Abstract
Latino sexual minority men (LSMM) experience high rates of HIV and co-occurring health inequities. Structural and psychosocial factors may lead to mental health problems and decreased engagement with biomedical HIV-prevention behaviors. This cross-sectional study assessed the extent to which structural life instability is related to biomedical HIV-prevention services engagement (HIV-testing and PrEP uptake) indirectly through psychological distress among 290 LSMM living in Greater Miami. Using hybrid structural equation modeling, significant direct effects from structural life instability to psychological distress emerged, as did effects from psychological distress (i.e., depression and anxiety) to HIV-prevention engagement. Structural life instability had a significant indirect effect to HIV-prevention engagement via psychological distress. Findings show a possible mechanism explaining the relationship between structural life instability and biomedical HIV-prevention engagement among a group of LSMM, a subpopulation at increased susceptibility for HIV acquisition in an U.S. HIV epicenter.
Keywords: Latino/a/x, Sexual minority men, Life instability, HIV-prevention services
Resumen
Los hombres latinos de minorías sexuales (LHLMS) experimentan altos índices de VIH y disparidades de salud concurrentes. Los factores estructurales y psicosociales pueden provocar problemas de salud mental y, a su vez, reducir la participación con los comportamientos biomédicas de prevención del VIH. Este estudio transversal evaluó el grado en qué la inestabilidad estructural de la vida (IEV) está relacionada con la participación de los servicios de prevención del VIH (pruebas del VIH y uso de PrEP) indirectamente a través de la angustia psicológica entre 290 LHLMS que viven en el Gran Miami, un epicentro del VIH. Utilizando modelos de ecuaciones estructurales híbridas, surgieron efectos directos significativos de SLI a la angustia psicológica, al igual que los efectos de la angustia psicológica a la participación en la prevención del VIH. El SLI tuvo un efecto indirecto significativo en la participación en la prevención del VIH a través de la angustia psicológica. Los resultados muestran un posible mecanismo que explica la relación entre el SLI y la participación en la biomédica prevención del VIH.
Keywords: latino /a/x, hombres de minorías sexuales, inestabilidad de la vida, servicios de prevención del VIH
Introduction
Over the last decade, HIV incidence among gay, bisexual, and other men who have sex with men has generally decreased and/or stabilized due to the development of effective biomedical HIV-prevention tools such as pre-exposure prophylaxis (PrEP) and rapid antiretroviral treatment (ART; [1]). Despite these advancements, some communities within the sexual minority male population continue to face HIV disparities, with sexual minority men (SMM) still experiencing the greatest HIV incidence in the United States (U.S.). While rates of HIV among White non-Latino1 SMM have plateaued, HIV incidence among Latino sexual minority men (LSMM) increased by almost 17% from 2010 to 2017 [3].
HIV disparities in sexual and racial/ethnic minority communities are driven by the synergy of interacting and co-occurring challenges rooted in inequities [4, 5], forming a syndemic. The experience of intersectional minority stress, or chronic stressors (e.g., discrimination) unique to having multiple marginalized identities (e.g., Latino/a/x, sexual minority, socioeconomic status, documentation status; [6, 7]) both generates and exacerbates health disparities perpetuating the syndemic of HIV, mental health, and structural inequities among LSMM. In turn, this syndemic can lead to increased condomless anal sex, increased substance use, and reduced utilization of biomedical HIV-prevention services [8].
To achieve HIV-related health equity, greater attention must be placed on scaling up and out psychosocial and biomedical interventions, including HIV-testing and PrEP, to LSMM. Although PrEP for HIV-prevention has been FDA approved from almost a decade, rates of PrEP uptake among men who have sex with men (MSM) are still quite low (less than 40%, [9], particularly among Latino MSM (30%, [10]. Although rates of HIV-testing are higher amongst Latina/o/x individuals and LSMM compared to their White heterosexual counterparts [11], people identifying as Latina/o/x are still at higher risk of late HIV diagnoses [12] and being undiagnosed [13] compared to other racial/ethnic groups. Compounding cultural factors and structural barriers such as lack of health insurance, immigration concerns, and financial hardship may also influence low PrEP uptake and suboptimal HIV-testing frequency amongst people who identify as Latino [14, 15]. Therefore, addressing these psychosocial and structural barriers that affect HIV-testing and PrEP engagement among LSMM is a necessary step in working towards the Ending the HIV Epidemic goals and improving HIV-related care for a population facing disparities [16].
The HIV-prevention literature suggests that structural and psychosocial factors influence an individuals’ likelihood of engaging in health promotive behaviors and that this “life instability,” or the cumulative negative effect of factors inducing unpredictability, chaos, or confusion in a person’s life, may provide a link between the two. According to Latkin and colleagues [17], the concept of “life instability” includes structural factors stemming from external influences outside the individual’s control (e.g., no health insurance, transportation concerns, poverty) that negatively impact overall health and health behavior. This life instability may interact with “life chaos” in people living with HIV which make managing routines, adhering to a treatment regimen, and preventing further morbidity challenging [18].
The negative impact of structural barriers on testing for HIV has been well documented [19, 20]. Among racial/ethnic minority SMM, structural factors related to marginalization, such as reduced income, minimal access to healthcare services, poverty, and housing instability are major barriers to engaging with biomedical HIV-prevention services [21–24]. Structural barriers are often a direct consequence of discrimination resulting from various systems of oppression and disproportionately affect LSMM and other individuals living at the nexus of multiple systems of marginalization compared to their heterosexual cisgender White male peers. As such, research is needed to understand how structural factors rooted in inequity create life instability among LSMM and in turn affect biomedical HIV-prevention engagement.
Life instability as a theoretical construct has also long been established as an influencing factor on psychological distress. Housing instability, poverty, and unemployment have been associated with psychological distress (i.e., depression, anxiety) among MSM [25–28]. Additionally, SMM exhibit greater psychological distress in the absence of adequate access to healthcare [29] further demonstrating the negative effects of structural life instability on mental health.
