Abstract
Racial/ethnic minorities have experienced higher COVID-19 infection rates than whites, but it is unclear how individual-level housing, occupational, behavioral, and socioeconomic conditions contribute to these disparities in a nationally representative sample. In this study, we assess the extent to which social determinants of health contribute to racial/ethnic differences in COVID-19 infection. Data are from the Understanding America Study's Understanding Coronavirus in America survey (UAS COVID-19 waves 7–29). UAS COVID-19 is one of the only nationally representative longitudinal data sources that collects information on household, work, and social behavioral context during the pandemic. We analyze onset of COVID-19 cases, defined as a positive test or a diagnosis of COVID-19 from a healthcare provider since the previous survey wave, over a year of follow-up (June 2020–July 2021). We consider educational attainment, economic resources, work arrangements, household size, and social distancing as key social factors that may be structured by racism. Cox hazard models indicate that Hispanic people have 48% higher risk of experiencing a COVID-19 infection than whites after adjustment for age, sex, local infection rate, and comorbidities, but we do not observe a higher risk of COVID-19 among Black respondents. Controlling for engagement in any large or small social gathering increases the hazard ratio for Hispanics by 9%, suggesting that had Hispanics had the same social engagement patterns as whites, they may have had even higher risk of COVID-19. Other social determinants—lower educational attainment, working away from home, and number of coresidents—all independently predict higher risk of COVID-19, but do not explain why Hispanic Americans have higher COVID-19 infection risk than whites.
Keywords: COVID-19, Infection risk, Social determinants, Structural racism, Health disparities, Hispanic Americans
1. Introduction
The COVID-19 pandemic has impacted our lives and health, but has done so unequally across the population. Black and Hispanic individuals in the U.S. have faced a higher rate of COVID-19 cases, severe illness, and mortality compared with whites (Mackey et al., 2021). According to COVID-NET surveillance data, the rates of COVID-19-associated hospitalization and ICU admission are highest among Hispanic individuals, followed by non-Hispanic Black individuals (Garg et al., 2021). Provisional death counts from February 2020–January 2022 show that the mortality rate for Hispanic and Black Americans is almost double the rate of whites (Centers for Disease Control and Prevention (CDC), 2022a). While vaccination has led to significant declines in COVID-19 cases and deaths, racial/ethnic disparities seem to remain persistent (CDC, 2022b).
In order to understand racial/ethnic disparities in the burden of COVID-19, it is crucial to consider how structural racism acts through various domains of social circumstance to shape infection risk. However, previous studies have typically used aggregate-level variables such as county-level education or poverty rates to identify potential drivers of racial/ethnic disparities in COVID-19 (Fielding-Miller et al., 2020; Hamidi and Hamidi, 2021). These findings tend to focus on samples from single states or specific communities and fail to capture variation across individuals (Chen and Krieger, 2021; Podewils et al., 2020). Beyond education and income, limited access to affordable housing, limited options to work from home, and inability to socially isolate have been posited as social determinants that place people of color at increased risk (Badri et al., 2021; M. A. Garcia et al., 2021; Thakur et al., 2020). However, such individual-level measures have received less empirical attention using nationally representative samples.
We extend prior work by considering how structural racism acts through educational attainment and multiple proximate social factors—work arrangements, income, household arrangements, and social distancing behaviors—which simultaneously contribute to the production of racial/ethnic disparities in COVID-19 infection. We use waves 7–29 of the Understanding America Study's Understanding Coronavirus in America Survey (UAS COVID-19), which followed respondents and tracked incident COVID-19 cases over a year from June 10, 2020–July 19, 2021. UAS COVID-19 is one of the only nationally representative longitudinal data sources that collects information on household, work, and social behavioral context during the pandemic. Informed by prior work that frames racism as a fundamental cause of racial disparities in health (Laster Pirtle, 2020; Phelan and Link, 2015; Williams and Collins, 2001), we posit that constraints in socioeconomic, occupational, living and behavioral conditions increase risk of COVID-19 infection by making social distancing and self-isolation difficult and limiting access to information and resources to prevent infection, and that because these key social determinants are shaped by racism, they contribute to racial/ethnic disparities in COVID-19 infection.
2. Background
Racial/ethnic disparities in COVID-19 have been shaped and exacerbated by many of the inequitable systems in American society. In the U.S., structural racism and discrimination are fundamental causes of health inequalities (Phelan and Link, 2015; Williams and Collins, 2001; Zalla et al., 2021). In the case of the pandemic, racial capitalism, racial segregation, colorblind racism, and racialized class hierarchy act together to produce disparities by creating unequal access to protective resources and opportunities, stratifying the social determinants of health, and restricting the lives of minoritized communities (Bonilla-Silva, 2020; M. A. Garcia et al., 2021; Laster Pirtle, 2020). An increasing number of studies suggest the social determinants of health—most often operationalized by area-level socioeconomic factors—are risk factors for COVID-19 (Credit, 2020; Dalsania et al., 2021; Do and Frank, 2021), yet relatively few studies have explored an empirical link between key racialized social determinants of health and racial/ethnic disparities in COVID-19 at the individual level. While this line of research has been critical in shifting narratives away from color-blind ideologies that naturalize racial disparities (Bonilla-Silva, 2020) and toward social exposures, it is limited by inadequate attention to the ways structural racism acts through multiple dimensions of the social determinants of health simultaneously.
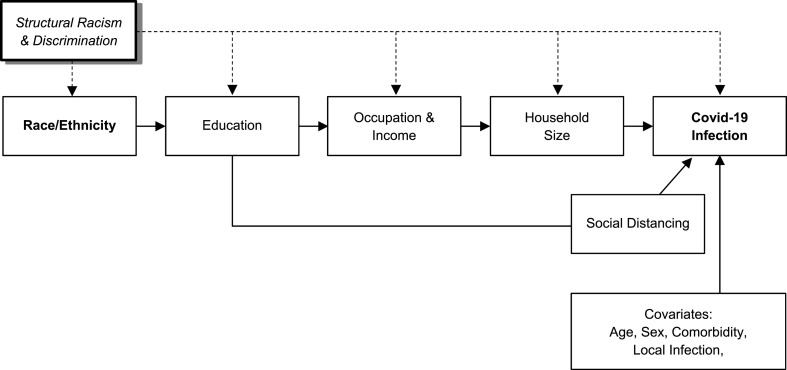
As shown in Fig. 1 , we focus here on five dimensions of social determinants of health that are known to be shaped by racism and discrimination, and estimate the role of these racialized social determinants in producing racial/ethnic disparities in COVID-19 infection. The five key dimensions of social determinants of health include educational attainment, economic resources, work arrangements, household size, and social distancing, all of which have the potential to differentiate risk of exposure in ways that disadvantage Black and Hispanic people and restrict their ability to avoid infection.
Fig. 1.
A conceptual framework that illustrates key social determinants of health pathways through which inequitable systems (structural racism and discrimination) contribute to racial/ethnic disparities in COVID-19 infection. The dashed line indicates the unmeasured influence of structural racism and discrimination on racial/ethnic disparities.
