BACKGROUND:
Patient satisfaction is an important indicator used to monitor quality of care and outcomes after spine surgery.
OBJECTIVE:
To examine the complex relationship between preoperative expectations, fulfillment of expectations, postsurgical outcomes, and satisfaction after spine surgery.
METHODS:
In this national study of patients undergoing elective surgery for degenerative spinal conditions from the Canadian Spine Outcomes and Research Network Registry, we used logistic regression to examine the relationships between patient satisfaction with surgery (1-5 scale), preoperative expectation score (0 = none to 100 = highest), fulfillment of expectations, and disability and pain improvement.
RESULTS:
Fifty-eight percent of patients were extremely satisfied, and 3% were extremely dissatisfied. Expectations were variable and generally high (mean 79.5 of 100) while 17.3% reported that none of their expectations were met, 49.8% reported that their most important expectation was met, and 32.9% reported that their most important expectation was not met but others were. The results from the fully adjusted ordinal logistic model for satisfaction indicate that satisfaction was higher among patients with higher preoperative expectations (odds ratio [OR] [95% CI]: 1.11, [1.04-1.19]), reporting important improvements in disability (OR [95% CI]: 2.52 [1.96-3.25]) and pain (OR [95% CI]: 1.64 [1.25-2.15]) and reporting that expectations were fulfilled (OR = 80.15, for all expectations were met). The results were similar for lumbar and cervical patients.
CONCLUSION:
Given the dominant impact of expectation fulfillment on satisfaction level, there is an opportunity for improving overall patient satisfaction by specifically assessing and mitigating the potential discrepancies between patients' preoperative expectations and likely surgical outcomes. The findings are likely relevant across elective surgical populations.
KEY WORDS: Disability, Expectations, Expectation fulfillment, Pain, Satisfaction, Surgery
ABBREVIATIONS:
- CIIs
clinically important improvements
- E-AD
expectation-actuality discrepancy
- NDI
Neck Disability Index
- ODI
Oswestry Disability Index.
Patient satisfaction is increasingly used as a patient-centric measure to monitor quality of care and outcomes after spine surgery.1 Studies examining the association of preoperative and postoperative factors with patient satisfaction after spine surgery have shown inconsistent results.2-5 Furthermore, the lack of consistent association between changes in patient-reported symptoms, function, or quality of life with patient satisfaction remains a concern in using satisfaction as a stand-alone measure of surgical outcomes.6
Findings from studies examining the relationship between preoperative expectations and satisfaction with spine surgery are also inconsistent.1,3,4,7 Fulfillment of expectations, however, has consistently been found to be associated with satisfaction after orthopaedic surgery.1,4,8-12 In addition, patient expectations have been shown to be strongly related to a patient's assessment of their functional outcome.4,5,13,14 The crux of these mixed findings is that to understand patient satisfaction after spine surgery, it is essential to consider each of these components simultaneously. Therefore, our study aimed to examine (1) the effect of preoperative expectations on functional outcome improvement after spine surgery, (2) the independent effect of preoperative expectations and functional outcome improvement on fulfillment of expectations, and (3) the independent effect of preoperative expectations, functional outcome improvement, and fulfillment of expectations on level of satisfaction with spine surgery.
METHODS
We conducted analysis of data from the Canadian Spine Outcomes and Research Network registry. This registry prospectively enrolls patients requiring elective surgical treatment for spinal problems from 50 neurosurgical and orthopaedic spine surgeons across 18 sites in Canada. Patients completed a range of questionnaires before (baseline) and 1 year after surgery. Each participating institution obtained ethics approval, and all participants consented to participate in the registry.15 The data used in this study are not publicly available because Canadian Spine Outcomes and Research Network participants did not agree for their data to be shared publicly.
We included patients undergoing elective procedures enrolled from January 2013 through July 2017 who were eligible for follow-up (n = 2343). We excluded 477 patients: 252 were loss to follow-up and 225 patients did not answer questions about satisfactions and fulfillment of expectations. This resulted in a sample of 1866 patients (79.6%) for analysis. There were no significant differences in sociodemographic and health-related factors between the analytical sample (n = 1866) and those excluded from the analysis (n = 477).
Preoperatively, patients reported their level of expectation (no change [0], somewhat better [1], better [2], and much better [3]) related to the following 6 dimensions: leg/arm pain, back/neck pain, independence in everyday activities, sporting activities/recreation, general physical capacity at work and home, and mental well-being. We calculated a preoperative expectation score by summing points for all six items and dividing by the total possible maximum score and then normalizing to a scale from 0 to 100, with higher scores reflecting greater preoperative expectations.16 Patients also reported what they deemed as the most important expected change from the above six dimensions.
