Abstract
Objective:
How couples communicate about cancer is an important predictor of psychological outcomes for men diagnosed with localised prostate cancer and their spouses. We examined the predictive role of disclosure, responsiveness, mutual avoidance, and holding back on depressive symptoms, psychological adjustment, cancer-specific distress, and cancer concerns.
Methods:
Eighty-one prostate cancer patients and their spouses completed measures of communication at baseline and measures of four psychological outcomes at baseline, five, 12, and 26 weeks after baseline. Dyadic growth models tested the effects of time and role on each outcome over time.
Results:
Higher disclosure and responsiveness predicted better psychological outcomes. Less mutual avoidance and holding back predicted poorer psychological outcomes. Across communication variables, individuals who engaged in poorer communication initially had poorer psychological outcomes that improved over time, whereas individuals who engaged in better communication initially maintained their more positive standing without change or changed in the positive direction. For all outcomes, those with better communication still had better psychological outcomes at six months.
Conclusion:
Couples’ cancer-specific relationship communication predicts their psychological outcomes. More research is needed to identify effective interventions, including a longer therapy course, individual communication training, or greater focus on addressing barriers to sharing and responsiveness.
Keywords: cancer, marital relationship, prostate cancer, relationship communication
1 |. INTRODUCTION
Along with the practical and emotional stressors that accompany the diagnosis of any type of cancer, current medical treatments for localised prostate cancer typically result in adverse long-term side-effects that can pose a challenge to the patient, partner, and their relationship. These long-term adverse side-effects include impaired erectile function, urinary incontinence, problematic bowel function and loss of libido (Burnett et al., 2007; Erim et al., 2019; Gacci et al., 2009; O’Shaughnessy et al., 2013; Penson et al., 2005; Salazar et al., 2019). Localised prostate cancer is also associated with elevated distress. Cross-sectional studies suggest that men diagnosed with localised prostate cancer report lower health-related quality of life and higher distress than men from the general population (Friberg et al., 2019; Love et al., 2008; Mols et al., 2006; Oba et al., 2017; van Stam et al., 2017). During the first 2 years after diagnosis, estimates of elevated depressive symptoms range from 15% to 38% of patients, and levels of anxiety range from 15% to 27% (e.g. Cliff & MacDonagh, 2000; Erim et al., 2019; Trinchieri et al., 2005; Watts et al., 2014). Longitudinal studies suggest that depressive symptoms steadily decline after the first year after diagnosis (Erim et al., 2019). Partners’ distress and quality of life are also adversely affected. Rates of depression and anxiety among partners are higher than the general population (e.g. (Couper et al., 2006; Garos et al., 2007; Oba et al., 2017), and 12.4%–22% of partners report elevated depression and/or anxiety (Couper et al., 2006; Soloway et al., 2005; Street et al., 2010). Indeed, some studies indicate that partners’ levels of anxiety and depression are higher, and quality of life is lower, than that reported by patients (Chien et al., 2018; Cliff & MacDonagh, 2000; Eton & Lepore, 2002; Kornblith et al., 1994; Soloway et al., 2005; Song et al., 2011). Similar to patients, studies suggest that partners’ anxiety and depression decline over time (Couper et al., 2006).
How couples communicate about cancer is an important predictor of psychological and relationship outcomes for both patients and partners (Manne & Badr, 2008). Unfortunately, some couples dealing with prostate cancer struggle to communicate openly and constructively about their concerns (Badr & Taylor, 2009; Haun et al., 2014; Manne et al., 2010, 2015). Holding back sharing cancer-related concerns, particularly concerns about sex and cancer recurrence, is relatively common among couples coping with prostate cancer (Manne et al., 2015). The relationship intimacy model of couple adaptation (Manne & Badr, 2008) describes a framework for how couples communication behaviours influence their relationship and psychological outcomes. The model proposes intimacy-enhancing communication (e.g. self-disclosure/open communication, responsiveness and relationship engagement) and intimacy-compromising communication (criticism, avoidance/holding back sharing, demand-withdraw communication). Research has supported the role of relationship-enhancing communication among couples coping with cancer, with studies suggesting that self-disclosure (Haun et al., 2014; Manne & Badr, 2010; Manne et al., 2018), perceived partner disclosure, perceived partner responsiveness and constructive and open communication (Badr & Taylor, 2009; Gotcher et al., 1995; Manne & Badr, 2010; Song et al., 2016), as well as observed behaviours such as humour (Manne et al., 2004) are associated with psychological and/or relationship outcomes. Relationship-compromising communication including self-reported mutual avoidance (Manne & Badr, 2010), holding back sharing concerns (Manne & Badr 2010) and pressure-withdraw interactions (Manne & Badr, 2010).
The goal of the current study was to evaluate couples’ communication about cancer as a predictor of their psychological outcomes. The cancer-specific relationship-enhancing communications we studied were self-disclosure, perceived partner disclosure and perceived responsiveness (Manne & Badr, 2008). We selected these communication behaviours because our prior work has illustrated that these behaviours are associated with both patient and partner psychological outcomes (Badr & Taylor, 2009; Gotcher, 1995; Haun et al., 2014; Manne et al., 2010, 2018; Song et al., 2016). Cancer-specific relationship-compromising processes we studied were holding back and mutual avoidance of discussing cancer-related issues. We focused on these relationship communication behaviours because our prior cross-sectional work illustrated that holding back (Manne et al., 2015) and mutual avoidance of talking about cancer were associated with patients’ and partners’ distress and well-being (Manne et al., 2015).
This study extends prior research in three ways. First, we examined specific relationship-enhancing and compromising communication behaviours using longitudinal data. Prior longitudinal studies evaluating relationship factors have assessed general relationship satisfaction (Chien et al., 2018; Harju et al., 2018; Ross et al., 2016) or general open communication (Song et al., 2011, 2016) but have not evaluated cancer-specific communication such as disclosure of cancer concerns, holding back sharing cancer concerns, and mutual avoidance of discussing cancer concerns. By assessing the role of cancer-specific communication behaviours such as mutual avoidance of discussing cancer concerns and holding back sharing concerns, we can obtain insight into specific communication behaviours to target in couple-focused interventions. Second, we evaluated the predictive role of relationship communication in one’s own psychological outcomes (actor effects) and one’s partner’s psychological outcomes (partner effects). There is limited longitudinal research evaluating actor and partner effects of couples’ communication on psychological and relationship outcomes. Third, we assessed a broad range of psychological outcomes, including cancer concerns. Prior longitudinal work on couples’ communication in the prostate cancer context has not included a broad range of psychological and relationship outcomes, and prior work has not included cancer concerns as an outcome.
This study had two aims. The first aim was to characterise changes in couples’ depressive symptoms, general psychological adjustment, cancer-specific distress and cancer-related concerns over a 6 month period. The second aim was to examine whether baseline relationship-enhancing and compromising communication predicts their own and their partner’s depressive symptoms, general psychological adjustment, cancer-specific distress and cancer-related concerns over this time period.
2 |. METHODS
2.1 |. Participants
Participants were men diagnosed with prostate cancer and their partners who were randomised into the Usual Care (UC) arm of a clinical trial of an intimacy-enhancing intervention (Manne et al., 2018). Participants were recruited from cancer centres in the Northeastern and Midwestern US. Eligibility criteria for patients were (a) diagnosed with localised prostate cancer; (b) underwent surgery or initiated radiation or androgen deprivation therapy within 18 months; and (c) married or cohabitating with partners (male or female) for ≥1 year. Additionally, patients and partners had to (a) be ≥18 years old, (b) speak and read English and (c) live within a 1-hr commuting distance to the recruitment site. Finally, couples were eligible if either the patient or partner reported at least mild-moderate distress as evidenced by a score of ≥16 for the patient or ≥17 for the partner on the Impact of Events Scale (IES) (Horowitz et al., 1979). This eligibility criterion was selected because the intimacy-enhancing intervention pilot intervention study that formed the basis of the larger intervention trial illustrated that the intervention was more effective for couples with greater baseline distress (Manne et al., 2011). Exclusion criteria were (a) the patient or partner has another cancer diagnosis (except non-melanoma skin cancer) and is in active treatment for that cancer, and (b) the patient or partner had a significant hearing impairment that could hinder participation in the intervention.
The current study analysed data obtained from the Usual Care arm within a clinical trial evaluating Usual Care with two couple-focused interventions. Acceptance into the parent intervention study which included all study arms was 15.2% (Manne et al., 2019). Participants consisted of 81 couples randomised to the UC arm of the trial. Participants completed measures at baseline, 5, 12 and 26 weeks after baseline. Of the 81 couples completing baselines, 70 patients and 70 spouses completed the 5-week survey, 73 patients and 72 spouses completed the 12-week survey, and 70 patients and 68 spouses completed the 26-week survey.
