Abstract
Purpose:
Maternal trauma has been linked with problematic parenting, including both harsh and permissive behaviors. However, little is known about mechanisms accounting for this association. The current study examined the potential impact of posttraumatic stress disorder (PTSD) and emotion regulation on dysfunctional parenting behaviors in a sample of community mothers. We hypothesized a mediation model wherein PTSD would be associated with dysfunctional parenting (i.e., lax and overreactive behaviors) indirectly through deficits in maternal emotion regulation.
Method:
Seventy-eight community mothers of 18- to 36-month-old children were administered the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) and 19 mothers met criteria for PTSD. Mothers also completed self-report measures of difficulties with emotion regulation and maternal laxness and overreactivity in parenting.
Results:
Results revealed that emotion dysregulation fully mediated relations between PTSD status and lax (but not overreactive) parenting behaviors. Compared to mothers without PTSD, those with PTSD reported greater lax parenting behaviors indirectly through greater emotion dysregulation.
Conclusions:
Mothers with PTSD may struggle to parent assertively when trauma symptoms interfere with emotion regulation abilities. The current study highlights the need to design interventions focused on helping trauma-exposed mothers manage distress, ultimately aiming to enhance parenting effectiveness and improve child outcomes.
Keywords: Emotion regulation, family, lax, mothers, permissive, parenting, posttraumatic stress disorder, trauma
Although a greater proportion of men than women experience traumatic events (61% versus 51%, respectively), the lifetime rate of PTSD is approximately twice as high among women (10% of women compared to 5% of men; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Moreover, data from the National Comorbidity Study show that nearly three-quarters of individuals meeting criteria for PTSD are mothers (Nicholson, Biebel, Williams, & Katz-Leavy, 2002). This figure is concerning, in part, because of the potential systemic impact of PTSD that can extend to survivors’ interpersonal relationships (e.g., Monson, Fredman, & Dekel, 2010), which include impaired parent-child interactions among adults with PTSD (e.g., Creech & Misca, 2017; DiLillo & Damashek, 2003; Leen-Feldner, Feldner, Bunaciu, & Blumenthal, 2011). However, relatively little research has examined factors that may mediate relations between maternal PTSD and parenting difficulties. The present study addresses this gap by examining the possible impact of PTSD on mothers’ discipline strategies with young children and investigating emotion dysregulation as a mechanism that may account for this association.
Emotion Regulation and Parenting
Child noncompliance is a normative aspect of toddlerhood, emerging as children begin to assert greater agency and autonomy (Kuczynski & Kochanska, 1990), and necessitating parent competence in managing conflictual interactions. Dix’s (1991) seminal model of parenting identifies three key components motivating parent competence, at the heart of which is emotion regulation. This model posits that (a) child behavior and contextual factors (e.g., high-stress, low-support environments) influence (b) parent emotion regulation, which in turn (c) motivates parents to engage in certain parenting behaviors. Interactions in which parents must manage child behavior they experience as aversive often evoke negative parental emotions (Dix, 1991; Lorber, 2007), and difficulties regulating these emotions may increase or inhibit particular parenting strategies (Dix, 1991; Lorber & Slep, 2005). Responding effectively to instances of noncompliance requires parents to manage their own feelings and reactions to prioritize their child’s wellbeing (e.g., calmly redirecting a child instead of yelling). In the absence of effective emotion regulatory skills, maladaptive parenting responses make take different forms. Maternal emotion dysregulation may lead to lax discipline behaviors due to mothers feeling the need to distance from their own emotions and avoid challenging child behaviors; alternatively, emotion dysregulation may lead to harsh discipline behaviors due to mothers feeling emotionally overwhelmed and thus responding to their child’s behavior in a hostile manner to gain quick compliance.
Effective emotion regulation is a prerequisite to adaptive parenting responses to child misbehavior (e.g., Deater-Deckard, Sewell, Petrill, & Thompson, 2010; Lorber, 2012). Recent reviews document linkages between effective emotion regulation and positive parenting (e.g., Crandall, Deater-Deckard, & Riley, 2015; Crandall, Ghazarian, Day, & Riley, 2016; Zalewski, Lewis, & Martin, 2018). Parenting behaviors that emphasize support and consistent instruction—behaviors indicative of good emotion regulation (Crandall et al., 2015)—are associated with positive child behavior and adjustment (Amato & Fowler, 2002). In contrast, parenting behaviors that communicate harshness or permissiveness (e.g., displays of anger or irritation, allowing rules to go unenforced; Arnold, O’Leary, Wolff, & Acker, 1993) can heighten child noncompliance in ways that persist and evolve into aggression and destructiveness over time (Campbell, Shaw, & Gilliom, 2000).
PTSD and Emotion Dysregulation
Aligned with Dix’s (1991) view that factors giving rise to parent emotion dysregulation might undermine effective parenting, PTSD may pose unique challenges to parent competence through its influence on emotion dysregulation. PTSD is characterized by a persistent sense of current threat that results in experiential, emotional, and behavioral avoidance, as individuals attempt to limit their own exposure to emotionally evocative cues (Foa & Rothbaum, 1998). However, these avoidance patterns are associated with a paradoxical increase in emotional distress (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996), as well as greater unpredictability of mood states (Kashdan, Uswatte, Steger, & Julian, 2006; Orsillo, Batten, Plumb, Luterek, & Roessner, 2004), lower distress tolerance (e.g., Vujanovic, Bonn-Miller, Potter, Marshall, & Zvolensky, 2011), and more intense emotional and physiological responses to negative stimuli (e.g., McDonagh-Coyle et al., 2001; Veazey, Blanchard, Hickling, & Buckley, 2004). Thus, mothers with PTSD may struggle to identify, tolerate, and respond to intense emotional arousal in ways needed to manage child misbehavior.