At baseline and at 1-year follow-up, patients reported their level of pain (back/neck and arm/leg) using a numerical pain rating scale that varied from 0 (no pain) to 10 (unbearable pain). For analysis, we selected the worst of back/neck and arm/leg pain reported. The modified Oswestry Disability Index and the Neck Disability Index for patients with thoracolumbar and cervical diagnoses, respectively, were also collected at these time points. The disability score ranges from 0 to 100 (highest disability). We created two variables identifying whether patients had clinically important improvements (CIIs) in pain and disability after surgery. We used a cutoff point of 2 for pain and 12.8 for the Oswestry Disability Index and 15.0 for the Neck Disability Index.17-19
At 1-year follow-up, patients indicated if their preoperative expectations were fulfilled: completely (2), somewhat (1), and not at all (0). Similar to Mannion et al,9 we calculated an expectation-actuality discrepancy (E-AD) measure. Fulfillment of expectations (ie, E-AD) was operationalized as 1 = all expectations were met, 2 = most important expectation was met, 3 = most important expectation was not met, and 4 = none were met.
At 1-year after surgery, patients reported their satisfaction with the results of their surgery (“extremely satisfied,””somewhat satisfied,”“neither satisfied nor dissatisfied,”“somewhat dissatisfied,”and “extremely dissatisfied”).
Data on the following variables were also collected: age, sex, educational level (less than high school, high school, or college/university), labor force status (currently working, in labor force but not currently working, or not in labor force), participation in physical activity (active vs inactive), smoking status (current smokers vs not current smokers), body mass index (<25.0, 25.0-29.9, ≥30.0), number of comorbidities (none, 1-2, or 3+), depression (Patients Health Questionnaire-8 scores >10 20), principal pathology (stenosis, spondylolisthesis, disk herniation, degenerative disk disorder, and deformity), the type of surgery (fusion vs other), and spine location (thoracolumbar vs cervical).
Statistical Analysis
We fit two multivariable logistic regression models to examine the effect of preoperative expectations on and achieving CII in disability and pain, respectively (objective 1). We fit nominal multivariate logistic regression models to examine the effect of preoperative expectations and achieving CII in disability and pain on fulfillment of expectations (“none were met” as the reference category) (objective 2). To address the third objective, we used multivariate ordinal logistic regression models to examine the effect of preoperative expectations, expectations fulfillment, and disability and pain improvement on level of satisfaction (lower to higher). All models were adjusted for covariates, and the results are presented as odds ratio with 95% CIs. All analyses were performed using SAS/STAT software version 9.4 (Copyright © 2020 SAS Institute Inc).
RESULTS
Of the 1866 patients included in the analysis, 48.6% were female and over 80% were age 45 years and older. Most patients (81.8%) had lumbar problems, and 55.9% had fusion surgery. The most common principal pathologies were stenosis (37.4%), spondylolisthesis (28.0%), and disk herniation (20.1%) (Table 1).
TABLE 1.
Patient Characteristics (n = 1866)
| Characteristic | No. of patients (%) |
|---|---|
| Sociodemographic factors | |
| Age groups | |
| <45 y | 360 (19.3) |
| 45-64 y | 827 (44.3) |
| 65+ y | 679 (36.4) |
| Sex | |
| Women | 907 (48.6) |
| Men | 959 (51.4) |
| Education level | |
| <High school | 235 (12.6) |
| High school | 806 (43.2) |
| >High school | 793 (42.5) |
| Labor force status | |
| Currently working | 569 (30.5) |
| Not working | 267 (14.3) |
| Not in labor force | 875 (46.9) |
| Health-related factors | |
| Smoking | |
| Current | 342 (18.3) |
| Not currently smoking | 1514 (81.1) |
| Physical activity | |
| Active | 806 (43.2) |
| Inactive | 1017 (54.5) |
| BMI groups | |
| Underweight/normal | 485 (26.0) |
| Overweight | 677 (36.3) |
| Obese | 632 (33.9) |
| Comorbidities | |
| None | 360 (19.3) |
| 1-2 | 879 (47.1) |
| 3+ | 627 (33.6) |
| Depressive symptomsa | |
| Yes | 938 (50.3) |
| No | 895 (48.0) |
| Surgical factors | |
| Principal pathology | |
| Stenosis | 697 (37.4) |
| Spondylolisthesis | 523 (28.0) |
| Disk herniation | 375 (20.1) |
| Degenerative disk disease | 169 (9.1) |
| Deformity | 102 (5.5) |
| Spine location | |
| Lumbar | 1526 (81.8) |
| Cervical | 340 (18.2) |
| Surgery type | |
| Fusion | 1044 (55.9) |
| Others | 822 (44.1) |
BMI, body mass index.