2.2 |. Procedures
Recruitment was conducted by letter, telephone or in person. After confirming eligibility, a written informed consent and questionnaire were sent. Participants signed an informed consent form approved by an Internal Review Board. Participants were considered ‘refusers’ if 3 months elapsed since the consent and questionnaire were sent without a response. Couples who did not return surveys at two adjacent time points were not sent any further surveys.
2.3 |. Outcome measures
2.3.1 |. Depressive symptoms
The Patient Health Questionnaire-9 (PHQ-9) is the 9-item depression module from the full PHQ (Kroenke et al., 2001; Spitzer et al., 2000). It has been widely used to assess depressive symptoms in cancer patients (Hartung et al., 2019; Hinz et al., 2016) and has cut-offs for mild (0–9), moderate (10–14) and severe depression (15–27). Coefficient alphas across waves ranged from 0.80 to 0.87.
2.3.2 |. Psychological adjustment
The Mental Health Inventory-38 (Veit & Ware, 1983) is a 38-item measure assessing psychological adjustment and used before in this setting (Manne et al., 2010). Coefficient alphas across waves ranged from 0.94 to 0.96.
2.3.3 |. Cancer-specific distress
The Impact of Events Scale (Horowitz et al., 1979), a 15-item scale measuring the severity of intrusive thoughts, worries and feelings about having (or one’s spouse having) cancer, avoidance and numbing; it has been used before in this setting (Manne et al., 2010). Coefficient alpha across waves ranged from 0.92 to 0.95.
2.3.4 |. Cancer-related concerns
Patients and spouses rated the degree to which they were concerned about ten cancer-related problems (e.g. the couples’ sexual relationship, fear of disease progression, finances) (Manne et al., 2010). Ratings ranged from 1 = not at all concerned to 5 = extremely concerned. Items were averaged within each partner for analyses. Coefficient alpha across waves ranged from 0.80 to 0.89.
2.4 |. Moderator measures
2.4.1 |. Disclosure communication
Six items were adapted from Laurenceau et al. (1998) and assessed the degree to which participants disclosed thoughts and feelings and perceived their partner disclosed thoughts and feelings when discussing cancer-related issues. Items were rated on a 7-point Likert scale (1 = not at all, 7 = very much). An average score was used. Internal consistency was 0.90 for patients and 0.94 for partners.
2.4.2 |. Perceived partner responsiveness
Three items were adapted from Laurenceau et al. (1998) and assessed the degree to which participants felt accepted, understood and cared for when discussing cancer-related issues. Items were rated on a 7-point Likert scale (1 = not at all, 7 = very much). An average score was used. Internal consistency was 0.90 for patients and 0.94 for partners.
2.4.3 |. Holding back
Holding back sharing concerns about cancer-related problems was assessed for patients and partners via a 10-item measure adapted from Pistrang and Barker (1995). Concerns included problems with physical symptoms, sexual function and cancer treatment. Ratings were on a 6-point Likert scale (0 = not at all, 5 = a lot). Internal consistency was 0.88 for patients and 0.87 for partners.
2.4.4 |. Mutual avoidant communication
The Mutual Avoidance subscale of the Communication Patterns Questionnaire (CPQ) (Christensen, 1988; Christensen & Sullaway, 1984; Heavey et al., 1993) was used. The scale contains three items rated on a 9-point Likert scale (1 = very unlikely, 9 = very likely). Internal consistency was 0.69 for patients and 0.68 for partners.
2.5 |. Covariates
2.5.1 |. Demographic and medical factors
Patients and partners completed questionnaires assessing age, sex, ethnicity, education, occupation, employment status, annual income and relationship length. Cancer stage was collected from medical chart.
2.5.2 |. Bowel function
The Prostate Cancer Index (Litwin et al., 1998) is a widely used measure that asssesses changes in bowel function (Davis et al., 2001). Higher scores indicate worse functioning. The internal consistency was 0.71.
2.6 |. Data analytic approach
Multilevel modelling (MLM; SPSS Version 24) with restricted maximum likelihood was used to estimate dyadic growth models testing the effects of time and role (Patient = 1, Spouse = −1; the term spouse is used for the partner regardless of marital status to avoid confusion with the partner effect in the Actor-Partner Interdependence Model or APIM; (Kenny et al., 2006) on each of the four outcomes. Time was coded as months since baseline and was grand-mean centred. Covariates included in all analyses were grand-mean centred and included the person’s age, relationship length, cancer stage and bowel functioning. Random effects included separate intercept variances for patients and spouses, a correlation between the intercepts, separate slope variances of time for patients and spouses, a correlation between the slopes, and separate residual variances for patients and spouses, and a correlation between the residuals. For depressive symptoms, the model that included random slopes did not converge to an admissible solution and so, for that outcome only, random intercepts and residuals were included. We considered four moderating variables including both partners’ baseline perceived disclosure, baseline perceived partner responsiveness, baseline mutual avoidant communication and baseline holding back sharing concerns.
When baseline disclosure communication, perceived partner responsiveness, mutual avoidant communication and holding back were treated as moderators, we used an APIM framework for the analysis. That is, each moderation model included both the person’s own value on the moderator (i.e. the actor effect) as well as the partner’s value on the moderator (i.e. the partner effect). Moderator variables were grand-mean centred. Thus, each moderation model included time, role and both actor and partner values for the moderators. All main effects and interactions between these variables were included in the models, with the exception that we did not specify any actor-moderator by partner-moderator interactions. Significant interactions were followed by simple slopes analyses at one standard deviation above and below the mean for the moderator.
3 |. RESULTS
3.1 |. Characteristics of the study sample
Most patients were white (76.5%), employed full-time (66.7%), had a Gleason score of 7 (69.1%), diagnosed with Stage 2 cancer (76.7%) and underwent only surgery (87.7%) (see Table 1). Most partners were white (72.8%) and employed full-time (51.9%). Patients reported an average age of 61, and partner age averaged 58 years. Table 2 presents the means, standard deviations, and correlations among variables. For the purposes of this table, each outcome score was averaged over time prior to computing the correlations.
TABLE 1.
Descriptive information for study sample
| Role |
||
|---|---|---|
| Patient |
Spouse |
|
| Variable | M (SD) | M (SD) |
| Age (years) | 61.2 (7.6) | 57.6 (8.8) |
| Relationship length (years) | 26.9 (13.5) | 29.6 (12.6) |
| Time since treatment (months) | 8.68 (6.9) | |
| N (%) | N (%) | |
| Gender | ||
| Male | 81 (100) | 1 (1.2) |
| Female | 0 (0) | 80 (98.8) |
| Race | ||
| White, non-hispanic | 62 (76.5) | 59 (72.8) |
| Black, non-hispanic | 17 (21.0) | 17 (20.9) |
| Asian | 1 (1.2) | 1 (1.2) |
| Hispanic | 1 (1.2) | 1 (1.2) |
| Native Hawaiian/PA | 0 (0) | 1 (1.2) |
| Missing | 0 (0) | 2 (2.5) |
| Employment | ||
| On leave/unemployed | 1 (1.2) | 2 (2.5) |
| Part-time | 4 (4.9) | 8 (9.9) |
| Full-time | 54 (66.7) | 42 (51.9) |
| Retired | 17 (21.0) | 19 (23.5) |
| Missing | 2 (1.2) | 7 (8.6) |
| Education | ||
| <HS | 18 (22.2) | 14 (17.3) |
| Some college | 12 (15.2) | 12 (14.8) |
| College degree | 21 (25.9) | 15 (18.5) |
| >College | 32 (39.5) | 48 (59.3) |
| Income (median) | $158,000 | $158,000 |
| Treatment | ||
| Surgery | 71 (87.7) | |
| Radiation | 8 (9.9) | |
| Both | 2 (2.5) | |
| Gleason Score | ||
| 6 | 16 (19.8) | |
| 7 | 56 (69.1) | |
| 8 | 2 (2.5) | |
| 9 | 7 (8.6) | |
| Stage | ||
| 1 | 5 (6.2) | |
| 2 | 54 (76.7) | |
| 3 | 22 (27.2) | |
TABLE 2.
