Abstract
Unheated and heat-treated homogenates were separately prepared from candidate probiotic bacteria, including Lactobacillus rhamnosus GG, Bifidobacterium lactis, Lactobacillus acidophilus, Lactobacillus delbrueckii subsp. bulgaricus, and Streptococcus thermophilus. We compared the phytohemagglutinin-induced proliferation of mononuclear cells in the presence of homogenates and in the presence of a control containing no homogenate by assessing thymidine incorporation in cell cultures. All homogenates suppressed proliferation, whether the enzymatic activity was inactivated or not inactivated by heating. When the proliferation assays were repeated with cytoplasmic and cell wall extracts derived from the homogenate of L. rhamnosus GG, the cytoplasmic extract but not the cell wall extract was suppressive. These findings indicate that candidate probiotic bacteria possess a heat-stable antiproliferative component(s). These bacteria may be used to generate microbiologically nonviable yet immunologically active probiotic food products that are easier to store and have a longer shelf life.
In the generation of novel functional foods with probiotics, an understanding of the mechanisms of probiotic action is crucial. Probiotics are defined as live microbial food ingredients which are beneficial to the health of their hosts (24). The most frequently used probiotic bacteria are lactic acid bacteria and bifidobacteria. Data on probiotic bacteria imply that they have both up- and downregulatory effects on immune responses. It has been shown that in vitro live probiotic bacteria potentiate nonspecific immunity by stimulating cytokine production (16, 18), which is beneficial in eradication of pathogens. Orally administered live probiotic bacteria have been shown to suppress intestinal inflammation in vivo (15) and thus are useful in controlling hypersensitivity reactions.
Suppression of inflammatory reactions to ubiquitous antigens is essential for the maintenance of physiological immune homeostasis (30). As the antigens are processed and induce specific systemic hyporesponsiveness, reexposure to them does not elicit hypersensitivity reactions (21, 30). Performing proliferation assays of lymphoid blood cells is a means of studying hypersensitivity to the antigens in question. The use of a mitogen as an antigen allows workers to study the modulation of nonspecific immune responses (14).
In a number of studies workers have described the immunomodulatory effects of nonviable forms of probiotic bacteria (5, 16, 18, 26, 27, 29). However, no study has dealt with differences between homogenates derived from candidate probiotic bacteria in relation to regulation of immune responses. The objective of the present study was to characterize the immunomodulatory effects of homogenates, with or without inactivation of their enzymes, obtained from Lactobacillus rhamnosus GG, Bifidobacterium lactis, Lactobacillus acidophilus, Lactobacillus delbrueckii subsp. bulgaricus, and Streptococcus thermophilus by using a mitogen-induced proliferation test in vitro. In addition, we performed a series of experiments to locate the immunomodulatory component(s) by fractionating the homogenates into cytoplasmic and cell wall extracts.
MATERIALS AND METHODS
Microorganisms.
L. rhamnosus GG ATCC 53103, L. acidophilus NCFB 1748, and L. delbrueckii subsp. bulgaricus ATCC 11842 were grown anaerobically in MRS broth (Lab M, Bury, United Kingdom) at 37°C for 13 h. B. lactis BB12 (Chr. Hansen, Horsholm, Denmark) was cultured anaerobically at 37°C for 22 h in MRS broth (Lab M), and S. thermophilus DSM 4022 was cultured anaerobically at 37°C for 13 h in whey permeate broth containing 5% whey permeate (Valio Ltd., Research and Development Centre, Helsinki, Finland), 2% casein hydrolysate (Valio Ltd.), and 1% yeast extract (Lab M). All strains were kindly provided by T. Suomalainen (Valio Ltd.). The organisms were harvested by centrifugation and washed three times with 0.1 M phosphate buffer (pH 6.9).
Preparation of bacterial homogenates.