Based on the Patient Health Questionnaire Depression Scale (PHQ-8). Depressive symptoms are defined as score ≥10.
Canadian Spine Outcomes and Research Network Database, 2013 to 2017.
Normal/underweight (BMI < 25.0), overweight (25.0 ≤ BMI > 30.0), and obese (≥30.0).
Most patients expected to be better or much better postoperatively in all dimensions (Figure 1A). The order of most important expectation dimensions were improvement of leg or arm pain (30.2%), improvement in back or neck pain (27.4%), improvement in general capacity/function (22.2%), improvement of independence in everyday activities (15.8%), sporting activities/recreation (3.9%), and mental well-being (0.5%) (Figure 1B). After surgery and across multiple domains, 33.0% to 55.3% of patients did not fulfill their preoperative expectations (Figure 1C). Half of all patients reported that their most important expectation was fulfilled (24.8% of all patients reported that all expectations were met, and 25.0% reported that their most important expectation was met but other expectations were not met), 32.9% reported that their most important expectation was not met but others were, and 17.3% reported that none of their expectations were met (Table 2).
FIGURE 1.
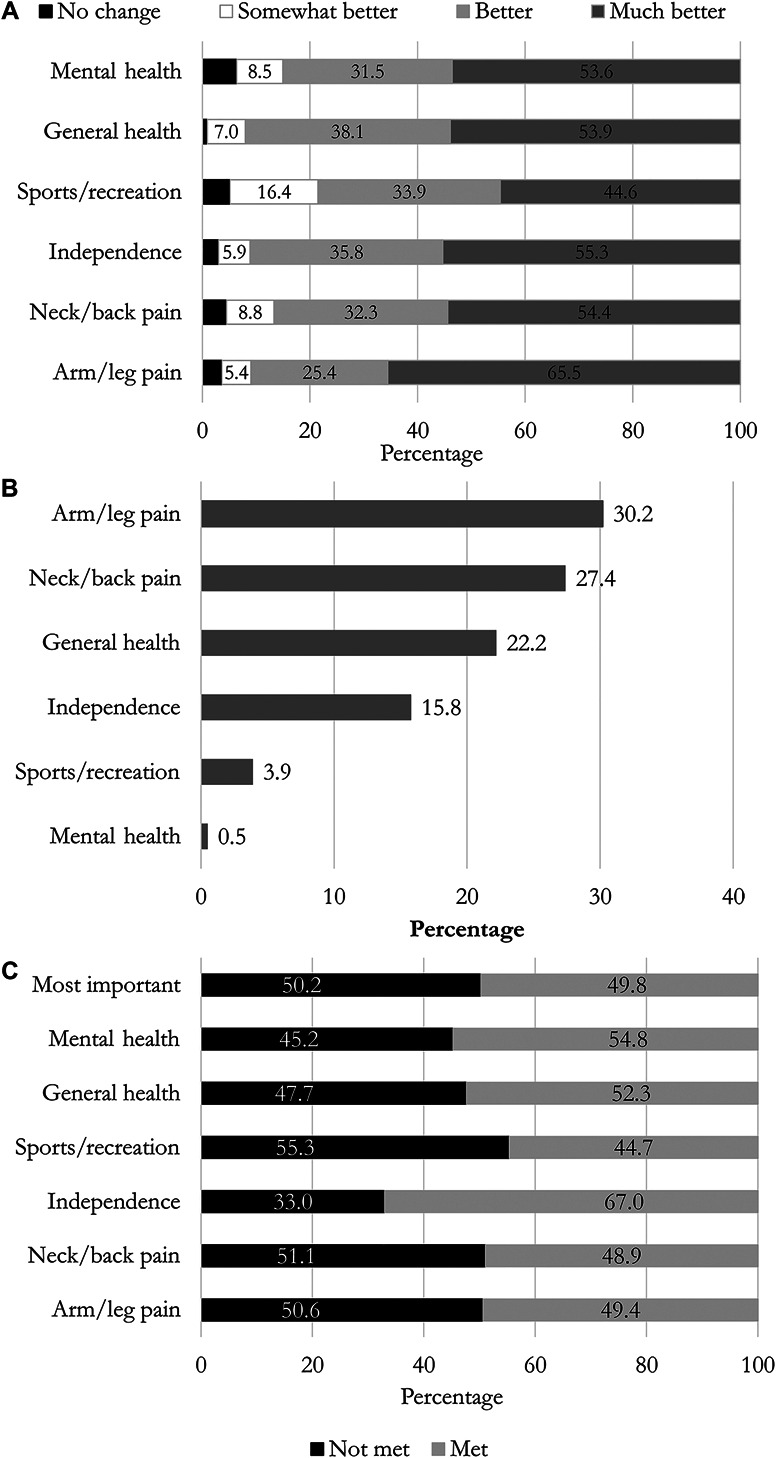
Description of preoperative expectations, most important preoperative expectation, and fulfillment of preoperative expectations. Canadian Spine Outcomes and Research Network Database, 2013 to 2017. A, Preoperatively, for each dimension, patients were asked “What changes would you expect (not hope) to experience as a result of an operation?” B, Preoperatively, patients reported what they deemed as the most important expected change from the above six dimensions. C, Postoperatively, for each dimension, patients were asked “Did the surgery fulfill your expectations?” Completely and somewhat are reported as met.