Correlations, means and standard deviations for the study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Avg. Depression | 0.23 * | 0.76** | 0.35** | 0.32** | −0.31** | −0.09 | −0.20 | 0.01 | −0.05 | −0.23* | 0.10 | 0.31** |
| 2. Avg. Psy. Adjustment | −0.75** | 0.24 * | −0.48** | −0.32** | 0.21 | 0.02 | 0.22 | −0.01 | 0.15 | 0.41** | −0.31** | −0.46** |
| 3. Avg. Cancer Distress | 0.61** | −0.59** | 0.22 | 0.47** | −0.18 | −0.13 | 0.09 | −0.19 | 0.01 | −0.10 | 0.31** | 0.40** |
| 4. Avg. Cancer Concerns | 0.56** | −0.48** | 0.56** | 0.39** | −0.25* | −0.01 | −0.03 | −0.16 | 0.11 | −0.02 | 0.16 | 0.27* |
| 5. Age | −0.18 | 0.19 | −0.26* | −0.12 | 0.81** | 0.54** | 0.18 | −0.06 | −0.18 | 0.14 | −0.21 | −0.33** |
| 6. Rel. Length | 0.02 | −0.02 | −0.08 | −0.02 | 0.40** | 1.00 | 0.08 | 0.00 | −0.05 | 0.25* | −0.14 | −0.14 |
| 7. Stage | 0.14 | −0.06 | 0.09 | 0.13 | 0.06 | 0.08 | 1.00 | −0.02 | 0.01 | −0.10 | −0.01 | 0.08 |
| 8. Bowel Function | −0.38** | 0.24* | −0.49** | −0.31** | −0.03 | 0.00 | −0.02 | 1.00 | −0.34** | −0.08 | 0.09 | −0.20 |
| 9. BL Disclosure | −0.20 | 0.18 | −0.05 | −0.10 | −0.00 | 0.07 | −0.02 | −0.12 | 0.23 * | 0.36** | −0.20 | −0.04 |
| 10. BL Perceived Responsiveness | −0.27* | 0.27* | 0.25* | 0.26* | 0.21 | 0.20 | −0.21 | 0.09 | 0.39** | 0.44 ** | −0.38** | −0.30** |
| 11. BL Mutual Avoid. | 0.15 | −0.26* | 0.24* | 0.28* | −0.18 | −0.26* | 0.05 | −0.17 | −0.20 | −0.58** | 0.31 ** | 0.40** |
| 12. BL Holding Back | 0.31** | −0.30** | 0.32** | 0.51** | −0.19 | −0.07 | 0.00 | −0.11 | −0.28* | −0.33** | 0.32** | 0.19 |
| Patient | ||||||||||||
| M | 3.63 | 183.75 | 18.37 | 2.24 | 61.19 | 26.95 | 3.01 | 15.33 | 4.95 | 6.24 | 6.41 | 1.78 |
| SD | 3.10 | 20.39 | 16.21 | 0.77 | 7.57 | 13.49 | 0.81 | 2.95 | 1.82 | 1.09 | 3.85 | 0.77 |
| Spouse | ||||||||||||
| M | 3.68 | 180.65 | 18.32 | 2.42 | 57.46 | 26.95 | 3.01 | 15.33 | 4.54 | 5.99 | 7.57 | 2.25 |
| SD | 3.46 | 21.42 | 16.38 | 0.64 | 8.24 | 13.49 | 0.81 | 2.95 | 1.82 | 1.34 | 4.81 | 0.94 |
Note: Bolded correlations are those between the patient and spouses scores. Correlations below the diagonal are for patients and those above the diagonal are for spouses. 'Avg’ indicates that the variable was averaged across the four waves of data collection for the purposes of this Table. ‘BL’ indicate that the variable was measured at baseline.
Abbreviations: Avoid., avoidant communication; Rel., relationship.
p < 0.05
p < 0.01.
3.2 |. Basic growth model
Across all four outcomes, the significant main effects of time in the initial growth models (see Table 3) indicate that depressive symptoms, cancer-specific distress and cancer concerns decreased over time and psychological adjustment increased. As indicated by the standardised coefficients, these changes were small to moderate in size. There were no significant role main effects. That is, patients and spouses did not differ on their average outcomes, averaging over time. There was only one significant role by time interaction, which was for psychological adjustment. Simple slopes analyses indicated that although both patients and spouses’ psychological adjustment increased over time, spouses’ adjustment (β = 0.192, b = 1.526, SE = 0.264, t(65) = 5.78, p < 0.001) increased significantly faster than patients’ adjustment (β = 0.107, b = 0.851, SE = 0.252, t(73) = 3.37, p = 0.001). Two covariates, age and bowel function, were significantly associated with most of the outcomes. Across outcomes, older patients reported less negative and more positive outcomes, and patients with better bowel function had lower negative outcomes. Most of the dyadic correlations were not statistically significant. However, patients and spouses were similar in their average levels of cancer concerns and in their time-specific levels of psychological adjustment.
TABLE 3.
Results for basic growth models predicting change in outcomes over time
| Depression | Psych adjustment | Cancer distress | Cancer concerns | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Fixed effects | β | b | SE | β | b | SE | β | b | SE | β | b | SE |
| Intercept | - | 3.60 | 0.27 | - | 182.51 | 1.78 | - | 18.04 | 1.21 | - | 2.32 | 0.06 |
| Time | −0.098 | −0.13** | 0.04 | 0.149 | 1.19** | 0.21 | −0.221 | −1.42** | .18 | −0.145 | −0.04** | 0.01 |
| Role | 0.046 | 0.17 | 0.24 | 0.012 | 0.28 | 1.54 | 0.049 | 0.90 | 1.20 | −0.069 | −0.06 | 0.05 |
| Time × Role | −0.003 | −0.00 | 0.03 | −0.042 | −0.34* | 0.16 | −0.012 | −0.08 | 0.17 | 0.002 | 0.00 | 0.01 |
| Age | −0.249 | −0.12** | 0.04 | 0.228 | 0.65* | 0.25 | −0.242 | −0.55** | 0.17 | −0.177 | −0.02* | 0.01 |
| Relationship length | 0.085 | 0.02 | 0.02 | −0.112 | −0.19 | 0.15 | 0.024 | 0.03 | 0.10 | 0.069 | 0.00 | 0.00 |
| Stage | 0.034 | 0.16 | 0.33 | 0.027 | 0.78 | 2.23 | 0.111 | 2.53 | 1.50 | 0.063 | 0.06 | 0.08 |
| Bowel function | −0.195 | −0.25** | 0.09 | 0.114 | 0.89 | 0.60 | −0.319 | −2.00** | 0.40 | −0.193 | −0.05* | 0.02 |
| Random effects | Patient | Spouse | Patient | Spouse | Patient | Spouse | Patient | Spouse | ||||
| Intercept variance | 6.50** | 10.17** | 370.12** | 424.46** | 160.89** | 234.95** | 0.489** | 0.322** | ||||
| Intercept dyadic r | 0.164 | 0.185 | 0.037 | 0.386** | ||||||||
| Slopes variance | NE | NE | 1.34 | 1.42 | 0.79 | 2.12* | 0.001 | 0.006* | ||||
| Slope dyadic r | NE | 0.304 | 0.029 | 0.563 | ||||||||
| Residual variance | 5.20** | 4.87** | 92.63** | 100.23** | 72.46** | 98.18** | 0.160** | 0.228** | ||||
| Residual dyadic r | 0.130 | 0.272** | 0.093 | −0.027 | ||||||||
Random effects are estimated from the unstandardised model. NE indicates that the variance or correlation was not estimable.
p < 0.05
p < 0.01.
3.3 |. Moderation effects
3.3.1 |. Disclosure communication
Individuals reporting higher disclosure at baseline reported significantly lower average depressive symptoms, β = −0.194, b = 0.436, SE = 0.156, t(142) = 2.80, p = 0.006, and significantly higher average psychological adjustment, β = 0.067, b = 2.772, SE = 1.050, t(143) = 2.64, p = 0.009, across the study. Although disclosure did not predict average cancer-specific distress, there was modest evidence that individuals whose partners reported higher disclosure communication tended to report higher average cancer concerns, β = 0.135, b = 0.068, SE = 0.034, t(135) = 1.99, p = 0.049.
The person’s own baseline disclosure moderated change in both depressive symptoms and psychological adjustment over time. For depressive symptoms, the interaction coefficient was β = 0.067, b = 0.052, SE = 0.022, t(389) = 2.42, p = 0.016. For psychological adjustment, the interaction coefficient was β = −0.049, b = −0.237, SE = 0.112, t(131) = 2.10, p = 0.037. These interactions are presented in Figure 1. When baseline disclosure was low, depressive symptoms were high but decreased significantly over time, β =−0.169, b = −0.219, SE = 0.052, t(308)=4.18, p < 0.001). However, when the person’s baseline disclosure was high, depressive symptoms were lower but did not change over time, β = −0.035, b = −0.046, p = 0.378.
FIGURE 1.
