Abstract
COVID19 has emerged as one of the worst pandemics in the history of mankind. Several vaccines have been approved by different government agencies worldwide, but data on their efficacy and safety are limited, and distribution remains a massive challenge. As per WHO, personal immunity is vital for protection against COVID19. Earlier, Vitamin C-mediated pathways have been shown to play critical role in boosting immunity attributed to its antioxidant properties. Recently, the involvement of such pathways in protection against COVID19 has been suggested. The controlled doses of Vitamin C administered through intravenous (IV) injections are being studied for determining its role in the prognosis of COVID19. In this article, we have discussed the potential role of Vitamin C in the management in COVID19 patients and presented recent clinical trials data. Additionally, we have elaborated the possibility of administering Vitamin C through inhalers in order to achieve local high concentration and the challenges of such approach.
Keywords: COVID19, Vitamin C, Therapeutic, Nutrition, Susceptibility, Oxidative radicals
1. Introduction
Since time immemorial, plant leaf extracts, soups, and citrus fruits are being administered for different ailments without much understanding of their mechanism, mode of action, and side-effects [[1], [2], [3], [4]]. Several research efforts have backed up few potential home remedies while contesting the claims of many others [5,6]. Interestingly, citrus fruits have showed potential in prevention and prognosis of minor infections including common cold [7,8]. Studies have shown the potential benefits of administering Vitamin C alongside antiviral treatment especially in vitamin deficient individuals. Recent studies have shown the inhibitory activity of Vitamin C in viral replication, including the replication of SARS-CoV-2 virus [9]. Due to lack of target specific therapeutics, vaccines are widely regarded as the key to overcome the COVID-19 pandemic however due to time constraints in its development, its efficacy and side-effects are still being studied and evaluated [10]. In the light of it, reviewing the role of Vitamin C in plausible prevention and prognosis of COVID19 becomes even more needed. Linus Pauling (recipient of two unshared Nobel Prizes) strongly advocated Vitamin C's role in protection against infection and building immunity of the body [11,12]. However, critics countered that utility of megadose supplementations and pointed out the mode of action was not clear and such dose may only lead to “expensive urine”. The FDA (Food and Drug Administration) recommends 75–90 mg/day of Vitamin C for adults in contrast to Pauling’s mega dose of 1–2 g/day [[13], [14], [15]]. According to the dietary reference intakes (DRIs), dietary recommendation varies with age and gender [16]. Smokers need 35 mg more than the required amount due to oxidative stress. Even though Vitamin C is an essential nutrient, the human body cannot store it. Intake of more than the dietary recommendation of Vitamin C can result in diarrhea, nausea, vomiting, heartburn, abdominal cramps, headache, kidney stone, cardiovascular problems, and insomnia [17]. The amount above the tolerable upper intake level has been proven to cause more harm than benefits. Health hazards due to the intake of excessive amount of Vitamin C have been observed to be more prevalent in people with other health conditions like renal diseases. Absorption of high dosage of Vitamin C can potentially cause oxidative damage and hemolysis in infants. In children and adolescence, side effects like stomach pain, skin rash, headache, nausea, and diarrhea have been reported in different clinical studies [18]. In case of infections, the production of cytokines is triggered as the first line of defense; however, in the severe cases of COVID19, the production of cytokines becomes uncontrolled to the extent that it starts damaging the healthy cells [[19], [20], [21], [22], [23]]. Further, self-damage is intensified by the high levels of free oxidative radicals, which act upon own cells (in lungs) instead of foreign particles like the virus [[24], [25], [26]]. Can Vitamin C be used as a natural anti-oxidant to restrain the harmful effects of oxidative radicals and cytokine storms? We will cover this aspect with an illustration of both benefits and caveats of such administration in this article. Many studies have suggested a correlation between plasma levels of Vitamin C and the subject's oxidative stress levels [[27], [28], [29]]. It is widely accepted that Vitamin C supplementation has positive implications on the prognosis of subjects with acute respiratory distress [30] but the molecular details are not well-understood and the subject requires more investigation. Recently, several clinical trials on the usage of higher dosage of Vitamin C have been concluded. It has been showed that patients administered with 200 mg/kg per day (high dosage, n = 8) and 50 mg/kg per day (low dosage, n = 8) of Vitamin C showed lesser sequential organ failure assessment (SOFA) scores as supported by the lower levels of pro-inflammatory markers in comparison to the placebo group (n = 8) under a randomized double blind placebo-controlled study [29,[31], [32], [33], [34], [35]]. Hemelia and Chalker conducted a clinical trial on critical patients with sepsis-induced ARDS (Acute respiratory distress syndrome) (n = 167) for evaluating the effects of Vitamin C (200 mg/kg per day) administered for four days. Though the SOFA scores and levels of such patients' inflammatory markers were similar to the placebo group, it was observed that the 28-day mortality was lower in the treatment group (29.8% versus 46.3%, P-value- 0.03) [36]. Interestingly, in another study, vitamin C and thiamine administration [intravenous vitamin C (50 mg/kg, maximum single dose 3 g) and thiamine (200 mg) in every 12 h for 48 h] did not improvise organ function in comparison to the placebo during early septic shock [37]. Vitamin C administered patients had better survival in intensive care units and were more likely to be discharged from hospitalization [36]. In another study, Vitamin C was administered along with the combination of with/without thiamine and hydrocortisone to the patients with sepsis and pneumonia [[38], [39], [40], [41]]. They reported reduced mortality, lower risk of progression to organ failure, and improved radiographic findings in the treated patients compared to the control. Several ongoing studies are evaluating the role of Vitamin C and its combination with melatonin for treating COVID19 patients [[42], [43], [44]]. The committed timeline for completion of this trial has been claimed to be at the end of December 2021 [45]. The other common complications of COVID19 include lung and cardio pathological related issues due to micro thrombi formation and coagulopathy [46]. The latter conditions were investigated by measuring the D-dimer levels in the blood sample of COVID19 patients (with 30% of FiO2 or more-requirement) [47]. Importantly, a case study has shown the reduction in levels of D-dimer and the decline of capillary plugging and microthrombi formation in subjects administered with Vitamin C (intravenously) [48]. The thrombotic complications of COVID19 patients also implicated the neutrophil extracellular traps (NETs) [49]. Interestingly, the administration of Vitamin C attenuated the formation of NETs in the sepsis model [50]. The WHO (World Health Organization) has described several scientific knowledge gaps in the clinical research outcome of the COVID19 pandemic [51]. On the same note, the WHO has highlighted the importance of Vitamin C administration in critically ill patients and elaborated its potential effects on reduction of the duration of mechanical ventilation and the number of days patients stay in ICU (intensive care unit) [36,52]. It has been suggested that the individuals with deficiency of Vitamin C are more susceptible towards the corona virus [53,54]. WHO observed and noted a significant increase in the production of Vitamin C and Remdesivir by the pharmaceutical companies across the world [[55], [56], [57]]. However, no clear indications on consumptions and dosages have been suggested that may lead to the variable dosages being advocated in different countries while benefits of Vitamin C are still being contested. The objective of this article was to review the role of Vitamin C in potential molecular cascades associated with host immune response against COVID19 and to discuss associated clinical trials and their limitations, if any.
