Abstract
Aims
To compare the effectiveness of cervical epidural injections of local anesthetic with vs. without a steroid.
Methods
Three databases (PubMed, Embase, and Cochrane library) were used to search and assess all clinical randomized controlled trials regarding the clinical efficacy of epidural injections from January 01, 2009, to October 31, 2020. Cochrane review criteria and the Interventional Pain Management Techniques-Quality Appraisal of Reliability and Risk of Bias Assessment instrument were used to evaluate the methodologic quality of the included studies. Qualitative and quantitative analyses were performed according to best evidence synthesis principles and by single-arm meta-analysis, respectively.
Results
Based on the search criteria, 4 RCTs were qualitatively and quantitatively analyzed in the single-arm meta-analysis. Treatment with lidocaine alone or with the steroid resulted in decreases of 4.46 and 4.29 points, respectively, in pain scores and of 15.8 and 14.46 points, respectively, in functional scores at 6 months. Similar trends were observed at the 1-year follow-up: pain scores decreased by 4.27 and 4.14 points, while functional scores decreased by 15.94 and 14.44 points in patients with neck pain who received lidocaine without or with the steroid, respectively. In the 3 studies that reported 2-year follow-up data, patients with neck pain treated with lidocaine or lidocaine + steroid showed 4.2- and 4.14-point decreases, in pain score and 15.92- and 14.89-point decreases, respectively, in functional scores.
Conclusions
The studies showed level I (strong) evidence for short- and long-term improvements in pain relief and functionality with cervical epidural injections of local anesthetic alone or with a steroid in the management of neck pain.
1. Introduction
Degenerative cervical spine lesions and cervical postoperative syndrome are the leading causes of neck pain, including cervical disc herniation and cervical stenosis, which bring higher economic burdens and disability rates to society [1–5]. Chronic cervical pain not only increases the burden of life on patients but also increases the psychological burden of patients and now ranks third among conditions that contribute to disability [6]. Current clinical treatment options for neck pain include conservative and surgical treatment. Conservative treatment is mainly oral drugs and physical therapy. However, conservative treatment is generally ineffective in the treatment of refractory neck pain, oral medication will increase the burden on the gastrointestinal tract, and adverse reactions such as gastric ulcers and bleeding may occur. However, the rate of reoperation due to the failure of surgical interventions is 32% [7–17]. Cervical epidural injections have been widely used to manage neck pain [18], especially in patients who are poor candidates for surgery [19, 20]. Although a number of randomized trials have investigated the efficacy of cervical epidural injections of local anesthetics alone or in conjunction with steroids, the long-term effectiveness of these treatments in managing chronic neck pain is controversial [8, 10, 12, 21–28].
Steroids are used in cervical epidural injections to control inflammation and suppress edema of the nerve root. In a preliminary report of a systematic review and meta-analysis of the efficacy of fluoroscopically guided cervical epidural steroid injection for the treatment of radicular pain, improvements in vital functions were reported in 58% of patients at 2 months [29]. The mechanisms of action of steroids include suppression of ectopic discharges from inflamed nerves as well as proinflammatory cytokines, improvement of blood flow, and lysing of iatrogenic and inflammatory adhesions [30]. Besides neck pain, steroids are widely used to manage painful diseases including osteoarthritis and gout and are typically combined with local anesthetics to achieve greater efficacy. However, local anesthetics alone can have a comparable effect in terms of pain relief, and there is no evidence that this is enhanced by the addition of steroids. Some studies have reported similar degrees of pain relief and functional improvement in patients with neck pain secondary to disc herniation or postsurgery syndrome who were treated by cervical epidural injections of local anesthetics without or with steroids [31–35].
In order to address this controversy, we carried out a systematic review and meta-analysis evaluating the long-term efficacy of cervical epidural injections with a local anesthetic alone or combined with a steroid in the management of neck pain.
2. Methods
2.1. Study Identification and Search Strategy
The PubMed (http://www.ncbi.nlm, http://nih.gov/pubmed), Embase (http://www.embase.com), and Cochrane library (http://www.thecochranelibrary.com) databases were searched for studies published between January 2009 to October 2020. The following search terms were used: (((((“injections, epidural” OR ((((((((((Extradural Injections OR Peridural Injections OR AND Peridural OR ((“injections” OR “injections” OR “injection” [All Fields]) AND (“Neck Pain” OR ((((((((((((((((((((((((((((((((((((((((Neck Pains OR Pain, Neck OR ((“pain” OR “pain” OR “pains”) AND Neck)) OR Neck Ache AND Cervical OR Posterior Cervical Pain AND Anterior Cervical) OR Anterior Neck Pain OR (Anterior [All Fields] AND Neck Pains)) OR ((“neck pain” [MeSH Terms] OR (“neck” AND “pain”) OR “neck pain”) AND Anterior) OR ((“neck pain” OR (“neck” [All Fields] AND “pain”) OR “neck pain” OR (“neck” AND “pains”) OR “neck pains”) AND (“2009/01/01” [PDAT]: “2020/10/20” [PDAT])))) AND (((((randomized controlled trial [Title/Abstract]) OR randomized [Title/Abstract]) OR placebo [Title/Abstract])) OR (((((((((Health Care Category [Title/Abstract]) OR (Environment [Title/Abstract] AND Public Health [Title/Abstract])) OR Public Health [Title/Abstract]) OR Epidemiologic Methods [Title/Abstract]) OR Epidemiologic Study Characteristics [Title/Abstract]) OR Epidemiologic Studies [Title/Abstract]) OR Case-Control Studies [Title/Abstract])) OR “Retrospective Studies”[MeSH])).
2.2. Study Selection
All studies that described the management of chronic neck pain and included outcome evaluations over a period of at least 6 months were reviewed. All randomized trials in all languages with appropriate statistical analyses were included. Study type: randomized controlled trial (RCT). Patients: all patients with neck pain secondary to cervical disc herniation, spondylosis, cervical, or postsurgery syndrome treated with cervical epidural injections of local anesthetic alone or in conjunction with a steroid. Intervention: cervical interlaminar injections of anesthetic (lidocaine) and steroid (betamethasone). Outcome: for pain relief, a 50% decrease from the baseline pain score or a change of at least 3 points on an 11-point pain scale was considered clinically significant. For functional status improvement, a change of ≥30% in disability score or 50% improvement from baseline was considered clinically significant. A study was judged to be positive if the effectiveness of the therapy was demonstrated through comparison with a control group or from baseline to follow-up. A negative study was defined as one in which no difference was seen as a result of the treatment or in which there was no measurable improvement from baseline. Reference point measurements were at 6 months, 1 year, and 2 years. Book chapters, case reports, and reports without a definitive diagnosis were excluded. Studies in which patients had acute trauma, fractures, malignancies, and inflammatory diseases were also excluded.