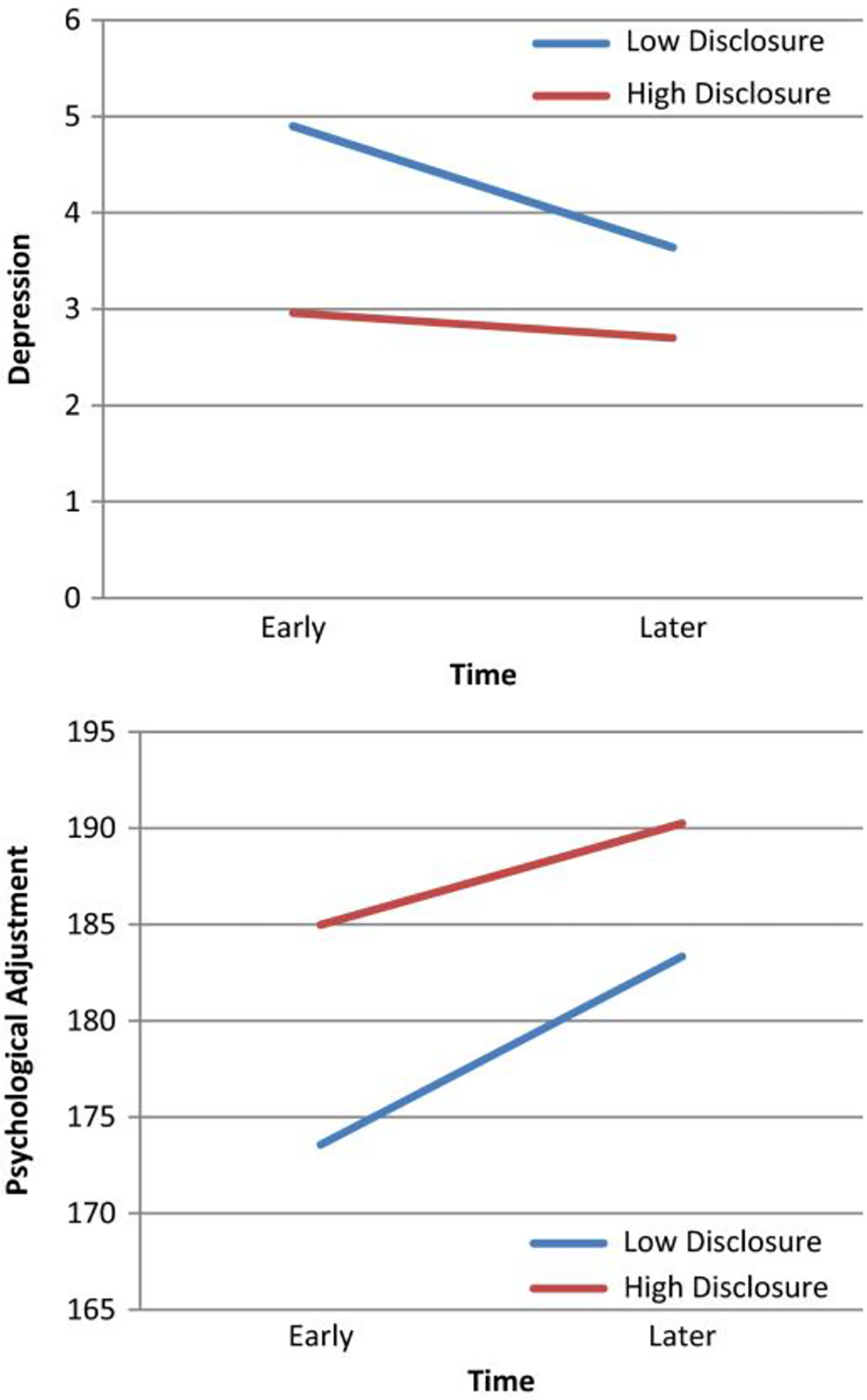
Graph of the interaction between a person’s own baseline disclosure communication (i.e. the actor effect) on changes in depressive symptoms (top panel) and psychological adjustment (bottom panel) over time
For psychological adjustment, individuals reporting low baseline disclosure had lower psychological adjustment than individuals reporting higher baseline disclosure. However, in both cases, there were significant increases in psychological adjustment over time. The increases for individuals reporting low disclosure were higher, β = 0.213, b = 1.698, SE = 0.284, t(90) = 5.97, p < 0.001, than for individuals reporting higher disclosure, β = 0.115, b = 0.916 SE = 0.282, t(109) = 3.25, p = 0.002. There were no associations between actor or partner baseline disclosure and either cancer-specific distress or cancer concerns (beyond the modest partner effect on concerns described earlier).
3.3.2 |. Perceived partner responsiveness
Individuals who reported that their partners were relatively high in responsiveness at baseline reported significantly lower average depression, β = −0.219, b = −0.667, SE = 0.220, t(136) = 3.03, p = 0.003. Responsiveness did not moderate change in depression over time. In contrast, for psychological adjustment there was evidence of both a main effect of responsiveness, β = 0.300, b = 5.616, SE = 1.433, t(132) = 3.92, p < 0.001, such that individuals who reported higher baseline partner responsiveness had higher average adjustment across the study, as well as a significant interaction with time, β = −0.071, b = −0.463, SE = 0.155, t(145) = 2.98, p = 0.003. As shown in Figure 2, although all individuals’ psychological adjustment increased over time, when individuals reported low partner responsiveness, the predicted change over time was larger than that for individuals reporting high responsiveness at baseline (low responsiveness: β = 0.212, b = 1.692, SE = 0.286, t(119) = 5.92, p < 0.001; high responsiveness: β = 0.070, b = 0.561, SE = 0.276, t(109) = 2.04, p = 0.044).
FIGURE 2.
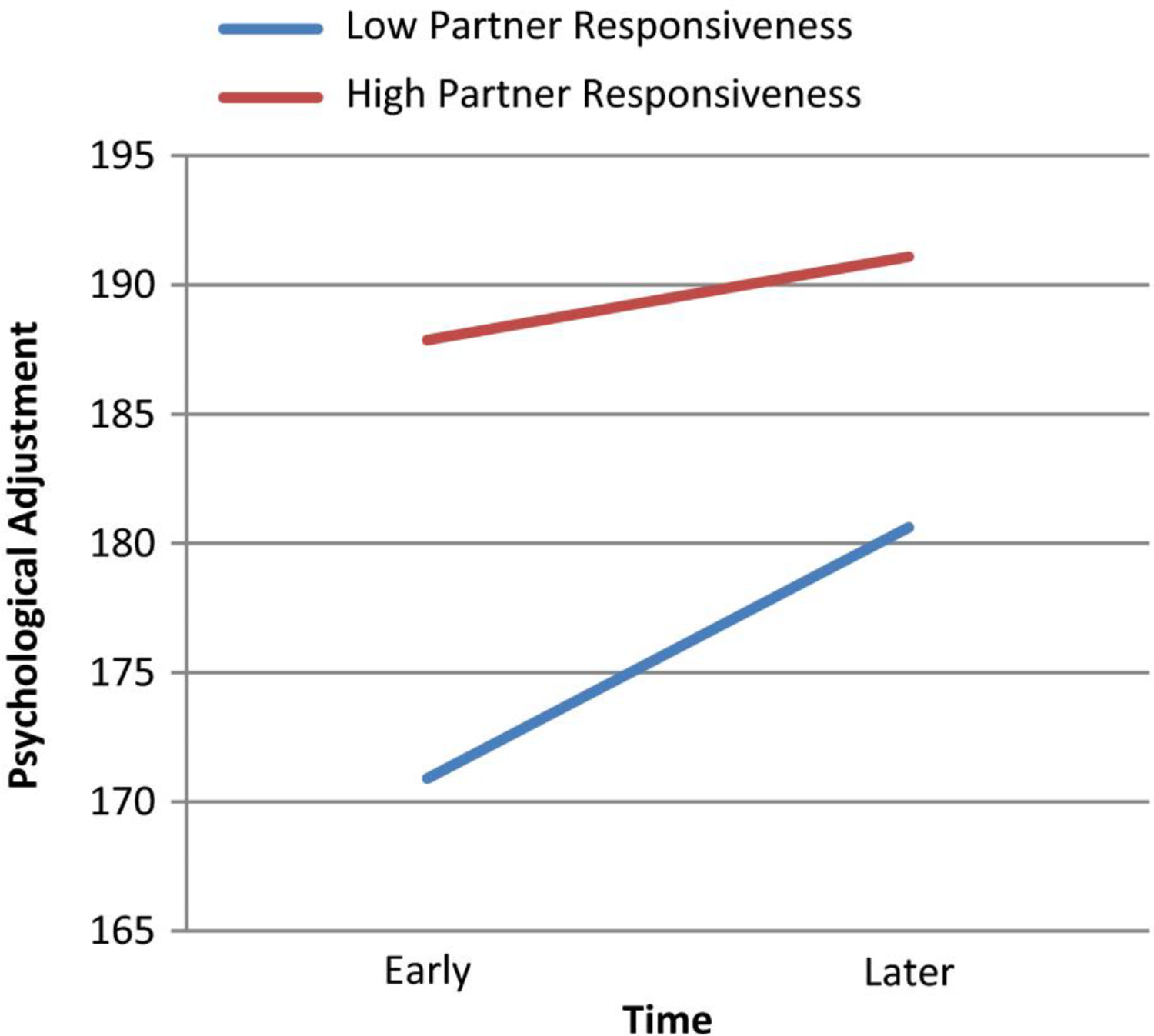
Graph of the interaction between actor’s baseline perceived partner responsiveness and time predicting psychological adjustment
The pattern of results for cancer-specific distress was somewhat different in that there was no evidence of main effects for partner responsiveness, but there were significant interactions between the actor effect for responsiveness and time, β = 0.059, b = 0.307, SE = 0.149, t(133) = 2.06, p = 0.041, as well as for the partner effect for responsiveness and time, β = −0.088, b = −0.461, SE = 0.158, t(109) = 2.91, p = 0.004. As shown in the top panel of Figure 3, the interaction between time and the person’s own perceived partner responsiveness suggests that although distress drops over time for all levels of baseline partner responsiveness, the drop is larger for individuals who perceived lower responsiveness at baseline, β = −0.287, b = −1.833, SE = 0.260, t(106) = 7.05, p < 0.001, than for individuals who perceived higher initial responsiveness, β = −0.170, b = −1.084, SE = 0.264, t(94) = 4.11, p < 0.001. The interaction with the partner effect for partner responsiveness (i.e. the effect of having a partner who perceives the individual as being responsive) is in the bottom panel of Figure 3. Individuals whose partners viewed them as relatively low in responsiveness at baseline decreased in distress over time at a considerably slower rate, β = −0.140, b = −0.895, SE = 0.281, t(93) = 3.18, p = 0.002, than did individuals whose partners viewed them as high in baseline responsiveness, β = −0.316, b = −2.02, SE = 0.259, t(95) = 7.81, p < 0.001. Finally, perceived partner responsiveness did not predict either the average level of cancer concerns or changes in concerns over time.