2. Vitamin C modulates immune cells, cytokines and cytokine storm
Previously, Vitamin C has been implicated in immune cell differentiation and proliferation [58,59]. It is known to modulate the gene regulation in B- and T-cells [[60], [61], [62], [63]]. Vitamin C deficiency has been shown to weaken immunity and thereby increase the susceptibility to infection [58,64]. Vitamin C exerts its antioxidant effects by acting as an electron donor and protects biomolecules like proteins, lipids, carbohydrates and nucleic acids [65,66]. Vitamin C also acts as a cofactor of enzymes monooxygenase and dioxygenase enzymes which are involved in biosynthesis and gene regulation in immune cells [58,66,67]. During phagocytosis, the Vitamin C has been reported to be depleted in neutrophils which change the balance between oxidants and antioxidants, thus impeding its immune response [58,[68], [69], [70]]. As we discussed before, studies have shown that Vitamin C attenuates the oxidative radical generation and affects NFкB (Nuclear factor kappa B) activation in neutrophils [58,71,72]. Vitamin C regulates redox-related cell signaling cascades by the thiol-containing proteins as they are sensitive to the changes in the redox potential in T cells [58]. It is well known that Vitamin C plays a key role in the T cell development and promotes its maturation [60,62]. It has been also reported that Vitamin C mediates faster regeneration of the natural killer cells [73,74]. In COVID19 patients’, lymphocyte count is not stable, and conditions like leukopenia, leukocytosis, and lymphopenia have been most commonly reported [[75], [76], [77], [78]]. Lymphocyte count in COVID19 patients varies with disease severity [79,80]. In severe cases of COVID19, the reduction in the cell count of CD4+ and CD8+ receptor cells has been noted in patients [[81], [82], [83]]. The involvement of Vitamin C in the regeneration and maturation of lymphocytes further strengthens the hypothesis for potential of Vitamin C in the treatment/prognosis of COVID19 [[84], [85], [86]]. The first line of defense includes natural killer cells, and once they are activated, it carries out cytotoxic degranulation and produces inflammatory cytokines such as IFNγ (Interferon gamma) and TNFα (Tumour necrosis factor alpha) [[87], [88], [89]]. Interestingly, levels of both IFNγ and TNFα have been reported to be reduced in COVID19 patients [90,91]. Other cytokines and receptors involved in the development of natural killer cells in COVID19 subjects should be further studied.
After infection, the SARS-CoV-2 virus replicates within the host epithelial cell. For this, it uses the biochemical machinery of the host cell. More recently, bacterial second messengers like (p)ppGpp [[92], [93], [94], [95]] have been shown to modulate the transcription of COVID19 genome though the evolutionary link which is not clear. Macrophages and neighboring endothelial and epithelial cells recognize the infected cells and release pro-inflammatory cytokines. These chemokines further recruit monocytes, macrophages, and T cells to the infection site. T cells produce IFNγ and elicit antiviral immune response. CD4+ T helper cells interact with the CD8+ T cells, mediate cytotoxic response, and kill the infected cells. CD8+ T cells directly recognize the viral peptides on infected cell’s surface and mediate apoptosis to prevent the spread of the virus. Additionally, a specialized subset of CD4+ T cells called follicular helper T cells induces B cells to produce antibodies by cytokines release through cell–cell interactions [96]. T cell development is a highly controlled process that occursin the thymus, and the mature T cells express either CD4 or CD8 receptor cells corresponding to the T helper cells or T cytotoxic cells (Fig. 1 ). Shah et al. observed that an immature T cell lacks the expression of CD4 and CD8 receptors and called it as “double negative” (DN) cells [97,98]. Kouakanou et al. observed that Vitamin C would enhance the T cell differentiation and proliferation in vitro [59]. It has been observed that Vitamin C is also required to transition double negative precursors to “double positive”cells (DP, CD4+/CD8+) [60,97,98]. José E. Belizário et al. reported that supplementation of Vitamin C in mice lead to the increase in the number of naive T cells, memory T cells in the spleen, and mature T cells in the thymus [99,100]. In the mousemodel, Th2 (T helper type 2) to Th1 (T helper type 1) immune shift has been observed corresponding to the Vitamin C levels. In 2018 Gwendolyn et al. conducted a study on Vitamin C in the mouse model, which was administered with 2,4,-dinitro-I-fluorobenzene (DNFB), and observed higher levels of Th1 cytokines (TNF-α and IFN-γ) and lower levels of Th2 cytokines (IL-4) [101]. It was noted that Vitamin C mediated the production of CD8+ memory T cells and by stimulating cytokines by dendritic cells (DC) in the mouse model. Interestingly, Vitamin C also has a role in the epigenetic regulation, where it acts as a cofactor for ten eleven translocation (TET) family of proteins that has a role in the DNA demethylation in the embryonic stem cells. An in-vitro study has observed an increase in production of IgM antibody in Vitamin C supplemented mice. Another study conducted on guinea pigs showed increased levels of immunoglobulin upon Vitamin C supplementation. Specifically, a direct correlation between Vitamin C concentration and the serum levels of IgG and IgM was observed. W Prinz et al. observed an increased level of IgG antibody in healthy volunteers after administration of Vitamin C for 1 week. The latter study concluded that Vitamin C helps in mediating B cell function [102,103].
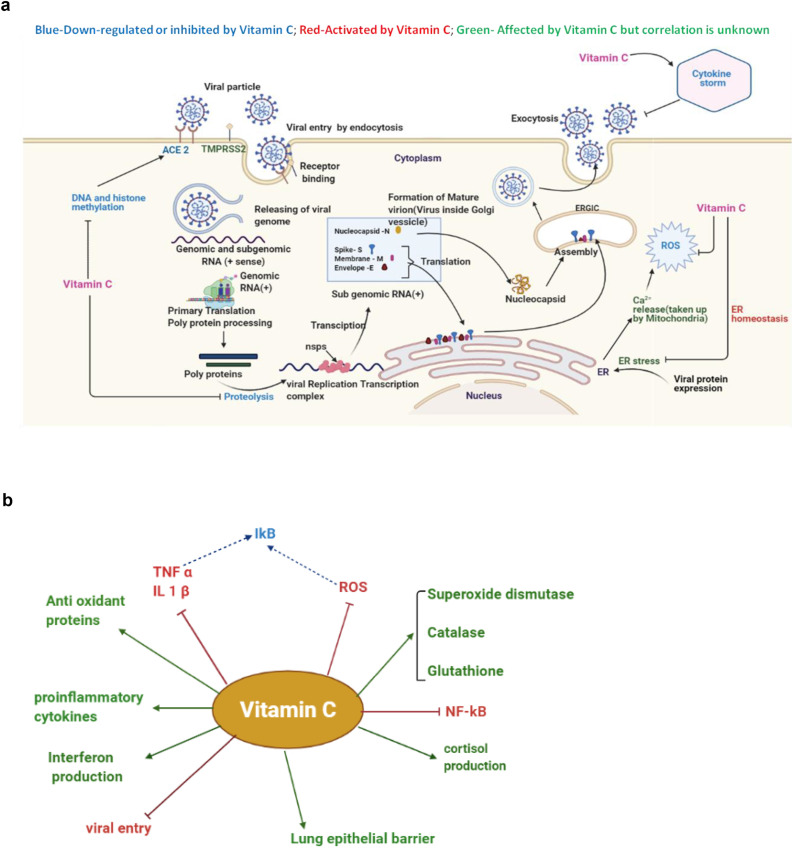
Fig. 1.
