Abstract
Background:
COVID-19 has profoundly affected sleep, although little research has focused on high-risk populations for poor sleep health, including American Indian/ Alaska Native (AI/AN) adolescents.
Methods:
This is the first longitudinal study to examine changes in sleep with surveys completed before the pandemic and during the early months of COVID-19 in a sample of urban AI/AN adolescents (N=118; mean age= 14 years at baseline; 63% female). We use a mixed-methods approach to explore how COVID-19 affected urban AI/AN adolescents’ sleep, daily routines, and interactions with family and culture. Quantitative analysis examined whether pandemic-related sleep changes were significant and potential moderators of COVID-19’s effect on sleep, including family and community cohesion and engagement in traditional practices.
Results:
Findings demonstrate changes in sleep, including increases in sleep duration, delays in bedtimes and waketimes, and increases in sleep-wake disturbances (p’s <.001). Higher levels of family cohesion and higher levels of engagement in traditional practices moderated pandemic-related increases in weekday sleep duration. Qualitative analyses revealed changes in adolescents’ sleep and daily behaviors, as well as strategies adolescents used to cope with pandemic-related disruptions in sleep and routines.
Conclusion:
Findings demonstrate positive and negative changes in sleep during COVID-19 stay-at-home orders, including simultaneous increases in sleep duration and sleep-wake disturbances. Results highlight the importance of considering multi-level influences on adolescent sleep, such as early school start times, family dynamics, and cultural factors. A multi-level approach may help guide prevention and intervention efforts to improve adolescent sleep health.
Keywords: COVID-19, coronavirus, sleep, adolescents, health disparities
COVID-19 has exacerbated existing inequities in health and socioeconomic status for certain racial/ethnic groups, including American Indian / Alaska Native (AI/AN) people (Owen, Sundberg, Dionne, & Kosobuski, 2021). For example, a study conducted in the early months of the COVID-19 pandemic found that among low-income racial/ethnic groups, Native American groups ran the highest risk of illness from COVID-19 (Raifman & Raifman, 2020). Furthermore, aggregate analyses of data from selected U.S. states documented higher COVID-19 incidence and mortality among AI/AN individuals compared to White individuals (Arrazola et al., 2020; Hatcher et al., 2020).
Even before the novel coronavirus pandemic (COVID-19) hit the United States (U.S.), AI/AN people were one of the highest risk racial/ethnic groups for health disparities, including high rates of obesity, diabetes, cardiovascular disease, and suicide, contributing to an average life expectancy five years shorter than that of the overall U.S. population (Sequist, 2021). These health disparities are driven by historic and present-day systemic oppression, including forced relocation from tribal lands, inequitable distribution of wealth, and unequal access to healthcare (Duran & Duran, 1995; Owen et al., 2021). Health disparities continue among AI/AN youth of today (Acton et al., 2002), due to both the intergenerational impacts of trauma and current exposure to systemic racism (Dickerson et al., 2019; V. B. Jernigan, Garroutte, Krantz, & Buchwald, 2013; Whitesell, Beals, Crow, Mitchell, & Novins, 2012). These effects may be particularly salient among urban AI/AN adolescents as they experience a unique accumulation of risk factors. For instance, urban AI/AN adolescents experience poverty, crowding, and reduced access to healthcare as well as decreased access to potential stress-buffering cultural activities, relative to those living on tribal lands (Henson, Sabo, Trujillo, & Teufel-Shone, 2017). Despite that over 70% of AI/AN people live in urban areas away from tribal land, urban AI/AN individuals, and adolescents in particular, remain under-recognized in research addressing the impact of COVID-19 (D’Amico et al. (2021).
Adolescence is a critical stage of development for health behaviors and lifestyle factors that can set the stage for future health and socioemotional development. Key adolescent developmental tasks include individuation from parents and increasing identification and affiliation with peers (Pfeifer & Berkman, 2018). Thus, adolescents may be especially affected by disruption to their daily social routines and rhythms caused by pandemic-related stay-at-home orders, such as lack of in-person social interactions with peers and increased time spent with parents and other family members. Research on COVID-19’s impact has shown an increase in insomnia symptoms (Beck, Léger, Fressard, Peretti-Watel, & Verger, 2020) as well as depression and anxiety symptoms among teens (Fish et al., 2020; Franic & Dodig-Curkovic, 2020; Zhou et al., 2020). Also, pandemic-related insomnia symptoms are associated with poorer mental health among teens and young adults (Gruber et al., 2021; Varma, Junge, Meaklim, & Jackson, 2021). On the other hand, several reports have identified increased sleep duration among teenagers and adults during the pandemic (Bruni et al., 2021; Cellini et al., 2021; Gruber, Saha, Somerville, Boursier, & Wise, 2020). Although insomnia is a somewhat predictable reaction to the stress of the pandemic, increased sleep duration is likely a reflection of the removal of a primary structural constraint on adolescent sleep duration during in-person schooling - early school start times.
Despite vulnerabilities, there are important protective factors that may buffer against the negative effects of COVID-19 disruptions on AI/AN adolescents. Specifically, our work in the early months of the pandemic (D’Amico et al., 2021) and prior research (Henson et al., 2017) has highlighted the importance of family, community connection, and culture as key protective factors among AI/AN adolescents. One key component of culture is engaging in traditional practices, which has been posited to have direct health protective effects(Bassett, Tsosie, & Nannauck, 2012). AI/AN traditional practices include a wide range of cultural activities, such as drumming, dancing, beading, learning one’s language, and attending AI/AN cultural events.
Our multi-disciplinary, community-based research team has worked for more than a decade with urban community organizations across the state of California (CA) to understand health disparities and experiences of urban AI/AN youth and adults (D’Amico et al; 2019; D’Amico et al., 2020; Dickerson & Johnson, 2011; Dickerson, Johnson, Castro, Naswood, & Leon, 2012; Dickerson et al., 2014). Thus, when COVID-19 hit in the Spring of 2020, with stay-at-home orders issued in much of the country (including CA), our team was poised to deploy an online survey and qualitative interviews to youth enrolled in an ongoing longitudinal study called Native American Youth Sleep Health and Wellness (NAYSHAW).
