Abstract
This study investigated the effects of nobiletin on cardiorenal changes and the underlying mechanisms involved in two-kidney, one-clip (2K-1C) hypertension. 2K-1C rats were treated with nobiletin (15 or 30 mg/kg/day) or losartan (10 mg/kg/day) for 4 weeks (n = 8/group). Nobiletin (30 mg/kg) reduced high levels of blood pressure and circulating angiotensin II and angiotensin-converting enzyme activity in 2K-1C rats. Left ventricular (LV) dysfunction and remodelling in 2K-1C rats were alleviated in the nobiletin-treated group (P < 0.05). Nobiletin reduced the upregulation of Ang II type I receptor (AT1R)/JAK (Janus kinase)/STAT (signal transducer and activator of transcription) protein expression in cardiac tissue of 2K-1C rats (P < 0.05). The reduction in kidney function, and accumulation of renal fibrosis in 2K-1C rats were alleviated by nobiletin (P < 0.05). Overexpression of AT1R and NADPH oxidase 4 (Nox4) protein in nonclipped kidney tissue was suppressed in the nobiletin-treated group (P < 0.05). The elevations in oxidative stress parameters and the reductions in antioxidant enzymes were attenuated in 2K-1C rats treated with nobiletin (P < 0.05). In summary, nobiletin had renin-angiotensin system inhibitory and antioxidant effects and attenuated LV dysfunction and remodelling via restoration of the AT1R/JAK/STAT pathway. Nobiletin also resolved renal damage that was related to modulation of the AT1R/Nox4 cascade in 2K-1C hypertension.
Subject terms: Molecular biology, Physiology
Introduction
Renovascular hypertension is initiated by renal artery narrowing or renovascular stenosis and reduced renal blood flow. Goldblatt and coworkers first developed a renovascular hypertension model in dogs, and later, the two-kidney, one-clip (2K-1C) model was established in rats1,2. It is well recognized that the renin-angiotensin system (RAS) plays an important role in the development of hypertension in the 2K-1C model. Increases in circulating angiotensin II (Ang II) and angiotensin-converting enzyme (ACE) activity have been confirmed to occur in 2K-1C-induced hypertension in animals3. Subsequently, activation of RAS-mediated cardiovascular dysfunction and hypertrophy in renovascular hypertension has been noted4. Impairment of kidney function as well as kidney injury induced by stenosis of a renal artery have been reported in an animal model of renovascular hypertension. These are clearly associated with a high level of circulating Ang II5,6. Ang II, the key product of RAS, is a powerful vasoconstrictor that promotes an elevation in systemic vascular resistance and high blood pressure. The most pathological actions of Ang II on the heart, vessels and kidneys are mediated by local tissue Ang II type I receptor (AT1R)7. The decline in left ventricular function induced by 2K-1C modelling is associated with high levels of Ang II8. Several studies have reported overexpression of AT1R protein in cardiac tissue that is related to hypertrophy and remodelling in 2K-1C animals9,10. In kidney tissue, glomerular and tubulointerstitial damage in the nonclipped kidney associated with increased serum Ang II has been observed in 2K-1C rats5. Additionally, 2K-1C-induced hypertensive rats have kidney interstitial fibrosis and kidney dysfunction that are linked to overactivation of ROS production11.
One of the molecular mechanisms of RAS activation-induced organ damage has been proposed to be associated with oxidative stress since Ang II binding to AT1R can stimulate NADPH oxidase (Nox)12. It is well established that NADPH oxidase plays an important role in producing a reactive oxygen species, the superoxide anion radical (O2·−). 2K-1C rat models show oxidative stress, as evidenced by high levels of systemic malondialdehyde (MDA) and vascular O2·− production as well as suppression of antioxidant enzymes13,14. A previous study has shown that hypertension-induced kidney injury in rats is mediated by activation of the AT1R/Nox4/oxidative stress signalling pathway15. Moreover, the molecular mechanism of Ang II-induced cardiac remodelling has been elucidated to be related to the activation of the AT1R/JAK (Janus kinase)/STAT (signal transducer and activator of transcription) signalling pathway16. The STATs are a family of transcription factors found in rat cardiac fibroblasts and myocytes17. Activation of the JAK/STAT3 pathway by Ang II has been confirmed to play an important role in hypertrophic growth of cardiac myocytes18. Recently, Ye et al. found that reducing the levels of phospho-STAT3 can attenuate Ang II-induced cardiac fibrosis and hypertrophy in cardiomyocytes19.
Nobiletin is a polymethoxylated flavone, a class of flavonoids mostly isolated from the peels of citrus species20–22. Substantial evidence has revealed a variety of pharmacological properties of nobiletin, such as anticancer, anti-insulin resistance, anti-inflammatory, and antioxidant activities23. Liu et al. demonstrated that nobiletin reduces the cell viability and proliferation of the breast cancer cell line MCF-724. Nobiletin has nephroprotective effects by reducing oxidative stress in rats with acute kidney injury25. The antidiabetic effects of nobiletin have also been demonstrated: nobiletin restores blood glucose and insulin levels and ameliorates kidney dysfunction, tubular collagen deposition and injury in diabetic rats26. Additionally, the potential effects of nobiletin on the signs and complications of metabolic syndrome induced by a high-fat diet in rats have been revealed27. In rats with L-NAME-induced hypertension, nobiletin exhibits antihypertensive effects that are related to reduction of the sympathetic nerve-mediated contractile response, improvement of endothelial-dependent vascular relaxation, and alleviation of vascular remodelling via restoration of Nrf-2/HO-1 and MMP protein expression28. This study aimed to investigate the effects of nobiletin on cardiorenal structural and functional alterations and the mechanisms involved in 2K-1C rats.
Results
Effects of nobiletin or losartan on blood pressure and haemodynamic parameters
Changes of systolic blood pressure (SP) throughout of 7 weeks of experiments are shown in Fig. 1. At the beginning of the experiment, SP was not different among groups. After 2K-1C and sham operation, SP progressively increased in the 2K-1C-operated groups and was significantly higher than that in the sham-operated group after 2 weeks of induction. Oral administration of nobiletin at a dose of 30 mg/kg for 4 weeks markedly decreased SP in hypertensive rats (P < 0.05), while nobiletin at a dose of 15 mg/kg had no effect on SP in hypertensive rats. In addition, nobiletin (30 mg/kg) did not show a hypotensive effect in sham-operated rats. Losartan (10 mg/kg), a positive control agent, significantly reduced SP in the hypertensive group (P < 0.05). Furthermore, the SP did not differ between the nobiletin (30 mg/kg) and losartan groups.
Figure 1.
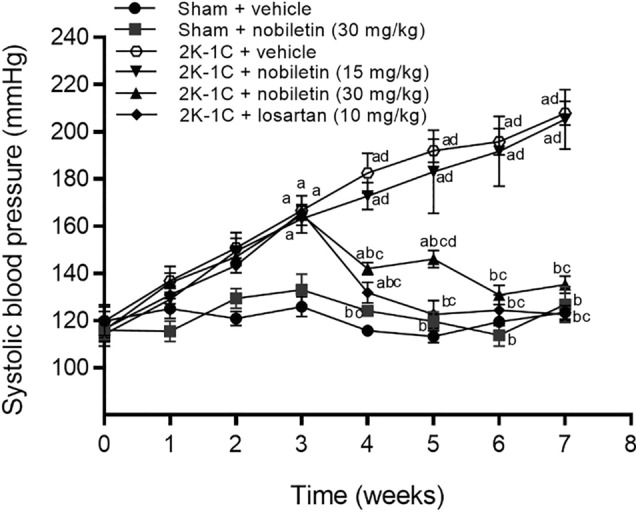
Effects of nobiletin or losartan on weekly systolic pressure (SP) in conscious 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C, cP < 0.05 vs. 2K-1C + nobiletin (15 mg/kg), dP < 0.05 vs. sham + nobiletin (30 mg/kg). 2K-1C two-kidney, one-clip.
The haemodynamic parameters measured under anaesthesia in all experimental groups are shown in Table 1. SP, DP, MAP, PP and HR were higher in 2K-1C rats than in control rats (P < 0.05). Compared to the untreated 2K-1C group, the group treated with nobiletin at a dose of 30 mg/kg significantly exhibited significantly attenuated alterations in these parameters, except HR, (P < 0.05). In addition, losartan treatment attenuated 2K-1C-induced hypertension and haemodynamic alterations. However, HR was not significantly different among the groups of 2K-1C rats.
Table 1.