a, Schematic view of SARS-CoV-2 Infection cycle-The virus particle first binds with the host cell receptor angiotensin-converting enzyme 2 (ACE2) receptor by its spike protein S1 subunit. Virus particle enters into the cytoplasm by acid-dependent proteolytic cleavage of S protein by furin, cathepsin, and transmembrane protease, serine 2 (TMPRSS2). Upon entry into the cytoplasm, virus particles release the genome. Then, the replicase enzyme is translated from the genomic RNA, followed by the assembly of viral replication–transcription complexes. In the cytoplasm, nucleocapsid (N Protein) interacts with hydrophobic M proteins (envelope protein) in the endoplasmic reticulum-Golgi intermediate compartment (ERGIC) and leads to the assembly of the virion. Mature virions bud from the membranes of the ERGIC and released by the exocytic pathway (nsps: non-structural proteins, ER: endoplasmic reticulum; genes represented in blue colour (ACE2) in Fig. 1a are down regulated by Vitamin C [[107], [108], [109]]) [110,111].1b: Schematic view of the potential function of Vitamin C in the state of COVID19 (figure represented has been created with BioRender.com and Microsoft PowerPoint).
Vitamin C mediates inflammation, and it has a role in the regulation of the expression of systemic and leukocyte-derived cytokines. Vitamin C plays a vital role in the neutrophil function and protection against toxicity by superoxides. It affects cell-mediated immune response more than the humoral immune response [104]. Importantly, it has a significant role in the regulation of the synthesis of type 1 interferon during immune response in viral infection. Many ongoing clinical trials are being carried out to determine if Vitamin C's administration as the potential intervention can facilitate treatment or prognosis of COVID19. A study conducted in Quebec, Canada (ClinicalTrials.gov ID NCT04401150) has shown a reduction in mortality and morbidity among patients who have been admitted with COVID19 upon Vitamin C administration. The elevated inflammatory markers lead to cytokine storms, whereas Vitamin C's anti-inflammatory and antioxidant activities can counter their effects. The Vitamin C dosage depends on the medical condition, treatment process, patient’s age, and administration route. For reasons described before, the average Vitamin C dosage for treatment is determined by further adjusted by considering several parameters like estimated average requirement (EAR), adequate intake level, tolerable upper intake level (ULs), and the recommended dietary allowance (RDA) [105,106].
3. Vitamin C protects against oxidative radicals
The oxidative damage due to the critical imbalance between free radical generation and antioxidant defenses is not desirable [112]. The oxidative stress usually arises from an imbalance between free radical production and lack of antioxidants, and it is associated with damage to a wide range of molecular species, including lipids, proteins, and nucleic acids [113]. In addition to infections, tissue injury, heart-related injuries, and excessive exercise often lead to short-term oxidative stress. In turn, the damaged tissues produce enzymes such as xanthine oxidase, lipoxygenase, cyclooxygenase, etc., that are capable of producing oxidative radicals [113]. Reactive oxygen species (ROS) have been implicated in the induction and complications of diabetes mellitus, age-related eye disease, and neurodegenerative disorders such as Parkinson’s disease [114]. Vitamin C is an effective water-soluble antioxidant, and numerous studies have reported that it influences phagocytosis and chemotaxis of leukocytes [58,115,116].
Vitamin C acts as an electron donor making it an efficient antioxidant. It inhibits the oxidation of other compounds by donating its electrons and getting oxidized. It acts as a reducing agent and neutralizes ROS [117,118]. Vitamin C is known to neutralize reactive oxygen species involved in human diseases. The relevant species include oxidative radicals such as superoxides and nitrogen-oxygen radicals. The antioxidant properties of vitamin C have been demonstrated in invitro [119]. Several studies have suggested that Vitamin C diminishes the rate and severity of bacterial and viral infections suggesting its physiological role [24]. Considering the above points, we hypothesize that Vitamin C may protect from oxidative radicals generated in COVID19 condition.
3.1. Recent clinical studies on antiviral properties of vitamin C
As discussed in previous sections, Vitamin C has been showed to help in prognosis of viral infections [120]. It has been reported that Vitamin C supplementation improved the immunity of patients with viral infections especially when nutrient-deficient, and thereby increased the survival rate in such patients. Hemilä et al. reported that reduction in the incidence, severity, and duration of the common cold upon supplementation with Vitamin C [121]. In another clinical study by Kim et al., in 2018, patients with Herpes zoster infection when administered with Vitamin C along with acyclovir and analgesics for five days resulted in a significant reduction in postherpetic neuralgia (PHN) and reduction in pain thus confirming its potential when complemented with other drugs [122].
The rapid replication rate of SARS-CoV2 is attributed to the presence of two cysteine proteases; PL-pro, a papain-like protease, and Mpro or 3CLpro where 3C-like protease is the major protease. Most interestingly, in 2021, Malla et al. has reported that l-ascorbate inhibits the 3CLpro in vitro by formation of a complex where Vitamin C binds to the active site of the latter.
They concluded that Vitamin C can be used in the near future as antiviral therapy [123].
3.2. Plausibility of the direct delivery of Vitamin C and the potential application of inhalers
The severe complications of COVID19 include hyper inflammation and increased levels of reactive oxidative species (ROS) in the respiratory system [124]. Vitamin C can be toxic at high dosage [14,15,125]. Therefore, inhalers can be an alternative for achieving immediate local high concentration of Vitamin C (if tested for safety and side-effects) [126,127]. Ivo E Pera et al. filed a patent on a dry powdered inhaler (DPI) method for dispensing antioxidant vitamins [128]. Inhalers can ensure proper assimilation of Vitamin C, unlike the oral and intravenous routes. A high concentration of Vitamin C is required to counter free radical accumulation, and it can be easily achieved through inhalers without any toxic effects [127]. The inhalation method can deliver dry micro-fine Vitamin C powder in a single step. Another mode of dispensing is meter dose inhaler (MDI) delivery. The aerosol is delivered with pressure in Metered Dosage inhaler. The high vapor pressure of the propellant used will give the necessary force to generate aerosol droplets. The particles bigger than 1 μl settle in the bronchioles whereas particles smaller than 0.5 μl are exhaled out. DPI is better than MDI considering the précised dosage and delivery [128]. Though Vitamin C is water soluble and can be excreted out by the body but high dosages through IV injections can still have side-effects [14,15]. Through this article, we hypothesize the usage of inhalers as the instrument of delivery can enable high concentration at the target site while curbing the side-effects.
