Abstract
Background
The past decade of research has seen theoretical and methodological advances in both implementation science and health equity research, opening a window of opportunity for facilitating and accelerating cross-disciplinary exchanges across these fields that have largely operated in siloes. In 2019 and 2020, the National Cancer Institute’s Consortium for Cancer Implementation Science convened an action group focused on ‘health equity and context’ to identify opportunities to advance implementation science. In this paper, we present a narrative review and synthesis of the relevant literature at the intersection of health equity and implementation science, highlight identified opportunities (i.e., public goods) by the action group for advancing implementation science in cancer prevention and control, and integrate the two by providing key recommendations for future directions.
Discussion
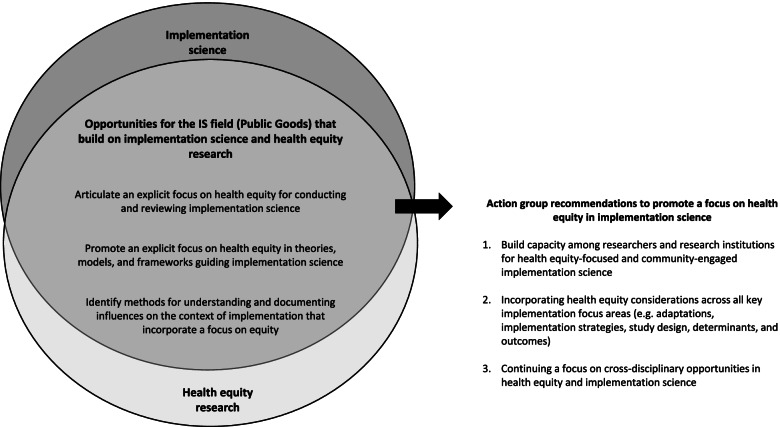
In the review and synthesis of the literature, we highlight recent advances in implementation science, relevant to promoting health equity (e.g., theories/models/frameworks, adaptations, implementation strategies, study designs, implementation determinants, and outcomes). We acknowledge the contributions from the broader field of health equity research and discuss opportunities for integration and synergy with implementation science, which include (1) articulating an explicit focus on health equity for conducting and reviewing implementation science; (2) promoting an explicit focus on health equity in the theories, models, and frameworks guiding implementation science; and (3) identifying methods for understanding and documenting influences on the context of implementation that incorporate a focus on equity.
Summary
To advance the science of implementation with a focus on health equity, we reflect on the essential groundwork needed to promote bi-directional learning between the fields of implementation science and health equity research and recommend (1) building capacity among researchers and research institutions for health equity-focused and community-engaged implementation science; (2) incorporating health equity considerations across all key implementation focus areas (e.g., adaptations, implementation strategies, study design, determinants, and outcomes); and (3) continuing a focus on transdisciplinary opportunities in health equity research and implementation science. We believe that these recommendations can help advance implementation science by incorporating an explicit focus on health equity in the context of cancer prevention and control and beyond.
Keywords: Health equity, Implementation science, Health disparities, Dissemination, Cancer prevention and control
Contributions to the literature.
This paper presents a narrative review and synthesis of the conceptual and empirical literature at the intersection of implementation science and health equity research.
We highlight opportunities identified at the health equity and context working group at the Consortium for Cancer Implementation Science to make a focus on health equity in IS foundational and explicit.
Informed by the narrative review and identified opportunities by the action group, we offer recommendations that reflect the essential groundwork needed to promote bi-directional learning and synergy between the fields of implementation science and health equity research.
Background
Over the past few decades, considerable public health and medical research has focused on identifying, understanding, and addressing health inequities, defined as unjust differences in health outcomes across population groups that are shaped by structural and social determinants of health [1–3]. The central role that these determinants play, in creating and reinforcing health inequities, has been particularly evident during the ongoing COVID-19 global pandemic [4, 5]. Consequently, there continue to be calls for a greater focus on health equity research that is social justice and action-oriented (e.g., focused on solutions), assets- or strengths-based, and actively seeks to promote and create conditions that facilitate the highest level of health for all [6, 7]. While there are recent conceptual, empirical, and methodological advances in Implementation Science (IS) [8], only a subset of this work has explicitly focused on promoting health equity [9], which we distinguish and operationalize using peer-reviewed literature in Table 1.
Table 1.
Concepts, definitions, and considerations on what the literature says about health equity
| Health differences | Health disparities / inequalities / inequities | Health equity / equality |
|---|---|---|
|
• When differences are noted in health outcomes, between two groups based on a specific characteristic such as race, income, among other social or structural attributes of the population • Not all health differences warrant focused attention but health differences adversely affecting socially disadvantaged groups are particularly unacceptable because ill health can be an obstacle to overcoming social disadvantage [10]. • “Not all health differences are health disparities;” Paula Braveman suggests that health disparities are concerned with social justice (i.e., justice with respect to treatment of more advantaged vs. less advantaged socioeconomic groups in terms of healthcare) [1] |
• Kawachi, I., and colleagues consider health inequality as a “generic term used to designate differences, variations, and disparities in the health achievements of individuals and groups.” [11] • Whitehead, M., suggests that “inequalities” in the European context have the same connotations of unfairness and injustice as the terms “inequities” [12] • Health disparities are differences that adversely affect socially disadvantaged groups; they are a specific subset of health differences that are relevant to social justice because they may arise from intentional or unintentional discrimination or marginalization and are likely to reinforce social disadvantage and vulnerability [7] • Health disparity is a more charged term; “to many a disparity implies an inequity or an injustice rather than a simple inequality” [13] • Health disparities emerge and persist through complex mechanisms that include socioeconomic, environmental, and system-level factors [14] • According to Kawachi, I. and colleagues, the term health inequity refers to those inequalities in health that are deemed to be unfair or stemming from some form on injustice [15] How to determine whether a difference in health outcomes between groups is a disparity or not (in other words, are they unjust and unfair?) • Which differences are inevitable, unavoidable, unnecessary, and unfair, will vary from country to country and from time to time [16]. • “Determining when a difference becomes a disparity may be problematic because a disparity is not measured directly, but rather as a residual or a difference between two groups, often only after other factors that might contribute to that difference have been statistically controlled for (more specifically in the context of racial and ethnic disparities” [13] |
• “Equality is providing everyone with the same tools and resources. Equity is providing tools and resources based on needs that allow everyone the opportunity to be as healthy as possible.” [17] • “Health equity is the principle underlying a commitment to reduce, and ultimately, eliminate disparities in health and in its determinants, including social determinants.” [1] • “Health disparities and their determinants are the metric for assessing health equity, the principle underlying a commitment to reducing disparities in health and its determinants; health equity is social justice in health.” [7] • “Attainment of the highest level of health for all people. Achieving health equity requires valuing people equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and healthcare disparities” (Healthy People, 2020) • Equity in health care is the equal access to available care for equal need; equal utilization for equal need; equal quality of care for all [16]. • The crux of the distinction between equality and equity is that what we identify as a health inequity, depend on our own theories of justice, what we believe is society, and our reasoning on why we think health inequities exist [11]. |
Outside IS, there is a long and continuing history of scholarship related to health equity and the critical role of community-based participatory research (CBPR) approaches with racially and ethnically diverse communities [18–20]. This scholarship recognizes and establishes the role of social determinants of health, structural and interpersonal racism, historical trauma, and cultural-centeredness for implementing evidence-based interventions, programs, practices, and policies (referred to henceforth as EBIs) [21–23]. Despite the development of many EBIs and their demonstrated effectiveness among populations experiencing health inequities, widespread uptake of these interventions to improve population health outcomes has been limited [24–26]. There continues to be a limited focus on understanding the intersection of important social and structural dimensions that impact health and include age, disability, sexual orientation, gender identity, and geographic location (e.g., rural, urban) [18, 19], which can have implications for differing access to resources, opportunities, power, and/or obstacles that promote or hinder health. Furthermore, health equity and implementation researchers have largely operated in siloes, resulting in a lack of clarity and articulation of existing and potential synergies across these fields of research.