Specifically, we posit that structural racism shapes the risk of COVID-19 infection for Hispanic and Black individuals largely through educational attainment and its consequences for work, economic resources, housing, and health behaviors. We hypothesize that educational attainment partially proxies for racialized social class and mediates some of the impact of structural racism in early life. In this sense, educational attainment precedes the other social determinants we measure. Racialized educational inequality, in turn, differentiates work arrangements and economic resources, but there are also countless direct ways that structural racism stratifies work and economic resources. For example, racialized immigration enforcement excludes many Hispanic immigrants from jobs that would allow for remote work. We also posit that lower levels of education and economic status place people of color at risk through limited access to information and resources to reduce COVID-19 health risks.
We then consider two more proximate social determinants that are frequently speculated about in media coverage of COVID-19 disparities, but less frequently measured: household size and social distancing, which we hypothesize to be additional pathways through which racialized educational inequality may drive COVID-19 disparities. The selected social determinants are not intended to be an exhaustive list – indeed it is impossible to measure all of the ways that structural racism drives COVID-19 disparities via social factors - but we have selected five key social determinants whose influence on COVID-19 infection risk may be modifiable through policy and targeted programs.
2.1. Education
Educational attainment in the U.S. is profoundly shaped by segregation and other forms of structural racism and likely shapes COVID-19 infection risk in multiple ways. First, mindful that it is difficult to measure and model racialized social class, educational attainment captures some of the influence of racialized social class on COVID-19 exposure (Bonilla-Silva, 2020; Laster Pirtle, 2020). Second, education likely confers greater health literacy and trust in science, which can allow people to understand the importance of adhering to social distancing and other recommended measures during the COVID-19 pandemic and the reasoning behind the measures being taken to prevent the spread of the virus (Greer et al., 2021). Researchers have found that Americans with more education had higher adherence to social distancing guidelines (Kim and Crimmins, 2020; Smail et al., 2021; Zhao et al., 2020) and were more likely to express intention to receive a vaccine against COVID-19 (Szilagyi et al., 2021).
Because of the potential for educational attainment to influence risk of COVID-19, prior research has posited that the lower educational attainment of Black and Hispanic Americans–shaped by systemic racism in educational quality and opportunity– may contribute to disparities in COVID-19 cases and deaths (Feldman and Bassett, 2021; Garcia et al., 2021; Phillips, 2011). However, very little research has examined the role of educational attainment in shaping racial/ethnic differences in COVID-19 (Feldman and Bassett, 2021). Because educational attainment is generally not collected as part of COVID-19 surveillance data, survey data can provide novel insights into the influence of educational inequality to COVID-19 infection risk.
2.2. Economic resources
As with education, large racial/ethnic gaps in income are likely to contribute to the elevated COVID-19 risks among Black and Hispanic Americans. While the median household income in 2020 for white households was $76,057, the medians for Black and Hispanic households were only $46,073 and $56,113, respectively (US Census Bureau, 2020).
Greater economic resources can allow individuals to pay a premium to avoid interactions with the public. Evidence indicates that residents of lower income neighborhoods in New York City did not reduce their subway usage as much as residents of higher income neighborhoods, reflecting both a necessity to commute to in-person work and a lack of safer transportation alternatives (Sy et al., 2021). Higher-income households were also more likely to pay for grocery delivery to avoid shopping in person than lower-income households (Unnikrishnan and Figliozzi, 2020). Just as higher income affords protections from exposure to infection, the constraints and instability of lower income are likely to make exposure to infection at work and at home more likely. However, this hypothesis is yet to be confirmed by individual-level data as most existing evidence on the association between SES and COVID-19 incidence has used aggregate level data (Clouston et al., 2021).
2.3. Work
Since the beginning of the pandemic in the US, workplaces were identified as potential sources of COVID-19 transmission, and many employers instituted work-from-home policies either voluntarily or in response to stay-at-home orders. However, many jobs deemed essential or frontline, such as those in the healthcare and manufacturing sectors, could not feasibly be done from home (Blau et al., 2020; Carlsten et al., 2021). As more data have become available, it has become apparent that infection and mortality rates were elevated among essential workers (J.T. Chen et al., 2021; Hawkins et al., 2021; Riley et al., 2021).
A long history of structural racism in the labor market has resulted in constrained opportunities for workers of color, resulting in their overrepresentation in low-wage, essential jobs and in jobs with characteristics considered risk factors for COVID-19, such as frequent exposure to infectious diseases or contact with external customers (Cox-Ganser and Henneberger, 2021; Goldman et al., 2021; Selden and Berdahl, 2020). Black and Hispanic workers have been historically concentrated in lower-wage jobs in the service, production, and transportations industries, and these types of jobs often lack flexible work arrangements and paid leave benefits (Garcia et al., 2021). Many researchers have speculated that these differential employment patterns by race and ethnicity have contributed to the high burden of COVID-19 cases and deaths among Black and Hispanic Americans and among individuals with less education (Andrasfay and Goldman, 2021; Y.-H. Chen et al., 2021; Riley et al., 2021; Rodriguez-Diaz et al., 2020). However, limited availability of individual-level data on both occupational information and COVID-19 outcomes has precluded previous studies from directly assessing how occupational exposures contribute to racial/ethnic disparities in COVID-19.
2.4. Household size
Due to policies and practices including redlining, racist housing discrimination, and predatory lending, white people have systemic advantages in housing which may allow them to better avoid COVID-19 at home. Larger households and denser living arrangements can limit the ability to isolate and may increase exposure to the virus. Especially in contexts of rising housing costs, large racial/ethnic education, income and occupational gaps make Black and Hispanic Americans more likely to live in dense, multigenerational households than whites (E. Garcia et al., 2021). Nationally, Hispanic households have an average of 1.6 wage earners, compared to 1.2 for white households (Bureau of Labor Statistics, 2018). This indicates that, on average, Hispanic households have more adults potentially leaving the home every day, which increases their likelihood of exposure to COVID-19-positive individuals through work and exposes other household members to the virus. Data from the 2016 American Community Survey also show that, among Hispanic and Black Americans, the shares living in multigenerational households are 27% and 26%, respectively, whereas only 16% of whites lived with extended family (Cohn and Passel, 2018). The prevalence of multigenerational living is thought to have increased during the pandemic as more families have merged with households out of financial and caregiving necessity, although this puts these families at increased risk of overcrowding (Binette et al., 2021).
Research has shown that living in multigenerational households or living with a large number of household members is associated with increased risk of COVID-19, but these studies have typically used area-level measures (e.g., average household size or proportion of multigenerational households in the area) from single states or some communities that may not be widely generalizable (Chen and Krieger, 2021; Hamidi and Hamidi, 2021). It remains largely unknown whether differences in the living conditions by race and ethnicity contributed to high risk of COVID-19 infection among people of color.
2.5. Social distancing
Social behaviors including gathering with friends and family and attending religious services are typically considered to be beneficial for health and wellbeing, but have been identified as risk factors during the COVID-19 pandemic. Previous work has shown that lower adherence to social distancing guidelines, including not avoiding public places or limiting gatherings, was associated with greater risk of COVID-19 infection (Andrasfay et al., 2022; Whaley et al., 2021). Adherence to social distancing guidelines has been found to be higher among older adults and women, but evidence regarding racial/ethnic differences in adherence to these guidelines has been more mixed, and these differences have varied over the course of the pandemic (Kim and Crimmins, 2020; Zhao et al., 2020).