PTSD and Parenting
Consistent with the above possibilities, survey and observational data reveal positive relations between PTSD symptom severity and dysfunctional parenting behaviors (e.g., Ammerman, Putnam, Chard, Stevens, & Van Ginkel, 2012; Hershkowitz, Dekel, Fridkin, & Freedman, 2017; Leen-Feldner et al., 2011; van Ee, Kleber, & Mooren, 2012). For example, researchers found a positive association between parental PTSD and moderate physical aggression toward children after accounting for socioeconomic status and other psychopathology (Leen-Feldner et al., 2011). Similarly, observations of interactions between asylum seekers and their children reveal positive associations between PTSD severity and insensitive, unstructured, and hostile parenting behaviors during free play (van Ee et al., 2012). Although several studies suggest that mothers exposed to trauma, including those who do not go on to develop significant psychopathology, may compensate for the potential effects of trauma by increasing positive parenting behaviors (e.g., Casaneuva, Martin, Runyan, Barth, & Bradley, 2008; Letourneau, Fedick, & Willms, 2007; Levendosky & Graham-Bermann, 2000; Levendosky, Huth-Bocks, Shapiro, & Semel, 2003), most literature points to PTSD as having a detrimental impact on parent-child relations (see Creech & Misca, 2017 and van Ee, Kleber, & Jongmans, 2015 for reviews).
Despite growing evidence linking PTSD to both parenting difficulties and emotion dysregulation (e.g., McDonagh-Coyle et al., 2001), as well as findings that emotion dysregulation undermines parenting behaviors (e.g., Lorber, 2012), scant research has examined whether emotion dysregulation mediates the link between PTSD and parenting. The present study addresses this gap in knowledge and addresses other limitations found in prior literature. First, most studies to date focus on specific trauma-exposed populations (e.g., combat veterans, mothers exposed to intimate partner violence); less is known about whether community samples of mothers with diverse trauma experiences are similarly affected. Second, in most prior work, PTSD symptoms and potential diagnoses are inferred from responses to symptom checklists. However, diagnostic interviewing methods, considered the gold standard approach to assessing PTSD (Wisco, Marx, & Keane, 2012), may facilitate more precise measurement of symptoms, and thus more accurate diagnoses. The present study addresses these limitations by utilizing a diagnostic interview to more rigorously assess PTSD in a community sample of mothers with diverse trauma experiences.
Aims and Hypotheses
In sum, prior literature suggests PTSD may contribute to dysfunctional parenting behaviors among parents and emotion regulation associated with PTSD may be an important mechanism through which these parenting difficulties occur. The goal of the present study was to test these possibilities by examining emotion regulation as a mediator of the association between PTSD and maternal parenting behaviors. First, we expected that mothers meeting diagnostic criteria for PTSD would report more dysfunctional parenting, as exhibited by greater lax and harsh parenting behaviors. Second, drawing on prior theory and research, we predicted that higher levels of emotion dysregulation associated with a diagnosis of PTSD would be associated with increased levels of both harsh and lax parenting behaviors. Finally, we expected that poorer emotion regulation would mediate the relation between PTSD and both lax and harsh parenting behaviors.
Method
Participants
Participants were 78 adult mothers of toddler-aged children recruited from a medium-sized Midwestern city. Mothers ranged in age from 21 to 45 years (M = 32.98; SD = 5.37). The majority of mothers identified as White (n = 71; 91%), while 6% (n = 5) identified as multiracial and 3% (n = 2) identified as Asian. Approximately 6% (n = 5) of mothers identified as Hispanic/Latina. Taken together, 15% (n = 12) of mothers identified with either a racial or ethnic minority group. Most mothers were married (n = 61; 78%) or currently in a romantic relationship (13%; n = 10). The majority were employed outside the home (n = 60; 77%), and 47% (n = 37) reported having bachelor’s degree. The modal combined family income was over $100,000 (n = 18), but ranged with approximately 47% (n = 37) of the sample earning at or below an income of $60,000.
Procedures
Recruitment.
Participants were part of a larger study examining the impact of PTSD on parenting among mothers and their 18- to 36-month-old children. Recruitment of mother-child dyads for the larger study occurred primarily through archived birth announcements published in the local newspaper. These birth announcements are provided to the newspaper by each hospital in the county and therefore reflect all the hospital births of children from the recruitment area. Using publically available contact information for parents listed in the birth announcements, potential participants were mailed letters inviting them to participate in a study of “parent-child interactions.” A total of 52 mothers were recruited via their children’s birth announcements; 16 mothers were recruited via flyers posted in daycares, community centers, grocery stores, and libraries; and remaining mothers were recruited via word of mouth (n = 4), university websites and listservs (n = 3), and Craigslist advertisements (n = 3). Mothers received $10 compensation after completing the 30-minute online survey and $15 per hour during the lab portion of the study.
Initial screening and data collection.
Mothers who responded to recruitment letters or advertisements were asked complete an online version of the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013a) followed by the PTSD Checklist for DSM-5 (PCL-5; Blevins, Weathers, Davis, Witte, & Domino, 2015). Oversampling was used during recruitment to ensure a sufficient number of participants had experienced trauma and PTSD. Eligible mothers were scheduled for a single lab visit. Upon arrival, mothers underwent informed consent procedures and then completed a demographics questionnaire, the CAPS-5 interview, measures of parenting and emotion dysregulation, and a series of additional tasks relevant to the larger study from which these data were drawn. Pregnant women were excluded from participation due to alterations in cortisol hormones occurring during pregnancy (Nolten, Lindheimer, Rueckert, Oparil, & Ehrlich, 1980), a variable relevant to the larger study. Steps were taken to minimize risk, including carefully obtaining informed consent, offering all participants referral information for trauma-specific treatment, and providing thorough debriefing about the purposes of the study. The university’s Institutional Review Board approved all study methods.
Measures
Demographics.
Mothers completed a demographics survey including questions about their age, race, ethnicity, total yearly household income, and highest level of education.
PTSD classification.
Mothers who reported a Criterion A trauma on the LEC-5 (Weathers et al., 2013a) were administered the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013b). The CAPS-5 was used for the final classification of participants into PTSD or no PTSD groups. The CAPS-5 produces a current (past month) diagnosis, symptom cluster severity, and overall symptom severity. The measure has strong interrater reliability (κ = .78 to 1.00 depending on scoring rule) and good test-retest reliability (ICC = .78), as well as strong convergent validity with related measures (e.g., CAPS-IV, PCL-5, anxiety, functional impairment; Weathers et al., 2017).