Effects of nobiletin or losartan on haemodynamic parameters in 2K-1C rats under anaesthesia.
| Parameter | Sham | 2K-1C | |||
|---|---|---|---|---|---|
| Vehicle | Vehicle | Nobiletin 15 mg/kg |
Nobiletin 30 mg/kg |
Losartan 10 mg/kg |
|
| SP (mmHg) | 122 ± 3.97 | 195.89 ± 9.50a | 178.24 ± 10.94a | 131.21 ± 2.09b,c | 124.20 ± 2.53b,c |
| DP (mmHg) | 79.89 ± 4.42 | 130.98 ± 6.39a | 99.61 ± 3.82b | 85.68 ± 2.87b | 83.10 ± 2 .57b |
| MAP (mmHg) | 93.93 ± 4.20 | 152.61 ± 7.32a | 125.52 ± 4.75a,b | 100.52 ± 2.34b,c | 96.80 ± 2.35b,c |
| PP (mmHg) | 42.11 ± 1.73 | 64.91 ± 4.07a | 79.08 ± 11.03a | 44.54 ± 2.57b,c | 41.10 ± 2.12b,c |
| HR (beats/min) | 361.89 ± 16.53 | 425.53 ± 16.7a | 415.48 ± 23.65 | 364.62 ± 19.15 | 352.96 ± 7.56b |
The data are expressed as the means ± SEMs.
SP systolic blood pressure, DP diastolic blood pressure, MAP mean arterial pressure, PP pulse pressure, HR heart rate, 2K-1C two-kidney, one-clip.
aP < 0.05 vs. sham.
bP < 0.05 vs. 2K-1C.
cP < 0.05 vs. 2K-1C + nobiletin (15 mg/kg).
Effects of nobiletin or losartan on organ weights
After 7 weeks of the experimental period, reduced final body weights of untreated 2K-1C rats compared to untreated sham rats were observed (P < 0.05; Table 2). Nobiletin at a dose of 30 mg/kg or losartan significantly improved the BW of 2K-1C rats. In addition, the HW/BW, VW/BW, and LVW/BW ratios were significantly increased in untreated 2K-1C rats compared with sham-operated rats (P < 0.05; Table 2). After treatment with nobiletin at a dose of 30 mg/kg or losartan, the elevations in these ratios were attenuated in 2K-1C rats (P < 0.05; Table 2). However, nobiletin at a dose of 15 mg/kg did not improve the BW or the ratios in 2K-1C rats.
Table 2.
Effects of nobiletin or losartan on organ weight/body weight ratios in 2K-1C rats.
| Parameter | Sham | 2K-1C | |||
|---|---|---|---|---|---|
| Vehicle | Vehicle | Nobiletin 15 mg/kg |
Nobiletin 30 mg/kg |
Losartan 10 mg/kg |
|
| BW (g) | 546.75 ± 8.58 | 433.71 ± 32.71a | 503.00 ± 32.34 | 526.71 ± 10.29b | 531.67 ± 16.44b |
| HW/BW (mg/g) | 2.55 ± 0.05 | 3.79 ± 0.16a | 3.71 ± 0.34a | 2.69 ± 0.12b,c | 2.71 ± 0.07b,c |
| VW/BW (mg/g) | 2.17 ± 0.03 | 3.30 ± 0.14a | 3.23 ± 0.42a | 2.34 ± 0.12b,c | 2.40 ± 0.09b,c |
| LVW/BW (mg/g) | 1.66 ± 0.02 | 2.74 ± 0.12a | 2.68 ± 0.226a | 1.82 ± 0.11b,c | 1.84 ± 0.09b,c |
| RKW/BW (mg/g) | 3.37 ± 0.09 | 4.97 ± 0.20a | 4.74 ± 0.27a | 3.87 ± 0.17b,c | 3.87 ± 0.14b,c |
| LKW/BW (mg/g) | 3.35 ± 0.05 | 2.56 ± 0.14a | 2.5 ± 0.37a | 2.96 ± 0.24 | 3.02 ± 0.17 |
The data are expressed as the means ± SEMs.
HW/BW heart weight/body weight ratio, VW/BW ventricular weight/body weight ratio, LVW/BW left ventricular weight/body weight ratio, RKW/BW right kidney weight/body weight ratio, LKW/BW left kidney weight/body weight ratio, 2K-1C.
aP < 0.05 vs. sham.
bP < 0.05 vs. 2K-1C.
c P < 0.05 vs. 2K-1C + nobiletin (15 mg/kg).
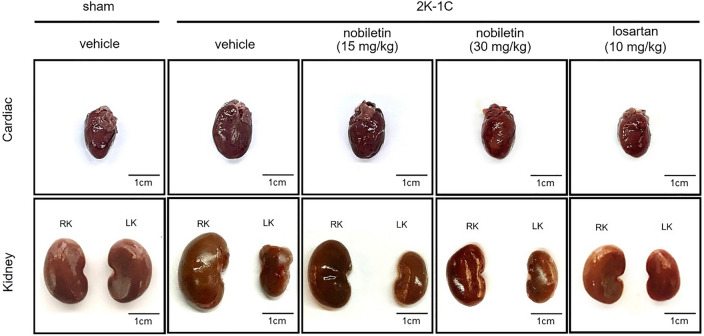
With regard to kidney weight, significant increases in RKW/BW and LKW/BW were found in 2K-1C rats compared to sham-operated rats (P < 0.05). Compared with no treatment, treatment with nobiletin at a dose of 30 mg/kg or losartan significantly reduced RKW/BW in 2K-1C rats (P < 0.05; Table 2). However, LKW/BW did not differ among the groups. Representative images of the hearts and kidneys are shown in Fig. 2.
Figure 2.
Representative images of the hearts (upper panel) and kidneys (lower panel) of 2K-1C rats after 7 weeks of the experiment (scale bar = 1 cm). RK right kidney (nonclipped side), LK left kidney (clipped side), 2K-1C two-kidney, one-clip.
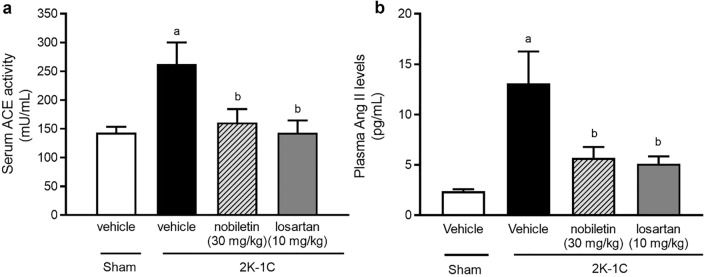
Effects of nobiletin and losartan on ACE activity and Ang II levels
The levels of serum ACE activity and plasma Ang II were significantly increased in the untreated 2K-1C group compared with the sham group (P < 0.05). However, nobiletin or losartan treatment alleviated RAS overactivity, as supported by the significant reductions in serum ACE activity and plasma Ang II levels in 2K-1C rats treated with nobiletin at a dose of 30 mg/kg or losartan compared with the levels in sham rats (P < 0.05), as shown in Fig. 3.
Figure 3.
Effects of nobiletin or losartan on serum angiotensin-converting enzyme activity (ACE; (a)) and plasma angiotensin II levels (Ang II, (b)) in 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C. 2K-1C two-kidney, one-clip.
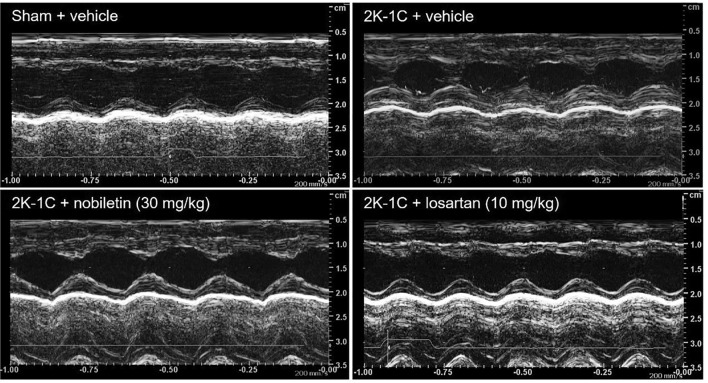
Effect of nobiletin or losartan on cardiac function
At 7 weeks after the 2K-1C operation, impairment of LV function was observed in the untreated 2K-1C group, represented by the elevations in IVSd, LVPWd, and ESV and reductions in %EF, SV, and %FS compared with the levels in the untreated sham group (P < 0.05; Table 3). Oral administration of nobiletin at a dose of 30 mg/kg or losartan for 4 weeks alleviated 2K-1C-induced LV dysfunction, supported by the recovery of ESV, EF, and FS compared with the levels in the untreated 2K-1C group (P < 0.05; Table 3). In addition, losartan treatment significantly reduced LVPWd compared with the value in the untreated 2K-1C group (P < 0.05; Table 3). Representative tracings of transthoracic echocardiographs in all groups of rats are shown in Fig. 4.
Table 3.