TABLE 2.
Preoperative Expectations, Proportion Reaching Clinically Important Disability and Pain Improvement, and Fulfillment of Expectations by Levels of Satisfaction With Spine Surgery
| Expectation and functional outcomes | Total (n = 1866) |
Satisfaction with surgery | P-value | ||||
|---|---|---|---|---|---|---|---|
| Extremely satisfied | Somewhat satisfied | Neither satisfied nor dissatisfied | Somewhat dissatisfied | Extremely dissatisfied | |||
| (n = 1079, 57.8%) | (n = 505, 27.1%) | (n = 111, 5.9%) | (n = 117, 6.3%) | (n = 54, 2.9%) | |||
| Preoperative expectations (mean) | |||||||
| Overall scorea | 78.2 (77.4-79.1) | 79.3 (78.2-80.4) | 76.4 (74.8-78.0) | 75.7 (72.2-79.1) | 79.4 (76.0-82.8) | 76.8 (71.0-82.5) | .0752 |
| Disabilityb and painc (%) | |||||||
| CII in disability | 61.2 (59.5-64.0) | 77.7 (75.1-80.2) | 47.5 (43.0-51.9) | 32.1 (23.2-41.0) | 21.6 (14.1-29.0) | 23.1 (11.6-34.5) | <.0001 |
| CII in pain | 79.0 (77.1-80.8) | 89.5 (87.6-91.3) | 71.5 (67.6-75.5) | 59.6 (50.4-68.9) | 53.8 (44.8-62.9) | 32.7 (19.9-45.5) | <.0001 |
| Fulfilled expectations (%) | <.0001 | ||||||
| All expectations met | 24.8 (22.9-26.8) | 41.0 (38.0-43.9) | 4.0 (2.3-5.7) | 0.0 (0.0-0.0) | 0.0 (0.0-0.0) | 1.9 (0.0-5.5) | |
| Most important met | 25.0 (23.0-26.9) | 30.2 (27.5-33.0) | 23.0 (19.3-26.6) | 10.8 (5.0-16.6) | 7.7 (2.9-12.5) | 5.6 (0.0-11.7) | |
| Most important not met (others met) | 32.9 (30.8-35.0) | 24.7 (22.1-27.2) | 45.0 (40.6-49.3) | 45.0 (35.8-54.3) | 41.0 (32.1-49.9) | 42.6 (29.4-55.8) | |
| None met | 17.3 (15.6-19.0) | 4.2 (3.0-5.4) | 28.1 (24.2-32.0) | 44.1 (34.9-53.4) | 51.3 (42.2-60.3) | 50.0 (36.7-63.3) | |
CII, Clinically important improvement; NDI, Neck Disability Index; ODI, Oswestry Disability Index.
Overall preoperative expectations score (0-100) with higher values reflecting greater preoperative expectations.
The ODI and the NDI for patients with thoracolumbar and cervical diagnosis, respectively. Clinically important improvement is defined as preoperative ODI/NDI minus postoperative ODI ≥ 12.8 and NDI ≥15.0. Reported as proportion achieving clinically important improvement.
Worst of back/neck pain and arm/leg pain with 0 = no pain and 10 = highest pain. Clinically important improvement is defined as preoperative pain minus postoperative pain ≥2.0. Reported as proportion achieving clinically important improvement.
P-values were obtained from unadjusted ordinal logistic regression with satisfaction as the outcome.
Means/% (95% CIs). Canadian Spine Outcomes and Research Network Database, 2013 to 2017.
Fifty-eight percent of patients were extremely satisfied, and only 3% were extremely dissatisfied with the outcome of their surgery at 1 year (Table 2). The overall unadjusted mean preoperative expectation score was 78.2 (95% CI, 77.4-79.1) with no significant differences across satisfaction levels (Table 2). There were significant differences in disability and pain improvement at 1 year after surgery by satisfaction levels (P < .0001), with higher proportions achieving CII in disability and pain with increasing levels of satisfaction. The proportion of patients reporting that their expectations were not met increased from 4.2% among those reporting being extremely satisfied to 50.0% among those extremely dissatisfied (P < .0001). Among the 463 patients reporting that all expectations were met, all but one reported being at least somewhat satisfied (95.5% were extremely satisfied).