Bacterial homogenates were isolated as previously described, with minor modifications (8). Briefly, the contents of bacterial cells were released by sonication with an Ultrasonic 1000 sonicator (B. Braun Biotech International Gmbh, Melsungen, Germany) on ice at 30-s intervals until the cells were disrupted. The degree of cell breakage was estimated, and the cell numbers were calculated by using light microscopy; the number of ruptured cells was determined by counting the intact cells before and after sonication and subtracting the number before sonication from the number after sonication. Each of the preparations was then suspended in 0.1 M phosphate buffer (pH 6.9) in order to equalize differences in the numbers of ruptured cells for the bacterial strains (108 cells/ml). Finally, the preparations were centrifuged at 1,000 × g for 30 min at 4°C, and each supernatant obtained, which was used as a homogenate, was stored at −70°C until it was used.
Preparation of cytoplasm and cell wall extracts of L. rhamnosus GG.
The L. rhamnosus GG homogenate was recentrifuged at 35,000 × g for 20 min at 4°C in order to obtain cell wall extracts in the pellet fraction and cytoplasm in the supernatant fraction. The cell wall extract was prepared from the pellet by suspension in 0.1 M phosphate buffer (pH 6.9) so that an amount equal to the amount of the supernatant was obtained. The samples were stored at −70°C until they were used.
Measurement of enzyme activity.
The enzyme activities of homogenates and extracts were measured by measuring protease activities as previously described, with minor modifications (1). Briefly, a homogenate was incubated with 0.15 mg of whey protein hydrolysate 80 LH (Valio Ltd.; low-heat-treated protein content, 80%; α-aminonitrogen content of total nitrogen, 30%) in 1 ml of phosphate buffer for 2 h at 37°C. Hydrolysis was stopped by adding 0.75 N trichloroacetic acid (Baker, Deventer, Holland). α-Amino groups released by hydrolysis reacted with o-phthaldialdehyde (FLUKA-Chemie Ag, Buchs, Switzerland) and β-mercaptoethanol (FLUKA-Chemie Ag) to form an adduct which absorbed strongly at 340 nm. Enzymatic activity was calculated by using tyrosine as the standard. This compound was destroyed by heating at 75°C for 15 min. This was confirmed by using a previously described method, with minor modifications (1).
Dilutions.
Two sets of test dilutions were prepared from unheated homogenates. In the first set, homogenates were diluted 1:10, 1:100, and 1:1,000 based on the number of ruptured cells per 1 ml of preparation; in the second, homogenates were diluted 1:10, 1:100, and 1:1,000 based on their enzymatic activities.
One set of dilutions was prepared from heat-treated homogenates. The homogenates were diluted 1:10, 1:100, and 1:1,000 based on the number of ruptured cells per 1 ml of preparation.
One set of dilutions was prepared from unheated and heat-treated cytoplasmic extracts and the corresponding cell wall extracts. The extracts were diluted 1:10, 1:100, and 1:1,000 based on the number of ruptured cells per 1 ml of preparation.
All of the preparations were filtered (Millex-GV; pore size, 0.22 μm; Nihon Millipore Kogyo Inc., Yonezawa, Japan) and added to cell cultures.
Proliferation assay.
A proliferation assay was used to measure mononuclear cell responses to antigens (14). The mitogen used, phytohemagglutinin (PHA; Difco Laboratories, Detroit, Mich.), mimics an antigen and induces T cell activation and replication (14). For the assay, leukocyte-rich buffy coat blood was obtained from 15 healthy donors (Finnish Red Cross Blood Transfusion Service, Turku, Finland). Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll-Paque (Pharmacia Fine Chemicals AB, Uppsala, Sweden) density gradient centrifugation, and cell viability was assessed by trypan blue exclusion. A total of 106 cells were suspended in 1 ml of complete Roswell Park Memorial Institute 1640 culture medium (GIBCO BRL Inc., Life Technologies, Paisley, Scotland) supplemented with 10% fetal calf serum, 10 mM HEPES buffer, 2 mM l-glutamine (GIBCO BRL Inc.), 50 U of benzylpenicillin (Sigma Chemical Co., St. Louis, Mo.), and 10 mg of gentamicin (Roussel Laboratories Ltd., Uxbridge, Middlesex, United Kingdom). Dilutions of the preparations studied were confirmed to be nontoxic to cells by dye exclusion studies performed with eosin. Proliferation was tested by adding the mitogen PHA to a final concentration of 125 μg/ml together with one of the preparations in one of three dilutions. Control cell cultures contained only PHA. Triplicate cell cultures were incubated in 96-well flat-bottom plates (Nunc, Roskilde, Denmark) for 96 h at 37°C in a humidified 5% CO2 atmosphere. [3H]thymidine (0.5 μCi/well; specific activity, 2.0 Ci/mmol/ml; Radiochemical Centre, Amersham, United Kingdom) was added 18 h before harvesting with an automatic harvester (Harvester 96, Mach III M, TOMTEC; Wallac Ltd., Turku, Finland). [3H]thymidine incorporation was estimated by using a liquid scintillation counter (model 1450 Microbeta PLUS; Wallac Ltd.), and data were expressed as counts per minute with the background value excluded.