Self-reported parenting behaviors.
To examine overreactive and lax parenting behaviors, mothers completed the Parenting Scale (Arnold, O’Leary, Wolff, & Acker, 1993). The Parenting Scale is a self-report measure in which parents rate their tendencies to engage in overreactive (10 items), lax (11 items), and verbose (7 items) discipline techniques. For the purpose of the current study, we only examined the overreactive and lax discipline items. Overreactive styles reflect the intensity and frequency of responding to child misbehavior in a hostile manner either verbally (e.g., yelling) or physically (e.g., grabbing an arm), while lax styles reflect the intensity and frequency of “giving in” to child misbehavior. Sample items from these scales include, “If my child gets upset, I back down and give in,” and “I raise my voice or yell,” for lax and overreactive discipline, respectively. Responses are coded on a 7-point Likert format scale (i.e., 1 = frequent use of effective discipline strategies to 7 = frequent use of discipline mistakes) and yield a continuous score. Research indicates convergent validity between discipline behaviors in both observed and self-report measures of overreactive (r = .61) and lax parenting behaviors (r = .65; Arnold, O’Leary, Wolff, & Acker, 1993), as well as high interrater reliability (rs ranging from .86 to .91; Arnold & O’Leary, 1995). In the current study, mean overreactive parenting was 24.96 (SD = 7.28; range 10–70) and mean lax parenting was 28.73 (SD = 9.14; range 11–77). The alpha coefficients across both scales were respectable (overreactive discipline α = .79; lax discipline α = .82).
Emotion regulation.
To assess emotion regulation, mothers completed the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004). The DERS is a 36-item self-report questionnaire that measures overall emotion regulation, as well as six specific subscales (i.e., non-acceptance of emotional responses, difficulty engaging in goal-directed behavior, impulse control difficulties, lack of emotional awareness, limited access to emotion regulation strategies, lack of emotional clarity). Sample items include, “When I’m upset, I lose control over my behavior,” and “When I’m upset, I have difficulty thinking about anything else.” Responses are coded on a 5-point Likert format scale (i.e., 1 = almost never to 5 = almost always) and yield a continuous score. Research indicates adequate construct and predictive validity of the DERS (Gratz & Roemer, 2004). For the purpose of the current study, items were summed across subscales and internal consistency was respectable (α = .85).
Child behavior problems.
Child internalizing and externalizing symptoms were assessed with the Child Behavior Checklist for Ages 1.5 to 5 (CBCL; Achenbach & Rescorla, 2000). Items were summed to create a total score and internal consistency was high (α = .92). The CBCL total score was included as a covariate in analyses.
Data Analytic Plan
Power considerations.
Statistical power for testing the models relevant to the larger study from which these data were drawn was estimated a priori using a Monte Carlo simulation (Muthén & Muthén, 1998–2017; Thoemmes, Mackinnon, & Reiser, 2010). These results indicated that 75 mother-child dyads would be sufficient for testing each of those proposed models, assuming medium effect sizes and power > .80). Although statistical power was not estimated a priori for these secondary data analyses, it is worth noting that the larger study aimed to test more complex models (i.e., a model with two predictors and two mediators), suggesting that the sample size is more than adequate for the present investigation.
Data screening.
Screening of the data revealed normal distributions and no missing data on any primary variables of interest. Frequencies and means were calculated for sample demographics, followed by bivariate correlations, which were conducted to determine associations among constructs of interest and identify potentially important covariates. Several demographic variables (i.e., maternal age, minority status, household income, educational attainment) and child characteristics (i.e., child age, child sex) were examined, but only household income and mother’s education level were identified for inclusion as covariates by virtue of their significant associations with PTSD status and emotion regulation. Specifically, mothers with lower household incomes were more likely to have PTSD (r = −0.39, p = .001) and report poorer emotion regulation (r = −0.32, p = .004). Additionally, mothers with lower educational attainment were more likely to report poorer emotion regulation (r = −0.29, p = .011). Child behavior problems (internalizing and externalizing symptoms assessed with the CBCL; Achenbach & Rescorla, 2000) were also associated with poorer maternal emotion regulation (r = 0.38, p = .001), as well as maternal overreactivity (r = 0.36, p = .001), and therefore was statistically controlled to account for differences in parenting attributable to child effects. We adjusted for these covariates by regressing our outcome variables (maternal laxness, overreactivity), as well as our mediator (maternal emotion regulation), on household income, educational attainment, and child behavior problems.
Hypothesis testing.
Next, using Mplus 8.1 (Muthén & Muthén, 1998–2017), we tested our primary hypotheses focusing on the direct and indirect effects of PTSD on maternal parenting behaviors (i.e., laxness and overreactivity) as mediated though emotion dysregulation. Here, we employed Hayes’ (2017) mediation criteria such that the inference of indirect effects should be based on the product of paths a and b (i.e., ab), as opposed to the individual hypothesis tests of a and b separately. Because the product of ab can be significantly different from zero even when a and b are not statistically significant, statistical significance of both a and b as separate entities are not requirements of mediation (Hayes, 2017, p. 116). Through this approach, a bias-corrected bootstrap technique with 5,000 resamples was used to derive the 95% CIs for direct and indirect effects. This non-parametric resampling method accounts for non-normal distribution of indirect effects and performs well in small samples by maximizing power while minimizing Type 1 error rate (Shrout & Bolger, 2002). Based on the number of paths, the model was just-identified (i.e., zero degrees of freedom). As global fit indices do not apply to just-identified models, only local fit indices are reported.