The relationship among the main study variables from the fully adjusted models is summarized in Figure 2, and models are presented in Supplemental Digital Content, Tables S1-S3, http://links.lww.com/NEU/D98. Higher preoperative expectations were significantly associated with postoperative improvements in disability (odds ratio [95% CI]: 1.12 [1.05-1.19]) and pain (odds ratio [95% CI]: 1.12 [1.05-1.20]). Preoperative expectations were significantly associated with expectation fulfillment: Patients with higher expectations were less likely to report that their expectations were met, independently of postoperative changes in disability and pain. Furthermore, disability and pain improvements were significantly associated with fulfillment of expectations (P < .0001 for both), reporting that all expectations were met was particularly common for those achieving CII in disability and pain.
FIGURE 2.

Summary of findings from models examining the relationship between preoperative expectations, pain and disability improvement, fulfillment of expectations, and satisfaction with spine surgery (full models are shown in the Supplemental Digital Content, Tables S1-S3, http://links.lww.com/NEU/D98). Numbers in the figure are odd ratios. All estimates were adjusted for sociodemographic and health-related control variables. Logistic regression modeling was used for pain and function, nominal logistic regression for fulfillment of expectations with “none met as reference,” and ordinal logistic regression for satisfaction (odds of transitioning from lower to higher level of satisfaction). Dashed lines indicate negative associations, and solid lines indicate positive associations. Overall preoperative expectations score (0-100) with higher values reflect greater preoperative expectations. Disability was measured using the ODI and the NDI for patients with thoracolumbar and cervical diagnosis, respectively. Improvement is defined as preoperative ODI/NDI minus postoperative ODI/NDI (ODI ≥ 12.8 and NDI ≥ 15.0). Pain was defined as the worst of reported back/neck pain and arm/leg pain with 0 = no pain and 10 = highest pain. Improvement is defined as preoperative pain minus postoperative pain ≥2.0. NDI, Neck Disability Index; ODI, Oswestry Disability Index.
The results from the final model for satisfaction considering all the main study variables together indicate that preoperative expectations, clinically important disability and pain improvements, and fulfillment of expectations were all positively associated with higher satisfaction with surgery. Patients with higher preoperative expectations, reporting important improvements in disability and pain, and reporting that expectations were fulfilled were more likely to report being satisfied with their spine surgery than their counterparts. The independent effect of expectation fulfillment on satisfaction with surgery is further illustrated in Figure 3.
FIGURE 3.
Illustration of the effect of expectation fulfillment disability improvement and preoperative expectations on satisfaction with spine surgery: A, low expectations and no disability improvement; B, low expectations and disability improvement; C, moderate expectations and no disability improvement; D, moderate expectations and disability improvement; E, high expectations and no disability improvement; and F, high expectations and disability improvement. Values obtained from the model for satisfaction are summarized in the Supplemental Digital Content, Table S3, http://links.lww.com/NEU/D98. The y-axis displays the predicted probability for each satisfaction level, and the x-axis displays expectation fulfillment. A-C, depict values calculated at low, middle, and high levels of preoperative expectations, respectively. Within each panel, values were calculated by disability improvement (yes/no). All other variables were held constant at their means.
DISCUSSION
Patients undergoing elective spine surgery in Canada have high expectations with variability as to what they deemed as the most important expectation. Generally, their expectations were higher than what they achieved: Only half of our patient population fulfilled their most important expectation and 17% reported that none of their expectations were fulfilled. Those with higher preoperative expectations of spine surgery were less likely to have their expectations fulfilled independent of their functional outcomes improvement. Despite this disparity, most patients (85%) were satisfied with the results of the surgery. Furthermore, preoperative expectations, disability, and pain improvement as well as fulfillment of expectation were positively associated with satisfaction with surgery. Fulfillment of preoperative expectations globally, and what patients deemed as the most important expectation, was the strongest predictor of higher satisfaction with surgery.