4. Discussion
In this article, the prospective role of Vitamin C against COVID19 has been highlighted. Its antiviral and antioxidative properties have opened a new window for its potential use for COVID19 treatment and prognosis. The properties of vitamins and their role in COVID19 have been well elaborated in the literature. As described in previous sections, recent studies on Vitamin C's role in prognosis, prevention, and infection of COVID19 are promising. However few clinical trials have also contested the potential use of Vitamin C in treating COVID19. In 2020, Hiedra et al. conducted a clinical study on 17 COVID 19 patients where patients administered with Vitamin C observed a significant decrease in the baseline inflammatory markers in patients who have administered Vitamin C however the sample size was small [9]. A recent clinical study conducted by Thomas et al. on 214 adult COVID19 patients has reported no significant reduction in the duration of symptoms upon administration of Vitamin C with zinc gluconate and alone however standard of care may vary from patient to patient in different population which could be the limitation of the study [129]. Malla et al. showed the inhibition of 3CLpro-major protease that can reduce the replication rate of SARS-CoV2 and suggested its potential use as therapeutic [123]. A recent study on 120 critically ill patients with COVID19 described the potential of vitamin C supplementation in increasing the survival of critically ill patients which is promising, but sample size has been small and the Vitamin C levels were not studied at different time points [130]. Another trial on 237 patients concluded that the treatment of COVID19 with HCQ, AZM, and zinc with high dose vitamin C enable better prognosis [131].
Using a nutrient as a therapeutic is a better remedy as they don’t have to undergo the long process of clinical trials and approvals. It is easier to enforce the individual dietary requirement than producing and distributing a new vaccine. Can Vitamin C help in treatment or prognosis is still not clear. Considering Vitamin C's role in immune response, a worldwide large-scale clinical trial is highly recommended for testing Vitamin C's efficacy. Recent reports have revealed that it helps in enhancing the lung epithelial barrier by inducing the transcriptional expression of the protein channels in the alveolar-capillary membrane [58,132]. We would also like to emphasize on the use of inhalers to achieving a higher concentration of Vitamin C at localized infection sites. Since a high dosage of Vitamin C is also toxic, inhalers can be a solution to this toxicity conundrum. Vitamin C has anti-inflammatory, immunomodulatory, antioxidant, and antiviral properties. In COVID19, Vitamin C could play a significant role in the downregulation of cytokines for protecting the endothelium from oxidation injury provided it is tested for efficacy and safety in different large clinical trials. Last but not least, we hypothesize that Vitamin C could have an immense potential against COVID19, and it requires the immediate attention of the worldwide scientific fraternity.
Declaration of competing interest
Authors have no conflict to declare.
Acknowledgments
Neethu RS acknowledges BITS-Pilani, Hyderabad campus for providing institutional Ph.D. fellowship. Dr. Kirtimaan Syal acknowledges BITS-Pilani for providing a research initiation grant (RIG) and Department of Biotechnology, Government of India for Ramalingaswami Re-Entry fellowship and for research funding.
References
- 1.Sarkar T., Salauddin M., Chakraborty R. In-depth pharmacological and nutritional properties of bael (Aegle marmelos): a critical review. J Agri Food Res. 2020;2 [Google Scholar]
- 2.Khameneh B., Iranshahy M., Soheili V., Fazly Bazzaz B.S. Review on plant antimicrobials: a mechanistic viewpoint. Antimicrob Resist Infect Control. 2019;8:118. doi: 10.1186/s13756-019-0559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cowan M.M. Plant products as antimicrobial agents. Clin Microbiol Rev. 1999;12:564–582. doi: 10.1128/cmr.12.4.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharifi-Rad J., Sureda A., Tenore G.C., Daglia M., Sharifi-Rad M., Valussi M., et al. Biological activities of essential oils: from plant chemoecology to traditional healing systems. Molecules. 2017;22 doi: 10.3390/molecules22010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bajpai V. vol. 2013. ISRN Public Health; 2013. (Rise of clinical trials industry in India: an analysis). [Google Scholar]
- 6.Sen S., Chakraborty R. Revival, modernization and integration of Indian traditional herbal medicine in clinical practice: importance, challenges and future. J Tradit Complement Med. 2017;7:234–244. doi: 10.1016/j.jtcme.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matheyambath A.C., Padmanabhan P., Paliyath G. In: Encyclopedia of food and health. Caballero B., Finglas P.M., Toldrá F., editors. Academic Press; Oxford: 2016. Citrus fruits; pp. 136–140. [Google Scholar]
- 8.Lv X., Zhao S., Ning Z., Zeng H., Shu Y., Tao O., et al. Citrus fruits as a treasure trove of active natural metabolites that potentially provide benefits for human health. Chem Cent J. 2015;9:68. doi: 10.1186/s13065-015-0145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hiedra R., Lo K.B., Elbashabsheh M., Gul F., Wright R.M., Albano J., et al. The use of IV vitamin C for patients with COVID-19: a case series. Expert Rev Anti-infect Ther. 2020;18:1259–1261. doi: 10.1080/14787210.2020.1794819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rashedi R., Samieefar N., Masoumi N., Mohseni S., Rezaei N. COVID-19 vaccines mix-and-match: the concept, the efficacy and the doubts. J Med Virol. 2021;94(4):1294–1299. doi: 10.1002/jmv.27463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.REPORTS T.S.A.W. In: Two-Time Nobel Winner Linus C. Pauling Dies at 93 : science: Noted researcher led fight against nuclear weapons and advocated large doses of Vitamin C. times La., editor. California Times; California: 1994. [Google Scholar]
- 12.Pauling L. 1986. How to live longer and feel better. [Google Scholar]
- 13.Ballmer P.E., Reinhart W.H., Jordan P., Buhler E., Moser U.K., Gey K.F. Depletion of plasma vitamin C but not of vitamin E in response to cardiac operations. J Thorac Cardiovasc Surg. 1994;108:311–320. [PubMed] [Google Scholar]
