Abstract
Scope-of-practice regulations, including prescribing limits and supervision requirements, may influence the propensity of providers to form care teams. Therefore, policymakers need to understand the effect of both team-based care and provider type on clinical outcomes. We examined how care management and biomarker outcomes following onset of three chronic diseases differed both by team-based versus solo care and by physician versus non-physician (i.e., nurse practitioner and physician assistant) care. Using 2013–2018 de-identified electronic health record data from U.S. primary care practices, we found that provider teams outperformed solo providers, irrespective of team composition. Among solo providers, physicians and non-physicians exhibited little meaningful difference in performance. As policymakers contemplate scope-of-practice changes, they should consider the effects of not only provider type but also team-based care on outcomes. Interventions that may encourage provider team formation, including but not limited to scope-of-practice reforms, may improve the value of care.
INTRODUCTION
In response to COVID-19, the Centers for Medicare and Medicaid Services (CMS) and many state governments have relaxed scope-of-practice restrictions for nurse practitioners (NPs) and physician assistants (PAs).(1–3) In states where NPs and PAs do not have full practice authority, scope-of-practice restrictions include physician supervision requirements and prescribing limits.(4–6) Insight into the impact of scope-of-practice changes is important beyond their relaxation during the COVID-19 pandemic, as the supply of NPs and PAs is projected to grow much faster than that of physicians.(7)
Primary care NPs and PAs commonly practice in teams with and without physicians,(8) and scope-of-practice regulations may impact practice environments,(9) such as the propensity of these different provider types to organize into care teams. For instance, direct supervision requires a physician to be in office when a non-physician performs a service,(10) possibly encouraging team formation. Conversely, by increasing the opportunity cost of hiring non-physicians, supervision requirements may potentially discourage team formation. To understand the potential impact of scope-of-practice changes, it is thus essential to understand not only differences in solo care outcomes by provider type, but also differences in outcomes of team-based versus solo care as well as by team composition. Importantly, since interprofessional teams are more common in primary care than are intraprofessional teams, differences between provider types may manifest as differences between team-based and solo care.(9,11)
While training curricula differ for primary care physicians, NPs, and PAs, all are trained to deliver many of the same services, including management of common chronic diseases like type 2 diabetes mellitus (T2DM).(12) Increasing the population of NPs and PAs is often viewed as a solution to primary care workforce shortages in the context of an aging population.(13,14)
Emerging evidence on the outcomes of care delivered by NPs and PAs versus physicians suggests broadly similar performance. A 2018 Cochrane Review found that the outcomes of NP care are similar to or better than those for physician care, though the evidence was rated of “low-to-moderate certainty”.(15) In a seminal study that randomized patients to NPs versus physicians, a broad range of care outcomes—including self-rated health and biomarker measurements—were largely indistinguishable between NPs and physicians at 6-month and 2-year follow-up.(16,17) Subsequent observational studies have found that utilization patterns, and thus costs, may differ for care delivered by NPs and PAs versus physicians due to lower labor costs(18) and use of acute care services.(19,20)
Empirically, little is known about outcomes for intra- and inter-professional teams of physicians involving either NPs or PAs.(21–23) Co-management of patients by physicians and NPs has been proposed, and interviews have found that such an approach may increase guideline-concordant care and access for patients.(24) Studies of chronic disease management by interprofessional teams at one large physician practice(25) and the Veterans Health Administration(26) have found few clinically meaningful differences across provider type or team composition. To our knowledge, however, there has been no large-scale empirical study that assesses the joint impact of provider type and team-based care across multiple independent practices and payers.
In this study, we examined whether and how outcomes following new chronic disease onset differed both by team-based versus solo care and by physician versus non-physician (i.e., NP or PA) care in a national sample of primary care practices from 2013 to 2018. For teams, we further investigated the role of team composition. Using de-identified electronic health record (EHR) data, we overcame two major empirical challenges inherent to the claims data that most prior studies have used to study care differences by provider type. First, traditional claims data often do not accurately record the rendering service provider, thus undercounting care provided by NPs and PAs that is billed under the physician with whom they work.(27) Second, unlike traditional claims data, our EHR data contained the very biomarker values on which providers base their clinical decisions, thus improving the relevance and precision of our outcomes and our risk adjustment. For three common chronic diseases—T2DM, hyperlipidemia, and hypertension—we assessed differences by team-based versus solo care and by physician versus non-physician care in diagnosis, prescribing, monitoring, and biomarker-based outcomes (notably hemoglobin A1c [A1c], LDL cholesterol [LDL], and systolic blood pressure) following disease onset.
METHODS
Data Source
We used de-identified EHR data from athenahealth, a large national EHR vendor, that included detailed visit-level information on over 12 million primary care visits for over one million patients from 2013 to 2018. In addition to sociodemographic characteristics, we observed visit-level biomarkers such as A1c, LDL, and blood pressure. Each visit was associated with its service provider, enabling us to investigate provider actions with greater precision than relying on the billing provider. Overall, the data included 2,028 primary care providers, of whom 59.6% (n=1,209) were physicians, 29.0% (n=588) were NPs, and 11.4% (n=231) were PAs. Our sample included a stable cohort of 250 practices belonging to 175 organizations. This study was deemed exempt by the authors’ Institutional Review Board.