2.3. Data Collection
Two investigators independently performed the initial search and completed study screening and data extraction according to the selection criteria. Disagreements were resolved through discussion between 2 investigators; a third investigator was consulted in cases where a consensus could not be reached. Data synthesis and analysis, including assessment of study quality, were performed by the 2 investigators, with a third investigator consulted as needed.
2.4. Methodological Quality of Studies
Cochrane review and the Interventional Pain Management Techniques Quality Appraisal of Reliability and Risk of Bias Assessment (IPM-QRB) criteria were used to evaluate the quality of each individual article for RCTs. Studies meeting at least 9 of the 13 Cochrane review inclusion criteria were considered to be of high quality; those meeting 5–8 criteria were deemed to be of moderate quality; and those meeting <5 criteria were low-quality studies that were excluded. Studies meeting the IPM-QRB inclusion criteria with a score of 32–48 were considered to be of high quality and were included in the analysis; those with a score of 16–31 were judged as being of moderate quality; and those meeting the inclusion criteria but with a score < 16 were low-quality studies that were excluded.
The methodologic quality and internal validity of each publication, as well as the quality of evidence, were independently assessed in an unblinded, standardized manner by 2 investigators. In the case of any disagreements, a third investigator performed the assessment and a consensus was reached. Outstanding issues were resolved through a discussion involving all investigators. The evidence was analyzed based on best-evidence synthesis principles and was modified and collated according to multiple criteria including Cochrane review and United States Preventive Services Task Force criteria (Table 1). The analysis was conducted based on 5 levels of evidence ranging from strong to opinion- or consensus-based. The results of best evidence as determined by the evidence level were used. If there were any conflicts of interest (e.g., authorship), the investigator in question was recused from the review of evidence.
Table 1.
Qualitative modified approach to grading of evidence.
| Level | Strength of evidence | Description |
|---|---|---|
| I | Strong | Evidence obtained from multiple relevant high-quality randomized controlled trials |
|
| ||
| II | Moderate | Evidence obtained from at least one relevant high-quality randomized controlled trial or multiple relevant moderate- or low-quality randomized controlled trials |
|
| ||
| III | Fair | Evidence obtained from at least one relevant moderate- or low-quality randomized controlled trial with multiple relevant observational studies OR Evidence obtained from at least one relevant high-quality nonrandomized trial or observational study with multiple moderate- or low-quality observational studies |
|
| ||
| IV | Limited | Evidence obtained from multiple moderate- or low-quality relevant observational studies |
|
| ||
| V | Consensus-based | Opinion or consensus of a large group of clinicians and/or scientists |
2.5. Statistical Analysis
The single-arm meta-analysis was performed using Comprehensive Meta-analysis v3.0 (Biostat, Englewood, NJ, USA). The I2 statistic was used to assess the heterogeneity of included studies. Data were displayed as forest plots to evaluate treatment effects. Pain and functional status improvement data from the included studies are reported as standardized mean differences with 95% confidence interval. All analyses were based on treatment modality and the injected solution. Short- and long-term improvement was defined as any improvement at 6 months and after 6 months, respectively.
3. Results
3.1. Study Selection
A flow diagram of the study selection process according to PRISMA guidelines is shown in Figure 1. Based on the search criteria, 10 publications were considered for inclusion; 6 of these were excluded because of duplicate publications or lack of data. Ultimately, 4 RCTs [31, 32, 34, 36] were included in the present analysis.
Figure 1.
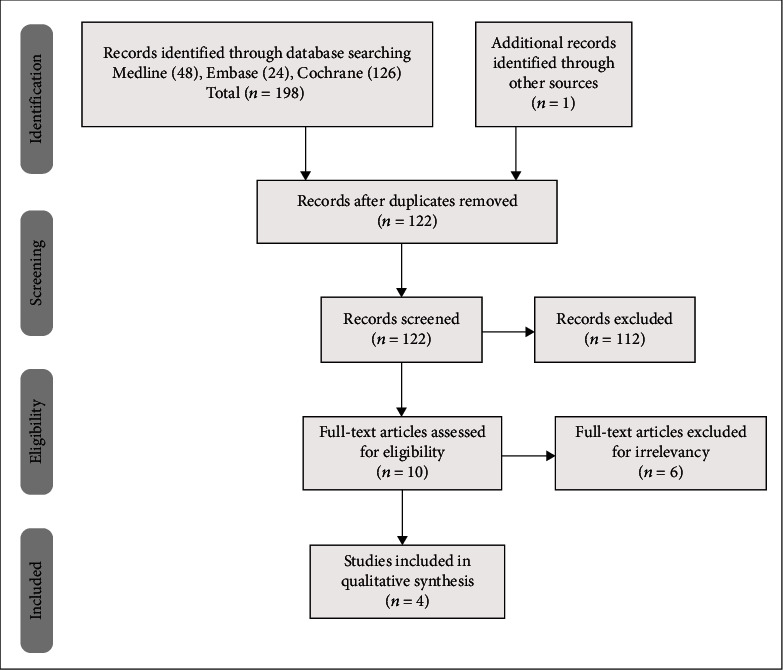
Flow diagram illustrating published literature evaluating epidural injection in neck pain.
3.2. Methodologic Quality and Risk of Bias Assessment
The results of the methodologic quality and risk of bias assessments for each of the included studies are shown in Tables 2 and 3. According to Cochrane review and IPM-QRB criteria [37, 38], all of the RCTs were of high quality.
Table 2.
Methodologic quality assessment according to Cochrane review criteria.
| Manchikanti 2012 (36) |
Manchikanti 2013 (37) |
Manchikanti 2014 (38) |
Manchikanti 2018 (39) |
|
|---|---|---|---|---|
| Adequate randomization | Y | Y | Y | Y |
| Concealed treatment allocation | Y | Y | Y | Y |
| Patient blinded | Y | Y | Y | Y |
| Care provider blinded | Y | Y | Y | Y |
| Outcome assessor blinded | N | N | N | N |
| Dropout rate described | Y | Y | Y | Y |
| All randomized participants analyzed in the group | Y | Y | Y | Y |
| Reports of the study free of suggestion of selective outcome reporting | Y | Y | Y | Y |
| Groups similar at baseline with respect to most important prognostic indicators | N | Y | N | N |
| Cointerventions avoided or similar | Y | Y | Y | Y |
| Compliance acceptable in all group | Y | Y | Y | Y |
| Time of outcome assessment in all groups similar | Y | Y | Y | Y |
| Other sources of potential bias unlikely | Y | Y | Y | Y |
| Score | 11/13 | 12/13 | 11/13 | 11/13 |
Y: yes; N: no; U: unclear.