Many theories of health behavior change highlight individual autonomy as an integral factor in influencing an individual’s health decision making. Theoretical frameworks such as the Theory of Planned Behavior [30], Health Belief Model [31, 32], and Social Cognitive Theory [33] all identify the strength of a person’s sense of agency as central to their ability to actually engage with behavior changes (e.g., obesity prevention, condom use, PrEP uptake). Accordingly, across the most utilized models of health behavior related to HIV-prevention, life instability may disrupt the mechanistic pathways towards behavior change by altering a person’s sense of agency. Furthermore, addressing life instability may help in “turning down the volume” on syndemic problems so that individuals are better able to capitalize on potential intentions to change health behaviors.
Life instability creates unique challenges associated with maintaining an organized routine. This disruption can cause fluctuations in how individuals perceive community norms, personal intentions to change behaviors, and even their self-efficacy to successfully alter their behaviors. In fact, in the South Florida area, factors of life instability (e.g., housing instability, financial strain, insurance status) were associated with poorer engagement in HIV-related health behaviors (e.g. ART and HIV-care appointment adherence) among a group of majority racial/ethnic minority older adults with HIV in South Florida [34] as well as with COVID-19 vaccine uptake, another biomedical prevention intervention, among a group of LSMM [35].
As such, the current study sought to utilize path analytic procedures to assess the extent to which structural life instability may affect engagement with biomedical HIV-prevention services indirectly through psychological distress among LSMM living in South Florida. Grounded in health behavior change theories such as the Theory of Planned Behavior [30] or Social Cognitive Theory [33], our outcome was a latent biomedical HIV-prevention engagement variable composed of potential HIV-testing and PrEP engagement (i.e., intention to use HIV-testing or PrEP services, HIV-testing and PrEP self-efficacy, HIV-testing and PrEP stigma, and HIV-testing and PrEP community norms). Informed by theories related to life instability, social stability, and syndemics, we examined (A) whether a structural life instability variable (indicators: history of incarceration, insurance status, employment status, and housing related financial distress) was directly associated with psychological distress and a biomedical HIV-prevention engagement outcome, (B) whether psychological distress (e.g., depression and anxiety) was associated with HIV-prevention engagement, and (C) whether there was an indirect relationship between structural life instability and biomedical HIV-prevention engagement through the psychological distress variable. Based on these research questions and prior theory, we hypothesized that for objective A, a structural life instability variable would be positively associated with a psychological distress outcome and negatively associated with a biomedical HIV-prevention engagement outcome. For objective B, we hypothesized that a psychological distress variable would be negatively associated with a biomedical HIV-prevention engagement outcome. And, for objective C, we anticipated that the relationship between structural life instability and biomedical HIV-prevention engagement would partially operate indirectly through the psychological distress variable.
Methods
Participants and Procedures
Participants included 290 LSMM living in South Florida who were enrolled in a larger 8-month longitudinal cohort study exploring factors related to access and engagement with HIV-prevention and behavioral health services at multiple timepoints. Participants were recruited from consent-to-contact databases, as well as through online advertising, word-of-mouth, and in-person recruitment events (e.g., Pride parades). Participants completed a baseline self-report online assessment battery via REDCap regarding mental health, sexual health, and HIV-prevention service use. Eligible individuals (a) identified as men, (b) reported being gay, bisexual, or a man who has sex with men, (c) identified as Latino, (d) lived in South Florida and (e) were 18–60 years old. Participants unable to provide consent or unable to speak and/or read in either English or Spanish were excluded. The data reported was collected during the baseline assessment between February 18, 2020, and August 26, 2020. All participants provided informed consent and all study procedures were approved by University of Miami Institutional Review Board. Additional details of the parent study are published elsewhere (Harkness et al., under review).
Measures
Overall, the measures employed in this study were chosen because they were the best available; however, there is not an extensive body of work examining their use among LSMM demonstrating a concerted need for greater validated measurement development among LSMM.
Demographics
Age, race/ethnicity, and sexual orientation were collected.
Life Instability
This was a latent factor (see Results) made up of participant reported experiences with four indicators of structural life instability including: (1) history of incarceration (1 = yes vs. 0 = no); (2) employment status (1 = not employed vs. 0 = employed); (3) health insurance status (1 = no vs. 0 = yes); (4) if they have ever worried about paying for their current housing situation (1 = almost always/usually/sometimes vs. 0 = rarely/never).
Psychological Distress
This was a latent factor made up of two indicators: depression and anxiety.
Depression
The 10-item Center for Epidemiologic Study of Depression questionnaire [36] was used to assess for depression symptoms (e.g., feeling as if everything is an effort, lonely, or fearful) over the past 2 weeks (study α = 0.87). Items were summed (range 0–60) with higher scores reflecting greater depression. This measure has been validated among Latina/o/x individuals [37] and sexual and gender minorities [38].
Anxiety
The 7-item Generalized Anxiety Disorder scale [39] was used to assess for anxiety symptoms (e.g., feeling anxious nervous or on edge, not being able to stop or control worry) over the past 2-weeks (study α = 0.93). Items were summed (range 0–21) with higher scores reflecting greater anxiety. This measure has been validated among Latinx individuals [40] and sexual and gender minorities [41].
Engagement with HIV Prevention Services
This latent factor outcome consisted of individual-level indicators selected based on constructs in the Theory of Planned Behavior: intention, attitudes (stigma), perception of subjective group norms, and perceived control (self-efficacy) for both HIV-testing and PrEP use.
Intention to Use HIV-Testing and PrEP
Participants were asked two questions on a scale from 1 (no intention/engagement) to 11 (maximum intention/engagement) regarding their intention to use PrEP or engage with HIV-testing in the next 6 months [42].
HIV-Testing Stigma
Stigma about HIV testing was assessed using a 6-item measure (study α = 0.87; [43]). Response options were reported on a 5-point Likert-type scale, ranging from 1 (“Strongly Disagree”) to 5 (“Strongly Agree”). Items were averaged with higher scores reflecting less stigma. Sample items include “my family would treat me differently if I test for HIV” or “people might think I have HIV if I test for HIV”.
