Abstract
Background
Published guidance concerning emergency management of left ventricular assist device (LVAD) recipients is both limited and lacking in consensus which increases the risk of delayed and/or inappropriate actions.
Methods
In our specialist tertiary referral centre we developed, by iteration, a novel in-hospital resuscitation algorithm for LVAD emergencies which we validated through simulation and assessment of our multi-disciplinary team. A Mechanical Life Support course was established to provide theoretical and practical education combined with simulation to consolidate knowledge and confidence in algorithm use. We assessed these measures using confidence scoring, a key performance indicator (the time taken to restart LVAD function) and a multiple-choice question (MCQ) examination.
Results
The mean baseline staff confidence score in management of LVAD emergencies was 2.4 ± 1.2 out of a maximum of 5 (n = 29). After training with simulation, mean confidence score increased to 3.5 ± 0.8 (n = 13).
Clinical personnel who were provided with the novel resuscitation algorithm were able to reduce time taken to restart LVAD function from a mean value of 49 ± 8.2 seconds (pre-training) to 20.4 ± 5 seconds (post-training) (n = 42, p < 0.0001).
The Mechanical Life Support course increased mean confidence from 2.5 ± 1.2 to 4 ± 0.6 (n = 44, p < 0.0001) and mean MCQ score from 18.7 ± 3.4 to 22.8 ± 2.6, out of a maximum of 28 (n = 44, p < 0.0001).
Conclusion
We present a simplified LVAD Advanced Life Support algorithm to aid the crucial first minutes of resuscitation where basic interventions are likely to be critical in assuring good patient outcomes.
Keywords: LVAD, Left ventricular assist device, Resuscitation, Advanced life support, Mechanical circulatory support, Cardiac arrest
Abbreviations: LVAD, Left Ventricular Assist Device; MDT, multi-disciplinary team; MLS, Mechanical Life Support; MCQ, multiple-choice exam; CPR, Cardio-Pulmonary Resuscitation; ALS, Advanced Life Support; ECMO, Extracorporeal Membrane Oxygenation; MAP, Mean Arterial Pressure; VT, Ventricular Tachycardia; VF, Ventricular Fibrillation; ETCO2, End Tidal Carbon Dioxide, kPa Kilopascal; CALS, Cardiac Advanced Life Support; DNAR, do not attempt resuscitation order
Introduction
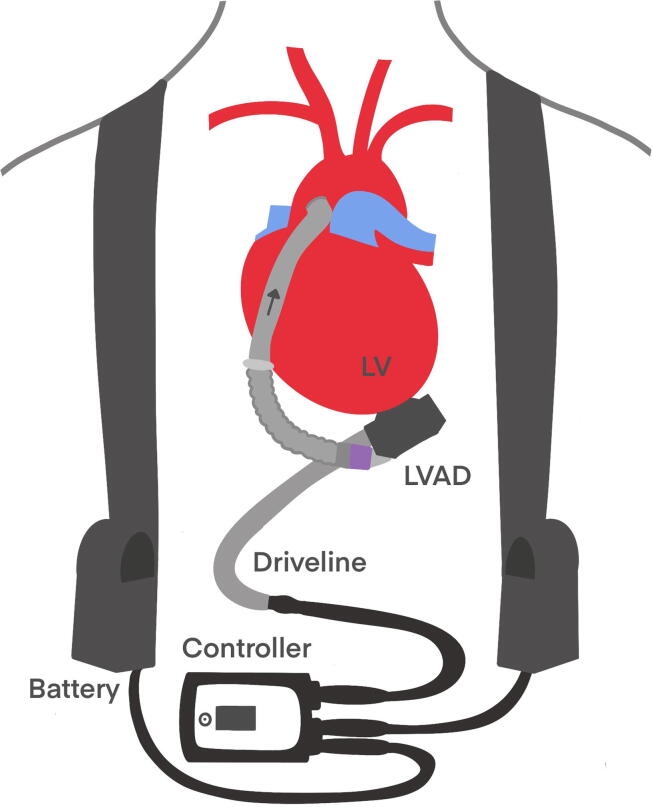
In the United Kingdom (UK), left ventricular assist device therapy (Fig. 1) in adults is centrally commissioned at the six cardiothoracic transplantation centres by the National Health Service as a bridge to heart transplantation or until recovery of native ventricular function1. There were 314 adults in the UK undergoing LVAD therapy in August 2020 (unpublished audit data) and despite being a relatively small patient cohort they experience a high burden of complications which frequently require rehospitalisation2., 3.. Contemporary devices are associated with lower complication rates than earlier designs yet up to 70% of patients will suffer either device failure, stroke, haemorrhage, infection or VAD thrombosis within the first year of implantation4.