The purpose of this paper is to present descriptive analyses from two surveys that were conducted two years apart and qualitative interviews concerning changes in daily routines and sleep within a sample of urban AI/AN youth before and during the early months of COVID-19. In addition, we examine whether there were significant pandemic-related changes in sleep outcomes and how protective factors operating at the family, community, and cultural levels may moderate effects of COVID-19 on adolescent sleep outcomes. We hypothesized that adolescents would experience significant changes in sleep as measured during the early months of COVID-19, including positive effects (e.g., increases in sleep duration) largely due to changes in school schedules, and negative effects (e.g., increases in delayed sleep patterns and poorer sleep quality). Furthermore, we hypothesized that higher levels of family cohesion, greater community cohesion, and greater participation in traditional practices (most of which were moved online) would moderate the effects of pandemic-related changes in sleep. We used qualitative data to provide a richer understanding of teens’ perceptions of changes in their sleep and daily activities, as well as the role of family and cultural factors during the pandemic.
METHODS
Sample
The sample included 118 adolescents from the NAYSHAW study who completed a baseline survey between March 2018–2020 and who participated in an additional COVID-19 survey between May-September 2021. The youth who completed the COVID-19 survey were a subset of participants who completed the baseline survey from NAYSHAW (N=142), a longitudinal study evaluating sleep and its role in health outcomes among urban AI/AN youth. Youth who completed the COVID-19 survey (n=118) did not significantly differ on any sociodemographic characteristics compared to those who did not complete this additional survey (n=24). As with our prior work with Native communities (D’Amico et al., 2020; Dickerson et al., 2020; Dickerson et al., 2014; V.B. Jernigan, D’Amico, Duran, & Buchwald, 2020), we used a community-based participatory research approach, collaborating with our community partner, Sacred Path Indigenous Wellness Center (SPIWC), to ensure culturally appropriate engagement and recruitment of urban AI/AN youth and families.
Eligibility criteria included the following: youth had to either verbally self-identify as AI/AN or be identified as AI/AN by a parent or community member, live in an urban community, and be in the age range of 12–16 at the time of the baseline survey. Both parental consent and youth assent were obtained prior to study participation. Adolescents with major neurologic conditions (e.g., intellectual disability), chronic medical conditions (e.g., cancer, diabetes, cardiovascular disease), or diagnosis of sleep apnea or restless legs syndrome were excluded. All recruitment, data collection, and analytic procedures for this study were approved by the RAND Institutional Review Board and vetted by our community partner and Elder Advisory Board.
Data come from the baseline assessment of NAYSHAW (March 2018- March 2020; during the school year) and our additional COVID-19 survey fielded from May – September 4, 2020. The COVID-19 survey was completed online to ensure the health and safety of participants and data collectors, and consistent with California’s stay-at-home orders (starting March 19, 2020). Youth were compensated $25 for the baseline survey and $30 for the COVID-19 survey. We used stratified random sampling across age, gender, and geographical location from the baseline survey to select 25 teens to participate in in-depth (approximately one hour) interviews conducted via Facetime. Participants were paid $35 for qualitative interviews, which were audio-recorded and transcribed.
Quantitative Measures
Demographic characteristics, which were included as covariates, were assessed at baseline. Sleep and daily activities were assessed at both baseline and the COVID-19 assessment to allow for evaluation of changes in daily routines and sleep patterns. Hypothesized moderators (i.e., family cohesion, community cohesion, and engagement in traditional practices) were collected during the COVID-19 survey.
Demographics.
Participants reported age, gender, race/ethnicity, and family structure (i.e., two-parent vs. single-parent household).
Sleep.
Sleep-wake patterns were measured by asking about bedtime and wakeup times on school days and weekends and are reported separately for weekends and weekdays (Troxel et al., 2017). Sleep quality was assessed by asking the participant to rate overall sleep quality in the past month from 1 (very good), 2 (fairly good), 3 (fairly bad), to 4 (very bad); higher scores reflect poorer sleep quality. Sleep disturbance was measured using a shortened (6-item) version of the sleep-wake problem subscale from the School Sleep Habits Survey for Adolescents (Carskadon, Seifer, & Acebo, 1991; Wolfson & Carskadon, 1998; Wolfson et al., 2003). Adolescents endorsed frequency of engagement in the following indicators of erratic and/or disturbed sleep/wake behaviors over the past 2 weeks: stayed up past 3:00 a.m. or later; slept in past noon; felt tired, dragged out or sleepy during the day; had an extremely hard time falling asleep; had nightmares or bad dreams; woke up in the middle of the night and had trouble falling back to sleep. Items were rated: 0 (never), 1 (once), 2 (twice), 3 (several times), to 4 (every day/night); we calculated the average of the six responses. Internal consistency for the shortened scale was adequate (α =.74). Higher scores indicate more sleep/wake problems.
Daily activities.
We used items drawn from the Youth Risk Behavior Survey (YRBS) to measure ten daily activities that teens may engage in on a “typical day”, including hours (0 – 4 or 5=“5 or more hours”) of playing computer games, watching movies/videos, doing homework, reading, and spending time with friends and family (Centers for Disease Control and Prevention, 2007). For the COVID-19 survey, the prompt was slightly modified to reference daily activities “since the stay-at-home order for coronavirus began”.
Family Cohesion.
Participants completed a validated seven-item scale that measured family cohesion (e.g., “In our family there is a feeling of togetherness”), drawn from the Brief Family Relationship Scale (BFRS) and anchored in the timeframe “since the stay-at-home order for coronavirus began” (Fok, Allen, Henry, & People Awakening, 2014). Items were rated from 0 (not at all), 1 (somewhat), to 2 (a lot); higher scores indicated more cohesion.
Community Cohesion.
Community cohesion was measured with a single item, “I felt people in my community were coming together and supporting each other,” with the time frame being “the last two weeks,” and response options ranging from 0 (not at all) to 3 (nearly every day).
Participation in traditional practices.
Youth reported participation in eight traditional practices, including beading, attending virtual powwows or talking circles “since the stay-at-home order for coronavirus began.” This list was compiled based on prior work and with our community partners (Kaufman et al., 2014). In particular, community partners emphasized how many traditional practices were moved to online/ virtual experiences during stay-at-home orders as a means to keep the community connected and supported. We derived a count of the number of traditional practices in which youth participated at least once.
Quantitative Analytic Strategy
First, we conducted descriptive analyses of demographics at baseline, sleep measures and daily activities from both baseline and COVID-19 assessments, and cohesion and traditional practices from the COVID-19 assessment. The primary analyses involved mixed effect models for repeated measures to examine whether there were significant changes in sleep from baseline to COVID-19 assessment in sleep, after covariate adjustment. The primary statistic of interest for these models is the fixed effect of time (coded as 0 = baseline/pre-COVID-19 wave and 1 = during COVID-19), after adjustment for covariates (age and sex). Follow-up analyses examined potential moderation, by adding in the interaction terms for each proposed moderator with the indicator variable for time in separate models (i.e., family cohesion, community cohesion, and participation in traditional practices). All models included a subject specific random intercept and time specific error term, and covariates including age and sex.