While Fundamental Cause Theory would suggest that people with more resources would be more likely to social distance, social distancing may be greater among Black and Hispanic communities in part due to racially-targeted social distancing enforcement in the early stages of the pandemic. Early arrest data indicate that, in mid-March to early May in 2020, Black and Hispanic populations were disproportionately arrested for not adhering to state and county guidelines in New York City, Chicago, and Ohio (Dunbar and Jones, 2021). This differential social distancing enforcement may have contributed to widespread variation in social distancing in communities across the country (Gibbons, 2021). Here, we focus on attendance at large and small gatherings to distinguish social distancing as a health behavior from the ability to distance as determined by one's work arrangement.
3. Data and methods
3.1. Data
Data are from the Understanding America Study's Understanding Coronavirus in America survey (UAS COVID-19) conducted by the Center for Economic and Social Research at the University of Southern California. The UAS is a nationally representative internet panel study of American adults that began in 2014 with the support of the National Institute on Aging, the Social Security Administration, and the Gates Foundation. Respondents answered the survey using a computer, tablet, or smartphone, and they were provided with a tablet and broadband internet if they did not have access to the internet. The UAS COVID-19 longitudinal survey, which ran from March 2020, through July 2021, surveyed UAS panel members about their experiences, behaviors, and beliefs during the pandemic. Follow-up waves were conducted every two weeks from March 2020–March 2021, and became monthly from March 2021–June 2021, for a total of 29 survey waves.
For this analysis, we use data from waves 7–29, covering the period from June 10, 2020–July 19, 2021, because these waves consistently ask about all measures required for our analyses. Of the 8628 respondents who participated in at least one of these survey waves, we restrict our analytic sample to individuals who did not report a COVID-19 infection or vaccination at their first interview in this period and who had at least one wave of follow-up (6% excluded), and individuals with complete information on all social, demographic, and behavioral questions in at least one wave (an additional 1% excluded), for a final analytic sample of 7647 respondents. We include follow-up observations of individuals until a report of a COVID-19 infection, receipt of at least one dose of a vaccination against COVID-19, or censoring due to loss to follow-up or the end of the study period, resulting in 110,440 observations over 5378 person-years of exposure.
3.2. Measures
3.2.1. Outcome variable
The outcome of our analysis is incident COVID-19 infection. In each wave, respondents reported whether they had received a positive COVID-19 test or a diagnosis of COVID-19 from a healthcare provider since their last survey wave. We consider either a positive test or diagnosis from a healthcare provider as the indication of COVID-19 infection. Because individuals do not report the date of test or diagnosis, we assign this to be the midpoint between the respondent's previous interview and the interview in which s/he reports the test or diagnosis.
3.2.2. Independent variables
To examine racial/ethnic differences in COVID-19, we construct a measure of race/ethnicity categorized as Non-Hispanic White, Non-Hispanic Black, Hispanic, and Non-Hispanic Other race. While the UAS allowed individuals to identify as Native American, Asian, Pacific Islander, or Mixed race, we chose to group these categories as “Other race” because we did not have adequate sample size to consider them separately. Note that we follow the survey language and the term Hispanic to refer to all Hispanic, Latino and Latinx individuals. We use the terms Black and white to refer to non-Hispanic Black and non-Hispanic white individuals.
We focus on five social determinants that may differentiate risk of infection in racialized ways: (1) education, (2) economic resources, (3) work arrangement, (4) household size, and (5) social distancing. Educational attainment is categorized as high school or less; some college; and college or more. As a marker of economic resources, we include household income categorized as less than $30,000, $30,000–59,999, $60,000–99,999, and $100,000 or more, which roughly correspond to the quartiles of household income in our sample. We combine responses from questions on labor force status and days worked from home in the previous week to create a time-varying measure of working arrangement categorized as working from home; working outside the home; retired; and unemployed or otherwise out of the labor force. A time-varying measure of household size is defined by the number of coresident household members (up to 12). In each wave in our study period, respondents reported about several behaviors related to social distancing in the previous 7 days, and we created time-varying measures of engagement in any large or small social gathering as markers of social distancing behaviors, following previous work (Andrasfay et al., 2021). Any large gathering or public interaction is defined by not avoiding public places, gatherings, or crowds; not avoiding eating at restaurants; going out to a bar, club, or other place where people gather; attending a gathering with more than 10 people; or attending an in-person religious service. Any small gathering is defined by not avoiding contact with high-risk people; having visitors at their residence; going to another's residence; or having close contact (within 6 ft) with people not in the household.
3.2.3. Covariates
Demographic characteristics include sex and age group at first interview (18–44, 45–64, and 65 and over). To proxy for geographic variation in the risk of infection, we include a time-varying measure of the case rate per 100,000 population in the respondent's state in the 7-day period prior to the respondent's interview; we log this measure in the multivariate models. These case rates were obtained from the Centers for Disease Control and Prevention's COVID Data Tracker (CDC, 2022b). Because the likelihood of seeking a test or medical help and receiving a diagnosis depends on the severity of infection, we also include a time-varying count of comorbid conditions that have been associated with severity of COVID-19. These include diabetes, cancer, heart disease, asthma, chronic lung disease, kidney disease, autoimmune disorders, hypertension, and obesity.
4. Statistical analysis
Following the conceptual framework laid out in Fig. 1, we fit a series of multivariate models to assess how the risk of COVID-19 infection differs by race/ethnicity and to what extent five key social determinants hypothesized to be mediators of the relationship between structural racism and risk of COVID-19 infection contribute to the estimated racial/ethnic disparities. To assess the magnitude of racial/ethnic disparities, we first fit a minimally-adjusted Model 1 predicting risk of COVID-19 infection by race/ethnicity, with sex, age, the log state-level case rate, and the number of comorbid conditions as covariates. We then sequentially add in the social determinants, starting with the most upstream and ending with the most proximate to COVID-19 infection.
The first social determinant we add is educational attainment in Model 2. Because systemic racism constrains educational opportunities early in life, we theorize that structural racism may be acting through educational attainment to drive disparities in COVID-19 infection. Next, Model 3 adds household income and working arrangement, both of which are influenced by structural racism indirectly via educational attainment and directly via hiring and work-related mechanisms, and which are likely associated with risk of COVID-19 infection. Model 4 adds the number of household coresidents, which is influenced by educational and economic resources and work and is associated with the ability to isolate from infected household members. Model 5 considers an alternative pathway through which racialized educational inequality may contribute to racial/ethnic disparities in COVID-19 infection: social distancing. In this model, participation in small gatherings and large gatherings or public interactions are added to the variables in Model 2 because we hypothesize there is an additional pathway from education to COVID-19 infection via health literacy which is distinct from the economic resources pathway. Last, we jointly consider both pathways through which racial/ethnic disparities in COVID-19 may emerge by including all social determinants together in Model 6 in order to assess the extent to which these five key social determinants contribute to racial/ethnic disparities in COVID-19.
We fit these models using Cox hazard models, which non-parametrically fit a baseline hazard of COVID-19 diagnosis at each day following June 10, 2020, which is the beginning of our study period, and estimate how this baseline hazard is proportionately increased or decreased by observable risk factors. Individuals in our sample are considered at risk for an incident COVID-19 infection from their first interview in our study period until they report an infection, receive at least one dose of a vaccine against COVID-19, or are otherwise censored. We censor individuals upon receipt of a COVID-19 vaccine because breakthrough infections were still considered rare during the study period (Christie et al., 2021) and because vaccination has been associated with the social behaviors that we study, which could bias the associations (CDC, 2022b). We split the follow-up time for each individual into intervals following each survey wave to allow certain independent variables to be time-varying. In cases where an individual reports a variable in one wave but is missing this variable in subsequent waves, we carry forward their previous values until they provide an updated response. All analyses include weights provided by the UAS and were done in R (version 4.0.3).