Fig. 1.
Schematic of left ventricular assist device design, LV: Left ventricle, LVAD: Left ventricular assist device.
Due to the particular characteristics of LVAD therapy, many new or rotational staff in specialist centres are unfamiliar with managing emergency situations involving these devices. Algorithms offer a clinically effective method which ensures a standardised, rapid, and structured approach to resuscitation5. Published guidance concerning emergency management of LVAD recipients in the hospital setting is both limited and deviates from standard advanced life support strategy which increases the risk of delayed and/or inappropriate decision making and actions that can ultimately lead to poor outcomes6., 7., 8., 9., 10..
LVAD recipients often have no palpable pulse and a dominant feature on auscultation is a LVAD-generated ‘hum’. Non-invasive blood pressure and oxygen saturation monitoring are frequently difficult to obtain9 which challenges clinical staff, who would usually rely on the absence of a pulse to confirm cardiac arrest. The blood flow profile generated by the LVAD is dependent on impeller rotation rate, preload, native heart contractility and systemic vascular compliance and resistance, which complicates physical assessment particularly under conditions of haemodynamic compromise where native ventricular function may be diminished. The decision to implement chest compressions in LVAD recipients remains controversial and may delay the implementation of more effective resuscitative manoeuvres in the LVAD patient with cardiovascular collapse.
Our group previously developed algorithms for ambulance clinicians to improve the safety of patients undergoing LVAD therapy requiring emergency treatment in the community2. These guidelines, endorsed by the Resuscitation Council UK and the Joint Royal Colleges Ambulance Liaison Committee, have been adopted nationally. The aim of this initiative is to extend these guidelines to the in-hospital setting to allow an appropriate response for deteriorating inpatients with implantable LVADs.
Methods
This initiative was conducted between January and October 2021 at Harefield Hospital, London, a specialist tertiary referral centre offering management of advanced heart failure including transplantation and left ventricular assist device therapy for a zonal area comprising 78 hospitals11. Most of the LVAD recipients in our centre, for whom the novel resuscitation guidance is intended to provide benefit, have either received a Medtronic Inc. (formerly Heartware Inc.) HVAD or an Abbott Inc. Heartmate 3.
Initially, we carried out a one day, in-house spot audit of our healthcare professionals working in both inpatient and outpatient settings to establish whether they felt confident in the management of LVAD emergencies. Responses were graded according to a Likert scale (1: not confident at all to 5: very confident).
Ward based simulation
Participants, simulator, environment
We instituted a series of ward-based simulation scenarios for staff using the out of hospital algorithm published previously2. Participants were staff rostered to work on the transplant ward. The simulation was conducted by three facilitators whose roles were to lead, to operate the LVAD, introduce alarms and to control the vital signs. We utilised a Laerdal Resusci Anne full body model with Sim Pad and a real in-hospital resuscitation trolley with standard airway, breathing and circulatory (including defibrillator) emergency equipment. We have also developed a bespoke LVAD simulator consisting of a LVAD and sealed bottle which allows the recirculation of water. This allows the LVAD to operate and by clamping the interconnecting tubing, low LVAD blood flow can be simulated. The LVAD in this model is connected to a standard controller and rechargeable batteries and is located adjacent to the mannequin during the simulation. Staff were briefed prior to initiation of the simulation with a particular emphasis on defibrillation safety.
Design of simulation scenarios
We simulated a wide range of clinical scenarios which included: LVAD driveline disconnection; electrical power failure; low LVAD flow alarms; arrhythmias; bleeding; sepsis and intracranial haemorrhage. We allocated three members to each scenario with identification of a team leader, and first and second responders. The team leader was encouraged to stand at the end of the bed, hold the algorithm in their hand and to give sequential instructions to their colleagues. The responders would communicate findings, such as controller alarms, back to the team leader who would then instruct them on the next step. We would typically run two scenarios of 5–10 minutes duration followed by 5 minutes reflection and feedback.
Feedback
After the simulation was completed, we asked participants and observers to comment on favourable responses and areas where they felt there was scope for improvement. We also discussed the physiology and medical management of different clinical situations. On leaving the room we asked participants to complete an anonymous online survey which included an assessment of their confidence in dealing with each scenario (using the method described above).