- 14.Syal K., Chatterji D. Vitamin C: a natural inhibitor of cell wall functions and stress response in Mycobacteria. Adv Exp Med Biol. 2018;1112:321–332. doi: 10.1007/978-981-13-3065-0_22. [DOI] [PubMed] [Google Scholar]
- 15.Syal K., Bhardwaj N., Chatterji D. Vitamin C targets (p)ppGpp synthesis leading to stalling of long-term survival and biofilm formation in Mycobacterium smegmatis. FEMS Microbiol Lett. 2017;364 doi: 10.1093/femsle/fnw282. [DOI] [PubMed] [Google Scholar]
- 16.Supplements NIoHOoD. Vitamin C fact sheet for health professionals. National Institute of Health Office of Dietary Supplements; 2020. [Google Scholar]
- 17.Nordqvist J. Vitamin C: why is it important? Med News Today. 2017;219352 [Google Scholar]
- 18.Medicine Io . The National Academies Press; Washington, DC: 2000. Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. [PubMed] [Google Scholar]
- 19.Ye Q., Wang B., Mao J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Costela-Ruiz V.J., Illescas-Montes R., Puerta-Puerta J.M., Ruiz C., Melguizo-Rodriguez L. SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. 2020;54:62–75. doi: 10.1016/j.cytogfr.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Syal K. Possibility of relapse of COVID19 in asymptomatic cases and risk assessment. Indian J Clin Biochem. 2022:1–2. doi: 10.1007/s12291-022-01029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Syal K. Guidelines on newly identified limitations of diagnostic tools for COVID-19 and consequences. J Med Virol. 2021;93:1837–1842. doi: 10.1002/jmv.26673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Syal K. COVID-19: herd immunity and convalescent plasma transfer therapy. J Med Virol. 2020;92:1380–1382. doi: 10.1002/jmv.25870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lobo V., Patil A., Phatak A., Chandra N. Free radicals, antioxidants and functional foods: impact on human health. Pharmacogn Rev. 2010;4:118–126. doi: 10.4103/0973-7847.70902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pham-Huy L.A., He H., Pham-Huy C. Free radicals, antioxidants in disease and health. Int J Biomed Sci. 2008;4:89–96. [PMC free article] [PubMed] [Google Scholar]
- 26.Di Meo S., Venditti P. Evolution of the knowledge of free radicals and other oxidants. Oxid Med Cell Longev. 2020;2020 doi: 10.1155/2020/9829176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnston C.S., Cox S.K. Plasma-Saturating intakes of vitamin C confer maximal antioxidant protection to plasma. J Am Coll Nutr. 2001;20:623–627. doi: 10.1080/07315724.2001.10719159. [DOI] [PubMed] [Google Scholar]
- 28.Sanchez-Moreno C., Dashe J.F., Scott T., Thaler D., Folstein M.F., Martin A. Decreased levels of plasma vitamin C and increased concentrations of inflammatory and oxidative stress markers after stroke. Stroke. 2004;35:163–168. doi: 10.1161/01.STR.0000105391.62306.2E. [DOI] [PubMed] [Google Scholar]
- 29.Popovic L.M., Mitic N.R., Miric D., Bisevac B., Miric M., Popovic B. Influence of vitamin C supplementation on oxidative stress and neutrophil inflammatory response in acute and regular exercise. Oxid Med Cell Longev. 2015;2015 doi: 10.1155/2015/295497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hunt C., Chakravorty N.K., Annan G., Habibzadeh N., Schorah C.J. The clinical effects of vitamin C supplementation in elderly hospitalised patients with acute respiratory infections. Int J Vitam Nutr Res. 1994;64:212–219. [PubMed] [Google Scholar]
- 31.Fowler A.A., 3rd, Syed A.A., Knowlson S., Sculthorpe R., Farthing D., DeWilde C., et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med. 2014;12:32. doi: 10.1186/1479-5876-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fowler A., Truwit J., Hite R., Morris P., Dewilde C., Priday A., et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: the CITRIS-ALI randomized clinical trial. JAMA. 2019;322:1261. doi: 10.1001/jama.2019.11825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hwang S.Y., Park J., Jo I.J., Kim S., Chung sp, Kong T., et al. Combination therapy of vitamin C and thiamine for septic shock in a multicentre, double-blind, randomized, controlled study (ATESS): study protocol for a randomized controlled trial. Trials. 2019;20 doi: 10.1186/s13063-019-3542-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Masse M.-H., Ménard J., Sprague S., Battista M.-C., Cook D.J., Guyatt G.H., et al. Lessening Organ dysfunction with VITamin C (LOVIT): protocol for a randomized controlled trial. Trials. 2020;21:42. doi: 10.1186/s13063-019-3834-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hwang S.Y., Ryoo S.M., Park J.E., Jo Y.H., Jang D.-H., Suh G.J., et al. Combination therapy of vitamin C and thiamine for septic shock: a multi-centre, double-blinded randomized, controlled study. Intensive Care Med. 2020;46:2015–2025. doi: 10.1007/s00134-020-06191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hemila H., Chalker E. Vitamin C can shorten the length of stay in the ICU: a meta-analysis. Nutrients. 2019;11 doi: 10.3390/nu11040708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hwang S.Y., Ryoo S.M., Park J.E., Jo Y.H., Jang D.H., Suh G.J., et al. Combination therapy of vitamin C and thiamine for septic shock: a multi-centre, double-blinded randomized, controlled study. Intensive Care Med. 2020;46:2015–2025. doi: 10.1007/s00134-020-06191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim W.-Y., Jo E.-J., Eom J.S., Mok J., Kim M.-H., Kim K.U., et al. Combined vitamin C, hydrocortisone, and thiamine therapy for patients with severe pneumonia who were admitted to the intensive care unit: propensity score-based analysis of a before-after cohort study. J Crit Care. 2018;47:211–218. doi: 10.1016/j.jcrc.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 39.Hager D.N., Hooper M.H., Bernard G.R., Busse L.W., Ely E.W., Fowler A.A., et al. The Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) Protocol: a prospective, multi-center, double-blind, adaptive sample size, randomized, placebo-controlled, clinical trial. Trials. 2019;20:197. doi: 10.1186/s13063-019-3254-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Balakrishnan M., Gandhi H., Shah K., Pandya H., Patel R., Keshwani S., et al. Hydrocortisone, Vitamin C and thiamine for the treatment of sepsis and septic shock following cardiac surgery. Indian J Anaesth. 