5. Results
Weighted summary statistics of participants in our analytic sample at their first observation in our study period are displayed in Table 1 . These statistics are also shown separately by race/ethnicity. Approximately 10% of the sample is infected with COVID-19 during follow-up, but there are substantial racial/ethnic differences, with Hispanic participants having the highest cumulative incidence (13.85%) and participants grouped as other race the lowest (8.29%). Hispanic participants had high levels of many of the social factors we hypothesized to be important social determinants linking structural racism to COVID-19 infection, including having the highest prevalence of working away from home and the largest number of household coresidents. Both Black and Hispanic participants had lower levels of college education than white or other race participants. Black participants had the lowest household income of all groups in the study. White participants, while advantaged in terms of living, working, and socioeconomic conditions, had the highest prevalence of engaging in risky social behaviors.
Table 1.
Summary statistics of analytic sample at first observation.
| Percent or Mean (SD) |
|||||
|---|---|---|---|---|---|
| Full sample | White | Black | Hispanic | Other | |
| Race/Ethnicity | |||||
| Non-Hispanic White | 61.4 | ||||
| Non-Hispanic Black | 11.9 | ||||
| Hispanic | 17.2 | ||||
| Non-Hispanic Other | 9.5 | ||||
| Ever infected with COVID-19 | 10.08 | 9.53 | 8.88 | 13.85 | 8.29 |
| Sex | |||||
| Female | 52.4 | 48.0 | 63.3 | 60.6 | 51.6 |
| Male | 47.6 | 52.0 | 36.7 | 39.4 | 48.4 |
| Age | |||||
| 18–44 | 49.6 | 43.6 | 53.3 | 64.5 | 57.5 |
| 45–64 | 32.0 | 32.5 | 34.1 | 28.9 | 31.4 |
| 65+ | 18.4 | 23.9 | 12.7 | 6.6 | 11.1 |
| State-level cases in past week (per 100 k) | 84.47 | 74.83 | 103.92 | 105.98 | 83.46 |
| Number of comorbidities | 0.9 (1.2) | 1 (1.2) | 1 (1.2) | 0.7 (1) | 0.7 (1.1) |
| Educational Attainment | |||||
| High school or less | 37.3 | 39.3 | 42.6 | 34.7 | 22.4 |
| Some college | 28.5 | 25.1 | 34.4 | 39.2 | 24.2 |
| College or more | 34.2 | 35.7 | 23.0 | 26.0 | 53.4 |
| Income | |||||
| Less than $30,000 | 27.9 | 23.6 | 50.3 | 29.4 | 25.2 |
| $30,000-$59,999 | 26.5 | 26.0 | 27.1 | 30.3 | 21.9 |
| $60,000-$99,999 | 23.3 | 25.6 | 13.4 | 21.9 | 23.5 |
| $100,000 or more | 22.3 | 24.8 | 9.3 | 18.4 | 29.4 |
| Employment Status | |||||
| Working, from home | 25.9 | 23.9 | 26.0 | 26.8 | 37.3 |
| Working, away from home | 32.2 | 31.6 | 30.0 | 38.6 | 28.0 |
| Unemployed or out of labor force | 25.2 | 22.7 | 34.6 | 28.8 | 23.5 |
| Retired | 16.6 | 21.8 | 9.4 | 5.8 | 11.2 |
| Number of household coresidents | 1.7 (1.5) | 1.7 (1.4) | 1.5 (1.5) | 2.1 (1.7) | 1.7 (1.5) |
| Social Behaviors | |||||
| Large gathering | 51.2 | 55.2 | 44.2 | 47.8 | 40.5 |
| Small gathering | 80.3 | 84.8 | 71.9 | 72.3 | 76.1 |
| Number of respondents | 7674 | 4987 | 608 | 1266 | 813 |
| Number of observations | 110,440 | 73,846 | 8575 | 16,324 | 11,695 |
| Person-years of follow-up | 5378 | 3501 | 438 | 867 | 572 |
Note: Data are from the UAS COVID-19 Study waves 7–29. Percentages and means are based on the first observation of each respondent in this period and are calculated using weights provided by the UAS.
Results from Cox hazard models predicting COVID-19 infection are shown in Table 2 . Model 1 estimates that Hispanic individuals have 48% higher risk (HR = 1.48, 95% CI = 1.13–1.93) of infection than whites after adjustment for age, sex, local infection rate, and comorbid conditions, but we do not observe a higher risk of COVID-19 among Black individuals in our sample. In Model 2, we additionally include educational attainment and find that, compared to those who have completed college, individuals with high school or less education and those with some college experience have higher risk of COVID-19. In this model, Hispanic individuals still have 42% higher risk (CI = 1.08–1.86) of COVID-19 than white individuals. Model 3 adds working arrangement and household income to Model 2. While working away from home appears to be associated with an increased risk of COVID-19 infection, neither working arrangement nor household income are significantly associated with COVID-19 infection. Model 4 adds the number of coresidents to Model 3. In this model, each additional coresident is associated with an 8% increased risk (CI = 1.01–1.16) of COVID-19, but the larger household size of Hispanic participants does not appear to account for their increased risk of COVID-19, as Hispanic participants maintain a 41% higher risk (CI = 1.07–1.85) of COVID-19 in this model. Next, Model 4 considers an alternative pathway in which education may impact risk of COVID-19 through its effects on social distancing behaviors. In this model, both attending a small gathering (HR = 1.41, CI = 1.08–1.84) or large gathering (HR = 1.43, CI = 1.16–1.75) are significantly associated with increased COVID-19 risk. These behaviors do not reduce the increased risk of COVID-19 among Hispanic individuals; rather, the hazard ratio (1.55, CI = 1.18–2.05) is slightly raised in this model, suggesting that had Hispanics had the same level of social engagement as whites, they may have had even higher risk of COVID-19.
Table 2.
