Abstract
The objective of this study is to conduct a systematic review and meta-analysis to assess the effect of psychosocial interventions in reducing problematic Internet use (PIU), anxiety, and depression symptoms in a sample of people. This review was registered on the PROSPERO database (CRD42020181912) and a total of 15 studies were included. Analyses of the effect of the interventions were conducted based on the standardized mean difference of the studied outcomes (PIU, anxiety, and depression). Most studies reported a positive effect of psychosocial interventions on reducing symptoms of PIU, depression, and anxiety among people with PIU. However, only one detected a robust effect in reducing symptoms of anxiety. For depression, this effect was more modest, and there was no difference between the different modalities of psychosocial interventions. The results suggest that psychosocial interventions are effective in reducing both symptoms of PIU and co-occurring symptoms of depression and anxiety in individuals with PIU.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11469-022-00846-6.
Keywords: Problematic Internet use, Depression, Anxiety, Interventions
Access to the Internet has proliferated substantially, with 5 billion people accessing the Internet daily (IWS, 2021). People are also spending more time on the Internet, and individuals are currently connected on average of 6 h and 40 min a day (InterNations, 2019). Many authors have reported that excessive Internet use has increased in many countries (Andrade et al., 2021a; Duong et al., 2020; Spritzer et al., 2022; Yang et al., 2018), particularly among younger people (Derevensky et al., 2019; Lin et al., 2018). The increase in excessive Internet use may be due to several factors, including greater ease of access, new forms of entertainment (social media), and devices with advanced technological resources (Geyer et al., 2021).
Currently, the term “problematic internet use” (PIU) has been used to describe behaviors related to lack of control, craving, and emotional instability caused by the lack of access to the Internet (Andrade et al., 2020b; Gómez et al., 2017). For this reason, PIU shares clinical similarities to substance and behavioral addictions, such as gambling, video game addiction, and sex addiction (Duong et al., 2020; Gómez et al., 2017). For instance, neuroimaging studies have shown that individuals with PIU exhibit activation of neural areas compared with substance use disorders (Chun et al., 2018) and behavioral addictions (Darnai et al., 2019).
As with other potentially addictive behaviors, there is no single factor that accounts for PIU. The theoretical Interaction of Person-Affect-Cognition-Execution (I-PACE) model proposed by Mathias Brand and colleagues was designed to explain the multi-faceted nature of the development and maintenance of behaviors related to PIU (Brand et al., 2016). The I-PACE considers the environmental aspects, individual characteristics, affect, and cognition associated with PIU. Regarding the affective component, studies indicate that individuals with PIU have lower quality of life (Andrade et al., 2021b) and a higher frequency of emotional problems (Cruz et al., 2018).
Importantly for the present study, there is evidence that symptoms of depression and anxiety are the disorders commonly associated with PIU (Li et al., 2017a, 2017b; Malak & Khalifeh, 2018). In a study conducted with over 15,000 Brazilian Internet users, those with PIU were 10 × more likely to have major depressive symptoms and 7 × more likely to have anxiety symptoms than individuals with no PIU (Andrade et al., 2020a). During the COVID-19 outbreak, some authors have found that symptoms of anxiety and depression have increased among individuals with PIU (Awan et al., 2021; Li et al., 2021). The association between PIU, anxiety, and depression have also been supported by mediation models between reinforcing stimuli and PIU (Casale et al., 2016; Wang et al., 2018) and in longitudinal approach that suggests certain psychopathologies may aggravate PIU symptoms over time (Dahl & Bergmark, 2020).
One of the links between emotional problems and PIU may be related to searching online for new relationships and virtual friendships. In this sense, the Internet is being used as an emotion regulation strategy (Faghani et al., 2020). These strategies are related to the cognition component in the I-PACE model in which cognitive skills are important to maintain or decrease the intensity of symptoms of PIU. In a study conducted by Spada and Marino (2017), emotion regulation was positively correlated with PIU. Together, these findings indicate that psychosocial interventions focused on regulating one or more of these components may be potentially effective in reducing PIU-related behaviors and the emotional problems associated with its use.
One of the first published intervention studies for people with PIU used Cognitive Behavioral Therapy (CBT) with a 12-session protocol (Young, 2011) that was later replicated with promising results (Young, 2013). In addition to CBT, other models, such as ecological (Stieger and Lewetz, 2018), positive psychology (Khazaei et al., 2017), and mindfulness (Quinones & Griffiths, 2019) have been used as a potential treatment for PIU with positive results. Although previous systematic reviews have assessed the effects of these interventions on PIU, few studies have reviewed whether these interventions also influence other components of the I-PACE model (Brand et al., 2019) that could be involved with the development and maintenance of PIU. A broader review of the effects of these interventions on additional components linked to the maintenance of the PIU may clarify the effectiveness of psychosocial interventions for PIU.
The present study aimed to conduct a systematic review and meta-analysis to examine the effect of different psychosocial interventions on PIU, depression, and anxiety symptoms in individuals with PIU. We hypothesized that (i) the psychosocial interventions would be effective both in reducing PIU-related symptoms and (ii) among studies that evaluated secondary measures, these interventions would also improve symptoms related to depression and anxiety.
Method
The protocol for this study was pre-registered on the International Prospective Register of Systematic Reviews platform (PROSPERO; no. CRD42020181912). This study was conducted in the following steps: (i) identification of research question; (ii) definition of inclusion and exclusion criteria; (iii) literature search; (iv) selection of studies; (v) data extraction; and (vi) assessment of publication bias and quality of studies.
Identification of the Research Question
The FINER criteria (Hulley et al., 2007) were used to assess whether the research question (Are psychological interventions for PIU also effective in reducing depression and anxiety?) was feasible, interesting, novel, ethical, and relevant. The research question indicated that it is feasible to be answered as this is a current topic, and there is a growing scope of literature that recognizes the importance of future research to assess treatments for people with PIU and their co-occurring mental health disorders.
Definition of Inclusion and Exclusion Criteria
We used the PICOS strategy to define the characteristics of the sample and the profile of the studies to be included (da Costa Santos et al., 2007). Individuals of all ages from empirical studies that presented the following methodological characteristics were included: (i) experimental or quasi-experimental studies; (ii) PIU was assessed using an instrument that was previously validated in the study country; (iii) studies also assessed anxiety and depression by means of previously validated instrument or clinical interview with a specialist in mental health (psychiatrist or psychologist); (iv) an independent follow-up assessment was conducted upon completion of the intervention; and (v) the studies included a protocol describing the intervention. We included only studies published in English, Portuguese, or Spanish.
We excluded studies that evaluated PIU associated with video game disorder, social media use, or substance use because some authors have shown that PIU can be confused with other behaviors with similar clinical characteristics (Shapira et al., 2003). As PIU is not considered a specific mental disorder, it may have clinical and behavioral characteristics confounding with behavioral addictions (Derevensky et al., 2019). Literature review studies, intervention protocols, and interventions focusing on the prevention of Internet use were also excluded. For more details, see Supplementary Table 1.
Literature Search
Six databases (CINAHL, LILACS, PsycArticles, PubMed, Scopus, and Web of Science) were searched on August 2020 and updated in November 2021. For the search strategy, the descriptors used were previously consulted in the Medical Subject Headings [MeSH] and/or [DeCS] thesaurus and combined using Boolean operators that formed specific algorithms for each database (Table 1). The presence of descriptors in any field of the manuscript (title, abstract, or full text) were considered for screening to maximize the retrieval of relevant articles. All articles found were exported to Rayyan software (Ouzzani et al., 2016).
Table 1.