Table 3.
Methodologic quality assessment using the Interventional Pain Management Techniques-Quality Appraisal of Reliability and Risk of Bias Assessment instrument.
| Manchikanti 2012 (36) |
Manchikanti 2013 (37) |
Manchikanti 2014 (38) |
Manchikanti 2018 (39) |
|
|---|---|---|---|---|
| I. Trial design and guidance reporting | ||||
| 1. Consort or spirit | 3 | 3 | 3 | 3 |
| II. Design factors | ||||
| 2. Type and design of trial | 2 | 2 | 2 | 2 |
| 3. Setting/physician | 2 | 2 | 2 | 2 |
| 4. Imaging | 3 | 3 | 3 | 3 |
| 5. Sample size | 2 | 3 | 3 | 2 |
| 6. Statistical methodology | 1 | 1 | 1 | 1 |
| III. Patient factors | ||||
| 7. Inclusiveness of population | 2 | 2 | 2 | 2 |
| 8. Duration of pain | 2 | 2 | 2 | 2 |
| 9. Previous treatments | 2 | 2 | 2 | 2 |
| 10. Duration of follow-up with appropriate interventions | 2 | 3 | 3 | 2 |
| IV. Outcomes | ||||
| 11. Outcome assessment criteria for significant improvement | 4 | 4 | 4 | 4 |
| 12. Analysis of all randomized participants in the groups | 2 | 2 | 2 | 2 |
| 13. Description of dropout rate | 2 | 2 | 2 | 2 |
| 14. Similarity of groups at baseline for important prognostic indicators | 1 | 0 | 1 | 1 |
| 15. Role of cointerventions | 1 | 1 | 1 | 1 |
| V. Randomization | ||||
| 16. Method of randomization | 2 | 2 | 2 | 2 |
| VI. Allocation concealment | ||||
| 17. Concealed treatment allocation | 2 | 2 | 2 | 2 |
| VII. Blinding | ||||
| 18. Patient blinding | 1 | 1 | 1 | 1 |
| 19. Care provider blinding | 1 | 1 | 1 | 1 |
| 20. Outcome assessor blinding | 0 | 0 | 0 | 0 |
| VIII. Conflicts of interest | ||||
| 21. Funding and sponsorship | 2 | 2 | 2 | 2 |
| 22. Conflicts of interest | 3 | 3 | 3 | 3 |
| Score | 42 | 43 | 44 | 42 |
3.3. Study Characteristics
The characteristics and outcomes of the included studies are shown in Table 4. The studies were not heterogeneous. One RCT [36] followed up patients treated with epidural injections of a steroid (n = 30) or without the steroid (n = 30) for 1 year; 50% pain relief associated with a 50% functional improvement was considered significant. Work status was also an outcome measure; at the 1-year follow-up, the effectiveness in terms of pain relief and functional improvement was 71.5%. The second RCT [32] included 120 patients, and the interventions and outcome measures for each group were similar to those in the first RCT. The rates of effectiveness for pain relief and functional improvements were 72% and 68% in patients who received epidural injections without and with the steroid, respectively. The third and fourth RCTs had similar interventions and outcome measures as the first 2, but the follow-up time was 2 years. One study [34] showed improvements in pain and function after an average of 6 treatment sessions over a period of 2 years. In the other study [31], patients receiving epidural injections without the steroid experienced 65.6 ± 37.8 weeks of pain relief over a period of 2 years compared to 59.4 ± 34.2 weeks in those receiving injections that included the steroid, with no significant difference between groups.
Table 4.
Characteristics of included studies on cervical epidural injections in neck pain.
| Study/study type Methodologic quality scoring |
Participants and interventions | Outcome measure | Follow-up period | Conclusions |
|---|---|---|---|---|
| Manchikanti et al. (36)/RCT Quality scores: Cochrane = 11/13; IPM − QRB = 42/48 |
N = 60 Epidural injections without steroid, n = 30 Epidural injections with steroid, n = 30 Group I: cervical interlaminar epidural injections with 5 ml of 0.5% lidocaine Group II: cervical interlaminar epidural injections with 4 ml of 0.5% lidocaine mixed with 1 mL or 6 mg of nonparticulate betamethasone |
NDI, NRS, opioid intake, work status | 1 year | Cervical interlaminar epidural injections had an efficacy of 71.5% for pain reduction and improvement in functional status for neck pain. |
|
| ||||
| Manchikanti et al. (37)/RCT Quality scores: Cochrane = 12/13; IPM − QRB = 43/48 |
N = 120 Epidural injections without steroid, n = 60 Epidural injections with steroid, n = 60 Group I: cervical interlaminar epidural injections with 5 ml of 0.5% lidocaine Group II: cervical interlaminar epidural injections with 4 ml of 0.5% lidocaine mixed with 1 ml or 6 mg of nonparticulate betamethasone |
NDI, NRS, opioid intake, work status | 2 years | Cervical interlaminar epidural injections for chronic neck pain was effective in 72% of patients in group I and 68% of patients in group 2. |
|
| ||||
| Manchikanti et al. (38)/RCT Quality scores: Cochrane = 11/13 IPM − QRB = 44/48 |
N = 120 Epidural injections without steroid, n = 60 Epidural injections with steroid, n = 60 Group I: cervical interlaminar epidural injections with 5 mL of 0.5% lidocaine Group II: cervical interlaminar epidural injections with 4 ml of 0.5% lidocaine mixed with 1 ml or 6 mg of nonparticulate betamethasone |
NDI, NRS, opioid intake, work status | 2 years | Cervical epidural injections of local anesthetic with or without steroids were effective in 71% of patients. |
|
| ||||
| Manchikanti et al. (39)/RCT Quality scores: Cochrane = 11/13 IPM − QRB = 42/48 |
N = 116 Epidural injections without steroid, n = 58 Epidural injections with steroid, n = 58 Group I: cervical interlaminar epidural injections with 5 ml of 0.5% lidocaine Group II: cervical interlaminar epidural injections with 4 ml of 0.5% lidocaine mixed with 6 mg of nonparticulate betamethasone |
NDI, NRS, work status | 2 years | Cervical interlaminar epidural injections for chronic neck pain alleviated pain relief and improved functional status by ≥50% in 69% of patients in group I and 71% of patients in group 2 at the 2-year follow-up. |
IPM-QRB: Interventional Pain Management Techniques-Quality Appraisal of Reliability and Risk of Bias Assessment; NDI: Neck Disability Index; NRS: numeric rating scale; RCT: randomized controlled trial.