Study Design and Sample Construction
We mitigated the risk that patients may have selected their providers based on disease severity by identifying time of disease onset using a patient’s first abnormal biomarker and attributing outcomes to the providers involved in care only through that time. Specifically, we used biomarker evidence to create separate study samples for T2DM, hyperlipidemia, and hypertension. For each condition, we identified patients with new disease onset based on biomarker evidence: A1c greater than or equal to 6.5% for T2DM,(28) LDL greater than or equal to 160 mg/dL for hyperlipidemia,(29) and three visits with systolic blood pressure greater than or equal to 140 mmHg (prior to 11/13/2017) or 130 mmHg (starting on 11/13/2017, per revised guidelines) for hypertension.(30) We identified time of disease onset as the first visit associated with a biomarker value meeting the above disease-specific thresholds. For each disease separately, we excluded patients with prior diagnosis of the disease or with prior relevant medication prescription. We also excluded patients who had a biomarker value above threshold associated with their first visit in our data (Exhibit A1).(31)
Identification of Provider Team and Type
We categorized patients as receiving solo or team-based care based on their visits at the same practice in the six months preceding disease onset (i.e., time of first abnormal diagnostic biomarker). We classified care during this time by just one provider as “solo” and care by multiple providers as “team-based”. We further distinguished teams and solo providers by provider type. Team categories were physician teams, non-physician (i.e., NP or PA) teams, and mixed teams (i.e., with both physicians and non-physicians). Solo provider categories were physician and non-physician (i.e., NP and PA). We aggregated NPs and PAs for our main analysis due to a relatively small number of patients receiving care from PA-only, NP-only, and mixed NP and PA teams. Results disaggregated by NP and PA providers remained substantially similar and are presented in the Appendix.(31)
Outcome Measurement
We examined process and outcome measures of chronic disease management, chosen to identify a range of care activities in the treatment pathway. Process measures included the presence of clinical diagnosis on a claim within 30 days of disease onset (to investigate whether providers recognized that biomarker evidence was consistent with disease onset), writing at least two prescriptions for disease-specific medication in the year following disease onset, and evidence of disease monitoring via follow-up biomarkers in the year after disease onset. Our main outcome measure was disease control within one year of disease onset. We defined disease control as an A1c of 7.0% or less for T2DM,(32) an LDL of 100 mg/dL or less for hyperlipidemia,(29) and a systolic blood pressure of less than 140 or 130 mmHg (see above) for hypertension.(30) See Appendix for additional biomarker-based outcomes.(31)
Statistical Analysis
We used linear probability models to estimate the association between provider team and type and outcomes. We included organization and year fixed effects to account for potential time-invariant organization characteristics (such as local practice protocols) and common time trends in outcomes. We adjusted for the possibility that patients may see a new provider following disease onset, as such care may not be attributable to the original provider team. Risk adjustment of all outcomes included disease-specific biomarker values at disease onset, body mass index, twelve indicators of common comorbidities, a count of primary care visits in the year prior to disease onset, and patient sociodemographic characteristics including age, sex, race, ZIP-level median income, and insurance payer. We clustered our standard errors at the organization level. Additional details are in the Appendix.(31)
Limitations
Our study had several limitations. First, because our study was retrospective, unmeasured confounders may have affected the relationship between provider team or type and outcomes. We mitigated this concern by leveraging data that included disease-specific biomarkers observed in clinical practice. Identification of disease onset using initial biomarker evidence further mitigated selection risk, as patients cannot have selected their initial provider based on knowledge of having the disease.
Second, an inherent limitation of our data is that we cannot observe interactions, communication, or collaboration between providers. At the extreme, it may be that patients whom we classified as receiving team-based care in fact received care from multiple non-interacting providers. All providers in our sample, however, use the same EHR and are thus, at a minimum, able to see each other’s chart entries and can communicate via the EHR. Importantly, erroneously identifying non-interacting providers as teams would bias our comparisons of team-based versus solo care toward not finding any difference.
Third, our definition of team-based care is necessarily narrow. We do not observe other provider types, such as social workers. We identified teams over the six months preceding an abnormal biomarker to balance the likelihood that patients had enough time for multiple visits against the risk of attributing outcomes to non-team providers. Identifying teams within 12 months versus 6 months prior to disease onset does not substantively change our findings (results not shown).
Fourth, we constructed our disease control measure based on the presence of at least one normal biomarker measurement. This may have overestimated sustained disease control, as patients’ biomarkers may have subsequently worsened. See Exhibit A4 for additional biomarker-based outcomes.(31) While we consulted professional society guidelines, there remains uncertainty over appropriate diagnostic and disease control biomarker levels based on unobserved patient factors. Hyperlipidemia guidelines are based on LDL levels and atherosclerotic cardiovascular disease (CVD) risk estimates, which factor in disease characteristics unavailable in our data. By relying only on LDL, our sample may include patients who have high LDL but low CVD risk and may not include patients who have high CVD risk despite low LDL. However, this is unlikely to differ by provider type or team-based care given our controls and thus should not affect relative performance.
Fifth, although our data only included primary care visits, the prescriptions, as well as A1c and LDL biomarkers, we observed may have been ordered by specialists and then attributed to the closest primary care visit within 30 days. We used organization fixed effects to mitigate potential bias from the possibility that specialist care may systematically differ across provider types and between team-based versus solo care across organizations.
Finally, although our sample was national in scope, it came from a single large EHR vendor and was not nationally representative. Our data lacked geographic identifiers, which prevented us from accounting for variation in state scope-of-practice laws. However, by comparing provider teams and types within the same organization—and thus likely state—our research design mitigated concerns that our results were attributable to variation in scope-of-practice laws. See Exhibit A2 for a comparison of our sample to a nationally representative sample.(31)
RESULTS
Study Sample and Descriptive Statistics
Our study samples included 22,874 individuals with new-onset T2DM, 24,510 individuals with new-onset hyperlipidemia, and 28,078 individuals with new-onset hypertension. For T2DM and hypertension, but not for hyperlipidemia, disease severity at initial presentation, as measured by baseline biomarker results, was slightly worse for non-physician solo providers and non-physician teams, compared to solo physicians, physician teams, and mixed teams (Exhibit A3).(31) We controlled for differences in baseline disease severity as well as other relevant patient, provider, and practice characteristics in subsequent analyses, as detailed in the appendix.(31)
We characterized team-based care and provider type based on the provider who conducted the index visit associated with an abnormal biomarker value and those who delivered care over the preceding six-month period. The percentage of patients who received care from a single physician provider was 58.5% for T2DM patients, 54.4% for hyperlipidemia patients, and 45.5% for hypertension. The next most common were single non-physician providers (ranging from 16.5% to 21.5% across the three diseases) and a mixed team of physicians and non-physician providers (ranging from 12.8% to 17.9%) Additional sample characteristics are in Exhibit A3.(31)
Teams outperformed solo providers in managing chronic disease
Upon receiving an initial abnormal biomarker result, teams submitted diagnostic claims at significantly higher rates than solo providers for T2DM (44.4% vs. 41.1%, p < 0.001) and hypertension (14.0% vs. 12.0%, p < 0.001), but did so at similar rates for hyperlipidemia (31.0% vs. 30.6%, p = 0.60) (Exhibit 1).
