Abstract
Objectives
To describe pediatric mental health emergency department (ED) visit rates and visit characteristics before and during the COVID-19 pandemic.
Methods
We conducted a cross-sectional study of ED visits by children 5–17 years old with a primary mental health diagnosis from March 2018 to February 2021 at a 10-hospital health system and a children's hospital in the Chicago area. We compared demographic and clinical characteristics of children with mental health ED visits before and during the pandemic. We conducted an interrupted time series analysis to determine changes in visit rates.
Results
We identified 8,127 pediatric mental health ED visits (58.5% female, 54.3% White, Not Hispanic/Latino and 42.4% age 13–15). During the pandemic, visits for suicide or self-injury increased 6.69% (95% CI 4.73, 8.65), and visits for disruptive, impulse control, conduct disorders increased 1.94% (95% CI 0.85, 3.03). Mental health ED visits by children with existing mental health diagnoses increased 2.29% (95% CI 0.34, 4.25). Mental health ED visits that resulted in medical admission increased 4.32% (95% CI 3.11, 5.53). The proportion of mental health ED visits at community hospitals increased by 5.49% (95% CI 3.31, 7.67). Mental health ED visit rates increased at the onset of the pandemic (adjusted incidence rate ratio [aIRR] 1.27, 95% CI 1.06, 1.50), followed by a monthly increase thereafter (aIRR 1.04, 95% CI 1.02, 1.06).
Conclusion
Mental health ED visit rates by children increased during the COVID-19 pandemic. Changes in mental health ED visit characteristics during the pandemic may inform interventions to improve children's mental health.
Keywords: adolescent, child, COVID-19, emergency service, hospital, mental health
What's New.
At a Chicago area health system and an academic children's hospital, we found increased ED visit rates for mental health conditions by children during the COVID-19 pandemic, including increased visits for suicide/self-injury and disruptive behaviors, and higher admission rates.
Alt-text: Unlabelled box
The Coronavirus Disease 2019 (COVID-19) pandemic led to a combination of physical, psychological, and economic stressors that adversely impacted the mental health of children and adolescents.1 Due to multiple factors including social isolation, the transition to virtual schooling, and difficulty accessing usual sources of care, symptoms of depression and anxiety among children have increased.1, 2, 3, 4 When mental health symptoms reach the point of crisis, children may seek care in the emergency department (ED). Centers for Disease Control and Prevention (CDC) National Syndromic Surveillance Program data indicate that pediatric mental health ED visit rates increased from early April to mid-October 2020.5 During the pandemic, ED visits for suicide attempts among female adolescents increased, and one center reported higher admission rates after mental health ED visits.6 , 7 However, the impact of the pandemic on pediatric mental health ED utilization has yet to be fully understood.
Importantly, national CDC surveillance data did not provide information about the race and ethnicity or socioeconomic status of children visiting the ED for mental health reasons.5 As both the medical and economic consequences of COVID-19 have been disproportionately felt by communities of color, and by those with lower incomes, clarification of mental health-related outcomes within these subpopulations is requisite.8 Recent publications on ED mental health visits mainly focus on children's hospitals, yet the majority of children in the US present to community hospitals for emergency care.9 , 10 Data from community hospital settings are needed.
Therefore, we aimed to describe changes in pediatric mental health ED visit rates before and during the COVID-19 pandemic in Chicago area EDs. Additionally, we sought to determine differences in demographic and clinical characteristics among children with mental health ED visits before and during the pandemic. We hypothesized that mental health visit rates increased, and that a higher proportion of pediatric mental health visits resulted in admission.
Methods
Study Design and Setting
We conducted a cross-sectional study of mental health ED visits by children age 5–17 from March 2018 to March 2021 at a 10-hospital academic medical system (1 academic medical hospital and 9 community hospitals) and an independent children's hospital in the Chicago area. The academic medical system has one ED that cares for children in a separate location staffed by pediatric emergency medicine physicians for 12 hours per day, while the other EDs see children and adults in the same space and are staffed by general emergency medicine physicians. We included data starting from March 2018 to allow for rigorous establishment of a baseline trajectory and seasonal variation prior to the onset of the pandemic.11 This study was deemed exempt by the IRB at Ann and Robert H. Lurie Children's Hospital of Chicago.