The COVID-19 survey was conducted between May to September 4, 2020. Given known variability in sleep during school versus summer vacation schedules, we conducted sensitivity analyses. These analyses added the interaction term for participants completing the survey during “summer” (n=70; defined as June 15- August 14) versus those completing during the typical school year for CA (n=48; May – June 14 and August 15 – September 4). For all sleep outcomes, there were no significant interactions for timing of assessment (summer versus school year) in models predicting changes in sleep from baseline to COVID-19. There were also no significant differences in sleep outcomes when comparing youth who completed the survey during the school year versus summer (analyses available upon request). Therefore, we present analyses for the full sample to retain sample size.
Qualitative Interviews
Drawing from literature reviews, findings from NAYSHAW interviews (Palimaru et al., 2020), and input from SPIWC, we designed the protocol to elicit narratives about pandemic-induced changes in six domains: (1) daily habits/routines; (2) family/social relationships; (3) sleep environments and arrangements; (4) sleep behavior; (5) quality of sleep; and (6) cultural dimensions of life and sleep (see supplemental material). Interviews followed a semi-structured protocol and lasted approximately one hour. All interviews were audio-recorded and transcribed verbatim.
Qualitative Analytic Strategy
The objective of the qualitative analyses was to provide interpretive context for findings from quantitative models. Transcripts were uploaded to Dedoose, a qualitative analysis platform that facilitates collaborative transcript management, coding, and analysis (“Dedoose Version 5.0.11 “, 2013). Due to the timely need for data about pandemic-related effects on health we complemented the rapid assessment (RA) of content in Dedoose (Johnson & Vindrola-Padros, 2017) with a keyword-in-context (KWIC) textual analysis conducted in NVivo to find additional relevant content (Ltd., 2018). The RA codebook was developed by two coders (AIP and RAB) based on pre-identified domains from the survey, with more than half the codes drawn from a previous codebook developed with the same population and a similar set of sleep-related questions (Palimaru et al., 2020), and additional codes added to cover unique pandemic-related content. These new pandemic-related codes focused on the changes that occurred during the pandemic in areas such as use of electronics, sleep behaviors and the sleep environment. As part of the RA approach, these codes were applied structurally following the pandemic-focused questions in the interview protocol, such as “How has your sleep quality been affected by coronavirus?” and “How has coronavirus changed your relationship with your parents?” As thematic categories were defined a priori by interview domains, we describe specific observations in these thematic categories through counts (and percentages) of times each was mentioned, as well as verbatim quotes to supplement these counts.
Both the qualitative and KWIC analyses were conducted by one coder (AIP). The KWIC analysis produced a raw frequency of distinctive words used in answer to protocol questions. The 50 most frequently used distinctive words were selected and analyzed in context, i.e., 15 words preceding and 15 words following each word. We excluded prepositions and conjunctions, as well as linguistic disfluencies that are common among this participant age group, such as “like.” The KWIC findings helped ensure that we captured all relevant content for each thematic area.
Results
Quantitative Results
Demographic characteristics are presented in Table 1. Mean age at baseline was 14 years, and 63% of the sample was female. Consistent with prior work D’Amico et al. (2021), most (89%) youth self-identified as AI/AN, though all teens were identified by their parents as AI/AN. Just over half of the sample reported living in a single-parent household.
Table 1.
NAYSHAW COVID-19 Supplement Sample Demographics and Moderators (N = 118).
| Demographics (measured at baseline) | M (SD, range) or N (%) |
|---|---|
| Age | |
| 12 years old | 18 (15%) |
| 13 years old | 28 (24%) |
| 14 years old | 29 (25%) |
| 15 years old | 19 (16%) |
| 16 years old | 24 (20%) |
| Mean age, years (continuous) | 14.0 (1.4, 12–16) |
| Sex | |
| Male | 44 (37%) |
| Female | 74 (63%) |
| Race/Ethnicity* | |
| Hispanic/Latino(a) | 59 (50%) |
| AI/AN | 106 (89%) |
| Asian/Asian American/Pacific Islander | 12 (10%) |
| Black/African American | 12 (10%) |
| White/Caucasian | 21 (18%) |
| Single-parent households | 61 (52%) |
|
| |
| Moderators (measured at COVID-19 survey) | M (SD, range) |
|
| |
| Family cohesion | 1.55 (0.42, 0 – 2) |
| Neighborhood cohesion | 1.50 (1.10, 0 – 3) |
| Traditional activity engagement | 2.54 (2.11, 0 – 8) |
Note.
race/ethnicity categories are not mutually exclusive.
Table 2 describes sleep measures before and during COVID-19. Teens showed a delay in bedtimes and waketimes on weekdays and weekends, but overall had longer sleep durations (roughly 2 hours more sleep) during COVID-19 compared to baseline. Teens also showed higher levels of sleep/wake disturbances during COVID-19, and a decrease in self-reported sleep quality.
Table 2.
Sleep-wake patterns and problems.
| Baseline | COVID-19 survey | Change | |
|---|---|---|---|
|
|
|||
| M (SD) | M (SD) | M (SD) | |
| Bedtime on weekdays | 10:25PM(71 min) | 12:18AM (109 min) | 112 (117 min) |
| Bedtime on weekends | 11:58PM (88 min) | 12:55AM (109 min) | 177 (107 min) |
| Wake time on weekdays | 6:25AM (44 min) | 9:22AM (97 min) | 57 (119 min) |
| Wake time on weekends | 9:19AM (112 min) | 10:07AM (104 min) | 49 (133 min) |
| Sleep duration on weekdays (minutes) | 415 (61 min) | 544 (106 min) | 130 (117 min) |
| Sleep duration on weekends (minutes) | 449 (75 min) | 552 (109 min) | 103 (127 min) |
| Sleep disturbance scale | 7.1 (4.6) | 9.4 (5.3) | 2.3 (6.0) |
| Sleep poor quality | 2.0 (0.7) | 2.2 (0.8) | 0.2 (0.8) |
Table 3 presents descriptive statistics for frequency of engagement in a variety of daily activities at both assessment points to show how teens’ daily behaviors may have changed. Overall, teens’ daily activities, including doing homework or hanging out with friends, remained relatively stable from baseline to during COVID-19, with some increases in time spent on the internet, communicating with friends digitally, and watching TV/videos/movies.