Search strategy based on algorithms tailored to each database
| Database | Algorithm | N |
|---|---|---|
| CINAHL | ("internet addiction" OR "problematic internet use" OR "dysfunctional internet use") AND (treatment OR intervention OR therapy OR psychotherapy) | 339 |
| LILACS | ("internet addiction" OR "problematic internet use" OR "dysfunctional internet use") AND (treatment OR intervention OR therapy OR psychotherapy) | 6 |
| PsycArticles | ("internet addiction" OR "problematic internet use" OR "dysfunctional internet use") AND (treatment OR intervention OR therapy OR psychotherapy) | 39 |
| PubMed | ("internet addiction"[All Fields] OR "problematic internet use"[All Fields] OR (dysfunctional[All Fields] AND ("internet"[MeSH Terms] OR "internet"[All Fields]))) AND (("therapy"[Subheading] OR "therapy"[All Fields] OR "treatment"[All Fields] OR "therapeutics"[MeSH Terms] OR "therapeutics"[All Fields]) OR ("methods"[MeSH Terms] OR "methods"[All Fields] OR "intervention"[All Fields]) OR ("therapy"[Subheading] OR "therapy"[All Fields] OR "therapeutics"[MeSH Terms] OR "therapeutics"[All Fields]) OR ("psychotherapy"[MeSH Terms] OR "psychotherapy"[All Fields])) | 1040 |
| Scopus | TITLE-ABS-KEY (("internet addiction” OR” problematic internet use” OR” dysfunctional internet use”) AND (treatment OR intervention OR therapy OR psychotherapy)) AND (LIMIT-TO (DOCTYPE,” ar”)) AND (LIMIT TO (LANGUAGE,” English”) OR LIMIT-TO (LANGUAGE, “Portuguese")) OR LIMIT-TO (LANGUAGE, "Spanish")) | 589 |
| Web of Science | (("internet addiction" OR "problematic internet use" OR "dysfunctional internet use") AND (treatment OR intervention OR therapy OR psychotherapy)) | 627 |
| Total | 2640 |
Selection of Studies
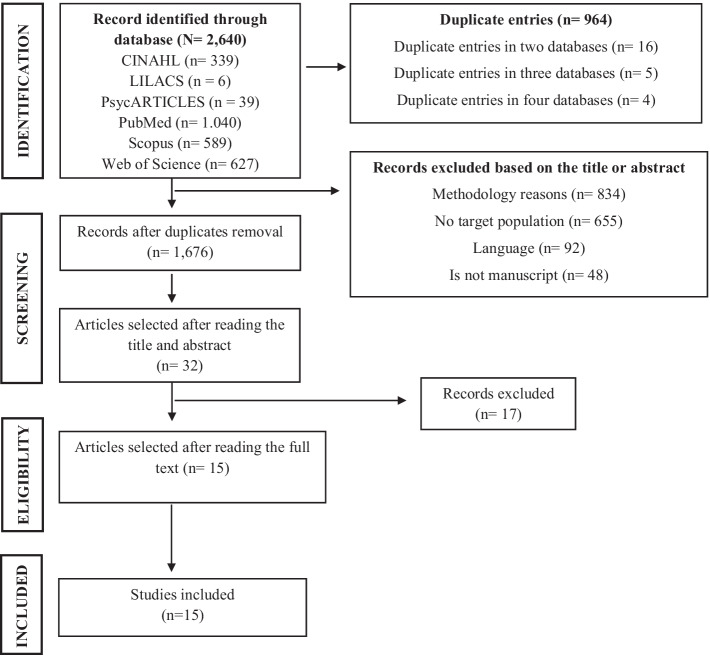
The screening and removal of duplicate records were conducted by two independent reviewers using Rayyan software (see Fig. 1 for a PRISMA diagram). After duplicates were removed, 1676 articles were assessed based on their title and abstract. Thirty-two studies were then included for full-text review. Three reviewers carefully read the complete text and 17 articles were removed at this stage. This process occurred blindly, using Rayyan software (Blind on), in which none of the reviewers had access to information from the others until the conclusion of the analyses. In total, 15 met the inclusion criteria and were included for synthesis and meta-analysis. Supplementary Table 1 shows the exclusion criteria for 17 studies according to each reviewer. We include this data for ethics and transparency of our protocol.
Fig. 1.
Flow diagram of search
Data Extraction
Data were imported from.RIS files for each of the databases to the Rayyan software, except for the CINAHL database, which was imported to Mendeley due to the incompatibility with Rayyan. Next, we used the Airtable Platform to extract and organize the following data: (i) publication details (author, year, country, sample profile, and age); (ii) measures used to assess PIU (instruments, interviews, and others); (iii) methodological design; (iv) conflict of interest; and (v) main results.
Assessment of Publication Bias and Quality of Studies
We used the ROBIS tool to assess the risk of bias in the systematic review (Whiting et al., 2016). This method comprises three steps: (i) assessing the relevance; (ii) identifying concerns about the review process; and (ii) judging the risk of bias which was defined as follows, whether the methods used in our systematic review minimized the risk of bias of the summary estimates and conclusions of the evaluated studies. Particularly in the second step, four dimensions assessed the risk of bias: (i) study eligibility criteria; (ii) identification and selection of studies; (iii) data collection and study appraisal; and (iv) synthesis and findings (see Supplementary Table 1).
Analyses
The analyses were conducted using the standardized mean difference as the outcome measure for all variables (PIU, anxiety, and depression). A random-effects model was fitted, and we estimated the amount of heterogeneity based on the maximum-likelihood estimator. Also, we used standardized residuals and Cook’s distances to detect whether interventions may be outliers and/or were influential in the context of the model. We considered as outliers those data with a Cook’s distance of three times greater than the mean. Finally, the funnel plot asymmetry was checked based on the rank correlation and regression test.
Results and Discussion
Regarding the description of the studies included (Table 2), a third of the studies (n = 5) were conducted with Chinese individuals, and more than half of the studies included Asian people (n = 8). These data are relevant because many authors have reported a high prevalence of PIU in Asian countries (Li et al., 2021). In some of these countries, the use of smartphones is encouraged by authorities to perform daily activities (paying bills, shopping, transport tickets) (Li, 2019), which may increase the risk of PIU.
Table 2.