Study Population
We defined pediatric mental health ED visits as those with a primary International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code in the previously validated Child and Adolescent Mental Health Disorders Classification Scheme (CAMHD-CS).12 While the classification scheme consists of 30 mental health diagnosis groups, we included 15 CAMHD-CS diagnosis groups representative of mental health conditions that are common reasons for ED visits and hospitalizations among children (Table S1).13 , 14 We chose to include the mental health diagnosis group titled “Miscellaneous”12 as it contained relevant ICD-10-CM codes such as “other emotional disturbances of childhood,” “persistent mood disorder, unspecified,” and “mental disorder not otherwise specified.”
Measures
The primary outcome was the ED visit rate for mental health conditions. The primary independent variable was the visit time period (pre-pandemic versus post-pandemic) with March 1, 2020 used to define pandemic onset.15
We compared ED mental health visits before and during the pandemic with respect to age group (5–8, 9–12, 13–15, or 16–17 years old), sex, self-identified race and ethnicity (Asian, Not-Hispanic/Latino; Black, Not-Hispanic/Latino; White, Hispanic/Latino; White, Not-Hispanic/Latino; other race, Hispanic/Latino, other/unknown), preferred language (English, Spanish, other), socioeconomic status, mental health diagnosis group, prior mental health diagnosis, behavioral health consultation, and disposition. We defined socioeconomic status based on insurance classified as private (commercial, managed care, Tri-care); public (Medicaid, Medicaid Replacement, Medicare); and other/uninsured (self-pay, worker compensation) and metropolitan area-normed Child Opportunity Index (COI) 2.0 based on the patient's zip code (classified as very low, low, moderate, high, or very high).16 The COI provides a composite measure of neighborhood-level resources and conditions affecting the health of children, including education, health and environment, and social and economic factors.16 Mental health diagnosis group was determined by the CAMHD-CS classification scheme for ICD-10-CM diagnosis codes.12 We reported findings individually for 11 CAMHD-CS diagnosis groups and combined 4 of the lower frequency groups as “other” mental health diagnoses. We identified mental health diagnoses in the electronic medical record within the previous 5 years. Disposition categories included home, inpatient psychiatric admission, medical admission (general medical unit admission or critical care/intermediate care admission), and other (left without being seen, against medical advice, or deceased).
Statistical Analysis
Descriptive statistics summarized the frequencies and percentages of the patient demographic and clinical characteristics associated with the pediatric ED mental health visits. The association of visit characteristics with pandemic status was examined using chi-square tests of independence or Fisher's exact tests (for expected cell counts below 5). Additionally, chi-square tests for homogeneity of proportions were conducted to test for differences in the proportions of the characteristics before versus during the pandemic.
We used segmented regression analysis for interrupted time series data to evaluate the pandemic effect on pediatric mental health ED visits. Due to overdispersion in pediatric mental health ED visits, negative binomial distribution with a log link for count data was assumed. An offset term of the ED pediatric visit count during the study period was included to model the rate. Given seasonal variation in mental health ED visits, the negative binomial regression model was adjusted for seasonality using Fourier terms consisting of two sine/cosine pairs.11 Presence of autocorrelation in the residuals was assessed using Durbin-Watson test before and after adjusting for seasonality. After adjusting for seasonality, the null hypothesis of no evidence of autocorrelation was not rejected (Durbin-Watson = 2.0, P = .10). Statistical significance was evaluated via a 2-sided type I error rate of 0.05. All statistical analyses were conducted using R version 4.1.0 within RStudio version 1.4.1717.
Results
During the study period, there were 8,127 mental health ED visits by children 5-17 years old. Children were 58.5% female, 54.3% White, Non-Hispanic/Latino, and 42.4% age 13–15 (Table ). There were 5278 visits (64.9%) in the 2 years prior to the COVID-19 pandemic (March 2018–February 2020) and 2849 visits (35.0%) during the year after pandemic onset (March 2020–February 2021). No statistically significant differences in sex, age, preferred language, or insurance were detected between prepandemic and pandemic time periods.
Table.