Patients who had higher preoperative expectations were less likely to have their expectations fulfilled but were more likely to report CIIs in disability and pain and were also more satisfied with the surgery. The negative association between preoperative expectations and expectation fulfillment has been reported previously,4,21 but contrasts with others.3,9,22-24 Studies examining the association between expectations and postoperative improvement in functional outcome and satisfaction with spine surgery have also shown inconsistent results.3,5,9,14 It has been suggested that the association between expectations and changes in disability and pain seen in some studies is explained by the fact that patients with worse disability and pain before surgery—who also have higher preoperative expectations—have the greatest room for improvement after the surgery, and, therefore, actual functional status preoperatively is more predictive of satisfaction than expectations of outcome.3,9 Our findings, however, did not support this notion because, in sensitivity analysis, we found that expectations were significantly associated with functional outcome improvement, independent of functional status at baseline. As previously reported, we found that higher preoperative expectations were associated with higher satisfaction21 and with better functional outcomes after surgery.4,21
The dominant impact of expectation fulfillment on satisfaction level demonstrated in our study is consistent with findings from the few studies that have assessed the effect of E-AD (mismatch between preoperative expectations and the actual result of the surgery, ie, the degree to which expectations are fulfilled) on satisfaction.9 In a systematic review, Witiw et al5 noted that studies consistently demonstrated that E-AD predicted satisfaction over and above the effect of change in pain and function and of preoperative expectations. Similar findings have been noted in studies of patient satisfaction after total hip or knee replacement.25,26 As discussed by Witiw et al,5 this observation is well supported by the “expectancy disconfirmation theory”27,28 which posits that satisfaction is a function of the degree of discrepancy between patients' prior expectations and their outcomes: If expectations exceed the outcomes, the resulting expectation discrepancy has a negative effect on satisfaction. It has also been posited that this effect is to some degree modulated by the “assimilation contrast.” 29 The idea is that small differences between expectations and outcomes have a small impact on satisfaction (assimilation effect) while large discrepancies lead to dissatisfaction. The significant graduated, nonlinear association between fulfillment of expectation and satisfaction that we found in our study supports this theory (Figure 3).
Our findings strongly support that efforts to mitigate the degree of E-AD (ie, increase expectation fulfillment) as part of the preoperative shared decision-making process are warranted. Although ideal, fulfilling all expectations in all patients is clearly unrealistic. However, it is anticipated that the levels of satisfaction and possibly outcome could be influenced by adjusting preoperative expectations to a more realistic level.30 Studies addressing this topic suggest that patients who used decisions aids (eg, pamphlets and videos) reported feeling clearer regarding their personal values and expectations and had greater participation in the decision-making process.31 Two studies of hip and knee arthroplasty patients showed that preoperative educational classes effectively modified patient expectations and were essential components for successful postoperative patient-reported outcomes.32,33 Furthermore, patient education and targeted interventions, including cognitive behavioral approaches aimed specifically at aligning expectations, have been showed to be effective.30,34
A large proportion of patients reported unfulfilled expectations of outcomes secondary to spine surgery, such as improvements in mental well-being. This may reflect unrealistic expectations that are ultimately unattainable and leading to patients' dissatisfaction with surgery.35 It has also been shown that there is a large discrepancy between surgeons' and patients' expectation across different expectation dimensions.36-38 Therefore, the extent of improvement that can be realistically achieved in these domains needs to be discussed in more detail with patients during the preoperative consultation process. It has been suggested that a balanced view of the surgical result requires that outcomes are assessed from both the patient's and the surgeon's perspective.37,38
Limitations
There are no standardized and validated questionnaires for assessing the expectations of patients undergoing spine surgery. We used a questionnaire previously published to assess preoperative expectations.9 We had no control over when the questionnaires were completed, and variability in the timing may have influenced the responses. We cannot determine the level of preoperative education each patient received. The differing amounts of instruction would presumably affect the patients' responses. Another limitation is the possibility of other unmeasured confounders that may influence reporting of fulfillment of expectations and patient satisfaction. Most of our sample had lumbar surgery (81.8%), which may affect the generalizability of our findings. However, sensitivity analysis showed that the patterns of the associations presented in the main analyses were similar across surgical sites (Supplemental Digital Content, Table S4, http://links.lww.com/NEU/D98.). These limitations notwithstanding our findings make an important contribution to the literature because no study has comprehensibly examined the complex relationship between patient satisfaction with surgery and preoperative expectation, expectation fulfillment, and pain and disability outcomes. The strengths of this study are that it stems from a national registry with a large sample size, has a longitudinal design, and a high follow-up rate. It includes a wide range of diagnoses and surgical techniques that are generalizable to the broad surgical spine population.
CONCLUSION
This study expands on previous work and provides new findings that shed light on the complex psychological interactions between preoperative expectations, fulfillment of these expectations, changes in pain and disability, and satisfaction with surgery. Our findings show that although expectations of spine surgery were variable across patients and typically exceeded the final result, satisfaction levels remained high and that fulfillment of expectations, even those not deemed most important, seem to be the most important determinant of the degree of overall satisfaction. The results highlight an important opportunity for improving individual patient satisfaction by explicitly assessing specific patient expectations of outcome and addressing (ie, level setting) potentially unrealistic expectations or misconceptions that may result in a large and negative expectation-actuality discrepancy.