Main methodological and intervention characteristics of each study
| No | Authors | Year | Country | Age | Method | Arms (n) | Measures | Intervention | No and length of sessions | Profile |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Du et al | 2010 | China | 12–17 | Es |
CG = 24 EG = 32 |
BDQIA, IOS-S, TMDS, SDQ, SCARED | EG = CBT | CBT = 8 (90–120 min) | G |
| 2 | Gholamian et al | 2019 | Iran | 16–17 | QeS |
CG = 60 EG = 60 |
BASNEF, NSKQ, YDQ | EG = BASNEF | BASNEF = 2 (NA) | G |
| 3 | Hui et al | 2017 | China | 19–25 | RCT |
CG = 37 EG1 = 39 EG2 = 36 |
YDQ, SCL-90, P50 |
EG1 = EA EG2 = CT EG3 = EA + CT |
EA = 10 (30 min) CBT = 5 (30 min) |
G + I |
| 4 | Ke et al. (a) | 2018 | Malaysia | 13–18 | QeS | EG = 4 5 | PIUQ, DASS-42, SIAS | EG = CBT | CBT = 8 (90 min) | G |
| 5 | Ke et al. (b) | 2018 | Malaysia | 13–18 | QeS | EG = 157 | PIUQ, DASS -42, SIAS | EG = CBT | CBT = 8 (90 min) | G |
| 6 | Khazaei et al | 2017 | Iran | 20–30 | RCT |
CG = 24 EG = 24 |
YDQ, Y-BOCS, QRI, SI | EG = PP | PP = 10 (NA) | G |
| 7 | Kim et al | 2018 | South Korea | 12–17 | QeS | EG = 17 | K-scale, YDQ, IAS, CDI, STAI | EG = CBT | CBT = 8 (120 min) | G |
| 8 | Pan | 2020 | China | 13–18 | QeS |
CG = 10 EG1 = 10 EG2 = 10 EG3 = 10 |
YDQ |
EG1 = CBT EG2 = PE EG3 = CBT + PE |
NA | G + I |
| 9 | Quinones et al | 2019 | UK | 39–42 | RCT |
CG = 148 EG1 = 343 EG2 = 151 |
CIU, FFMQ, PHQ-ADS |
EG1 = MDF EG2 = GR |
Using app = 14 (10 min) | I |
| 10 | Santos et al | 2017 | Brazil | 18–65 | QeS |
EG1 = 42 EG2 = 42 |
IAT, HAM-A, HDRS, CGI |
EG1 = PPE EG2 = CBT + pharmacotherapy |
CBT = 8–10 (NA) | G + I |
| 11 | Tas et al | 2018 | Turkey | 15 | QeS |
CG = 12 EG = 12 |
YDQ, SCL-90 | EG = PPE | PPE = 10 (50 min) | G |
| 12 | Thorens et al | 2014 | Swiss | 13–67 | QeS | EG = 57 | ACP, IAT | EG = CBT | CBT = 6 (50 min) | Individual |
| 13 | Yang et al | 2017 | China | 18–30 | RCT |
EG1 = 15 EG2 = 14 |
IAS, BIS-11, MRS |
EG1 = EA EG2 = PP |
EA = 45 (30 min) PP = 11 (120 min) |
G + I |
| 14 | Young | 2013 | EUA | 22–56 | QeS | EG = 128 | COQ, IAT | EG = CBT | CBT = 12 (NA) | - |
| 15 | Zhu et al | 2012 | China | 19–25 | RCT |
EG1 = 39 EG2 = 36 EG3 = 37 |
IAT, WMS |
EG1 = EA EG2 = CT EG3 = EA + CT |
EA = 10 (30 min) CBT = 5 (30 min) |
G + I |
Legend: Es, experimental study; QeS, quasi-experimental study; CG, control group; EG, experimental groups; CBT, cognitive-behavioral therapy; PP, positive psychology; G, group therapy; I, individual therapy; EA, electroacupuncture; CT, comprehensive therapy; PPE, psychoeducational program; PE, physical exercise; APP, applicative; MDF, mindfulness; GR, gradual relaxation; BASNEF, Belief, Attitude, Subjective Norm, and Enabling Factors; NA, not available; BDQIA, Beard’s Diagnostic Questionnaire for Internet addiction; IOS-S, Internet Overuse Self-Rating Scale; TMDS, Time Management Disposition Scale; SDQ, Strength and Difficulties Questionnaire; SCARED, Screen for Child Anxiety Related Emotional Disorders; BASNEF, Belief, Attitude, Subjective Norm, and Enabling Factors; NSKQ, Knowledge Questionnaire; YDQ, Young’s Diagnostic Questionnaire; SCL-90, Brief Symptom Inventory; PIUQ, Problematic Internet Use Questionnaire; DASS, Depression, Anxiety, Stress Scales; SIAS, Social Interaction Anxiety Scale; Y-BOCS, Yale–Brown Obsessive Compulsive Scale; QRI, Quality of Relationships nventory); SI, severity of Internet use; K-scale, Korean Internet addiction self-report test; IAS, Young’s Internet Addiction Scale; CDI, Children’s Depression Inventory; STAI, State-Trait Anxiety Inventory; CIU, Compulsive Internet use; FFMQ, Five Facet Mindfulness Questionnaire; PHQ-ADS, Patient Health Questionnaire Anxiety and Depression Scale; IAT Internet addiction test; HAM-A, Hamilton Anxiety Scale; HDRS, Hamilton Depression Scale; CGI, Clinical Global Impressions; SCL-90, Brief Symptom Inventory; ACP, Avaliação clínica psiquiatrica; BIS-11, Barratt Impulsiveness Scale; MRS, Magnetic Resonance System; COQ, client outcome questionnaire); WMS, Wechsler Memory Scale
Although some authors have reported a higher prevalence of PIU among younger individuals (Andrade et al., 2021c; Derevensky et al., 2019), we identified only five studies evaluating the effect of psychosocial interventions exclusively in adolescents with PIU (studies 1, 2, 3, 5, and 8 in Table 2). The remaining studies were conducted in populations with vast age ranges (between 13 and 65 years). There is a large amount of evidence that adolescents present not only a higher prevalence of PIU compared to adults but also a higher frequency of comorbidities (Andrade et al., 2020c; Cruz et al., 2018; Dahl & Bergmark, 2020; Gómez et al., 2017), which tends to be more intense in adults (Pan et al., 2020).
Therefore, further studies are needed to investigate interventions that may be effective in reducing PIU, depression, and anxiety symptoms among adolescents with PIU. The main results are synthesized in Table 3. In all the evaluated studies, positive effects were reported in reducing the intensity of PIU and emotional problems regardless of the treatment modality. However, a meta-analysis was conducted to assess each study’s weight in reducing PIU symptoms and emotional problems. Considering the type of intervention, most studies (n = 9) used cognitive-behavioral therapy (CBT) as the main therapeutic method, followed by positive psychology (PP; n = 2), and electro-acupuncture (EA; n = 2).
Table 3.
Main results found in the assessed studies
| N | Authors | Main results |
|---|---|---|
| 1 | Du et al | CBT reduced PIU scores in adolescents, mainly in self-time management compared to CG. The intervention also significantly reduced Internet usage time, improved emotional management and cognitive bias, and reduced internet-related behavior |
| 2 | Gholamian et al | BASNEF significantly reduced Internet usage time compared to CG. The intervention also significantly increased the scores for the variables: knowledge; attitude; subjective norms; perceived behavioral control; facilitating factors for Internet use |
| 3 | Hui et al | The group that received the combined intervention (CBT + EA) had significantly lower PIU scores and lower levels of anxiety and depression compared to the other groups. The combined intervention also increased the amplitude and latency of P50 of Auditory Evoked Potential in subjects with PIU |
| 4 | Ke et al. A | CBT prevented a more damaging progression of PIU and reduced participants’ anxiety, stress, and phobic interaction. These results were maintained 1 month after the study (follow-up) |
| 5 | Ke et al. B | CBT significantly reduced the intensity of Internet usage time; PIU score and social anxiety. Most participants were able to manage their Internet usage time better and increase social interaction. These results were maintained 1 month after the study (follow-up) |
| 6 | Khazaei et al | PP reduced Internet severity rates and the number of individuals with PIU compared to CG. The authors also reported that PP promoted an improvement in the quality of social relationships |
| 7 | Kim et al | CBT reduced PIU, anxiety and depression scores in adolescents compared to CG. After 1 month, the PIU scores were lower than baseline, but the intensity of anxiety and depression symptoms was even lower immediately after the program |