Characteristics of Emergency Department Visits by Children for Mental Health Conditions, Before and During the COVID-19 Pandemic
| ED Visit Characteristic | Total ED Visits (N = 8127)* | ED Visits Prepandemic, Mar 2018–Feb 2020 (N = 5278)* | ED Visits During the Pandemic Mar 2020–Feb 2021, (N = 2849)* | Pandemic–Prepandemic Risk Difference (95% CI) |
|---|---|---|---|---|
| Sex | ||||
| Female | 4754 (58.5%) | 3048 (57.7%) | 1706 (59.9%) | 2.15 (−0.09, 4.39) |
| Male | 3372 (41.5%) | 2230 (42.3%) | 1142 (40.1%) | −2.15 (−4.39, 0.09) |
| Age Group | ||||
| 5-8 years | 399 (4.9%) | 255 (4.8%) | 144 (5.1%) | 0.22 (−0.77, 1.21) |
| 9-12 years | 1577 (19.4%) | 1027 (19.5%) | 550 (19.3%) | −0.15 (−1.95, 1.65) |
| 13-15 years | 3445 (42.4%) | 2209 (41.9%) | 1236 (43.4%) | 1.53 (−0.72, 3.79) |
| 16-17 years | 2706 (33.3%) | 1787 (33.9%) | 919 (32.3%) | −1.60 (−3.74, 0.54) |
| Race and Ethnicity | ||||
| Asian, Not-Hispanic/Latino | 258 (3.2%) | 176 (3.3%) | 82 (2.9%) | −0.46 (−1.24, 0.33) |
| Black, Not-Hispanic/Latino | 1069 (13.2%) | 716 (13.6%) | 353 (12.4%) | −1.18 (−2.7, 0.35) |
| White, Hispanic/Latino | 883 (10.9%) | 621 (11.8%) | 262 (9.2%) | −2.57 (−3.94, −1.20) |
| White, Not-Hispanic/Latino | 4413 (54.3%) | 2834 (53.7%) | 1579 (55.4%) | 1.73 (−0.54, 4.0) |
| Other Race, Hispanic/Latino | 1138 (14.0%) | 720 (13.6%) | 418 (14.7%) | 1.03 (−0.57, 2.63) |
| Other /Unknown | 366 (4.5%) | 211 (4.0%) | 155 (5.4%) | 1.44 (0.46, 2.43) |
| Preferred Language | ||||
| English | 7544 (92.8%) | 4898 (92.8%) | 2646 (92.9%) | 0.07 (−1.10, 1.25) |
| Spanish | 535 (6.6%) | 349 (6.6%) | 186 (6.5%) | −0.08 (−1.21, 1.04) |
| Other | 48 (0.6%) | 31 (0.6%) | 17 (0.6%) | 0.01 (−0.34, 0.36) |
| Insurance | ||||
| Private | 4538 (55.8%) | 2976 (56.4%) | 1562 (54.8%) | −1.56 (−3.82, 0.71) |
| Public | 3,488 (42.9%) | 2238 (42.4%) | 1250 (43.9%) | 1.47 (−0.79, 3.73) |
| Other/Uninsured | 101 (1.2%) | 64 (1.2%) | 37 (1.3%) | 0.09 (−0.42, 0.60) |
| Child Opportunity Index | ||||
| Very Low | 824 (10.5%) | 574 (11.3%) | 250 (9.0%) | −2.25 (−3.63, −0.88) |
| Low | 1258 (16.0%) | 834 (16.4%) | 424 (15.3%) | −1.08 (−2.76, 0.60) |
| Moderate | 1584 (20.1%) | 960 (18.8%) | 624 (22.5%) | 3.66 (1.77, 5.54) |
| High | 1978 (25.1%) | 1221 (24.0%) | 757 (27.3%) | 3.33 (1.30, 5.36) |
| Very High | 2226 (28.3%) | 1507 (29.6%) | 719 (25.9%) | −3.65 (−5.71, −1.60) |
| Mental Health Group | ||||
| Accidental or Undetermined Poisoning | 32 (0.4%) | 17 (0.3%) | 15 (0.5%) | 0.20 (−0.10, 0.51) |
| Anxiety Disorders | 1228 (15.1%) | 856 (16.2%) | 372 (13.1%) | −3.16 (−4.75, −1.57) |
| Bipolar and Related Disorders | 120 (1.5%) | 72 (1.4%) | 48 (1.7%) | 0.32 (−0.25, 0.89) |