2018;62:934–939. doi: 10.4103/ija.IJA_361_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Litwak J.J., Cho N., Nguyen H.B., Moussavi K., Bushell T. Vitamin C, hydrocortisone, and thiamine for the treatment of severe sepsis and septic shock: a retrospective analysis of real-world application. J Clin Med. 2019;8 doi: 10.3390/jcm8040478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sahebnasagh A., Saghafi F., Avan R., Khoshi A., Khataminia M., Safdari M., et al. The prophylaxis and treatment potential of supplements for COVID-19. Eur J Pharmacol. 2020;887 doi: 10.1016/j.ejphar.2020.173530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bahrampour Juybari K., Pourhanifeh M.H., Hosseinzadeh A., Hemati K., Mehrzadi S. Melatonin potentials against viral infections including COVID-19: current evidence and new findings. Virus Res. 2020;287 doi: 10.1016/j.virusres.2020.198108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vlachou M., Siamidi A., Dedeloudi A., Konstantinidou S.K., Papanastasiou I.P. Pineal hormone melatonin as an adjuvant treatment for COVID-19 (Review) Int J Mol Med. 2021;47:47. doi: 10.3892/ijmm.2021.4880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou J.Q., Kleinstein S.H. Position-dependent differential targeting of somatic hypermutation. J Immunol. 2020;205:3468–3479. doi: 10.4049/jimmunol.2000496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jose R.J., Williams A., Manuel A., Brown J.S., Chambers R.C. Targeting coagulation activation in severe COVID-19 pneumonia: lessons from bacterial pneumonia and sepsis. Eur Respir Rev. 2020;29 doi: 10.1183/16000617.0240-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hiedra R., Lo K.B., Elbashabsheh M., Gul F., Wright R.M., Albano J., et al. The use of IV vitamin C for patients with COVID-19: a case series. Expert Rev Anti Infect Ther. 2020;18:1259–1261. doi: 10.1080/14787210.2020.1794819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tyml K. vol. 6. 2017. (Vitamin C and microvascular dysfunction in systemic inflammation. Antioxidants (Basel)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Middleton E.A., He X.Y., Denorme F., Campbell R.A., Ng D., Salvatore S.P., et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mohammed B.M., Fisher B.J., Kraskauskas D., Farkas D., Brophy D.F., Fowler A.A., 3rd, et al. Vitamin C: a novel regulator of neutrophil extracellular trap formation. Nutrients. 2013;5:3131–3151. doi: 10.3390/nu5083131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Organization W.H. In: A coordinated global research roadmap. Organization W.H., editor. World Health Organization; Geneva: 2020. 2019 Novel Coronavirus. [Google Scholar]
- 52.Hemila H., Chalker E. Vitamin C may reduce the duration of mechanical ventilation in critically ill patients: a meta-regression analysis. J Intensive Care. 2020;8:15. doi: 10.1186/s40560-020-0432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simonson W. Vitamin C and coronavirus. Geriatr Nurs. 2020;41:331–332. doi: 10.1016/j.gerinurse.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoang B.X., Shaw G., Fang W., Han B. Possible application of high-dose vitamin C in the prevention and therapy of coronavirus infection. J Glob Antimicrob Resist. 2020;23:256–262. doi: 10.1016/j.jgar.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rosa S.G.V., Santos W.C. Clinical trials on drug repositioning for COVID-19 treatment. Rev Panam Salud Publica. 2020;44:e40. doi: 10.26633/RPSP.2020.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Michienzi S.M., Badowski M.E. Can vitamins and/or supplements provide hope against coronavirus? Drugs Context. 2020;9 doi: 10.7573/dic.2020-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Drugs.com. Drug interactions between remdesivir and vitamin C. Drugs A to Z Drugs.com.
- 58.Carr A.C., Maggini S. Vitamin C and immune function. Nutrients. 2017;9 doi: 10.3390/nu9111211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kouakanou L., Xu Y., Peters C., He J., Wu Y., Yin Z., et al. Vitamin C promotes the proliferation and effector functions of human γδ T cells. Cell Mol Immunol. 2020;17:462–473. doi: 10.1038/s41423-019-0247-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Manning J., Mitchell B., Appadurai D.A., Shakya A., Pierce L.J., Wang H., et al. Vitamin C promotes maturation of T-cells. Antioxidants Redox Signal. 2013;19:2054–2067. doi: 10.1089/ars.2012.4988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kouakanou L., Peters C., Sun Q., Floess S., Bhat J., Huehn J., et al. Vitamin C supports conversion of human γδ T cells into FOXP3-expressing regulatory cells by epigenetic regulation. Sci Rep. 2020;10:6550. doi: 10.1038/s41598-020-63572-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Manning J., Mitchell B., Appadurai D., Shakya A., Pierce L., Wang H., et al. Vitamin C promotes maturation of T-cells. Antioxidants Redox Signal. 2012;19 doi: 10.1089/ars.2012.4988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tsukagoshi K.H. Role of ascorbic acid in modulation of gene expression. Biochem Biochem Cell Biol. 1996;25 doi: 10.1007/978-1-4613-0325-1_3. [DOI] [PubMed] [Google Scholar]
- 64.Chakraborty S., Syal K., Bhattacharyya R., Banerjee D. 2014. Vitamin deficiency and tuberculosis: need for urgent clinical trial for management of tuberculosis. [Google Scholar]
- 65.Traber M., Stevens J. Vitamins C and E: beneficial effects from a mechanistic perspective. Free Radic Biol Med. 2011;51:1000–1013. doi: 10.1016/j.freeradbiomed.2011.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Norma Francenia Santos-Sánchez R.S.-C., Villanueva-Cañongo Claudia, Hernández-Carlos Beatriz. intechopen; 2019. Antioxidant compounds and their antioxidant mechanism. [Google Scholar]
- 67.Fenech M., Amaya I., Valpuesta V., Botella M.A. Vitamin C content in fruits: biosynthesis and regulation. Front Plant Sci. 2019;9 doi: 10.3389/fpls.2018.02006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kurutas E.B. The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutr J. 2016;15:71. doi: 10.1186/s12937-016-0186-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bozonet S.M., Carr A.C. The role of physiological vitamin C concentrations on key functions of neutrophils isolated from healthy individuals. Nutrients. 2019;11 doi: 10.3390/nu11061363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abobaker A., Alzwi A., Alraied A.H.A. Overview of the possible role of vitamin C in management of COVID-19. Pharmacol Rep. 2020;72:1517–1528. doi: 10.1007/s43440-020-00176-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carcamo J.M., Pedraza A., Borquez-Ojeda O., Golde D.W. Vitamin C suppresses TNF alpha-induced NF kappa B activation by inhibiting I kappa B alpha phosphorylation. Biochemistry. 2002;41:12995–13002. doi: 10.1021/bi0263210. [DOI] [PubMed] [Google Scholar]