Associations between social and contextual characteristics and COVID-19 diagnosis: Hazard ratios and 95% confidence intervals.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Race/Ethnicity (ref = Non-Hispanic White) | ||||||
| Non-Hispanic Black | 0.84 (0.60, 1.18) | 0.82 (0.58, 1.15) | 0.85 (0.60, 1.19) | 0.85 (0.61, 1.20) | 0.90 (0.64, 1.26) | 0.92 (0.66, 1.30) |
| Hispanic | 1.48 (1.13, 1.93) | 1.42 (1.08, 1.86) | 1.43 (1.09, 1.88) | 1.41 (1.07, 1.85) | 1.55 (1.18, 2.05) | 1.53 (1.16, 2.01) |
| Other | 0.88 (0.60, 1.31) | 0.93 (0.63, 1.37) | 0.95 (0.64, 1.40) | 0.95 (0.64, 1.40) | 1.00 (0.68, 1.48) | 1.01 (0.68, 1.50) |
| Educational attainment (ref = College) | ||||||
| Some college | 1.50 (1.17, 1.93) | 1.50 (1.15, 1.95) | 1.46 (1.13, 1.89) | 1.45 (1.13, 1.86) | 1.42 (1.09, 1.83) | |
| High school or less | 1.29 (1.01, 1.65) | 1.33 (1.00, 1.76) | 1.27 (0.96, 1.68) | 1.26 (0.99, 1.61) | 1.23 (0.93, 1.64) | |
| Income (ref = $100,000 or more) | ||||||
| $60,000-$99,999 | 1.15 (0.87, 1.54) | 1.18 (0.89, 1.58) | 1.19 (0.89, 1.58) | |||
| $30,000-$59,999 | 1.04 (0.77, 1.39) | 1.09 (0.81, 1.46) | 1.10 (0.82, 1.48) | |||
| Less than $30,000 | 1.02 (0.74, 1.41) | 1.11 (0.80, 1.55) | 1.14 (0.82, 1.57) | |||
| Working arrangement (ref = working from home) | ||||||
| Working away from home | 1.23 (0.94, 1.62) | 1.24 (0.94, 1.63) | 1.16 (0.88, 1.53) | |||
| Retired | 0.82 (0.57, 1.19) | 0.84 (0.58, 1.21) | 0.84 (0.58, 1.22) | |||
| Unemployed or out of labor force | 0.90 (0.66, 1.23) | 0.89 (0.65, 1.22) | 0.90 (0.66, 1.23) | |||
| Number of coresidents | 1.08 (1.01, 1.16) | 1.08 (1.01, 1.15) | ||||
| Social behaviors in past 7 days | ||||||
| Any large gathering | 1.41 (1.08, 1.84) | 1.37 (1.05, 1.78) | ||||
| Any small gathering | 1.43 (1.16, 1.75) | 1.40 (1.14, 1.72) | ||||
| Covariates | ||||||
| Male | 0.89 (0.74, 1.09) | 0.92 (0.75, 1.12) | 0.88 (0.72, 1.08) | 0.89 (0.73, 1.09) | 0.90 (0.74, 1.09) | 0.88 (0.72, 1.08) |
| Age group (ref = 18–44) | ||||||
| Age 45-64 | 1.12 (0.90, 1.41) | 1.12 (0.90, 1.40) | 1.14 (0.91, 1.43) | 1.21 (0.96, 1.53) | 1.17 (0.94, 1.46) | 1.26 (1.00, 1.59) |
| Age 65+ | 0.67 (0.48, 0.94) | 0.68 (0.48, 0.95) | 0.81 (0.56, 1.17) | 0.88 (0.60, 1.29) | 0.73 (0.52, 1.02) | 0.92 (0.63, 1.35) |
| Logged state-level 7-day case rate | 1.55 (1.32, 1.83) | 1.55 (1.31, 1.83) | 1.54 (1.31, 1.82) | 1.55 (1.31, 1.83) | 1.56 (1.32, 1.84) | 1.56 (1.32, 1.84) |
| Number of comorbidities | 1.09 (1.00, 1.19) | 1.08 (0.99, 1.17) | 1.10 (1.01, 1.20) | 1.09 (1.01, 1.19) | 1.09 (1.01, 1.19) | 1.11 (1.01, 1.20) |
| Number of observations | 110,440 | 110,440 | 110,440 | 110,440 | 110,440 | 110,440 |
| Number of COVID-19 diagnoses | 801 | 801 | 801 | 801 | 801 | 801 |
Note: Data are from the UAS COVID-19 Study waves 7–29. Hazard ratios are from Cox proportional hazards models that include weights provided by the UAS.
Last, we include all of these social determinants together in Model 6. In this model, we continue to see evidence that education, number of coresidents, and social behaviors are statistically significant predictors of COVID-19 infection. After adjusting for all of these social determinants together, Hispanic individuals still have 53% higher risk (CI = 1.16–2.01) of COVID-19 infection than whites with the same characteristics.
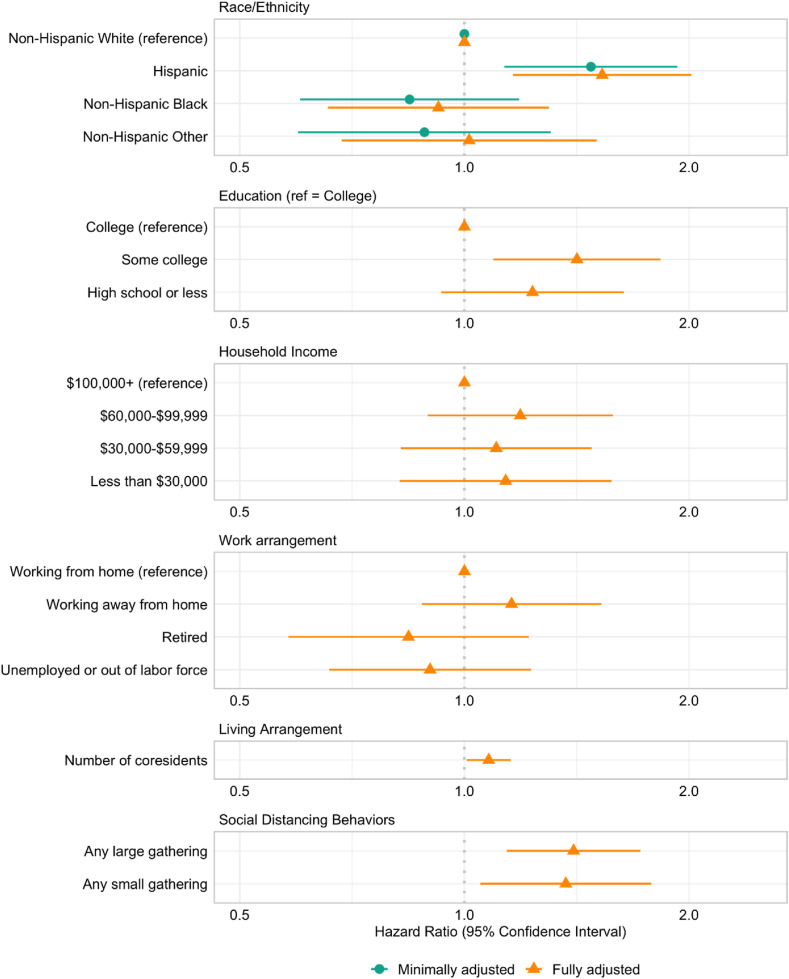
The racial/ethnic differences in Model 1 compared to Model 6 are displayed in Fig. 2 , along with the hazard ratios of the social determinants. This figure illustrates that while several social determinants–educational attainment, number of coresidents, and small and large social gatherings–appear to have an association with COVID-19 infection, their inclusion in this model does not reduce the substantially higher risk of COVID-19 among Hispanics in our data.
Fig. 2.
Hazard ratios and 95% confidence intervals of the associations between social risk factors and COVID-19 infection. The minimally-adjusted model (Model 1) includes sex, age, the log state-level case rate, and the number of comorbid conditions. The fully-adjusted model (Model 7) additionally includes the listed social determinants.
In each of the models containing one or more social determinants of COVID-19 infection, the hazard ratio associated with Hispanic race/ethnicity remains within 5% of the hazard ratio estimated in the minimally adjusted model. Thus, we do not find evidence that these social determinants are important mediators of the association between structural racism, as captured by race/ethnicity, and COVID-19 infection.