Acknowledgments
The authors thank all of the patients who participated in the study and the support/research coordinator staff and investigators from the CSORN contributing sites.
Footnotes
Supplemental digital content is available for this article at neurosurgery-online.com.
Y. Raja Rampersaud and Mayilee Canizares contributed equally to this work.
Funding
This study did not receive any funding or financial support. Dr Johnson's institution receives financial support from Stryker to support the research department. Dr Phan has a research grant from Stryker.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article. Dr Christie has financial relationships with Medtronic Canada and has had with Bioventus. Dr Manson has financial relationships with Medtronic Canada. Dr Fisher has financial relationships with Medtronic, Nuvasive, and AOSpine.
Supplemental Digital Content
Supplemental Digital Content. Additional data results. Table S1. Effect of preoperative expectations on disability and pain improvement: the results of multivariable logistic models. Table S2. Effect of preoperative expectations and disability and pain improvement on fulfillment of expectations: the results of multivariable nominal logistic models. Table S3. Effect of preoperative expectations, disability and pain improvement, and fulfillment of expectation on satisfaction: the results of multivariable ordinal logistic models. Table S4. Effect of preoperative expectations, disability and pain improvement, and fulfillment of expectation on satisfaction: the results of multivariable ordinal logistic models by lumbar and cervical surgical site.
REFERENCES
- 1.Swarup I, Henn CM, Gulotta LV, Henn RF. Patient expectations and satisfaction in orthopaedic surgery: a review of the literature. J Clin Orthop Trauma. 2019;10(4):755-760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auer CJ, Glombiewski JA, Doering BK, et al. Patients' expectations predict surgery outcomes: a meta-analysis. Int J Behav Med. 2016;23(1):49-62. [DOI] [PubMed] [Google Scholar]
- 3.McGregor AH, Doré CJ, Morris TP. An exploration of patients' expectation of and satisfaction with surgical outcome. Eur Spine J. 2013;22(12):2836-2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soroceanu A, Ching A, Abdu W, McGuire K. Relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery: a multicenter study. Spine (Phila Pa 1976). 2012;37(2):E103-E108. [DOI] [PubMed] [Google Scholar]
- 5.Witiw CD, Mansouri A, Mathieu F, Nassiri F, Badhiwala JH, Fessler RG. Exploring the expectation-actuality discrepancy: a systematic review of the impact of preoperative expectations on satisfaction and patient reported outcomes in spinal surgery. Neurosurg Rev. 2018;41(1):19-30. [DOI] [PubMed] [Google Scholar]
- 6.Godil SS, Parker SL, Zuckerman SL, et al. Determining the quality and effectiveness of surgical spine care: patient satisfaction is not a valid proxy. Spine J. 2013;13(9):1006-1012. [DOI] [PubMed] [Google Scholar]
- 7.Ryu WHA, Platt A, O'Toole JE, Fontes R, Fessler RG. Patient expectations of adult spinal deformity correction surgery. World Neurosurg. 2021;146:e931-e939. [DOI] [PubMed] [Google Scholar]
- 8.Dyck BA, Zywiel MG, Mahomed A, Gandhi R, Perruccio AV, Mahomed NN. Associations between patient expectations of joint arthroplasty surgery and pre- and post-operative clinical status. Expert Rev Med Devices. 2014;11(4):403-415. [DOI] [PubMed] [Google Scholar]
- 9.Mannion AF, Junge A, Elfering A, Dvorak J, Porchet F, Grob D. Great expectations: really the novel predictor of outcome after spinal surgery? Spine (Phila Pa 1976). 2009;34(15):1590-1599. [DOI] [PubMed] [Google Scholar]
- 10.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35-43. [DOI] [PubMed] [Google Scholar]
- 11.Palazzo C, Jourdan C, Descamps S, et al. Determinants of satisfaction 1 year after total hip arthroplasty: the role of expectations fulfilment. BMC Musculoskelet Disord. 2014;15(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saban KL, Penckofer SM. Patient expectations of quality of life following lumbar spinal surgery. J Neurosci Nurs. 2007;39(3):180-189. [DOI] [PubMed] [Google Scholar]
- 13.Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you'll do? A systematic review of the evidence for a relation between patients' recovery expectations and health outcomes. CMAJ. 2001;165(2):174-179. [PMC free article] [PubMed] [Google Scholar]