| 8 | Pan | The combined intervention (CBT + PE) significantly reduced the other groups’ PIU symptoms (time and motivation to use the Internet) |
| 9 | Quinones et al | The MDF and GR interventions were equally effective in reducing symptoms of anxiety and depression, and the MDF had a significantly greater effect in reducing PIU |
| 10 | Santos et al | CBT combined with medication significantly reduced PIU and anxiety compared to PPE group participants |
| 11 | Tas et al | PPE significantly reduced PIU, and psychological symptoms compared to CG. It was effective in reducing psychological symptoms and Internet addiction. These results were maintained 45 days after the end of the study (follow-up) |
| 12 | Thorens et al | Participants undergoing CBT significantly improved their PIU symptoms and CGI score concerning themselves before the intervention |
| 13 | Yang et al | Both EA and PP reduced PIU scores, and EA more intensely reduced scores related to PIU subfactors (behavioral control, impulsivity control, and protection of brain neurons) |
| 14 | Young | CBT significantly reduced PIU scores from baseline. In addition, more than 95% of participants improved the way they manage PIU-related symptoms. Almost 80% of these participants remained recovered 6 months after the study (follow-up) |
| 15 | Zhu et al | In the three groups (EA; CT; EA + CT), a reduction in PIU scores and an increase in short-term memory capacity was detected. In the CT group, the PIU scores were even lower compared to the other groups |
Legend: CBT, cognitive-behavioral therapy; PIU, problematic Internet use); CG, control group; BASNEF, Belief, Attitude, Subjective Norm, and Enabling Factors); EA, electroacupuncture; PP, positive psychology; PE, physical exercise; MDF, mindfulness; GR, gradual relaxation; PPE, psychoeducational program; CGI, Clinical Global Impressions; CT, comprehensive therapy
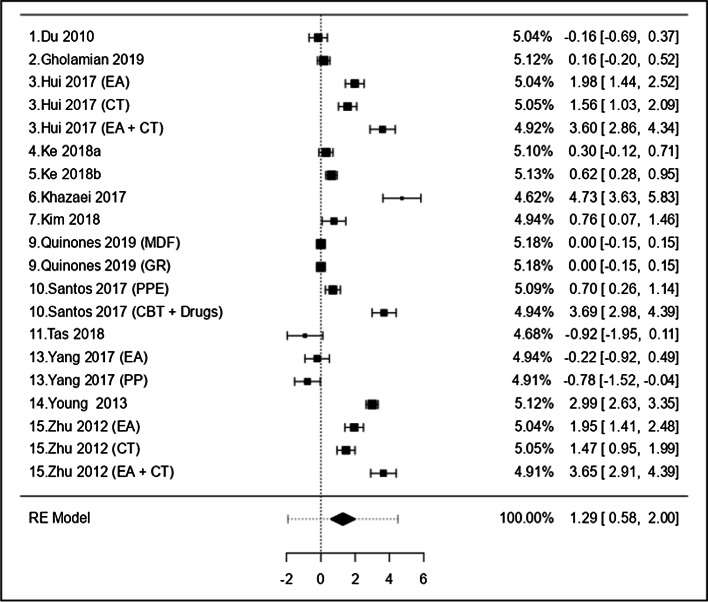
Effects on Symptoms of PIU
A total of 20 interventions derived from the 15 studies were included to assess the effect on PIU symptoms, as shown in Fig. 2. The observed standardized mean differences ranged from − 0.92 to 4.72, with the majority (70%) of positive estimates and the rest of them the true outcome may be negative. The standardized residuals indicated that none of the studies had a value larger than ± 3.02; and there was no indication of outliers. None of the studies were identified as being overly influential when evaluating the values of Cook’s distance. Neither the rank correlation nor the regression test indicated any funnel plot asymmetry (p = 0.12 and p = 0.12, respectively). The data indicated that none of the tested interventions (alone or in conjunction with any other) had a greater influence on reducing PIU symptoms. These findings are in accordance with previous studies in the literature (Saletti et al., 2021; Winkler et al., 2013). On the other hand, these same authors could not identify a robust effect of interventions in reducing PIU symptoms.
Fig. 2.
Forest plot showing standardized mean difference (95% CI) and the studies weighted regarding different interventions to reduce problematic internet use. Notes: (i) The repeating studies in the plot indicate the effect of each separate intervention; (ii) the studies 1, 2, 6, 9, 11, and 13 were compared with control groups, and the others were compared before and after the intervention; (iii) we excluded studies 8 and 12 from this plot due to the impossibility of calculating the standardized mean difference based on the data available in these articles
One unexpected finding was that CBT did not stand out as an intervention that significantly influenced the reduction of PIU symptoms. Reviews of randomized controlled trials have shown a positive effect of CBT in treating problems related to impulse disorders, but the effect size was generally modest (Campbell et al., 2018; Carroll & Kiluk, 2017; Perry & Lawrence, 2017). Therefore, in clinical practice for people with addiction symptoms, even the best available research evidence still has limited success rates, which shows the complexity and multifactorial factors involved in these behaviors (Carroll & Kiluk, 2017; Lopes et al., 2021).
Considering the similarities of PIU with addictive behaviors and impulse-control disorders, the interventions and recommendations discussed above tend to present good responses in the treatment of PIU as seen in the meta-analysis conducted in this study. Spada (2014) warned of the relevance of assessment tools and interventions aimed at controlling one’s use of the Internet since this behavior leads to negative consequences in daily life.
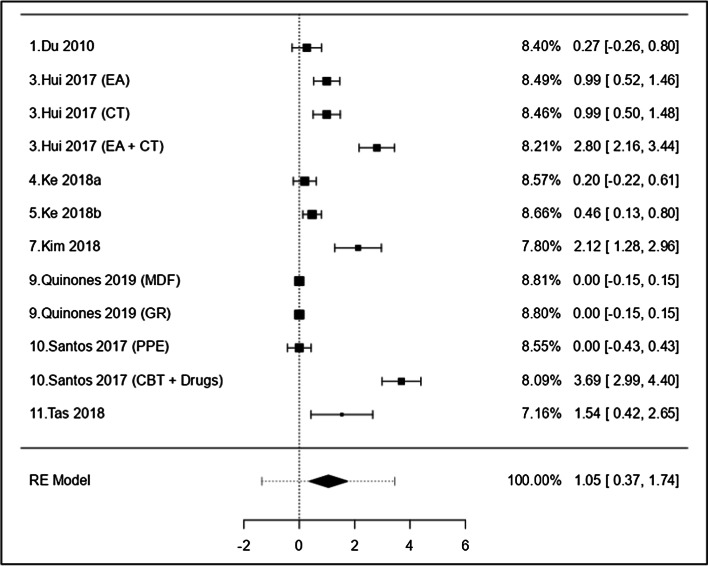
Effects on Symptoms of Anxiety
Figure 3 shows the effect of 12 interventions derived from the 8 studies in reducing anxiety symptoms. The observed standardized mean differences ranged from 0.0 to 3.69, and we mainly found positive estimates (75%). Only one intervention (CBT + pharmacotherapy) had standardized residuals larger than ± 2.86 and could be overly influential (Santos et al., 2017).
Fig. 3.
Forest plot showing standardized mean difference (95% CI) and the studies weighted regarding different interventions to reduce anxiety symptoms among individuals with PIU. Notes: (i) The repeating studies in the plot indicate the effect of each separate intervention; (ii) the studies 1, 9, and 11 were compared with control groups, and the others were compared before and after the intervention
These results may be related not only to the methodological characteristics of the studies (which are largely like each other) but also to the interventions’ profile (type of therapist, group or individual therapy, length of time, participant engagement, rate drop out, etc.). In the review by Lee et al. (2019) regarding the prevention strategies and interventions for PIU, the authors listed some challenges to effective prevention and intervention programs focused on PIU. First, there are few studies on this topic because the concept of PIU is relatively new and complex as it must be considered in the context of how people handle with the speed of the development of new technologies. Second, it is plausible that several forms of PIU exist (different factors linked to the craving, abstinence, excessive use, etc.) because Internet use is strongly connected with different technologies (smartphone usage, video games, watching videos and movies, messaging, etc.), which can influence the strategic goals of each intervention.
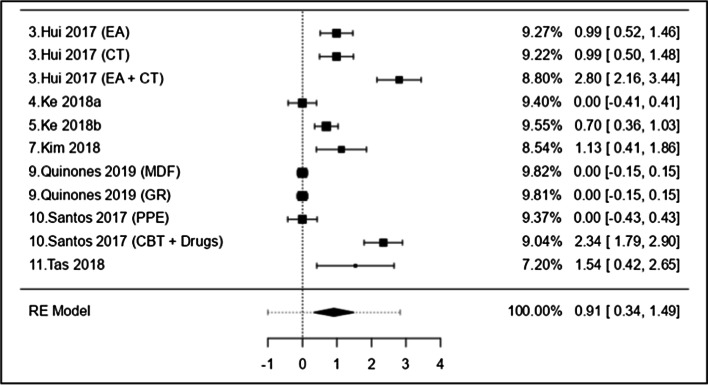
Effects on Symptoms of Depression
For depression (Fig. 4), 11 interventions were analyzed from 7 studies. The observed standardized mean differences ranged from 0.00 to 2.79, with the most positive estimates (64%). Therefore, the mean outcome differed significantly from zero (z = 3.12, p < 0.01). According to the Q-test, the true outcomes appear to be heterogeneous (Q (10) = 174.56, p < 0.01, tau2 = 0.8670, I2 = 96.84%). According to Cook’s distances, none of the studies were considered overly influential.