5.1. Supplementary analyses
We ran additional analyses to test the sensitivity of our results to the definition of incident COVID-19 cases used in our analyses. We considered a narrower definition of positive tests only (Table A1) and a broader definition that included instances when respondents thought they had COVID-19 but did not have a test or diagnosis (Table A2). In these analyses, the increased COVID-19 risks among Hispanic individuals are of lower magnitude than the main specification and are not consistently significant, but we come to the same conclusion that social determinants appear to be important predictors of COVID-19 but cannot explain the increased risks experienced by Hispanic individuals.
In addition to the social determinants, we examined in our main specifications, we considered alternative measures of these constructs (Table A3). We considered immigrant status and the language in which the respondent completed the UAS survey as proxies for barriers to accurate health information, as well as a count of scientific sources the respondent relied on for COVID-19 information, but we did not find these to be significantly associated with COVID-19. In lieu of the more parsimonious number of coresidents, we included indicators for whether the respondent lives with a working age adult and whether s/he lives with a child under age 18. The point estimates suggested that both of these living arrangements were associated with higher risk of COVID-19, but they were not statistically significant.
6. Discussion
This is one of the first studies to examine the role of racialized social determinants of health as contributors to racial/ethnic disparities in COVID-19 using nationally representative survey data. We find that Hispanic Americans, but not Black Americans, have a substantially higher risk of experiencing a COVID-19 infection compared to whites. Lower educational attainment and higher-risk working and living arrangements all predict higher risk of COVID-19, but do not explain why Hispanics have higher risk of COVID-19 infection than whites. Contrary to media speculation based on cultural stereotypes (Villarreal, 2020), we find that Hispanic individuals had better adherence to social distancing guidelines and that their risk of COVID-19 may have been even higher had they had the same engagement in small or large social gatherings as whites.
Of course, the extensive ways structural racism influences health to produce disparities go beyond the five social determinants we measured. As shown in Fig. 1, we theorized that structural racism's influence on racial/ethnic disparities in COVID-19 infection is only partially mediated by what was measurable with available survey data. Still, our findings of persistent Hispanic-white gaps in infection risk across the models offer surprising insights about several key mechanisms thought to drive disparities in infection.
We hypothesized that one of the mechanisms linking educational attainment and infection risk would be social distancing due to differences in health literacy, but it is possible that educational attainment may not capture individuals’ full capacity to find, understand, and use information about health-protective behaviors. Information about the virus, prevention methods to avoid becoming ill, and available treatment options are included in fact sheets provided by the CDC, but these are not easily accessible to all. Individuals with language and literacy barriers may therefore find it difficult to access necessary information about how to avoid infection. Previous research has found that respondents who relied on multiple professional sources–including the WHO, the US Department of Health and Human Services, the CDC, local public health officials, and physicians–to understand the pandemic had better adherence to risk mitigation guidelines than those who relied on fewer professional sources (Zhao et al., 2020). We explored whether individuals who relied on more of these professional sources had lower risk of COVID-19 infection, but we found neither a significant association nor evidence that fewer sources of accurate health information contributed to the higher risk of infection among Hispanics (Table A3). More importantly, there are likely unmeasured social factors which constraint the ability to act on risk mitigation guidance to protect oneself from infection either at home or in the workplace.
Another explanation for the persistent Hispanic-white gap in infection risk is that unmeasured variation in occupational risk factors may contribute to the higher risk of COVID-19 among Hispanics. For example, our measure of working arrangement in this analysis provides information on whether one worked outside the home in the past week but does not allow us to infer the level of COVID-19 exposure outside the home. Nor does it capture the privilege to stay home when sick and to work in a place that would allow others to stay home when sick. Ideally, we would be able to include information about workplace protections and the frequency with which respondents work in close physical proximity to their colleagues and have contact with external customers, which have been identified as important risk factors for COVID-19 in other studies (Cox-Ganser and Henneberger, 2021; Goldman et al., 2021; Selden and Berdahl, 2020). Although UAS periodically asks about occupation as part of its non-COVID-19 surveys, this information is not available for all UAS COVID-19 participants, and the detailed occupation codes that would allow linkages to external sources of occupational exposure are not currently available to researchers.
Another possible explanation is that it may be household crowding, rather than household size, that increases the risk of COVID-19 transmission for Hispanic individuals because household members cannot adequately isolate if exposed or infected. Other studies have examined aggregate-level household crowding and found that communities with a higher prevalence of household crowding had higher COVID-19 mortality (Chen and Krieger, 2021; Rodriguez-Diaz et al., 2020). However, because UAS infrequently surveyed respondents about the number of rooms in their residences, we were unable to assess how household crowding during the pandemic predicted infection with COVID-19.
We do not find an elevated risk of COVID-19 infection among Black individuals in our study. Although Black Americans continue to experience higher COVID-19 mortality (CDC, 2022b; Wong et al., 2021), some recent studies of disparities in infection have not found increased risks among Black Americans. In a study of the Medicaid managed care population in northern California, Jacobson et al. (2021) similarly report higher odds of positive tests among Hispanic patients, but not Black patients, after accounting for SES disparities. In addition, racial disparities in infection are likely to vary over time and across geographic contexts in the U.S. In an analysis of the early months of the pandemic, Rentsch et al. (2020) found that the disparity in testing positive between Black and white individuals was stronger in the Midwest than the West. Studies using longer follow-up periods have found that Black-white differences in COVID-19 infection rates have narrowed since the initial wave of the pandemic (CDC, 2022b; Wong et al., 2021).
Strengths of the current study include utilization of an individual-level data source to examine the importance of multiple social determinants of health as contributors to racial/ethnic disparities in COVID-19. Most existing evidence on the association between the social determinants of health and racial/ethnic disparities in COVID-19 used aggregate level data. We also use a nationally representative sample of U.S. adults with over a year of follow-up, overcoming the limitations of previous studies that typically relied on geographically narrow sampling designs or observed only early COVID-19 cases during the first wave of the pandemic.
Despite these strengths, we acknowledge several limitations. First, individuals who had severe symptoms of COVID-19 may have been lost or dropped out of the survey, which may result in misspecification of COVID-19 diagnosis. Further, depending on timing and geographic context, underdiagnosis of COVID-19 may be racially patterned such that our results are conservative estimates of the magnitude of infection disparities. Second, unobserved variables such as the occupational characteristics of household members may contribute to the association between race/ethnicity and risk of COVID-19. Previous research has found that Black and Hispanic Americans are more likely than whites to live with individuals working in jobs at high risk of exposure to COVID-19 (Kong et al., 2021; Selden and Berdahl, 2020). Third, due to sample constraints we were unable to estimate separate results for Native American or Pacific Islander individuals, two groups that have been documented to have higher rates of COVID-19. Lastly, structural racism is deeply rooted in myriad discriminatory practices in federal, state, and local policies that harm minoritized communities and multiple unmeasured mechanisms likely put Hispanic and Black individuals at higher risk for COVID-19 infection (Zalla et al., 2021). For example, due to the differential application of environmental regulations, Black and Hispanic people are more likely to live in communities with poorer air quality (Jones et al., 2014) which may exacerbate infection risk (Fattorini and Regoli, 2020). Future research exploring important yet unmeasured contextual factors shaped by structural racism is critically needed to expand our understanding of the association between structural racism and racial/ethnic disparities in COVID-19 via the social determinants of health.