PrEP Stigma
Stigma about using PrEP was assessed using a 5-item measure (study α = 0.77; [44]). Response options were reported on a 5-point Likert-type scale, ranging from 1 (“Strongly Disagree”) to 5 (“Strongly Agree”). Items were averaged with higher scores reflecting less stigma. Sample items include “people who take PrEP are promiscuous” or “if I were to take PrEP, I would be concerned if my friends found out I was taking it”.
Community Norms Regarding HIV-Testing and PrEP
Community norms regarding HIV-testing and PrEP were assessed with two single items asking participants how many people they know who: (1) have had a recent (past 6 month) HIV test and (2) have taken PrEP. Response options were reported on a 5-point Likert-type scale, ranging from 0 (“Don’t know”) to 4 (“All or almost all”). Responses were dichotomized into 0 = none/few people and 1 = many/all or almost all) to facilitate model fit due to their categorical nature. The HIV-testing norms question [43] was used to develop the PrEP community norms question.
HIV-Testing Self-efficacy
This 6-item Likert scale measure assessed self-efficacy for engaging with HIV-testing (study α = 0.75), which has been validated among SMM populations [45]. Response options ranged from 1 to 5; items were averaged with higher scores reflecting higher self-efficacy. Sample items include “how certain are you that you could get tested at an HIV testing center” or “if you feel fear about your HIV test results, how certain are you that you could be tested for HIV?”.
PrEP Self-efficacy
This 8-item Likert scale measure assessed for self-efficacy for taking PrEP (study α = 0.83) and can be used regardless of whether someone is currently taking PrEP or not. Response options ranged from 1 to 5; items were averaged with higher scores reflecting higher self-efficacy. The questionnaire has been validated among SMM populations [43]. Sample items include “how difficult would it be for you to seek out more information about PrEP to decide if it is right for you?” or “How difficult would it be for you to visit a doctor who can provide PrEP?”.
Data Analysis
Analyses were conducted in Mplus version 8 [46]. To satisfy the assumptions of linear regression analyses via structural equation modeling, descriptive statistics were assessed for all variables included in the analyses, including the distribution of any scale scores. Linearity, normality, and homoscedasticity were all met. The primary data analytic plan was hybrid structural equation modeling.
First, a measurement model was constructed using confirmatory factor analysis (CFA) for the two latent endogenous variables in the model, psychological distress and HIV-prevention engagement. Next, after the two measurement models were established, a formative factor analysis (FFA) was conducted for one exogenous variable in the model, structural life instability. Since a formative construct is under-identified unless it is embedded in a model in which it possesses two outgoing paths (e.g. to psychological distress and HIV-prevention engagement), we could not conduct the formative factor analysis independently without the prior measurement models [47]. Following these guidelines, to maintain sufficient identification in an FFA, the scale for the latent variable must be defined in the formative model by setting a path to one of the indicators. Finally, because the formative approach utilizes a methodological approach in which the factor is created by an estimated weighted sum of the indicators, there is no measurement error parsed out thereby requiring the residual variance of the factor to equal 0.
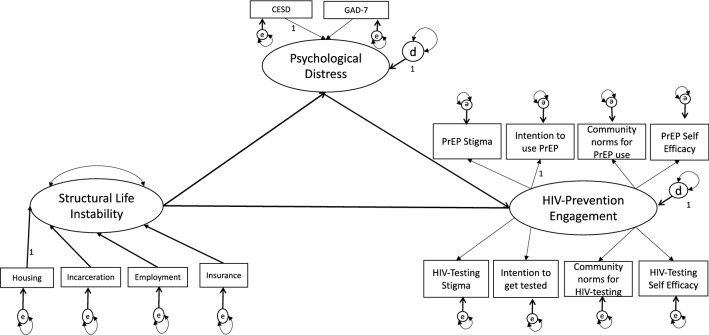
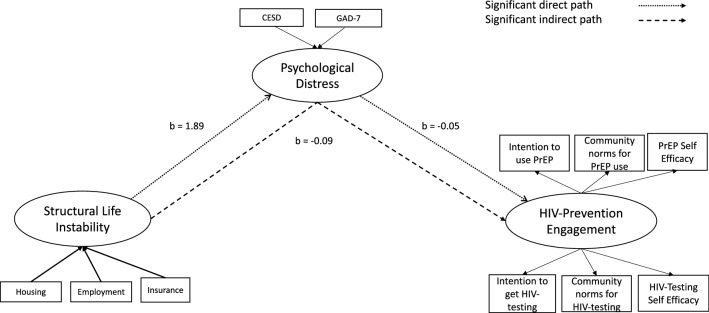
Once the CFA and FFA models were appropriately fitted, a multivariable structural model using weighted least square mean and variance adjusted estimation was constructed to assess the study’s research question. Within the model, direct effects included structural life instability to psychological distress, structural life instability to HIV-prevention engagement, and psychological distress to HIV-prevention engagement. Indirect effects included structural life instability to HIV-prevention engagement via psychological distress. The proposed and initially tested model is presented in Fig. 1 and the final model is presented graphically in Fig. 2. Chi-Square test of model fit (χ2; p > 0.05), Root mean squared error of approximation (RMSEA; < 0.06), comparative fit index (CFI; > 0.95), and standardized root mean square residual (SRMR; < 0.08) were used as model fit indices.
Fig. 1.
Proposed and initially tested hybrid structural equation model examining how structural life instability affecting HIV-prevention engagement via psychological distress among Latino sexual minority men
Fig. 2.
Simplified final hybrid structural equation model examining how structural life instability affecting HIV-prevention engagement via psychological distress among Latino Sexual Minority Men
Results
Participant Characteristics
Most participants identified as White-Latino (79.3%), self-identified as gay (83.8%), and were on average 31.99 years old (SD = 8.32). Most (80.3%) completed the survey in English. Full participant characteristics are shown in Table 1 while correlations between variables are shown in Table 2.
Table 1.