Fig. 4.
Forest plot showing standardized mean difference (95% CI) and the studies weighted regarding different interventions to reduce depression symptoms among individuals with PIU. Notes: (i) The repeating studies in the plot indicate the effect of each separate intervention; (ii) the studies 9 and 11 were compared with control groups, and the others were compared before and after the intervention
In addition to identifying the effect on reducing PIU symptoms, anxiety was the most studied disorder (n = 8, 53.3%), followed by depression (n = 7; 46.6%). These data are in accordance with findings indicating a high prevalence of mood and anxiety disorders in individuals with PIU (Andrade et al., 2020a, 2020b, 2020c; Faghani et al., 2020). One of the causes may be related to neurochemical mechanisms in common neural pathways, for addictive behaviors and depression and anxiety. It is well well-known that individuals who use substances have hyperactivation of dopaminergic pathways (e.g., mesolimbocortical) and consequent release of dopamine in the nucleus accumbens (Chun et al., 2018). These findings have also been detected in preclinical studies (Burton et al., 2015) and among depressive patients with severe symptoms of anhedonia (Foell et al., 2021). Hyperactivation of glutamatergic pathways from the prefrontal cortex to the nucleus accumbens has been associated with fissure and withdrawal (Murray et al., 2021) but may also be related to anxiety symptoms (Nasir et al., 2020).
Therefore, the greater the levels of anxiety and depression, the greater the intensity of Internet use. Consequently, this overuse may further increase these symptoms due to cognitive bias (Sussman et al., 2016). In the updated I-PACE model (Brand et al., 2019), a cognitive bias is a component that influences individuals’ decision-making based on coping strategies for stressful situations. Thus, when individuals cannot handle effectively with stressful situations, they may resort to escape/avoidance behaviors through different devices with Internet access. Therefore, cognitive bias may have an indirect effect on PIU as a mediating role. Previous findings support this hypothesis. In a study conducted with 219 Serbian children, psychopathological symptoms had a mediating effect on irrational beliefs and PIU (Vukosavljevic-Gvozden et al., 2015). Furthermore, the most influential mediating variable was derived from the symptoms of obsessive–compulsive disorder. Regarding irrational beliefs, low frustration tolerance was positively correlated with the length of time using video games. According to the authors mentioned above, when an individual is facing a stressful event in their real life, they believe that they are not able to handle the situation, leading them to seek immediate gratification from the Internet, which increases the risk of PIU (Vukosavljevic-Gvozden et al., 2015).
Limitations
Our research has methodological limitations. First, we included studies with small samples and others that did not have control groups. Second, as the definition of PIU is still broad in the literature, we included all studies that measured PIU based on at least a specific validated instrument or questions related to Internet use. However, we did not consider smartphone or video game addiction, which can be a confounding variable with PIU (Montag & Rumpf, 2021). The included studies also have limitations that should be considered. First, in our quality assessment, several studies did not provide adequate information. For example, two studies (Table 2, studies 8 and 12) did not report mean and standard deviation information and were not included in the meta-analysis. Second, the date on which the studies were conducted wasn’t indicated, which is important due to how the Internet interacts with the advancement of technological development. This difficulty was also reported in a recent systematic review evaluating the association between PIU and substance use (Lanthier-Labonté et al., 2020).
Conclusion and Future Directions
In summary, although we found that psychosocial interventions effectively reduced PIU, depression, and anxiety, in individuals with PIU no specific psychosocial intervention was overly influential compared to each other in reducing PIU symptoms and depression. Only one study was found to be influential in reducing anxiety symptoms (CBT + pharmacotherapy). Further research is needed to investigate the effect of other modalities as their use in reducing PIU symptoms is still recent. Furthermore, more longitudinal studies are needed to examine whether the improvements in reducing symptoms of PIU, anxiety, and depression are stable, given that most studies reported a follow-up period of 1 month. Qualitative studies that assess the impact of these interventions could also contribute to a better understanding of how these interventions can benefit participants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix. ROBIS Checklist
Phase 1: Assessing relevance (optional)
| Category | Target question (e.g., overview or guideline) | Review being assessed |
|---|---|---|
| Patients/population(s) | Individuals with problematic internet use | How effective are psychological treatments/interventions for reducing symptoms of PIU, depression, and anxiety in individuals with problematic Internet use? |
| Intervention(s) | Psychotherapeutic; psychoeducational; psychosocial | |
| Comparator(s) | No intervention or intervention gold standard | |
| Outcome(s) | Treatment effectiveness for Internet abuse and the variables: anxiety and depression |
Phase 2: Identifying concerns with the review process
Legend: Y=Yes, PY=Probably yes, PN=Probably no, N=No, NI=No information
| Domain 1: Study eligibility criteria | ||
|---|---|---|
| 1.1Did the review adhere to pre-defined objectives and eligibility criteria? | Y/PY/PN/N/NI | |
| 1.2 Were the eligibility criteria appropriate for the review question? | Y/PY/PN/N/NI | |
| 1.3 Were eligibility criteria unambiguous? | Y/PY/PN/N/NI | |
| 1.4 Were any restrictions in eligibility criteria based on study characteristics appropriate (e.g., date, sample size, study quality, outcomes measured)? | Y/PY/PN/N/NI | |
| 1.5 Were any restrictions in eligibility criteria based on sources of information appropriate (e.g., publication status or format, language, availability of data)? | Y/PY/PN/N/NI | |
| Domain 2: Identification and selection of studies | ||
| 2.1 Did the search include an appropriate range of databases/electronic sources for published and unpublished reports? | Y/PY/PN/N/NI | |
| 2.2 Were methods additional to database searching used to identify relevant reports? | Y/PY/PN/N/NI | |
| 2.3 Were the terms and structure of the search strategy likely to retrieve as many eligible studies as possible? | Y/PY/PN/N/NI | |
| 2.4 Were restrictions based on date, publication format, or language appropriate? | Y/PY/PN/N/NI | |
| 2.5 Were efforts made to minimize error in selection of studies? | Y/PY/PN/N/NI | |
| Domain 3: Data collection and study appraisal | ||
| 3.1 Were efforts made to minimize error in data collection? | Y/PY/PN/N/NI | |
| 3.2 Were sufficient study characteristics available for both review authors and readers to be able to interpret the results? | Y/PY/PN/N/NI | |
| 3.3 Were all relevant study results collected for use in the synthesis? | Y/PY/PN/N/NI | |
| 3.4 Was risk of bias (or methodological quality) formally assessed using appropriate criteria? | Y/PY/PN/N/NI | |
| 3.5 Were efforts made to minimize error in risk of bias assessment? | Y/PY/PN/N/NI | |
| Domain 4: Synthesis and findings | ||
| 4.1 Did the synthesis include all studies that it should? | Y/PY/PN/N/NI | |
| 4.2 Were all pre-defined analyses reported or departures explained? | Y/PY/PN/N/NI | |
| 4.3 Was the synthesis appropriate given the nature and similarity in the research questions, study designs, and outcomes across included studies? | Y/PY/PN/N/NI | |
| 4.4 Was between-study variation (heterogeneity) minimal or addressed in the synthesis? | Y/PY/PN/N/NI | |
| 4.5 Were the findings robust, e.g., as demonstrated through funnel plot or sensitivity analyses? | Y/PY/PN/N/NI | |
| 4.6 Were biases in primary studies minimal or addressed in the synthesis? | Y/PY/PN/N/NI | |
Phase 3: Judging risk of bias (summarize the concerns identified during the phase 2 assessment).