Exhibit 1: Adjusted diagnosis rates for patients with new onset of type 2 diabetes, hyperlipidemia, or hypertension by team-based care and provider type, 2013–2018.
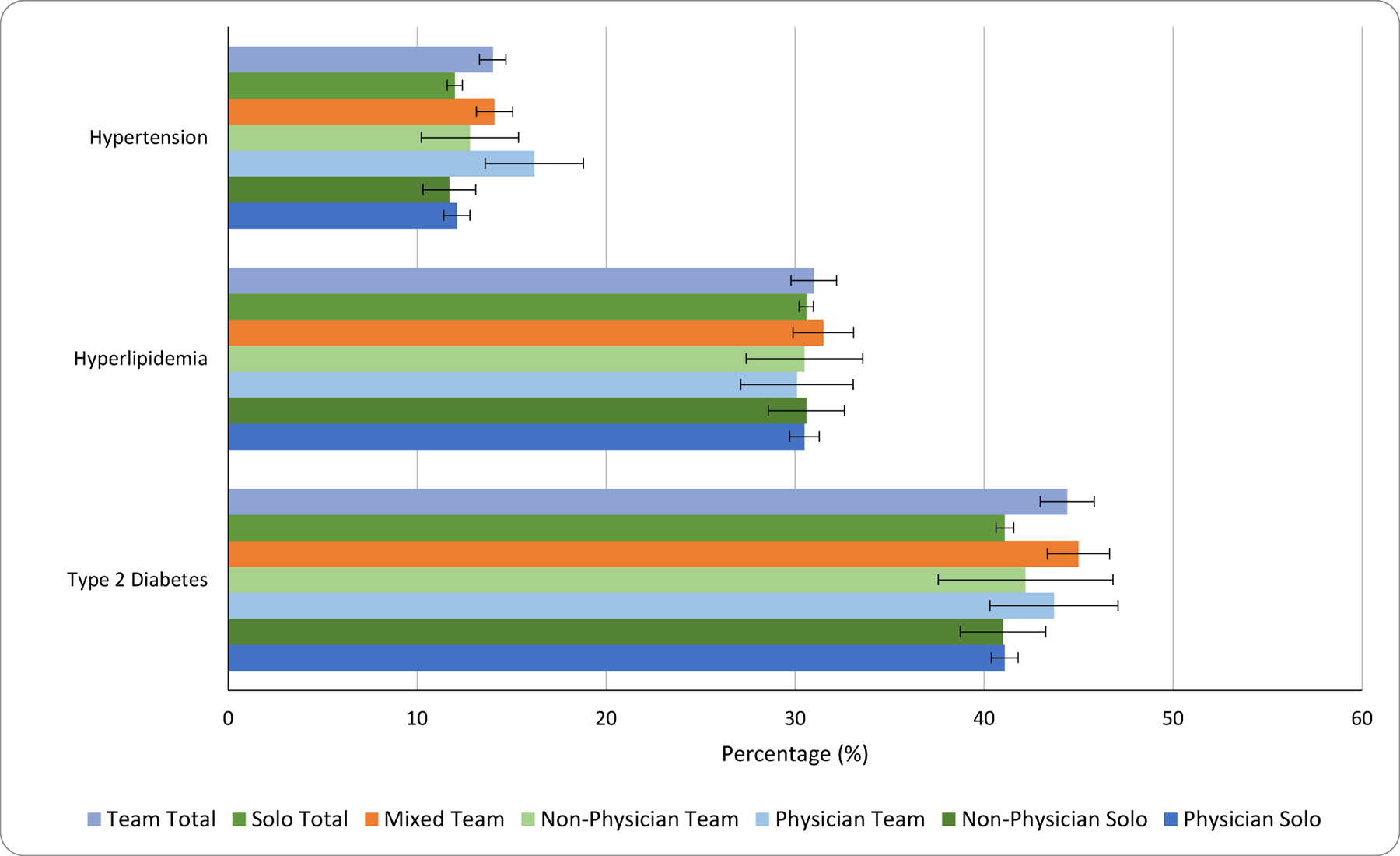
Source: Authors’ analysis of de-identified electronic health record data from 2013 to 2018 for adults with a new chronic disease as identified by an abnormal biomarker (N = 22,874 for type 2 diabetes, N = 24,510 for hyperlipidemia, and N = 28,078 for hypertension).
Notes: Colored bars indicate the predicted values from a regression of a claims-based diagnosis indicator on provider, including organization fixed effects as well as patient and disease severity covariates as described in the text. Error bars represent 95% confidence intervals. p-values for team total vs. solo total were as follows: diabetes, <0.001; hyperlipidemia, 0.595; hypertension, <0.001.. Non-physician providers are physician assistants and nurse practitioners. A mixed team is composed of both physician and non-physician providers.
Prescription ordering by teams versus solo providers differed substantially for all three chronic diseases (Exhibit 2). For example, 50.6% of T2DM patients treated by teams received at least two prescriptions (including refills) within 1 year, compared to 40.5% of patients treated by solo providers (p < 0.001).
Exhibit 2. Adjusted prescription rates for patients with new onset of type 2 diabetes, hyperlipidemia, or hypertension by team-based care and provider type, 2013–2018.