3.4. Analysis of Study Quality
The quality of evidence of the included studies was assessed using a modified version of evidence grading [39] with high evidence (level I) from multiple relevant high-quality RCTs. All studies reported pain relief and functional improvement in patients who received epidural injections with or without the steroid. Conventional meta-analysis was not feasible because there were no significant differences between patients receiving epidural injections with lidocaine alone vs lidocaine + steroid. To assess pain relief and functional improvement, we performed a single-arm meta-analysis of the data from the 4 studies [31, 32, 34, 36].
3.5. Pain and Functionality at 6 Months, 1 Year, and 2 Years
Four studies [31, 32, 34, 36] were included in this single-arm meta-analysis of pain relief and functional improvement (Figures 2(a) and 2(b)). Treatment with lidocaine alone or with the steroid resulted in decreases of 4.46 and 4.29 points, respectively, in pain scores (Figures 3(a) and 3(b)) and of 15.8 and 14.46 points, respectively, in functional scores (Figures 2(a) and 2(b)) at 6 months. Similar trends were observed at the 1-year follow-up: pain scores decreased by 4.27 and 4.14 points (Figures 4(a) and 4(b)), while functional scores decreased by 15.94 and 14.44 points (Figures 5(a) and 5(b)) in patients with neck pain who received lidocaine without or with the steroid, respectively. In the 3 studies that reported 2-year follow-up data [31, 32, 34], patients with neck pain treated with lidocaine or lidocaine + steroid showed 4.2- and 4.14-point decreases, in pain score (Figures 6(a) and 6(b)) and 15.92- and 14.89-point decreases, respectively, in functional scores (Figures 7(a) and 7(b)).
Figure 2.
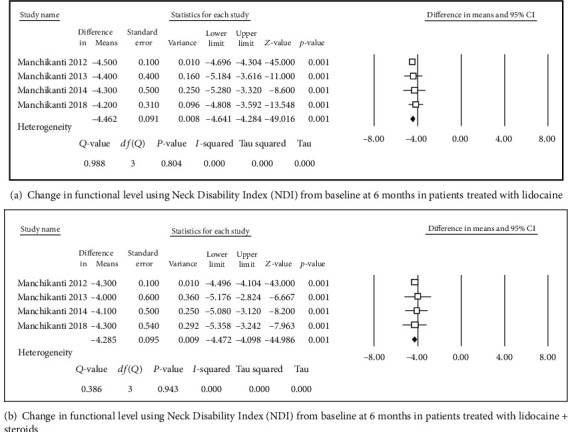
Change in functional level using Neck Disability Index (NDI).
Figure 3.
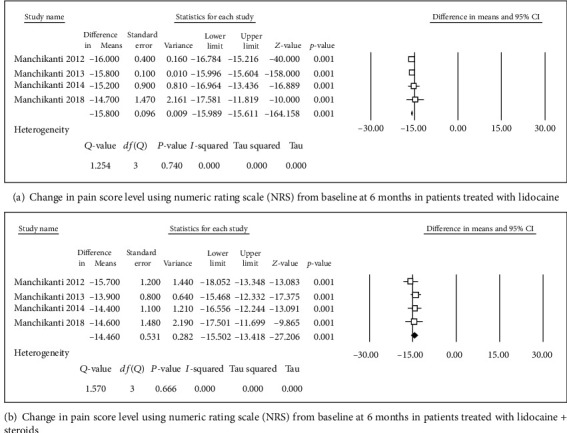
Change in pain score level using numeric rating scale (NRS).
Figure 4.
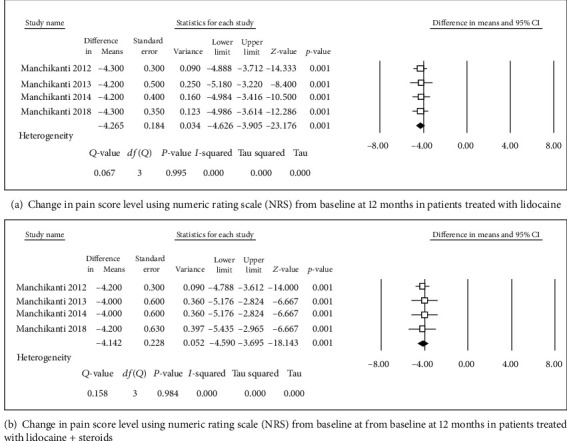
Change in pain score level using numeric rating scale (NRS).
Figure 5.
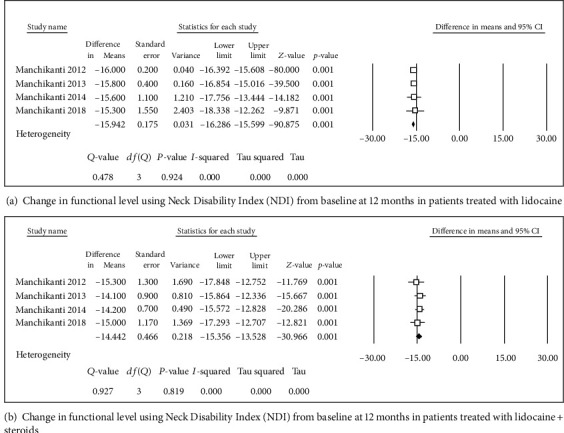
Change in functional level using Neck Disability Index (NDI).
Figure 6.
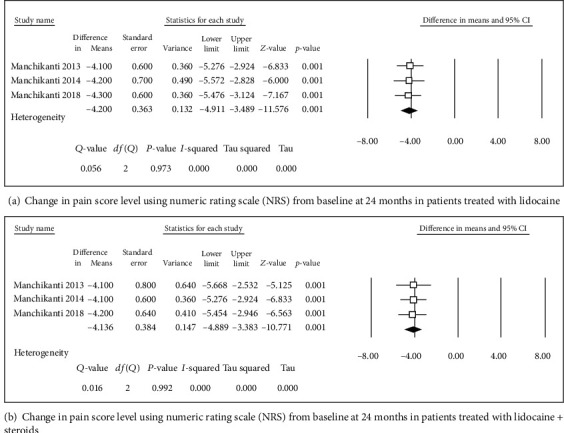
Change in pain score level using numeric rating scale (NRS).
Figure 7.