While vaccines are now widely available in the U.S., COVID-19 cases are quickly rising yet again due to the surge in infections caused by new variants (CDC, 2022b). Racial/ethnic minorities appear to still be disproportionately affected by new COVID-19 surges (Andrasfay and Goldman, 2022; CDC, 2022b). Our study suggests that several key social determinants of health influence the risk of COVID-19 but the influence of structural racism on COVID-19 infection goes beyond these factors to contribute to racial/ethnic disparities. Future research should continue to explore the proximate determinants of these racial/ethnic inequalities because such information is necessary to target policies and interventions to block structural racism from influencing COVID-19 outcomes and prevent further infection among people at high risk.
Credit author statement
Haena Lee: Conceptualization; Methodology; Visualization; Writing – original draft; Writing – review & editing. Theresa Andrasfay: Conceptualization; Data curation; Formal analysis; Visualization; Writing – original draft; Writing – review & editing. Alicia Riley: Conceptualization; Writing – review & editing. Qiao Wu: Data curation; Writing – original draft. Eileen M. Crimmins: Funding acquisition; Supervision; Writing – review & editing.
Acknowledgments
Support for this study was provided by grants from the National Institute on Aging (T32 AG000037 and P30 AG017265). The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. The collection of the UAS COVID-19 tracking data is supported in part by the Bill & Melinda Gates Foundation and by grant U01AG054580 from the National Institute on Aging, and many others.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.115098.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Andrasfay T., Goldman N. Association of the COVID-19 pandemic with estimated life expectancy by race/ethnicity in the United States, 2020. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.14520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay T., Goldman N. 2022. Reductions in US Life Expectancy from COVID-19 by Race and Ethnicity: Is 2021 a Repetition of 2020? [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay T., Wu Q., Lee H., Crimmins E. Adherence to social distancing and personal hygiene behavior guidelines and risk of COVID-19 diagnosis: evidence from the understanding America study. Am. J. Publ. Health. 2022;112:169–178. doi: 10.2105/AJPH.2021.306565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badri S., Sardá V., Moncada J.S., Merçon M., Rezai K., Weinstein R.A., Trick W.E. Disparities and temporal trends in COVID-19 exposures and mitigating behaviors among Black and hispanic adults in an urban setting. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.25187. e2125187–e2125187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binette J., Houghton A., Firestone S. AARP; 2021. Living in a Multigenerational Household before and during COVID-19. [WWW Document] [DOI] [Google Scholar]
- Blau F.D., Koebe J., Meyerhofer P.A. National Bureau of Economic Research; 2020. Who Are the Essential and Frontline Workers? (Working Paper No. 27791), Working Paper Series. [DOI] [Google Scholar]
- Bonilla-Silva E. Color-blind racism in pandemic times. Soc. Race Ethn. 2020 doi: 10.1177/2332649220941024. 2332649220941024. [DOI] [Google Scholar]
- Bureau of Labor Statistics . 2018. Consumer Expenditures in 2018 : BLS Reports: U.S. Bureau of Labor Statistics.https://www.bls.gov/opub/reports/consumer [WWW Document] [Google Scholar]
- Carlsten C., Gulati M., Hines S., Rose C., Scott K., Tarlo S.M., Torén K., Sood A., Hoz de la R.E. COVID-19 as an occupational disease. Am. J. Ind. Med. 2021;64:227–237. doi: 10.1002/ajim.23222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau U.S. 2020. Income and Poverty in the United States: 2020.https://www.census.gov/library/publications/2021/demo/p60-273.html [WWW Document]. Census.gov. 3.2.22. [Google Scholar]
- Centers for Disease Control and Prevention . 2022. Cases, Data, and Surveillance [WWW Document]. Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity.https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html 4.28.22. [Google Scholar]
- Centers for Disease Control and Prevention . 2022. COVID-19 Weekly Cases and Deaths Per 100,000.https://covid.cdc.gov/covid-data-tracker/#demographicsovertime Population by Age, Race/Ethnicity, and Sex [WWW Document] 4.28.22. [Google Scholar]
- Chen J.T., Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J. Publ. Health Manag. Pract. 2021;27:S43–S56. doi: 10.1097/PHH.0000000000001263. [DOI] [PubMed] [Google Scholar]
- Chen J.T., Testa C., Waterman P., Krieger N. Harvard Center for Population and Development Studies, HCPDS Working Paper; 2021. Intersectional Inequities in COVID-19 Mortality by Race/ethnicity and Education in the United States, January 1, 2020–January 31, 202; pp. 21–22. [Google Scholar]
- Chen Y.-H., Glymour M., Riley A., Balmes J., Duchowny K., Harrison R., Matthay E., Bibbins-Domingo K. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through November 2020. PLoS One. 2021;16 doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie A., Mbaeyi S.A., Walensky R.P. CDC interim recommendations for fully vaccinated people: an important first step. JAMA. 2021;325:1501–1502. doi: 10.1001/jama.2021.4367. [DOI] [PubMed] [Google Scholar]
- Clouston S.A.P., Natale G., Link B.G. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc. Sci. Med. 2021;268 doi: 10.1016/j.socscimed.2020.113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn D., Passel J.S. Pew Research Center; 2018. A Record 64 Million Americans Live in Multigenerational Households.https://www.pewresearch.org/fact-tank/2018/04/05/a-record-64-million-americans-live-in-multigenerational-households/ [WWW Document] 10.7.21. [Google Scholar]
- Cox-Ganser J.M., Henneberger P.K. Occupations by proximity and indoor/outdoor work: relevance to COVID-19 in all workers and black/hispanic workers. Am. J. Prev. Med. 2021;60:621–628. doi: 10.1016/j.amepre.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Credit K. Neighbourhood inequity: exploring the factors underlying racial and ethnic disparities in COVID-19 testing and infection rates using ZIP code data in Chicago and New York. Reg. Sci. Pol. Pract. 2020;12:1249–1271. doi: 10.1111/rsp3.12321. [DOI] [Google Scholar]
- Dalsania A.K., Fastiggi M.J., Kahlam A., Shah R., Patel K., Shiau S., Rokicki S., DallaPiazza M. The relationship between social determinants of health and racial disparities in COVID-19 mortality. J. Racial Ethnic Health Disparities. 2021;9:288–295. doi: 10.1007/s40615-020-00952-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do D.P., Frank R. Unequal burdens: assessing the determinants of elevated COVID-19 case and death rates in New York City's racial/ethnic minority neighbourhoods. J. Epidemiol. Community Health. 2021;75:321–326. doi: 10.1136/jech-2020-215280. [DOI] [PubMed] [Google Scholar]