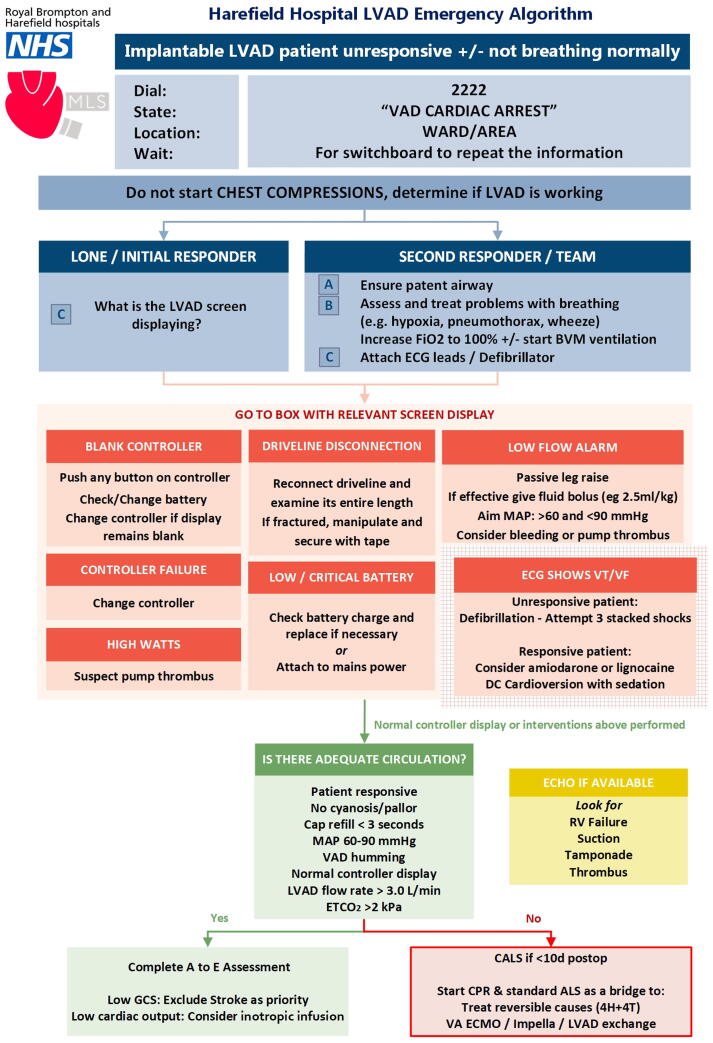
In-hospital algorithm design
Through simulation we identified aspects of the out of hospital algorithm that could be improved and refined. We established a working group consisting of key medical and nursing stakeholders in cardiology, transplant surgery, intensive care, and resuscitation to develop a bespoke resuscitation algorithm for in-hospital use. Through a process of simulation and testing, the algorithm was iterated until it was deemed to be safe and clinically efficacious (Fig. 2, Appendix 1 for explanation of algorithm steps). We also identified a Key Performance Indicator: the time taken for a member of staff to recognise and resolve a LVAD driveline disconnection event. The initial focus of the algorithm is the prompt diagnosis of LVAD dysfunction, and the implementation of remedial actions according to the alarm message displayed on the LVAD controller. The algorithm was presented to all hospital staff through our clinical governance programme and was approved for use in July 2021. We have placed laminated copies of the algorithm on all cardiac arrest trollies within the hospital and on the walls in the bedspaces of admitted LVAD patients.
Fig. 2.
Left ventricular assist device in hospital resuscitation algorithm, LVAD Left Ventricular Assist Device, FiO2 Fraction of Inspired Oxygen, BVM Bag Valve Mask, ECG Electrocardiography, MAP Mean Arterial Pressure, DC Direct Current, ETCO2 End tidal Carbon Dioxide, A to E Airway to Exposure, GCS Glasgow Coma Scale, CALS Cardiac Advanced Life Support, CPR Cardio-Pulmonary Resuscitation, ALS Advanced Life Support, 4H & 4 T Hypoxia/Hypokalaemia/Hyperkalaemia/Hypothyermia/Hyperthermia/Hypovolaemia & Tension Pneumothorax/Tamponade/Thrombosis/Toxins, VA ECMO Veno-Arterial Extracorporeal Membrane Oxygenation.
Mechanical life support © course
The in-hospital algorithm facilitates troubleshooting by initial responders and is based on complications likely to be encountered in the clinical setting. The proposed algorithm assumes a basic level of understanding of LVADs, including familiarity with electrical connections and normal operating parameters. By means of a half-day course and assuming minimal prior LVAD patient management experience, we sought to teach and consolidate a foundational understanding of LVAD therapy.