Participant characteristics and factor loadings for latent variables (N = 290)
| Demographics | M (SD) or n (%) |
|---|---|
| Age | 31.99 years (8.32) |
| Race/ethnicity | |
| White-Hispanic/Latino | 230 (79.3%) |
| Black-Hispanic/Latino | 14 (4.8%) |
| Asian-Hispanic/Latino | 2 (0.7%) |
| Indigenous-Hispanic/Latino | 11 (3.8%) |
| Multiracial-Hispanic/Latino | 26 (9.0%) |
| Sexual orientation | |
| Gay | 243 (83.8%) |
| Bisexual | 26 (9.0%) |
| Other | 19 (6.4%) |
| Structural life instability indicators | |
|---|---|
| Housing instability (stressed about paying rent/mortgage, etc.)a | 187 (64.5%) |
| Currently employed | 212 (73.1%) |
| Currently insured | 219 (75.5%) |
| History of incarceration | 33 (11.4%) |
| Psychological distress indicators | |
|---|---|
| Depression (CESD)b | 11.33 (96.90) |
| Anxiety (GAD-7)c | 8.57 (6.23) |
| HIV-prevention engagement indicators | |
|---|---|
| Intention to use PrEPd | 5.82 (4.08) |
| Intention to HIV-testd | 8.08 (3.93) |
| Community norms around PrEPe | 210 (72.4%) |
| Community norms around HIV-testinge | 206 (71.0%) |
| PrEP self-efficacyg | 3.19 (0.60) |
| HIV-testing self-efficacyg | 3.92 (0.77) |
| PrEP stigmaf | 3.98 (0.84) |
| HIV-testing stigmaf | 4.33 (0.75) |
aHigher scores = more stressed about paying
bRange 0–60, higher scores = greater depressive symptoms
cRange 0–21, higher scores = greater anxiety symptoms
dRange 0–11, higher scores = greater intention to engage in behavior change
eKnow none/few people on PrEP and tested for HIV in last year
fRange 1–5, higher scores = more self-efficacy
gRange 1–5 = higher scores = less stigma
Table 2.
Correlation matrix of variables in a priori model
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Intention to use PrEP | 1 | |||||||||||||
| 2. PrEP self-efficacy | 0.26 | 1 | ||||||||||||
| 3. PrEP stigma | − 0.05 | − 0.03 | 1 | |||||||||||
| 4. Community norms about PrEP | 0.33 | 0.26 | − 0.10 | 1 | ||||||||||
| 5. Intention to HIV-test | 0.53 | 0.14 | 0.02 | 0.18 | 1 | |||||||||
| 6. HIV-testing self-efficacy | 0.03 | 0.44 | − 0.07 | 0.30 | 0.11 | 1 | ||||||||
| 7. HIV-testing stigma | 0.05 | − 0.01 | 0.36 | 0.08 | 0.03 | − 0.06 | 1 | |||||||
| 8. Community norms about HIV-testing | 0.32 | 0.27 | − 0.03 | 0.71 | 0.25 | 0.20 | 0.01 | 1 | ||||||
| 9. Depression | − 0.04 | − 0.31 | 0.05 | − 0.05 | − 0.10 | − 0.21 | − 0.04 | − 0.19 | 1 | |||||
| 10. Anxiety | − 0.07 | − 0.31 | 0.05 | − 0.04 | − 0.13 | − 0.17 | − 0.02 | − 0.06 | 0.82 | 1 | ||||
| 11. Housing instability | 0.08 | − 0.24 | − 0.07 | 0.15 | 0.05 | − 0.22 | 0.01 | 0.09 | 0.29 | 0.31 | 1 | |||
| 12. History of incarceration | 0.03 | − 0.06 | − 0.01 | − 0.03 | 0.01 | 0.01 | − 0.01 | 0.01 | 0.02 | 0.02 | 0.10 | 1 | ||
| 13. Insurance | − 0.02 | − 0.05 | − 0.06 | 0.03 | 0.15 | − 0.04 | − 0.03 | 0.08 | − 0.06 | − 0.12 | 0.10 | 0.18 | 1 | |
| 14. Working status | − 0.04 | − 0.06 | − 0.01 | − 0.02 | 0.03 | − 0.02 | 0.01 | − 0.05 | 0.16 | 0.07 | 0.07 | 0.22 | 0.14 | 1 |
Preliminary Analysis
CFA Measurement Model
The psychological distress and HIV-prevention engagement latent factors were specified in a measurement model. The a priori measurement model for HIV-prevention engagement latent factor resulted in poor model fit, χ2(19) = 96.58, p < 0.001; CFI = 0.73; RMSEA = 0.12; SRMR = 0.11, leading to the removal of the PrEP and HIV-testing stigma indicators from the final measurement model due to low factor loadings. Additionally, after examining the data (i.e., model modification indices and normalized residuals), additional covariances between residuals were added in an iterative fashion to improve model fit (i.e., largest absolute value normalized residuals were added first). This continued iterative re-specification resulted in a model that appropriately fit the data, χ2(10) = 9.79, p = 0.46; CFI = 1.00; RMSEA < 0.001; SRMR = 0.02, and thus retained as the final measurement model (Fig. 2). See Table 3 for final included covariances between indicators.
Table 3.