Statistical analyses.
Data are presented below as medians (interquartile ranges) based on 6 to 15 experiments. Friedman’s nonparametric analysis of variance (3) was used to compare six experiments, five performed with homogenates and one performed with a control cell culture. Wilcoxon’s matched pairs test (2) was used in pairwise comparisons of heat-treated and unheated strains and in comparisons of cellular components and control cell cultures.
RESULTS
Suppression of mitogen-induced proliferation by unheated homogenates.
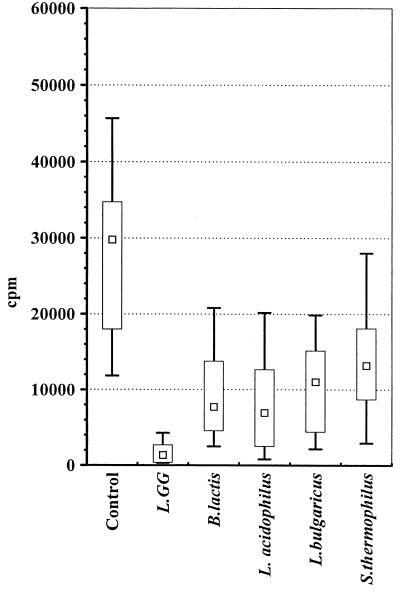
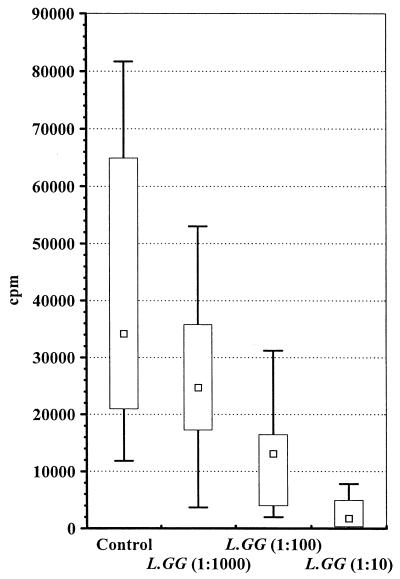
Initially, we compared unheated homogenates from five bacterial strains with the control culture. Figure 1 shows the mitogen-induced proliferation of PBMCs in homogenates at a dilution of 1:10 and in control cultures. There were significant differences among the proliferation results obtained in the six experiments (P < 0.001, as determined by Friedman’s test). The most potent suppression of proliferation was observed with L. rhamnosus GG homogenate. As shown in Fig. 2, dilution of the homogenate gradually reduced the antiproliferative effect.
FIG. 1.
Mitogen-induced proliferative responses of PBMCs to unheated homogenates of L. rhamnosus GG, B. lactis, L. acidophilus, L. delbrueckii subsp. bulgaricus, and S. thermophilus at a dilution of 1:10 and to a control culture. The results are expressed in counts per minute; the boxes indicate the lower and upper quartiles, and each central point is the median. The upper end of each bar is the maximum value, and the lower end is the minimum value (n = 8 for each study group). L. GG, L. rhamnosus GG; L. bulgaricus, L. delbrueckii subsp. bulgaricus.
FIG. 2.