| Domain | Concern | Rationale for concern |
|---|---|---|
| 1. Concerns regarding specification of study eligibility criteria | LOW | According to the criteria identified in domain 1, the risk potential is LOW because the analyses included all information |
| 2. Concerns regarding methods used to identify and/or select studies | LOW | All criteria for study identification and selection were met and included in this paper |
| 3. Concerns regarding methods used to collect data and appraise studies | LOW | All three domain criteria are detailed in the manuscript, reducing the risk of bias |
| 4. Concerns regarding the synthesis and findings | LOW | Based on the items suggested in the results summary, item 4.6 was not conducted. As for item 4.2, the participants’ losses were not detailed. Although most studies used CBT, other therapies were also detected, making the results more imprecise |
| Risk of bias in the review | ||
| Describe whether conclusions were supported by the evidence: Some studies had small sample sizes, and others had no control groups; there was difficulty in defining PIU (problematic internet use) in some papers | ||
| A. Did the interpretation of findings address all the concerns identified in Domains 1 to 4? | Y/PY/PN/N/NI | |
| B. Was the relevance of identified studies to the review’s research question appropriately considered? | Y/PY/PN/N/NI | |
| C. Did the reviewers avoid emphasizing results based on their statistical significance? | Y/PY/PN/N/NI | |
| Risk of bias in the review | LOW/HIGH/UNCLEAR | |
| Rationale for risk: Two reviewers performed the first assessment paired and independently based on the FINER criteria and the PICOS strategy. Three further reviewers evaluated independently, blindly, and critically the inclusion or exclusion of the 32 selected articles. These manuscripts were read and evaluated in full by a fourth reviewer. All reviewers were experts in the field of Internet addiction. The evaluations were conducted autonomously, and disagreements were discussed via online meetings | ||
Author Contribution
André Luiz Monezi Andrade: Conceptualization, methodology, formal analysis, original draft writing. Gabriella Di Girolamo Martins: Conceptualization, Data curation, review and editing. Adriana Scatena: Conceptualization, methodology, review and editing. Fernanda Machado Lopes: Methodology, formal analysis, review and editing. Wanderlei Abadio de Oliveira: Methodology, review and editing. Hyoun S Kim: Methodology, review and editing. Denise de Micheli: Conceptualization, methodology, supervision, project administration.
Funding
This study was partly supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ, no. 303163/2020–8) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) (no 2019/19972–9).
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
André Luiz Monezi Andrade, Email: andre.andrade@puc-campinas.edu.br.
Gabriella Di Girolamo Martins, Email: gabriella.dgm@puccampinas.edu.br.
Adriana Scatena, Email: adriana.scatena7@gmail.com.
Fernanda Machado Lopes, Email: femlopes23@gmail.com.
Wanderlei Abadio de Oliveira, Email: wanderlei.oliveira@puc-campinas.edu.br.
Hyoun S. Kim, Email: andrewhs.kim@ryerson.ca
Denise De Micheli, Email: demicheli.unifesp@gmail.com.
References
- Andrade ALM, Kim DJ, Scatena A, Enes CC, Enumo SRF, De Micheli D. Validity and reliability of the Brazilian version of the smartphone addiction scale-long version (SAS-LV) Trends in Psychology. 2021;29(2):302–319. doi: 10.1007/s43076-020-00046-y. [DOI] [Google Scholar]
- Andrade, A. L. M., Scatena, A., de Oliveira Pinheiro, B., de Oliveira, W. A., Lopes, F. M., & De Micheli, D. (2021b). Psychometric properties of the Smartphone Addiction Inventory (SPAI-BR) in Brazilian adolescents. International Journal of Mental Health and Addiction,1–16,. 10.1007/s11469-021-00542-x
- Andrade, A. L. M., Enumo, S. R. F., Passos, M. A. Z., Vellozo, E. P., Schoen, T. H., Kulik, M. A., … & Vitalle, M. S. D. S. (2021c). Problematic Internet use, emotional problems and quality of life among adolescents. Psico-USF,26, 41–51. 10.1590/1413-82712021260104
- Andrade A, Scatena A, Bedendo A, Enumo S, Dellazzana-Zanon LL, Prebianchi HB, de Lara Machado W, de Micheli D. Findings on the relationship between Internet addiction and psychological symptoms in Brazilian adults. International Journal of Psychology. 2020;55(6):941–950. doi: 10.1002/ijop.12670. [DOI] [PubMed] [Google Scholar]
- Andrade, A. L. M., Kim, D. J., Caricati, V. V., Martins, G. D. G., Kirihara, I. K., Barbugli, B. C., … & De Micheli, D. (2020b). Validity and reliability of the Brazilian version of the Smartphone Addiction Scale-Short Version for university students and adult population. Estudos De Psicologia (campinas),37, e190117. 10.1590/1982-0275202037e190117
- Andrade, A. L. M., Scatena, A., Martins, G. D. G., de Oliveira Pinheiro, B., da Silva, A. B., Enes, C. C., … & Kim, D. J. (2020c). Validation of smartphone addiction scale–Short version (SAS-SV) in Brazilian adolescents. Addictive Behaviors,110, 106540. 10.1016/j.addbeh.2020.106540 [DOI] [PubMed]
- Awan HA, Aamir A, Diwan MN, Ullah I, Pereira-Sanchez V, Ramalho R, Orsolini L, de Filippis R, Ojeahere MI, Ransing R, Vadsaria AK, Virani S. Internet and pornography use during the COVID-19 pandemic: Presumed impact and what can be done. Frontiers in Psychiatry. 2021;12:623508. doi: 10.3389/fpsyt.2021.623508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand M, Wegmann E, Stark R, Müller A, Wölfling K, Robbins TW, Potenza MN. The Interaction of Person-Affect-Cognition-Execution (I-PACE) model for addictive behaviors: Update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neuroscience and Biobehavioral Reviews. 2019;104:1–10. doi: 10.1016/j.neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Brand M, Young KS, Laier C, Wölfling K, Potenza MN. Integrating psychological and neurobiological considerations regarding the development and maintenance of specific Internet-use disorders: An Interaction of Person-Affect-Cognition-Execution (I-PACE) model. Neuroscience and Biobehavioral Reviews. 2016;71:252–266. doi: 10.1016/j.neubiorev.2016.08.033. [DOI] [PubMed] [Google Scholar]
- Burton AC, Nakamura K, Roesch MR. From ventral-medial to dorsal-lateral striatum: Neural correlates of reward-guided decision-making. Neurobiology of Learning and Memory. 2015;117:51–59. doi: 10.1016/j.nlm.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell EJ, Lawrence AJ, Perry CJ. New steps for treating alcohol use disorder. Psychopharmacology (Berl) 2018;235(6):1759–1773. doi: 10.1007/s00213-018-4887-7. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD. Cognitive behavioral interventions for alcohol and drug use disorders: Through the stage model and back again. Psychology of Addictive Behaviors. 2017;31(8):847–861. doi: 10.1037/adb0000311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casale S, Caplan SE, Fioravanti G. Positive metacognitions about Internet use: The mediating role in the relationship between emotional dysregulation and problematic use. Addictive Behaviors. 2016;59:84–88. doi: 10.1016/j.addbeh.2016.03.014. [DOI] [PubMed] [Google Scholar]
- Cheng YS, Ko HC, Sun CK, Yeh PY. The relationship between delay discounting and Internet addiction: A systematic review and meta-analysis. Addictive Behaviors. 2021;114:106751. doi: 10.1016/j.addbeh.2020.106751. [DOI] [PubMed] [Google Scholar]