FIGURE 3.
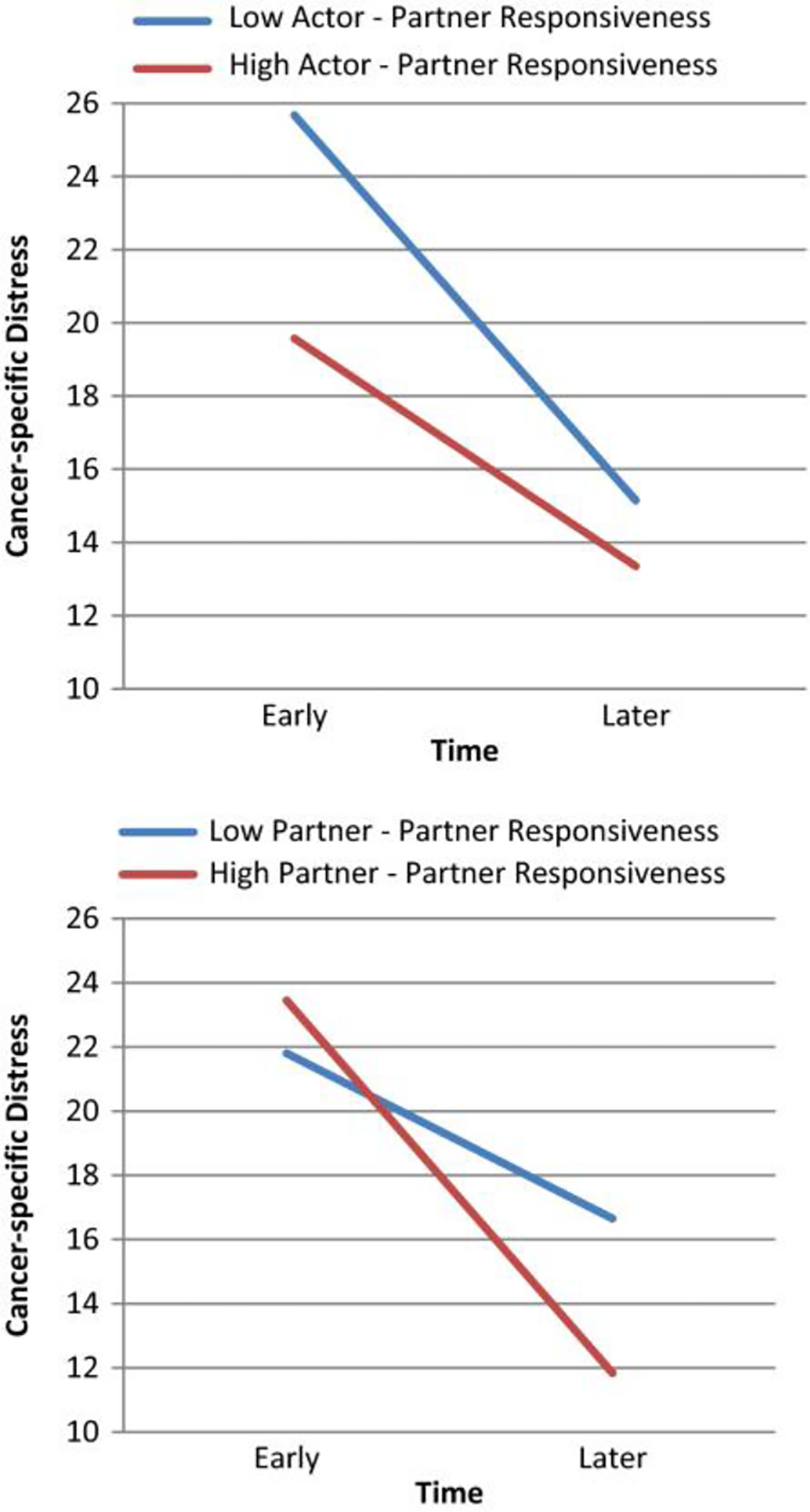
Graph of the interaction between a person’s own baseline perceived partner responsiveness on changes in distress (i.e. actor effect; top panel) and the partner’s baseline perceived partner responsiveness on changes in distress (i.e. partner effect; bottom panel) over time
3.3.3 |. Mutual avoidant communication
Neither actor nor partner effects of mutual avoidant communication predicted depressive symptoms. There were significant main effects of the person’s own avoidant communication on psychological adjustment, β =− .228, b = −1.194, SE = 0.396, t(138) = 3.02, p = 0.003, and cancer concerns, β = 0.165, b = 0.663, SE = 0.289, t(131) = 2.33, p = 0.021. Participants reporting more avoidant communication at baseline reported lower average psychological adjustment and higher average concerns over time. There were no significant interactions between actor or partner mutual avoidant communication on these variables.
There was a significant main effect of actor mutual avoidant communication on cancer-specific distress, β = .158, b = 0.663, SE = 0.289, t(131) = 2.30, p = 0.023, as well as a significant interaction between actor avoidant communication, role and time, β = 0.079, b = 0.115, SE =0.042, t(108) = 2.75, p = 0.007. Simple slopes were computed separately for patients and spouses. The interaction between actor avoidant communication and time occurred only for spouses, β = −0.024, b = −0.153, t(63) = 2.64, p = 0.010. For patients, the interaction coefficient was β = 0.12, b = 0.077, SE = 0.060, t(68) = 11.28, p = 0.207 (see Figure 4). When avoidant communication was low, patient cancer-specific distress declined significantly over time. Although spouse cancer-specific distress was lower on average, it did not change significantly over time. When actor avoidant communication was high, both patients and spouses reported relatively high average distress, and this distress decreased significantly over time for the couple.
FIGURE 4.

Graph of the interaction between actor’s baseline mutual avoidant communication, role and time predicting cancer-specific distress
3.3.4 |. Holding back
Individuals who reported higher holding back at baseline reported higher average depressive symptoms over time, β = 0.206, b = 0.868, SE = 0.297, t(147) = 2.93, p = 0.004. Holding back also moderated change in depressive symptoms over time, β = −0.066, b = −0.096, SE = 0.041, t(399) = 2.33, p = 0.021. Individuals who held back more reported lower average psychological adjustment, β = −0.326, b = −8.430, SE = 1.015, t(142) = 4.40, p < 0.001, and differential change over time, β = 0.066, b = 0.600, SE = 0.210, t(141) = 2.86, p = 0.005. Likewise, actor holding back predicted average cancer-specific distress, β = 0.226, b = 4.690, SE = 1.412, t(144) = 3.32, p = 0.001, and the change in cancer-specific distress over time, β = −0.058, b = −0.422, SE = 0.206, t(140) = 2.04, p = 0.043. As shown in Figure 5, individuals who held back more had more cancer-specific distress or lower psychological adjustment early in the study, but they improved significantly over time. Individuals who did not hold back a great deal initially either maintained their more positive standing without change or changed somewhat, but again in the positive direction.
FIGURE 5.