Mitogen-induced proliferative responses of PBMCs to unheated homogenates of L. rhamnosus GG at three dilutions (1:1,000, 1:100, and 1:10) and to a control culture. The results are expressed in counts per minute; the boxes indicate the lower and upper quartiles, and each central point is the median. The upper end of each bar is the maximum value, and the lower end is the minimum value (n = 15 for each study group). L. GG., L. rhamnosus GG.
The effect of enzymatic activity on the proliferation rate was evaluated separately. The enzymatic activities in the preparations studied varied between 12 and 137 nmol · ml−1 · min−1. After dilution, each homogenate contained the same enzymatic activity. Table 1 shows the mitogen-induced proliferation of PBMCs in homogenates diluted 1:10 and in control cultures. The differences among the results of the six experiments were statistically significant (P < 0.001, as determined by Friedman’s test). Potent suppression of proliferation compared with the control was observed with L. rhamnosus GG, B. lactis, L. acidophilus, and L. delbrueckii subsp. bulgaricus but not with S. thermophilus when the preparation was diluted to the same enzymatic activity level as the other bacterial preparations.
TABLE 1.
Effects of unheated homogenates from L. rhamnosus GG, B. lactis, L. delbrueckii subsp. bulgaricus, L. acidophilus, and S. thermophilus on mitogen-induced proliferation of PBMCs when the homogenates were equalized on the basis of their enzymatic activities
| Prepn | No. | Proliferation of PBMCs (cpm)a
|
|
|---|---|---|---|
| Median | Interquartile range | ||
| Mitogen | 6 | 29,771 | 29,161–34,131 |
| Mitogen + L. rhamnosus GG | 6 | 823 | 331–2,288 |
| Mitogen + B. lactis | 6 | 9,749 | 4,724–15,092 |
| Mitogen + L. acidophilus | 6 | 4,954 | 2,713–6,654 |
| Mitogen + L. delbrueckii subsp. bulgaricus | 6 | 9,097 | 3,921–13,808 |
| Mitogen + S. thermophilus | 6 | 28,480 | 11,750–29,161 |
A 1:10 dilution was used in each experiment.
Suppression of mitogen-induced proliferation by heat-treated homogenates.
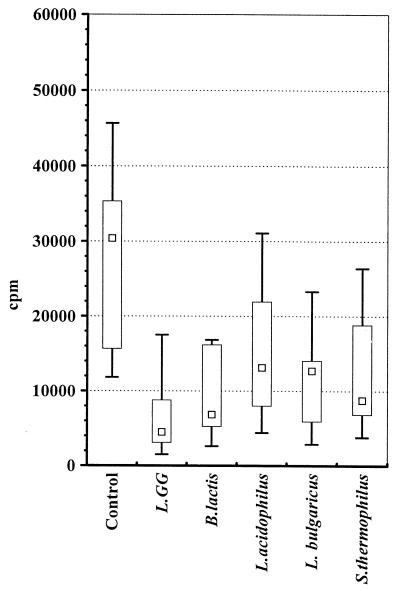
In order to assess the effect of inactivation of enzymes of probiotic bacteria on proliferation, homogenates were heat treated and enzyme inactivation was confirmed. The homogenates were then added to cultures diluted based on the number of ruptured cells per ml of preparation. Figure 3 shows the mitogen-induced proliferation of PBMCs in the homogenates at a 1:10 dilution and in control cultures. Significant differences in proliferation were observed in the six experiments (P < 0.001, as determined by Friedman’s test).
FIG. 3.
Mitogen-induced proliferative responses of PBMCs to heat-treated homogenates of L. rhamnosus GG, B. lactis, L. acidophilus, L. delbrueckii subsp. bulgaricus, and S. thermophilus at a dilution of 1:10 and to a control culture. The results are expressed in counts per minute; the boxes indicate the lower and upper quartiles, and each central point is the median. The upper end of each bar is the maximum value, and the lower end is the minimum value (n = 7 for each study group). L. GG., L. rhamnosus GG; L. bulgaricus, L. delbrueckii subsp. bulgaricus.