- 72.Engin A.B., Engin A. CRC Press; 2013. Endothelium: molecular aspects of metabolic disorders. [Google Scholar]
- 73.Grudzien M., Rapak A. Effect of natural compounds on NK cell activation. J Immunol Res. 2018;2018 doi: 10.1155/2018/4868417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Huijskens M., Walczak M., Sarkar S., Atrafi F., Gijsbers B.L.M.G., Tilanus M.G.J., et al. Ascorbic acid promotes proliferation of natural killer cell populations in culture systems applicable for natural killer cell therapy. Cytotherapy. 2015;17 doi: 10.1016/j.jcyt.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 75.Safarpour D., Srinivasan K., Farooqui M., Roth C., Ghouse M. A case of COVID-19-induced lymphocytosis in a patient with treatment-naive CLL: should it Be treated? Clin Lymphoma Myeloma Leuk. 2021;21:69–72. doi: 10.1016/j.clml.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu X., Zhang R., He G. Hematological findings in coronavirus disease 2019: indications of progression of disease. Ann Hematol. 2020;99:1421–1428. doi: 10.1007/s00277-020-04103-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Huang I., Pranata R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis. J Intensive Care. 2020;8:36. doi: 10.1186/s40560-020-00453-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saluja M., Pillai D. COVID-19 versus H1N1: pandemic to pandemic − a comparative analysis of clinical presentation, lab parameters, disease severity and outcome. J Ass Chest Physi. 2021;9:7–15. [Google Scholar]
- 79.Li X., Liu C., Mao Z., Xiao M., Wang L., Qi S., et al. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: a systematic review and meta-analysis. Crit Care. 2020;24:647. doi: 10.1186/s13054-020-03374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.-Q., et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Targeted Ther. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cox R.J., Brokstad K.A. Not just antibodies: B cells and T cells mediate immunity to COVID-19. Nat Rev Immunol. 2020;20:581–582. doi: 10.1038/s41577-020-00436-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen Z., John Wherry E. T cell responses in patients with COVID-19. Nat Rev Immunol. 2020;20:529–536. doi: 10.1038/s41577-020-0402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu L., Xu L., Lin C. T cell response in patients with COVID-19. Blood Sci. 2020;2:76–78. doi: 10.1097/BS9.0000000000000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Derbyshire E., Delange J. COVID-19: is there a role for immunonutrition, particularly in the over 65s? BMJ Nutr Prev Health. 2020;3:100–105. doi: 10.1136/bmjnph-2020-000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.van Gorkom G., Klein Wolterink R., Elssen C., Wieten L., Germeraad W., Bos G. Influence of vitamin C on lymphocytes: an overview. Antioxidants. 2018;7:41. doi: 10.3390/antiox7030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Holford P., Carr A.C., Jovic T.H., Ali S.R., Whitaker I.S., Marik P.E., et al. Vitamin C-an adjunctive therapy for respiratory infection, sepsis and COVID-19. Nutrients. 2020:12. doi: 10.3390/nu12123760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang R., Jaw J.J., Stutzman N.C., Zou Z., Sun P.D. Natural killer cell-produced IFN-gamma and TNF-alpha induce target cell cytolysis through up-regulation of ICAM-1. J Leukoc Biol. 2012;91:299–309. doi: 10.1189/jlb.0611308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Paul S., Lal G. The molecular mechanism of natural killer cells function and its importance in cancer immunotherapy. Front Immunol. 2017;8:1124. doi: 10.3389/fimmu.2017.01124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Abel A.M., Yang C., Thakar M.S., Malarkannan S. Natural killer cells: development, maturation, and clinical utilization. Front Immunol. 2018;9 doi: 10.3389/fimmu.2018.01869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Karki R., Sharma B.R., Tuladhar S., Williams E.P., Zalduondo L., Samir P., et al. Synergism of TNF-alpha and IFN-gamma triggers inflammatory cell death, tissue damage, and mortality in SARS-CoV-2 infection and cytokine shock syndromes. Cell. 2021;184:149–168 e17. doi: 10.1016/j.cell.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Karki R., Sharma B.R., Tuladhar S., Williams E.P., Zalduondo L., Samir P., et al. bioRxiv; 2020. COVID-19 cytokines and the hyperactive immune response: synergism of TNF-alpha and IFN-gamma in triggering inflammation, tissue damage, and death. [Google Scholar]
- 92.Syal K., Rs N., Reddy M. The extended (p)ppGpp family: new dimensions in Stress response. Curr Res Microb Sci. 2021;2 doi: 10.1016/j.crmicr.2021.100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bhardwaj N., Syal K., Chatterji D. The role of omega-subunit of Escherichia coli RNA polymerase in stress response. Gene Cell. 2018;23:357–369. doi: 10.1111/gtc.12577. [DOI] [PubMed] [Google Scholar]
- 94.Syal K., Chatterji D. Differential binding of ppGpp and pppGpp to E. coli RNA polymerase: photo-labeling and mass spectral studies. Gene Cell. 2015;20:1006–1016. doi: 10.1111/gtc.12304. [DOI] [PubMed] [Google Scholar]
- 95.Wang B., Svetlov V., Wolf Y.I., Koonin E.V., Nudler E., Artsimovitch I. Allosteric activation of SARS-CoV-2 RNA-dependent RNA polymerase by remdesivir triphosphate and other phosphorylated nucleotides. mBio. 2021;12 doi: 10.1128/mBio.01423-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Annette Plüddemann JKA. What is the role of T cells in COVID-19 infection? Why immunity is about more than antibodies. The Centre for Evidence-Based Medicine. University of Oxford: Centre for Evidence-Based Medicine, Nuffield Department of Primary Care Health Sciences University of Oxford; October 19, 2020. p. Evidence Service to support the COVID-19 response.
- 97.Divya K. Shah SRI, Toronto Canada. T-cell development in thymus. British society for immunology.
