Abstract
COVID-19, the most recent and globally impactful zoonotic viral pandemic in the last 20 years, has now entered its third year. As the global dental profession returns to providing as full a range of services as possible, in addition to embedding the new infection-control processes that were developed for this pandemic, it should also take full advantage of digital conventional radiology (intraoral, extraoral, and panoramic radiography) and cone-beam computed tomography. Regardless of vaccinations, new or yet-to-manifest variants, and testing, some dentists may be working in communities where the asymptomatic but potentially infectious patient poses a real risk. This needs to be met with not only the whole COVID-19 panoply the dentist is already too familiar with but also the need to minimise aerosol generation production by dental radiography. A flowchart and a table that compares the attributes of the above modalities are included.
Keywords: COVID-19, Radiology, Radiography, Cone-beam computed tomography
Introduction
Radiology, particularly intraoral radiography, is central to the practice of dentistry. Unfortunately, it is an aerosol-generating procedure (AGP) and thus enhances the spread of infections, such as COVID-19. In January 2021, guidelines by the American Academy of Oral and Maxillofacial Radiology (AAOMR)1 presented an appropriate dental radiologic response to COVID-19 just when worldwide vaccinations were beginning. Although “effectiveness of full vaccination is 88% against infection, 94% against hospitalisation, and 95% against death,”2 the recent Omicron variant in the space of a few months has become the dominant strain in many countries.3 Though less lethal than most of the earlier variants, its higher transmissibility and its high proportion of “breakthrough” amongst even the fully vaccinated suggest that vaccines alone will not end the pandemic.4 Therefore, it is now important to take the next step and assist the dentist providing a fuller service to the community in what has become the “new normal” in this third year of the pandemic. This new normal is simply not just the provision of the full scope of dental treatment to patients who have been deprived of regular dental treatment by the pandemic for the last 2 years; it includes treatment for patients with “long COVID” now compromised by neurologic, cardiovascular, and clotting problems.5 Although dentists did not experience the higher mortality of their medical colleagues, reflecting both the stringent infection control dentists applied globally and the fact that most patients with severe acute COVID-19 did not present to their dentists,6 the present review upholds the full infection control gamut of the AAOMR's guidelines, which are still required by most jurisdictions globally. Whilst the primary focus of AAOMR guidelines was on the dental emergency patient,1 this review, summarised in Figure 1 and the Table, focusses on the fuller range of services provided by the general and/or specialist dentist to their regular patient and therefore the ever-present need to adhere to ALARA (as low as reasonably achievable).7 This approach should be adapted by the public health directives and recommendations appropriate to the dentist's jurisdiction.
Fig. 1.
Flowchart identifying the imaging modalities that may be available in dental offices and their application in patients presenting with a clinically indicated need for radiography and their COVID-19 status. CBCT, cone-beam computed tomography; FOV, field of view; PPE, personal protective equipment. This figure is a development of Figure 1 in MacDonald et al.1
Table.
A comparison of the attributes of 5 radiologic modalities now used in dentistry.
| Feature | IBWs | EBWs, Segmental DPR | DPR | CBCT |
|---|---|---|---|---|
| Availability | Most dental office | Available in most modern DPR units | Most dental offices | Still fewer dental offices |
| SR (fine detail) | Best for caries | Posteriorly focussed proximally optimised for interproximal surfaces of posterior teeth and therefore better than DPR for caries | Moderate: Most units not good enough for caries, but adequate for review of the entire jaws and upper neck | Least: But choose best SR (0.076-0.09 mm voxel size) for endodontics, impacted teeth, and small lesions |
| Diagnostic efficiency | Best for most studies of individual teeth | Equivalent to IBW on basis of in vitro studies Lower half of sinus to upper neck |
Reveals entire jaws, from condyle to condyle and lower half of sinus to upper neck | Best when cross-sectional information required |
| Need for awareness of incidental findings | Nothing beyond crowns and cervical half of roots | Supernumeraries, lesions in lower sinus, posterior body of mandible and upper neck | Same as EBWs and condyles, ramus and anterior sextant | Particularly of base of skull and vertebrae in large FOVs |
| Reduced patient compliance | Children and gaggers and those prone to coughing | Most current units require the patient to be standing or seated vertically; therefore, not ideal for elderly and sick patients | ||
| Aerosol production likelihood | Highest because of the above need to bag/barrier receptors | Least, since nothing enters the oral cavity | ||
| Positioning artefact likelihood | High | Low to moderate | Low to moderate | Low to moderate |
| Movement artefact likelihood | Minimal: short exposure time | Moderate | Moderate: circa 14-16 seconds | High: up to 30 seconds |