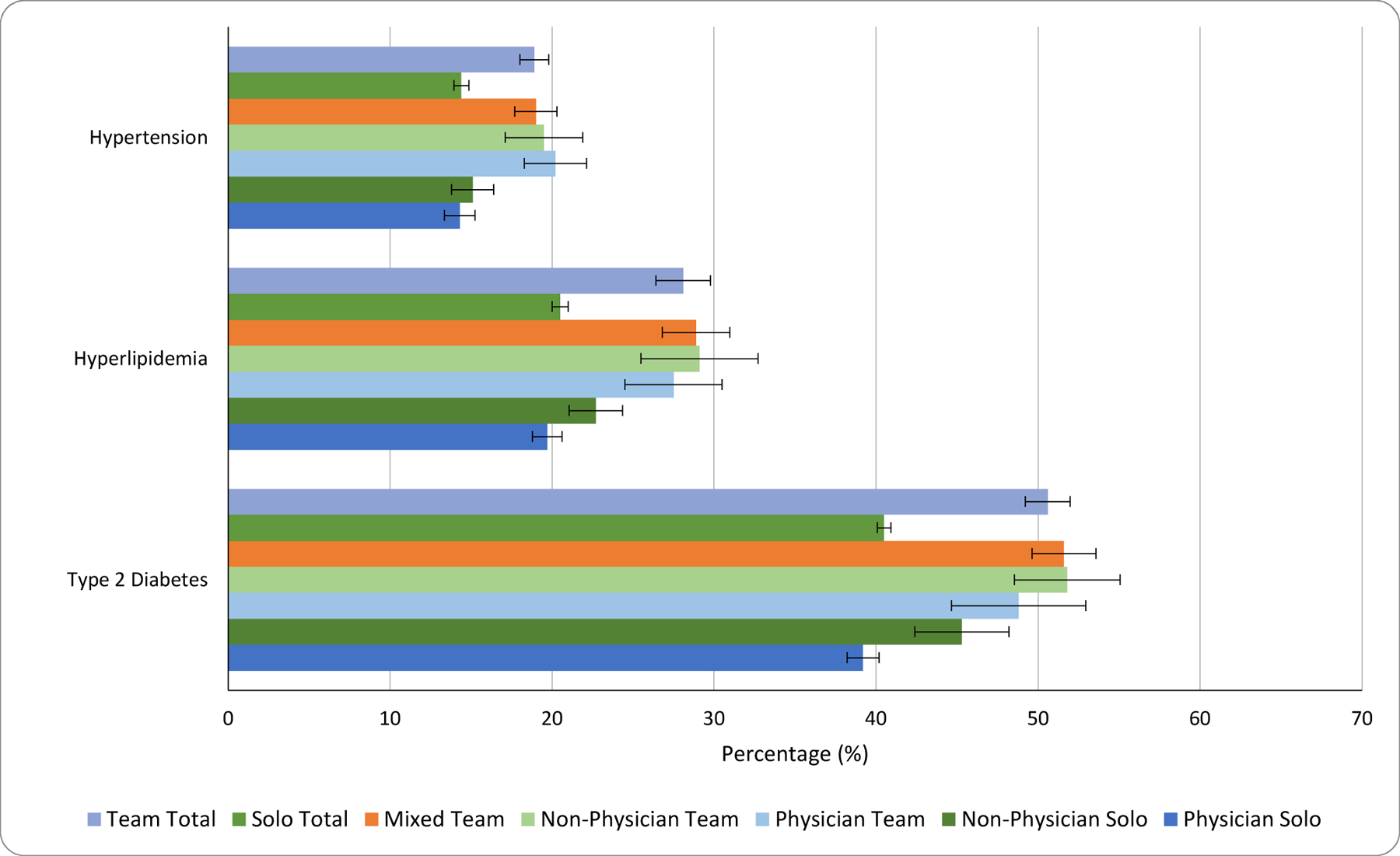
Source: Authors’ analysis of de-identified electronic health record data from 2013 to 2018 for adults with a new chronic disease as identified by an abnormal biomarker (N = 22,874 for type 2 diabetes, N = 24,510 for hyperlipidemia, and N = 28,078 for hypertension).
Notes: Colored bars indicate the predicted values from a regression of an indicator for a patient receiving at least two disease-appropriate prescription orders (including refills) within one year on provider, including organization fixed effects as well as patient and disease severity covariates as described in the text. Error bars represent 95% confidence intervals. p-values for team total vs. solo total were as follows: diabetes, <0.001; hyperlipidemia, <0.001; hypertension, <0.001. Non-physician providers are physician assistants and nurse practitioners. A mixed team is composed of both physician and non-physician providers.
Exhibit 3 presents our results for follow-up biomarker monitoring. Frequent monitoring on the order of every 3 to 6 months via biomarkers is part of standard guidelines for T2DM and hyperlipidemia. We found that teams were more likely to order at least one follow-up biomarker test within a year of an initial abnormal biomarker result for T2DM (56.3% vs. 46.5%, p < 0.001) and hyperlipidemia (60.4% vs. 47.1%, p < 0.001). We did not examine this care indicator for hypertension, as office blood pressures are routinely taken during office visits, rendering them a less-informative indicator of active monitoring.
Exhibit 3. Adjusted lab monitoring rates for patients with new onset of type 2 diabetes or hyperlipidemia by team-based care and provider type, 2013–2018.