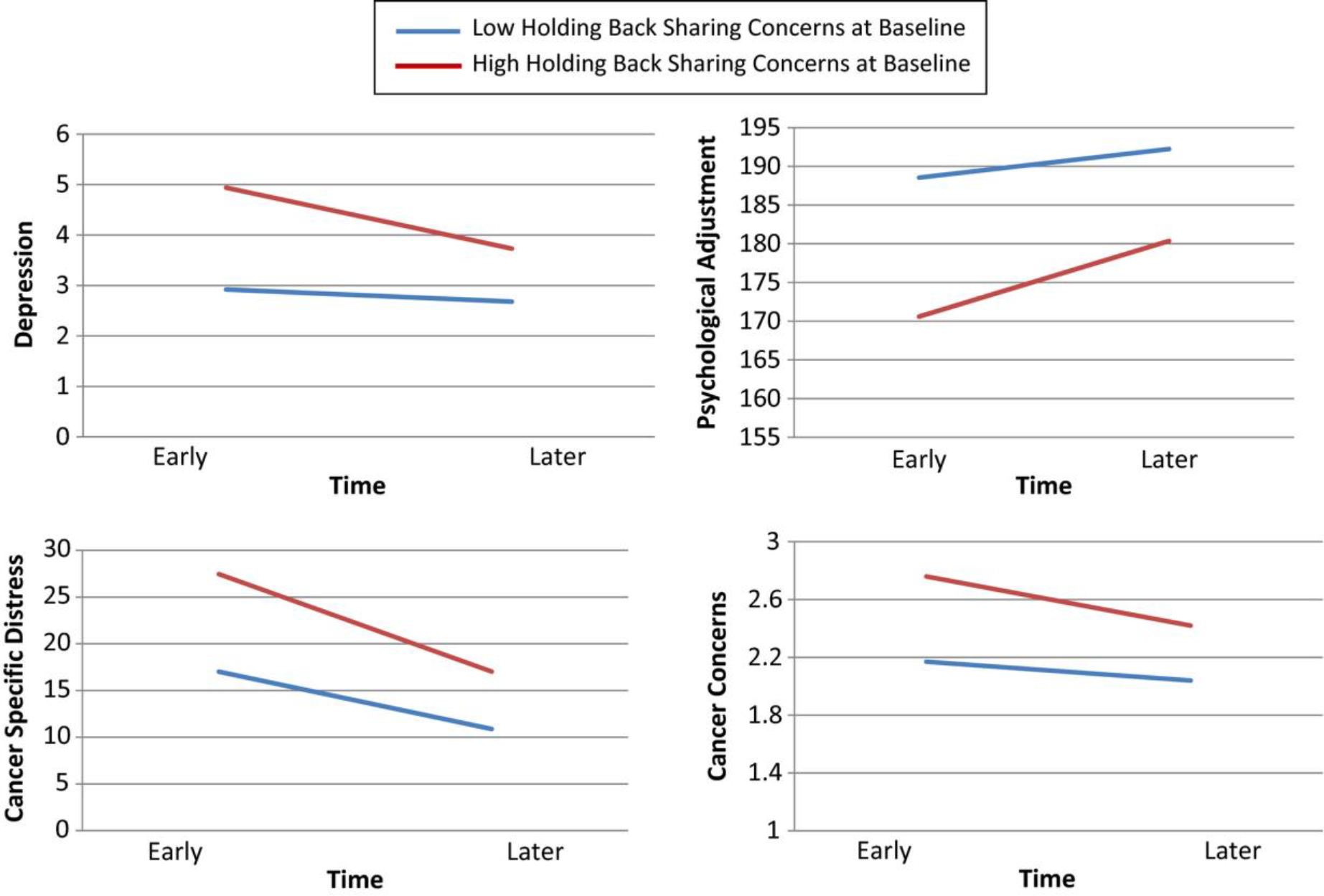
Interactions between a person’s own reports of holding back sharing concerns and time predicting each of the four outcomes
There was a significant main effect of actor holding back at baseline on cancer concerns, β = 0.291, b = 0.272, SE = 0.061, t(140) = 4.48, p < 0.001, as well as a significant actor by role interaction, β = 0.163, b = 0.153, SE = 0.061, t(121) = 2.48, p = 0.015. For patients, the effect of holding back was relatively strong and statistically significant, β = 0.512, b = 0.424, SE = 0.094, t(76) = 4.54, p < 0.001, but it was not significant for spouses, β = 0.144, b = 0.119, SE = 0.079, t(77) = 1.52, p = 0.133. These results suggest that patients who held back more at baseline tended to have higher average cancer concerns. There was also a significant partner effect for holding back, β = 0.188, b = 0.176, SE = 0.060, t(140) = 2.92, p = 0.004. Individuals (both patients and spouses) whose partners reported holding back more at baseline tended to have higher cancer concerns on average. Finally, as with the other three outcomes, there was a significant interaction between actor holding back at baseline and change in cancer concerns over time, β = 0.065, b = 0.021, SE = 0.010, t(134) = 2.21, p = 0.029. These interactions are shown in the lower panel of Figure 5.
4 |. DISCUSSION
The marital relationship is thought to influence the course of psychological outcomes for patient and spouse due to constructive communication occurring between partners. We examined the role of cancer-specific communication in predicting a broad range of general and cancer-specific psychological outcomes and evaluated the course of these outcomes over 6 months after cancer treatment was initiated. Depression, cancer-specific distress and cancer concerns declined and general psychological adjustment improved over time for patients and spouses, with few differences between them. Only spouses’ psychological adjustment increased faster than patients’ adjustment. These findings are consistent with the majority of longitudinal studies of this population which have reported declines in patients’ cancer-specific distress (Bisson et al., 2002; Chambers et al., 2017) and depressive symptoms (Bisson et al., 2002; Erim et al., 2019; Watts et al., 2014) over time. Our findings add to this knowledge base by indicating that patients’ cancer-related concerns decline and general psychological adjustment improves over time. Further, our findings are consistent with the limited literature evaluating longitudinal psychological outcomes among spouses by illustrating that depression and cancer-related distress decline over time (Couper et al., 2006; Oba et al., 2017). While many studies have indicated that spouses are more distressed than patients (Chien et al., 2018; Cliff & MacDonagh, 2000; Eton & Lepore, 2002; Kornblith et al., 1994; Soloway et al., 2005; Song et al., 2011), our findings do not suggest this. One potential explanation for this difference is that our eligibility screening included only couples where at least one partner exhibited elevated cancer distress, which biased the sample towards more distressed couples.
The overall pattern of results suggests that initial cancer-related communication predicts later psychological outcomes. Disclosure communication and partner responsiveness predicted lower depressive symptoms and better psychological adjustment, holding back predicted higher depressive symptoms and cancer-specific distress and lower psychological adjustment, and mutual avoidance predicted lower psychological adjustment and higher cancer concerns over time. These findings are consistent with our prior cross-sectional work in this patient population (Manne et al., 2010, 2015). However, despite predicting that perceived communication would impact one’s partner, there were only two partner effects noted. First, individuals whose partners perceived them as less responsive at baseline decreased in cancer-specific distress over time at a slower rate than individuals whose partners viewed them as more responsive at baseline. Thus, responsiveness has a beneficial impact on the person who is providing the caring, understanding and accepting responses as well as on the person receiving the responsive communication (Manne & Badr, 2008). Our results are consistent with the extensive general psychological literature indicating beneficial psychological effects of providing emotional support in close relationships (e.g. Brown et al., 2008; Morelli et al., 2015). Second, individuals whose partners reported holding back more at baseline reported higher cancer concerns. Our prior cross-sectional work had not suggested partner effects for holding back (Manne et al., 2018). One explanation is that when a partner holds back, the likelihood that the concerns are discussed or addressed by the couple may be reduced and may subsequently result in the person experiencing elevated concerns. In addition, one partner may become aware that other partner is holding back to protect them from upset, which may elevate concerns for that person. Because the measure of holding back does not assess motivations for doing so and we did not ask participants to rate their partner’s concerns, this is only a potential explanation. There were no other partner effects. This is surprising, because our prior cross-sectional work has illustrated partner effects for disclosure on the person’s perceptions of relationship intimacy (Manne et al., 2018).
A consistent pattern for moderation was illustrated for early levels of relationship communication in predicting outcomes. This pattern was most striking and most consistent for holding back sharing concerns. Across all psychological outcomes, when early holding back was high, negative outcomes were high and declined over time, but remained higher than among individuals reporting less holding back, whose negative outcomes were lower and remained lower. A similar pattern was seen for early holding back and psychological adjustment. Individuals who did not hold back either maintained their more positive standing without change or changed somewhat, but in the positive direction. A similar moderator role was seen for disclosure communication in predicting depressive symptoms and psychological adjustment and for partner responsiveness in predicting cancer-specific distress, with both actor and partner effects for higher initial responsiveness on persistently lower cancer-specific distress over time. Taken together, our findings suggest that it would be beneficial for psychosocial care providers to assess these aspects of communication–disclosure communication, responsiveness, holding back and mutual avoidance–early in medical treatment for localised prostate cancer.