- Dunbar A., Jones N.E. Race, police, and the pandemic: considering the role of race in public health policing. Ethn. Racial Stud. 2021;44:773–782. doi: 10.1080/01419870.2020.1851381. [DOI] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman J.M., Bassett M.T. Variation in COVID-19 mortality in the US by race and ethnicity and educational attainment. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.35967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielding-Miller R.K., Sundaram M.E., Brouwer K. Social determinants of COVID-19 mortality at the county level. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M.A., Homan P.A., García C., Brown T.H. The color of COVID-19: structural racism and the disproportionate impact of the pandemic on older Black and Latinx adults. J. Gerontol.: Ser. B. 2021;76:e75–e80. doi: 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg S., Patel K., Pham H., Whitaker M., O'Halloran A., Milucky J., Anglin O., Kirley P.D., Reingold A., Kawasaki B., Herlihy R., Yousey-Hindes K., Maslar A., Anderson E.J., Openo K.P., Weigel A., Teno K., Ryan P.A., Monroe M.L., Reeg L., Kim S., Como-Sabetti K., Bye E., Shrum Davis S., Eisenberg N., Muse A., Barney G., Bennett N.M., Felsen C.B., Billing L., Shiltz J., Sutton M., Abdullah N., Talbot H.K., Schaffner W., Hill M., Chatelain R., Wortham J., Taylor C., Hall A., Fry A.M., Kim L., Havers F.P. Clinical trends among U.S. Adults hospitalized with COVID-19, March to december 2020. Ann. Intern. Med. 2021 doi: 10.7326/M21-1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons J. Distancing the socially distanced: racial/ethnic composition's association with physical distancing in response to COVID-19 in the U.S. PLoS One. 2021;16 doi: 10.1371/journal.pone.0251960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N., Pebley A.R., Lee K., Andrasfay T., Pratt g. 2021. Racial and Ethnic Differentials in COVID-19-Related Job Exposures by Occupational Standing in the US. medRxiv 2020.11.13.20231431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer M.L., Sample S., Jensen H.K., McBain S., Lipschitz R., Sexton K.W. COVID-19 is connected with lower health literacy in rural areas. Stud. Health Technol. Inf. 2021;281:804–808. doi: 10.3233/SHTI210286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Hamidi I. Subway ridership, crowding, or population density: determinants of COVID-19 infection rates in New York city. Am. J. Prev. Med. 2021;60:614–620. doi: 10.1016/j.amepre.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins D., Davis L., Kriebel D. COVID-19 deaths by occupation, Massachusetts, March 1–July 31, 2020. Am. J. Ind. Med. 2021;64:238–244. doi: 10.1002/ajim.23227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson M., Chang T., Shah M., Pramanik R., Shah S.B. Racial and ethnic disparities in SARS-CoV-2 testing and COVID-19 outcomes in a Medicaid managed care cohort. Am. J. Prev. Med. 2021;61:644–651. doi: 10.1016/j.amepre.2021.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M.R., Diez-Roux A.V., Hajat A., Kershaw K.N., O'Neill M.S., Guallar E., Post W.S., Kaufman J.D., Navas-Acien A. Race/ethnicity, residential segregation, and exposure to ambient air pollution: the multi-ethnic study of atherosclerosis (MESA) Am. J. Publ. Health. 2014;104:2130–2137. doi: 10.2105/AJPH.2014.302135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.K., Crimmins E.M. How does age affect personal and social reactions to COVID-19: results from the national Understanding America Study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong S.T.J., Lee R.Y., Rodriguez F., Scheinker D. Racial and ethnic disparities in household contact with individuals at higher risk of exposure to COVID-19. J. Gen. Intern. Med. 2021;36:1470–1472. doi: 10.1007/s11606-021-06656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laster Pirtle W.N. Racial capitalism: a fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Educ. Behav. 2020;47:504–508. doi: 10.1177/1090198120922942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey K., Ayers C.K., Kondo K.K., Saha S., Advani S.M., Young S., Spencer H., Rusek M., Anderson J., Veazie S., Smith M., Kansagara D. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths. Ann. Intern. Med. 2021;174:362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015;41:311–330. [Google Scholar]
- Phillips M. Diversity in American Higher Education. Routledge; New York, NY: 2011. Ethnic and social class disparities in academic skills: their origins and consequences; pp. 7–24. [Google Scholar]
- Podewils L.J., Burket T.L., Mettenbrink C., Steiner A., Seidel A., Scott K., Cervantes L., Hasnain-Wynia R. Disproportionate incidence of COVID-19 infection, hospitalizations, and deaths among persons identifying as hispanic or latino - denver, Colorado march-october 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1812–1816. doi: 10.15585/mmwr.mm6948a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentsch C.T., Kidwai-Khan F., Tate J.P., Park L.S., Jr J.T.K., Skanderson M., Hauser R.G., Schultze A., Jarvis C.I., Holodniy M., Iii V.L.R., Akgün K.M., Crothers K., Taddei T.H., Freiberg M.S., Justice A.C. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A.R., Chen Y.-H., Matthay E.C., Glymour M.M., Torres J.M., Fernandez A., Bibbins-Domingo K. Excess mortality among latino people in California during the COVID-19 pandemic. SSM - Population Health. 2021:100860. doi: 10.1016/j.ssmph.2021.100860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Diaz C.E., Guilamo-Ramos V., Mena L., Hall E., Honermann B., Crowley J.S., Baral S., Prado G.J., Marzan-Rodriguez M., Beyrer C., Sullivan P.S., Millett G.A. Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Ann. Epidemiol. 2020;52 doi: 10.1016/j.annepidem.2020.07.007. 46-53.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selden T.M., Berdahl T.A. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff. 2020;39:1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- Smail E., Schneider K.E., DeLong S.M., Willis K., Arrington-Sanders R., Yang C., Alexander K.A., Johnson R.M. Health beliefs and preventive behaviors among adults during the early COVID-19 pandemic in the United States: a latent class Analysis. Prev. Sci. 2021;22:1013–1022. doi: 10.1007/s11121-021-01273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sy K.T.L., Martinez M.E., Rader B., White L.F. Socioeconomic disparities in subway use and COVID-19 outcomes in New York city. Am. J. Epidemiol. 2021;190:1234–1242. doi: 10.1093/aje/kwaa277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi P.G., Thomas K., Shah M.D., Vizueta N., Cui Y., Vangala S., Fox C., Kapteyn A. The role of trust in the likelihood of receiving a COVID-19 vaccine: results from a national survey. Prev. Med. 2021;153 doi: 10.1016/j.ypmed.2021.106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur N., Lovinsky-Desir S., Bime C., Wisnivesky J.P., Celedón J.C. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic. What's our role? Am. J. Respir. Crit. Care Med. 2020;202:943–949. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unnikrishnan A., Figliozzi M. Civil and Environmental Engineering Faculty Publications and Presentations; 2020. A Study of the Impact of COVID-19 on Home Delivery Purchases and Expenditures. [Google Scholar]
- Villarreal A. The Guardian; 2020. ‘You Can't Get Close, yet You Can't Stay Away’: Latino Cultural Beliefs Clash with Pandemic Safety. [Google Scholar]
- Whaley C.M., Cantor J., Pera M., Jena A.B. Assessing the association between social gatherings and COVID-19 risk using birthdays. JAMA Intern. Med. 2021;181:1090–1099. doi: 10.1001/jamainternmed.2021.2915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Publ. Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M.S., Haderlein T.P., Yuan A.H., Moy E., Jones K.T., Washington D.L. Time trends in racial/ethnic differences in COVID-19 infection and mortality. Int. J. Environ. Res. Publ. Health. 2021;18:4848. doi: 10.3390/ijerph18094848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalla L.C., Martin C.L., Edwards J.K., Gartner D.R., Noppert G.A. A geography of risk: structural racism and coronavirus disease 2019 mortality in the United States. Am. J. Epidemiol. 2021;190:1439–1446. doi: 10.1093/aje/kwab059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao E., Wu Q., Crimmins E.M., Ailshire J.A. Media trust and infection mitigating behaviours during the COVID-19 pandemic in the USA. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2020-003323. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.