2022). In addition to interpersonal racism, people of color experienced systemic racism during the pandemic, accentuated by economic racial disparities; they were more likely to be essential workers and have living arrangements that may have contributed directly to worry via increased vulnerability (see Selden and Berdahl, 2020). In fact, evidence suggests structural racism mediates the association between COVID-related distress and poorer mental health (i.e., higher anxiety and depression; Fisher et al., 2022). Such collective experiences, along with higher rates of death and disease related to COVID in people of color generally, are examples of racial traumas which are thought to have a negative impact for overall health through chronic and repeated exposure to stress (Comas-Díaz et al., 2019; Liu and Modir, 2020). PC might be an important mechanism here, as it might allow past stressors (e.g., racial traumas) to remain cognitively present and thus detrimental for health (Ottaviani et al., 2016; Verkuil et al., 2010; Williams et al., 2017). Finally, future research should consider the social determinants of health in relation to PC as they are associated with COVID-19 pandemic-related health disparities and may be a source of worry for many people of color (Dalsania et al., 2022).
4. Conclusions
The COVID-19 pandemic has presented a substantial threat to mental health and well-being (Ettman et al., 2020; Luo et al., 2020; Pappa et al., 2020; Salari et al., 2020; Vindegaard and Benros, 2020), with people of color, who have borne the economic brunt of the pandemic, experiencing higher pandemic-related morbidity and mortality rates relative to White individuals (Centers for Disease Control, 2021; Couch et al., 2020; Kandil et al., 2020). We examined racial/ethnic differences in PC—specifically worry related to COVID-19--to shed light on racial disparities in mental health and well-being at the onset of the pandemic. We present early empirical data to suggest COVID-19-related PC was greater among people of color relative to White individuals. Such mental health disparities highlight potential “early predictors” of COVID-19-related health disparities that could inform public health responses to mitigate risk in communities of color. Forthcoming prospective studies must work to understand whether and how pandemic-related PC at the onset is associated with downstream mental and physical health in people of color.
Author contributions
Conceptualization: DPW, NMJ, EAH; Data curation and analysis: NMJ; Funding: EAH; Supervision: EAH; Visualization: NMJ; Writing original draft: DPW, NMJ; Substantive writing, reviewing, and editing: EAH; NMJ; DPW.
Acknowledgements and Sources of Funding
Funding for this study was provided by U.S. National Science Foundation RAPID grant SES 2026337 to Roxane Cohen Silver, E. Alison Holman, and Dana Rose Garfin; a UC Irvine COVID-19 Basic, Translational and Clinical Research Funding Award to E. Alison Holman and Roxane Cohen Silver, and a UC Irvine Office of Inclusive Excellence Advancing Equity Faculty Award to E. Alison Holman and Dewayne Williams. We thank Drs. Roxane Cohen Silver and Dana Rose Garfin for their support with study funding, design, and administration. Authors would like to thank the NORC AmeriSpeak team of J. Michael Dennis and David Reisner for their survey research and sampling guidance, for preparation of the online surveys, and for preparation of the data files. We also thank Rebecca R. Thompson, Daniel Relihan, Emma Grisham, and Kayley Estes for their contributions to the larger project from which these data were drawn. NSF Grant # SES-2049932 for Roxane C. Silver, E. Alison Holman, and Dana R. Garfin.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.115105.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Brosschot J.F., Gerin W., Thayer J.F. The perseverative cognition hypothesis: a review of worry, prolonged stress-related physiological activation, and health. J. Psychosom. Res. 2006;60(2):113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Brosschot J.F., Verkuil B., Thayer J.F. Generalized Unsafety Theory of Stress: unsafe environments and conditions, and the default stress response. Int. J. Environ. Res. Publ. Health. 2018;15(3):1–27. doi: 10.3390/ijerph15030464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control . Centers for Disease Control and Prevention; 2021. Coronavirus Disease 2019 (COVID-19)https://www.cdc.gov/coronavirus/2019-ncov/index.html [Google Scholar]