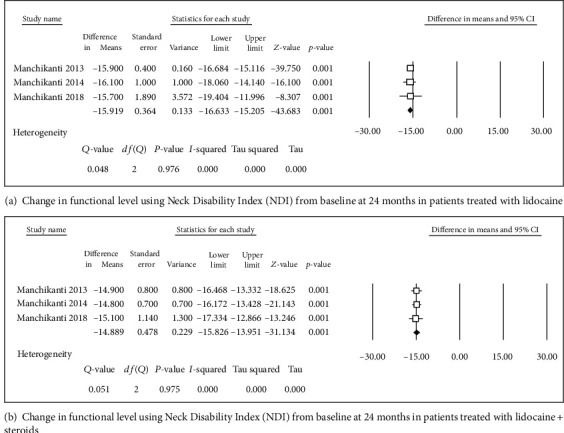
Change in functional level using Neck Disability Index (NDI).
4. Discussion
This systematic review and single-arm meta-analysis of 4 RCTs provided evidence that cervical epidural injections with lidocaine alone or in combination with the steroid betamethasone alleviated pain and improved functionality in patients with neck pain. According to Cochrane review and IPM-QRB criteria, all studies were of high quality. Furthermore, the studies included descriptions of sample size and employed similar injection approaches and pharmacologic agents, which increased the reliability and consistency, respectively, of reported outcomes. All of the studies demonstrated that both treatments were effective for the management of neck pain secondary to cervical disc herniation, spondylosis, or postsurgery syndrome. One of the studies [36] included 1-year follow-up data and the other 3 [31, 32, 34] followed up patients for 2 years, which reduced the bias in outcome reporting. Additionally, opioid intake by the patients was significant decreased by the 2 two treatments. However, there was no significant difference between the 2 treatments in terms of efficacy in any of the RCTs.
The cervical spine has two natural spaces in structure, namely, the cervical foramen and the cervical intervertebral space. Therefore, cervical injection treatment involves an epidural injection through the cervical intervertebral plate and an epidural injection through the cervical intervertebral foramen. The former is commonly used to treat central or paracentral or multisegment disc herniation, while the latter is primarily used for single-segment disc herniation [40–42]. Both have some complication rates, and many studies comparing interlamellar and transforaminal approaches to neck pain have shown a greater risk of neurological complications [19, 43–47], including infarction of the spinal cord, brainstem, brain, or cerebellum [40]. Potential complications of the interlamina approach include needle placement, infection, or the need for additional medication [2].
The most common causes of neck pain are cervical intervertebral herniation, spondylosis, or stenosis; facet joint, vertebral body, meningeal, blood vessel, nerve sheath, or nerve pathology; and postsurgery syndrome [32, 48–51]. Axial neck pain is associated with disc herniation, facet joint degeneration, cervical spondylosis, or ligamentous diseases. Given the relationship between axial neck pain and disc herniation with radiculitis and spinal stenosis, cervical epidural injections are used to manage axial neck pain [38]. Some patients have a long history of neck pain, which is difficult to manage from a clinical standpoint. Conservative treatments for chronic neck pain include oral analgesics or anti-inflammatory drugs or physical therapy, which can eliminate pain symptoms in some patients by up to 80% [9, 52–64]. Nevertheless, a subset of patients requires decompression surgery although this is not always an option because of the high cost and surgical contraindications. Besides surgery, cervical epidural injections are a valid treatment approach [10, 65, 66] that were shown to be effective in many studies [12, 19, 41, 43, 47].
Dexamethasone is a nonparticulate steroid while triamcinolone and betamethasone are particulate steroids [67]. The use of steroids is linked to the risk of spinal cord injury [67–70]. No significant differences in efficacy have been reported between the 2 types of steroid for the treatment of cervical radiculopathy [71]. Steroids can suppress ectopic discharges from inflamed nerves, improve blood flow, and induce the lysis of iatrogenic and inflammatory adhesions and proinflammatory cytokines.
A washout function has also been ascribed to local anesthetics [40, 72]. Thus, it is possible that the reason there were no differences observed between treatment with anesthetic alone or in conjunction with a steroid in the 4 RCTs is that both agents play the same roles in pain relief and functional improvement. In the evaluation of epidural anesthesia plus corticosteroids for the treatment of cervical arm radiculolargia [73], continuous epidural control of chronic cervical-arm pain was better compared with a single injection. Although both injections use corticosteroids. Thus, local anesthetics have an independent or additive effect.
5. Conclusions
This systematic review and single-arm meta-analysis of 4 RCTs showed strong (level I) evidence for the efficacy of fluoroscopic cervical epidural injections of a local anesthetic alone or combined with a steroid in the treatment of neck pain secondary to cervical disc herniation, spondylosis, stenosis, or postsurgery syndrome. Given the risks and adverse effects associated with both types of drug and potential interaction effects, additional studies are needed to determine whether the 2 treatments are equally effective, in which case the use of steroids can be avoided.
Acknowledgments
This work was supported by the Hospital Level General Project of Hubei Provincial Hospital of Traditional Chinese Medicine (Grant no. 2021YJKT-3). Our study was supported by the innovation of Traditional Chinese Medicine research project of Hubei provincial health and family planning commission (ZY2019M044), and the seventh batch of young and middle-aged medical backbone talent training project of Wuhan [2019]87].
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Bang-zhi Li, Wen-hai Tang, Ming-guo Liu, and Sheng-xue Bao have contributed equally to this work.