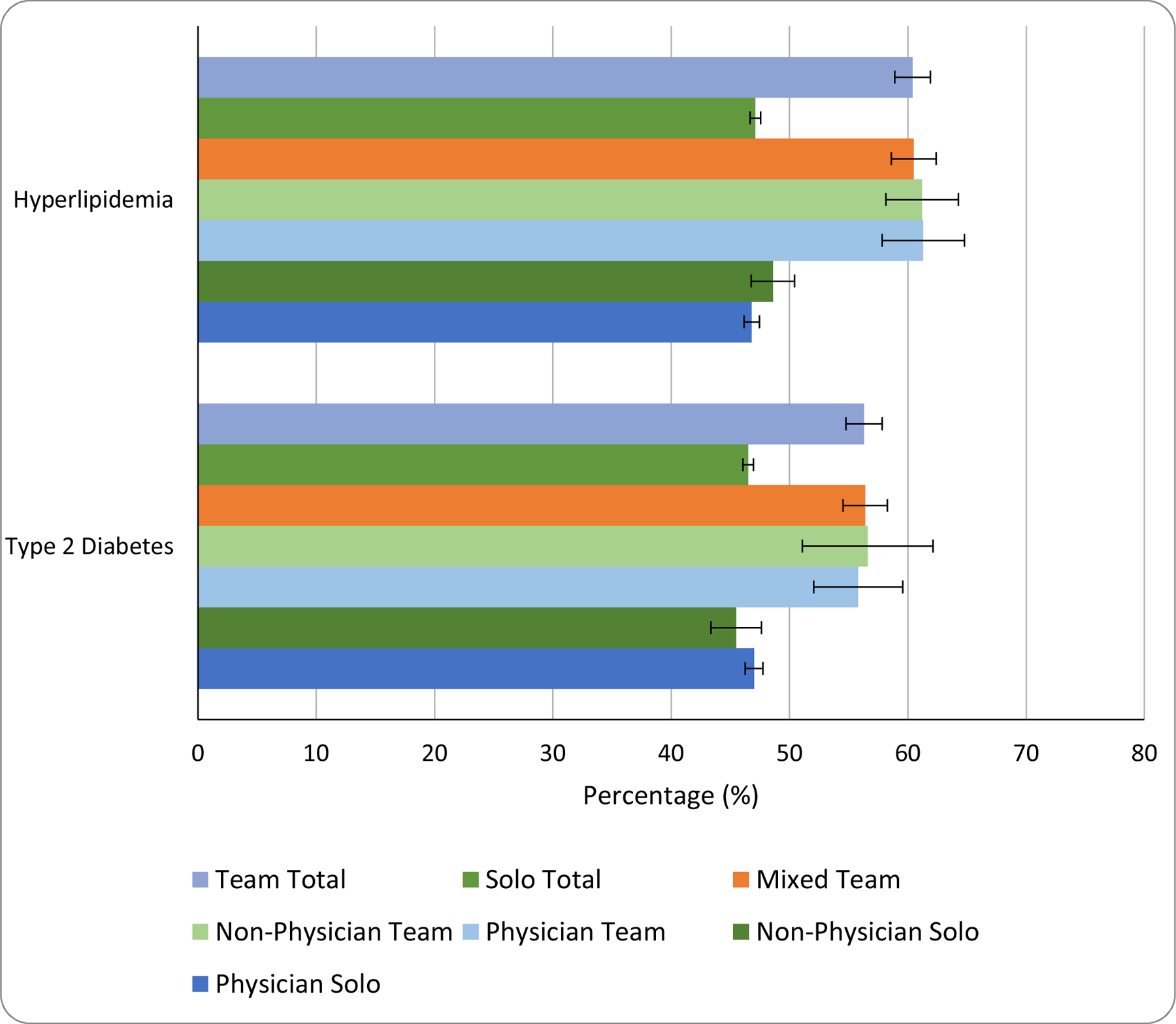
Source: Authors’ analysis of de-identified electronic health record data from 2013 to 2018 for adults with a new chronic disease as identified by an abnormal biomarker (N = 22,874 for type 2 diabetes, and N = 24,510 for hyperlipidemia).
Notes: Colored bars indicate the predicted values from a regression of an indicator for a patient having at least one disease-appropriate lab result within one year (i.e., hemoglobin A1c for type 2 diabetes and LDL cholesterol for hyperlipidemia) on provider, including organization fixed effects as well as patient and disease severity covariates as described in the text. Error bars represent 95% confidence intervals. p-values for team total vs. solo total were as follows: diabetes, <0.001; hyperlipidemia, <0.001. Non-physician providers are physician assistants and nurse practitioners. A mixed team is composed of both physician and non-physician providers. This outcome was not examined for hypertension since blood pressures are routinely taken during visits and thus may not be informative of active hypertension monitoring.
Exhibit 4 presents our results for disease control based on biomarkers—A1c for T2DM, LDL for hyperlipidemia, and systolic blood pressure for hypertension. For all three chronic diseases, teams were more likely than solo providers to have patients whose disease was brought under control. For example, patients seen by teams were 9.2 percentage points more likely to have their T2DM brought under control (63.9% vs. 54.7%, p < 0.001); for hyperlipidemia and hypertension, patients seen by teams were, respectively, 2.3 percentage points (9.1% vs. 6.8%, p < 0.001) and 6.1 percentage points (71.0% vs. 64.9%, p < 0.001) more likely to have their disease brought under control.
Exhibit 4. Adjusted biomarker-based disease control outcomes for patients with new onset of type 2 diabetes, hyperlipidemia, and hypertension by team-based care and provider type, 2013–2018.
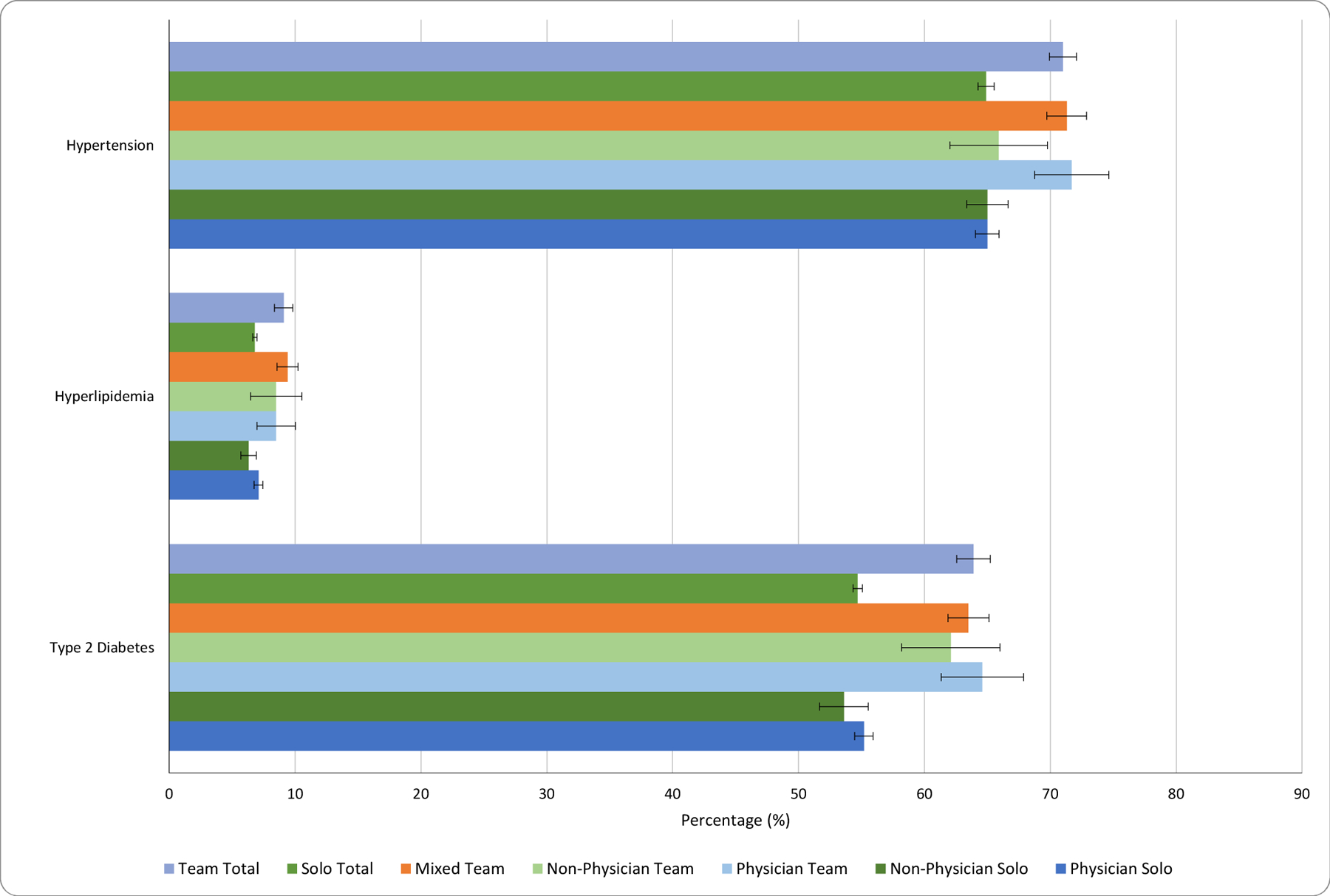
Source: Authors’ analysis of de-identified electronic health record data from 2013 to 2018 for adults with a new chronic disease as identified by an abnormal biomarker (N = 22,874 for type 2 diabetes, N = 24,510 for hyperlipidemia, and N = 28,078 for hypertension).
Notes: Colored bars indicate the predicted values from a regression of disease control, as measured by disease-specific biomarker levels below guideline-concordant biomarker targets within one year, on provider, including organization fixed effects as well as patient and disease severity covariates as described in the text. Error bars represent 95% confidence intervals. p-values for team total vs. solo total were as follows: diabetes, <0.001; hyperlipidemia, <0.001; hypertension, <0.001. Non-physician providers are physician assistants and nurse practitioners. A mixed team is composed of both physician and non-physician providers.
For all outcomes, we also examined differences by team composition (i.e., physician team, non-physician team, mixed team). Physician-only and mixed teams performed better than non-physician teams in the management of hypertension (e.g., 71.7% and 71.3%, respectively, vs. 65.9% of patients achieved control within one year, both p < 0.001), but we otherwise found no significant differences by team composition for the outcomes in the main text. See Exhibit A4 for additional biomarker-based outcomes.(31)