| Depressive Disorders | 2563 (31.5%) | 1734 (32.9%) | 829 (29.1%) | −3.76 (−5.85, −1.66) |
| Disruptive, Impulse Control and Conduct Disorders | 451 (5.5%) | 257 (4.9%) | 194 (6.8%) | 1.94 (0.85, 3.03) |
| Mental Health Symptom | 592 (7.3%) | 373 (7.1%) | 219 (7.7%) | 0.62 (−0.58, 1.82) |
| Miscellaneous | 207 (2.5%) | 140 (2.7%) | 67 (2.4%) | −0.30 (−1.01, 0.40) |
| Schizophrenia Spectrum and Other Psychotic Disorders | 133 (1.6%) | 92 (1.7%) | 41 (1.4%) | −0.30 (−0.87, 0.26) |
| Substance-Related and Addictive Disorders | 500 (6.2%) | 339 (6.4%) | 161 (5.7%) | −0.77 (−1.85, 0.30) |
| Suicide or Self-Injury | 1849 (22.8%) | 1077 (20.4%) | 772 (27.1%) | 6.69 (4.73, 8.65) |
| Trauma and Stressor-Related Disorders | 346 (4.3%) | 236 (4.5%) | 110 (3.9%) | −0.61 (−1.51, 0.29) |
| Other Disorders (Dissociative, Obsessive-Compulsive, Somatic, Sleep-Wake) | 106 (1.3%) | 85 (1.6%) | 21 (0.7%) | −0.87 (−1.34, −0.41) |
| Prior Mental Health Diagnosis | ||||
| No | 6197 (76.3%) | 4067 (77.1%) | 2130 (74.8%) | −2.29 (−4.25, −0.34) |
| Yes | 1930 (23.7%) | 1211 (22.9%) | 719 (25.2%) | 2.29 (0.34, 4.25) |
| Behavioral Health Consult | ||||
| No | 3337 (41.1%) | 2236 (42.4%) | 1101 (38.6%) | −3.72 (−5.95, −1.49) |
| Yes | 4790 (58.9%) | 3042 (57.6%) | 1748 (61.4%) | 3.72 (1.49, 5.95) |
| Hospital Type | ||||
| Community Hospital | 5073 (62.4%) | 3193 (60.5%) | 1880 (66.0%) | 5.49 (3.31, 7.67) |
| Academic Medical | 132 (1.6%) | 105 (2.0%) | 27 (0.9%) | −1.04 (−1.56, −0.52) |
| Children's Hospital | 2922 (36.0%) | 1980 (37.5%) | 942 (33.1%) | −4.45 (−6.62, −2.28) |
| Disposition from ED | ||||
| Home | 4568 (57.8%) | 3061 (59.8%) | 1507 (54.0%) | −5.81 (−8.10, −3.53) |
| Psychiatric Admission | 2843 (35.9%) | 1813 (35.4%) | 1030 (36.9%) | 1.48 (−0.74, 3.70) |
| Medical Admission | 490 (6.2%) | 239 (4.7%) | 251 (9.0%) | 4.32 (3.11, 5.53) |
| General Medical Unit | 388 (4.8%) | 178 (3.4%) | 210 (7.4%) | 4.05 (2.95, 5.15) |
| Critical Care/ Intermediate Care Unit | 102 (1.3%) | 61 (1.2%) | 41 (1.4%) | 0.28 (−0.26, 0.81) |
| Other† | 8 (0.1%) | 5 (0.1%) | 3 (0.1%) | 0.01 (−0.14, 0.16) |
n (%); proportions estimated based on non-missing data.
Left Without Being Seen, Against Medical Advice, Deceased.
Pediatric mental health ED visits for White, Hispanic/Latino children decreased by 2.57% (95% CI −3.94, −1.20) and visits by children of other/unknown race and ethnicity increased by 1.44% (95% CI 0.46, 2.43). ED visits by children from very low and very high COI areas decreased by 2.25% (95% CI −3.63, −0.88) and 3.65% (95% CI −5.71, −1.60) respectively, while those from moderate and high COI areas increased by 3.66% (95% CI 1.77, 5.54) and 3.33% (95% CI 1.30, 5.36) respectively.