Results
Preliminary Analyses
Recruitment efforts resulted in a final sample of 19 mothers meeting criteria for PTSD and 59 who did not meet criteria for PTSD. Participants with PTSD identified a range of events on the LEC-5 as their “worst” index trauma, including physical and/or sexual domestic violence (n = 5; 26.3%), physical and/or sexual child abuse (n = 4; 21.1%), sexual assault by a stranger or friend (n = 2; 10.5%), transportation accident (n = 1; 5.3%), kidnapping/captivity (n = 1; 5.3%), exposure to a war-zone (n = 1; 5.3%), experiencing life-threatening illness/injury (n = 1; 5.3%), witnessing a life threatening illness/injury (n = 2; 10.5%), learning about a loved one’s sexual assault (n = 1; 5.3%), and learning about a sudden violent death (n = 1; 5.3%). Participants with PTSD received an average severity score of 31.95 (SD = 8.95).
Bivariate Relations
Bivariate correlations were estimated using Pearson’s formula. As expected, PTSD status significantly correlated with greater emotion dysregulation (r = .29, p < .01). Greater emotion dysregulation significantly correlated with greater maternal laxness (r = .38, p < .01), as well as greater overreactivity (r = .28, p < .05). Surprisingly, PTSD status was not significantly associated with either maternal laxness or overreactivity. All variables were sufficiently distinct (rs < .70), and thus there were no concerns about multicollinearity (Tabachnick & Fidell, 1996).
Path Analyses
Lax parenting.
As shown in Figure 1, among mothers with PTSD, compared to those without PTSD, results indicated a nonsignificant direct path from PTSD status to maternal laxness, b = 2.08, SE = 2.75, 95% CI [−3.44, 7.35]. PTSD status did not predict greater emotion dysregulation, b = 8.90, SE = 5.28, 95% CI [−0.94, 19.50]; however, greater emotion dysregulation significantly predicted higher maternal laxness, b = 0.15, SE = 0.07, 95% CI [0.03, 0.29]. Further, PTSD status was significantly related to higher maternal laxness indirectly through greater emotion dysregulation, b = 1.34, SE = 1.00, 95% CI [0.05, 4.49], thus meeting criteria for mediation. Regarding the covariates, child behavior problems was significantly associated with greater emotion dysregulation, b = 0.35, SE = 0.15, 95% CI [0.08, 0.66]. The model accounted for 21% of the variance in emotion dysregulation and 16% of the variance in lax parenting.
Figure 1.
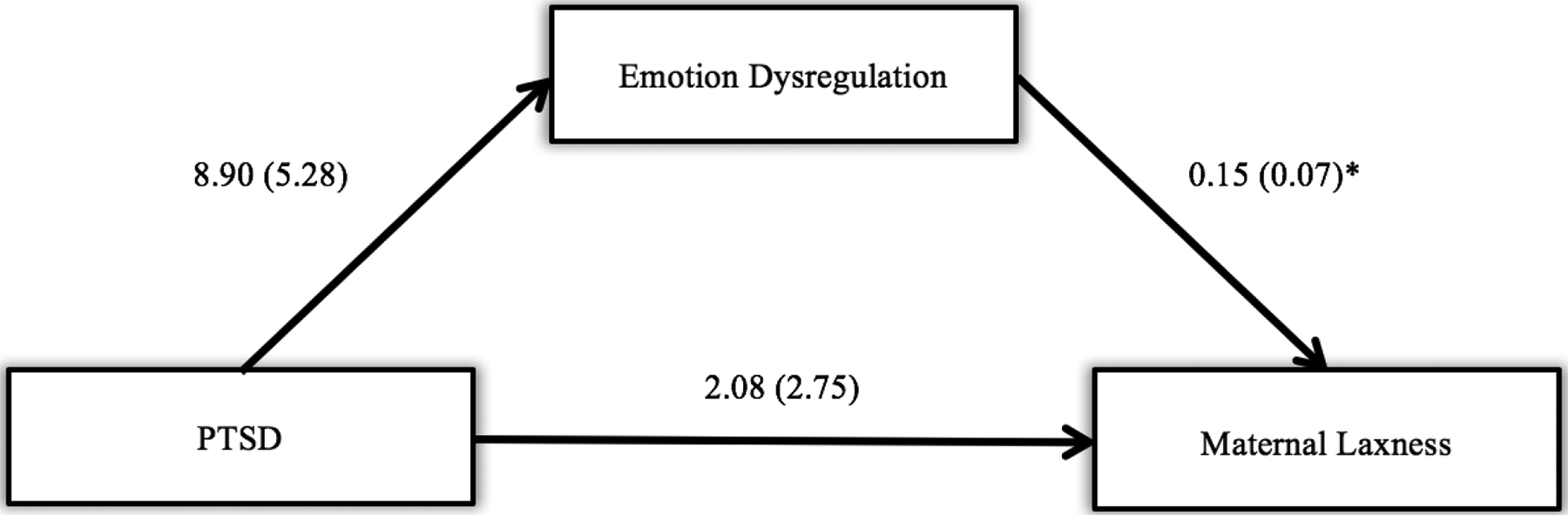
Unstandardized regression coefficients (b) and standard errors (SE) in path model depicting the influence of PTSD diagnosis and emotion dysregulation on maternal laxness. PTSD status was significantly related to higher maternal laxness indirectly through greater emotion dysregulation, b = 1.34, SE = 1.00, 95% CI [0.05, 4.49]. Estimates with asterisks are significant at p < .05.
Overreactive parenting.
Among mothers with PTSD, results indicated a nonsignificant direct path from PTSD status to maternal overreactivity, b = −1.39, SE = 2.42, 95% CI [−5.77, 3.77]. PTSD status did not predict greater emotion dysregulation, b = 8.89, SE = 5.28, 95% CI [−0.96, 17.78], and greater emotion dysregulation did not significantly predict higher maternal overreactivity, b = 0.07, SE = .04, 95% CI [−0.01, 0.16]. Further, PTSD status was not significantly related to maternal overreactivity indirectly through emotion dysregulation, b = 0.58, SE = 0.56, 95% CI [−0.51, 2.41], thus not meeting criteria for mediation. Regarding the covariates, child behavior problems was significantly associated with greater emotion dysregulation b = 0.35, SE = 0.15, 95% CI [0.08, 0.66], and greater overreactive parenting behaviors, b = 0.12, SE = 0.06, 95% CI [0.00, 0.25].