Solo physician and non-physician providers performed similarly
Across chronic disease management outcomes, non-physicians largely performed similarly to physicians. We found no significant differences between solo physicians and non-physicians with respect to diagnosis rates for all three diseases (Exhibit 1), follow-up labs for T2DM (Exhibit 3), or biomarker-based outcomes for hypertension (Exhibit 4).
Notably, we did find meaningful differences in prescribing behavior for T2DM and hyperlipidemia, with physicians less likely to prescribe antidiabetics by 6.1 percentage points and cholesterol-lowering drugs by 3.0 percentage points, compared to non-physicians (39.2% vs. 45.3% and 19.7% vs. 22.6%, respectively, both p < 0.05). Prescribing for antihypertensives, however, was similar (14.3% for physicians vs. 15.1% for non-physicians, p = 0.46) (Exhibit 2).
Results remained substantially similar when we disaggregated non-physicians into NPs and PAs. One notable exception was the management of T2DM. For example, prescribing of antidiabetics was significantly higher for NPs (49.4%) compared to both physicians (41.4%, p < 0.001) and PAs (42.8%, p < 0.001), and similar for PAs and physicians (p = 0.58). See Exhibits A5–A9 for additional results.(31)
DISCUSSION
We provide, to our knowledge, the first large-scale comparison of new-onset chronic disease management by team-based versus solo care and by physician versus non-physician (i.e., NP or PA) care across multiple independent provider organizations and payers. Our findings suggest that teams outperformed solo providers, largely irrespective of team composition. Teams of all compositions were roughly equally effective in managing new-onset T2DM and hyperlipidemia, but non-physician teams performed worse in controlling new-onset hypertension. Among solo providers, we found little meaningful difference between physician and non-physician providers, though physicians were less likely than non-physicians to prescribe medications for T2DM and hyperlipidemia.
Team performance
Provider teams may have outperformed solo providers for several reasons. Having multiple providers allows for several sets of eyes that may catch details a single individual may miss. Having multiple providers may also allow for “team sourcing” of knowledge rather than relying on the knowledge of a single provider.(33) Further, teams may benefit from complementarities between the human capital of different providers that produce synergies that go beyond the sum of individual contributions. For instance, prior research using similar data to ours has shown that scheduled visit duration is substantially longer for NPs compared to physicians,(34) which may indicate that NPs provide more high-touch relational care. Care-improving complementarities may exist between this type of care and care by physicians. Finally, providing care in teams may relax time or capacity constraints on solo providers. Future research should aim to disentangle these potential mechanisms.
Our team definition captures whether a patient had visits with multiple providers, likely a necessary but not sufficient prerequisite for meaningful teamwork. Given inherent data limitations, we are unable to directly observe interaction among team members. The increasing availability of data sources that include EHR communications or organization-specific team charts, however, may enable such work in the future.