ED visits for suicide or self-injury increased from 20.4% of all mental health visits in the prepandemic period to 27.1% in the pandemic period (an increase by 6.69%; 95% CI 4.73, 8.65). Fewer visits occurred for depressive disorders (−3.76%; 95% CI −5.85, -1.66) and anxiety (−3.16%, 95% CI −4.75, −1.57), while visits for disruptive, impulse control, and conduct disorders increased by 1.94% (95% CI 0.85, 3.03).
During the pandemic, significantly more visits had a prior mental health diagnosis in the past 5 years (an increase of 2.29%; 95% CI 0.34, 4.25). More visits had behavioral health consultation during the pandemic (an increase of 3.72%; 95% CI 1.49, 5.95). Additionally, visits with a disposition of discharge to home decreased by 5.81% (95% CI −8.10, −3.53). More visits resulted in medical admission (4.7% prepandemic vs 9.0% pandemic; 4.32% increase; 95% CI 3.11, 5.53) and general medical unit (noncritical care) admissions (prepandemic 3.4% vs pandemic 7.4%, 4.05% increase; 95% CI 2.95, 5.15). Finally, ED visits at community hospitals increased, relative to those at the academic medical hospital or children's hospital (60.5% pre-pandemic vs 66.0% pandemic, 5.49% increase; 95% CI 3.31,7.67).
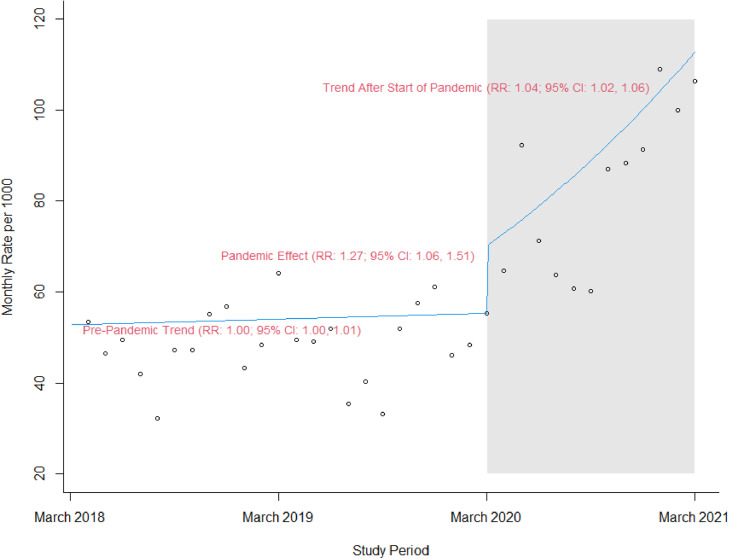
The interrupted time series analysis (Figure ) demonstrated a 27% increase (adjusted incidence rate ratio [aIRR] 1.27, 95% CI 1.06, 1.51) in the pediatric mental health ED visit rate at the onset of the pandemic in March 2020, after adjusting for seasonality. This was followed by a 4% monthly increase in the pediatric mental health ED visit rate through February 2021 (aIRR 1.04, 95% CI 1.02, 1.06).
Figure.
Emergency Department Visit Rate by Children for Mental Health Conditions, March 2018–March 2021. Seasonally adjusted emergency department visit rate by children for mental health conditions from March 2018 to March 2021. Circles represent observed monthly rates. The gray shaded region represents the pandemic period (March 2020–February 2021). The solid line is the deseasonalized trend of modeled rates fitted to data.
Discussion
In Chicago area EDs, we found pediatric mental health ED visits increased 27% at the onset of the COVID-19 pandemic, followed by a 4% increase monthly through February 2021. We noted changes in mental health ED visits during the pandemic in terms of socioeconomic status, mental health diagnosis groups, prior mental health ED visits, behavioral health consultation, disposition, and the proportion of visits at community versus children's hospitals.