Table 3.
Descriptive analyses of typical daily activities before and during COVID.
| Baseline | COVID-19 Survey | Change | |
|---|---|---|---|
|
|
|||
| M (SD) | M (SD) | M (SD) | |
| Hanging out with friends | 1.53 (1.48) | 1.43 (1.94) | −0.10 (2.17) |
| Hanging out with family members | 3.42 (1.58) | 3.42 (1.69) | −0.01 (2.10) |
| Helping family with housework or caregiving | 2.02 (1.35) | 2.57 (1.65) | 0.55 (2.01) |
| Communicating with friends digitally a | 2.49 (1.64) | 3.18 (1.87) | 0.69 (1.99) |
| Playing video games | 2.64 (1.60) | 2.97 (1.80) | 0.33 (2.14) |
| Surfing the internet | 1.12 (1.49) | 1.76 (1.58) | 0.64 (1.95) |
| Watching TV / videos / movies | 2.62 (1.40) | 3.36 (1.44) | 0.74 (1.66) |
| Reading for fun | 1.08 (1.39) | 1.21 (1.46) | 0.13 (1.60) |
| Homework or other academic activities | 2.03 (1.38) | 1.91 (1.71) | −0.13 (2.04) |
| Working for pay | 0.18 (0.62) | 0.69 (1.57) | 0.52 (1.64) |
“Change” is from baseline to the COVID-19 survey – that is, the value at the COVID-19 survey minus the value at the baseline survey. All items have response options ranging from 0 (“No hours”) to 5 (5 or more hours).
Includes “communicating with friends by email, instant messaging, texting on your phone, or through social media sites, such as Instagram or Snapchat”.
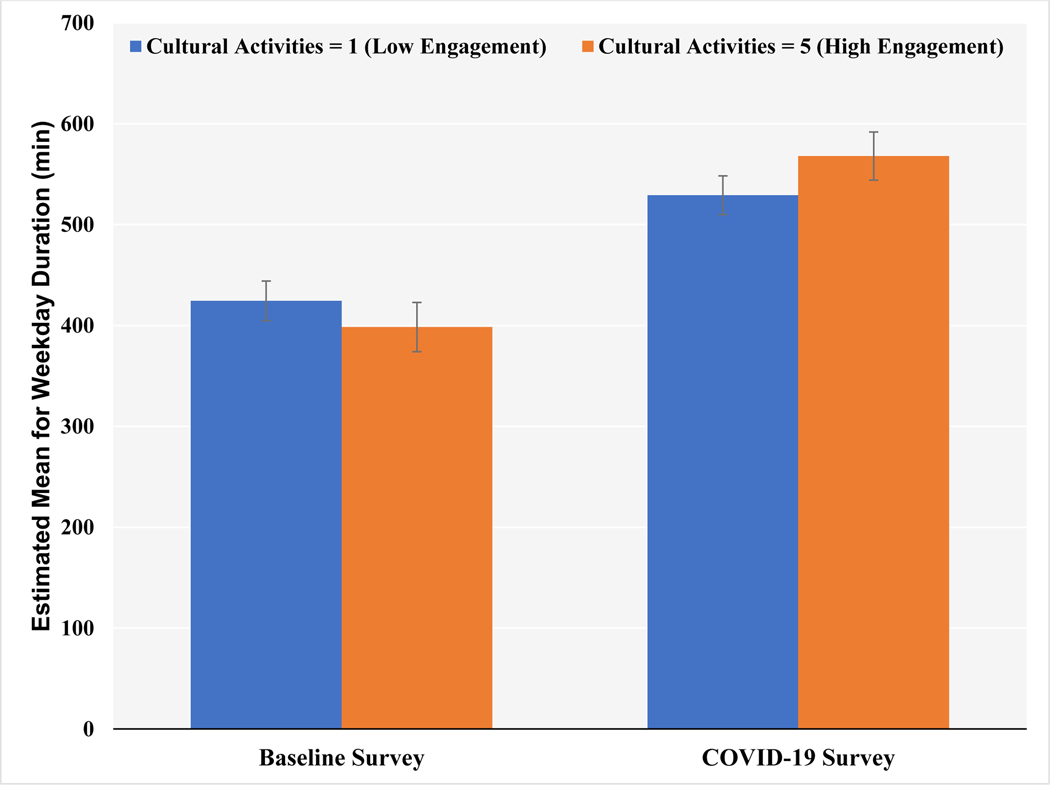
The repeated measures analysis (Table 4) shows significant changes in all sleep outcomes comparing baseline to the pandemic period. Compared to baseline, bedtimes and waketimes during COVID-19 were significantly delayed (p’s <.001), both on weekdays and weekends, though the delay was larger for weekdays than weekends. Similarly, there was a significant increase in sleep duration from baseline to COVID-19, with a larger increase observed on weekdays (β = 129.55, SE = 10.92, p < 0.001) versus weekends (β = 103.75, SE = 11.93, p < 0.001). Participants also experienced increases in sleep/wake disturbances and poorer sleep quality during COVID-19 (β = 2.25, SE = 0.55, p <.001 and β = 0.18, SE = 0.07, p = 0.02, respectively). Overall, our analysis of potential moderators of observed changes in sleep yielded few significant results. We observed significant moderating effects of family and cultural factors on weekday sleep duration, such that higher levels of family cohesion or higher participation in traditional practices moderated the COVID-related increase in weekday sleep duration. To facilitate interpretation of the interactions, Figure 1 demonstrates adjusted mean weekday sleep duration at “high” and “low” levels of participation in traditional practices before and during COVID-19. As shown, while weekday sleep duration increased from baseline to COVID-19 overall, those who participated in more traditional practices showed an even greater increase in weekday sleep duration than those engaged in fewer traditional practices.
Table 4.