- Chun JW, Choi J, Cho H, Choi MR, Ahn KJ, Choi JS, Kim DJ. Role of frontostriatal connectivity in adolescents with excessive smartphone use. Frontiers in Psychiatry. 2018;9:437. doi: 10.3389/fpsyt.2018.00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz FAD, Scatena A, Andrade ALM, De Micheli D. Evaluation of Internet addiction and the quality of life of Brazilian adolescents from public and private schools. Estudos De Psicologia (Campinas) 2018;35(2):193–204. doi: 10.1590/1982-02752018000200008. [DOI] [Google Scholar]
- da Costa Santos CM, de Mattos Pimenta CA, Nobre MR. The PICO strategy for the research question construction and evidence search. Revista Latino-Americana De Enfermagem. 2007;15(3):508–511. doi: 10.1590/s0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- Dahl D, Bergmark KH. Problematic internet use: A scoping review – longitudinal research on a contemporary social problem, 2006–2017. Nordic Studies on Alcohol and Drugs. 2020;37(6):497–525. doi: 10.1177/1455072520941997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnai G, Perlaki G, Zsidó AN, Inhóf O, Orsi G, Horváth R, Nagy SA, Lábadi B, Tényi D, Kovács N, Dóczi T, Demetrovics Z, Janszky J. Internet addiction and functional brain networks: Task-related fMRI study. Scientific Reports. 2019;9(1):15777. doi: 10.1038/s41598-019-52296-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derevensky JL, Hayman V, Gilbeau L. Behavioral addictions: Excessive gambling, gaming, Internet, and smartphone use among children and adolescents. Pediatric Clinics of North America. 2019;66(6):1163–1182. doi: 10.1016/j.pcl.2019.08.008. [DOI] [PubMed] [Google Scholar]
- Du YS, Jiang W, Vance A. Longer term effect of randomized, controlled group cognitive behavioural therapy for Internet addiction in adolescent students in Shanghai. Australian & New Zealand Journal of Psychiatry. 2010;44(2):129–134. doi: 10.3109/00048670903282725. [DOI] [PubMed] [Google Scholar]
- Duong XL, Liaw SY, Augustin J. How has Internet addiction been tracked over the last decade? A literature review and 3C paradigm for future research. International Journal of Preventive Medicine. 2020;11:175. doi: 10.4103/ijpvm.IJPVM_212_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faghani N, Akbari M, Hasani J, Marino C. An emotional and cognitive model of problematic Internet use among college students: The full mediating role of cognitive factors. Addictive Behaviors. 2020;105:106252. doi: 10.1016/j.addbeh.2019.106252. [DOI] [PubMed] [Google Scholar]
- Foell J, Klawohn J, Bruchnak A, Brush CJ, Patrick CJ, Hajcak G. Ventral striatal activation during reward differs between major depression with and without impaired mood reactivity Psychiatry Research. Neuroimaging. 2021;313:111298 . doi: 10.1016/j.pscychresns.2021.111298. [DOI] [PubMed] [Google Scholar]
- Gao T, Meng X, Qin Z, Zhang H, Gao J, Kong Y, Hu Y, Mei S. Association between parental marital conflict and internet addiction: A moderated mediation analysis. Journal of Affective Disorders. 2018;240:27–32. doi: 10.1016/j.jad.2018.07.005. [DOI] [PubMed] [Google Scholar]
- Garner B. Research on the diffusion of evidence-based treatments within substance abuse treatment: A systematic review. Journal of Substance Abuse Treatment. 2009;36(4):376–399. doi: 10.1016/j.jsat.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyer, K., Ellis, D. A., Shaw, H., & Davidson, B. I. (2021). Open-source smartphone app and tools for measuring, quantifying, and visualizing technology use. Behavior Research Methods,1–12,. 10.3758/s13428-021-01585-7 [DOI] [PMC free article] [PubMed]
- Gholamian B, Shahnazi H, Hassanzadeh A. The effect of educational intervention based on BASNEF model for reducing internet addiction among female students: A quasi-experimental study. Italian Journal of Pediatrics. 2019;45(1):164. doi: 10.1186/s13052-019-0761-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez P, Rial A, Braña T, Golpe S, Varela J. Screening of problematic Internet use among Spanish adolescents: Prevalence and related variables. Cyberpsychology, Behavior and Social Networking. 2017;20(4):259–267. doi: 10.1089/cyber.2016.0262. [DOI] [PubMed] [Google Scholar]
- Hulley SB, Cummings SR, Browner WS, Grady DG, editors. Designing clinical research. 3. Lippincott Williams & Wilkins; 2007. [Google Scholar]
- Li H, Jin R, Yuan K, Zheng B, Zheng Z, Luo Y, Ye H, Huang B, Zhu T. Effect of electro-acupuncture combined with psychological intervention on mental symptoms and P50 of auditory evoked potential in patients with internet addiction disorder. Journal of Traditional Chinese Medicine. 2017;37(1):43–48. doi: 10.1016/s0254-6272(17)30025-0. [DOI] [PubMed] [Google Scholar]
- Internet World Stats - IWS. (2021). Internet users in the world by regions - 2021 MAR. Retrieved August 26 from: https://cms.internations.org/sites/default/files/2019-05/20190522_Digital_Life_Abroad_Report_by_InterNations.pdf
- Ke GN, Wong SF. A healthy mind for problematic internet use. Cyberpsychology, Behavior, and Social Networking. 2018;21(10):637–645. doi: 10.1089/cyber.2018.0072. [DOI] [PubMed] [Google Scholar]
- Ke GN, Wong SF. Outcome of the psychological intervention program: Internet use for youth. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2018;36(2):187–200. doi: 10.1007/s10942-017-0281-3. [DOI] [Google Scholar]
- Khazaei F, Khazaei O, Ghanbari-H B. Positive psychology interventions for Internet addiction treatment. Computers in Human Behavior. 2017;72:304–311. doi: 10.1016/j.chb.2017.02.065. [DOI] [Google Scholar]
- Kim SH, Yim HW, Jo SJ, Jung KI, Lee K, Park MH. The effects of group cognitive behavioral therapy on the improvement of depression and anxiety in adolescents with problematic internet use. Journal of the Korean Academy of Child and Adolescent Psychiatry. 2018;29(2):73–79. doi: 10.5765/jkacap.2018.29.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanthier-Labonté S, Dufour M, Milot DM, Loslier J. Is problematic Internet use associated with alcohol and cannabis use among youth? A Systematic Review. Addictive Behaviors. 2020;106:106331. doi: 10.1016/j.addbeh.2020.106331. [DOI] [PubMed] [Google Scholar]
- Lee SY, Kim MS, Lee HK. Prevention strategies and interventions for Internet use disorders due to addictive behaviors based on an integrative conceptual model. Current Addiction Reports. 2019;6(3):303–312. doi: 10.1007/s40429-019-00265-z. [DOI] [Google Scholar]
- Li, Y. (2019). The role of public authorities in the development of mobility-as-a-service. In The Governance of Smart Transportation Systems (229–245). Springer. 10.1007/978-3-319-96526-0_12
- Li JB, Lau J, Mo P, Su XF, Tang J, Qin ZG, Gross DL. Insomnia partially mediated the association between problematic Internet use and depression among secondary school students in China. Journal of Behavioral Addictions. 2017;6(4):554–563. doi: 10.1556/2006.6.2017.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YY, Sun Y, Meng SQ, Bao YP, Cheng JL, Chang XW, Ran MS, Sun YK, Kosten T, Strang J, Lu L, Shi J. Internet addiction increases in the general population during COVID-19: Evidence from China. The American Journal on Addictions. 2021;30(4):389–397. doi: 10.1111/ajad.13156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin MP, Wu JY, You J, Hu WH, Yen CF. Prevalence of internet addiction and its risk and protective factors in a representative sample of senior high school students in Taiwan. Journal of Adolescence. 2018;62:38–46. doi: 10.1016/j.adolescence.2017.11.004. [DOI] [PubMed] [Google Scholar]