| Metal artefact likelihood | None | Provided patient properly prepared and positioned | Provided patient properly prepared and positioned | Greatest likelihood |
| Ghosting artefact likelihood | None | Moderate | Moderate to high | Low |
| Cross-sectional display | None | None | None | Best |
| Optimal indications | Caries and periodontal pocketing Single rooted endodontics |
Posteriorly focussed proximally optimised for interproximal surfaces of posterior teeth and thus better for caries | Panoramic view of jaws, particularly in patients with multiple or complex pathology | Complex or retreated endodontics and impacted teeth |
| Radiation dose imparted | Least | Greater than IBW and lower than DPR | Equivalent to 4 IBWs | Highest even with small FOVs |
| Other relevant comments | Phosphor plates have a wider dynamic range than solid state (CCD and CMOS) receptors | 1. 2 EBW images instead of 4 IBWs 2. Displays dento-alveolus of both jaws on one image 3. Reduced retakes compared to IBWs |
Anterior focal trough is narrower in many units and vertebral column is superimposed on it = artefacts | Requires technical expertise and experience particularly with small FOVs |
CBCT, cone-beam computed tomography; CCD, charge-couple device; CMOS, complementary metal-oxide semiconductor; DPR, dental panoramic radiograph; EBW, extraoral bitewing; FOV, field of view; IBW, intraoral bitewing; SR, spatial resolution.
This table is a development of Table III in MacDonald et al.1
Assessment of the patient with potential COVID-19 in 2022
Whilst it is clear that those patients with active COVID-19 or being investigated for it be treated only on an emergency basis, what about the likelihood of those who are infected but asymptomatic? There are 2 primary screening methods for COVID-19, questionnaires with temperature-taking and COVID-19 testing. A medical emergency room (ER) discovered that 60% of the patients who tested negative for COVID-19 had the infection,8 thus indicating that false negatives through testing are an issue, even in a medical ER. As “more evidence is needed about the effectiveness of testing outside of hospital settings and in mild or asymptomatic cases,”9 the dentist should continue to assume that each patient who is asymptomatic for COVID-19 might be infectious, as it is possible “that the oral cavity actively participates in SARS-CoV-2 transmission.”10 Enhanced history-taking and donning and doffing personal protective equipment in the appropriate manner, effective room ventilation, and cleansing and sterilisation (or disinfection) of equipment1 protect not only dentists and their patients but also particularly those with underlying conditions that place them at a heightened risk for a severe or fatal outcome if COVID-19 is contracted.11
Changes in radiographic technology available to the dentist in this late COVID-19 pandemic stage
The most important developments in dental radiology over the last 3 decades have been digital conventional radiography, which includes both intraoral and dental panoramic radiography (DPR) and cone-beam computed tomography (CBCT). An earlier encounter with severe acute respiratory syndrome (SARS) of 2003 and 2004, the forerunner of the SARS-CoV-2 virus of the current COVID-19 pandemic, raised concerns about digital intraoral radiography's infection control, resulting in the development of an effective bagging/barrier system for the phosphor plate system.12 Since then, effective bagging/barrier systems have been tested for solid-state receptors.13 Unfortunately, these barriers do not prevent the generation and dispersal of aerosols into the clinical environment. Although it is possible to eliminate this with room cleaning with the appropriate Environmental Protection Agency (EPA)–equivalent agents and solutions, high-efficiency particulate air (HEPA) filters, or other exhaustion of air to the outside, as detailed elsewhere,1 aerosol generation should be minimised if not avoided.
Whilst most patients presenting for emergency dental treatment can be diagnosed by a clinical examination alone, some form of radiography may be required. This is particularly most likely when the patient is previously unknown to the dentist or has not presented regularly for routine care and/or for patients whose clinical presentation indicates that radiography is necessary to evaluate the problem more fully before appropriate treatment can be offered. Nevertheless, this avoidance of intraoral radiography presents the dentist with a conundrum.14 Regardless of COVID-19 status, every prescription for radiography should be based on sound clinical indications arising from a proper history and clinic examination.15 This dictated that radiography should be performed when clinically necessary. A strategy had been developed early on in the pandemic to minimise aerosol generation in an intraoral radiographic context, such as using a dual operator system with one “clean” operator, who handled only the computer and exposure operation, and the “unclean” operator, who handled only the patient and receptor.1 This could not work when the patient was a child, a gagger, or someone who was resistant to intraoral radiography. Radiography in such cases should be restricted to extraoral modalities, which are intrinsically non-AGP. These are extraoral bitewings (EBWs) (Figure 2) and extraoral periapical radiographs and CBCT (Figure 1 and Table.).