Final model results (N = 290)
| Models | β | b | SE(b) | b/SE | p value |
|---|---|---|---|---|---|
| Structural life instability on | |||||
| Housing instability | 0.94 | 1.00 | – | – | – |
| Employment status | 0.28 | 0.82 | 0.45 | 1.80 | 0.07 |
| Insurance status | 0.30 | 0.91 | 0.46 | 1.95 | 0.05 |
| Psychological distress | |||||
| Depression | 0.94 | 1.00 | – | – | – |
| Anxiety | 0.88 | 0.85 | 0.09 | 9.53 | < 0.01 |
| HIV-prevention engagement | |||||
| Intention to use PrEP | 0.22 | 1.00 | – | – | – |
| PrEP self-efficacy | 0.80 | 0.54 | 0.22 | 2.53 | 0.01 |
| Community norms for PrEP | 0.45 | 0.51 | 0.21 | 2.39 | 0.02 |
| Intention to engage with HIV-testing | 0.19 | 0.86 | 0.38 | 2.25 | 0.03 |
| HIV-testing self-efficacy | 0.55 | 0.48 | 0.20 | 2.41 | 0.02 |
| Community norms for HIV-testing | 0.41 | 0.46 | 0.19 | 2.38 | 0.02 |
| Direct effects | |||||
| Structural life instability → Psychological distress | 0.38 | 1.89 | 0.32 | 5.95 | < 0.01 |
| Structural life instability → HIV-prevention engagement | − 0.14 | − 0.09 | 0.06 | − 1.57 | 0.12 |
| Psychological distress → HIV-prevention engagement | − 0.35 | − 0.05 | 0.02 | − 2.18 | 0.03 |
| Indirect effect | |||||
| Structural life instability → Psychological distress → HIV-prevention engagement | − 0.13 | − 0.09 | 0.04 | − 2.19 | 0.03 |
| Covariances | |||||
| Intention to use PrEP with intention to HIV-test | 0.51 | 7.91 | 2.26 | 3.50 | < 0.01 |
| Intention to use PrEP with community norms for PrEP | 0.28 | 1.06 | 0.33 | 3.17 | < 0.01 |
| Intention to use PrEP with community norms for HIV-testing | 0.28 | 1.03 | 0.33 | 3.10 | < 0.01 |
| Intention to use PrEP with insurance status | − 0.20 | − 0.35 | 0.12 | − 3.02 | < 0.01 |
| Intention to use PrEP with housing instability | 0.15 | 0.72 | 0.33 | 2.17 | 0.03 |
| Community norms for PrEP with community norms for HIV-testing | 0.67 | 0.58 | 0.08 | 7.73 | < 0.01 |
| Community norms for PrEP with housing instability | 0.31 | 0.35 | 0.11 | 3.25 | < 0.01 |
| Community norms for HIV-testing with intention to HIV-test | 0.20 | 0.71 | 0.33 | 2.17 | 0.03 |
| Insurance status with intention to HIV-test | − 0.16 | − 0.25 | 0.12 | − 2.07 | 0.04 |
| Insurance status with employment status | − 0.14 | − 0.03 | 0.01 | − 2.61 | 0.01 |
χ2(30) = 37.73, p = 0.16; CFI = 0.98; RMSEA = 0.03; SRMR = 0.04
FFA Within Structural Model
Given that the fit of the FFA (life instability) needed to be assessed within the structural model, fit indices were examined for this latent prior to examination of the rest of the model. The proposed structural model (see Fig. 1) was tested, and results demonstrated poor model fit, χ2(37) = 55.00, p = 0.03; CFI = 0.94; RMSEA = 0.04; SRMR = 0.07. Based on poor factor loadings for the history of incarceration indicator and suggestions from the data (i.e., model modification indices and normalized residuals), history of incarceration was dropped as an indicator and covariances between residuals were added in an iterative fashion based on relevant modification indices to improve model fit (i.e., largest absolute value normalized residuals were added first). The new model exhibited sufficient model fit, χ2(23) = 20.74, p = 0.60; CFI = 1.00; RMSEA < 0.001; SRMR = 0.03. Parameter estimates were examined and any covariances that were non-significant were removed. Removing the nonsignificant covariances did not worsen model fit, χ2∆(7) = 6.99, p = 0.43, and the respecified more parsimonious model fit the data, χ2(30) = 37.73, p = 0.16; CFI = 0.98; RMSEA = 0.03; SRMR = 0.04, and was thus retained. See Table 3 for final included covariances between indicators.
Primary Analysis: Structural Model
Table 3 and Fig. 2 present the results from the final model. There was a significant direct positive effect from structural life instability to psychological distress (b = 1.89, SE = 0.32, p < 0.001, 95% CI [(1.27, 2.51]) such that increases in structural life instability were associated with increases in psychological distress among LSMM participants. Also as hypothesized, there was a significant direct negative effect from psychological distress to HIV-prevention engagement (b = − 0.05, SE = 0.02, p < 0.05, 95% CI [− 0.09, − 0.01]) such that increases in psychological distress were associated with decreases in HIV-prevention engagement among LSMM participants. Furthermore, structural life instability had a significant indirect negative effect on HIV-prevention engagement via psychological distress (b = − 0.09, SE = 0.04, p < 0.05, 95% BTSP [− 0.17, − 0.01]) such that increases in structural life instability were associated with decreases in HIV-prevention engagement through increased psychological distress. Of note, contrary to our second hypothesis for objective A, when we removed the intermediary variable from the model, the direct effect from structural life instability to HIV-prevention engagement (b = − 0.09, SE = 0.06, p > 0.05, 95% CI [− 0.21, 0.02]) was no longer statistically significant.
Discussion
The current study employed a hybrid structural equation model to investigate the effects of structural life instability on components of biomedical HIV-prevention engagement among a community sample composed of people with multiple marginalized identities in a U.S. HIV epicenter. Current findings add to the literature by establishing an inverse relationship such that as structural life instability increased, engagement with biomedical HIV-prevention services decreased, through the effects of increases in psychological distress among LSMM. Findings provide evidence to inform future research exploring more complex risk factor frameworks that include both structural and individual level factors to better understand possible drivers of biomedical HIV-prevention engagement among LSMM.
Overall, this data suggests that structural inequities are primary motivators of biomedical HIV-prevention engagement disparities among LSMM in an epicenter of the HIV-epidemic in the Southeast U.S. Although implementing mid-level structural interventions that focus on altering norms, changing intentions, and bolstering self-efficacy may improve engagement with biomedical HIV-prevention services in the short-run, larger systems of inequity (e.g., income inequality, unfair immigration policies, differential access to healthcare services, inadequate educational systems) must be dismantled so to bolster LSMM’s sense of agency more permanently in the long-term. Policy makers should work alongside researchers and members of these underserved communities to identify how the specific systems, structures, and social contexts of their given city may affect access to biomedical HIV-prevention services for LSMM and other marginalized groups and in turn, advocate for structural change at the societal level (e.g., increasing access to health insurance and regulated employment with fair pay).