Recently however, there is a recognizable and explicit shift towards greater focus on health equity within IS [20–22]. For example, Baumann and Cabassa encourage integration of health equity across all IS aspects with a focus on reach from the start of the research projects, designing and selecting interventions with underserved populations, developing implementation strategies that help reduce disparities, advancing the science of adaptation, and using an equity lens for implementation outcomes [27]. Building on this, Brownson and colleagues propose establishing a scientific evidence base for health equity in IS, strengthening methods and measures, and focusing more on context—each requiring involvement of a wide range of stakeholders including researchers, program evaluators, funders, practitioners, communities, and advocates [9]. A recent article by Loper and colleagues operationalized equitable implementation as “including an explicit attention to the culture, history, values, assets and needs of the community and integration of these in to the principles, strategies, frameworks, and tools of IS” [23].
For this paper, consistent with prior definitions [24], we consider and refer to IS as a scientific field that incorporates perspectives from research, practice, and policy with the intent to bridge the gap between these and include a focus on both dissemination and implementation research. We argue that a greater focus is needed in IS on actively promoting health equity through explicit consideration of the social and structural injustices [25, 26]. Such an approach is critical and central to implementation science, with important implications for the types of EBIs we prioritize, disseminate, and implement in both our research and practice efforts. In this paper, we reflect on opportunities for cross-disciplinary, bi-directional, and collaborative learning between the fields of IS and health equity scholarship, and provide recommendations for enhancing a focus on health equity in the context of cancer prevention and control research.
Consortium for Cancer Implementation Science (CCIS)
Research to promote health equity is an important area of focus for cancer prevention and control, which encompasses the “conduct of basic and applied research in the behavioral, social, and population sciences to create or enhance interventions that, independently or in combination with biomedical approaches, reduce cancer risk, incidence, morbidity and mortality, and improve quality of life” [28, 29]. To advance the mission of cancer prevention and control, the National Cancer Institute’s (NCI) Implementation Science team led the charge on creating the first Consortium for Cancer Implementation Science (CCIS) (previously called the Implementation Science Consortium in Cancer) as an innovative approach to produce “public goods” (considered to be papers, future meetings, workshops, and funding opportunities) and facilitate multidisciplinary collaborations in priority areas of research (i.e., technology, policy, learning health care systems, community participation, global health, health equity, complex/multilevel interventions, and study designs). Over two annual consortium meetings, in 2019 (in-person and virtual) and 2020 (only virtual), 522 researchers and practitioners from across the globe came together to engage in working groups dedicated to advancing the science of implementation [30, 31].
Members of the “Health Equity and Context” action group and their co-leads (authors, PA & RS for 2019 and PA, RS, AO, SW, AK for 2020) were charged with broadly reflecting on the intersection of IS and health equity research and exploring opportunities for synergy and learning across these fields, particularly in the context of cancer prevention and control. In preparation for the working group discussions (both in 2019 and 2020), co-leads conducted comprehensive scans of the literature that included a focus on IS and health equity research. This literature was synthesized and briefly presented to the action group for grounding, at the meetings in both 2019 and 2020. This paper is a result of the action group discussions that identified a need to review recent advances in IS and recognize the extensive history of health equity research that can inform IS through identified opportunities. Ninety unique participants (a mix of researchers and practitioners interested in IS and equity research, of varying levels of expertise) met over 2 days in 2019 and 2020 to learn, discuss priorities, and generate opportunities for incorporating a focus on health equity and context within IS. We present below the identified opportunities that are guided by a narrative review and synthesis of the extant literature, as ‘public goods’ to advance the science of implementation focused on cancer prevention and control.
Opportunity 1: articulate an explicit focus on health equity for conducting and reviewing implementation science
Action group discussants identified a lack of explicit focus on health equity within IS and recognized the utility of developing a statement for the field about the importance of promoting and incorporating a focus on health equity. These discussions began in 2019 and were further emphasized in 2020, given the inequities highlighted with the ongoing global COVID-19 pandemic and national reckoning around structural racism [5]. In addition, discussants suggested addressing fundamental issues in the IS field that shape the nature of the research conducted, including provision of explicit language and definitions of health equity (attempted in Table 1) for funding announcements and review criteria in IS. Ultimately, the group sought to make equity a foundational grounding for the field which could ensure that we do not reinforce health inequities through our research [9, 32].
Discussants reviewed several opportunities with the goal of articulating an explicit focus on health equity in IS that could guide research and peer review. First, participants suggested developing a “checklist” that could guide considerations for health equity in implementation research. Examples of such equity-focused checklists, widely used in reporting studies (outside the field of IS) include the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRIMSA)-Equity checklist [27, 33] and the Consolidated Standards of Reporting Trials (CONSORT)-Equity extension for improved reporting of health equity in randomized trials [34]. The Campbell and Cochrane Equity Methods group has lead the development of such checklists, in addition to the ongoing international effort to incorporate a focus on equity for the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [35]. Similar to these checklists for study designs, participants recommended creating a IS-specific checklist to guide both researchers and funders as they proposed and reviewed studies focused on health equity.
Another opportunity identified to increase the focus on health equity in IS was the development of a values-orientation statement or a self-reflection guide that could be used by implementation researchers and practitioners to examine personal beliefs and biases related to health equity. Such an approach could also incorporate considerations for research institutions, community partners, and funding agencies, to operationalize how equity can be a fundamental consideration for IS studies [5, 9]. Such a guide could be informed by theories such as Critical Race Theory and the proposed Public Health Critical Race Praxis, which explicitly recognizes the societal and structural forms of racial discrimination and the consequences this may have for the effectiveness and sustainability of interventions [36, 37]. Finally, the group also recommended curating either exemplar research studies, case studies, or existing resources to reflect the integration of health equity in IS.
Opportunity 2: promote an explicit focus on health equity in theories, models, and frameworks guiding implementation science
The action group discussions prioritized considering how equity could be integrated into existing implementation theories, models, and frameworks (TMFs). With approximately 150 TMFs [38, 39], implementation scientists have emphasized the value of TMFs and theorizing [39, 40] in research studies. Despite a wealth of TMFs, very few have included an explicit focus on improving health equity [41, 42] or been modified to incorporate a health equity focus [20]. Noting a recent trend, a few determinant frameworks have been revised critically to an explicit focus on health equity and include the Health Equity Implementation Framework by Woodward and colleagues [20], the race-conscious adaptation of the Consolidated Framework for Implementation Research [43], and application of an intersectionality lens to the Theoretical Domains Framework [44]. In terms of outcome frameworks, a recent extension of RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) model [41] now incorporates an explicit focus on equity and cost to facilitate the long-term sustainability and evolvability of EBIs over time [45]. Despite this progress, none of the TMFs comprehensively or explicitly incorporate or integrate established determinants of health equity (e.g., social determinants of health, structural discrimination, and racism) [5], which could be improved with continued efforts to engage health equity researchers.
The group also suggested conducting a scoping review of existing health equity frameworks that have a strong relevance for IS. This was recently highlighted in a scoping review of TMFs widely used in anthropology (e.g., theories of intersectionality, structural governance) and how they could inform a focus on health equity in ongoing and future implementation-focused studies [46]. Such integration of key health equity theories into IS can provide more depth in recognizing the role of structural and social determinants of health. Additionally, the group also recognized opportunities for bi-directional learning for health equity researchers to incorporate implementation considerations. For example, health equity research could benefit from the explicit considerations for implementation determinants at multiple socioecological levels and for partners involved in the delivery and implementation of EBIs [47], particularly as they relate to implementing change in organizational and policy contexts [48–50]. To integrate relevant work across these fields, the action group suggested convening a meeting of IS and health equity TMF developers and users to adapt existing frameworks to explicitly incorporate a health equity focus.