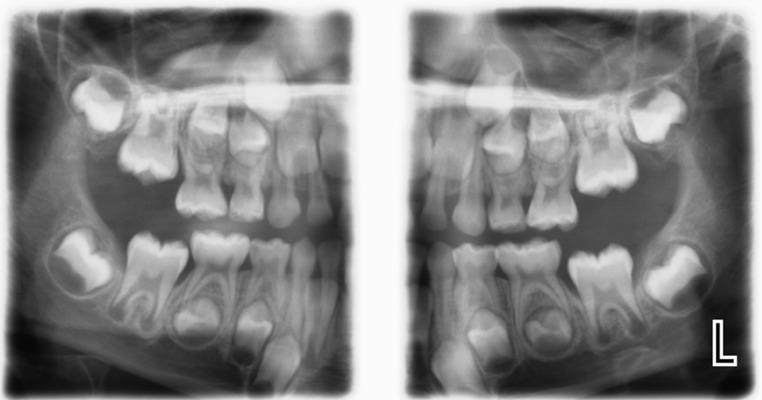
Fig. 2.
Extraoral bitewing of a child. It, unlike the dental panoramic radiograph, is posteriorly focussed and proximally optimised for interproximal surfaces of posterior teeth. It is therefore better than dental panoramic radiography for identifying caries.
In many cases, such reliance on extraoral technology may be the investigation of choice on the basis of best evidence. Small field-of-view (FOV) cross-sectional imaging of CBCT permits significantly better radiologic diagnosis and treatment planning of endodontic lesions, such as periapical radiolucencies (Figure 3), missed canals, adjacent anatomy, and root fractures.16 This study was one of the first and the largest so far to ascend to the mid-tiers of the 6-tier Fryback and Thornbury hierarchical model for efficacy,17 these being diagnostic impact and treatment impact. Going forwards, it is hoped that more future research in dental radiology ascends even to Fryback and Thornbury's highest tiers of patient outcome efficacy and societal efficacy.18
Fig. 3.
a, A periapical radiographic display of a previously endodontically treated left maxillary molar. The recurrence of the infection is due to a second mesiobuccal root canal, which was previously missed. b, c, and d represent the 4-cm diameter field-of-view cone-beam computed tomography of this molar. The radiolucency encompasses the mesiobuccal root from apex to the alveolar crest. The cause is a missed second mesiobuccal canal as is clear in b, where only one canal has been filled. The relationship of the lesion with the adjacent anatomy, the floor of the maxillary sinus, is also displayed.
Whilst the full-mouth survey (FMS) remained a routine element of the dental care for a century, it should not be prescribed routinely, but rather in response to a particular patient's dental needs. This is now reinforced by the significant association between the FMS and salivary gland cancers.19 Although the DPR, since its appearance in the 1960s, had developed to such a degree that DPR was considered by an authority a feasible alternative to the FMS,20 others have questioned this advice with regards to caries.20
Dental caries, although preventable and having experienced a general decline in prevalence, remains the most prevalent chronic disease in both children and adults, particularly where social disparities remain.21 The 2 ultimate goals of radiography are being reproducible and accurate in the detection of caries and estimating their depth as well as distinguishing between cavitated and noncavitated lesions.22 Nevertheless, recently, the visual-tactile approach was determined to be significantly more effective in the true-positive diagnosis of caries than radiography, which resulted in false positives.23
In addition to caries, periodontal disease is a globally prevalent chronic disease. Although a recent study on the trends of this disease in America was unable to determine whether it was increasing or decreasing, the fact that people are living longer and are also retaining their teeth for longer means that it is “reasonable to speculate that there are increasing numbers of people and teeth with periodontitis.”24 Although generally the FMS is considered optimal for assessment of periodontal bone loss, “the ability to zoom in and magnify defects and to adjust dynamically the contrast and brightness allows” the DPR “for vastly improved ‘visualization’ of bone levels and intra-bony defects.”25