To complement systemic structural changes that could influence disparities in HIV-prevention engagement among LSMM, theories that specifically focus on an individuals’ agency in decision making, such as the Theory of Planned Behavior [30] or self-efficacy [33], may be useful to holistically frame the relationship between structural life instability and engagement in biomedical HIV-prevention behaviors among LSMM. Although measures associated with PrEP and HIV-testing stigma—factors that reflect personal attitudes toward behavior—were not retained in the final hybrid structural equation model, the final model does include indicators that mirror the other relevant components from these theories including perceived control (e.g. PrEP and HIV-testing self-efficacy), intention to engage in the behavior (e.g. intention to use PrEP and get HIV tested), and perception of subjective group norms (e.g. community norms associated with PrEP and HIV testing). These findings not only parallel past research [48, 49] on theories that focus on the mechanisms by which an individual’s sense of agency can help to better understand individuals’ engagement with health behavior change, but also expand these theories by suggesting that factors related to psychological distress and structural life instability may interact with these change components to affect engagement with biomedical HIV-prevention behaviors among LSMM, a marginalized group.
Furthermore, as our data indicates, structural barriers, rather than individual differences, were at the root of LSMM’s lower HIV-prevention engagement. This observation demonstrates the need for researchers, clinicians, and policy makers to synthesize how components of theoretical frameworks that capitalize on individual-level factors (e.g., intentions, psychological distress) can be used as areas to guide intervention at the structural level when evaluating barriers to LSMM’s biomedical HIV prevention engagement rather than putting the onus solely on the individuals to self-motivate. It is possible that an individual level factor like psychological distress is the mechanism through which more structural indicators of life instability at the community or societal level operate to impact LSMM’s intentions to engage with biomedical HIV prevention services. Therefore, a multilevel (e.g., structural and individual) approach may be needed, wherein resources are allocated to offer support in reducing structural life instability at the community and societal levels thereby improving general mental health well-being within LSMM communities at the individual level rather than only focusing on changing an individual’s perception as a way of reducing barriers to accessing care.
Limitations of the study should be noted. First, due to the cross-sectional nature of the data, issues related to bidirectionality or opposite directionality may have occurred since neither temporal order nor causality can be determined. Second, although the path model identified (Fig. 2) was based on a review of the current empirical literature, it is possible that an alternative model may also adequately explain the complex interplay of risk factors for lower HIV-prevention engagement among LSMM living in an U.S. HIV epicenter. Third, as with most studies, it is crucial to consider the generalizability of our findings. Although the parent study centered on the experiences of South Florida based LSMM aged 18 years or older and, therefore, caution should perhaps be taken when generalizing to other populations, this model may be useful in exploring potential factors and mechanisms associated with intention to engage in HIV-prevention behaviors among other groups affected by HIV. Existing health behavior change models often fail to account for mental health (i.e., psychological distress) or socio-environmental context (i.e., life instability) which limits exploration into the experiences of sub-populations at increased susceptibility for HIV-acquisition. We encourage future research to expand on this current work by similarly incorporating multiple levels of influence in different populations other than LSMM affected by HIV to extend the reach of these findings in informing public health practice, and addressing HIV disparities. Additionally, because data collection primarily occurred during the COVID-19 pandemic, it is important to acknowledge the potential implications that the pandemic may have had on our findings as it relates to the structural inequities, psychological distress, and engagement with HIV-prevention behaviors experienced by LSMM in our study, as has been documented in other work [50, 51]. Finally, although there were re-specifications needed to achieve sufficient model fit, these do not reflect covariance in constructs (i.e., validity of model interpretation), but indicate correlated measurement error between indicators that are likely a consequence of measure structure.
To achieve the Ending the HIV Epidemic goals, it is important to scale up and out HIV-testing and PrEP to LSMM, one of the communities with the highest HIV incidence [16, 46]. Employing a structural equation modeling approach, findings suggest that structural life instability is a driver of psychological distress, an individual level factor, that leads to engagement in constructs related to HIV-prevention behaviors among LSMM living in South Florida, an HIV epicenter. Future research should build upon these findings by continuing to investigate how the interaction between structural and individual level factors may alter intentions to engage in HIV-prevention related health behaviors among LSMM, an often underserved and overlooked population in widespread HIV-prevention research, and by developing culturally-informed interventions and implementation strategies to scale up and out evidence-based HIV-prevention tools and simultaneously address the negative individual level mental health effects of structural factors.
Author Contributions
Conceptualization (EW, TG, AH), formal analysis (EW, TG), funding acquisition (AH, SAS), investigation (EW, TG, AH), methodology (EW, TG, AH), project administration (EW, AH), writing—original draft (EW, TG, AH), writing—review and editing (EW, TG, ES, SAS, AH), visualization (EW).
Funding
Data collection for this study was supported by P30AI073961 (Pahwa) and U54MD002266 (Behar-Zusman). Additional research support was provided by P30MH116867 (Safren). Some of the author time was supported by K24DA040489 (Safren) and K23MD015690 (Harkness). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data Availability
The data that support the findings of this study are available within the article and/or its supplementary materials. All other data are available from the corresponding author, EW, upon reasonable request.
Code Availability
All code for data cleaning and analysis is available upon request from EW.
Declarations
Conflict of interest
Dr. Safren receives royalties from Oxford University Press, Guilford Publications, and Springer/Humana press for books on cognitive behavioral therapy. The authors have no other conflicts of interest to disclose.
Ethical Approval
All study procedures were approved by the University of Miami’s Institutional Review Board.
Consent to Participate
Singed informed consent for study protocols was obtained from all participants.
Consent for Publication
Singed informed consent regarding publishing of participants’ de-identified data was obtained from all participants.