Discussion
The goal of this study was to examine whether PTSD predicted maternal parenting behaviors, as well as the possible mechanistic role of emotion dysregulation in explaining this association. Contrary to expectations, there was no direct association between PTSD status and self-reported dysfunctional parenting behaviors. However, results revealed an indirect effect of maternal PTSD on lax (but not overreactive) parenting behaviors through greater emotion dysregulation. We discuss the implications of these findings below.
PTSD and dysfunctional parenting.
Our finding that PTSD status was not directly associated with either lax or overreactive parenting contrasts with prior work linking PTSD to negative parenting outcomes (e.g., Leen-Feldner et al., 2011; van Ee et al., 2012). Nevertheless, other literature suggests that mothers exposed to trauma may compensate for the adverse impact of these events by increasing their focus on effective parenting behaviors, such as positive discipline, sensitivity, and consistency (e.g., Casaneuva et al., 2008; Letourneau, Fedick, & Willms, 2007; Levendosky & Graham-Bermann, 2000). Some of the trauma-exposed mothers in the present study may similarly have tried to offset the systemic impact of their trauma history through increased focus on positive parenting behaviors. Our sample was also characterized by a relatively high level of socioeconomic status and education, both of which may serve as protective factors against parenting difficulties (e.g., Neitzel & Stright, 2004; Pinderhughes, Dodge, Bates, Pettit, & Zelli, 2000), even among mothers with PTSD. For example, these mothers may have access to resources (e.g., counseling services, social support from family and friends) that could buffer the potential impact of PTSD on their parenting behaviors—a possibility supported by findings that better access to resources is associated with more effective parenting practices (Kotchick & Forehand, 2002). Alternatively, mothers concerned with impression management may have underreported negative behaviors on the self-report parenting measure used here (i.e., social desirability effects). If mothers internalized societal pressures and attempted to depict themselves in an idealized fashion, this could have resulted in the minimizing of parenting difficulties (see Morsbach & Prinz, 2006 and Schaeffer, 2000 for discussions).
PTSD, emotion regulation, and lax parenting.
As predicted, greater emotion dysregulation mediated associations between PTSD status and greater lax parenting. Results are consistent with prior work linking PTSD to greater emotion dysregulation (e.g., Orsillo et al., 2004, McDonagh-Coyle et al., 2001; Veazey, Blanchard, Hickling, & Buckley, 2004), and complements a recent study of mothers of older children, which found that emotion dysregulation mediated the association between PTSD and supportive parenting reactions (Gurtovenko & Katz, 2017). However, multiple prior studies of community samples (without regard to trauma history) have not found support for the link between parental negative emotion and permissive parenting behaviors, concluding that maternal emotion regulation may be less relevant for lax discipline (Leung & Slep, 2006; Lorber & Slep, 2005; Lorber, 2012). The present findings align more with early research linking maternal trauma to permissive parenting, possibly as a result of mothers having diminished emotional resources to enforce discipline or communicate consistent behavioral expectations to their children (see DiLillo & Damashek, 2003 for a discussion). In particular, the avoidance and emotional numbing component of PTSD may have a particularly deleterious effect on the parent-child relationship (Samper et al., 2004). Together with present findings, work in this area suggests that PTSD may increase mothers’ tendency to avoid managing child misbehavior when greater levels of emotion regulation are needed for effective, approach-oriented discipline.
PTSD, emotion regulation, and overreactive parenting.
The lack of mediation between PTSD and overreactive parenting through emotion regulation was unexpected in light of prior work linking (a) PTSD to greater emotion dysregulation during emotionally evocative situations (e.g., McDonagh-Coyle et al., 2001; Veazey et al., 2004) and (b) poor emotion regulation to harsh parenting (e.g., Lorber, 2012). We did, however, find the expected bivariate associations between PTSD status and emotion dysregulation and between emotion dysregulation and both overreactive and lax parenting. Although PTSD status was not significantly associated with either maternal laxness or overreactivity, the strength of the correlation between PTSD and laxness (r = .21, p = .06) was substantially higher than that of PTSD and overreactivity (r =.04, p = .70). Moreover, some items on the Parenting Scale clearly reflect face-valid dysfunctional parenting practices (e.g., “When my child does something I don’t like, I insult my child, say mean things, or call my child names”), which may lead to underreporting of these behaviors due to social desirability bias. Future research could reduce these biases by using observational methods in which researchers measure actual parenting behaviors during routine discipline encounters.
Limitations
Although the current study contributes to prior knowledge about PTSD and parenting, its findings should be viewed in light of several limitations. First, the cross-sectional design precludes conclusions about causation and the temporal order of variables in our model. Further examination of PTSD, emotion regulation, and parenting outcomes in the context of a longitudinal study are needed to address these issues. Second, our sample was relatively small, ethnically homogenous, of higher socioeconomic status, and well-educated. It is possible that individuals from varying racial/ethnic and socioeconomic groups may experience PTSD and emotion regulation to differing degrees due to reduced access to mental health care and increased exposure to daily stressors (Myers, 2009; Santiago, Wadsworth, & Stump, 2011). Mothers in the current sample may have more such resources at their disposal, whereas mothers from disadvantaged backgrounds may lack access to myriad types of support (e.g., community networks, financial resources, educational environments; Kotchick & Forehand, 2002). Research has long documented associations between economic strain and increased behavioral problems among children via greater caregiver negative emotionality and harsher discipline practices among parents (see Evans, 2004 for a review). Future research should include a more demographically diverse sample to facilitate broader generalization of findings. In addition to the possible underreporting of parenting difficulties noted earlier, mothers who have difficulty regulating their emotions may also struggle to accurately report upon certain facets of emotion regulation. For example, individuals who have difficulty identifying their own affective states may misrepresent the intensity and frequency of their emotions on self-report questionnaires (Gratz & Roemer, 2004). Using observational or interview methods to more comprehensively assess emotion regulation and parenting behaviors may address this issue.