Results from mixed effect models examining change in sleep outcomes before and during COVID-19 and moderation effects.
| Main effect of time | Models to Test Moderation: Time by Moderator Interaction | |||
|---|---|---|---|---|
|
| ||||
| Family cohesion | Neighborhood cohesion | Traditional Practices | ||
|
| ||||
| β (SE) | β (SE) | β (SE) | β (SE) | |
| Bedtime on weekdays (hours after noon) | 1.87 (0.18)*** | −0.12 (0.44) | −0.26 (0.16) † | −0.15 (0.08) |
| Bedtime on weekends (hours after noon) | 0.96 (0.18)*** † | −0.03 (0.44) † | −0.27 (0.16)† | −0.04 (0.09)† |
| Wake time on weekdays (hours after midnight) | 2.95 (0.16)*** | 0.36 (0.39) | 0.11 (0.15) | 0.01 (0.08) |
| Wake time on weekends (hours after midnight) | 0.81 (0.20)*** † | 0.23 (0.49) † | −0.30 (0.19) † | −0.02 (0.10) † |
| Sleep duration on weekdays (minutes) | 129.55 (10.92)*** | 56.14 (25.71)* | 16.55 (9.94) | 16.21 (5.01)** |
| Sleep duration on weekends (minutes) | 103.75 (11.93)*** | 20.88 (28.88) | 10.65 (11.05) | 9.46 (5.62) |
| Sleep disturbance scale | 2.25 (0.55)***† | −0.59 (1.33)† | −0.45 (0.50)† | 0.08 (0.26)† |
| Sleep poor quality | 0.18 (0.07)*† | −0.07 (0.18)† | −0.08 (0.07)† | −0.04 (0.04)† |
p<.05
p<.01
p<.001
Significant (p<.05) within-person differences per random effect
All results are from a series of mixed linear repeated measures regression models with a random effect for individual and fixed effects for age and gender. Coefficients for “overall change” represent adjusted change in the outcome from baseline to the COVID-19 survey in a model with a main effect for time and covariates. Coefficients for moderation are for interactions between time and the moderator, representing whether higher values of the moderator are associated with a positive or negative change relative to those with lower values of the moderator.
Figure 1.
Effect Modification by Engagement with Traditional Practices on Weekday Sleep Durations (min) Contrasting Baseline Versus COVID-19 Surveys)
Qualitative Results
Teens’ perceptions of key contributors to changes in sleep behaviors and sleep quality
Thematic findings align with survey results that capture dramatic changes in bedtimes and wake times. During the pandemic, more than half of the teens (n= 15, 60%) described going to bed between midnight and 3:00 am on weeknights, and three (12%) mentioned instances of going to bed after 3:00 am. For many, weekends blended into weekdays, so sleep patterns extended through the entire week, as this 16-year-old female explains: “Now there’s not really a difference between weekends and weekdays for me because I do the same thing every day.”
Participants linked sleep changes to the shift to online schooling, and described two main implications for their sleep. First, participants described how they did not have to worry about being ready for school or wake up early to get to school during the pandemic, thus removing an element of stress from pre-bedtime routines and allowing more opportunity for sleep in the mornings: “I feel like I’m a bit more relaxed to actually go to sleep because there was a different school schedule” (male, age 16). Another said before the pandemic “I would wake up at like, 5:00 or a little bit after 5:00, and now I can wake up at 7:00 because that’s when school starts” (male, age 12). Second, half of participants said they were not as tired during the day compared to before the pandemic, but they were also less sleepy at night, largely due to the absence of school-related activities. For example, one female participant (age 14) said “It was a lot easier for me to go to sleep because before we were going to school and I was actually doing something. I was able to do something every single day. So I would get tired from doing something. But when you have to stay at home… that doesn’t really make you tired.”
Although the quantitative analyses revealed an increase in poor sleep quality during COVID-19, only four interviewees (16%) mentioned poorer sleep quality. Stated reasons for poor sleep included worries about the pandemic and disruptions in sleep schedules, as illustrated here: “When I sleep on a schedule, I tend to get better sleep. But now since I’m not sleeping on any type of schedule and I just sleep whenever I feel like it, it’s just like the sleeps don’t feel good, like quality good” (female, age 14). For nearly a third of participants (n=7) sleep quality remained unaffected, whereas for another third sleep quality improved primarily due to an increase in sleep duration.
Teens’ perceptions regarding changes in daily activities
Participants expressed frustration with the disruption to their schedules and associated effects on their sleep, and half of the sample spoke about strategies they implemented daily to mitigate sleep-related consequences of these disruptions. Almost a third of teens (n=7) described exercising throughout the day or just before bedtime. One 14-year-old male explained that “Before I go to bed I do ten pushups just to be able to get a little tired,” while this 16-year-old female said “I try exercising to get myself tired. I’ll exercise in the morning, I’ll exercise at night thinking I’ll get tired.”
Consistent with findings in Table 3 showing an increase in daily use of electronics, most teens (n=21, 84%) described increases in time spent on electronic devices such as phones, tablets, laptops and game consoles. As one 16-year-old female stated: “It’s definitely gone up a lot. I’m not usually on my phone or on my computer a lot during school because I am pretty involved in my school… And now especially since everything’s online and all my homework’s online, I think I’ve definitely been on my phone more.” Nearly half of teens (n=12) cited boredom as a driver of online activity, describing getting “bored with being in the house” (male, age 13) or being bored because “I can’t do anything or go out” (female, age 15). For a quarter of participants (n=6), using their electronic devices was part of their bedtime routine, as this 12-year-old female explained: “Sometimes I’ll be on it [phone] for a couple of hours to fall asleep.”
Teens’ perceptions regarding family and participation in traditional practices
Although the analysis of potential moderators yielded few significant results, teens revealed key insights into how family cohesion evolved during the pandemic, especially in tandem with family engagement in traditional practices. Forty percent of teens (n=10) described spending more time with their parents, and in some cases, getting closer to them: “Before coronavirus, my mom wasn’t living with us. So I didn’t really have a relationship with her. But now that during the virus she has to stay home with us, like she can’t go anywhere, I feel like it’s helping our relationship a lot. It’s helping all of that be better” (female, age 14). For nearly a quarter of teens, this relationship remained unchanged, whereas a few (n=4, 16%) described mild conflict during the pandemic, such as “little stuff that I get bickered at” (male, age 13).
Engagement in traditional practices, either by themselves or with their families, was another important theme. Half of interviewed teens described traditional practices that either helped them cope with the stresses of the pandemic or helped improve sleep. This 13-year-old male said “We go to the online meetings and we talk to the people. It’s like a bunch of other tribes. It’s like a team, all the teams from different tribes.” Some narratives suggested family discussions to make sense of the pandemic whilst drawing on Native ancestral knowledge: “I don’t know, but like, my dad always says, like, this has always been coming, I guess. So, it’s like not a shocker that something bad like this is going to happen. Like, in history this is normal, I guess, if you look back in history. Like, this isn’t just like a once in a lifetime thing, it’s already happened before” (male, age 15).