References
- 1.Manchikanti L., Cash K. A., Pampati V., Wargo B. W., Malla Y. Management of chronic pain of cervical disc herniation and radiculitis with fluoroscopic cervical interlaminar epidural injections. International Journal of Medical Sciences . 2012;9(6):424–434. doi: 10.7150/ijms.4444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galaasen Bakken A., Axén I., Eklund A., O’Neill S. The effect of spinal manipulative therapy on heart rate variability and pain in patients with chronic neck pain: a randomized controlled trial. Trials . 2019;20(1):p. 590. doi: 10.1186/s13063-019-3678-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLean S. M., May S., Klaber-Moffett J., Sharp D. M., Gardiner E. Risk factors for the onset of non-specific neck pain: a systematic review. Journal of Epidemiology and Community Health . 2010;64(7):565–572. doi: 10.1136/jech.2009.090720. [DOI] [PubMed] [Google Scholar]
- 4.Dieleman J. L., Cao J., Chapin A., et al. US health care spending by payer and health condition, 1996-2016. JAMA . 2020;323(9):863–884. doi: 10.1001/jama.2020.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meraya A. M., Raval A. D., Sambamoorthi U. Chronic condition combinations and health care expenditures and out-of-pocket spending burden among adults, medical expenditure panel survey, 2009 and 2011. Preventing Chronic Disease . 2015;12:p. E12. doi: 10.5888/pcd12.140388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray C. J., Abraham J., Ali M. K., et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA . 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gutman G., Rosenzweig D. H., Golan J. D. Surgical treatment of cervical radiculopathy. Spine . 2018;43(6):E365–E372. doi: 10.1097/BRS.0000000000002324. [DOI] [PubMed] [Google Scholar]
- 8.Choi J. W., Lim H. W., Lee J. Y., et al. Effect of cervical interlaminar epidural steroid injection: analysis according to the neck pain patterns and MRI findings. Korean J Pain . 2016;29(2):96–102. doi: 10.3344/kjp.2016.29.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen S. P., Hooten W. M. Advances in the diagnosis and management of neck pain. BMJ . 2017;358:p. j3221. doi: 10.1136/bmj.j3221. [DOI] [PubMed] [Google Scholar]
- 10.Doan L., Patel H., Aronova Y., Gharibo C. Variations in interlaminar epidural steroid injection practice patterns by interventional pain management physicians in the United States. Pain Physician . 2018;21(5):E493–e499. doi: 10.36076/ppj.2018.5.E493. [DOI] [PubMed] [Google Scholar]
- 11.House L. M., Barrette K., Mattie R., McCormick Z. L. Cervical epidural steroid injection: techniques and evidence. Physical Medicine and Rehabilitation Clinics of North America . 2018;29(1):1–17. doi: 10.1016/j.pmr.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Joswig H., Neff A., Ruppert C., Hildebrandt G., Stienen M. N. The value of short-term pain relief in predicting the long-term outcome of 'indirect' cervical epidural steroid injections. Acta Neurochirurgica . 2018;160(5):935–943. doi: 10.1007/s00701-018-3511-2. [DOI] [PubMed] [Google Scholar]
- 13.Kesikburun S., Aras B., Kelle B., Yavuz F., Yaşar E., Taşkaynatan M. A. The effectiveness of cervical transforaminal epidural steroid injection for the treatment of neck pain due to cervical disc herniation: long-term results. Pain Manag . 2018;8(5):321–326. doi: 10.2217/pmt-2018-0002. [DOI] [PubMed] [Google Scholar]
- 14.Kwak S. Y., Chang M. C. Effect of intradiscal pulsed radiofrequency on refractory chronic discogenic neck pain: a case report. Medicine (Baltimore) . 2018;97(16):p. e0509. doi: 10.1097/MD.0000000000010509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mesregah M. K., Feng W., Huang W. H., et al. Clinical effectiveness of interlaminar epidural injections of local anesthetic with or without steroids for managing chronic neck pain: a systematic review and meta-analysis. Pain Physician . 2020;23(4):335–348. [PubMed] [Google Scholar]
- 16.Wei J. J., Chotai S., Sivaganesan A., et al. Effect of pre-injection opioid use on post-injection patient-reported outcomes following epidural steroid injections for radicular pain. The Spine Journal . 2018;18(5):788–796. doi: 10.1016/j.spinee.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 17.Yang X. N., Geng Z. S., Zhang X. L., et al. Single intracutaneous injection of local anesthetics and steroids alleviates acute nonspecific neck pain: a CONSORT-perspective, randomized, controlled clinical trial. Medicine (Baltimore) . 2018;97(28, article e11285) doi: 10.1097/MD.0000000000011285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang W. Y., Lee J. W., Lee E., Kang Y., Ahn J. M., Kang H. S. Systemic effects of fluoroscopically guided epidural steroid injection with dexamethasone. The Korean journal of pain . 2019;32(3):178–186. doi: 10.3344/kjp.2019.32.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi E., Nahm F. S., Lee P. B. Comparison of contrast flow and clinical effectiveness between a modified paramedian interlaminar approach and transforaminal approach in cervical epidural steroid injection. British Journal of Anaesthesia . 2015;115(5):768–774. doi: 10.1093/bja/aev342. [DOI] [PubMed] [Google Scholar]
- 20.Hashemi M., Dadkhah P., Taheri M., Dehghan K., Valizadeh R. Cervical epidural steroid injection: parasagittal versus midline approach in patients with unilateral cervical radicular pain; a randomized clinical trial. Bulletin of emergency and trauma . 2019;7(2):137–143. doi: 10.29252/beat-070208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benditz A., Brunner M., Zeman F., et al. Effectiveness of a multimodal pain management concept for patients with cervical radiculopathy with focus on cervical epidural injections. Scientific Reports . 2017;7(1):p. 7866. doi: 10.1038/s41598-017-08350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhatti A. B., Kim S. Application of the harms technique to treat undiagnosed intractable C1-C2 unilateral neck pain: a case report. Cureus . 2016;8(9, article e793) doi: 10.7759/cureus.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joswig H., Neff A., Ruppert C., Hildebrandt G., Stienen M. N. The value of short-term pain relief in predicting the 1-month outcome of 'indirect' cervical epidural steroid injections. Acta Neurochirurgica . 2017;159(2):291–300. doi: 10.1007/s00701-016-2997-8. [DOI] [PubMed] [Google Scholar]
- 24.Kang H. Y., Kim J. E., Kim Y. J., Park S. W., Kim Y. An unusual delayed onset of systemic toxicity after fluoroscopy-guided cervical epidural steroid injection with levobupivacaine: a case report. Pain Practice . 2019;19(7):762–766. doi: 10.1111/papr.12802. [DOI] [PubMed] [Google Scholar]
- 25.LaFave J., Bramante R. Upper cervical epidural abscess resulting in respiratory compromise after lumbar steroid injection. The Journal of Emergency Medicine . 2019;57(1):66–69. doi: 10.1016/j.jemermed.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Lee D. G., Chang M. C. Effect of interlaminar epidural steroid injection in patients with central cervical spinal stenosis. World Neurosurgery . 2018;109:e150–e154. doi: 10.1016/j.wneu.2017.09.123. [DOI] [PubMed] [Google Scholar]