Future Directions
Future research is needed to better understand the role of PTSD in parenting difficulties. Like most work in this area, the current study focused on mothers; however, fathers are underrepresented in the parenting literature (e.g., Davison, Charles, Khandpur, & Nelson, 2017; Phares, Fields, Kamboukos, & Lopez, 2005), and initial work indicates that men with PTSD also experience parenting difficulties (Stover, Hall, McMahon, & Easton, 2012). More research is needed to fully understand the nature of parenting difficulties experienced by fathers and to identify the mechanisms underlying this relation. Second, our a priori hypotheses focused on global emotion regulation. However, emotional regulation can be conceptualized as a multidimensional construct involving the awareness, understanding, and acceptance of one’s emotions; the ability to control impulsive behaviors and engage in goal-directed behaviors when upset; and the flexible use of strategies to manage the intensity and duration of emotions in responses to specific situations (Gratz & Roemer, 2004). Thus, the present findings could be extended by examining specific facets of emotion regulation in relation to maternal PTSD and parenting behaviors. For example, mothers with impulse control difficulties may be more likely to struggle with managing overt displays of irritability (i.e., harsh parenting), whereas mothers with limited access to particular emotion regulation strategies might have difficulty modulating their distress in order to set limits on their children (i.e., lax parenting). Third, PTSD is likely to operate upon parenting via a variety of pathways and additional mechanisms may account for these associations. For instance, cross-sectional data suggest that parenting stress may mediate associations between PTSD and child outcomes (e.g., Samuelson, Wilson, Padrón, Lee, & Gavron, 2017). Certain trauma-related thoughts and beliefs (i.e., posttraumatic cognitions) are also known increase both PTSD symptoms (Foa, Ehlers, Clark, Tolin, & Orsillo, 1999; Mordeno, Carpio, Nalipay, & Saavedra, 2017) and parental distress (Tutus & Goldbeck, 2016), and thus could be important constructs of interest. In particular, preoccupation with negative cognitions related to the self (e.g., “I am unlovable”) may lead to ineffective parenting practices (i.e., permissive parenting) in an attempt to achieve greater closeness with one’s child. Finally, future research should examine moderators of the association between PTSD and parenting, which may be critical to enhancing effective parenting among mothers with PTSD. To name a few possibilities, perceived social support, close alliance with a mental health professional, and psychological resilience are all factors known to buffer the harmful effects of trauma on functional impairment (e.g., Charuvastra & Cloitre, 2008; Pietrzak et al., 2010).
Clinical Implications and Conclusion
The current study provides new information regarding the role that PTSD symptomology and emotion regulation might play in increasing dysfunctional parenting behaviors. Results suggest that mothers who have experienced a traumatic event resulting in PTSD may be at risk for problems with emotion regulation and, in turn, lax or permissive parenting behaviors. It is possible that permissive parenting reflects challenges in distress tolerance manifesting in difficulty withstanding the emotional distress associated with parenting (e.g., when needing to set firm boundaries with misbehaving children). For this reason, interventions centered around improving emotion regulation skills and interpersonal effectiveness (e.g., Dialectical Behavior Therapy [DBT]; Linehan, 1993a, 1993b), as well as skills training in managing child misbehavior (e.g., Parent-Child Interaction Therapy [PCIT]; Eyberg, 1988), may be used in tandem for helping mothers with PTSD persist with assertive parenting behaviors even when experiencing strong negative emotions. Coaching mothers with PTSD to respond more firmly to child misbehavior could increase parental effectiveness, as well as feelings of self-efficacy, and may ultimately improve long-term child outcomes.
References
- Achenbach TM, & Rescorla LA (2000). Child Behavior Checklist. Burlington, VT: ASEBA. [Google Scholar]
- Amato PR, & Fowler F (2002). Parenting practices, child adjustment, and family diversity. Journal of Marriage and Family, 64, 703–716. doi: 10.1111/j.1741-3737.2002.00703.x [DOI] [Google Scholar]
- Ammerman RT, Putnam FW, Chard KM, Stevens J, & Van Ginkel JB (2012). PTSD in depressed mothers in home visitation. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 186–195. doi: 10.1037/a0023062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold DS, O’Leary SG, Wolff LS, & Acker MM (1993). The Parenting Scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment, 5, 137–144. doi: 10.1037/1040-3590.5.2.137 [DOI] [Google Scholar]
- Arnold EH & O’Leary SG (1995). The effect of child negative affect on maternal discipline behavior. Journal of Abnormal Child Psychology, 23, 585–595. doi: 10.1007/BF01447663 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Campbell SB, Shaw DS, & Gilliom M (2000). Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Development and Psychopathology, 12, 467–488. Doi: 10.1017/S0954579400003114 [DOI] [PubMed] [Google Scholar]
- Casanueva C, Martin SL, Runyan DK, Barth RP, & Bradley RH (2008). Quality of maternal parenting among intimate-partner violence victims involved with the child welfare system. Journal of Family Violence, 23, 413–427. doi: 10.1007/s10896-008-9167-6 [DOI] [Google Scholar]
- Charuvastra A, & Cloitre M (2008). Social bonds and posttraumatic stress disorder. Annual Review of Psychology, 59, 301–328. doi: 10.1146/annurev.psych.58.110405.085650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall A, Deater-Deckard K, & Riley AW (2015). Maternal emotion and cognitive control capacities and parenting: A conceptual framework. Developmental Review, 36, 105–126. doi: 10.1016/j.dr.2015.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall A, Ghazarian SR, Day RD, & Riley AW (2016). Maternal emotion regulation and adolescent behaviors: The mediating role of family functioning and parenting. Journal of Youth and Adolescence, 45, 2321–2335. doi: 10.1007/s10964-015-0400-3 [DOI] [PubMed] [Google Scholar]