Opportunity 3: identify methods for understanding and documenting influences on the context of implementation that incorporate a focus on equity
In planning for implementation, studies often assess and understand context [51, 52] that is operationalized across multiple levels of socioecological influence within healthcare settings [53]. Several discussants highlighted the importance of including an operationalization of health equity as part of “context” when studying the implementation of EBIs. Although the field needs to prioritize harmonizing the conceptualization of context across implementation studies, there is an urgent need to include a focus on historical and ongoing aspects of context that reflect structural roots of inequities such as structural racism [5] and historical trauma [54]. According to a recent review, only three TMFs in IS (i.e., Consolidated Framework for Implementation Research [51], Theoretical Domain Framework [55], and the integrated Promoting Action on Research Implementation in Health Services framework [56]) provide a specific definition of context [57], but without an explicit consideration for social and structural determinants of health. Even with considerable variations in the conceptualization of context, the most common dimensions identified were organizational support, financial resources, social relations and support, and leadership, suggesting that important gaps remain with respect to understanding and addressing health equity [57]. Outer context (i.e., external policies and incentives) which is an important but understudied aspect has an important influence on health equity, as it has important implications for distribution of resources and opportunities, and can set the broader environment in which organizational settings operate and provide services, with potential implications for inequitable implementation and delivery of care across resource-limited settings and underserved populations [58].
Understanding the impact of interventions on multiple socioecological levels is a priority for the NCI (https://healthcaredelivery.cancer.gov/mlti/) and refining methods for contextual assessment can be critical to supporting empirical studies that aim at promoting health equity. Contextual assessments can also inform the development and testing of implementation strategies across diverse settings and populations [59, 60]. Specifically, the group recognized the need to expand considerations for context beyond healthcare organizations to include interpersonal, community, and policy context. Recognizing ongoing efforts [61], the group proposed conducting a review of best practices for methods and measures that inform an assessment of contextual determinants and barriers/facilitators, particularly relevant to resource-limited settings and understudied populations. Such a review could inform the development of a methodology document for best practices that promotes an equity focus and includes specific measures that have been used for structural racism, discrimination, historical trauma, persistent poverty, and social deprivation, among others.
Discussion
Taken together, the narrative review and the CCIS action group discussions highlight the growing importance of making health equity an explicit, central, foundational focus in IS. In advancing this work, our review makes it clear that there is a significant literature base around health equity [62–67]. This work can help IS researchers and practitioners reflect on and potentially evaluate whether or not their work reduces or inadvertently exacerbates inequities; additionally, for those without training and experience, there may be opportunities to partner with existing health equity experts, elevate and learn from their work, and ultimately advance research in this area. We acknowledge some limitations of this work. This was not a formal data collection effort for the participants in the working group; instead, discussions were undertaken as a participatory approach to engage researchers interested in health equity and context. In this vein, we may have missed some important perspectives. The intent of this review was to ground and contextualize the ideas and reflections during the working group discussions and we may have missed relevant literature in this narrative review. The authors of this paper, however, collectively support the opportunities identified by the CCIS Health Equity and Context action group related to focusing on health equity in conducting and peer-reviewing IS, in applying a health equity focus in IS-related TMFs, and when conducting contextual assessments. In order for these opportunities to advance the science of implementation, we present broad recommendations beyond the field of cancer prevention and control that can ensure progress in bi-directional learning and synergies between the fields of IS and health equity research (as shown in Fig. 1).
Fig. 1.
Opportunities and recommendations to promote health equity in implementation science, perspectives from the Health Equity and Context working group at the Consortium for Cancer Implementation Science
Recommendation 1: build capacity among researchers and research institutions for health equity-focused and community-engaged IS
As a field, IS emphasizes the importance of multidisciplinary, stakeholder-engaged research for implementing EBIs, yet engagement with communities is not widespread in IS [8, 68–70]. CBPR is a broad term and reflects approaches, such as participatory action research, community-partnered, -engaged, and/or -based research, which exist along a continuum in terms of extent of community involvement, equitable resources, and decision-making power [71]. The central role of stakeholder and community engagement in promoting health equity has been the result of decades of work using CBPR approaches that prioritize community engagement in addressing inequities [63, 72]. In most instances, there is an emphasis on action, social justice, capacity building, and facilitating equitable partnerships [73]. As implementation scientists, partnering with community-engaged researchers can be critical in not rushing to “quick action”, and incorporating prior knowledge so as not to mischaracterize the inequities prevalent in the implementation context or the solutions to address them [74].
Researchers can incorporate CBPR approaches to make community and stakeholder voices integral to implementation research [68, 75]. While much of CBPR has focused on the community level, implementation scientists have the opportunity to expand this lens and apply it to a range of stakeholders at the policy, organizational, healthcare systems that include providers, healthcare administrators, and patients. The field of IS offers a natural fit for the commitment of participatory approaches which includes co-producing knowledge and action, as well as for systems change. An implementation brief put forth by the National Implementation Research Network proposes establishing a “co-creation environment” to promote collaborations among these various stakeholders and supports the capacity to promote the adoption, implementation, and sustainability of research evidence [76]. Such cross-disciplinary approaches have been used to build capacity and identify and implement breast cancer prevention-related EBIs across multiple jurisdictions in California, which led to the development of sustainable infrastructure models for primary prevention of breast cancer programs and implementation of research evidence [77, 78].
Recognizing the potential synergy between the fields of IS and CBPR, a special issue in the Journal of Translational Behavioral Medicine focused on “community-engaged dissemination or implementation research,” which included studies to implement EBIs within clinical or community-based settings using CBPR approaches [79]. From an equity perspective, it may be useful to take a “participatory implementation science” approach in IS while considering the levels of engagement between researchers and partners involved or impacted by the implementation efforts [68]. Consistent with capacity building, this approach ensures that diverse organizations and stakeholders have the knowledge, skills, and resources to implement and sustain EBIs [75] and is especially important as we strive to improve the quality and quantity of practice-based evidence to inform implementation efforts. As examples, frameworks such as Intervention Mapping [80, 81] and Transcreation Framework [82] incorporate co-creation of EBIs from the start in partnerships with communities, providing step-by-step processes to develop and evaluate interventions for the real-world community settings and account for important contextual factors and other influences in a population and setting. In fact, to effectively “design for dissemination” intervention researchers and/or program developers must assess, document, and address real-world needs, assets, and contextual realities of priority populations through consistent participatory engagement and co-learning [37, 83].
Pursuing health equity-oriented research can be demanding even for experienced researchers, and promoting training and opportunities to gain the skills and knowledge to do this work effectively is important for the advancing the field. Although there has been an increase (up to 55% in 2018) of implementation scientists engaging with stakeholders, there continues to be a lack of specificity around the methods of engagement and a misalignment with academic priorities of tenure and promotion [84, 85]. Determining the required competencies for researchers focused on health equity may serve as important next steps [86], with a specific focus on IS [87]; further, evaluating perceptions of researchers working at the intersection of health equity and IS might allow for a comprehensive understanding of the motivations and barriers to proposing and conducting equity-oriented IS. Efforts at the national level [88] are needed to provide career development opportunities that prioritize recruitment and retention of scholars from under-represented groups and support scholars conducting or interested in learning how to conduct equity-oriented research.