Regardless of the clinical indication, the entire image, particularly the DPR and lateral cephalogram, and CBCT data set should be reviewed for incidental findings (IFs) so that their treatment, if required, may be attended to in a timely manner. A review of the largest and most recent case series of digital DPRs amongst new patients found IFs in one-third of them. The most frequent IF was impacted teeth, particularly third molars.26 Whether such asymptomatic impacted teeth are to be removed or retained varies with jurisdiction and will not be discussed further, except to mention a recent Cochrane Review, which reported “insufficient evidence” either for their routine removal or for their retention.27 Other findings were areas of periapical sclerosis or radiolucencies, at 1.0% and 0.4%, respectively, which are suggestive of nonvital teeth requiring treatment.26 One of the earliest of such studies revealed that although the majority of IFs were not registered in the clinical record, it is most likely that they were observed but were not considered for further investigation and treatment at that time.28 Nevertheless, this raises 2 issues. In both reports, routine DPRs in new patients were required as standard practice. Going forwards, all radiographic investigations should be comprehensively reviewed to identify all IFs and to record them. Attention should also be paid to IFs such as calcified carotid artery atheromas on DPRs, as these may indicate the need for further assessment and treatment of cardiovascular disease.29
Evolution in DPR technology introduced “sectional” DPRs 3 decades ago with the aim to restrict the area irradiated, thus reducing radiation dose. A species of these segmented DPRs is the EBW (Figure 2). The EBW uses posteriorly focussed proximally optimised panoramic radiograph-like images with non-overlapping proximal surfaces of posterior teeth in a single scan.30 Therefore, the EBW is different from a single DPR coned down to the posterior sextant. Although the EBW displays the entire dento-alveolar apparatus in contrast to only the crowns and adjacent roots and alveolus in intraoral bitewings (IBWs), it is primarily prescribed to assist in the diagnosis of caries, particularly in children and young adults.
There was no significant difference in posterior proximal surface caries detection between IBWs and EBWs, except that detection of open proximal contact points was better for IBWs.31 Such EBWs, based on clinical experience, may be rendered clinically completely useless due to the superimpositions of the secondary images of a heavily restored mouth. This is most likely to be observed on an EBW of an older adult patient, rather than in the child or younger adult. Nevertheless, stainless-steel crowns and ongoing fixed orthodontic treatment could similarly compromise its use.
The gradual replacement of analogue (dental film) intraoral radiography by digital technologies—phosphor plate (also called photostimulable phosphors; PSPs) and solid state (charge-couple devices [CCDs] and complementary metal–oxide–semiconductor [CMOS])—since their development 3 decades ago, has been achieved to such a degree that a return to analogue/dental film is unlikely. Furthermore, these technologies create an environmentally safer workplace by replacing hazardous chemicals.
A frequently overlooked aspect of digital radiography is the quality of image display (the inherent brightness and spatial resolution of the monitor), which is in turn dependent upon the viewing conditions. For analogue/film-based radiography, the viewing conditions include a bright light box with a luminance (brightness) of 1500 to 3000 cd/m2, as well as an illuminance (reduced ambient lighting) of 100 lux or less. In digital radiography, the display monitor, which replaces the light box, is less bright and indeed was not bright enough, which was a major problem 2 decades ago. Fortunately, in the intervening 2 decades the quality of monitors has so improved that most high-quality monitors are adequate for image display.32 Although these should be viewed in a reduced ambient environment, rather than under the bright dental chairside light,32 a selection of smartphones and tablets displayed statistically similar accuracy to detect incipient caries on digital bitewing radiographs.33
Radiation dose
The onset of COVID-19 does not in any way devalue our focus on ALARA, which endeavours to minimise the likelihood of radiation-induced lesions. These range from malignancies, such as oral and salivary cancers, benign brain tumours such as meningiomas, damage to the eyes (cataracts), and irradiation of the thyroid glands.