Effects of nobiletin or losartan on cardiac function in 2K-1C rats.
| Parameter | Sham | 2K-1C | ||
|---|---|---|---|---|
| Vehicle | Vehicle | Nobiletin 30 mg/kg |
Losartan 10 mg/kg |
|
| IVSd (mm) | 1.61 ± 0.04 | 2.00 ± 0.08a | 1.76 ± 0.09 | 1.64 ± 0.13b |
| IVSs (mm) | 2.56 ± 0.05 | 2.85 ± 0.15 | 2.90 ± 0.19 | 2.63 ± 0.14 |
| LVIDd (mm) | 8.29 ± 0.02 | 8.20 ± 0.23 | 8.04 ± 0.13 | 8.29 ± 0.13 |
| LVIDs (mm) | 4.65 ± 0.07 | 5.33 ± 0.17a | 4.39 ± 0.23b | 4.65 ± 0.14b |
| LVPWd (mm) | 1.73 ± 0.05 | 2.30 ± 0.02a | 2.08 ± 0.11 | 1.64 ± 0.14b |
| LVPWs (mm) | 2.66 ± 0.08 | 3.10 ± 0.23 | 2.98 ± 0.16 | 2.57 ± 0.25b |
| EDV (mL) | 1.26 ± 0.08 | 1.16 ± 0.09 | 1.13 ± 0.05 | 1.23 ± 0.07 |
| ESV (mL) | 0.25 ± 0.02 | 0.36 ± 0.04a | 0.22 ± 0.03b | 0.25 ± 0.02b |
| EF (%) | 79.73 ± 0.73 | 69.28 ± 0.97a | 80.82 ± 1.97b | 79.78 ± 0.81b |
| SV (mL) | 1.00 ± 0.06 | 0.805 ± 0.05a | 0.91 ± 0.03 | 0.99 ± 0.03b |
| FS (%) | 43.75 ± 0.85 | 34.65 ± 0.58a | 45.24 ± 2.35b | 42.65 ± 0.68b |
The data are expressed as the means ± SEMs.
IVSd interventricular septum thickness at diastole, IVSs interventricular septum thickness at systole, LVIDd left ventricular internal dimension at end-diastole, LVIDs left ventricular internal dimension at end-systole, LVPWd left ventricular posterior wall thickness at diastole, LVPWs left ventricular posterior wall thickness at systole, EDV end-diastolic volume, ESV end-systolic volume, SV stroke volume, EF ejection fraction, FS fractional shortening, 2K-1C two-kidney, one-clip.
aP < 0.05 vs. sham.
bP < 0.05 vs. 2K-1C.
Figure 4.
Representative tracings of transthoracic echocardiographs in 2K-1C rats. 2K-1C two-kidney, one clip.
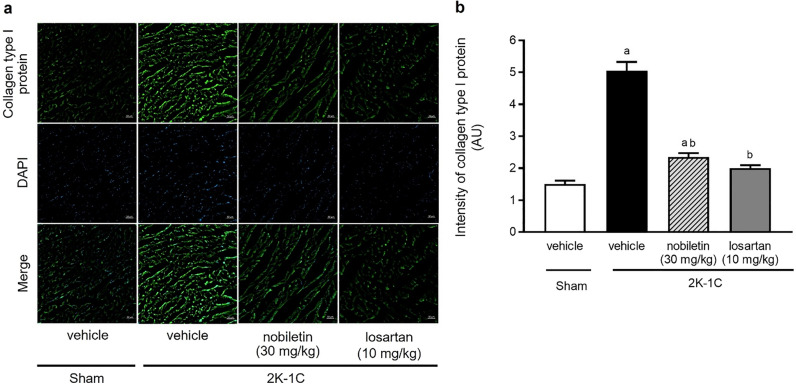
Effect of nobiletin or losartan on collagen type I protein expression in cardiac tissue
The immunofluorescence images of collagen type I protein expression in the LV are shown in Fig. 5a. The fluorescence signals of collagen type I in the LV were significantly intensified in untreated 2K-1C rats compared with untreated sham rats (P < 0.05). However, treatment with nobiletin at a dose of 30 mg/kg or losartan for 4 weeks attenuated the overexpression of collagen type I in the LV observed in the untreated 2K-1C rats. These results were supported by the quantitative data for collagen type I protein, as shown in Fig. 5b. The intensity of collagen type I protein staining in the untreated 2K-1C group was significantly lower than that in the untreated sham group (P < 0.05).
Figure 5.
Representative images of the immunofluorescence of collagen type I (a) in left ventricular tissue (magnification is × 10, scale bar = 50 µm). Quantitative data for collagen type I (b) in cardiac tissue in 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C. 2K-1C two-kidney, one-clip.
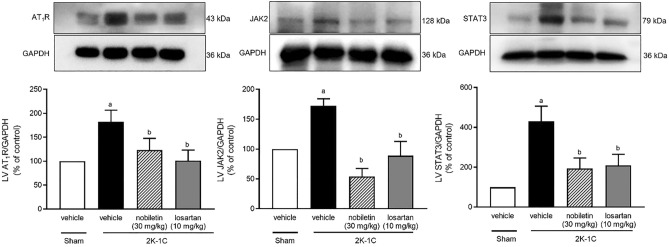
Effects of nobiletin and losartan on AT1R, JAK2, and STAT3 protein expression in cardiac tissue
The protein expression levels of AT1R, JAK2, and STAT3 in cardiac tissue were higher in the untreated 2K-1C group than in the sham-operated group (P < 0.05). However, nobiletin or losartan significantly reduced the upregulation of AT1R, JAK2, and STAT3 expression in 2K-1C rats (P < 0.05), as shown in Fig. 6.
Figure 6.
Effects of nobiletin or losartan on AT1R (n = 6) (a), JAK2 (n = 3) (b), and STAT3 (n = 6) (c) protein expression in cardiac tissue in 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C. 2K-1C two-kidney, one-clip. The blots were cut prior to hybridisation with antibodies during blotting, uncropped blots are included in Supplementary Information.
Effects of nobiletin and losartan on kidney function
The 2K-1C operation induced kidney damage, as supported by the greater proteinuria and albuminuria in renovascular hypertensive rats than in control rats (P < 0.05, Table 4). In addition, the levels of serum creatinine were significantly higher, while urine creatinine and the eGFR were significantly lower, in 2K-1C rats than in sham-operated rats (P < 0.05; Table 4). The albumin/creatinine ratio was higher in hypertensive rats than in control rats. Oral administration of nobiletin or losartan ameliorated kidney damage by reducing albuminuria in 2K-1C rats compared with untreated 2K-1C rats (P < 0.05; Table 4). In addition, nobiletin and losartan significantly improved the eGFR and albumin/creatinine ratio in 2K-1C rats (P < 0.05; Table 4).
Table 4.
Effects of nobiletin or losartan on kidney function in 2K-1C rats.
| Parameter | Sham | 2K-1C | ||
|---|---|---|---|---|
| Vehicle | Vehicle | Nobiletin 30 mg/kg |
Losartan 10 mg/kg |
|
| Urine creatinine (mg/dL) | 137.42 ± 15.82 | 67.02 ± 17.26a | 116.68 ± 15.67 | 116.88 ± 12.81 |
| Urine flow (mL/min) | 0.02 ± 0.003 | 0.015 ± 0.002 | 0.01 ± 0.001 | 0.02 ± 0.004 |
| Serum creatinine (mg/dL) | 0.97 ± 0.11 | 1.38 ± 0.09a | 0.81 ± 0.48b | 0.81 ± 0.08b |
| eGFR (mL/min) | 2.95 ± 0.32 | 0.91 ± 0.35a | 1.82 ± 0.34b | 2.47 ± 0.33b |
| Albuminuria (mg/dL) | 18.81 ± 3.5 | 187.59 ± 11.82a | 117.61 ± 2.08a,b | 86.06 ± 9.33a,b |
| Albumin/creatinine ratio | 0.14 ± 0.03 | 4.58 ± 1.48a | 1.26 ± 0.17b | 0.88 ± 0.09b |
The data are expressed as the means ± SEMs.
2K-1C two-kidney, one-clip, eGFR estimated glomerular filtration rate.
aP < 0.05 vs. sham.
bP < 0.05 vs. 2K-1C.