Recommendation 2: incorporate health equity considerations across key implementation focus areas (e.g., adaptation, implementation strategies, study design, determinants, and outcomes)
With growing number of EBIs, existing guidance has helped researchers identify where along the translational pipeline to intervene, when addressing health inequities. For example, Chinman et al. outlined a decision tree to help researchers select an effectiveness and/or implementation trial design, depending on the goal of either identifying, understanding, or addressing disparities/inequities [89]. McNulty et al. highlight methodological approaches for conducting implementation research to advance health equity that includes a paradigm of focusing on existing data with systems science methods, including populations with inequities to design new studies, or a focus exclusively on populations experiencing inequities [90]. Incorporating a focus on health equity has important implications for the research questions being answered and whether or not the outcomes of an implementation effort would differ based on the incorporation of diverse settings and populations. Despite the focus on implementation, most interventions are not optimized prior to delivery and may influence both the effectiveness and the implementation of the EBIs. Consequently, a significant focus in the field of IS has been on studying the adaptation of interventions as a potential opportunity to enhance effectiveness, improve fit in the implementation context, and increase the likelihood of sustainability [91].
The science of adaptation has tremendous promise in promoting health equity [21, 67]. Although adaptations can improve the EBI’s effectiveness [92–94], it could also render the intervention less effective if key components are removed [95, 96]. For these reasons, it is important to specifically and systematically report considerations for why and how the adaptations were made, especially when working with resource-limited settings and underserved populations. Frameworks such as the Framework for Reporting Adaptations and Modifications – Expanded (FRAME) [97] support the systematic documentation of adaptation and can contribute to understanding the impact of adaptation on health equity. Complementary to this effort, a scoping review identified 13 frameworks that were consolidated to identify eight commonly used adaptation steps or processes to guide researchers and practitioners in the field [98]. A synthesis of the key steps required for facilitating planned adaptations provides an important contribution to the field; however, evidence is still needed to determine whether these steps need to be modified based on the type of intervention or setting. It is also critical to ensure that the guidance offered is actionable in organizations that may not have staff with formal training in public health, health disparities, or IS, which also presents a unique opportunity to test these adaptation frameworks with respect to health equity goals.
Since the push in 2013 for reporting and specifying implementation strategies [99], the field has progressed tremendously with the introduction of the Expert Recommendations for Implementing Change (ERIC) taxonomy [100], with calls for more focus on effectiveness research evaluating discrete implementation strategies [59] as well as mechanisms through which strategies influence implementation and health outcomes [60]. What is often missing in this discussion, however, are implications on advancing equity [46]. There is an urgent need to explicitly evaluate whether certain implementation strategies are effective at promoting equity or reducing inequities [9, 59]. Questions to consider regarding strategies may be as follows: (1) which are more acceptable and feasible in resource-limited settings or underserved populations; (2) which are more appropriate or effective in promoting equity; and (3) what are the specific mechanisms through which they operate to promote equity when creating change? Implementation Mapping as a methodology provides a systematic process for planning (or selecting and tailoring) implementation strategies and explicitly integrates both a participatory and an equity perspective [101]. Although future work is needed to validate this method, the process guides the engagement of the community throughout the process and considers the possibility of tailoring (differentiating) specific strategies depending on the unique needs of subgroups within the populations of interest. Future research is needed to integrate an explicit attention to the culture, context, history, and needs of the communities, when prioritizing the selection and tailoring of strategies that can facilitate the effective implementation and sustainment of EBIs among historically and systematically underserved populations, supported in the projects designed at optimizing strategies [102], in the recently funded Implementation Science Centers in Cancer Control [103].
Recommendation 3: continuing a focus on cross-disciplinary opportunities in health equity and implementation science
True to the spirit of IS, we believe in continuing conversations with researchers and practitioners across disciplines, to generate cross-disciplinary, multi-sector solutions that promote health equity. The recent calls from the National Institutes of Health, and the NCI in particular, provide important opportunities to provide information on innovative and provoking ideas to promote health equity and address inequities and promote a diverse biomedical workforce [104, 105]. Emerging cross-disciplinary conversations among implementation, policy scientists, and economists showcase the added value of and the promising strategies to promote equity while advancing the science of implementation [49]. Researchers will also need to seek out opportunities to engage communities across a range of social and structural dimensions (i.e., race/ethnicity, socioeconomic status, age, disability, sexual orientation, gender identity, and geographic location (e.g., rural, urban)). In 2020, the CCIS steering committee promoted the inclusion of practitioners and policymakers as essential partners for integrating IS and health equity research to produce meaningful and sustained impact [30]. Such integration is aligned with Health in All Policies initiatives [106, 107], multisectoral approaches [108, 109], and promotion of community engagement in IS [70], all of which are crucial in generating relevant, feasible, and sustainable solutions to promoting health equity.
While multidisciplinary collaborations will be critical, it is also important to recognize the growing research around implementing interventions across diverse populations (i.e., among indigenous Maori community in New Zealand [110]), settings (i.e., applications of CFIR in low-and middle-income countries [111]), research institutions (i.e., among Clinical and Translational Science awardees [22] and offices of community outreach and engagement in NCI-designated cancer centers [112]), and for non-cancer-focused research priorities (i.e., cardiovascular disease [113, 114], genomic medicine [115]). Lessons learned from such applications of IS methods, TMFs, and study designs can highlight innovative and effective strategies to promote health equity. Even when new EBIs are developed and tested for diverse populations and settings, alignment with or consideration of IS will be critical. Guidance from the recent theoretical advances, such as the ConNECT framework, put forth collectively by the Society for Behavioral Medicine’s Ethnic Minority and Multicultural Health Special Interest group, can be key in integrating context, fostering a norm of inclusion, ensuring equitable diffusion of innovations, harnessing communication technology, and prioritizing specialized training [116]. Research networks like CPCRN that are building capacity through trainings on “Putting Public Health Evidence into Action” can serve as additional opportunities for diverse stakeholders to understand intervention impact and utility across the implementation continuum [117, 118].
Inventive and resourceful collaborations are essential in tackling evolving challenges on addressing the adverse influences of multiple socioecological levels on health and healthcare [119], study the impact of complex interventions [120], and achieve sustainability for potential impact and value/return on investment in interventions [121]. Decades of intervention research produced in controlled environments, coupled with traditional linear approaches, have failed to achieve the intended population health outcomes in the real-world settings [53, 122]. Although the complexity associated with interventions needed to change health outcomes has a long history of recognition, only recently have there been efforts in improving the capacity in terms of skills and collaborations [80, 123]. More often than not, research takes place in settings that have sufficient resources enabling them to participate in research without disrupting the provision of clinical, community, or public health services. When funding ends, implementing and sustaining interventions often requires additional resources in terms of staff, time, and money, or scaling out of the intervention to reach diverse settings [124]. The current funding climate requires researchers to think creatively and keep sustainability at the center of all decisions related to research and partnerships its potential impact and potential value/return on investment, in terms of practice [91]. Implementation researchers could also benefit and contribute towards health equity goals by proposing studies using pragmatic designs [125], incorporating multilevel analyses [53], and engaging in the science of complex interventions [126].
Conclusions
The ongoing COVID-19 pandemic has made apparent the longstanding structural inequities and systems that create widespread health inequities at a population level [127]. Addressing these will require a sharp focus on understanding the varied mechanisms by which underlying fundamental injustices (e.g., racism, discrimination) and social determinants of health influence, and in some case hinder, the implementation of policies and programs for populations. The complex, multilevel array of factors that contribute to health inequities also have important implications for the implementation of EBIs across diverse settings/populations [128], though they have not always been explicitly identified as such [129, 130]. While we recognize the complexity in addressing these structural, upstream challenges, the ongoing public-health crises present important opportunities for changing systems on a broad scale by taking a proactive approach to incorporate a focus on health equity in ongoing and future implementation studies [25, 131].