Candidates, structure, simulator, environment
The course was advertised to all hospital staff and 10 participants from nursing, medical and allied healthcare professional backgrounds attended each course. The range of experience ranges from daily exposure to no previous experience with LVADs. The venue was the hospital simulation suite, and we utilised the same equipment to that described in the ward simulation. Prior to the course, the novel algorithm and the publication on resuscitation in LVAD recipients2 was distributed to the candidates.
Lectures provided introductory teaching on advanced heart failure, temporary and long-term mechanical support, and transplantation. Subsequently, candidates spent an hour practising disconnecting and reconnecting the external LVAD equipment, and safely performing battery and controller exchanges under the supervision of specialist LVAD nurses. Candidates then participated in a wide range of clinical simulations as described in the ward simulation to train in emergency algorithm use. Finally, targeted training sessions were conducted in which candidates learned how to perform a brachial arterial Doppler measurement of arterial blood pressure, advanced LVAD parameter interpretation, ETCO2 measurement, echocardiography image interpretation and right ventricular management.
Feedback and assessment
Pre and post course MCQs and ongoing observational assessments were conducted to determine if a candidate had gained sufficient experience. Additional teaching was provided to those candidates who needed further support outside of the course on a 1:1 basis. We assessed the effectiveness of the course according to the change in confidence score (as previously described) and a multiple-choice question examination based on potential clinical emergencies (Appendix 2).
Statistical analysis
Numerical variables are presented as mean ± standard deviation and comparisons between groups were performed using the paired t test or the Wilcoxon signed rank test. The estimate of the difference between the pre and post means was calculated by direct subtraction while for the Signed Rank Test the difference between pre and post values was estimated with the Hodges-Lehman estimator. All tests were 2 sided and a p value < 0.05 was considered significant. The analysis was performed using the statistical software Stata version 17 StataCorp LLC, Texas.
Results
The mean baseline staff confidence score for doctors, nurses and allied healthcare professionals in our transplant department in the management of LVAD emergencies was 2.4 ± 1.2 out of a maximum of 5 (n = 29).
Ward based simulation using the out of hospital algorithm took place over eight separate sessions and involved 47 participants from representative clinical backgrounds. The mean post-training confidence score of those who completed the feedback increased to 3.5 ± 0.8 (n = 13).
With introduction of the novel in hospital algorithm we reduced the time taken to restart the LVAD from a mean value of 49 ± 8.2 seconds (pre-training) to 20.4 ± 5 seconds (post-training) (n = 42, p < 0.0001).
Following implementation of the Mechanical Life Support course and the novel resuscitation algorithm in a 44-candidate course cohort, mean confidence score increased from 2.5 ± 1.2 to 4 ± 0.6 (p < 0.0001) and theoretical knowledge, as assessed by mean MCQ score, increased from 18.7 ± 3.4 to 22.8 ± 2.6, out of a maximum of 28 (p < 0.0001).
Discussion
A deteriorating LVAD patient can be a challenging situation for clinical staff and frequently the first responders have limited clinical experience. We identified a low baseline level of confidence in our staff in the management of LVAD emergencies. In response to this clinical risk we devised a programme of simulation, algorithm design and didactic teaching aligned as closely as possible with modern resuscitation protocols.
We adapted previous algorithms2 for in hospital use over several iterations through simulation and MDT review. There was strong consensus that troubleshooting and restarting the LVAD function remains pivotal in achieving a positive outcome. Thus, the focus of our algorithm was the prompt reversal of the causes of LVAD dysfunction. We also provided guidance for the assessment of adequate circulation and when to initiate CPR as this remains a common concern of frontline staff. This initiative culminated in the development of the Mechanical Life Support course and led to significant improvements in confidence and theoretical knowledge as assessed by MCQ examination. We also demonstrated a significant improvement in a novel key performance indicator; the time taken for a member of staff to recognise and resolve an LVAD driveline disconnection event.
The most intensely debated aspect of our algorithm related to the safety, timing and efficacy of CPR in LVAD recipients. CPR is associated with a perceived risk of anastomotic rupture but the limited evidence available suggests this risk may have been overestimated, particularly if the LVAD implant duration is prolonged. Retrograde flow through the non-occlusive (valve-less) dysfunctional LVAD blood path is likely to reduce the effectiveness of chest compressions. Yet if there is no intrinsic cardiac or LVAD function, then pragmatically, the implementation of CPR could not worsen the clinical situation. Our group has previously advocated only using CPR as a) a temporising measure until the LVAD can be restarted or b) as a last resort which concurs with the consensus statement from the American Heart Association that places emphasis on restarting LVAD function2., 9.. If there is failure to re-establish LVAD function, it is reasonable to initiate CPR as a bridge to temporary mechanical support or medical intervention such as thrombolysis.