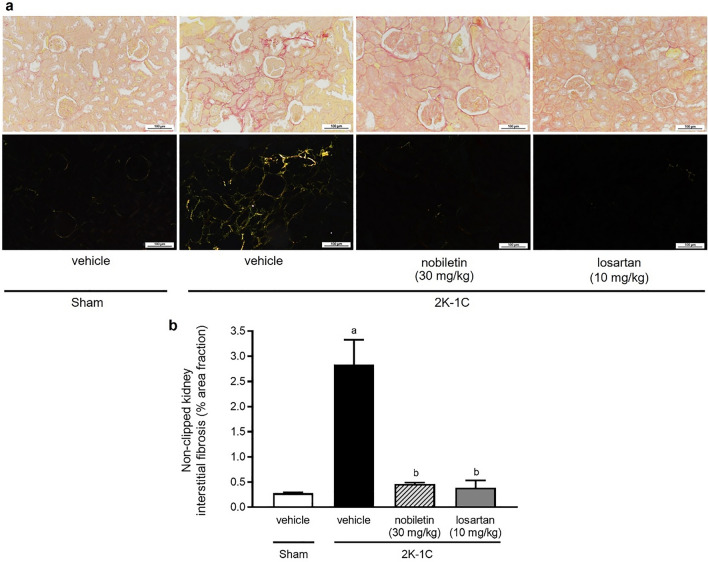
Effects of nobiletin and losartan on kidney morphology
The interstitial fibrosis accumulation of nonclipped kidneys in the untreated 2K-1C group was more intense than that in the other groups (Fig. 7a), accompanied by an increase in the % area fraction of interstitial fibrosis (P < 0.05; Fig. 7b). However, nobiletin or losartan treatment ameliorated the fibrotic changes of the kidney observed in the untreated 2K-1C group (P < 0.05).
Figure 7.
Effects of nobiletin or losartan on renal fibrosis in 2K-1C rats. Representative images of nonclipped kidney sections (a) stained with picrosirius red. All pictures were imaged under a light microscope (upper panel) and a polarized light microscope (lower panel) (magnification is × 20, scale bar = 100 µm). Quantitative data for the level of fibrosis (b) in nonclipped kidney tissue in 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C, 2K-1C two-kidney, one-clip.
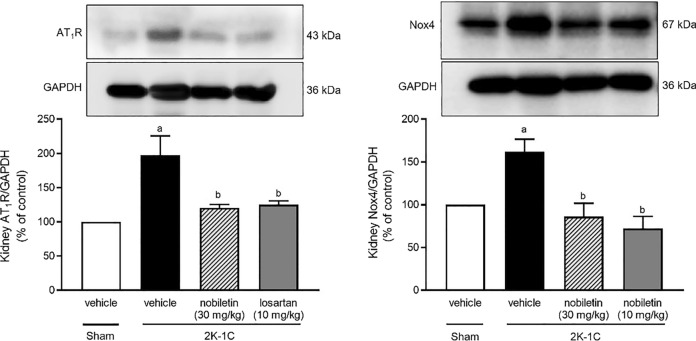
Effects of nobiletin and losartan on kidney AT1R and Nox4 protein expression
Significant increases in AT1R and Nox4 protein expression in kidney tissue were observed in the untreated 2K-1C group compared with the untreated sham group (P < 0.05). However, nobiletin at a dose of 30 mg/kg or losartan significantly reduced the kidney protein expression of AT1R and Nox4 compared with that in untreated 2K-1C rats (P < 0.05), as shown in Fig. 8.
Figure 8.
Effects of nobiletin or losartan on AT1R (n = 4) (a) and Nox4 (n = 5) (b) protein expression in nonclipped kidney tissue in 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C. 2K-1C two-kidney, one-clip. The blots were cut prior to hybridisation with antibodies during blotting, uncropped blots are included in Supplementary Information.
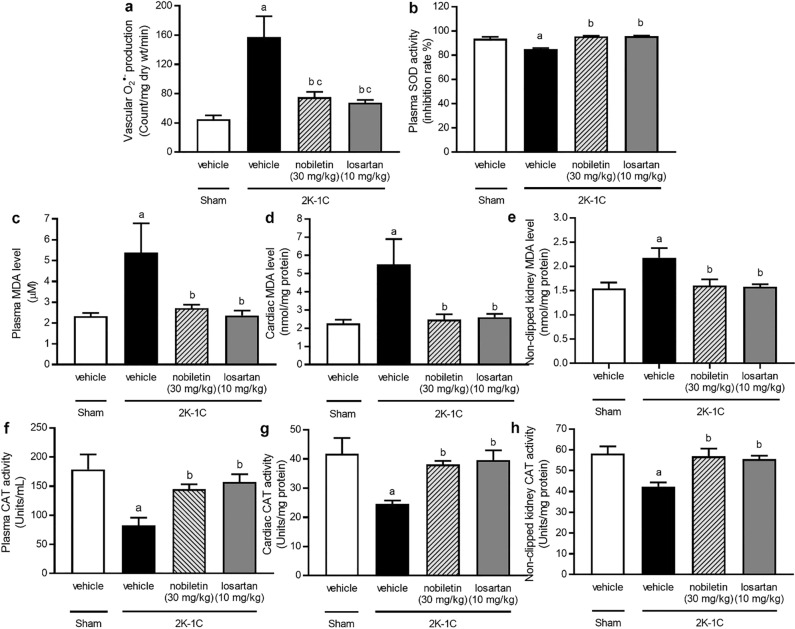
Effects of nobiletin and losartan on oxidative stress markers and endogenous antioxidant enzymes
At 7 weeks after the 2K-1C operation, elevated vascular O2·− production and increased MDA levels in plasma, cardiac tissue, and nonclipped kidney tissue were observed in the untreated 2K-1C group compared with the sham-operated group (P < 0.05). In addition, significant reductions in plasma CAT and SOD, cardiac CAT, and nonclipped kidney CAT activity were observed in the untreated 2K-1C group compared with the untreated sham group (P < 0.05). Nobiletin and losartan treatments, however, improved oxidative status by reducing oxidative stress marker levels and increasing endogenous antioxidant enzyme activity in 2K-1C rats (P < 0.05), as shown in Fig. 9.
Figure 9.
Effects of nobiletin or losartan on vascular O2·− production (a), plasma superoxide dismutase (SOD) activity (b), plasma malondialdehyde (MDA) levels (c), cardiac MDA levels (d), nonclipped kidney MDA levels (e), plasma catalase (CAT) activity (f), cardiac CAT activity (g), and nonclipped kidney CAT activity (h) in 2K-1C rats. The data are expressed as the means ± SEMs. aP < 0.05 vs. sham, bP < 0.05 vs. 2K-1C. 2K-1C two-kidney, one-clip.
Discussion
We found that nobiletin alleviated haemodynamic changes and normalized heart and kidney weights in 2K-1C hypertensive rats. High levels of serum ACE activity and plasma Ang II were reduced in 2K-1C rats treated with nobiletin. Impairment of cardiac function, as indicated by reductions in %EF and %FS, was observed in the hypertensive group, but this impairment was ameliorated by nobiletin treatment. Nobiletin also mitigated LV hypertrophy and fibrosis in 2K-1C hypertensive rats. These effects were relevant to suppression of the upregulation of AT1R/JAK2/STAT3 protein expression in cardiac tissue after treatment with nobiletin. The induction of kidney injury by left renal artery occlusion was supported by a reduction in the eGFR, an increase in albuminuria and accumulation of interstitial fibrosis in nonclipped kidney tissue. This kidney dysfunction and fibrosis in 2K-1C rats were ameliorated after nobiletin treatment. The protein expression of AT1R/Nox4 was upregulated in nonclipped kidney tissue, while in 2K-1C rats treated with nobiletin did not find the upregulation of these protein. The antioxidant effects of nobiletin were observed in 2K-1C rats since it reduced systemic and organ oxidative stress by reducing plasma and tissue MDA and O2·− generation as well as recovering CAT and SOD activities. Losartan was a positive control in this experiment, and it exerted biological activity similar to that of nobiletin.
Nobiletin can attenuate haemodynamic alterations in renovascular hypertensive rats. The results demonstrated that nobiletin at a dose of 30 mg/kg was an effective dose. The 2K-1C procedure establishes what is known as RAS activation-induced high blood pressure. Several studies have reported activation of the RAS after unilateral occlusion of the renal artery in rats and mice29–31. The antihypertensive effect of nobiletin in the present study was related to a reduction in ACE activity and subsequent reductions in circulating Ang II levels. This study might be the first to report the inhibitory effects of nobiletin on ACE activity in 2K-1C hypertensive rats. The findings are consistent with many studies showing that other citrus flavonoids, such as hesperidin, diosmetin and naringenin, inhibit ACE activity32–34. Nobiletin also showed antioxidant effects in this animal model since it reduced systemic lipid peroxidation and restored endogenous antioxidant enzyme activity levels. These results are supported by several studies showing that nobiletin exhibits antioxidant properties both in vitro and in vivo28,35. There is strong evidence to confirm that oxidative stress is required to sustain high blood pressure in the rat model of 2K-1C36. Therefore, the antioxidant properties of nobiletin might have partially mediated the antihypertensive effect of nobiletin in 2K-1C rats in the present study. After 7 weeks of chronic RAS activation, the BW in 2K-1C rats was reduced comparing to sham group. The effect of a 2K-1C procedure on BW was controversy. It was not different from control rats11,37 while some studies showed reduction of BW in 2K-1C rats38–40. The reduction of BW in 2K-1C rats in the present study was consistent with previous study38–40. It is well known that BW is influenced by food intake and energy expenditure. We observed that food intake was not different among group. It is possible that increased energy expenditure might cause BW loss in 2K-1C rats in the present study. This was supported by the study that Ang II promotes the sympathetic outflow to increase energy expenditure and contribute to weigh loss in rats41. Nobiletin normalized rat BW might be related with suppression of RAS activation in 2K-1C rats.