Myriad factors within the field of IS contribute to a lack of explicit focus on health equity [84]. However, the underlying premise of the IS field is to make sure EBIs have widespread impact and that they benefit populations representing diversity with respect to race/ethnicity, socioeconomic status, age, disability, sexual orientation, gender identity, and geographic location (e.g., rural, urban) [132, 133]. Identifying and integrating research that reflects the long history of equity research can propel IS to be more inclusive of and committed to health equity. On the other hand, a continued lack of explicit focus on equity in the field can make it difficult to track whether health equity goals are achieved and increase the risk of expanding the translation gap with greater exclusion of those who may benefit most from interventions to improve health. Increasing health equity is within reach, if we commit to building capacity and continue to collaborate with multidisciplinary researchers, practitioners both in health and non-health sectors, policy makers, and most importantly individuals with lived experiences, with a reframe of our theories, frameworks, and methods with equity at the forefront. Beginning with the acknowledgement that health is not distributed across all populations equally, we can work collectively to promote a science for implementation that benefits all, with no one left behind.
Acknowledgements
We thank all participants of the Consortium for Cancer Implementation Science (previously known as Implementation Science Consortium in Cancer) for their ideas and insights contributed during the group discussions that informed the thinking for this paper.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- IS
Implementation science
- NIH
National Institutes of Health
- ISCC
Implementation Science Consortium in Cancer
- CCIS
Consortium for Cancer Implementation Science
- NCI
National Cancer Institute
- EBI
Evidence-based intervention
- TMF
Theories, Models, and Frameworks
Authors’ contributions
PA and RS conceptualized the article and drafted the manuscript. DC, HM, MF, SR, ET, JL, BB, LF, CE, KE, MS, AO, AK, and SW participated in the workgroup discussions that informed the manuscript making substantial contributions to the design and analysis presented in the paper and revised it critically for important intellectual content. All authors have provided final approval of the manuscript and agree with all aspects of the work.
Funding
PA: This work was conducted as a part of the Cancer Prevention Fellowship Program, funded by the National Cancer Institute. The research was also supported by an Internal Research Grant (PI: Adsul, P.) from the American Cancer Society 131567-IRG-17-178-22-IRG (PI: Ozbun, M.).
HMB: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number P30CA021765 and the American Lebanese and Syrian Associated Charities (ALSAC) of St. Jude Children’s Research Hospital.
Availability of data and materials
All meeting reports from the 2019 and 2020 Consortium for Cancer Implementation Science (previously known as the Implementation Science Consortium in Cancer) are available at: https://cancercontrol.cancer.gov/is/initiatives/iscc
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors approved the final version of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Prajakta Adsul, Email: padsul@salud.unm.edu.
David Chambers, Email: dchambers@mail.nih.gov.
Heather M. Brandt, Email: heather.brandt@stjude.org
Maria E. Fernandez, Email: Maria.E.Fernandez@uth.tmc.edu
Shoba Ramanadhan, Email: sramanadhan@hsph.harvard.edu.
Essie Torres, Email: torrese@ecu.edu.
Jennifer Leeman, jleeman@email.unc.edu.
Barbara Baquero, Email: bbaquero@uw.edu.
Linda Fleischer, Email: linda.fleisher@fccc.edu.
Cam Escoffery, Email: cescoff@emory.edu.
Karen Emmons, Email: kemmons@hsph.harvard.edu.
Montserrat Soler, Email: solerm@ccf.org.
April Oh, Email: april.oh@nih.gov.
Ariella R. Korn, Email: ariella.korn@nih.gov
Stephanie Wheeler, Email: stephanie_wheeler@unc.edu.
Rachel C. Shelton, Email: rs3108@cumc.columbia.edu
References
- 1.Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep (Washington, DC: 1974) 2014;129(Suppl 2):5–8. doi: 10.1177/00333549141291S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braveman PA. Swimming against the tide: challenges in pursuing health equity today. Acad Med. 2019;94(2):170–171. doi: 10.1097/ACM.0000000000002529. [DOI] [PubMed] [Google Scholar]
- 4.Lopez L, III, Hart LH, III, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 5.Shelton RC, Adsul P, Oh A. Recommendations for addressing structural racism in implementation science: a call to the field. Ethn Dis. 2021;31(Suppl 1):357–364. doi: 10.18865/ed.31.S1.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Srinivasan S, Williams SD. Transitioning from health disparities to a health equity research agenda: the time is now. Public Health Rep (Washington, DC: 1974) 2014;129(Suppl 2):71–76. doi: 10.1177/00333549141291S213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braveman PA, Kumanyika S, Fielding J, Laveist T, Borrell LN, Manderscheid R, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(Suppl 1):S149–SS55. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brownson RC, Colditz GA, Proctor EK. Dissemination and implementation research in health: translating science to practice. New York: Oxford University Press; 2017.
- 9.Brownson RC, Kumanyika SK, Kreuter MW, Haire-Joshu D. Implementation science should give higher priority to health equity. Implement Sci. 2021;16(1):28. doi: 10.1186/s13012-021-01097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sen A. Development as freedom. New York: A division of random house. Inc; 1999. p. 3. [Google Scholar]
- 11.Kawachi I, Subramanian SV, Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health. 2002;56(9):647–652. doi: 10.1136/jech.56.9.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitehead M. A typology of actions to tackle social inequalities in health. J Epidemiol Community Health. 2007;61(6):473–478. doi: 10.1136/jech.2005.037242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hebert PL, Sisk JE, Howell EA. When does a difference become a disparity? Conceptualizing racial and ethnic disparities in health. Health Aff. 2008;27(2):374–382. doi: 10.1377/hlthaff.27.2.374. [DOI] [PubMed] [Google Scholar]
- 14.Brown AF, Ma GX, Miranda J, Eng E, Castille D, Brockie T, et al. Structural interventions to reduce and eliminate health disparities. Am J Public Health. 2019;109(S1):S72–Ss8. doi: 10.2105/AJPH.2018.304844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106. doi: 10.3402/gha.v8.27106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whitehead M. The concepts and principles of equity and health. Health Promot Int. 1991;6(3):217–228. doi: 10.1093/heapro/6.3.217. [DOI] [PubMed] [Google Scholar]
- 17.Society AC. Making the case for health equity: American Cancer Society; 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-prevention-and-earlydetection-facts-and-figures/making-the-case-for-health-equity.pdf.
- 18.Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and funding trends. Cancer Epidemiol Biomarkers Prev. 2017;26(7):992–997. doi: 10.1158/1055-9965.EPI-17-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weaver SJ, Blake KD, Vanderpool RC, Gardner B, Croyle RT, Srinivasan S. Advancing rural cancer control research: National Cancer Institute efforts to identify gaps and opportunities. Cancer Epidemiol Biomark Prev. 2020;29(8):1515–1518. doi: 10.1158/1055-9965.EPI-20-0453. [DOI] [PubMed] [Google Scholar]
- 20.Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement Sci. 2019;14(1):26. doi: 10.1186/s13012-019-0861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res. 2020;20(1):190. doi: 10.1186/s12913-020-4975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nooraie RY, Kwan BM, Cohn E, AuYoung M, Roberts MC, Adsul P, et al. Advancing health equity through CTSA programs: opportunities for interaction between health equity, dissemination & implementation and translational science. J Clin Transl Sci. 4(3):168–175. [DOI] [PMC free article] [PubMed]
- 23.Loper A, Woo B, Metz A. Equity is fundamental to implementation science. Stanf Soc Innov Rev. 2021;19(3):A3–A5. [Google Scholar]
- 24.DHHS . PAR-19-274 dissemination and implementation research in health. 2019. [Google Scholar]
- 25.Chambers DA. Considering the intersection between implementation science and COVID-19. Implement Res Pract. 2020;1:0020764020925994. doi: 10.1177/0020764020925994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shelton RC, Adsul P, Oh A, Moise N, Griffith DM. Application of an antiracism lens in the field of implementation science (IS): recommendations for reframing implementation research with a focus on justice and racial equity. Implement Res Pract. 2021;2:26334895211049482. doi: 10.1177/26334895211049482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Welch V, Petticrew M, Tugwell P, Moher D, O’Neill J, Waters E, et al. PRISMA-Equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. 2012;9(10):e1001333. doi: 10.1371/journal.pmed.1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.NCI . Cancer control framework and synthesis rationale. 1998. [Google Scholar]
- 29.Adjei BA, White DP, McCarthy S, Priede LM, Baker M, Kent EE, et al. Opportunities for cancer health care disparities and care delivery research: an analysis of the NCI Health Care Delivery Research Program Portfolio. J Health Care Poor Underserved. 2021;32(3):1475–1492. doi: 10.1353/hpu.2021.0145. [DOI] [PubMed] [Google Scholar]
- 30.NCI . Implementation Science Consortium in Cancer (ISCC) meeting summary report 2020. 2020. [Google Scholar]
- 31.NCI. Implementation Science Consortium in Cancer meeting summary report 2019. Available from: https://cancercontrol.cancer.gov/sites/default/files/2020-05/ISCC-MeetingSummary.pdf. Cited 2021.