Limitations of this initiative include a single centre study design and inadequate evidence to provide prescriptive guidance in advanced life support in LVAD recipients. While the evidence base remains limited, we believe that experience guided by clinical practice and repeated simulation provides the best interim approach.
Conclusion
Left ventricular assist devices have both idiosyncratic features and a complex effect on human physiology. Initial responders to LVAD emergencies are often the least experienced members of the multi-disciplinary team in LVAD management. We present a simplified VAD Advanced Life Support algorithm to aid the crucial first minutes of resuscitation where basic interventions are likely to be critical in assuring good patient outcomes.
Funding Sources
Nil.
Conflicts of Interest
None
Ethical statement
Ethics approval was not required for the algorithm design and educational course.
CRediT authorship contribution statement
Waqas Akhtar: Methodology, Formal analysis, Investigation, Writing – original draft, Supervision. Brigitte Gamble: Methodology, Formal analysis, Investigation, Writing – original draft, Supervision. Kristine Kiff: Methodology, Validation, Resources. Agnieszka Wypych-Zych: Methodology, Validation, Resources. Binu Raj: Methodology. Junko Takata: Methodology, Validation, Resources. Fernando Riesgo Gil: Methodology, Validation, Resources. Ana Hurtado: Methodology, Validation, Resources. Alex Rosenberg: Methodology, Validation, Resources. Christopher T. Bowles: Methodology, Validation, Supervision.
Acknowledgements
We would like to thank all the medical, nursing and allied healthcare professionals who contributed to the development of this algorithm. We are grateful to Winston Banya, Medical Statistician, for assisting with the statistical analyses.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100254.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Parameshwar J., Hogg R., Rushton S., et al. Patient survival and therapeutic outcome in the UK bridge to transplant left ventricular assist device population. Heart. 2019;105:291–296. doi: 10.1136/heartjnl-2018-313355. [DOI] [PubMed] [Google Scholar]
- 2.Bowles C.T., Hards R., Wrightson N., et al. Algorithms to guide ambulance clinicians in the management of emergencies in patients with implanted rotary left ventricular assist devices. Emergency Med J : EMJ. 2017;34:842–850. doi: 10.1136/emermed-2016-206172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bottle A., Faitna P., Aylin P.P., Cowie M.R. Five-year outcomes following left ventricular assist device implantation in England. Open Heart. 2021;8:e001658. doi: 10.1136/openhrt-2021-001658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirklin J.K.N.D., Kormos R.L., Stevenson L.W., Pagani F.D., Miller M.A., Baldwin J.T., Young J.B. Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J Heart Lung Transplant. 2013;32:141–156. doi: 10.1016/j.healun.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Kleber C., Giesecke M.T., Lindner T., Haas N.P., Buschmann C.T. Requirement for a structured algorithm in cardiac arrest following major trauma: Epidemiology, management errors, and preventability of traumatic deaths in Berlin. Resuscitation. 2013;85:405–410. doi: 10.1016/j.resuscitation.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Vierecke J., Schweiger M., Feldman D., et al. Emergency procedures for patients with a continuous flow left ventricular assist device. Emergency Med J. 2017;34:831–841. doi: 10.1136/emermed-2015-204912. [DOI] [PubMed] [Google Scholar]
- 7.Scandroglio A.M.M.D., Kaufmann F.D.I.N.G., Pieri M.M.D., et al. Diagnosis and Treatment Algorithm for Blood Flow Obstructions in Patients With Left Ventricular Assist Device. J Am Coll Cardiol. 2016;67:2758–2768. doi: 10.1016/j.jacc.2016.03.573. [DOI] [PubMed] [Google Scholar]
- 8.Guglin M. Approach to Unresponsive Patient with LVAD. VAD J. 2018;4 [Google Scholar]
- 9.Peberdy M.A., Gluck J.A., Ornato J.P., et al. Cardiopulmonary Resuscitation in Adults and Children With Mechanical Circulatory Support: A Scientific Statement From the American Heart Association. Circulation. 2017;135:1115–1134. doi: 10.1161/CIR.0000000000000504. [DOI] [PubMed] [Google Scholar]
- 10.Yuzefpolskaya M, Uriel N, Takayama H, et al. Proposal for Advanced Life Support Algorithm in Unresponsive Hospitalized LVAD Patients. The Journal of heart and lung transplantation 2013;32(4).
- 11.Transplant NBa. DATASHEET DAT2981/3. In: NHSBT, ed. Bristol, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.