Impairment of LV function and reductions in %EF and %FS were present in rats with high blood pressure induced by the 2K-1C operation in the present study. This LV dysfunction might have been caused by LV morphological changes that were indicated by LV remodelling in the hypertensive rats. LV hypertrophy was indicated by the elevations in HW/BW, VW/BW, LVW/BW, IVSd, and LVPWd, whereas LV fibrosis was also indicated by the increased intensity of LV collagen type I protein expression. However, nobiletin treatment alleviated LV abnormalities in 2K-1C hypertensive rats. This finding is consistent with a previous review showing that LV hypertrophy and fibrosis are commonly found in pathologic hearts, contributing to LV dysfunction42,43. Cardiac hypertrophy is mainly caused by an adaptive response to chronic high-pressure load to preserve cardiac output44. Additionally, the nonhemodynamic factor Ang II might participate in the development of LV remodelling7. Therefore, nobiletin may have improved cardiac function in this study through mechanisms related to its antihypertensive and ACE-inhibitory effects. The consequence of the reduction in RAS activation affected the Ang II/AT1R/JAK2/STAT3 signalling pathway. This study found that overexpression of AT1R/JAK2/STAT3 in 2K-1C rats mediates the cardiac remodelling process. There is evidence to show the association between AT1R/STAT3 and cardiac hypertrophy progression45. Additionally, many studies have provided evidence that Ang II is a growth factor that mediates the cardiac remodelling process via activation of AT1R, JAK2 and STAT3 in cardiac tissue17,46,47. It is possible that the molecular mechanisms of the beneficial effects of nobiletin on LV remodelling and function in the present study were associated with suppression of the AT1R/JAK2/STAT3 signalling pathway in 2K-1C rats.
It is well documented that 2K-1C rats have kidney injury, as indicated by accumulation of kidney interstitial fibrosis in nonclipped kidneys and increases in albuminuria and the albumin-to-creatinine ratio. An elevation in KW/BW on the nonclipped side was observed in 2K-1C rats, suggesting kidney hypertrophy. In addition, kidney function was impaired in 2K-1C rats, as indicated by the high levels of serum creatinine and the low eGFR values in these rats. The induction of kidney injury by renal artery occlusion has been supported by numerous studies48,49. Lee et al. reported that 2K-1C-induced ACE/Ang II/AT1R overactivation causes kidney interstitial fibrosis and impairs kidney function, as indicated by high concentrations of serum creatinine, albuminuria, and albumin/creatinine ratio levels11,50. Our results showed that nobiletin alleviated 2K-1C-induced kidney abnormalities. This effect was associated with suppression of RAS activation and kidney oxidative stress. Furthermore, the finding suggested that oxidative stress in kidney tissue might have been the consequence of Ang II action on its receptor, AT1R. We found upregulation of AT1R and Nox4 protein expression in nonclipped kidneys. There is increasing evidence to support the idea that Nox subunit 4, or Nox4, is located in kidney tissue and contributes to oxidative stress and the pathology of kidney injury15,51,52. We found that 2K-1C rats that received nobiletin had recovered AT1R and Nox4 protein expression in nonclipped kidneys. Nobiletin has been reported to suppress Nox2 or gp91phox to alleviate cardiac hypertrophy53.
Losartan is an angiotensin II receptor blocker that is widely recommended for hypertension treatment54. It was used as a positive control agent in this study. It was found that losartan reduced blood pressure and attenuated cardiorenal alterations in 2K-1C rats. Losartan also had inhibitory effects on RAS activation and oxidative stress in 2K-1C rats. Angiotensin II receptor blockers can prevent and alleviate organ damage55,56. The mechanisms of action of losartan on cardiorenal tissue in this study were related to blockade of RAS and subsequent suppression of the AT1R/JAK/STAT signalling pathway as well as the AT1R/Nox4 cascade. It has been reported that losartan also acts as an antioxidant and anti-inflammatory agent57. In an animal model of NO depletion-induced hypertension, losartan reduced blood pressure and cardiorenal damage by reducing oxidative stress58.
In summary, nobiletin showed beneficial effects on cardiorenal abnormalities induced by the 2K-1C procedure, similar to the losartan used in the experiment. It ameliorated LV dysfunction and remodelling by reducing oxidative stress as well as by suppressing the Ang II/AT1R/JAK/STAT signalling pathway in cardiac tissue. Furthermore, the RAS-inhibitory and antioxidant properties of nobiletin resolved renal injury in a manner related to the AT1R/Nox4 pathway in renovascular hypertensive rats.
Materials and methodology
Drugs and animals
Nobiletin was obtained from INDOFINE Chemical Company, Inc. (NJ, USA). Losartan (Cozaar 50 mg) was obtained from MSD. Merck & Co., Inc., (NJ, USA).
This study used male Sprague–Dawley rats (5–6 weeks of age weighing 160–180 g) that were provided by Nomura Siam International Co., Ltd., Bangkok, Thailand. The rats were raised in an HVAC (heating, ventilation and air-conditioning)-equipped room (23 ± 2 °C) with a 12 h dark–light cycle at the Northeast Laboratory Animal Center. All animal procedures complied with the standards for the care and use of experimental animals and were approved by the Animal Ethics Committee of Khon Kaen University, Khon Kaen, Thailand (IACUC-KKU-73/63). This study is reported in accordance with Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines.
Induction of 2K-1C hypertension and experimental protocols
After a week of acclimatization, hypertension was induced in the rats by reducing renal blood flow. The 2K-1C procedure was performed under anaesthesia with intraperitoneal injection of xylazine (5 mg/kg) followed by zoletil (25 mg/kg). A silver clip (0.2 mm i.d.) was carefully verified and placed on the left renal artery. Sham-operated rats were also used. Three weeks after the operation, the rats that had a systolic blood pressure (SP) > 160 mmHg were included as 2K-1C hypertensive rats29. There were six experimental groups (n = 8/each group) as follows:
One sham group was given vehicle (propylene glycol, 1.5 mL/kg).
Another sham group was given 30 mg/kg nobiletin.
A 2K-1C group was given vehicle (propylene glycol, 1.5 mL/kg).
A 2K-1C group was given 15 mg/kg nobiletin.
A 2K-1C group was given 30 mg/kg nobiletin.
A 2K-1C group was given losartan (10 mg/kg).
Nobiletin, losartan and propylene glycol were intragastrically administered daily by using a gavage feeding tube for 4 weeks during the experimental period. Rats that treated nobiletin and losartan received propylene glycol, 1.5 mL/kg.
Assessment of systolic blood pressure during 7 weeks of experiments
SP was detected once a week without anaesthesia using noninvasive tail cuff plethysmography (IITC/Life Science Instrument Model 229 and Model 179 amplifier: Woodland Hills, CA, USA). Conscious rats were placed on a restrainer and allowed to acclimate prior to blood pressure measurement. The measurement was repeated 3 times, and the results are expressed as the mean values from each rat.
Cardiac function and intraarterial blood pressure measurement
On the last day of experiment, all rats were anaesthetized with thiopental sodium (60 mg/kg, i.p.). Their chests were shaved and cleaned and they were placed on one side on a specially designed apparatus. LV function was assessed by echocardiogram using a GE Logiq S7 Ultrasound Machine (GE Healthcare, WI, USA). anaesthetized The LV function and structure were measured from the two-dimensional short-axis view, and M-mode tracings were recorded for the LV internal dimension at end-diastole (LVIDd), LV internal dimension at end-systole (LVIDs), interventricular septum thickness at diastole (IVSd), interventricular septum thickness at systole (IVSs), LV posterior wall thickness at diastole (LVPWd), LV posterior wall thickness at systole (LVPWs), end diastolic volume (EDV), end systolic volume (ESV), and stroke volume (SV) from three consecutive cardiac cycles. The LV fractional shortening (% FS) was calculated with the following equation: % LVFS = [(LVIDd − LVIDs)/LVIDd] × 100.