Solo performance
Our finding that solo primary care providers exhibited little meaningful difference between physicians and non-physicians echoes the results of prior studies.(15,35) While some may be concerned that patient severity differed between provider types—with physicians caring for sicker patients—this did not appear to be the case; if anything, it appears that non-physicians in our sample were caring for slightly sicker patients (see Exhibit A2).(31) We did, however, observe differences in prescribing behavior between solo physicians and non-physicians. Although medication initiation is often a shared decision between the patient and provider,(36) and lifestyle changes can be a first-line treatment, such differences in prescribing—without commensurate differences in biomarker outcomes—suggest an avenue for further study.
A competing explanation for the lack of a substantive difference between provider types is the increased routinization of care for common chronic diseases,(37) which may tend to equalize both processes and resulting outcomes across providers. Future work should investigate whether our findings hold for less common or more acute conditions.
Low absolute performance
Although we found meaningful relative differences in chronic disease management for team-based versus solo care, we also found low absolute performance across the board. Patients may have sought additional care from providers outside athenahealth’s EHR, which our data would not capture. Low absolute performance, however, is in line with prior work documenting low outpatient care quality on process-based measures.(38,39) Though we note the data limitations discussed previously and are hesitant to argue that the goal for our measures is 100% completion, the presence of gaps in diagnosis, prescription, and monitoring of the magnitude we observed raises concerns and provides further motivation for chronic disease management improvement interventions, particularly for hyperlipidemia, for which we observed very low disease control rates.
Policy implications
Our findings demonstrated improved performance of provider teams over solo providers. To improve primary care outcomes, policymakers should consider a set of interventions that could encourage team formation and practice, such as innovative primary care delivery models and value-based payment reform that rewards collaboration. Risk-adjusted capitation may be one strategy to encourage primary care practices to adopt team-based care, though relatively generous payments may be needed to make this financially sustainable for practices.(40) By increasing the proportion of non-physician providers, accountable care organizations (ACOs) may also encourage team formation.(41) Given that non-physicians’ labor costs are lower and their ranks projected to grow much faster compared to physicians,(7) facilitating interprofessional teams may be an option with particularly high value that retains the option value of potential synergies between the skill sets of different provider types.
Our findings may contribute to discussions on changing scope-of-practice regulations. Scope-of-practice laws may impact outcomes by changing the propensity of providers to form teams even if they do not affect how provider types perform individually. Should scope-of-practice regulation indeed influence team formation, then policymakers need to understand the effect of team-based care in order to appropriately evaluate the potential effect of scope-of-practice changes on care outcomes. It is an open question, however, whether scope-of-practice restrictions do encourage team formation, which future work should explore.
CONCLUSION
Provider teams of all compositions outperformed solo providers in the management of three common, new-onset chronic diseases across a national sample of primary care practices from 2013 to 2018. Among solo providers, care management and outcomes showed little difference between physicians and non-physicians (i.e., NPs and PAs). As policymakers contemplate scope-of-practice regulation, they should consider the effect of not only provider type but also team-based care on care outcomes. Interventions that may encourage provider team formation, including but not limited to scope-of-practice reforms, may improve the value of care.
Supplementary Material
Contributor Information
Maximilian J. Pany, Harvard Medical School, in Boston, Massachusetts.
Lucy Chen, Harvard Medical School, in Boston, Massachusetts.
Bethany Sheridan, athenahealth, Inc., in Watertown, Massachusetts.
Robert S. Huckman, Harvard Business School, in Boston, Massachusetts.
REFERENCES
- 1.HHS Secretary Azar’s March 24, 2020 Letter to Governors [Internet] [cited 2020 Aug 6]. Available from: https://www.nga.org/wp-content/uploads/2020/03/Governor-Letter-from-Azar-March-24.pdf
- 2.COVID-19 State Emergency Response: Temporarily Suspended and Waived Practice Agreement Requirements [Internet] AANP. [cited 2020 Aug 6]. Available from: https://www.aanp.org/advocacy/state/covid-19-state-emergency-response-temporarily-suspended-and-waived-practice-agreement-requirements
- 3.COVID-19 State Emergency Response [Internet] AAPA. [cited 2020 Aug 6]. Available from: https://www.aapa.org/news-central/covid-19-resource-center/covid-19-state-emergency-response/
- 4.NP Scope of Practice Laws [Internet] Barton Associates. [cited 2020 Aug 6]. Available from: https://www.bartonassociates.com/locum-tenens-resources/nurse-practitioner-scope-of-practice-laws
- 5.PA Scope of Practice Laws [Internet] Barton Associates. [cited 2020. Aug 6]. Available from: https://www.bartonassociates.com/locum-tenens-resources/pa-scope-of-practice-laws
- 6.American Medical Association. Physician assistant scope of practice [Internet] 2018. [cited 2020 Aug 6]. Available from: https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/arc-public/state-law-physician-assistant-scope-practice.pdf
- 7.U.S. Bureau of Labor Statistics. Healthcare Occupations [Internet]. Occupational Outlook Handbook 2020. [cited 2020 Nov 17]. Available from: https://www.bls.gov/ooh/healthcare/home.htm
- 8.Auerbach DI, Staiger DO, Buerhaus PI. Growing Ranks of Advanced Practice Clinicians — Implications for the Physician Workforce. N Engl J Med 2018. Jun 21;378(25):2358–60. [DOI] [PubMed] [Google Scholar]