It is important to interpret our findings in light of limitations. First, the sample was comprised of couples assigned to the usual care arm of a randomised clinical trial evaluating two types of couple-focused interventions, which may have biased the sample. Couples participating in an intervention trial may differ in their communication and distress. Second, a summary measure of holding back was used. It is possible that holding back sharing sexual concerns and/or other specific concerns played a stronger role in predicting outcomes. Third, as noted in the intervention publication for the larger trial (Manne et al., 2019), refusal was relatively high and may have biased our results. Fourth, differences between the current study and prior couple communication studies may have influenced our findings. Our screening schema included couples where patient, spouse and/or couple included endorsed high cancer distress. Our study included both partners, whereas some prior work focused solely on patient reports (Haun et al., 2014). Some prior work used different measures of couples’ communication (e.g. Song et al., 2016). Fifth, our sample was composed primarily of heterosexual, non-Hispanic white couples and patients who underwent surgery. The findings may have differed if our sample was more heterogeneous with regard to sexual orientation, race/ethnicity and included men who underwent radiation treatment. Sixth, given the strong associations between holding back and outcomes, it will be important to understand couples’ motivations for withholding concerns, as this understanding will foster more effective intimacy-enhancing interventions. Sixth, the study utilised self-report measures of relationship communication which may not reflect actual communication behaviours. Future work may benefit from an observational assessment of couples’ communication. Finally, in our analysis, we chose to analyse the four communication variables separately, as each addresses a different component of spousal communication. An alternative strategy would be to treat the four variables as indicators of a latent variable and then evaluate the communication variable as a single mediator.
In conclusion, couples’ cancer-specific communication appears to predict their psychological outcomes. In contrast, the Intimacy-Enhancing Treatment (IET) offered in the randomised clinical trial which focused on facilitating couples’ disclosure and responsiveness to each other did not show a beneficial impact of IET on these outcomes. Given our current findings suggest that disclosure, responsiveness, holding back and avoidance are associated with the same outcomes, more research is needed to identify effective interventions for this population. These interventions may include a longer course of couples’ therapy, individual communication skills training or a specific focus on overcoming barriers to sharing and responsiveness.
ACKNOWLEDGEMENTS
We would like to thank Sara Frederick, Shira Hichenberg, Luba Popivker, George Olekson and Kristen Sorice for project management, Kara Buda, Katie Darabos, Meghan Eisenberg, Lauren Faust, Travis Logan, Kellie McWilliams, Evangelynn Murphy, Liliana Phan, Danielle Ryan and Caitlin Scally for data collection. We would also like to thank the surgical and radiation oncologists at the study sites.
Funding information
This work was funded by a grant from the National Cancer Institute (R01CA140297) awarded to Sharon Manne, Ph.D.
Footnotes
CONFLICT OF INTEREST
The authors declare they have no conflicts of interest.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Badr H, & Taylor CL (2009). Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psychooncology, 18(7), 735–746. 10.1002/pon.1449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisson JI, Chubb HL, Bennett S, Mason M, Jones D, & Kynaston H (2002). The prevalence and predictors of psychological distress in patients with early localized prostate cancer. BJU International, 90(1), 56–61. 10.1046/j.1464-410x.2002.02806.x [DOI] [PubMed] [Google Scholar]
- Brown SL, Brown RM, House JS, & Smith DM (2008). Coping with spousal loss: Potential buffering effects of self-reported helping behavior. Personality and Social Psychology Bulletin, 34(6), 849–861. 10.1177/0146167208314972 [DOI] [PubMed] [Google Scholar]
- Burnett AL, Aus G, Canby-Hagino ED, Cookson MS, D’Amico AV, Dmochowski RR, Eton DT, Forman JD, Goldenberg SL, Hernandez J, Higano CS, Kraus S, Liebert M, Moul JW, Tangen C, Thrasher JB, & Thompson I (2007). Erectile function outcome reporting after clinically localized prostate cancer treatment. Journal of Urology, 178(2), 597–601. 10.1016/j.juro.2007.03.140 [DOI] [PubMed] [Google Scholar]
- Chambers SK, Ng SK, Baade P, Aitken JF, Hyde MK, Wittert G, Frydenberg M, & Dunn J (2017). Trajectories of quality of life, life satisfaction, and psychological adjustment after prostate cancer. Psychooncology, 26(10), 1576–1585. 10.1002/pon.4342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien CH, Chuang CK, Liu KL, Wu CT, Pang ST, & Chang YH (2018). Positive and negative affect and prostate cancer-specific anxiety in Taiwanese patients and their partners. European Journal of Oncology Nursing, 37, 1–11. 10.1016/j.ejon.2018.09.004 [DOI] [PubMed] [Google Scholar]
- Christensen A (1988). Dysfunctional interaction patterns in couples. In Noller P & Fitzpatrick MA (Eds.), Perspectives on marital interaction (pp. 31–52). Multilingual Matters. [Google Scholar]
- Christensen A, & Sullaway M (1984). Communication patterns questionnaire. University of California, Los Angeles. Unpublished manuscript. [Google Scholar]
- Cliff AM, & MacDonagh RP (2000). Psychosocial morbidity in prostate cancer: II. A comparison of patients and partners. BJU International, 86(7), 834–839. 10.1046/j.1464-410x.2000.00914.x [DOI] [PubMed] [Google Scholar]
- Couper JW, Bloch S, Love A, Duchesne G, Macvean M, & Kissane DW (2006). The psychosocial impact of prostate cancer on patients and their partners. Medical Journal of Australia, 185(8), 428–432. [DOI] [PubMed] [Google Scholar]
- Davis JW, Kuban DA, Lynch DF, & Schellhammer PF (2001). Quality of life after treatment for localized prostate cancer: Differences based on treatment modality. Journal of Urology, 166(3), 947–952. [PubMed] [Google Scholar]
- Erim DO, Bensen JT, Mohler JL, Fontham ETH, Song L, Farnan L, Delacroix SE, Peters ES, Erim TN, Chen RC, & Gaynes BN (2019). Prevalence and predictors of probable depression in prostate cancer survivors. Cancer, 125(19), 3418–3427. 10.1002/cncr.32338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eton DT, & Lepore SJ (2002). Prostate cancer and health-related quality of life: A review of the literature. Psychooncology, 11(4), 307–326. 10.1002/pon.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friberg AS, Dalton SO, Larsen SB, Andersen EW, Krøyer A, Helgstrand JT, Røder MA, Johansen C, & Brasso K (2019). Risk of depression after radical prostatectomy-A nationwide registry-based study. European Urology Oncology, S2588–9311(19), 30101–30104. 10.1016/j.euo.2019.06.020 [DOI] [PubMed] [Google Scholar]
- Gacci M, Simonato A, Masieri L, Gore JL, Lanciotti M, Mantella A, Rossetti MA, Serni S, Varca V, Romagnoli A, Ambruosi C, Venzano F, Esposito M, Montanaro T, Carmignani G, & Carini M (2009). Urinary and sexual outcomes in long-term (5+ years) prostate cancer disease free survivors after radical prostatectomy. Health and Quality of Life Outcomes, 7, 94. 10.1186/1477-7525-7-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garos S, Kluck A, & Aronoff D (2007). Prostate cancer patients and their partners: Differences in satisfaction indices and psychological variables. The Journal of Sexual Medicine, 4(5), 1394–1403. 10.1111/j.1743-6109.2007.00545.x [DOI] [PubMed] [Google Scholar]
- Gotcher JM (1995). Well-adjusted and maladjusted cancer patients: An examination of communication variables. Health Communication, 7(1), 21–33. 10.1207/s15327027hc0701_2 [DOI] [Google Scholar]
- Harju E, Rantanen A, Helminen M, Kaunonen M, Isotalo T, & Astedt-Kurki P (2018). Marital relationship and health-related quality of life of patients with prostate cancer and their spouses: A longitudinal clinical study. Journal of Clinical Nursing, 27(13–14), 2633–2639. 10.1111/jocn.14343 [DOI] [PubMed] [Google Scholar]
- Hartung TJ, Fried EI, Mehnert A, Hinz A, & Vehling S (2019). Frequency and network analysis of depressive symptoms in patients with cancer compared to the general population. Journal of Affective Disorders, 256, 295–301. 10.1016/j.jad.2019.06.009 [DOI] [PubMed] [Google Scholar]