- 32.Adsul P, Chambers DA. Advancing research practice partnerships to achieve population-level mental health outcomes. Glob Soc Welf. 2019;6(3):155–158. doi: 10.1007/s40609-018-0130-z. [DOI] [Google Scholar]
- 33.Welch V, Petticrew M, Petkovic J, Moher D, Waters E, White H, et al. Extending the PRISMA statement to equity-focused systematic reviews (PRISMA-E 2012): explanation and elaboration. J Clin Epidemiol. 2016;70:68–89. doi: 10.1016/j.jclinepi.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Welch VA, Norheim OF, Jull J, Cookson R, Sommerfelt H, Tugwell P. CONSORT-Equity 2017 extension and elaboration for better reporting of health equity in randomised trials. BMJ (Clinical research ed) 2017;359:j5085. doi: 10.1136/bmj.j5085. [DOI] [PubMed] [Google Scholar]
- 35.Methods C. STROBE-Equity: improving social justice in observational studies [2.23.2021]. Available from: https://methods.cochrane.org/equity/projects/strobe-equity. Accessed 28 May 2022.
- 36.Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–1398. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 37.Ford CL, Airhihenbuwa CO. Critical Race Theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(Suppl 1):S30–S35. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Strifler L, Cardoso R, McGowan J, Cogo E, Nincic V, Khan PA, et al. Scoping review identifies significant number of knowledge translation theories, models, and frameworks with limited use. J Clin Epidemiol. 2018;100:92–102. doi: 10.1016/j.jclinepi.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 39.Damschroder LJ. Clarity out of chaos: use of theory in implementation research. Psychiatry Res. 2020;283:112461. doi: 10.1016/j.psychres.2019.06.036. [DOI] [PubMed] [Google Scholar]
- 40.Kislov R, Pope C, Martin GP, Wilson PM. Harnessing the power of theorising in implementation science. Implement Sci. 2019;14(1):103. doi: 10.1186/s13012-019-0957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glasgow RE, Askew S, Purcell P, Levine E, Warner ET, Stange KC, et al. Use of RE-AIM to Address Health Inequities: application in a low-income community health center based weight loss and hypertension self-management program. Transl Behav Med. 2013;3(2):200–210. doi: 10.1007/s13142-013-0201-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eslava-Schmalbach J, Garzón-Orjuela N, Elias V, Reveiz L, Tran N, Langlois EV. Conceptual framework of equity-focused implementation research for health programs (EquIR) Int J Equity Health. 2019;18(1):80. doi: 10.1186/s12939-019-0984-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allen M, Wilhelm A, Ortega LE, Pergament S, Bates N, Cunningham B. Applying a race(ism)-conscious adaptation of the CFIR framework to understand implementation of a school-based equity-oriented intervention. Ethn Dis. 2021;31(Suppl 1):375–388. doi: 10.18865/ed.31.S1.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Etherington N, Rodrigues IB, Giangregorio L, Graham ID, Hoens AM, Kasperavicius D, et al. Applying an intersectionality lens to the theoretical domains framework: a tool for thinking about how intersecting social identities and structures of power influence behaviour. BMC Med Res Methodol. 2020;20(1):169. doi: 10.1186/s12874-020-01056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shelton RC, Chambers DA, Glasgow RE. An extension of RE-AIM to enhance sustainability: addressing dynamic context and promoting health equity over time. Frontiers. Public Health. 2020;8:134. doi: 10.3389/fpubh.2020.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Snell-Rood C, Jaramillo ET, Hamilton AB, Raskin SE, Nicosia FM, Willging C. Advancing health equity through a theoretically critical implementation science. Transl Behav Med. 2021;11(8):1617–1625. doi: 10.1093/tbm/ibab008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davison CM, Ndumbe-Eyoh S, Clement C. Critical examination of knowledge to action models and implications for promoting health equity. Int J Equity Health. 2015;14:49. doi: 10.1186/s12939-015-0178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spitzer-Shohat S, Chin MH. The “waze” of inequity reduction frameworks for organizations: a scoping review. J Gen Intern Med. 2019;34(4):604–617. doi: 10.1007/s11606-019-04829-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oh A, Abazeed A, Chambers DA. Policy implementation science to advance population health: the potential for learning health policy systems. Front Public Health. 2021;9:681602. doi: 10.3389/fpubh.2021.681602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Purtle J, Peters R, Brownson RC. A review of policy dissemination and implementation research funded by the National Institutes of Health, 2007-2014. Implement Sci. 2016;11:1. doi: 10.1186/s13012-015-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health Ment Health Serv Res. 2011;38(1):4–23. doi: 10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taplin SH, Anhang Price R, Edwards HM, Foster MK, Breslau ES, Chollette V, et al. Introduction: understanding and influencing multilevel factors across the cancer care continuum. J Natl Cancer Inst Monogr. 2012;2012(44):2–10. doi: 10.1093/jncimonographs/lgs008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Whitbeck LB, Adams GW, Hoyt DR, Chen X. Conceptualizing and measuring historical trauma among American Indian people. Am J Community Psychol. 2004;33(3-4):119–130. doi: 10.1023/B:AJCP.0000027000.77357.31. [DOI] [PubMed] [Google Scholar]
- 55.Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2016;11:33. doi: 10.1186/s13012-016-0398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189. doi: 10.1186/s12913-019-4015-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hoagwood KE, Purtle J, Spandorfer J, Peth-Pierce R, Horwitz SM. Aligning dissemination and implementation science with health policies to improve children's mental health. Am Psychol. 2020;75(8):1130–1145. doi: 10.1037/amp0000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, et al. Enhancing the impact of implementation strategies in healthcare: a research agenda. Front Public Health. 2019;7:3. doi: 10.3389/fpubh.2019.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lewis CC, Boyd MR, Walsh-Bailey C, Lyon AR, Beidas R, Mittman B, et al. A systematic review of empirical studies examining mechanisms of implementation in health. Implement Sci. 2020;15(1):21. doi: 10.1186/s13012-020-00983-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Squires JE, Graham ID, Hutchinson AM, Michie S, Francis JJ, Sales A, et al. Identifying the domains of context important to implementation science: a study protocol. Implement Sci. 2015;10(1):135. doi: 10.1186/s13012-015-0325-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Parker M, Wallerstein N, Duran B, Magarati M, Burgess E, Sanchez-Youngman S, et al. Engage for equity: development of community-based participatory research tools. Health Educ Behav. 2020;47(3):359–371. doi: 10.1177/1090198120921188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(S1):S40–SS6. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–323. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 65.Gurewich D, Garg A, Kressin NR. Addressing social determinants of health within healthcare delivery systems: a framework to ground and inform health outcomes. J Gen Intern Med. 2020. 10.1007/s11606-020-05720-6. [DOI] [PMC free article] [PubMed]
- 66.Ford CL, Griffith DM, Bruce MA, Gilbert KL. Racism: science & tools for the public health professional. Washington, DC: American Public Health Association; 2019. [Google Scholar]
- 67.Cabassa LJ, Baumann AA. A two-way street: bridging implementation science and cultural adaptations of mental health treatments. Implement Sci. 2013;8:90. doi: 10.1186/1748-5908-8-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ramanadhan S, Davis MM, Armstrong R, Baquero B, Ko LK, Leng JC, et al. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control. 2018;29(3):363–369. doi: 10.1007/s10552-018-1008-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.NCI . Resources for stakeholder and community engagement. 2021. [Google Scholar]
- 70.Pinto RM, Park S, Miles R, Ong PN. Community engagement in dissemination and implementation models: a narrative review. Implement Res Pract. 2021;2:2633489520985305. doi: 10.1177/2633489520985305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wallerstein N, Duran B, Oetzel J, Minkler M, editors. Community-based participatory research for health: advancing social and health equity. 3. San Francisco: Jossey-Bass; 2018. [Google Scholar]
- 72.Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, et al. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100(11):2094–2102. doi: 10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wallerstein N, Belone L, Burgess E, Dickson E, Gibbs L, Parajon LC, Silver G. Community based participatory research: embracing praxis for transformation. International SAGE handbook for participatory research. Thousand Oaks: Sage. In press.