- 98.Juvet S.C., Zhang L. Double negative regulatory T cells in transplantation and autoimmunity: recent progress and future directions. J Mol Cell Biol. 2012;4:48–58. doi: 10.1093/jmcb/mjr043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Belizário J.E., Brandão W., Rossato C., Peron J.P. Thymic and postthymic regulation of naïve CD4+ T-cell lineage fates in humans and mice models. Mediat Inflamm. 2016;2016 doi: 10.1155/2016/9523628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Oyarce K., Campos-Mora M., Gajardo-Carrasco T., Pino-Lagos K. Vitamin C fosters the in vivo differentiation of peripheral CD4+ Foxp3− T cells into CD4+ Foxp3+ regulatory T cells but impairs their ability to prolong skin allograft survival. Front Immunol. 2018;9 doi: 10.3389/fimmu.2018.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.van Gorkom G.N.Y., Klein Wolterink R.G.J., Van Elssen C., Wieten L., Germeraad W.T.V., Bos G.M.J. Influence of vitamin C on lymphocytes: an overview. Antioxidants. 2018;vol. 7 doi: 10.3390/antiox7030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vallance S. Relationships between ascorbic acid and serum proteins of the immune system. Br Med J. 1977;2:437–438. doi: 10.1136/bmj.2.6084.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Prinz W., Bortz R., Bregin B., Hersch M. The effect of ascorbic acid supplementation on some parameters of the human immunological defence system. Int J Vitam Nutr Res. 1977;47:248–257. [PubMed] [Google Scholar]
- 104.Chambial S., Dwivedi S., Shukla K.K., John P.J., Sharma P. Vitamin C in disease prevention and cure: an overview. Indian J Clin Biochem. 2013;28:314–328. doi: 10.1007/s12291-013-0375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Carr A.C., Rowe S. The emerging role of vitamin C in the prevention and treatment of COVID-19. Nutrients. 2020;12 doi: 10.3390/nu12113286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lykkesfeldt J., Tveden-Nyborg P. The pharmacokinetics of vitamin C. Nutrients. 2019;11 doi: 10.3390/nu11102412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Junaid K., Qasim S., Yasmeen H., Ejaz H., Alsrhani A., Ullah M.-I., et al. Potential inhibitory effect of vitamins against COVID-19. Computers, Materials \& Continua. 2021;66:707–714. [Google Scholar]
- 108.Ivanov V., Goc A., Ivanova S., Niedzwiecki A., Rath M. Inhibition of ACE2 expression by ascorbic acid alone and its combinations with other natural compounds. Infect Dis (Auckl) 2021;14 doi: 10.1177/1178633721994605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Holford P., Carr A.C., Jovic T.H., Ali S.R., Whitaker I.S., Marik P.E., et al. Vitamin C—an adjunctive therapy for respiratory infection, sepsis and COVID-19. Nutrients. 2020;12:3760. doi: 10.3390/nu12123760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sofi M.S., Hamid A., Bhat S.U. SARS-CoV-2: a critical review of its history, pathogenesis, transmission, diagnosis and treatment. Biosafety and Health. 2020;2:217–225. doi: 10.1016/j.bsheal.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.V’kovski P., Kratzel A., Steiner S., Stalder H., Thiel V. Coronavirus biology and replication: implications for SARS-CoV-2. Nature Reviews Microbiology. 2020;19:155–170. doi: 10.1038/s41579-020-00468-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rock C.L., Jacob R.A., Bowen P.E. Update on the biological characteristics of the antioxidant micronutrients: vitamin C, vitamin E, and the carotenoids. J Am Diet Assoc. 1996;96:693–702. doi: 10.1016/S0002-8223(96)00190-3. ; quiz 3-4. [DOI] [PubMed] [Google Scholar]
- 113.McCord J.M. The evolution of free radicals and oxidative stress. Am J Med. 2000;108:652–659. doi: 10.1016/s0002-9343(00)00412-5. [DOI] [PubMed] [Google Scholar]
- 114.Rao A., Bharani M., Pallavi V. Role of antioxidants and free radicals in health and disease. Adv Pharmacol Toxicol. 2006;7:29–38. [Google Scholar]
- 115.Mousavi S., Bereswill S., Heimesaat M.M. Immunomodulatory and antimicrobial effects of vitamin C. Eur J Microbiol Immunol (Bp) 2019;9:73–79. doi: 10.1556/1886.2019.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wu R., Wang L., Kuo H.-C.D., Shannar A., Peter R., Chou P.J., et al. An update on current therapeutic drugs treating COVID-19. Current Pharmacology Reports. 2020;6:56–70. doi: 10.1007/s40495-020-00216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pehlivan F.E. intechopen; 2017. Vitamin C: an antioxidant agent. [Google Scholar]
- 118.Forman H.J., Zhang H., Rinna A. Glutathione: overview of its protective roles, measurement, and biosynthesis. Mol Aspects Med. 2009;30:1–12. doi: 10.1016/j.mam.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ho Y.S., Magnenat J.L., Gargano M., Cao J. The nature of antioxidant defense mechanisms: a lesson from transgenic studies. Environ Health Perspect. 1998;106(Suppl 5):1219–1228. doi: 10.1289/ehp.98106s51219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Colunga Biancatelli R.M.L., Berrill M., Marik P.E. The antiviral properties of vitamin C. Expert Review of Anti-infective Therapy. 2020;18:99–101. doi: 10.1080/14787210.2020.1706483. [DOI] [PubMed] [Google Scholar]
- 121.Hemila H., Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013:CD000980. doi: 10.1002/14651858.CD000980.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kim M.S., Kim D.J., Na C.H., Shin B.S. A study of intravenous administration of vitamin C in the treatment of acute herpetic pain and postherpetic neuralgia. Ann Dermatol. 2016;28:677–683. doi: 10.5021/ad.2016.28.6.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Malla T.N., Pandey S., Aldama L., Feliz D., Noda M., Poudyal I., et al. Vitamin C binds to SARS coronavirus-2 main protease essential for viral replication. bioRxiv. 2021:2021. [Google Scholar]
- 124.Pisoschi A.M., Pop A., Iordache F., Stanca L., Geicu O.I., Bilteanu L., et al. Antioxidant, anti-inflammatory and immunomodulatory roles of vitamins in COVID-19 therapy. Eur J Med Chem. 2022;232 doi: 10.1016/j.ejmech.2022.114175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kim K., Bae O.-N., Koh S.-H., Kang S., Lim K.-M., Noh J.-Y., et al. High-dose vitamin C injection to cancer patients may promote thrombosis through procoagulant activation of erythrocytes. Toxicological Sciences. 2015;147:350–359. doi: 10.1093/toxsci/kfv133. [DOI] [PubMed] [Google Scholar]
- 126.Syal K., Chakraborty S., Bhattacharyya R., Banerjee D. Combined inhalation and oral supplementation of Vitamin A and Vitamin D: a possible prevention and therapy for tuberculosis. Med Hypotheses. 2015;84:199–203. doi: 10.1016/j.mehy.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 127.Labiris N.R., Dolovich M.B. Pulmonary drug delivery. Part I: physiological factors affecting therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol. 2003;56:588–599. doi: 10.1046/j.1365-2125.2003.01892.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pera I.L. In: Method ed. Patent U.S., editor. vol. 31. USAAug; 1999. Method for dispensing antioxidant vitamins BY inhalation background OF the invention; p. 6. (US patent documents). [Google Scholar]
- 129.Thomas S., Patel D., Bittel B., Wolski K., Wang Q., Kumar A., et al. Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial. JAMA Network Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.0369. e210369-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Majidi N., Rabbani F., Gholami S., Gholamalizadeh M., BourBour F., Rastgoo S., et al. The effect of vitamin C on pathological parameters and survival duration of critically ill coronavirus disease 2019 patients: a randomized clinical trial. Front Immunol. 2021;12 doi: 10.3389/fimmu.2021.717816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ried K., BinJemain T., Sali A. Therapies to prevent progression of COVID-19, including hydroxychloroquine, azithromycin, zinc, and vitamin D3 with or without intravenous vitamin C: an international, multicenter, randomized trial. Cureus. 2021;13 doi: 10.7759/cureus.19902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Erol N., Saglam L., Saglam Y.S., Erol H.S., Altun S., Aktas M.S., et al. The protection potential of antioxidant vitamins against acute respiratory distress syndrome: a rat trial. Inflammation. 2019;42:1585–1594. doi: 10.1007/s10753-019-01020-2. [DOI] [PubMed] [Google Scholar]