- Haun MW, Sklenarova H, Brechtel A, Herzog W, & Hartmann M (2014). Distress in cancer patients and their caregivers and association with the caregivers’ perception of dyadic communication. Oncol Res Treat, 37(7–8), 384–388. 10.1159/000364885 [DOI] [PubMed] [Google Scholar]
- Heavey CL, Layne C, & Christensen A (1993). Gender and conflict structure in marital interaction: A replication and extension. Journal of Consulting and Clinical Psychology, 61(1), 16–27. 10.1037//0022-006x.61.1.16 [DOI] [PubMed] [Google Scholar]
- Hinz A, Mehnert A, Kocalevent RD, Brahler E, Forkmann T, Singer S, & Schulte T (2016). Assessment of depression severity with the PHQ-9 in cancer patients and in the general population. BMC Psychiatry, 16, 22. 10.1186/s12888-016-0728-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, & Alvarez W (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218. [DOI] [PubMed] [Google Scholar]
- Kenny D, Kashy DA, & Cook WL (2006). Dyadic data analysis. Guilford press. [Google Scholar]
- Kornblith AB, Herr HW, Ofman US, Scher HI, & Holland JC (1994). Quality of life of patients with prostate cancer and their spouses. The value of a data base in clinical care. Cancer, 73(11), 2791–2802. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurenceau JP, Barrett LF, & Pietromonaco PR (1998). Intimacy as an interpersonal process: The importance of self-disclosure, partner disclosure, and perceived partner responsiveness in interpersonal exchanges. Journal of Personality and Social Psychology, 74(5), 1238–1251. [DOI] [PubMed] [Google Scholar]
- Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, & Brook RH (1998). The UCLA Prostate Cancer Index: Development, reliability, and validity of a health-related quality of life measure. Medical Care, 36(7), 1002–1012. 10.1097/00005650-199807000-00007 [DOI] [PubMed] [Google Scholar]
- Love AW, Scealy M, Bloch S, Duchesne G, Couper J, Macvean M, Costello A, & Kissane DW (2008). Psychosocial adjustment in newly diagnosed prostate cancer. Australian and New Zealand Journal of Psychiatry, 42(5), 423–429. 10.1080/00048670801961081 [DOI] [PubMed] [Google Scholar]
- Manne S, & Badr H (2008). Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer, 112(11 Suppl), 2541–2555. 10.1002/cncr.23450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Badr H, Zaider T, Nelson C, & Kissane D (2010). Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship, 4(1), 74–85. 10.1007/s11764-009-0109-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Kashy DA, Zaider T, Kissane D, Lee D, Kim IY, Heckman CJ, Penedo FJ, Murphy E, & Virtue SM (2019). Couple-focused interventions for men with localized prostate cancer and their spouses: A randomized clinical trial. The British Journal of Health Psychology, 24(2), 396–418. 10.1111/bjhp.12359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Kashy DA, Zaider T, Lee D, Kim IY, Heckman C, Penedo F, Kissane D, & Virtue SM (2018). Interpersonal processes and intimacy among men with localized prostate cancer and their partners. Journal of Family Psychology, 32(5), 664–675. 10.1037/fam0000404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Kissane DW, Nelson CJ, Mulhall JP, Winkel G, & Zaider T (2011). Intimacy-enhancing psychological intervention for men diagnosed with prostate cancer and their partners: A pilot study. The Journal of Sexual Medicine, 8(4), 1197–1209. 10.1111/j.1743-6109.2010.02163.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Kissane D, Zaider T, Kashy D, Lee D, Heckman C, & Virtue SM (2015). Holding back, intimacy, and psychological and relationship outcomes among couples coping with prostate cancer. Journal of Family Psychology, 29(5), 708–719. 10.1037/fam0000096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, & Fox K (2004). Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. Journal of Consulting and Clinical Psychology, 72(4), 660–670. 10.1037/0022-006X.72.4.660 [DOI] [PubMed] [Google Scholar]
- Mols F, van de Poll-Franse LV, Vingerhoets AJJM, Hendrikx A, Aaronson NK, Houterman S, Coebergh JWW, & Essink-Bot ML (2006). Long-term quality of life among Dutch prostate cancer survivors: Results of a population-based study. Cancer, 107(9), 2186–2196. 10.1002/cncr.22231 [DOI] [PubMed] [Google Scholar]
- Morelli SA, Lee IA, Arnn ME, & Zaki J (2015). Emotional and instrumental support provision interact to predict well-being. Emotion, 15(4), 484–493. 10.1037/emo0000084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oba A, Nakaya N, Saito-Nakaya K, Hasumi M, Takechi H, Arai S, & Shimizu N (2017). Psychological distress in men with prostate cancer and their partners before and after cancer diagnosis: A longitudinal study. Japanese Journal of Clinical Oncology, 47(8), 735–742. 10.1093/jjco/hyx066 [DOI] [PubMed] [Google Scholar]
- O’Shaughnessy PK, Ireland C, Pelentsov L, Thomas LA, & Esterman AJ (2013). Impaired sexual function and prostate cancer: A mixed method investigation into the experiences of men and their partners. Journal of Clinical Nursing, 22(23–24), 3492–3502. 10.1111/jocn.12190 [DOI] [PubMed] [Google Scholar]
- Penson DF, McLERRAN D, Feng Z, Li L, Albertsen PC, Gilliland FD, Hamilton A, Hoffman RM, Stephenson RA, Potosky AL, & Stanford JL (2005). 5-year urinary and sexual outcomes after radical prostatectomy: Results from the prostate cancer outcomes study. Journal of Urology, 173(5), 1701–1705. 10.1097/01.ju.0000154637.38262.3a [DOI] [PubMed] [Google Scholar]
- Pistrang N, & Barker C (1995). The partner relationship in psychological response to breast cancer. Social Science and Medicine, 40(6), 789–797. 10.1016/0277-9536(94)00136-h [DOI] [PubMed] [Google Scholar]
- Ross KM, Ranby KW, Wooldridge JS, Robertson C, & Lipkus IM (2016). Effects of physical and mental health on relationship satisfaction: A dyadic, longitudinal examination of couples facing prostate cancer. Psychooncology, 25(8), 898–904. 10.1002/pon.3931 [DOI] [PubMed] [Google Scholar]
- Salazar A, Regis L, Planas J, Celma A, Diaz F, Gallardo I, & Morote J (2019). Early continence after radical prostatectomy: A systematic review. Actas Urologicas Espanolas, 43, 526–535. 10.1016/j.acuro.2019.06.003 [DOI] [PubMed] [Google Scholar]
- Soloway CT, Soloway MS, Kim SS, & Kava BR (2005). Sexual, psychological and dyadic qualities of the prostate cancer ‘couple’. BJU International, 95(6), 780–785. 10.1111/j.1464-410X.2005.05400.x [DOI] [PubMed] [Google Scholar]
- Song L, Northouse LL, Braun TM, Zhang L, Cimprich B, Ronis DL, & Mood DW (2011). Assessing longitudinal quality of life in prostate cancer patients and their spouses: A multilevel modeling approach. Quality of Life Research, 20(3), 371–381. 10.1007/s11136-010-9753-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song L, Rini C, Ellis KR, & Northouse LL (2016). Appraisals, perceived dyadic communication, and quality of life over time among couples coping with prostate cancer. Supportive Care in Cancer, 24(9), 3757–3765. 10.1007/s00520-016-3188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, & McMurray J (2000). Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: The PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American Journal of Obstetrics and Gynecology, 183(3), 759–769. 10.1067/mob.2000.106580 [DOI] [PubMed] [Google Scholar]
- Street AF, Couper JW, Love AW, Bloch S, Kissane DW, & Street BC (2010). Psychosocial adaptation in female partners of men with prostate cancer. European Journal of Cancer Care, 19(2), 234–242. 10.1111/j.1365-2354.2008.01012.x [DOI] [PubMed] [Google Scholar]
- Trinchieri A, Nicola M, Masini F, & Mangiarotti B (2005). Prospective comprehensive assessment of sexual function after retropubic non nerve sparing radical prostatectomy for localized prostate cancer. Archivio Italiano di Urologia, Andrologia, 77(4), 219–223. [PubMed] [Google Scholar]
- van Stam MA, van der Poel HG, Bosch J, Tillier CN, Horenblas S, Mols F, & Aaronson NK (2017). Prevalence and correlates of mental health problems in prostate cancer survivors: A case-control study comparing survivors with general population peers. Urologic Oncology, 35(8), 531.e531–531.e537. 10.1016/j.urolonc.2017.03.028 [DOI] [PubMed] [Google Scholar]
- Veit CT, & Ware JE Jr (1983). The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology, 51(5), 730–742. 10.1037//0022-006x.51.5.730 [DOI] [PubMed] [Google Scholar]
- Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S, & Lewith G (2014). Depression and anxiety in prostate cancer: A systematic review and meta-analysis of prevalence rates. British Medical Journal Open, 4(3), e003901. 10.1136/bmjopen-2013-003901 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