- Creech SK, & Misca G (2017). Parenting with PTSD: A review of research on the influence of PTSD on parent-child functioning in military and veteran families. Frontiers in Psychology, 8, 1101. doi: 10.3389/fpsyg.2017.01101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison K, Charles J, Khandpur N, & Nelson T (2017). Fathers’ perceived reasons for their underrepresentation in child health research and strategies to increase their involvement. Maternal & Child Health Journal, 21, 267–274. doi: 10.1007/s10995-016-2157-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deater-Deckard K, Sewell MD, Petrill SA, & Thompson LA (2010). Maternal working memory and reactive negativity in parenting. Psychological Science, 21, 75–79. doi: 10.1177/0956797609354073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLillo D, & Damashek A (2003). Parenting characteristics of women reporting a history of childhood sexual abuse. Child Maltreatment, 8, 319–333. doi: 10.1177/1077559503257104 [DOI] [PubMed] [Google Scholar]
- Dix T (1991). The affective organization of parenting: Adaptive and maladaptive processes. Psychological Bulletin, 110, 3–25. doi: 10.1037/0033-2909.110.1.3 [DOI] [PubMed] [Google Scholar]
- Evans GW (2004). The environment of childhood poverty. American Psychologist, 59, 77–92. doi: 10.1037/0003-066X.59.2.77 [DOI] [PubMed] [Google Scholar]
- Eyberg S (1988). Parent-child interaction therapy: Integration of traditional and behavioral concerns. Child & Family Behavior Therapy, 10, 33–46. doi: 10.1300/J019v10n01_04 [DOI] [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. doi: 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- Foa EB, & Rothbaum BO (1998). Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. New York, NY: Guilford Press. [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. doi: 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Gurtovenko K, & Katz LF (2017). Posttraumatic stress, mother’s emotion regulation, and parenting in survivors of intimate partner violence. Journal of Interpersonal Violence, 1–23. doi: 10.1177/0886260517690874 [DOI] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, & Strosahl K (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64, 1152–1168. doi: 10.1037/0022-006X.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). New York, NY: Guilford Publications. [Google Scholar]
- Hershkowitz M, Dekel R, Fridkin S, & Freedman S (2017). Posttraumatic stress disorder, parenting, and marital adjustment among a civilian population. Frontiers in Psychology, 8, 1655–1660. doi: 10.3389/fpsyg.2017.01655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Uswatte G, Steger MF, & Julian T (2006). Fragile self-esteem and affective instability in posttraumatic stress disorder. Behaviour Research and Therapy, 44, 1609–1619. doi: 10.1016/j.brat.2005.12.003 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kotchick BA, & Forehand R (2002). Putting parenting in perspective: A discussion of the contextual factors that shape parenting practices. Journal of Child and Family Studies, 11, 255–269. doi: 10.1023/A:1016863921662 [DOI] [Google Scholar]
- Kuczynski L, & Kochanska G (1990). Development of children’s noncompliance strategies from toddlerhood to age 5. Developmental Psychology, 26, 398–408. doi: 10.1037/0012-1649.26.3.398 [DOI] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Bunaciu L, & Blumenthal H (2011). Associations between parental posttraumatic stress disorder and both offspring internalizing problems and parental aggression within the National Comorbidity Survey-Replication. Journal of Anxiety Disorders, 25, 169–175. doi: 10.1016/j.janxdis.2010.08.017 [DOI] [PubMed] [Google Scholar]
- Letourneau NL, Fedick CB, & Willms JD (2007). Mothering and domestic violence: A longitudinal analysis. Journal of Family Violence, 22, 649–659. doi: 10.1007/s10896-007-9099-6 [DOI] [Google Scholar]
- Leung DW, & Slep AMS (2006). Predicting inept discipline: The role of parental depressive symptoms, anger, and attributions. Journal of Consulting and Clinical Psychology, 74, 524–534. doi: 10.1037/0022-006X.74.3.524 [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Huth-Bocks AC, Shapiro DL, & Semel MA (2003). The impact of domestic violence on the maternal-child relationship and preschool-age children’s functioning. Journal of Family Psychology, 17, 275–287. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Lynch SM, & Graham-Bermann SA (2000). Mothers’ perceptions of the impact of woman abuse on their parenting. Violence Against Women, 6, 247–271. [Google Scholar]
- Linehan MM (1993a). Skills training manual for treating borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Linehan MM (1993b). Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press [Google Scholar]
- Lorber MF (2007). Validity of video-mediated recall procedures for mothers’ emotion and child ratings. Journal of Family Psychology, 21, 520–528. doi: 10.1037/0893-3200.21.3.520 [DOI] [PubMed] [Google Scholar]
- Lorber MF (2012). The role of maternal emotion regulation in overreactive and lax discipline. Journal of Family Psychology, 26, 642–647. doi: 10.1037/a0029109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber MF, & Slep AMS (2005). Mothers’ emotion dynamics and their relations with harsh and lax discipline: Microsocial time series analyses. Journal of Clinical Child and Adolescent Psychology, 34, 559–568. doi: 10.1207/s15374424jccp3403_11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonagh-Coyle A, McHugo GJ, Friedman MJ, Schnurr PP, Zayfert C, & Descamps M (2001). Psychophysiological reactivity in female sexual abuse survivors. Journal of Traumatic Stress, 14, 667–683. doi: 10.1023/A:1013081803429 [DOI] [PubMed] [Google Scholar]
- Monson CM, Fredman SJ, & Dekel R (2010). Posttraumatic stress disorder in an interpersonal context. In Beck JG (Ed.), Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment (pp. 179–208). Washington, DC, US: American Psychological Association. doi: 10.1037/12084-007 [DOI] [Google Scholar]
- Mordeno IG, Carpio JGE, Nalipay MJN, & Saavedra RLJ (2017). PTSD’s underlying dimensions in typhoon Haiyan survivors: Assessing DSM-5 symptomatology-based PTSD models and their relation to posttraumatic cognition. Psychiatric Quarterly, 88, 9–23. doi: 10.1007/s11126-016-9429-z [DOI] [PubMed] [Google Scholar]