Our study provides important information on the pandemic's impact on the distribution of mental health diagnoses for pediatric ED mental health visits. During the pandemic, we found fewer visits for depression and anxiety and more visits for suicide or self-injury. While a meta-analysis described higher depressive and anxiety symptoms among children during the pandemic, our findings suggest that emergency care is increasingly reserved for more severe cases of mood disorders involving risk of self-harm.3 Our findings are consistent with national CDC surveillance data demonstrating rising ED visits by youth for suicide attempts since the onset of the pandemic, particularly among adolescent females.6 We found a significant increase in disruptive, impulse control, conduct disorders, which may have worsened because of inability to access outpatient services or because of psychosocial stressors imposed by the pandemic.1 We found more pediatric mental health ED visits resulted in admission during the pandemic. Another study reported increased admission rates following pediatric ED mental health visits during the pandemic,7 but we additionally found more admissions to general medical units versus critical care/intermediate care.
Differences in pediatric mental health ED visits by neighborhood resources and conditions and race and ethnicity during the pandemic have important health equity implications. A single-center study found that mental health ED visits decreased during the pandemic among Black youth compared to White youth.17 In contrast, we did not find differences in ED visit rates by Black race, but we did find a decrease in ED visits by White, Hispanic/Latino children and an increase in visits of children with other or unknown race and ethnicity, which is difficult to interpret due to the group's heterogeneity. We found increased mental health ED visits during the pandemic by children from moderate and high COI areas and decreased visits by children from very low and very high COI areas. Another study found increased mental health ED visit rates during the pandemic by children with commercial insurance,7 which typically correlates with higher socioeconomic status. In contrast, we did not find differences in ED visit rates by insurance type. Despite disproportionate medical and economic impacts of the pandemic on low-income families and families of color,8 pediatric mental health ED visits do not appear to follow the same pattern.
Our study is unique in its examination of trends in pediatric mental health ED visits at community hospitals. We observed a relative increase in the proportion of children presenting to community hospitals compared to a children's hospital and academic medical ED during the pandemic. Given that most pediatric emergency care occurs at non-children's hospitals18 and the declaration of a national emergency in pediatric mental health by the American Academy of Pediatrics,19 all EDs should be equipped with adequate resources, policies, and staff training to manage pediatric mental health needs.20
The pandemic has fueled acceleration of the pediatric mental health crisis, and opportunities to strengthen mental health infrastructure must be explored. Increasing the availability of acute mental health services for children, such as psychiatric urgent care centers and crisis behavioral health teams, may help to reduce pediatric mental health ED visits.21 , 22 Recruitment and retention of mental health professionals should be supported through workforce development programs such as loan repayment programs.22 Tele mental health services may also represent a promising avenue to improve access to care.23 Mental health services must be embedded in schools, primary care clinics, and communities to promote prevention and early identification of mental health needs.24 Upstream prevention should aim to reduce adverse childhood experiences and address social determinants of health.22
Our study was limited to EDs in one metropolitan area; thus, these results may not be generalizable across the country. Also, visits were identified via diagnosis codes, which may be subject to some misclassification. For smaller subgroups, such as ED visits for less common mental health diagnosis groups, the study sample size may have been too small to detect statistical differences, even if true differences existed before versus during the pandemic.
In conclusion, pediatric mental health ED visit rates increased at the onset of the COVID-19 pandemic and continued to increase monthly thereafter. An understanding of changes in demographic and clinical characteristics of pediatric ED mental health visits during the pandemic may provide targeted opportunities to address the mental health needs of specific populations of children.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article to disclose.
Acknowledgments
Acknowledgment
This work was supported by the U.S. Agency for Healthcare Research and Quality (grant number 5K12HS026385-03). Funders/sponsors did not participate in the work.
Funding/Support
Dr. Hoffmann receives support from the U.S. Agency for Healthcare Research and Quality (grant number 5K12HS026385-03). Funders/sponsors did not participate in the work.
Footnotes
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.acap.2022.05.022.