Heat treatment of homogenates significantly reduced but did not eliminate the suppressive effects of L. rhamnosus GG and L. acidophilus. In the experiment performed with control culture, the median (interquartile range) mitogen-induced proliferation was 30,381 cpm (15,625 to 35,340 cpm). The levels of proliferation in unheated and heat-treated homogenates of L. rhamnosus GG were 1,755 cpm (602 to 3,670 cpm) and 5,482 cpm (3,138 to 8,609 cpm) (P = 0.017, as determined by Wilcoxon’s matched pairs test), respectively, and the levels of proliferation in L. acidophilus homogenates were 8,074 cpm (2,288 to 15,645 cpm) and 13,108 cpm (7,967 to 21,939 cpm) (P = 0.018, as determined by Wilcoxon’s matched pairs test), respectively.
Effects of L. rhamnosus GG cytoplasmic and cell wall extracts on mitogen-induced proliferation.
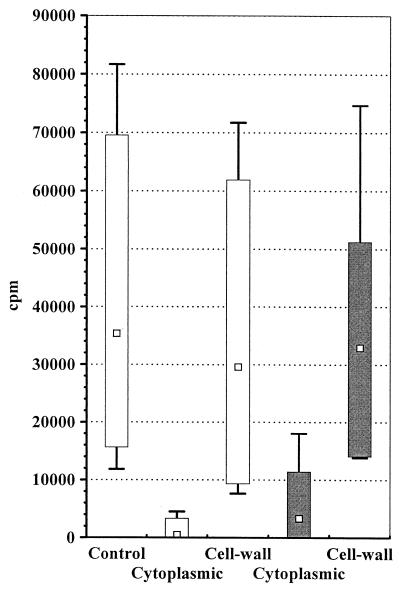
Figure 4 shows the mitogen-induced proliferation of PBMCs in unheated and heat-treated L. rhamnosus GG cytoplasmic and cell wall extracts at a 1:10 dilution and in control cultures. Both unheated and heat-treated cytoplasmic extracts significantly suppressed mitogen-induced proliferation compared with the control (P = 0.018 and P = 0.018, respectively, as determined by Wilcoxon’s matched pairs test). Cell wall extract did not modify proliferation. Heat treatment slightly interfered with the suppressive effect of cytoplasmic extract; the median (interquartile range) mitogen-induced proliferation in heat-treated cytoplasmic extracts and in unheated cytoplasmic extracts were 3,308 cpm (53 to 11,383 cpm) and 473 cpm (91 to 3,319 cpm) (P = 0.062, as determined by Wilcoxon’s matched pairs test), respectively.
FIG. 4.
Mitogen-induced proliferative responses of PBMCs to unheated (open bars) (n = 8) and heat-treated (solid bars) (n = 7) cytoplasmic and cell wall extracts of L. rhamnosus GG at a dilution of 1:10 and to a control culture. The results are expressed in counts per minute; the boxes indicate the lower and upper quartiles, and each central point is the median. The upper end of each bar is the maximum value, and the lower end is the minimum value.
DISCUSSION
Our finding that homogenates derived from L. rhamnosus GG, B. lactis, L. acidophilus, L. delbrueckii subsp. bulgaricus, and S. thermophilus suppress mitogen-induced proliferation of PBMCs suggests that such homogenates could be used in controlling hypersensitivity reactions. Homogenates of these organisms appeared to have similar antiproliferative components. Differences in the levels of suppression may arise from the proportions of these components in specific probiotic strains.