Discussion
COVID-19 has presented numerous challenges to our daily rhythms and routines, and has introduced significant stress that can negatively affect sleep. There has been particular concern about effects of the pandemic and associated stay-at-home orders on adolescents given that (even pre-pandemic) adolescents were already a high-risk population for sleep-wake problems (Keyes, Maslowsky, Hamilton, & Schulenberg, 2015) as well as mental health problems (Merikangas et al., 2010). This is also a developmental stage characterized by increased need for social connections outside the home, especially with peers (Orben, Tomova, & Blakemore, 2020). To our knowledge, this is the first longitudinal (pre- and during the early months of COVID-19) analysis of changes in sleep patterns and disturbances in adolescents, as prior work has been cross-sectional or retrospective, and with few exceptions, focused on adults (Bruni et al., 2021; Cellini et al., 2021; Gruber et al., 2020). In addition, our focus on urban AI/AN youth is unique and important as this is a population under-recognized in sleep research in general. Furthermore, similar to other racial/ethnic groups in the United States, AI/AN individuals experience disproportionate socioeconomic and health burdens related to COVID-19. Finally, our analysis makes a unique contribution by describing both quantitative and qualitative changes in teens’ daily activities during the pandemic, and exploring the role of key potential protective factors at the family, community, and cultural levels.
Consistent with limited prior work during the first few months of COVID-19 (Gruber et al., 2020), we found significant delays in adolescent bedtimes and waketimes; however, delays in waketimes more than compensated for delays in bedtimes, as teens also demonstrated a roughly two-hour increase in sleep duration during the early months of COVID-19. Findings were more pronounced for weekdays. Given that the timing of the COVID-19 assessment (May- September 4) included months when most teens were engaged in remote school as well as summer vacation months (mid-June through August), findings cannot conclusively determine that increased sleep duration is entirely due to removal of early school start times. However, findings are suggestive of this possibility and consistent with other reports (Gruber et al., 2020), and supported by sensitivity analyses conducted in the subsample who completed the COVID-19 survey in May or June. Furthermore, the relatively small difference in hours spent doing homework suggests that findings are largely due to COVID-related changes in school schedules, rather than the transition to summer schedules. Regardless, findings clearly demonstrate teens’ natural, delayed sleep-wake patterns are misaligned with school start times, which in the U.S., on average begin at 8:03 am (Troxel & Wolfson, 2017). Although teens were sleeping more, they simultaneously experienced increases in sleep-wake disturbances, which included indicators of phase delay (e.g., staying up past 3 a.m.) and insomnia-related symptoms (i.e., trouble falling asleep or staying asleep). It is perhaps not surprising that teens experienced increases in these symptoms during the early months of the pandemic, as they are indicative of the disruption to daily routines resulting from COVID-related closures and stay-at-home orders, as well as COVID-related increases in stress and anxiety (Jones, Mitra, & Bhuiyan, 2021; Tang, Xiang, Cheung, & Xiang, 2021). Moreover, other disruptions related to stay-at-home orders including lack of consistency in routines in general, potential crowding within homes as family members stay at home, and changes in sleep patterns of the family, may have also contributed to the observed changes in sleep.
Overall, we found few significant moderating effects of family cohesion, community cohesion, or participation in traditional practices. However, adolescents who reported greater family cohesion or greater participation in traditional practices also reported greater weekday sleep duration during COVID-19. Of note, interview findings highlighted that for some teens greater family cohesion meant becoming closer with parents and engaging in traditional practices together. Such moderating effects, though limited in the current study, are consistent with prior work on protective factors for teens’ mental health during COVID-19 (Tang et al., 2021), and on protective factors for AI/AN teens’ mental health in general (Henson et al., 2017).
Our study provides an important “first look” at pandemic-related changes to urban AI/AN adolescents’ typical daily activities. Somewhat surprisingly, teens showed relatively little change in activity patterns during COVID-19, with the exception of increased electronics/media use. The pandemic-related increase in screen time is notable, as even pre-pandemic screen time rates were high among AI/AN and other teens (Hicks & Diamond, 2011; Palimaru et al., 2020). Interview themes aligned with survey findings regarding changes in sleep patterns, and revealed teens’ agency in coping with these changes, such as deliberate use of physical exercise and electronics as ways to increase tiredness and help transition to nighttime sleep. Narratives also suggested that in the absence of typical school-related routines, teens had more time available with less structure; as a result, managing boredom was a daily challenge. Results invite further exploration of how technology could be harnessed to support teens in managing their time, improving sleep, and engaging in health-promoting activities such as exercise and participation in traditional practices.
Limitations and Strengths
Several limitations are noteworthy. First, participants in this study resided in urban areas in southern, central, and northern California, so views and experiences may not reflect those of urban AI/AN individuals elsewhere in the U.S. Second, survey and interview data were collected between May and September 2020, when stay-at-home orders and local restrictions varied across the state, which may have introduced heterogeneity. Further, overlap with summer schedules may have confounded results. In addition, the rapid assessment qualitative approach was conducted in Dedoose by one coder while the KWIC analysis was completed in NVivo, which meant we did not calculate inter-coder reliability. However, more than half of the codebook had been developed and assessed for reliability previously. It is also important to note that the limited support for moderation may reflect limitations in the measures themselves (e.g., community cohesion was based on a single-item), as well as the relatively small sample size, which may have limited statistical power. Finally, this study is focused on an under-recognized population that has been disproportionately affected by COVID-19. However, given that the study does not include a comparator population, findings cannot be interpreted as evidence that AI/AN teens have experienced more or worse sleep disturbances compared to other populations. Future work is needed to consider downstream effects of COVID-19 on racially/ethnically diverse populations of youth, including AI/AN individuals, in order to identify disparities as well as potential unique sources of risk and resilience across racial/ ethnic groups.
These limitations notwithstanding, the study also has several notable strengths. First, the focus on AI/AN teenagers is important in order to understand how COVID-19 has affected sleep and daily rhythms in this population, and to identify potential protective factors that may be specifically salient for this group. Second, our focus on adolescence, a developmental stage that is vulnerable to both sleep disturbances and mental health consequences and that may be specifically vulnerable to pandemic-related stay-at-home orders, is important to identify opportunities for intervention. Finally, our repeated measures assessment of sleep and daily activities across two waves of data collection, and the inclusion of qualitative and quantitative methods, is a notable strength, given that most existing studies on sleep during COVID-19 have been cross-sectional or have included retrospective reports of sleep, and have not included qualitative analyses.