- Comas-Díaz L., Hall G.N., Neville H.A. Racial trauma: theory, research, and healing: introduction to the special issue. Am. Psychol. 2019;74(1):1–5. doi: 10.1037/amp0000442. [DOI] [PubMed] [Google Scholar]
- Couch K.A., Fairlie R.W., Xu H. Early evidence of the impacts of COVID-19 on minority unemployment. J. Publ. Econ. 2020;192 doi: 10.1016/j.jpubeco.2020.104287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Rajaratnam S.M. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. CDC Morbidity and Mortality Weekly Report (MMWR) 2020;69(32):1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalsania A.K., Fastiggi M.J., Kahlam A., Shah R., Patel K., Shiau S., DallaPiazza M. The relationship between social determinants of health and racial disparities in COVID-19 mortality. J. Racial Ethn. Health Dispar. 2022;9(1):288–295. doi: 10.1007/s40615-020-00952-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher K.A., Nguyen N., Crawford S., Fouayzi H., Singh S., Mazor K.M. Preferences for COVID-19 vaccination information and location: associations with vaccine hesitancy, race and ethnicity. Vaccine. 2021;39(45):6591–6594. doi: 10.1016/j.vaccine.2021.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher C.B., Tao X., Yip T. The Effects of COVID-19 Victimization Distress and Racial Biason Mental Health Among AIAN, Asian, Black, and Latinx Young Adult. Cult. Divers Ethnic Minor. Psychol. 2022 doi: 10.1037/cdp0000539. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma: Theor. Res. Pract. Pol. 2020;12(S1):S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel Coronavirus (COVID-19) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39:355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg S., Kim L., Whitaker M., et al. CDC Morbidity and Mortality Weekly Report (MMWR) 2020. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1-30.https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e3.htm 2020 Apr 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hisler G.C., Twenge J.M. Sleep characteristics of US adults before and during the COVID-19 pandemic. Soc. Sci. Med. 2021;276:113849. doi: 10.1016/j.socscimed.2021.113849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman E.A., Silver R.C., Poulin M., Andersen J., Gil-Rivas V., McIntosh D.N. Terrorism, acute stress, and cardiovascular health: a 3-year national study following the September 11th attacks. Arch. Gen. Psychiatr. 2008;65:73–80. doi: 10.1001/archgenpsychiatry.2007.6. [DOI] [PubMed] [Google Scholar]
- Holman E.A., Thompson R.R., Garfin D.R., Silver R.C. The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the U.S. Sci. Adv. 2020 doi: 10.1126/sciadv.abd5390. eabd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs M., Burch A.E. Anxiety during the pandemic: racial and ethnic differences in the trajectory of fear. J. Affect. Disord. 2021;292:58–66. doi: 10.1016/j.jad.2021.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation . Kaiser Family Foundation; 2021. KFF COVID-19 Vaccine Monitor.https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/ [Google Scholar]
- Kandil E., Attia A.S., Youssef M.R., Hussein M., Ibraheem K., Abdelgawad M., Al-Qurayshi Z., Duchesne J. African Americans struggle with the current COVID-19. Ann. Surg. 2020;272(3):e187–e190. doi: 10.1097/SLA.0000000000004185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni N. The impact of the COVID-19 pandemic on marginalized populations in the United States: a research agenda. J. Vocat. Behav. 2020;119:103439. doi: 10.1016/j.jvb.2020.103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S.R., Modir S. The outbreak that was always here: Racial trauma in the context of COVID-19 and implications for mental health providers. Psychol. Trauma: Theor. Res. Pract. Pol. 2020;12(5):439–442. doi: 10.1037/tra0000784. [DOI] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public –- A systematic review and meta-analysis. Psychiatr. Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey K., Ayers C.K., Kondo K.K., Saha S., Advani S.M., Young S., Kansagara D. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: A systematic review. Annals of internal medicine. 2021;174(3):362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novacek D.M., Hampton-Anderson J.N., Ebor M.T., Loeb T.B., Wyatt G.E. Mental health ramifications of the COVID-19 pandemic for Black Americans: clinical and research recommendations. Psychol. Trauma: Theor. Res. Pract. Pol. 2020;12(5):449–451. doi: 10.1037/tra0000796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottaviani C., Thayer J.F., Verkuil B., Lonigro A., Medea B., Couyoumdjian A., Brosschot J.F. Physiological concomitants of perseverative cognition: a systematic review and meta-analysis. Psychol. Bull. 2016;142(3):231–259. doi: 10.1037/bul0000036. [DOI] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; 2021. R: A Language and Environment for Statistical Computing.https://www.R-project.org/ [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selden T.M., Berdahl T.A. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition: study examines potential explanations for racial-ethnic disparities in COVID-19 hospitalizations and mortality. Health Aff. 2020;39(9):1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- Silge J., Robinson D. tidytext: text mining and analysis using tidy data principles in R. J. Open Sour. Softw. 2016;1(3):1–3. doi: 10.21105/joss.00037. [DOI] [Google Scholar]
- Thayer J.F., Sternberg E. Beyond heart rate variability: vagal regulation of allostatic systems. Annals of the New York Academy of Sciences. 2006;1088(1):361–372. doi: 10.1196/annals.1366.014. [DOI] [PubMed] [Google Scholar]
- Thompson R.R., Jones N.M., Holman E.A., Silver R.C. Media exposure to mass violence events can fuel a cycle of distress. Sci. Adv. 2019;5(4) doi: 10.1126/sciadv.aav3502. eaav3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkuil B., Brosschot J.F., Gebhardt W.A., Thayer J.F. When worries make you sick: a review of perseverative cognition, the default stress response and somatic health. J. Exper. Psychopathol. 2010;1(1):87–118. doi: 10.5127/jep.009110. [DOI] [Google Scholar]
- Vince R.A. Eradicating racial injustice in medicine–If not now, when? JAMA. 2020;324(5):451–452. doi: 10.1001/jama.2020.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virani S.S., Alonso A., Benjamin E.J., Bittencourt M.S., Callaway C.W., Carson A.P., Chamberlain A.M., Chang A.R., Cheng S., Delling F.N., others Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- Williams D.P., Feeling N.R., Hill L.K., Spangler D.P., Koenig J., Thayer J.F. Resting heart rate variability, facets of rumination and trait anxiety: implications for the Perseverative Cognition Hypothesis. Front. Hum. Neurosci. 2017;11(520):1–10. doi: 10.3389/fnhum.2017.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.P., Koenig J., Carnevali L., Sgoifo A., Jarczok M.N., Sternberg E.M., Thayer J.F. Heart rate variability and inflammation: a meta-analysis of human studies. Brain Behav. Immun. 2019;80:219–226. doi: 10.1016/j.bbi.2019.03.009. [DOI] [PubMed] [Google Scholar]
- Wu C., Qian Y., Wilkes R. Anti-Asian discrimination and the Asian-white mental health gap during COVID-19. Ethn. Racial Stud. 2021;44(5):819–835. doi: 10.1080/01419870.2020.1851739. [DOI] [Google Scholar]
- Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- Yip T., Feng Y., Fowle J., Fisher C.B. Sleep disparities during the COVID-19 pandemic: an investigation of AIAN, Asian, Black, Latinx, and White young adults. Sleep Health. 2021;7(4):459–467. doi: 10.1016/j.sleh.2021.05.008. [DOI] [PubMed] [Google Scholar]
- Yip T., Chung K., Chae D.H. Vicarious racism, ethnic/racial identity, and sleep among Asian Americans. Cult. Divers Ethnic Minor. Psychol. 2022 doi: 10.1037/cdp0000534. Advance online publication. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.