Commensal and pathogenic bacteria differ in terms of their action on immune cells in the gut (7, 12, 17). Bacteria and bacterial homogenates of the commensal gut microflora do not stimulate proliferation of mononuclear cells (7) and play an important role in the maintenance of hyporesponsiveness to foreign antigens (19). Pathogens, in contrast, activate mucosal immune cells and result in the proliferation of these cells, triggering an inflammatory reaction (7, 12). The strains which we studied, L. rhamnosus GG ATCC 53103, B. lactis BB12, L. acidophilus NCFB 1748, L. delbrueckii subsp. bulgaricus ATCC 11842, and S. thermophilus DSM 4022, were found to suppress proliferation. This phenomenon may be attributed to the fact that L. rhamnosus GG ATCC 53103, B. lactis BB12, and L. acidophilus NCFB 1748 belong to the healthy human flora (10, 22, 25). Likewise, the yogurt organisms L. delbrueckii subsp. bulgaricus and S. thermophilus have been shown to share properties with microflora strains found in healthy humans (5, 6, 20, 23, 28, 29). Here we demonstrated that homogenates from these candidate probiotic bacteria suppress immune responses in vitro, a property associated with the function of commensal microflora rather than pathogenic bacteria in the gut.
Viability and survival in the gastrointestinal tract have been considered essential properties of probiotic bacteria (24). It is expected that most bacteria encountered via the enteric route will be disrupted, their cell walls will be broken, and their cell contents will be released (4). Proteases of intestinal bacteria are capable of hydrolyzing luminal proteins into peptides (9), rendering immune cells inert to such proteins, as a part of the natural immune defense (21). In this manner, it is plausible that proteases in homogenates interfere with cell viability during proliferation.
However, the proteases present in preparations are not directly associated with suppression of mitogen-induced proliferation. First, cell viability, as assessed in this study by microscopic evaluation, was not influenced by the addition of preparations containing enzymatic activity. Second, equalization of homogenates on the basis of their enzymatic activities did not result in comparable immunosuppressive activities. Third, heat treatment (i.e., inactivation of proteases) reduced but did not eliminate the suppressive effect of the homogenates. Thus, we concluded that enzyme activity contributes to the suppressive activity of probiotic bacteria; the major mediator of the suppressive effect appears to be the amount of heat-stable bacterial products released from broken cells.
Judging from our findings, the components in homogenates considered to be responsible for immunosuppressive effects are located in the cytoplasm, not in the cell wall. It has been suggested previously that bacterial cell wall and cytoplasmic components modulate the action of immune cells via their receptors (6, 28). More recently, oral ingestion of cytoplasmic fractions of probiotic bacteria has resulted in enhancement of immunoglobulin A responses; this finding is similar to findings obtained after oral supplementation with live probiotic bacteria (11, 13, 26, 27). Furthermore, the antiproliferative effects of the homogenates which we studied confirm previous findings which indicated that probiotic bacteria are involved in the suppression of cytokine production by T cells (28) and thereby help in the generation of T-cell-mediated systemic hyporesponsiveness (30). The precise mechanisms by which these immunomodulatory components operate remain to be investigated.
In summary, the immunomodulatory effects of candidate probiotic strains were associated not only with live microorganisms (in fact, this is the definition of probiotics) but also with nonviable organisms. The use of nonviable probiotics should result in longer shelf life and easier storage. The possible use of probiotic homogenates as components of functional foods must be studied further, and clinical studies are in progress to validate the acceptability of such organisms.
ACKNOWLEDGMENTS
This work was supported by the Academy of Finland.
We thank Mikko Hurme for advice during the study and Tuija Poussa for statistical consultation.