Conclusion
In this study of urban AI/ AN adolescents, we found significant effects of COVID-19 stay-at-home orders on adolescents’ sleep-wake patterns and disturbances, including some positive changes (an increase in sleep duration) and some negative changes (increases in sleep problems). Teens also indicated resilience through their own agency, and via family and community support, suggesting that opportunities to connect with their Native culture and communities helped them cope. Prevention strategies should incorporate sleep and stress management aids, as well as technology-based support for teens’ daily organization and planning. Finally, strength-based strategies, such as family-level engagement with culture and tradition should be encouraged and supported.
Supplementary Material
Acknowledgements
The authors would like to thank all study participants, their family members, and our community partners. The authors also thank study coordinators (Jennifer Parker, Keisha McDonald, Nina Ozbardakci), survey research group technological team (Evelyn Bogdon, Roberto Guevara, and Eric Min), and our data collection team.
Funding
This work was supported by the National Center on Minority Health and Health Disparities under Grant R01MD012190 (MPIs: Troxel, D’Amico, Dickerson).
Role of Funder/Sponsor: The NIH had no role in the design and conduct of the study.
Footnotes
Disclosure statement
WMT serves on the editorial board for Behavioral Sleep Medicine and Sleep Health and serves on scientific advisory board for Feelmore Labs and sleepfoundation.org. No other conflicts of interest were reported by the author(s).
References
- Acton KJ, Burrows NR, Moore K, Querec L, Geiss LS, & Engelgau MM (2002). Trends in Diabetes Prevalence Among American Indian and Alaska Native Children, Adolescents, and Young Adults. 92(9), 1485–1490. doi: 10.2105/ajph.92.9.1485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrazola J, Masiello MM, Joshi S, Dominguez AE, Poel A, Wilkie CM, . . . Landen M. (2020). COVID-19 Mortality Among American Indian and Alaska Native Persons - 14 States, January-June 2020. MMWR. Morbidity and mortality weekly report, 69(49), 1853–1856. doi: 10.15585/mmwr.mm6949a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett D, Tsosie U, & Nannauck S. (2012). “Our culture is medicine”: perspectives of Native healers on posttrauma recovery among American Indian and Alaska Native patients. The Permanente journal, 16(1), 19–27. doi: 10.7812/tpp/11-123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck F, Léger D, Fressard L, Peretti-Watel P, & Verger P. (2020). Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. Journal of Sleep Research. doi: 10.1111/jsr.13119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Dickerson DL, & D’Amico EJ (2016). Cultural identity among urban American Indian/Alaska Native youth: Implications for intervention design. Prevention Science, 17(7), 852–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Dickerson DL, Klein DJ, Agniel D, Johnson C, & D’Amico EJ (2019). Identifying as American Indian/Alaska Native: Implications for adolescent behavioral health and well-being. Youth & Society( 10.1177/0044118X19840048). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni O, Malorgio E, Doria M, Finotti E, Spruyt K, Melegari MG, . . . Ferri R. (2021). Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Medicine, S1389–9457(1321)00094–00090. doi: 10.1016/j.sleep.2021.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Seifer R, & Acebo C. (1991). Reliability of six scales in a sleep questionnaire for adolescents. Sleep Research, 20, 421. [Google Scholar]
- Cellini N, Conte F, De Rosa O, Giganti F, Malloggi S, Reyt M, . . . Ficca G. (2021). Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med, 77, 112–119. doi: 10.1016/j.sleep.2020.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2007). Youth Risk Behavior Survey. Retrieved from www.cdc.gov/yrbss
- Clark R, & Johnson CL (2008). Overview of issues facing native women who are survivors of violence in urban communities. In Deer S, Clairmont B, Martell CA, & Eagle M. L. White (Eds.), Sharing our stories of survival: Native women surviving violence (pp. 87–99). New York, NY: AltaMira Press. [Google Scholar]
- D’Amico EJ, Dickerson DL, Brown RA, Klein DJ, Agniel D, & Johnson C. (2019). Unveiling an ‘invisible’ population: Health, substance use, sexual behavior, culture, and discrimination among urban American Indian/Alaska Native adolescents in California. Ethnicity & Health. doi: 10.1080/13557858.2018.1562054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Dickerson DL, Brown RA, Johnson C, Agniel D, & Klein D. (2020). Motivational Interviewing and Culture for Urban Native American Youth (MICUNAY): A randomized controlled trial. Journal of Substance Abuse Treatment, 111, 86–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Palimaru AI, Dickerson DL, Dong L, Brown RA, Johnson CL, . . . Troxel WM (2021). Risk and Resilience Factors in Urban American Indian and Alaska Native Youth during the Coronavirus Pandemic. American Indian Culture and Research Journal, 44(2), 21–48. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedoose Version 5.0.11 (2013). Los Angeles: SocioCultural Research Consultants, LLC. [Google Scholar]
- Dickerson DL, Baldwin JA, Belcourt A, Belone L, Gittelsohn J, Kaholokula K, . . . Wallerstein N. (2020). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prevention Science, 21, 33–42. doi: 10.1007/s11121-018-0926-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Brown RA, Klein DJ, Agniel D, Johnson C, & D’Amico EJ (2019). Overt perceived discrimination and racial microaggressions and their association with health risk behaviors among a sample of urban American Indian/Alaska Native adolescents. Journal of Racial and Ethnic Health Disparities, 6(4), 733–742. doi: 10.1007/s40615-019-00572-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, & Johnson CL (2011). Design of a behavioral health program for urban American Indian/Alaska Native youths: A community informed approach. Journal of Psychoactive Drugs, 43(4), 337–342. [DOI] [PubMed] [Google Scholar]
- Dickerson DL, Johnson CL, Castro C, Naswood E, & Leon JMP (2012). CommUNITY Voices: Integrating traditional healing services for urban American Indians/Alaska Natives in Los Angeles County. In Learning Collaborative Summary Report. Los Angeles, Calif.: Los Angeles County Department of Mental Health. [Google Scholar]
- Dickerson DL, Venner KL, Duran B, Annon JJ, Hale B, & Funmaker G. (2014). Drum-Assisted Recovery Therapy for Native Americans (DARTNA): Results from a pretest and focus groups. American Indian and Alaska Native Mental Health Research, 21(1), 35–58. doi: 10.5820/aian.2101.2014.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duran E, & Duran B. (1995). Native American post-colonial psychology. New York, NY: Suny Press. [Google Scholar]