After echocardiogram, their femoral arteries were cannulated using polyethylene tubes. Baseline values of SP, diastolic blood pressure (DP), mean arterial pressure (MAP), and heart rate (HR) were continuously monitored for 30 min through a pressure transducer and recorded using Acknowledge Data Acquisition software (Biopac Systems Inc., Santa Barbara, CA, USA). After hemodynamic assessment, the animals were sacrificed by exsanguinations, collecting blood samples from abdominal aorta. The blood samples were collected in ethylenediaminetetraacetic acid tubes to prepare plasma and normal test tube to prepare serum. Tissue samples including heart and kidney were collected by dissection. All tissues were washed with saline solution and weighed. Data were expressed as a relation between regional tissue weights (g)/100 g BW.
Angiotensin-converting enzyme activity and angiotensin II measurements
Serum ACE activity was evaluated using a fluorescence assay, as previously described, with some modifications3. The serum of each rat was mixed with hippuryl-l-histidyl-l-leucine (HHL) in assay buffer and then incubated at 37 °C for 30 min. After that, NaOH was added to stop the reaction, and the product of the reaction was fluorogenically labelled with O-phthaldialdehyde (OPA). The fluorescence was read at an excitation wavelength of 355 nm and an emission wavelength of 535 nm using a fluorescent plate reader.
Ang II levels were detected in plasma following the standard procedure recommendations of an Angiotensin II EIA Kit (RAB0010; Sigma–Aldrich, Merck KGaA, Darmstadt, Germany).
Kidney function and albuminuria measurements
All rats were housed in metabolic cages for 24 h (Pestel et al.) for blood and urine collection. After urine collection, blood samples were obtained from the lateral tail veins. Serum and urine creatinine levels were evaluated using a creatinine assay kit (ab65340; Abcam Plc, Cambridge, U.K.). The estimated glomerular filtration rate (eGFR) was obtained from creatinine clearance measurement in ml/min as follows: eGFR = (Ucr × V)/Pcr, Ucr = creatinine concentration in urine (mg/dL), V = urine flow rate (mL/min), and Pcr = creatinine concentration in plasma or serum (mg/dL)59.
The albuminuria levels were evaluated using a rat albumin ELISA Kit (ab108789; Abcam Plc, Cambridge, U.K.). The albuminuria results are expressed in ng/mL. Thereafter, urine creatinine and urine albumin levels were calculated as the urinary albumin-to-creatinine ratio to indicate the level of kidney damage.
Picrosirius red staining in kidney tissue
To investigate the level of renal interstitial fibrosis, nonclipped kidneys were fixed with 4% paraformaldehyde for 24 h. Thereafter, the renal tissues were routinely processed, embedded in paraffin, and sectioned at 2 µm. Renal interstitial fibrosis was evaluated by picrosirius red staining. Images were captured using an Eclipse Ci-POL polarised light microscope (Nikon Tokyo, Japan). The level of kidney interstitial fibrosis was analysed using ImageJ morphometric software (NIH), and the result is expressed as a percentage of the area fraction60.
Immunofluorescence in cardiac tissue
Heart tissues were fixed in 4% paraformaldehyde for 48 h at 4 °C. Thereafter, the tissues were transferred to 30% sucrose in phosphate-buffered saline (PBS) at 4 °C overnight. The heart tissues were embedded in embedding medium for frozen tissue specimens (4583, Sakura Finetek USA, Inc., Torrance, CA, USA) and cut into 10 µm thick sections at − 25 °C by using a Cryostat Microm HM 525 instrument (Thermo Fisher Scientific, Walldorf, Germany).
After that, the tissue sections were processed as previously described61. Briefly, the slides were processed and incubated with the primary antibody anti-collagen type I (ab34710, Abcam, Plc, Cambridge, U.K., dilution 1:200) at 4 °C overnight. After primary antibody incubation, Alexa Fluor® 488 (ab150077, Abcam, Plc, Cambridge, U.K., dilution 1:1000) was used as the secondary antibody in a 2 h incubation at 37 °C, and the nuclei were stained using DAPI (D9542, Sigma–Aldrich, USA, dilution 1:1000) for 10 min at 37 °C. Thereafter, the slides were mounted, and fluorescence was visualized with a laser scanning confocal microscope (Carl Zeiss, Germany) with an appropriate filter. Confocal imaging was detected by a 10× objective lens and acquired with 1024 × 1024 pixels. The fluorescence intensity values of collagen type I and DAPI (average fluorescence intensity per pixel) were analysed by Zeiss Zen Blue analysis wizard software.
Western blot analysis of AT1R, Nox4, JAK2, and STAT3 protein expression
The levels of AT1R and Nox4 protein expression in nonclipped kidney tissue and AT1R, JAK2, and STAT3 protein expression in cardiac tissue were evaluated by using the Western blot method. The tissue samples were electrophoresed through a sodium dodecyl sulfate polyacrylamide gel and transferred onto a polyvinylidenedifluoride (PVDF) membrane. Membranes were cut prior to hybridisation with antibodies during blotting. A mouse monoclonal antibody against AT1R (G-3) (SC-515884, dilution 1:1000), mouse monoclonal IgG2b antibody against JAK2 (C-10) (SC-390539, dilution 1:1000) (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA), mouse monoclonal IgG2a antibody against STAT3 (124H6, dilution 1:800) (Cell Signaling Technology, Inc., Danvers, USA), rabbit monoclonal antibody against NADPH oxidase 4 (ab133303, dilution 1:1000), and mouse monoclonal antibody against GAPDH (ab133303, dilution 1:4000) (Abcam, Plc, Cambridge, UK) were used. GAPDH was used as a protein loading control to compare the intensities of protein expression. Densitometric analysis was performed using an ImageQuantTM 4000 imager (GE Healthcare Life Science, Piscataway, NJ, USA). The data are expressed as a percentage of the target protein (actin) expression level compared to that in the control groups.
Measurements of oxidative stress markers
O2·− production was detected in carotid arteries using lucigenin-enhanced chemiluminescence based on a technique described previously62. MDA production in plasma, nonclipped kidney tissue, and LV tissue was measured with a thiobarbituric acid-reactive substances (TBARS) assay using a spectrophotometric method as previously described63.
For detection of endogenous antioxidant enzymes and CAT enzyme activity in plasma, nonclipped kidney tissue, and LV tissue, the protocol followed previous reports64,65. In addition, plasma SOD activity was measured by colorimetric analysis using a spectrophotometer with corresponding detection kits (Sigma–Aldrich, Merck KGaA, Darmstadt, Germany) according to the manufacturer’s protocols.
Statistical analysis
The results are shown as the mean ± the standard error of the mean (SEM). One-way analysis of variance (ANOVA) followed by Tukey’s test was used to analyse the differences among groups. The data were considered to show a statistically significant difference when the p value was less than 0.05.
Supplementary Information
Acknowledgements
This project is funded by National Research Council of Thailand (NRCT) (N42A650239), The Research Fund for Supporting Lecturer to Admit High Potential Student to Study and Research on His Expert Program Year 2020 (631JH217) from the Graduate School; and the Invitation Research Fund (IN65119), Faculty of Medicine, Khon Kaen University, Thailand.
Author contributions
P.P. conceived and designed the experiments and wrote the manuscript. M.I., A.P., Pr.P., S.R., P.M., Pa.P., and W.I. performed the experiments. P.P. and M.I. analysed the data and wrote the paper together. All authors reviewed and approved the final version of manuscript.
Funding
The funding was also provided by Talented Mid-Career Researchers; the National Research Council of Thailand (N42A650239), graduate School (631JH217), Invitation Research Fund (IN65119).
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-13513-6.