Footnotes
Following the guidance of Dr. del Rio-Gonzalez [2], we use Latino/a/x when referring to the whole community, whereas we use Latino when specifically referring to men. Similarly, we use “sexual minority men” to describe gay, bisexual, and other non-heterosexual men. In some cases, we use the term “men who have sex with men” (MSM) to correspond with the language used in the referenced literature.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CDC. HIV and Gay and Bisexual Men [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2020 Oct 7]. Available from: https://www.cdc.gov/hiv/group/msm/index.html
- 2.del Río-González AM. To Latinx or not to Latinx: a question of gender inclusivity versus gender neutrality. Am J Public Health. 2021;111(6):1018–1021. doi: 10.2105/AJPH.2021.306238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Disease Control and Prevention. Latinos | Race/Ethnicity | HIV by Group | HIV/AIDS | CDC [Internet]. 2019 [cited 2019 Nov 5]. Available from: https://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/index.html
- 4.Martinez O, Lee JH, Bandiera F, Santamaria EK, Levine EC, Operario D. Sexual and behavioral health disparities among sexual minority Hispanics/Latinos: findings from the national health and nutrition examination survey, 2001–2014. Am J Prev Med. 2017;53(2):225–231. doi: 10.1016/j.amepre.2017.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet Lond Engl. 2017;389(10072):941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- 6.Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995;36(1):38–56. doi: 10.2307/2137286. [DOI] [PubMed] [Google Scholar]
- 7.Rhodes SD, Martinez O, Song E-Y, Daniel J, Alonzo J, Eng E, et al. Depressive symptoms among immigrant Latino sexual minorities. Am J Health Behav. 2013;37(3):404–413. doi: 10.5993/AJHB.37.3.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blashill AJ, Brady JP, Rooney BM, Rodriguez-Diaz CE, Horvath KJ, Blumenthal J, et al. Syndemics and the PrEP cascade: results from a sample of young Latino men who have sex with men. Arch Sex Behav. 2020;49(1):125–135. doi: 10.1007/s10508-019-01470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamitani E, Johnson WD, Wichser ME, Adegbite AH, Mullins MM, Sipe TA. Growth in proportion and disparities of HIV PrEP use among key populations identified in the United States national goals: systematic review & meta-analysis of published surveys. J Acquir Immune Defic Syndr. 2020;84(4):379–386. doi: 10.1097/QAI.0000000000002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finlayson T. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men—20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep [Internet]. 2019 [cited 2019 Jul 26]; 68. Available from: https://www.cdc.gov/mmwr/volumes/68/wr/mm6827a1.htm [DOI] [PMC free article] [PubMed]
- 11.Agénor M, Pérez AE, Koma JW, Abrams JA, McGregor AJ, Ojikutu BO. Sexual orientation identity, race/ethnicity, and lifetime HIV testing in a national probability sample of U.S. women and men: an intersectional approach. LGBT Health. 2019;6(6):306–318. doi: 10.1089/lgbt.2019.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall HI, Song R, Tang T, An Q, Prejean J, Dietz P, et al. HIV trends in the United States: diagnoses and estimated incidence. JMIR Public Health Surveill [Internet]. 2017 Feb 3 [cited 2017 Dec 8]; 3(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5315764/ [DOI] [PMC free article] [PubMed]
- 13.Centers for Disease Control. First year geographic focus ending the hiv epidemic: a plan for America [Internet]. 2019 [cited 2019 Nov 5]. Available from: https://www.cdc.gov/endhiv/docs/Ending-HIV-geographic-focus-508.pdf
- 14.Harkness A, Rogers BG, Puccinelli M, Ivardic I, Ironson G, Safren SA. Engaging, retaining, and providing transdiagnostic integrated cognitive–behavioral therapy and motivational interviewing for underserved people with HIV. Psychotherapy. 2020;57(1):15–22. doi: 10.1037/pst0000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harkness A, Bainter SA, O’Cleirigh C, Albright C, Mayer KH, Safren SA. Longitudinal effects of syndemics on HIV-positive sexual minority men’s sexual health behaviors. Arch Sex Behav. 2019;48(4):1159–1170. doi: 10.1007/s10508-018-1329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 17.Latkin C, Weeks MR, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS Behav. 2010;14(2):222–238. doi: 10.1007/s10461-010-9804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007;22(9):1286–1291. doi: 10.1007/s11606-007-0265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levy ME, Wilton L, Phillips G, Glick SN, Kuo I, Brewer RA, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014;18(5):972–996. doi: 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacKellar DA, Hou S-I, Whalen CC, Samuelsen K, Sanchez T, Smith A, et al. Reasons for not HIV testing, testing intentions, and potential use of an over-the-counter rapid HIV test in an internet sample of men who have sex with men who have never tested for HIV. Sex Transm Dis. 2011;38(5):419–428. doi: 10.1097/OLQ.0b013e31820369dd. [DOI] [PubMed] [Google Scholar]
- 21.Philbin MM, Hirsch JS, Wilson PA, Ly AT, Giang LM, Parker RG. Structural barriers to HIV prevention among men who have sex with men (MSM) in Vietnam: diversity, stigma, and healthcare access. PLoS ONE. 2018;13(4):e0195000. doi: 10.1371/journal.pone.0195000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quinn KG. Applying an intersectional framework to understand syndemic conditions among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2022;1(295):112779. doi: 10.1016/j.socscimed.2019.112779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harkness A. Barriers and facilitators to Latino MSM’s engagement in HIV-prevention and behavioral health services: preliminary qualitative findings. Miami: Miami Center for AIDS Research Rapid Fire Seminar Series; 2019. [Google Scholar]