- Lopes FM, Luz WL, Bizarro L. Cognitive-behavioral therapy in the treatment of substance use disorders. In: Andrade ALM, De Micheli D, Silva EA, Lopes FM, Pinheiro B, Reichert RA, editors. Psychology of Substance Abuse Psychotherapy, Clinical Management and Social Intervention. SpringerNature; 2021. pp. 139–154. [Google Scholar]
- Malak MZ, Khalifeh AH. Anxiety and depression among school students in Jordan: Prevalence, risk factors, and predictors. Perspectives in Psychiatric Care. 2018;54(2):242–250. doi: 10.1111/ppc.12229. [DOI] [PubMed] [Google Scholar]
- Manuel JK, Hagedorn HJ, Finney JW. Implementing evidence-based psychosocial treatment in specialty substance use disorder care. Psychology of Addictive Behaviors. 2011;25(2):225–237. doi: 10.1037/a0022398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag, C., & Rumpf, H. J. (2021). The Potential of Digital Phenotyping and Mobile Sensing for Psycho-Diagnostics of Internet Use Disorders. Current Addiction Reports, 1–9. 10.1007/s40429-021-00376-6 [DOI] [PMC free article] [PubMed]
- Murray CH, Christian DT, Milovanovic M, Loweth JA, Hwang EK, Caccamise AJ, Funke JR, Wolf ME. mGlu5 function in the nucleus accumbens core during the incubation of methamphetamine craving. Neuropharmacology. 2021;186:108452. doi: 10.1016/j.neuropharm.2021.108452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasir M, Trujillo D, Levine J, Dwyer JB, Rupp ZW, Bloch MH. Glutamate systems in DSM-5 anxiety disorders: Their role and a review of glutamate and GABA psychopharmacology. Frontiers in Psychiatry. 2020;11:548505 . doi: 10.3389/fpsyt.2020.548505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-A web and mobile app for systematic reviews. Systematic Reviews. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinones C, Griffiths MD. Reducing compulsive Internet use and anxiety symptoms via two brief interventions: A comparison between mindfulness and gradual muscle relaxation. Journal of Behavioral Addictions. 2019;8(3):530–536. doi: 10.1556/2006.8.2019.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, T. (2020). Psychological and exercise interventions for teenagers with internet addiction disorder. Revista Argentina de Clínica Psicológica, 29(2), 226–231. 10.24205/03276716.2020.228
- Pan YC, Chiu YC, Lin YH. Systematic review and meta-analysis of epidemiology of Internet addiction. Neuroscience and Biobehavioral Reviews. 2020;118:612–622. doi: 10.1016/j.neubiorev.2020.08.013. [DOI] [PubMed] [Google Scholar]
- Perry CJ, Lawrence AJ. Addiction, cognitive decline and therapy: Seeking ways to escape a vicious cycle. Genes, Brain and Behavior. 2017;16:205–218. doi: 10.1111/gbb.12325. [DOI] [PubMed] [Google Scholar]
- Saletti, S. M. R., Van den Broucke, S., & Chau, C. (2021). The effectiveness of prevention programs for problematic Internet use in adolescents and youths: A systematic review and meta-analysis. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 15(2). 10.5817/CP2021-2-10
- Santos, V., Freire, R., Zugliani, M., Cirillo, P., Santos, H. H., Nardi, A. E., & King, A. L. S. (2017). Treatment outcomes in patients with Internet addiction and anxiety. Medical Express, 4(2). 10.5935/MedicalExpress.2017.02.06
- Shapira NA, Lessig MC, Goldsmith TD, Szabo ST, Lazoritz M, Gold MS, Stein DJ. Problematic internet use: Proposed classification and diagnostic criteria. Depression and Anxiety. 2003;17(4):207–216. doi: 10.1002/da.10094. [DOI] [PubMed] [Google Scholar]
- Spada MM. An overview of problematic Internet use. Addictive Behaviors. 2014;39(1):3–6. doi: 10.1016/j.addbeh.2013.09.007. [DOI] [PubMed] [Google Scholar]
- Stieger S, Lewetz D. A week without using social media: Results from an ecological momentary intervention study using smartphones. Cyberpsychology, Behavior, and Social Networking. 2018;21(10):618–624. doi: 10.1089/cyber.2018.0070. [DOI] [PubMed] [Google Scholar]
- Spritzer, D. T., Andrade, A. L. M., Xavier, A. Z., da Silva, G. T., Kim, H. S., Kaliszewska-Czeremska, K., … & Hauck, S. (2022). The Self-perception of Text message Dependence Scale (STDS): A Brazilian-Portuguese validation and expansion of its psychometric properties. Current Psychology,1–12,. 10.1007/s12144-022-02957-8 [DOI] [PMC free article] [PubMed]
- Tabatabaee, H. R., Rezaianzadeh, A., & Jamshidi, M. (2018). Mediators in the relationship between Internet addiction and body mass index: A path model approach using partial least square. Journal of research in health sciences, 18(3). [PMC free article] [PubMed]
- Tas, İ., & Ayas, T. (2018). Effects of psychoeducational program for reducing psychological symptoms on Internet addiction among adolescents. Egitim ve Bilim, 43(196). 10.15390/EB.2018.7652
- Thorens, G., Achab, S., Billieux, J., Khazaal, Y., Khan, R., Pivin, E., … & Zullino, D. (2014). Characteristics and treatment response of self-identified problematic Internet users in a behavioral addiction outpatient clinic. Journal of Behavioral Addictions,3(1), 78–81. 10.1556/JBA.3.2014.008 [DOI] [PMC free article] [PubMed]
- Tumeleiro, L. F., Costa, A. B., DebastianiHalmenschlager, G., Garlet, M., e Schmitt, J. (2018). Dependência de internet: um estudo com jovens do último ano do ensino médio. Gerais: Revista Interinstitucional de Psicologia, 11(2), 279–293. 10.36298/gerais2019110207
- Vukosavljevic-Gvozden T, Filipovic S, Opacic G. The mediating role of symptoms of psychopathology between irrational beliefs and internet gaming addiction. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2015;33(4):387–405. doi: 10.1007/s10942-015-0218-7. [DOI] [Google Scholar]
- Wang W, Li D, Li X, Wang Y, Sun W, Zhao L, Qiu L. Parent-adolescent relationship and adolescent internet addiction: A moderated mediation model. Addictive Behaviors. 2018;84:171–177. doi: 10.1016/j.addbeh.2018.04.015. [DOI] [PubMed] [Google Scholar]
- Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R, ROBIS group, ROBIS: A new tool to assess risk of bias in systematic reviews was developed. Journal of Clinical Epidemiology. 2016;69:225–234. doi: 10.1016/j.jclinepi.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler A, Dörsing B, Rief W, Shen Y, Glombiewski JA. Treatment of internet addiction: A meta-analysis. Clinical Psychology Review. 2013;33(2):317–329. doi: 10.1016/j.cpr.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Yang Y, Li H, Chen XX, Zhang LM, Huang BJ, Zhu TM. Electro-acupuncture treatment for internet addiction: Evidence of normalization of impulse control disorder in adolescents. Chinese Journal of Integrative Medicine. 2017;23(11):837–844. doi: 10.1007/s11655-017-2765-5. [DOI] [PubMed] [Google Scholar]
- Yang J, Guo Y, Du X, Jiang Y, Wang W, Xiao D, Wang T, Lu C, Guo L. Association between problematic Internet use and sleep disturbance among adolescents: The role of the child's sex. International Journal of Environmental Research and Public Health. 2018;15(12):2682. doi: 10.3390/ijerph15122682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young KS. CBT-IA: The first treatment model for Internet addiction. Journal of Cognitive Psychotherapy. 2011;25(4):304–312. doi: 10.1891/0889-8391.25.4.304. [DOI] [Google Scholar]
- Young, K. S. (2013). Treatment outcomes using CBT-IA with Internet-addicted patients. Journal of Behavioral Addictions, 2(4), 209–215. 10.1556/JBA.2.2013.4.3 [DOI] [PMC free article] [PubMed]
- Zhu TM, Li H, Jin RJ, Zheng Z, Luo Y, Ye H, Zhu HM. Effects of electro-acupuncture combined psycho-intervention on cognitive function and event-related potentials P300 and mismatch negativity in patients with internet addiction. Chinese Journal of Integrative Medicine. 2012;18(2):146–151. doi: 10.1007/s11655-012-0990-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.