References
- 1.Wiesel P, Mazzolai L, Nussberger J, Pedrazzini T. Two-kidney, one clip and one-kidney, one clip hypertension in mice. Hypertension (Dallas) 1997;29:1025–1030. doi: 10.1161/01.hyp.29.4.1025. [DOI] [PubMed] [Google Scholar]
- 2.Miksche LW, Miksche U, Gross F. Effect of sodium restriction on renal hypertension and on renin activity in the rat. Circ. Res. 1970;27:973–984. doi: 10.1161/01.res.27.6.973. [DOI] [PubMed] [Google Scholar]
- 3.Maneesai P, et al. Effect of asiatic acid on the Ang II-AT1R-NADPH oxidase-NF-kappaB pathway in renovascular hypertensive rats. Naunyn Schmiedebergs Arch. Pharmacol. 2017;390:1073–1083. doi: 10.1007/s00210-017-1408-x. [DOI] [PubMed] [Google Scholar]
- 4.Yu TT, et al. Effects of traditional Chinese medicine Xin-Ji-Er-Kang formula on 2K1C hypertensive rats: Role of oxidative stress and endothelial dysfunction. BMC Complement. Altern. Med. 2013;13:173. doi: 10.1186/1472-6882-13-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gudbrandsen OA, et al. Prevention of hypertension and organ damage in 2-kidney, 1-clip rats by tetradecylthioacetic acid. Hypertension (Dallas) 2006;48:460–466. doi: 10.1161/01.hyp.0000233018.60736.70. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, Niu M, Yin S, Zhang F, Shi R. Nephroprotective effects of nebivolol in 2K1C rats through regulation of the kidney ROS-ADMA-NO pathway. Pharmacol. Rep. 2018;70:917–929. doi: 10.1016/j.pharep.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Paul M, Poyan Mehr A, Kreutz R. Physiology of local renin-angiotensin systems. Physiol. Rev. 2006;86:747–803. doi: 10.1152/physrev.00036.2005. [DOI] [PubMed] [Google Scholar]
- 8.Sawant SH, Bodhankar SL. Flax lignan concentrate attenuate hypertension and abnormal left ventricular contractility via modulation of endogenous biomarkers in two-kidney-one-clip (2K1C) hypertensive rats. Rev. Bras. Farmacogn. 2016;26:601–610. doi: 10.1016/j.bjp.2016.05.005. [DOI] [Google Scholar]
- 9.Liu S-Y, et al. Hydrogen sulfide improves myocardial remodeling via downregulated angiotensin II/AT1R pathway in renovascular hypertensive rats. Am. J. Hypertens. 2016;30:67–74. doi: 10.1093/ajh/hpw104. [DOI] [PubMed] [Google Scholar]
- 10.Zhang JQ, Sun HL, Ma YX, Wang DW. Effects of RNA interference targeting angiotensin 1a receptor on the blood pressure and cardiac hypertrophy of rats with 2K1C hypertension. Zhonghua Yi Xue Za Zhi. 2006;86:1138–1143. [PubMed] [Google Scholar]
- 11.Alam MA, Chowdhury MRH, Jain P, Sagor MAT, Reza HM. DPP-4 inhibitor sitagliptin prevents inflammation and oxidative stress of heart and kidney in two kidney and one clip (2K1C) rats. Diabetol. Metab. Syndr. 2015;7:107. doi: 10.1186/s13098-015-0095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW. Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circ. Res. 1994;74:1141–1148. doi: 10.1161/01.res.74.6.1141. [DOI] [PubMed] [Google Scholar]
- 13.Toklu HZ, et al. Resveratrol improves cardiovascular function and reduces oxidative organ damage in the renal, cardiovascular and cerebral tissues of two-kidney, one-clip hypertensive rats. J. Pharm. Pharmacol. 2010;62:1784–1793. doi: 10.1111/j.2042-7158.2010.01197.x. [DOI] [PubMed] [Google Scholar]
- 14.Maneesai P, et al. Effect of asiatic acid on the Ang II-AT(1)R-NADPH oxidase-NF-κB pathway in renovascular hypertensive rats. Naunyn-Schmiedeberg's Arch. Pharmacol. 2017;390:1073–1083. doi: 10.1007/s00210-017-1408-x. [DOI] [PubMed] [Google Scholar]
- 15.Saengnak B, et al. Clitoria ternatea L. extract prevents kidney damage by suppressing the Ang II/Nox4/oxidative stress cascade in l-NAME-induced hypertension model of rats. Ann. Anat. 2021;238:151783. doi: 10.1016/j.aanat.2021.151783. [DOI] [PubMed] [Google Scholar]
- 16.McWhinney CD, Hunt RA, Conrad KM, Dostal DE, Baker KM. The type I angiotensin II receptor couples to Stat1 and Stat3 activation through Jak2 kinase in neonatal rat cardiac myocytes. J. Mol. Cell. Cardiol. 1997;29:2513–2524. doi: 10.1006/jmcc.1997.0489. [DOI] [PubMed] [Google Scholar]
- 17.Dostal DE, et al. Molecular mechanisms of angiotensin II in modulating cardiac function: Intracardiac effects and signal transduction pathways. J. Mol. Cell. Cardiol. 1997;29:2893–2902. doi: 10.1006/jmcc.1997.0524. [DOI] [PubMed] [Google Scholar]
- 18.Kishore R, Verma SK. Roles of STATs signaling in cardiovascular diseases. Jak-Stat. 2012;1:118–124. doi: 10.4161/jkst.20115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye S, et al. Celastrol attenuates angiotensin II-induced cardiac remodeling by targeting STAT3. Circ. Res. 2020;126:1007–1023. doi: 10.1161/circresaha.119.315861. [DOI] [PubMed] [Google Scholar]
- 20.Yoshigai E, et al. Citrus nobiletin suppresses inducible nitric oxide synthase gene expression in interleukin-1β-treated hepatocytes. Biochem. Biophys. Res. Commun. 2013;439:54–59. doi: 10.1016/j.bbrc.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 21.Noguchi S, Atsumi H, Iwao Y, Kan T, Itai S. Nobiletin: A citrus flavonoid displaying potent physiological activity. Acta Crystallogr. Sect. C Struct. Chem. 2016;72:124–127. doi: 10.1107/s2053229616000577. [DOI] [PubMed] [Google Scholar]
- 22.Singh SP, Wahajuddin TD, Patel K, Jain GK. Permeability determination and pharmacokinetic study of nobiletin in rat plasma and brain by validated high-performance liquid chromatography method. Fitoterapia. 2011;82:1206–1214. doi: 10.1016/j.fitote.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Alok PS, Jai BK, Rajeev KS, Havagiray C. Nobiletin a biologically active phytoconstituent: Systematic review. J. Biol. Active Prod. Nat. 2021;11:204–211. doi: 10.1080/22311866.2021.1920461. [DOI] [Google Scholar]
- 24.Liu J, et al. Nobiletin inhibits breast cancer via p38 mitogen-activated protein kinase, nuclear transcription factor-κB, and nuclear factor erythroid 2-related factor 2 pathways in MCF-7 cells. Food Nutr. Res. 2018 doi: 10.29219/fnr.v62.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salma M, et al. Nobiletin ameliorates cisplatin-induced acute kidney injury due to its anti-oxidant, anti-inflammatory and anti-apoptotic effects. Exp. Toxicol. Pathol. 2015;67:427–433. doi: 10.1016/j.etp.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 26.Xu M, Wang R, Fan H, Ni Z. Nobiletin ameliorates streptozotocin-cadmium-induced diabetic nephropathy via NF-κB signalling pathway in rats. Arch. Physiol. Biochem. 2021 doi: 10.1080/13813455.2021.1959617. [DOI] [PubMed] [Google Scholar]
- 27.Bunbupha S, Pakdeechote P, Maneesai P, Prasarttong P. Nobiletin alleviates high-fat diet-induced nonalcoholic fatty liver disease by modulating AdipoR1 and gp91(phox) expression in rats. J. Nutr. Biochem. 2021;87:108526. doi: 10.1016/j.jnutbio.2020.108526. [DOI] [PubMed] [Google Scholar]
- 28.Potue P, et al. Nobiletin alleviates vascular alterations through modulation of Nrf-2/HO-1 and MMP pathways in l-NAME induced hypertensive rats. Food Funct. 2019;10:1880–1892. doi: 10.1039/c8fo02408a. [DOI] [PubMed] [Google Scholar]
- 29.Chidambaram SB, et al. Venthamarai chooranam, a polyherbal Siddha medicine, alleviates hypertension via AT(1)R and eNOS signaling pathway in 2K1C hypertensive rats. Exp. Biol. Med. (Maywood). 2014 doi: 10.1177/1535370214525317. [DOI] [PubMed] [Google Scholar]
- 30.Weissheimer KV, Franci CR, Lucion AB, Sanvitto GL. The role of AT1 receptor-mediated reproductive function in renovascular hypertension in male rats. Horm. Behav. 2012;62:43–49. doi: 10.1016/j.yhbeh.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 31.Navar LG, et al. Unraveling the mystery of goldblatt hypertension. Physiology. 1998;13:170–176. doi: 10.1152/physiologyonline.1998.13.4.170. [DOI] [PubMed] [Google Scholar]
- 32.Kim DS, Lim SB. Semi-continuous subcritical water extraction of flavonoids from citrus unshiu peel: Their antioxidant and enzyme inhibitory activities. Antioxidants. 2020 doi: 10.3390/antiox9050360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wunpathe C, et al. Hesperidin suppresses renin-angiotensin system mediated NOX2 over-expression and sympathoexcitation in 2K–1C hypertensive rats. Am. J. Chin. Med. 2018;46:751–767. doi: 10.1142/s0192415x18500398. [DOI] [PubMed] [Google Scholar]