- 27.McCormick Z. L., Burnham T., Cunningham S., et al. Effect of low-dose lidocaine on objective upper extremity strength and immediate pain relief following cervical interlaminar epidural injections: a double-blinded randomized controlled trial. Regional Anesthesia and Pain Medicine . 2020;45(10):767–773. doi: 10.1136/rapm-2020-101598. [DOI] [PubMed] [Google Scholar]
- 28.Patel K., Chopra P., Upadhyayula S. Stat Pearls. Treasure Island (FL): Stat Pearls Publishing Copyright © 2020 . Stat Pearls Publishing LLC; 2020. Epidural steroid injections. [PubMed] [Google Scholar]
- 29.Conger A., Cushman D. M., Speckman R. A., Burnham T., Teramoto M., McCormick Z. L. The effectiveness of fluoroscopically guided cervical transforaminal epidural steroid injection for the treatment of radicular pain; a systematic review and meta-analysis. Pain medicine (Malden, Mass) . 2020 doi: 10.1093/pm/pnz127. undefined (undefined): undefined. [DOI] [PubMed] [Google Scholar]
- 30.Manchikanti L., Nampiaparampil D. E., Manchikanti K. N., et al. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: a systematic review of randomized controlled trials. Surgical Neurology International . 2015;6(5):194–235. doi: 10.4103/2152-7806.156598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manchikanti L., Malla Y., Cash K. A., Pampati V., Hirsch J. A. Comparison of effectiveness for fluoroscopic cervical interlaminar epidural injections with or without steroid in cervical post-surgery syndrome. The Korean journal of pain . 2018;31(4):277–288. doi: 10.3344/kjp.2018.31.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manchikanti L., Cash K. A., Pampati V., Wargo B. W., Malla Y. A randomized, double-blind, active control trial of fluoroscopic cervical interlaminar epidural injections in chronic pain of cervical disc herniation: results of a 2-year follow-up. Pain Physician . 2013;16(5):465–478. [PubMed] [Google Scholar]
- 33.Manchikanti L., Cash K. A., Pampati V., Wargo B. W., Malla Y. Cervical epidural injections in chronic-discogenic neck pain without disc herniation or radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician . 2010;13(4):E265–E278. doi: 10.36076/ppj.2010/13/E265. [DOI] [PubMed] [Google Scholar]
- 34.Manchikanti L., Cash K. A., Pampati V., Malla Y. Two-year follow-up results of fluoroscopic cervical epidural injections in chronic axial or discogenic neck pain: a randomized, double-blind, controlled trial. International Journal of Medical Sciences . 2014;11(4):309–320. doi: 10.7150/ijms.8069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.is an Interventional, Malla, Manchikanti L. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical postsurgery syndrome: preliminary results of a randomized, double-blind, active control trial. Pain Physician . 2012;15(1):13–25. doi: 10.36076/ppj.2012/15/13. [DOI] [PubMed] [Google Scholar]
- 36.Manchikanti L., Malla Y., Cash K. A., McManus C. D., Pampati V. Fluoroscopic epidural injections in cervical spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician . 2012;15(1):E59–E70. doi: 10.36076/ppj.2012/15/E59. [DOI] [PubMed] [Google Scholar]
- 37.Furlan A. D., Malmivaara A., Chou R., et al. 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976) . 2015;40(21):1660–1673. doi: 10.1097/BRS.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 38.Manchikanti L., Hirsch J. A., Cohen S. P., et al. Assessment of methodologic quality of randomized trials of interventional techniques: development of an interventional pain management specific instrument. Pain Physician . 2014;17(3):E263–E290. doi: 10.36076/ppj.2014/17/E263. [DOI] [PubMed] [Google Scholar]
- 39.Manchikanti L., Falco F. J., Benyamin R. M., Kaye A. D., Boswell M. V., Hirsch J. A. A modified approach to grading of evidence. Pain Physician . 2014;17(5):E319–E325. doi: 10.36076/ppj.2014/17/E319. [DOI] [PubMed] [Google Scholar]
- 40.Costandi S. J., Azer G., Eshraghi Y., et al. Cervical transforaminal epidural steroid injections. Regional Anesthesia and Pain Medicine . 2015;40(6):674–680. doi: 10.1097/AAP.0000000000000323. [DOI] [PubMed] [Google Scholar]
- 41.Nishio I. Cervical transforaminal epidural steroid injections. Regional Anesthesia and Pain Medicine . 2014;39(6):546–549. doi: 10.1097/AAP.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 42.Bise S., Pesquer L., Feldis M., et al. Comparison of three CT-guided epidural steroid injection approaches in 104 patients with cervical radicular pain: transforaminal anterolateral, posterolateral, and transfacet indirect. Skeletal Radiology . 2018;47(12):1625–1633. doi: 10.1007/s00256-018-3027-0. [DOI] [PubMed] [Google Scholar]
- 43.Lee J. H., Lee S. H. Comparison of clinical efficacy between interlaminar and transforaminal epidural injection in patients with axial pain due to cervical disc herniation. Medicine (Baltimore) . 2016;95(4):p. e2568. doi: 10.1097/MD.0000000000002568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Furman M. B., Giovanniello M. T., O'Brien E. M. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976) . 2003;28(1):21–25. doi: 10.1097/00007632-200301010-00007. [DOI] [PubMed] [Google Scholar]
- 45.Benny B., Azari P., Briones D. Complications of cervical transforaminal epidural steroid injections. American Journal of Physical Medicine & Rehabilitation . 2010;89(7):601–607. doi: 10.1097/PHM.0b013e3181e2d07c. [DOI] [PubMed] [Google Scholar]
- 46.Hoang J. K., Massoglia D. P., Apostol M. A., Lascola C. D., Eastwood J. D., Kranz P. G. CT-guided cervical transforaminal steroid injections: where should the needle tip be located? AJNR. American Journal of Neuroradiology . 2013;34(3):688–692. doi: 10.3174/ajnr.A3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen B., Rispoli L., Stitik T. P., Foye P. M., Georgy J. S. Optimal needle entry angle for cervical transforaminal epidural injections. Pain Physician . 2014;17(2):139–144. doi: 10.36076/ppj.2014/17/139. [DOI] [PubMed] [Google Scholar]
- 48.Skillgate E., Pico-Espinosa O. J., Côté P., et al. Effectiveness of deep tissue massage therapy, and supervised strengthening and stretching exercises for subacute or persistent disabling neck pain. The Stockholm Neck (STONE) randomized controlled trial. Musculoskeletal Science & Practice . 2020;45, article 102070 doi: 10.1016/j.msksp.2019.102070. [DOI] [PubMed] [Google Scholar]
- 49.Weber K. A., Wager T. D., Mackey S., Elliott J. M., Liu W. C., Sparks C. L. Evidence for decreased neurologic pain signature activation following thoracic spinal manipulation in healthy volunteers and participants with neck pain. Neuro Image Clinical . 2019;24(undefined, article 102042) doi: 10.1016/j.nicl.2019.102042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen J., Wang Z., Tu Y., et al. Regional homogeneity and multivariate pattern analysis of cervical spondylosis neck pain and the modulation effect of treatment. Frontiers in Neuroscience . 2018;12:p. 900. doi: 10.3389/fnins.2018.00900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Krøll L. S., Hammarlund C. S., Linde M., Gard G., Jensen R. H. The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial. Cephalalgia: an international journal of headache . 2018;38(12):1805–1816. doi: 10.1177/0333102417752119. [DOI] [PubMed] [Google Scholar]