- Morsbach SK, & Prinz RJ (2006). Understanding and improving the validity of self-report of parenting. Clinical Child and Family Psychology Review, 9, 1–21. doi: 10.1007/s10567-006-0001-5 [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Myers HF (2009). Ethnicity-and socio-economic status-related stresses in context: An integrative review and conceptual model. Journal of Behavioral Medicine, 32, 9–19. doi: 10.1007/s10865-008-9181-4 [DOI] [PubMed] [Google Scholar]
- Nicholson J, Biebel K, Williams VF, & Katz-Leavy J (2002). Prevalence of parenthood in adults with mental illness: Implications for state and federal policy, programs, and providers. In Manderscheid RW, & Henderson MJ (Ed.), Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services (pp. 120–137). Rockville, MD. [Google Scholar]
- Neitzel C, & Dopkins Stright A (2004). Parenting behaviours during child problem solving: The roles of child temperament, mother education and personality, and the problem-solving context. International Journal of Behavioral Development, 28, 166–179. doi: 10.1080/01650250344000370 [DOI] [Google Scholar]
- Nolten WE, Lindheimer MD, Rueckert P, Oparil A, & Ehrlich E,N (1980). Diurnal patterns and regulation of cortisol secretion in pregnancy. The Journal of Clinical Endocrinology & Metabolism, 51, 466–472. doi: 10.1210/jcem-51-3-466 [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Batten SV, Plumb JC, Luterek JA, & Roessner BM (2004). An experimental study of emotional responding in women with posttraumatic stress disorder related to interpersonal violence. Journal of Traumatic Stress, 17, 241–248. doi: 10.1023/B:JOTS.0000029267.61240.94 [DOI] [PubMed] [Google Scholar]
- Phares V, Fields S, Kamboukos D, & Lopez E (2005). Still looking for poppa. American Psychologist, 60, 735–736. doi: 10.1037/0003-066X.60.7.735 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Rivers AJ, Morgan CA, & Southwick SM (2010). Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and postdeployment social support. Journal of Affective Disorders, 120, 188–192. doi: 10.1016/j.jad.2009.04.015 [DOI] [PubMed] [Google Scholar]
- Pinderhughes EE, Dodge KA, Bates JE, Pettit GS, & Zelli A (2000). Discipline responses: Influences of parents’ socioeconomic status, ethnicity, beliefs about parenting, stress, and cognitive-emotional processes. Journal of Family Psychology, 14, 380–400. doi: 10.1037/0893-3200.14.3.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samper RE, Taft CT, King DW, & King LA (2004). Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. Journal of Traumatic Stress, 17, 311–315. doi: 10.1023/B:JOTS.0000038479.30903.ed [DOI] [PubMed] [Google Scholar]
- Samuelson KW, Wilson CK, Padrón E, Lee S, & Gavron L (2017). Maternal PTSD and children’s adjustment: Parenting stress and emotional availability as proposed mediators. Journal of Clinical Psychology, 73, 693–706. doi: 10.1002/jclp.22369 [DOI] [PubMed] [Google Scholar]
- Santiago CD, Wadsworth ME, & Stump J (2011). Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effects on psychological syndromes among diverse low-income families. Journal of Economic Psychology, 32, 218–230. doi: 10.1016/j.joep.2009.10.008 [DOI] [Google Scholar]
- Schaeffer NC (2000). Asking questions about threatening topics: A selective overview. In Stone AA, Turkkan JS, Bachrach CA, Jobe JB, Kurtzman HS, & Cain VS (Eds.), The science of self-report: Implications for research and practice (pp. 105–121). Mahwah, NJ: Earlbaum. [Google Scholar]
- Shrout PE, & Bolger N (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7, 422–445. doi: 10.1037/1082-989X.7.4.422 [DOI] [PubMed] [Google Scholar]
- Stover CS, Hall C, McMahon TJ, & Easton CJ (2012). Fathers entering substance abuse treatment: An examination of substance abuse, trauma symptoms and parenting behaviors. Journal of Substance Abuse Treatment, 43, 335–343. doi: 10.1016/j.jsat.2011.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (1996). Using multivariate statistics (3rd ed.). New York, NY: HarperCollins. [Google Scholar]
- Thoemmes F, MacKinnon DP, & Reiser MR (2010). Power analysis for complex mediational designs using Monte Carlo methods. Structural Equation Modeling, 17, 510–534. doi: 10.1080/10705511.2010.489379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tutus D, & Goldbeck L (2016). Posttraumatic symptoms and cognitions in parents of children and adolescents with PTSD. European Child & Adolescent Psychiatry, 25, 997–1005. doi: 10.1007/s00787-016-0821-x [DOI] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Jongmans MJ (2015). Relational patterns between caregivers with PTSD and their nonexposed children. Trauma, Violence & Abuse, 17, 186–203. doi: 10.1177/1524838015584355 [DOI] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Mooren T (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant Mental Health Journal, 33, 459–468. doi: 10.1002/imhj.21324 [DOI] [PubMed] [Google Scholar]
- Veazey CH, Blanchard EB, Hickling EJ, & Buckley TC (2004). Physiological responsiveness of motor vehicle accident survivors with chronic posttraumatic stress disorder. Applied Psychophysiology and Biofeedback, 29, 51–62. doi: 10.1023/B:APBI.0000017863.35714.a1 [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Potter CM, Marshall EC, & Zvolensky MJ (2011). An evaluation of the relation between distress tolerance and posttraumatic stress within a trauma-exposed sample. Journal of Psychopathology and Behavioral Assessment, 33, 129–135. doi: 10.1007/s10862-010-9209-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013a). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov.
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013b). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). Interview available from the National Center for PTSD at www.ptsd.va.gov. [DOI] [PMC free article] [PubMed]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, … & Marx BP (2017). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30, 383–395. doi: 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, & Keane TM (2012). Screening, Diagnosis, and Treatment of Post-Traumatic Stress Disorder. Military Medicine, 117, 7–13. doi: 10.7205/MILMED-D-12-00111 [DOI] [PubMed] [Google Scholar]
- Zalewski M, Lewis JK, & Martin CG (2018). Identifying novel applications of dialectical behavior therapy: Considering emotion regulation and parenting. Current Opinion in Psychology, 21, 122–126. doi: 10.1016/j.copsyc.2018.02. [DOI] [PubMed] [Google Scholar]