- 14.Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res. 2008;466(5):1154-1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moe J, O'Sullivan F, McGregor MJ, et al. Characteristics of frequent emergency department users in British Columbia, Canada: a retrospective analysis. CMAJ Open. 2021;9(1):E134-E141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Canizares M, Gleenie RA, Perruccio AV, et al. Patients' expectations of spine surgery for degenerative conditions: results from the Canadian Spine Outcomes and Research Network (CSORN). Spine J. 2020;20(3):399-408. [DOI] [PubMed] [Google Scholar]
- 17.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8(6):968-974. [DOI] [PubMed] [Google Scholar]
- 18.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149-158. [DOI] [PubMed] [Google Scholar]
- 19.Hung M, Saltzman CL, Kendall R, et al. What are the MCIDs for PROMIS, NDI, and ODI instruments among patients with spinal conditions? Clin Orthop Relat Res. 2018;476(10):2027-2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163-173. [DOI] [PubMed] [Google Scholar]
- 21.Mancuso CA, Duculan R, Cammisa FP, et al. Fulfillment of patients' expectations of lumbar and cervical spine surgery. Spine J. 2016;16(10):1167-1174. [DOI] [PubMed] [Google Scholar]
- 22.Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. J Gen Intern Med. 1999;14(12):740-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. Patients' expectations and satisfaction in lumbar spine surgery. Spine (Phila Pa 1976). 2005;30(23):2689-2694. [DOI] [PubMed] [Google Scholar]
- 24.Iversen MD, Daltroy LH, Fossel AH, Katz JN. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Educ Couns. 1998;34(2):169-178. [DOI] [PubMed] [Google Scholar]
- 25.Hamilton DF, Lane JV, Gaston P, et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open. 2013;3(4):e002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012;94(7):974-981. [DOI] [PubMed] [Google Scholar]
- 27.Oliver RL. Effect of expectation and disconfirmation on postexposure product evaluations: an alternative interpretation. J Appl Psychol. 1977;62(4):480-486. [Google Scholar]
- 28.Thompson AG, Suñol R. Expectations as determinants of patient satisfaction: concepts, theory and evidence. Int J Qual Health Care. 1995;7(2):127-141. [DOI] [PubMed] [Google Scholar]
- 29.Hovland CI, Harvey OJ, Sherif M. Assimilation and contrast effects in reactions to communication and attitude change. J Abnorm Psychol. 1957;55(2):244-252. [DOI] [PubMed] [Google Scholar]
- 30.Doering BK, Glombiewski JA, Rief W. Expectation-focused psychotherapy to improve clinical outcomes. Int Rev Neurobiol. 2018;138:257-270. [DOI] [PubMed] [Google Scholar]
- 31.Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mancuso CA, Graziano S, Briskie LM, et al. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin Orthop Relat Res. 2008;466(2):424-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Padilla JA, Feng JE, Anoushiravani AA, Hozack WJ, Schwarzkopf R, Macaulay WB. Modifying patient expectations can enhance total hip arthroplasty postoperative satisfaction. J Arthroplasty. 2019;34(7):S209-S214. [DOI] [PubMed] [Google Scholar]
- 34.Powell R, Scott NW, Manyande A, et al. Psychological preparation and postoperative outcomes for adults undergoing surgery under general anaesthesia. Cochrane Database Syst Rev. 2016;2016(5):CD008646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mancuso CA, Jout J, Salvati EA, Sculco TP. Fulfillment of patients' expectations for total hip arthroplasty. J Bone Joint Surg Am. 2009;91(9):2073-2078. [DOI] [PubMed] [Google Scholar]
- 36.Aoude A, Litowski M, Aldebeyan S, et al. A comparison of patient and surgeon expectations of spine surgical outcomes. Global Spine J. 2021;11(3):331-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carlson J, Youngblood R, Dalton JA, Blau W, Lindley C. Is patient satisfaction a legitimate outcome of pain management? J Pain Symptom Manage. 2003;25(3):264-275. [DOI] [PubMed] [Google Scholar]
- 38.Lattig F, Fekete TF, OʼRiordan D, et al. A comparison of patient and surgeon preoperative expectations of spinal surgery. Spine (Phila Pa 1976). 2013;38(12):1040-1048. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content. Additional data results. Table S1. Effect of preoperative expectations on disability and pain improvement: the results of multivariable logistic models. Table S2. Effect of preoperative expectations and disability and pain improvement on fulfillment of expectations: the results of multivariable nominal logistic models. Table S3. Effect of preoperative expectations, disability and pain improvement, and fulfillment of expectation on satisfaction: the results of multivariable ordinal logistic models. Table S4. Effect of preoperative expectations, disability and pain improvement, and fulfillment of expectation on satisfaction: the results of multivariable ordinal logistic models by lumbar and cervical surgical site.