- 52.Vertebral augmentation involving vertebroplasty or kyphoplasty for cancer-related vertebral compression fractures: a systematic review. Ont Health Technol Assess Ser . 2016;16(11):1–202. [PMC free article] [PubMed] [Google Scholar]
- 53.Chou R., Côté P., Randhawa K., et al. The global spine care initiative: applying evidence-based guidelines on the non-invasive management of back and neck pain to low- and middle-income communities. European Spine Journal . 2018;27(Suppl 6):851–860. doi: 10.1007/s00586-017-5433-8. [DOI] [PubMed] [Google Scholar]
- 54.Corey D. L., Comeau D. Cervical radiculopathy. The Medical Clinics of North America . 2014;98(4):791–799. doi: 10.1016/j.mcna.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 55.Côté P., Yu H., Shearer H. M., et al. Non-pharmacological management of persistent headaches associated with neck pain: a clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. European Journal of Pain . 2019;23(6):1051–1070. doi: 10.1002/ejp.1374. [DOI] [PubMed] [Google Scholar]
- 56.Dissing K. B., Hartvigsen J., Wedderkopp N., Hestbæk L. Conservative care with or without manipulative therapy in the management of back and neck pain in Danish children aged 9-15. Study protocol for a randomized controlled trial. Chiropr Man Therap . 2016;24(1):p. 5. doi: 10.1186/s12998-016-0086-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dissing K. B., Hartvigsen J., Wedderkopp N., Hestbæk L. Conservative care with or without manipulative therapy in the management of back and/or neck pain in Danish children aged 9-15: a randomised controlled trial nested in a school-based cohort. BMJ Open . 2018;8(9, article e021358) doi: 10.1136/bmjopen-2017-021358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Du J. J., Chen Y. F., Peng Y., Li X. J., Ma W. Calcification of the intervertebral disc and ossification of posterior longitudinal ligament in children. BMC Musculoskeletal Disorders . 2018;19(1):p. 316. doi: 10.1186/s12891-018-2227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kelly J., Ritchie C., Sterling M. Clinical prediction rules for prognosis and treatment prescription in neck pain: a systematic review. Musculoskeletal Science & Practice . 2017;27:155–164. doi: 10.1016/j.math.2016.10.066. [DOI] [PubMed] [Google Scholar]
- 60.Kim J. I., Kim Y. I., Kim E., et al. Effectiveness and safety of polydioxanone thread embedding acupuncture compared to physical therapy in the treatment of patients with non-specific chronic neck pain: study protocol for an assessor-blinded, randomized, controlled, clinical trial. Medicine (Baltimore) . 2019;98(32, article e16768) doi: 10.1097/MD.0000000000016768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Manchikanti L., Nampiaparampil D. E., Candido K. D., et al. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician . 2015;18(1):39–60. doi: 10.36076/ppj/2015.18.39. [DOI] [PubMed] [Google Scholar]
- 62.Martins-de-Sousa P. H., Guimarães Almeida M. Q., da Silva Junior J. M., et al. Program of therapeutic exercises associated with electrotherapy in patients with chronic neck pain: protocol for a randomized controlled trial. Journal of Bodywork and Movement Therapies . 2020;24(1):25–30. doi: 10.1016/j.jbmt.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 63.Nyström B., Svensson E., Larsson S., Schillberg B., Mörk A., Taube A. A small group whiplash-associated-disorders (WAD) patients with central neck pain and movement induced stabbing pain, the painful segment determined by mechanical provocation: fusion surgery was superior to multimodal rehabilitation in a randomized trial. Scandinavian Journal of Pain . 2016;12(1):33–42. doi: 10.1016/j.sjpain.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 64.Pillastrini P., Castellini G., Chiarotto A., et al. Comparative effectiveness of conservative and pharmacological interventions for chronic non-specific neck pain: protocol of a systematic review and network meta-analysis. Medicine (Baltimore) . 2019;98(33, article e16762) doi: 10.1097/MD.0000000000016762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gungor S., Aiyer R., Erkan D. Cervical epidural injection in the management of refractory pain and stiffness in spondyloarthropathy: a case report series. Pain practice: the official journal of World Institute of Pain . 2018;18(4):532–538. doi: 10.1111/papr.12616. [DOI] [PubMed] [Google Scholar]
- 66.Park J. Y., Karm M. H., Kim D. H., Lee J. Y., Yun H. J., Suh J. H. Optimal angle of contralateral oblique view in cervical interlaminar epidural injection depending on the needle tip position. Pain Physician . 2017;20(1):E169–E175. doi: 10.36076/2017.1.E169. [DOI] [PubMed] [Google Scholar]
- 67.Gazelka H. M., Burgher A. H., Huntoon M. A., Mantilla C. B., Hoelzer B. C. Determination of the particulate size and aggregation of clonidine and corticosteroids for epidural steroid injection. Pain Physician . 2012;15(1):87–93. doi: 10.36076/ppj.2012/15/87. [DOI] [PubMed] [Google Scholar]
- 68.Grosu I., Lavand'homme P. Continuous regional anesthesia and inflammation: a new target. Minerva Anestesiologica . 2015;81(9):1001–1009. [PubMed] [Google Scholar]
- 69.Crespo S., Dangelser G., Haller G. Intrathecal clonidine as an adjuvant for neuraxial anaesthesia during caesarean delivery: a systematic review and meta-analysis of randomised trials. International Journal of Obstetric Anesthesia . 2017;32:64–76. doi: 10.1016/j.ijoa.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 70.Schäfer M., Mousa S. A., Shaqura M., Tafelski S. Background and current use of adjuvants for regional anesthesia: from research to evidence-based patient treatment. Anaesthesist . 2019;68(1):3–14. doi: 10.1007/s00101-018-0522-6. [DOI] [PubMed] [Google Scholar]
- 71.Dreyfuss P., Baker R., Bogduk N. Comparative effectiveness of cervical transforaminal injections with particulate and nonparticulate corticosteroid preparations for cervical radicular pain. Pain Medicine . 2006;7(3):237–242. doi: 10.1111/j.1526-4637.2006.00162.x. [DOI] [PubMed] [Google Scholar]
- 72.Friedly J. L., Comstock B. A., Turner J. A., et al. A randomized trial of epidural glucocorticoid injections for spinal stenosis. The New England Journal of Medicine . 2014;371(1):11–21. doi: 10.1056/NEJMoa1313265. [DOI] [PubMed] [Google Scholar]
- 73.Pasqualucci A., Varrassi G., Braschi A., et al. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: single injection versus continuous infusion. The Clinical Journal of Pain . 2007;23(7):551–557. doi: 10.1097/AJP.0b013e318074c95c. [DOI] [PubMed] [Google Scholar]