- 74.Lett E, Adekunle D, McMurray P, Asabor EN, Irie W, Simon MA, et al. Health equity tourism: ravaging the justice landscape. J Med Syst. 2022;46(3):17. doi: 10.1007/s10916-022-01803-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ramanadhan S, Aronstein D, Martinez-Dominguez V, Xuan Z, Viswanath K. Designing capacity-building supports to promote evidence-based programs in community-based organizations working with underserved populations. Prog Community Health Partnersh. 2020;14(2):149–160. doi: 10.1353/cpr.2020.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Metz A. Implementation brief: the potential of co-creation in implementation science. 2015. [Google Scholar]
- 77.Kerner JF, Kavanaugh-Lynch MHE, Baezconde-Garbanati L, Politis C, Prager A, Brownson RC. Doing what we know, knowing what to do: Californians Linking Action with Science for Prevention of Breast Cancer (CLASP-BC) Int J Environ Res Public Health. 2020;17(14):5050. doi: 10.3390/ijerph17145050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kerner JF, Kavanaugh-Lynch MHE, Politis C, Baezconde-Garbanati L, Prager A, Brownson RC. Californians Linking Action with Science for Prevention of Breast Cancer (CLASP-BC)-Phase 2. Int J Environ Res Public Health. 2020;17(23):8863. doi: 10.3390/ijerph17238863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Holt CL, Chambers DA. Opportunities and challenges in conducting community-engaged dissemination/implementation research. Transl Behav Med. 2017;7(3):389–392. doi: 10.1007/s13142-017-0520-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.NCI . NCI Multilevel Intervention Training Institute (MLTI) evaluation. 2021. [Google Scholar]
- 81.Fernandez ME, Ruiter RA, Markham CM, Kok G. Intervention mapping: theory-and evidence-based health promotion program planning: perspective and examples. Front Public Health. 2019;7:209. doi: 10.3389/fpubh.2019.00209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nápoles AM, Stewart AL. Transcreation: an implementation science framework for community-engaged behavioral interventions to reduce health disparities. BMC Health Serv Res. 2018;18(1):710. doi: 10.1186/s12913-018-3521-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kwan BM, Brownson RC, Glasgow RE, Morrato EH, Luke DA. Designing for dissemination and sustainability to promote equitable impacts on health. Annu Rev Public Health. 2022;43:331–353. doi: 10.1146/annurev-publhealth-052220-112457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am J Public Health. 2013;103(9):1693–1699. doi: 10.2105/AJPH.2012.301165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Knoepke CE, Pilar Ingle M, Matlock DD, Brownson RC, Glasgow RE. Dissemination and stakeholder engagement practices among dissemination & implementation scientists: results from an online survey. bioRxiv. 2019;14(11):e0216971. [DOI] [PMC free article] [PubMed]
- 86.Shea CM, Young TL, Powell BJ, Rohweder C, Enga ZK, Scott JE, et al. Researcher readiness for participating in community-engaged dissemination and implementation research: a conceptual framework of core competencies. Transl Behav Med. 2017;7(3):393–404. doi: 10.1007/s13142-017-0486-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Baumann AA, Woodward E, Singh RS, Adsul P, Shelton RS. Assessing researchers’ capabilities, opportunities, and motivation to conduct equity-oriented dissemination and implementation research, an exploratory cross-sectional study. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Boyce CA, Barfield W, Curry J, Shero S, Green Parker M, Cox H, et al. Building the next generation of implementation science careers to advance health equity. Ethn Dis. 2019;29(Suppl 1):77–82. doi: 10.18865/ed.29.S1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chinman M, Woodward EN, Curran GM, Hausmann LRM. Harnessing implementation science to increase the impact of health equity research. Med Care. 2017;55(Suppl 9 2):S16–S23. doi: 10.1097/MLR.0000000000000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McNulty M, Smith JD, Villamar J, Burnett-Zeigler I, Vermeer W, Benbow N, et al. Implementation research methodologies for achieving scientific equity and health equity. Ethn Dis. 2019;29(Suppl 1):83–92. doi: 10.18865/ed.29.S1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health. 2018;39(1):55–76. doi: 10.1146/annurev-publhealth-040617-014731. [DOI] [PubMed] [Google Scholar]
- 92.Steinka-Fry KT, Tanner-Smith EE, Dakof GA, Henderson C. Culturally sensitive substance use treatment for racial/ethnic minority youth: a meta-analytic review. J Subst Abus Treat. 2017;75:22–37. doi: 10.1016/j.jsat.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 93.Rathod S, Gega L, Degnan A, Pikard J, Khan T, Husain N, et al. The current status of culturally adapted mental health interventions: a practice-focused review of meta-analyses. Neuropsychiatr Dis Treat. 2018;14:165–178. doi: 10.2147/NDT.S138430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cultural adaptations: tools for evidence-based practice with diverse populations. Bernal G, Domenech Rodríguez MM, editors. Washington, DC: American Psychological Association; 2012. p. xix, 307-xix.
- 95.Castro FG, Barrera M, Martinez CR. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci. 2004;5(1):41–45. doi: 10.1023/B:PREV.0000013980.12412.cd. [DOI] [PubMed] [Google Scholar]
- 96.Kumpfer KL, Scheier LM, Brown J. Strategies to avoid replication failure with evidence-based prevention interventions: case examples from the strengthening families program. Eval Health Prof. 2020;43(2):75–89. doi: 10.1177/0163278718772886. [DOI] [PubMed] [Google Scholar]
- 97.Wiltsey Stirman S, Baumann AA, Miller CJ. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci. 2019;14(1):58. doi: 10.1186/s13012-019-0898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Escoffery C, Lebow-Skelley E, Udelson H, Böing EA, Wood R, Fernandez ME, et al. A scoping study of frameworks for adapting public health evidence-based interventions. Transl Behav Med. 2018;9(1):1–10. doi: 10.1093/tbm/ibx067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8(1):139. doi: 10.1186/1748-5908-8-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. 2019;7:158. doi: 10.3389/fpubh.2019.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lewis CC, Hannon PA, Klasnja P, Baldwin LM, Hawkes R, Blackmer J, et al. Optimizing Implementation in Cancer Control (OPTICC): protocol for an implementation science center. Implement Sci Commun. 2021;2(1):44. doi: 10.1186/s43058-021-00117-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Oh A, Vinson CA, Chambers DA. Future directions for implementation science at the National Cancer Institute: Implementation Science Centers in Cancer Control. Transl Behav Med. 2021;11(2):669–675. doi: 10.1093/tbm/ibaa018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.NIH. NOT-OD-21-066 Request for Information (RFI): inviting comments and suggestions to advance and strengthen racial equity, diversity, and inclusion in the biomedical research workforce and advance health disparities and health equity research. 2021. Available from: https://grants.nih.gov/grants/guide/notice-files/NOT-OD-21-066.html.