REFERENCES
- 1.Church F C, Swaisgoo H E, Porter D H, Catign G L. Spectrophotometric assay using o-phthaldialdehyde for determination of proteolysis in milk and isolated milk proteins. J Dairy Sci. 1983;66:1219–1227. [Google Scholar]
- 2.Conover W J. The one sample or matched pairs case: the Wilcoxon signed ranks test. In: Conover W J, editor. Practical nonparametric statistics. New York, N.Y: John Wiley & Sons, Inc.; 1980. pp. 280–288. [Google Scholar]
- 3.Conover W J. The one sample or matched pairs case: the Friedman test. In: Conover W J, editor. Practical nonparametric statistics. New York, N.Y: John Wiley & Sons, Inc.; 1980. pp. 299–309. [Google Scholar]
- 4.Conway P L, Gorbach S L, Goldin B R. Survival of lactic acid bacteria in the human stomach and adhesion to intestinal cells. J Dairy Sci. 1987;70:1–12. doi: 10.3168/jds.S0022-0302(87)79974-3. [DOI] [PubMed] [Google Scholar]
- 5.De Simone C, Vasely R, Nergi R, Bianchi-Salvadori B, Zanzoglu S, Cilli A, Lucci L. Enhancement of immune response of murine Peyer’s patches by a diet supplemented with yogurt. Immunopharmacol Immunotoxicol. 1987;9:87–100. doi: 10.3109/08923978709035203. [DOI] [PubMed] [Google Scholar]
- 6.De Simone C, Grassi P P, Bianchi-Salvadori B, Miragliotta G, Vasely R, Jirillo E. Adherence of specific yogurt micro-organisms to human peripheral blood lymphocytes. Microbios. 1988;55:49–57. [PubMed] [Google Scholar]
- 7.Duchman R, Kaiser I, Hermann E, Mayet W, Ewe K, Meyer zum Büschenfeld K H. Tolerance exists towards resident intestinal flora but is broken in active inflammatory bowel disease. Clin Exp Immunol. 1995;102:448. doi: 10.1111/j.1365-2249.1995.tb03836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Exerkate F A, Veer G J C M. Partial isolation and degradation of caseins by cell wall proteinase(s) of Streptococcus cremoris HP. Appl Environ Microbiol. 1985;49:328–332. doi: 10.1128/aem.49.2.328-332.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibson S A W, McFarlan C, Hay S, Macfarlane G T. Significance of microflora in proteolysis in the colon. Appl Environ Microbiol. 1989;55:679–683. doi: 10.1128/aem.55.3.679-683.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldin B R, Goldin S L, Saxelin M, Barakat S, Gualtieri L, Salminen S. Survival of Lactobacillus species (strain GG) in human gastrointestinal tract. Dig Dis Sci. 1992;37:121–128. doi: 10.1007/BF01308354. [DOI] [PubMed] [Google Scholar]
- 11.Isolauri E, Majamaa H, Arvola T, Rantala I, Arvilommi H. Lactobacillus strain GG reverses increased intestinal permeability induced by cow milk in suckling rats. Gastroenterology. 1993;105:1643–1650. doi: 10.1016/0016-5085(93)91059-q. [DOI] [PubMed] [Google Scholar]
- 12.Jiang Y, Magli L, Russo M. Bacterium-dependent induction of cytokines in mononuclear cells and their pathogenic consequences in vivo. Infect Immun. 1999;67:2125–2130. doi: 10.1128/iai.67.5.2125-2130.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaila M, Isolauri E, Saxelin M, Arvilommi H, Vesikari T. Viable versus inactivated Lactobacillus strain GG in acute rotavirus diarrhoea. Arch Dis Child. 1995;72:51–53. doi: 10.1136/adc.72.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirkpatrick C H. Lymphocyte transformation test. In: Roitt I V, Delves P J, editors. Encyclopedia of immunology. New York, N.Y: Academic Press; 1992. pp. 1005–1008. [Google Scholar]
- 15.Majamaa H, Isolauri E. Probiotics: novel approach in management of food allergy. J Allergy Clin Immunol. 1996;99:179–185. doi: 10.1016/s0091-6749(97)70093-9. [DOI] [PubMed] [Google Scholar]
- 16.Marin M L, Lee J H, Murtha J, Ustunol Z, Pestka J J. Differential cytokine production in clonal macrophage and T-cell lines cultured with bifidobacteria. J Dairy Sci. 1997;80:2713–2720. doi: 10.3168/jds.S0022-0302(97)76232-5. [DOI] [PubMed] [Google Scholar]