- 9.Poghosyan L, Boyd DR, Clarke SP. Optimizing full scope of practice for nurse practitioners in primary care: A proposed conceptual model. Nurs Outlook 2016. Apr;64(2):146–55. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Medicare & Medicaid Services (CMS). CMS Manual System: Pub 100–07 State Operations Provider Certification [Internet] 2007. Available from: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R29SOMA.pdf
- 11.Donelan K, DesRoches CM, Dittus RS, Buerhaus P. Perspectives of physicians and nurse practitioners on primary care practice. N Engl J Med 2013. May 16;368(20):1898–906. [DOI] [PubMed] [Google Scholar]
- 12.Dewan MJ, Norcini JJ. Pathways to Independent Primary Care Clinical Practice: How Tall Is the Shortest Giant? Acad Med 2019. Jul;94(7):950–954. [DOI] [PubMed] [Google Scholar]
- 13.Fairman JA, Rowe JW, Hassmiller S, Shalala DE. Broadening the Scope of Nursing Practice. N Engl J Med 2011. Jan 20;364(3):193–6. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health [Internet] Washington, D.C.: National Academies Press; 2011. [cited 2020 Aug 6]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK209880/ [PubMed] [Google Scholar]
- 15.Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev 2018. 16;7:CD001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mundinger MO, Kane RL, Lenz ER, Totten AM, Tsai W-Y, Cleary PD, et al. Primary Care Outcomes in Patients Treated by Nurse Practitioners or Physicians: A Randomized Trial. JAMA 2000. Jan 5;283(1):59–68. [DOI] [PubMed] [Google Scholar]
- 17.Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary Care Outcomes in Patients treated by Nurse Practitioners or Physicians: Two-Year Follow-Up. Med Care Res Rev 2004. Sep 1;61(3):332–51. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Bureau of Labor Statistics. May 2019 Occupation Profiles [Internet] Occupational Employment Statistics. 2020. [cited 2020 Nov 17]. Available from: https://www.bls.gov/oes/current/oes_stru.htm#29-0000 [Google Scholar]
- 19.Morgan PA, Smith VA, Berkowitz TSZ, Edelman D, Van Houtven CH, Woolson SL, et al. Impact Of Physicians, Nurse Practitioners, And Physician Assistants On Utilization And Costs For Complex Patients. Health Aff (Millwood) 2019. Jun 1;38(6):1028–36. [DOI] [PubMed] [Google Scholar]
- 20.Perloff J, DesRoches CM, Buerhaus P. Comparing the Cost of Care Provided to Medicare Beneficiaries Assigned to Primary Care Nurse Practitioners and Physicians. Health Serv Res 2016. Aug;51(4):1407–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poghosyan L, Norful AA, Martsolf GR. Primary Care Nurse Practitioner Practice Characteristics. J Ambulatory Care Manage 2017;40(1):77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? JAMA 2004. Mar 10;291(10):1246–51. [DOI] [PubMed] [Google Scholar]
- 23.Körner M, Bütof S, Müller C, Zimmermann L, Becker S, Bengel J. Interprofessional teamwork and team interventions in chronic care: A systematic review. J Interprof Care 2016. Jan;30(1):15–28. [DOI] [PubMed] [Google Scholar]
- 24.Norful AA, de Jacq K, Carlino R, Poghosyan L. Nurse Practitioner–Physician Comanagement: A Theoretical Model to Alleviate Primary Care Strain. Ann Fam Med 2018. May;16(3):250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Everett CM, Thorpe CT, Palta M, Carayon P, Bartels C, Smith MA. Physician Assistants and Nurse Practitioners Perform Effective Roles on Teams Caring for Medicare Patients with Diabetes. Health Affairs 2013. Nov;32(11):1942–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Everett CM, Morgan P, Smith VA, Woolson S, Edelman D, Hendrix CC, et al. Primary care provider type: Are there differences in patients’ intermediate diabetes outcomes? JAAPA Off J Am Acad Physician Assist 2019. Jun;32(6):36–42. [DOI] [PubMed] [Google Scholar]
- 27.Kuo Y-F, Raji MA, Lin Y-L, Ottenbacher ME, Jupiter D, Goodwin JS. Use of Medicare Data to Identify Team-based Primary Care: Is it Possible? Med Care 2019. Nov;57(11):905–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018. Jan 1;41(Supplement 1):S13–27. [DOI] [PubMed] [Google Scholar]
- 29.Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. European Heart Journal 2016. Oct 14;37(39):2999–3058. [DOI] [PubMed] [Google Scholar]
- 30.Whelton Paul K, Carey Robert M, Aronow Wilbert S, Casey Donald E, Collins Karen J, Dennison Himmelfarb Cheryl, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018. Jun 1;71(6):e13–115. [DOI] [PubMed] [Google Scholar]
- 31. To access the appendix, click on the Details tab of the article online.
- 32.American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018. Jan 1;41(Supplement 1):S55–64. [DOI] [PubMed] [Google Scholar]
- 33.Staats BR, Valentine M, Edmondson AC. Performance Tradeoffs in Team Knowledge Sourcing. SSRN Electron J [Internet] 2011. [cited 2020 Aug 6]; Available from: http://www.ssrn.com/abstract=1677627 [Google Scholar]
- 34.Neprash HT, Smith LB, Sheridan B, Hempstead K, Kozhimannil KB. Practice Patterns of Physicians and Nurse Practitioners in Primary Care. Medical Care 2020. Oct;58(10):934–41. [DOI] [PubMed] [Google Scholar]
- 35.Kurtzman ET, Barnow BS. A Comparison of Nurse Practitioners, Physician Assistants, and Primary Care Physicians’ Patterns of Practice and Quality of Care in Health Centers: Med Care 2017. Jun;55(6):615–22. [DOI] [PubMed] [Google Scholar]
- 36.Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared Decision Making: A Model for Clinical Practice. J Gen Intern Med 2012. Oct;27(10):1361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Institute of Medicine. Clinical Practice Guidelines We Can Trust [Internet] Washington, D.C.: National Academies Press; 2011. [cited 2020 Aug 6]. Available from: https://www.nap.edu/catalog/13058 [Google Scholar]
- 38.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The Quality of Health Care Delivered to Adults in the United States. N Engl J Med 2003. Jun 26;348(26):2635–45. [DOI] [PubMed] [Google Scholar]
- 39.Levine DM, Linder JA, Landon BE. The Quality of Outpatient Care Delivered to Adults in the United States, 2002 to 2013. JAMA Intern Med 2016. Dec 1;176(12):1778–90. [DOI] [PubMed] [Google Scholar]
- 40.Basu S, Phillips RS, Song Z, Bitton A, Landon BE. High Levels Of Capitation Payments Needed To Shift Primary Care Toward Proactive Team And Nonvisit Care. Health Affairs 2017. Sep;36(9):1599–605. [DOI] [PubMed] [Google Scholar]
- 41.Nyweide DJ, Lee W, Colla CH. Accountable Care Organizations’ Increase In Nonphysician Practitioners May Signal Shift For Health Care Workforce. Health Affairs 2020. Jun 1;39(6):1080–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