- 105.NCI. NOT-CA-21-066 Request for Information (RFI): seeking stakeholder input on enhancing cancer health disparities research. 2021. Available from: https://grants.nih.gov/grants/guide/notice-files/NOT-CA-21-066.html.
- 106.Gase LN, Schooley T, Lee M, Rotakhina S, Vick J, Caplan J. A practice-grounded approach for evaluating health in all policies initiatives in the United States. J Public Health Manag Pract. 2017;23(4):339–347. doi: 10.1097/PHH.0000000000000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gase LN, Pennotti R, Smith KD. “Health in All Policies”: taking stock of emerging practices to incorporate health in decision making in the United States. J Public Health Manag Pract. 2013;19(6):529–540. doi: 10.1097/PHH.0b013e3182980c6e. [DOI] [PubMed] [Google Scholar]
- 108.Salunke S, Lal DK. Multisectoral approach for promoting public health. Indian J Public Health. 2017;61(3):163–168. doi: 10.4103/ijph.IJPH_220_17. [DOI] [PubMed] [Google Scholar]
- 109.Remiker M, Sabo S, Jiménez D, Samarron Longorio A, Chief C, Williamson H, et al. Using a multisectoral approach to advance health equity in rural Arizona: community-engaged survey development and implementation study. JMIR Form Res. 2021;5(5):e25577. doi: 10.2196/25577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Oetzel J, Scott N, Hudson M, Masters-Awatere B, Rarere M, Foote J, et al. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Glob Health. 2017;13(1):69. doi: 10.1186/s12992-017-0295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Means AR, Kemp CG, Gwayi-Chore M-C, Gimbel S, Soi C, Sherr K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low-and middle-income countries: a systematic review. Implement Sci. 2020;15(1):1–19. doi: 10.1186/s13012-020-0977-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Paskett ED, Hiatt RA. Catchment areas and community outreach and engagement: the new mandate for NCI-designated cancer centers. Cancer Epidemiol Biomark Prev. 2018;27(5):517–519. doi: 10.1158/1055-9965.EPI-17-1050. [DOI] [PubMed] [Google Scholar]
- 113.Mensah GA, Cooper RS, Siega-Riz AM, Cooper LA, Smith JD, Brown CH, et al. Reducing cardiovascular disparities through community-engaged implementation research: a National Heart, Lung, and Blood Institute Workshop Report. Circ Res. 2018;122(2):213–230. doi: 10.1161/CIRCRESAHA.117.312243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sterling MR, Echeverría SE, Commodore-Mensah Y, Breland JY, Nunez-Smith M. Health equity and implementation science in heart, lung, blood, and sleep-related research. Circ Cardiovasc Qual Outcomes. 2019;12(10):e005586. doi: 10.1161/CIRCOUTCOMES.119.005586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roberts MC, Mensah GA, Khoury MJ. Leveraging implementation science to address health disparities in genomic medicine: examples from the field. Ethn Dis. 2019;29(Suppl 1):187–192. doi: 10.18865/ed.29.S1.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Alcaraz KI, Sly J, Ashing K, Fleisher L, Gil-Rivas V, Ford S, et al. The ConNECT Framework: a model for advancing behavioral medicine science and practice to foster health equity. J Behav Med. 2017;40(1):23–38. doi: 10.1007/s10865-016-9780-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.White A, Sabatino SA, Vinson C, Chambers D, White MC. The Cancer Prevention and Control Research Network (CPCRN): advancing public health and implementation science. Prev Med. 2019;129s:105824. doi: 10.1016/j.ypmed.2019.105824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mainor AG, Decosimo K, Escoffrey C, Farris P, Shannon J, Winters-Stone K, et al. Scaling up and tailoring the “Putting Public Health in Action” Training Curriculum. Health Promot Pract. 2018;19(5):664–672. doi: 10.1177/1524839917741486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Taplin SH, Yabroff KR, Zapka J. A multilevel research perspective on cancer care delivery: the example of follow-up to an abnormal mammogram. Cancer Epidemiol Biomark Prev. 2012;21(10):1709–1715. doi: 10.1158/1055-9965.EPI-12-0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ (Clinical research ed) 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wolfenden L, Chai LK, Jones J, McFadyen T, Hodder R, Kingsland M, et al. What happens once a program has been implemented? A call for research investigating strategies to enhance public health program sustainability. Aust N Z J Public Health. 2019;43(1):3–4. doi: 10.1111/1753-6405.12867. [DOI] [PubMed] [Google Scholar]
- 122.Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8(1):117. doi: 10.1186/1748-5908-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Norton WE, Zwarenstein M, Czajkowski S, Kato E, O'Mara A, Shelburne N, et al. Building internal capacity in pragmatic trials: a workshop for program scientists at the US National Cancer Institute. Trials. 2019;20(1):779. doi: 10.1186/s13063-019-3934-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aarons GA, Sklar M, Mustanski B, Benbow N, Brown CH. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implement Sci. 2017;12(1):111. doi: 10.1186/s13012-017-0640-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tuzzio L, Larson EB, Chambers DA, Coronado GD, Curtis LH, Weber WJ, et al. Pragmatic clinical trials offer unique opportunities for disseminating, implementing, and sustaining evidence-based practices into clinical care: proceedings of a workshop. Healthcare (Amsterdam, Netherlands) 2019;7(1):51–57. doi: 10.1016/j.hjdsi.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hawe P. Lessons from complex interventions to improve health. Annu Rev Public Health. 2015;36:307–323. doi: 10.1146/annurev-publhealth-031912-114421. [DOI] [PubMed] [Google Scholar]
- 127.Williams DR, Cooper LA. COVID-19 and health equity-a new kind of “herd immunity”. JAMA. 2020;323(24):2478–2480. doi: 10.1001/jama.2020.8051. [DOI] [PubMed] [Google Scholar]
- 128.Galaviz KI, Breland JY, Sanders M, Breathett K, Cerezo A, Gil O, et al. Implementation science to address health disparities during the coronavirus pandemic. Health Equity. 2020;4(1):463–467. doi: 10.1089/heq.2020.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yancey AT, Glenn BA, Ford CL, Bell-Lewis L. Dissemination and implementation research in health: translating science to practice. 2017. Dissemination and implementation research among racial/ethnic minority and other vulnerable populations; pp. 449–470. [Google Scholar]
- 130.Ford CL, Griffith DM, Bruce MA, Gilbert KL. 1. Introduction. Racism: science & tools for the public health professional. APHA Press; 2019. 10.2105/9780875533049.
- 131.Yousefi Nooraie R, Shelton RC, Fiscella K, Kwan BM, McMahon JM. The pragmatic, rapid, and iterative dissemination and implementation (PRIDI) cycle: adapting to the dynamic nature of public health emergencies (and beyond) Health Res Policy Syst. 2021;19(1):110. doi: 10.1186/s12961-021-00764-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Neta G, Glasgow RE, Carpenter CR, Grimshaw JM, Rabin BA, Fernandez ME, et al. A framework for enhancing the value of research for dissemination and implementation. Am J Public Health. 2014;105(1):49–57. doi: 10.2105/AJPH.2014.302206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Admin Pol Ment Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All meeting reports from the 2019 and 2020 Consortium for Cancer Implementation Science (previously known as the Implementation Science Consortium in Cancer) are available at: https://cancercontrol.cancer.gov/is/initiatives/iscc