- 24.Maiorana A, Kegeles SM, Brown S, Williams R, Arnold EA. Substance use, intimate partner violence, history of incarceration and vulnerability to HIV among young Black men who have sex with men in a Southern US city. Cult Health Sex. 2021;23(1):37–51. doi: 10.1080/13691058.2019.1688395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191(Supplement_1):S115–S122. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- 26.Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav. 2007;11(2):101–115. doi: 10.1007/s10461-007-9276-x. [DOI] [PubMed] [Google Scholar]
- 27.Clatts MC, Goldsamt L, Yi H, Viorst GM. Homelessness and drug abuse among young men who have sex with men in New York city: a preliminary epidemiological trajectory. J Adolesc. 2005;28(2):201–214. doi: 10.1016/j.adolescence.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts DE. The social and moral cost of mass incarceration in African American communities. Stanford Law Rev. 2003;2004(56):1271. [Google Scholar]
- 29.Reisner SL, Mimiaga MJ, Skeer M, Bright D, Cranston K, Isenberg D, et al. Clinically significant depressive symptoms as a risk factor for HIV infection among black MSM in massachusetts. AIDS Behav. 2009;13(4):798–810. doi: 10.1007/s10461-009-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 31.Becker MH. The health belief model and sick role behavior. Health Educ Monogr. 1974;2(4):409–419. doi: 10.1177/109019817400200407. [DOI] [Google Scholar]
- 32.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–335. doi: 10.1177/109019817400200403. [DOI] [PubMed] [Google Scholar]
- 33.Bandura A, Adams NE. Analysis of self-efficacy theory of behavioral change. Cogn Ther Res. 1977;1(4):287–310. doi: 10.1007/BF01663995. [DOI] [Google Scholar]
- 34.Weinstein ER, Harkness A, Ironson G, Shrader CH, Duncan DT, Safren SA. Life instability associated with lower ART adherence and other poor HIV-related care outcomes in older adults with HIV. Int J Behav Med. 2022 doi: 10.1007/s12529-022-10095-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weinstein ER, Balise R, Metheny N, et al. Factors associated with Latino sexual minority men’s likelihood and motivation for obtaining a COVID-19 vaccine: a mixed-methods study. J Behav Med. 2022 doi: 10.1007/s10865-022-00315-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 37.González P, Nuñez A, Merz E, Brintz C, Weitzman O, Navas EL, et al. Measurement properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): findings from HCHS/SOL. Psychol Assess. 2017;29(4):372–381. doi: 10.1037/pas0000330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herek GM, Cogan JC, Gillis JR, Glunt EK. Correlates of internalized homophobia in a community sample of lesbians and gay men. J Gay Lesbian Med Assoc. 1998;2:17–25. [Google Scholar]
- 39.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 40.Mills SD, Fox RS, Malcarne VL, Roesch SC, Champagne BR, Sadler GR. The psychometric properties of the Generalized Anxiety Disorder-7 Scale in Hispanic Americans with English or Spanish language preference. Cultural Divers Ethnic Minor Psychol. 2014;20(3):463–468. doi: 10.1037/a0036523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Borgogna NC, Brenner RE, McDermott RC. Sexuality and gender invariance of the PHQ-9 and GAD-7: implications for 16 identity groups. J Affect Disord. 2021;1(278):122–130. doi: 10.1016/j.jad.2020.09.069. [DOI] [PubMed] [Google Scholar]
- 42.Stassek L. HIV testing among young Latino men who have sex with men (MSM): the role of HIV-related stigma and internalized homosexual stigma [Internet] [Thesis]. 2014 [cited 2020 Nov 24]. Available from: https://digital.lib.washington.edu:443/researchworks/handle/1773/26326
- 43.Andrinopoulos K, Hembling J, Guardado ME, de Maria HF, Nieto AI, Melendez G. Evidence of the negative effect of sexual minority stigma on HIV testing among MSM and transgender women in San Salvador, El Salvador. AIDS Behav. 2015;19(1):60–71. doi: 10.1007/s10461-014-0813-0. [DOI] [PubMed] [Google Scholar]
- 44.Walsh JL. Applying the information–motivation–behavioral skills model to understand PrEP intentions and use among men who have sex with men. AIDS Behav. 2019;23(7):1904–1916. doi: 10.1007/s10461-018-2371-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Solorio R, Norton-Shelpuk P, Forehand M, Montaño D, Stern J, Aguirre J, et al. Tu Amigo Pepe: evaluation of a multi-media marketing campaign that targets young Latino immigrant MSM with HIV testing messages. AIDS Behav. 2016;20(9):1973–1988. doi: 10.1007/s10461-015-1277-6. [DOI] [PubMed] [Google Scholar]
- 46.Muthén LK, Muthén BO. Mplus User′s Guide. 7th Edn. Los Angeles, CA: Muthén & Muthén; 2017.
- 47.Bollen KA, Davis WR. Causal indicator models: identification, estimation, and testing. Struct Equ Model Multidiscip J. 2009;16(3):498–522. doi: 10.1080/10705510903008253. [DOI] [Google Scholar]
- 48.Vissman AT, Hergenrather KC, Rojas G, Langdon SE, Wilkin AM, Rhodes SD. Applying the theory of planned behavior to explore HAART adherence among HIV-positive immigrant Latinos: elicitation interview results. Patient Educ Couns. 2011;85(3):454–460. doi: 10.1016/j.pec.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 49.Meadowbrooke CC, Veinot TC, Loveluck J, Hickok A, Bauermeister JA. Information behavior and HIV testing intentions among young men at risk for HIV/AIDS. J Assoc Inf Sci Technol. 2014;65(3):609–620. doi: 10.1002/asi.23001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harkness A, Weinstein ER, Atuluru P, Hernandez Altamirano D, Vidal R, Rodriguez-Diaz CE, et al. Latino sexual minority men’s intersectional minority stress, general stress, and coping during COVID-19: a rapid qualitative study. J Gay Lesbian Ment Health. 2022 doi: 10.1080/19359705.2021.1995096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Harkness A, Weinstein ER, Atuluru P, Mayo D, Vidal R, Rodriguez-Diaz C, et al. Latinx sexual minority men’s access to HIV and behavioral health services during COVID-19: barriers, facilitators, and implications for innovation. J Assoc Nurses AIDS Care. 2021 doi: 10.1097/JNC.0000000000000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available within the article and/or its supplementary materials. All other data are available from the corresponding author, EW, upon reasonable request.
All code for data cleaning and analysis is available upon request from EW.