The average radiation dose for one intraoral radiograph is less than 1.5 µSv based on an FMS consisting of 14 periapical radiographs and 4 bitewing radiographs, using phosphor plate or F-speed analogue/dental film.34 Whilst the mean DPR was equivalent to 4 periapical radiographs, for some units this may be even fewer, whereas for others it may be equivalent to as many as 16 periapical radiographs.34 Although the radiation dose of a CBCT can vary from about 8 periapical radiographs to more than 700,34 according to a more recent report, the dosimetry of only 20% of the 279 units produced by 47 manufacturers have been included in systematic reviews (SRs).35 Therefore, objective dosimetry on the majority of CBCTs is lacking. Furthermore, many SRs, though imprecise, noted that a reduced FOV height reduced the “effective dose” delivered to the patient and was best with small FOVs. 35
Almost every current CBCT has a DPR facility. Although an in vitro study revealed that CBCT-produced DPR images are similar to those produced on a stand-alone DPR unit, the latter's advantage was that the spectrum of manually selected exposure factors for the child and adolescent patient prevented either over- or underestimation of the radiation dose.36 Although radiation doses in dentistry overall are proportionally miniscule to those from medical sources, children are more susceptible to radiation-induced damage than mature adults and also have their whole lives ahead of them in which it may manifest. Therefore, minimise the radiation dose to children and young patients.
CBCT: more on fields of view
The size of FOV used should be that small enough to be confined to the jaws, as this is the traditional realm of the dentist. Medium and small FOVs are appropriate for implant, endodontic, impacted teeth, and lesion cases. Large FOVs include the eyes, the base of the skull, and the neck,32 which are the proper realm of the medical doctor. If large FOVs are required for investigation of craniofacial anomalies, such as cleft lip and palate cases, the data sets should be reviewed by medical or oral and maxillofacial radiologists.
Many dentists who review their own CBCT data sets only use the multiplanar reconstruction (MPR; Figure 4A), which is the default reconstruction for most CBCT units. As this only produces axial, coronal, and sagittal reconstructions, which have been traditionally used in medical radiology, it is on its own generally inadequate to display the jaws, which follow a catenary arc. Before the advent of CBCT in clinical dentistry in 1999, the Dentoscan software was developed for medical computed tomography to assist implantologists by following the catenary arc selected for each patient. This is now available to CBCT as the “curved” or “panoramic” reconstructions (Figure 4B). Although it is most commonly used by implantologists, it contributes to endodontics (Figure 2), where the 3-dimensional reconstruction of the tooth is displayed in its normal mesiodistal disposition rather than obliquely as by MPR. Both reconstructions can be used together when reviewing the data set of lesions (Figure 4) and impacted teeth.
Fig. 4.
A medium-sized field of view (cone-beam computed tomography [CBCT] of a neoplasm affecting the anterior sextant of the maxilla extending backwards into the posterior sextant and the anterior wall of the left maxillary sinus. (a) represents the multiplanar reconstruction (MPR), whereas (b) represents the “curved” or “panoramic” or formerly the Dentoscan reconstruction. Each reconstruction displays different aspects of the lesion. The MPR is the default reconstruction for most CBCT software, whereas the “curved” reconstruction is manually generated by first plotting out the alveolar arch on the axial reconstruction from which the panoramic and transaxial reconstruction are generated. The lesion is an odontogenic keratocyst, also known as a keratocytocystic odontogenic tumour. See MacDonald D. Oral and maxillofacial radiology: a diagnostic approach. 2nd Edn. British Columbia: Wiley-Blackwell. 2020.
Conclusions
Our response to COVID-19 has already prepared us for the next pandemic, which assuredly will arrive. This preparation may be achieved by “deep mutational scanning” observing “surface antigens drifts and shifts of the pathogens in silico using artificial intelligence and machine learning.”6 In the meanwhile, the dentists should review all existing technology, particularly radiographic, adapting and developing it further so that it not only addresses new infection control challenges, reducing the radiation dose to their patients, but also improves the quality of the display of the patient and the accompanying disease. This also means developing technologies that do not use ionising radiation, such as qualitative light-induced fluorescence for the diagnosis of early caries37 and magnetic resonance imaging (MRI) optimally used for temporomandibular joint diseases38 and lesions of the salivary glands and other soft-tissue of the face, jaws, and upper neck. Although MRI units are generally only sited in medical facilities, ultrasonography can be used in the dental office.