- 17.Mestecky J, Russell M W, Elson C O. Intestinal IgA: novel views on its function in the defence of the largest mucosal surface. Gut. 1999;44:2–5. doi: 10.1136/gut.44.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miettinen M, Vuopio-Varkila J, Varkila K. Production of human tumor necrosis factor alpha, interleukin-6, and interleukin-10 is induced by lactic acid bacteria. Infect Immun. 1996;64:5403–5405. doi: 10.1128/iai.64.12.5403-5405.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moreau M C, Corthier G. Effect of gastrointestinal microflora on induction and maintenance of oral tolerance to ovalbumin in C3H/HeJ mice. Infect Immun. 1988;56:2766–2768. doi: 10.1128/iai.56.10.2766-2768.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakafuchi S, Takahashi T, Yajima T, Kuwata T, Hirayama K, Itoh K. Strain dependency of the immunopotentiating activity of Lactobacillus delbrückii subsp. bulgaricus. Biosci Biotechnol Biochem. 1999;63:474–479. doi: 10.1271/bbb.63.474. [DOI] [PubMed] [Google Scholar]
- 21.Peng H J, Turner M W, Strobel S. The generation of a tolerogen after ingestion of ovalbumin is time dependent and unrelated to serum levels of immunoreactive antigen. Clin Exp Immunol. 1990;81:520–525. doi: 10.1111/j.1365-2249.1990.tb05365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pochart P, Marteau P, Bouhnik Y, Goderle I, Bourlioux P, Rambaud J P. Survival of bifidobacteria ingested via fermented milk during their passage through the human small intestine: an in vivo study using intestinal perfusion. Am J Clin Nutr. 1992;55:78–80. doi: 10.1093/ajcn/55.1.78. [DOI] [PubMed] [Google Scholar]
- 23.Saavedra J M, Bauman N A, Oung I, Perman J A, Yolken R H. Feeding of Bifidobacterium bifidum and Streptococcus thermophilus to infants in hospital for prevention of diarrhoea and shedding of rotavirus. Lancet. 1994;344:1046–1049. doi: 10.1016/s0140-6736(94)91708-6. [DOI] [PubMed] [Google Scholar]
- 24.Salminen S, Bouley C, Boutron-Ruault M C, Cummings J H, Franck A, Gibson G R, Isolauri E, Moreau M C, Roberfroid M, Rowland I. Functional food science and gastrointestinal physiology and function. Br J Nutr. 1998;80:S147–S171. doi: 10.1079/bjn19980108. [DOI] [PubMed] [Google Scholar]
- 25.Sarem-Damerji L O, Sarem F, Marchal L, Nicolas J P. In vitro colonization ability of human colon mucosa by exogenous Lactobacillus strains. FEMS Microbiol Lett. 1995;131:133–137. doi: 10.1111/j.1574-6968.1995.tb07767.x. [DOI] [PubMed] [Google Scholar]
- 26.Takahashi T, Oka T, Iwana H, Kuwata T, Yamamoto Y. Immune response of mice to orally administered lactic acid bacteria. Biosci Biotechnol Biochem. 1993;57:1557–1560. [Google Scholar]
- 27.Takahashi T, Nakagawa E, Nata T, Yajima T, Kuwata T. Effects of orally ingested Bifidobacterium logum on the mucosal IgA response of mice to dietary antigens. Biosci Biotechnol Biochem. 1998;62:10–15. doi: 10.1271/bbb.62.10. [DOI] [PubMed] [Google Scholar]
- 28.Tejada-Simon M V, Ustunol Z, Pestka J J. Ex vivo effects of lactobacilli, streptococci, and bifidobacteria ingestion on cytokine and nitric oxide production in a murine model. J Food Prot. 1999;62:162–169. doi: 10.4315/0362-028x-62.2.162. [DOI] [PubMed] [Google Scholar]
- 29.Vasely R, Nergi R, Bianchi-Salvadori B, Lavezzari D, De Simone C. Influence of a diet additioned with yogurt on the mouse immune system. Immunopharmacology. 1985;51:30–35. [Google Scholar]
- 30.Weiner H L, Friedman A, Miller A, Khoury S J, Al-Sabbagh A, Santos L, Sayegh M, Nussenblatt R B, Trentham D E, Hafler D A. Oral tolerance: immunological mechanisms and treatment of animal and human organ-specific autoimmune diseases by oral administration of autoantigens. Annu Rev Immunol. 1994;12:809–837. doi: 10.1146/annurev.iy.12.040194.004113. [DOI] [PubMed] [Google Scholar]