- 34.Meephat S, et al. Diosmetin attenuates metabolic syndrome and left ventricular alterations via the suppression of angiotensin II/AT1 receptor/gp(91phox)/p-NF-κB protein expression in high-fat diet fed rats. Food Funct. 2021;12:1469–1481. doi: 10.1039/d0fo02744h. [DOI] [PubMed] [Google Scholar]
- 35.Zhu C, et al. Variations of flavonoid composition and antioxidant properties among different cultivars, fruit tissues and developmental stages of citrus fruits. Chem. Biodivers. 2020;17:e1900690. doi: 10.1002/cbdv.201900690. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira-Sales EB, et al. Oxidative stress contributes to renovascular hypertension. Am. J. Hypertens. 2008;21:98–104. doi: 10.1038/ajh.2007.12. [DOI] [PubMed] [Google Scholar]
- 37.Wang Z, et al. Naringenin ameliorates renovascular hypertensive renal damage by normalizing the balance of renin-angiotensin system components in rats. Int. J. Med. Sci. 2019;16:644–653. doi: 10.7150/ijms.31075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pereira SC, et al. Quercetin decreases the activity of matrix metalloproteinase-2 and ameliorates vascular remodeling in renovascular hypertension. Atherosclerosis. 2018;270:146–153. doi: 10.1016/j.atherosclerosis.2018.01.031. [DOI] [PubMed] [Google Scholar]
- 39.Chelko SP, Schmiedt CW, Lewis TH, Lewis SJ, Robertson TP. A novel vascular clip design for the reliable induction of 2-kidney, 1-clip hypertension in the rat. J. Appl. Physiol. (Bethesda) 2012;112:362–366. doi: 10.1152/japplphysiol.01015.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rahman MM, et al. Polyphenolic compounds of amla prevent oxidative stress and fibrosis in the kidney and heart of 2K1C rats. Food Sci. Nutr. 2020;8:3578–3589. doi: 10.1002/fsn3.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Porter JP, Anderson JM, Robison RJ, Phillips AC. Effect of central angiotensin II on body weight gain in young rats. Brain Res. 2003;959:20–28. doi: 10.1016/S0006-8993(02)03676-4. [DOI] [PubMed] [Google Scholar]
- 42.Travers JG, Kamal FA, Robbins J, Yutzey KE, Blaxall BC. Cardiac fibrosis: The fibroblast awakens. Circ. Res. 2016;118:1021–1040. doi: 10.1161/circresaha.115.306565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vilhena JC, et al. Açaí reverses adverse cardiovascular remodeling in renovascular hypertension: A comparative effect with enalapril. J. Cardiovasc. Pharmacol. 2021;77:673–684. doi: 10.1097/fjc.0000000000001003. [DOI] [PubMed] [Google Scholar]
- 44.Simko F. Physiologic and pathologic myocardial hypertrophy–physiologic and pathologic regression of hypertrophy? Med. Hypotheses. 2002;58:11–14. doi: 10.1054/mehy.2001.1399. [DOI] [PubMed] [Google Scholar]
- 45.Yue H, Li W, Desnoyer R, Karnik SS. Role of nuclear unphosphorylated STAT3 in angiotensin II type 1 receptor-induced cardiac hypertrophy. Cardiovasc. Res. 2010;85:90–99. doi: 10.1093/cvr/cvp285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yue H, Li W, Desnoyer R, Karnik SS. Role of nuclear unphosphorylated STAT3 in angiotensin II type 1 receptor-induced cardiac hypertrophy. Cardiovasc. Res. 2009;85:90–99. doi: 10.1093/cvr/cvp285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen Y, et al. JAK-STAT signalling and the atrial fibrillation promoting fibrotic substrate. Cardiovasc. Res. 2017;113:310–320. doi: 10.1093/cvr/cvx004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim YG, et al. Sequential activation of the intrarenal renin-angiotensin system in the progression of hypertensive nephropathy in Goldblatt rats. Am. J. Physiol. Renal Physiol. 2016;311:F195–F206. doi: 10.1152/ajprenal.00001.2015. [DOI] [PubMed] [Google Scholar]
- 49.Hong MH, et al. Antihypertensive effects of Gynura divaricata (L.) DC in rats with renovascular hypertension. Nutrients. 2020;12:3321. doi: 10.3390/nu12113321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee SH, et al. Sex-related differences in the intratubular renin-angiotensin system in two-kidney, one-clip hypertensive rats. Am. J. Physiol. Renal Physiol. 2019;317:F670–F682. doi: 10.1152/ajprenal.00451.2018. [DOI] [PubMed] [Google Scholar]
- 51.Yang Q, et al. Nox4 in renal diseases: An update. Free Radic. Biol. Med. 2018;124:466. doi: 10.1016/j.freeradbiomed.2018.06.042. [DOI] [PubMed] [Google Scholar]
- 52.Poasakate A, et al. Genistein alleviates renin-angiotensin system mediated vascular and kidney alterations in renovascular hypertensive rats. Biomed. Pharmacother. 2022;146:112601. doi: 10.1016/j.biopha.2021.112601. [DOI] [PubMed] [Google Scholar]
- 53.Zhang N, et al. Nobiletin, a polymethoxy flavonoid, protects against cardiac hypertrophy induced by pressure-overload via inhibition of NAPDH oxidases and endoplasmic reticulum stress. Cell. Physiol. Biochem. 2017;42:1313–1325. doi: 10.1159/000478960. [DOI] [PubMed] [Google Scholar]
- 54.Barreras A, Gurk-Turner C. Angiotensin II receptor blockers. Baylor Univ. Med. Center. 2003;16:123–126. doi: 10.1080/08998280.2003.11927893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abdelkader NF, Abd El-Latif AM, Khattab MM. Telmisartan/17β-estradiol mitigated cognitive deficit in an ovariectomized rat model of Alzheimer's disease: Modulation of ACE1/ACE2 and AT1/AT2 ratio. Life Sci. 2020;245:117388. doi: 10.1016/j.lfs.2020.117388. [DOI] [PubMed] [Google Scholar]
- 56.Zornoff LA, Matsubara LS, Matsubara BB, Paiva SA, Spadaro J. Effects of losartan on ventricular remodeling in experimental infarction in rats. Arq. Bras. Cardiol. 2000;75:459–470. doi: 10.1590/s0066-782x2000001200001. [DOI] [PubMed] [Google Scholar]
- 57.Karanovic D, et al. Effects of single and combined losartan and tempol treatments on oxidative stress, kidney structure and function in spontaneously hypertensive rats with early course of proteinuric nephropathy. PLoS ONE. 2016;11:e0161706. doi: 10.1371/journal.pone.0161706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khattab M, Ahmad M, Al-Shabanah OA, Raza M. Effects of losartan on blood pressure, oxidative stress, and nitrate/nitrite levels in the nitric oxide deficient hypertensive rats. Recep. Channels. 2004;10:147–157. doi: 10.3109/10606820490936141. [DOI] [PubMed] [Google Scholar]
- 59.Probert JL, editor. Urology: An Atlas of Investigation and Diagnosis. Clinical Publishing Oxford; 2018. [Google Scholar]
- 60.Bunbupha S, Apaijit K, Maneesai P, Prasarttong P, Pakdeechote P. Nobiletin ameliorates high-fat diet-induced vascular and renal changes by reducing inflammation with modulating AdipoR1 and TGF-β1 expression in rats. Life Sci. 2020;260:118398. doi: 10.1016/j.lfs.2020.118398. [DOI] [PubMed] [Google Scholar]
- 61.Givvimani S, Narayanan N, Pushpakumar SB. Anti-parstatin promotes angiogenesis and ameliorates left ventricular dysfunction during pressure overload. Int. J. Biomed. Sci. 2014;10:1–7. [PMC free article] [PubMed] [Google Scholar]
- 62.Lu FJ, Lin JT, Wang HP, Huang WC. A simple, sensitive, non-stimulated photon counting system for detection of superoxide anion in whole blood. Experientia. 1996;52:141–144. doi: 10.1007/bf01923359. [DOI] [PubMed] [Google Scholar]
- 63.Bunbupha S, Pakdeechote P, Kukongviriyapan U, Prachaney P, Kukongviriyapan V. Asiatic acid reduces blood pressure by enhancing nitric oxide bioavailability with modulation of eNOS and p47phox expression in L-NAME-induced hypertensive rats. Phytother. Res. 2014;28:1506–1512. doi: 10.1002/ptr.5156. [DOI] [PubMed] [Google Scholar]
- 64.Ozmen B, et al. Lens superoxide dismutase and catalase activities in diabetic cataract. Clin. Biochem. 2002;35:69–72. doi: 10.1016/s0009-9120(01)00284-3. [DOI] [PubMed] [Google Scholar]
- 65.Góth L. A simple method for determination of serum catalase activity and revision of reference range. Int. J. Clin. Chem. 1991;196:143–151. doi: 10.1016/0009-8981(91)90067-m. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.