Conflict of interest
None disclosed.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.MacDonald DS, Colosi DC, Mupparapu M, Kumar V, Shintaku WH, Ahmad M. Guidelines for oral and maxillofacial imaging: COVID-19 considerations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131(1):P99–110. doi: 10.1016/j.oooo.2020.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cochin S, Zibo F, Facchin G, et al. The effectiveness of a diverse COVID-19 vaccine portfolio and its impact on the persistence of positivity and length of hospital stays: the Veneto region's experience. Vaccines (Basel) 2022;10(1):107. doi: 10.3390/vaccines10010107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parums DV. Editorial: the 2022 World Health Organization (WHO) priority recommendations and response to the Omicron variant (B.1.1.529) of SARS-CoV-2. Med Sic Monit. 2022;28 doi: 10.12659/MSM.936199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adam D. Will Omicron end the pandemic? Here's what experts say. Nature. 2022;602:20–21. doi: 10.1038/d41586-022-00210-7. [DOI] [PubMed] [Google Scholar]
- 5.France K, Glick M. Long COVID and oral health care considerations. J Am Dent Assoc. 2022;153(2):P167–P174. doi: 10.1016/j.adaj.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samaranayake L, Fakhreddin KS. Pandemics past, present, and future: their impact on oral health care. J Am Dent Assoc. 2021;152(12):P972–P980. doi: 10.1016/j.adaj.2021.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryant PA, Croft J, Cole P. Integration of risks from multiple hazards into a holistic ALARA/ALARP demonstration. J Radiol Prot. 2018;38(1):81. doi: 10.1088/1361-6498/aa8e53. [DOI] [PubMed] [Google Scholar]
- 8.Jarrom D, Elston L, Washington J, et al. Effectiveness of tests to detect the presence of SARS-CoV-2 virus, and antibodies to SARS-CoV-2, to inform COVID-19 diagnosis: a rapid systematic review. BMJ Evid Based Med. 2022;27:33–45. doi: 10.1136/bmjebm-2020-111511. [DOI] [PubMed] [Google Scholar]
- 9.Caramello V, Macciotta A, Bar F, et al. The broad spectrum of COVID-like patients initially negative at RT-PCR testing: a cohort study. BMC Public Health. 2022;22:45. doi: 10.1186/s12889-021-12409-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang N, Pérez P, Kato T, et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat Med. 2021;27:892–903. doi: 10.1038/s41591-021-01296-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corrao G, Rea F, Carle F, et al. Monitoring and assessing care pathways (MAP) working group of the Italian Ministry of Health. Stratification of the risk of developing severe or lethal Covid-19 using a new score from a large Italian population: a population-based cohort study. BMJOpen. 2021;11 doi: 10.1136/bmjopen-2021-053281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald DS, Waterfield JD. Infection control in digital intraoral radiography: evaluation of microbiological contamination of photostimulable phosphor plates in barrier envelopes. J Can Dent Assoc. 2011;77:b93. PMID: 21929948. [PubMed] [Google Scholar]
- 13.Choi JW. Perforation rate of intraoral barriers for direct digital radiography. Dentomaxillofac Radiol. 2015;44:3. doi: 10.1259/dmfr.20140245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaur H, Gupta H, Dadlani H, et al. Delaying intraoral radiographs during the COVID-19 pandemic: a conundrum. Biomed Res Int. 2022 doi: 10.1155/2022/8432856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Dental association. Dental radiographic examinations: recommendations for patient selection and limiting radiation dose. Revised 2012. U.S. Department of Health and Human Resources. Food and Drug Administration. Available from:https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/ada-fda-guide-patient-selection-dental-radiographs. Accessed 25 April 2022.
- 16.Bhatt M, Coil J, Chehroudi B, Esteves A, Aleksejuniene J, MacDonald D. Clinical decision-making and importance of the AAE/AAOMR position statement for CBCT examination in endodontic cases. Int Endod J. 2021;54:26–37. doi: 10.1111/iej.13397. [DOI] [PubMed] [Google Scholar]
- 17.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making. 1991;11(2):88–94. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]
- 18.Rohlin M, Horner K, Lindh C, Wenzel A. Through the quality kaleidoscope: reflections on research in dentomaxillofacial imaging. Dentomaxillofac Radiol. 2020;49(6) doi: 10.1259/dmfr.20190484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang SY, Choi ES, Kim YS, Gim BE, Ha M, Kim HY. Health effects from exposure to dental diagnostic X-ray. Environ Health Toxicol. 2018;33(4) doi: 10.5620/eht.e2018017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farman AG. There are good reasons for selecting panoramic radiography to replace the intraoral full-mouth series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):P653–P654. doi: 10.1067/moe.2002.129766. [DOI] [PubMed] [Google Scholar]
- 21.National Institutes of Health and Craniofacial Research (NIH). Dental caries (tooth decay). Available from:https://www.nidcr.nih.gov/research/data-statistics/dental-caries. Accessed 25 April 2022.