Appendix. Supplementary Data
References
- 1.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 2.Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Racine N, McArthur BA, Cooke JE, et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis: a meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verlenden JV, Pampati S, Rasberry CN, et al. Association of children's mode of school instruction with child and parent experiences and well-being during the COVID-19 pandemic — COVID experiences survey, United States, October 8–November 13, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:369–376. doi: 10.15585/mmwr.mm7011a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic - United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675–1680. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yard E, Radhakrishnan L, Ballesteros MF, et al. Emergency department visits for suspected suicide attempts among persons aged 12-25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 2021;70:888–894. doi: 10.15585/mmwr.mm7024e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krass P, Dalton E, Doupnik SK, et al. US pediatric emergency department visits for mental health conditions during the COVID-19 pandemic. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.8533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen CY-C, Byrne E, Vélez T. Impact of the 2020 pandemic of COVID-19 on families with school-aged children in the United States: roles of income level and race. J Fam Issues. 2021;43:719–740. doi: 10.1177/0192513X21994153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaiyachati BH, Agawu A, Zorc JJ, et al. Trends in pediatric emergency department utilization after institution of Coronavirus disease-19 mandatory social distancing. J Pediatr. 2020;226:274–277.e1. doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gausche-Hill M, Schmitz C, Lewis RJ. Pediatric preparedness of US emergency departments: a 2003 survey. Pediatrics. 2007;120:1229–1237. doi: 10.1542/peds.2006-3780. [DOI] [PubMed] [Google Scholar]
- 11.Marshall R, Ribbers A, Sheridan D, et al. Mental health diagnoses and seasonal trends at a pediatric emergency department and hospital, 2015-2019. Hosp Pediatr. 2021;11(3):199–206. doi: 10.1542/hpeds.2020-000653. [DOI] [PubMed] [Google Scholar]
- 12.Zima BT, Gay JC, Rodean J, et al. Classification system for international classification of diseases, ninth revision, clinical modification and tenth revision pediatric mental health disorders. JAMA Pediatr. 2020;174:620–622. doi: 10.1001/jamapediatrics.2020.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133:602–609. doi: 10.1542/peds.2013-3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cutler GJ, Rodean J, Zima BT, et al. Trends in pediatric emergency department visits for mental health conditions and disposition by presence of a psychiatric unit. Acad Pediatr. 2019;19:948–955. doi: 10.1016/j.acap.2019.05.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO director-general's opening remarks at the media briefing on COVID-19 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–11-march-2020; Accessed August 16, 2020.
- 16.Noelke C, McArdle N, Baek M, et al. Child Opportunity Index 2.0 Technical Documentation. https://www.diversitydatakids.org/sites/default/files/2020-02/ddk_coi2.0_technical_documentation_20200212.pdf; Accessed March 3, 2022.
- 17.Leff RA, Setzer E, Cicero MX, et al. Changes in pediatric emergency department visits for mental health during the COVID-19 pandemic: a cross-sectional study. Clin Child Psychol Psychiatry. 2021;26:33–38. doi: 10.1177/1359104520972453. [DOI] [PubMed] [Google Scholar]
- 18.Remick K, Gausche-Hill M, Joseph MM, et al. Pediatric readiness in the emergency department. Ann Emerg Med. 2018;72:e123–e136. doi: 10.1016/j.annemergmed.2018.08.431. [DOI] [PubMed] [Google Scholar]
- 19.AAP, AACAP, CHA declare national emergency in children's mental health. https://www.aappublications.org/news/2021/10/19/children-mental-health-national-emergency-101921; Accessed October 23, 2021 2021.
- 20.Cree RA, So M, Franks J, et al. Characteristics associated with presence of pediatric mental health care policies in emergency departments. Pediatr Emerg Care. 2019 doi: 10.1097/PEC.0000000000001920. Published Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services . U.S. Department of Health and Human Services; Rockville, Maryland: 2019. Health Resources and Services Administration, Maternal and Child Health Bureau. Critical crossroads pediatric mental health care in the emergency department: A care pathway resource toolkit. [Google Scholar]
- 22.Hoffmann JA, Duffy SJ. Supporting youth mental health during the COVID-19 pandemic. Acad Emerg Med. 2021 doi: 10.1111/acem.14398. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cunningham NR, Ely SL, Barber Garcia BN, et al. Addressing pediatric mental health using telehealth during Coronavirus disease-2019 and beyond: a narrative review. Acad Pediatr. 2021;21:1108–1117. doi: 10.1016/j.acap.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duong MT, Bruns EJ, Lee K, et al. Rates of mental health service utilization by children and adolescents in schools and other common service settings: a systematic review and meta-analysis. Adm Policy Ment Health. 2021;48:420–439. doi: 10.1007/s10488-020-01080-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.