- 22.Wenzel A. Radiographic modalities for diagnosis of caries in a historical perspective: from film to machine-intelligence supported systems. Dentomaxillofac Radiol. 2021;50(5) doi: 10.1259/dmfr.20210010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baelum V, Hintze H, Wenzel A, Danielsen B, Nyvad B. Implications of caries diagnostic strategies for clinical management decisions. Community Dent Oral Epidemiol. 2012;40:257–266. doi: 10.1111/j.1600-0528.2011.00655.x. [DOI] [PubMed] [Google Scholar]
- 24.Eke PI, Borgnakke WS, Genco RJ. Recent epidemiologic trends in periodontitis in the USA. Periodontol 2000. 2020;82:257–267. doi: 10.1111/prd.12323. [DOI] [PubMed] [Google Scholar]
- 25.Corbit EF, Ho DK, Lai SM. Radiographs in periodontal disease diagnosis and management. Aust Dent J. 2009;54:S27–S43. doi: 10.1111/j.1834-7819.2009.01141.x. [DOI] [PubMed] [Google Scholar]
- 26.MacDonald D, Yu W. Incidental findings in a consecutive series of digital panoramic radiographs. Imaging Sci Dent. 2020;50(1):53–64. doi: 10.5624/isd.2020.50.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghaeminia H, Nienhuijs ME, Toedtling V, et al. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst Rev. 2020;5 doi: 10.1002/14651858.CD003879.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MacDonald-Jankowski DS. The detection of abnormalities in the jaws: a radiological survey. Br Dent J. 1991;170:215–218. doi: 10.1038/sj.bdj.4807482. [DOI] [PubMed] [Google Scholar]
- 29.MacDonald D, Chan A, Harris A, Vertinsky T, Farman AG, Scarfe WC. Diagnosis and management of calcified carotid artery atheroma: dental perspectives. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(4):P533–P547. doi: 10.1016/j.oooo.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 30.Johnson KB, Mol A, Tyndall DA. Extraoral bite-wing radiographs: a universally accepted paradox. J Am Dent Assoc. 2021;152(6):P444–P447. doi: 10.1016/j.adaj.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 31.Terry GL, Noujeim M, Langlais RP, Moore WS, Prihoda TJ. A clinical comparison of extraoral panoramic and intraoral radiographic modalities for detecting proximal caries and visualizing open posterior interproximal contacts. Dentomaxillofac Radiol. 2016;45(4) doi: 10.1259/dmfr.20150159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacDonald D, editor. Oral and maxillofacial radiology: a diagnostic approach. 2nd ed. Wiley-Blackwell; Hoboken, New Jersey: 2020. pp. 47–55. 362, and 519–609. [Google Scholar]
- 33.Melo CA, Santos MAL, Menezes LS, Santana FS, Melo MFB, Takeshita WM. Use of smartphones and tablets in radiographic evaluation: accuracy of caries detection on bitewing radiographs. Gen Dent. 2021;69(4):28–34. PMID: 33136050. [PubMed] [Google Scholar]
- 34.van der Stelt PF. Panoramische röntgenopnamen in de tandheelkundige diagnostiek [Panoramic radiographs in dental diagnostics] Ned Tijdschr Tandheelkd (Dutch) 2016;123(4):181–187. doi: 10.5177/ntvt.2016.04.15208. [DOI] [PubMed] [Google Scholar]
- 35.Al-Okshi A, Horner K, Rohlin M. A meta-review of effective doses in dental and maxillofacial cone beam CT using the ROBIS tool. Br J Radiol. 2021;94:1123. doi: 10.1259/bjr.20210042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wahid MA, Choi E, MacDonald DS, Ford NL. Dosimetry analysis of panoramic-imaging devices in different-sized phantoms. J Appl Clin Med Phys. 2017;18:197–205. doi: 10.1002/acm2.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gomez J. Detection and diagnosis of the early caries lesion. BMC Oral Health. 2015;15:S3. doi: 10.1186/1472-6831-15-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ito S, Mine Y, Yoshimi Y, et al. Automated segmentation of articular disc of the temporomandibular joint on magnetic resonance images using deep learning. Sci Rep. 2022;12:221. doi: 10.1038/s41598-021-04354-w. [DOI] [PMC free article] [PubMed] [Google Scholar]