- Fish JN, McInroy LB, Paceley MS, Williams ND, Henderson S, Levine DS, & Edsall RN (2020). I’m kinda stuck at home with unsupportive parents right now’: LGBTQ youths’ experiences with Covid-19 and the importance of online support. Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2020.06.002 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fok CCT, Allen J, Henry D, & People Awakening T. (2014). The Brief Family Relationship Scale: A Brief Measure of the Relationship Dimension in Family Functioning. Assessment, 21(1), 67–72. doi: 10.1177/1073191111425856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franic T, & Dodig-Curkovic K. (2020). Covid-19, child and adolescent mental health – Croatian (in)experience. Irish Journal of Psychological Medicine. doi: 10.1017/ipm.2020.55 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R, Gauthier-Gagne G, Voutou D, Somerville G, Saha S, & Boursier J. (2021). Pre-pandemic sleep behavior and adolescents’ stress during Covid-19: a prospective longitudinal study. Child and Adolescent Psychiatry and Mental Health, 15(1), 43. doi: 10.1186/s13034-021-00399-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R, Saha S, Somerville G, Boursier J, & Wise MS (2020). The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Medicine, 76, 33–35. doi: 10.1016/j.sleep.2020.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher SM, Agnew-Brune C, Anderson M, Zambrano LD, Rose CE, Jim MA, . . . McCollum J. (2020). COVID-19 Among American Indian and Alaska Native Persons - 23 States, January 31-July 3, 2020. MMWR. Morbidity and mortality weekly report, 69(34), 1166–1169. doi: 10.15585/mmwr.mm6934e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson M, Sabo S, Trujillo A, & Teufel-Shone N. (2017). Identifying Protective Factors to Promote Health in American Indian and Alaska Native Adolescents: A Literature Review. J Prim Prev, 38(1–2), 5–26. doi: 10.1007/s10935-016-0455-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks AM, & Diamond LM (2011). Don’t go to bed angry: Attachment, conflict, and affective and physiological reactivity. Personal Relationships, 18(2), 266–284. doi: 10.1111/j.1475-6811.2011.01355.x [DOI] [Google Scholar]
- Jernigan VB, D’Amico EJ, Duran B, & Buchwald D. (2020). Multilevel and community-level interventions with Native Americans: Challenges and opportunities. Prevention Science, 21, 65–73. doi: 10.1007/s11121-018-0916-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan VB, Garroutte E, Krantz EM, & Buchwald D. (2013). Food insecurity and obesity among American Indians and Alaska Natives and Whites in California. Journal of Hunger & Environmental Nutrition, 8(4), 458–471. doi: 10.1080/19320248.2013.816987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson GA, & Vindrola-Padros C. (2017). Rapid qualitative research methods during complex health emergencies: A systematic review of the literature. Soc Sci Med, 189, 63–75. doi: 10.1016/j.socscimed.2017.07.029 [DOI] [PubMed] [Google Scholar]
- Jones EAK, Mitra AK, & Bhuiyan AR (2021). Impact of COVID-19 on Mental Health in Adolescents: A Systematic Review. Int J Environ Res Public Health, 18(5), 2470. doi: 10.3390/ijerph18052470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman CE, Black K, Keane EM, Big Crow CK, Shangreau C, Arthur-Asmah R, . . . Tuitt N. (2014). Planning for a Group-Randomized Trial With American Indian Youth. Journal of Adolescent Health, 54(3, Supplement), S59–S63. doi: 10.1016/j.jadohealth.2013.12.028 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Maslowsky J, Hamilton A, & Schulenberg J. (2015). The Great Sleep Recession: Changes in Sleep Duration Among US Adolescents, 1991–2012. Pediatrics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ltd., Q. I. P. (2018). NVivo 12 Teams (Version Version 12). [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, . . . Swendsen J (2010). Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49(10), 980–989. doi:S0890–8567(10)00476–4 [pii]; 10.1016/j.jaac.2010.05.017 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben A, Tomova L, & Blakemore S-J (2020). The effects of social deprivation on adolescent development and mental health. The Lancet. Child & adolescent health, 4(8), 634–640. doi: 10.1016/S2352-4642(20)30186-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen MJ, Sundberg MA, Dionne J, & Kosobuski AW (2021). The Impact of COVID-19 on American Indian and Alaska Native Communities: A Call for Better Relational Models. 111(5), 801–803. doi: 10.2105/ajph.2021.306219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palimaru AI, Brown RA, Troxel WM, Dickerson DL, Johnson CL, & D’Amico EJ (2020). Understanding sleep facilitators, barriers, and cultural dimensions in Native American urban youth. Sleep Health, 6(4), 478–488. doi: 10.1016/j.sleh.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeifer JH, & Berkman ET (2018). The Development of Self and Identity in Adolescence: Neural Evidence and Implications for a Value-Based Choice Perspective on Motivated Behavior. Child Dev Perspect, 12(3), 158–164. doi: 10.1111/cdep.12279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman M, & Raifman J. (2020). Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. American Journal of Preventive Medicine. doi: 10.1016/j.amepre.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sequist TD (2021). Improving the Health of the American Indian and Alaska Native Population. Jama, 325(11), 1035–1036. doi: 10.1001/jama.2021.0521%JJAMA [DOI] [PubMed] [Google Scholar]
- Tang S, Xiang M, Cheung T, & Xiang YT (2021). Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J Affect Disord, 279, 353–360. doi: 10.1016/j.jad.2020.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Shih RA, Ewing B, Tucker JS, Nugroho A, & D’Amico EJ (2017). Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health and Place, 45, 39–45. doi: 10.1016/j.healthplace.2017.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, & Wolfson AR (2017). The intersection between sleep science and policy: introduction to the special issue on school start times. Sleep Health, 3(6), 419–422. doi: 10.1016/j.sleh.2017.10.001 [DOI] [PubMed] [Google Scholar]
- Varma P, Junge M, Meaklim H, & Jackson ML (2021). Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Progress in neuro-psychopharmacology & biological psychiatry, 109, 110236–110236. doi: 10.1016/j.pnpbp.2020.110236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Crow CB, Mitchell CM, & Novins DK (2012). Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. The American Journal of Drug and Alcohol Abuse, 38(5), 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR, & Carskadon MA (1998). Sleep schedules and daytime functioning in adolescents. Child Dev, 69(4), 875–887. [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, & Martin JL (2003). Evidence for the validity of a sleep habits survey for adolescents. Sleep, 26(2), 213–216. [DOI] [PubMed] [Google Scholar]
- Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, . . . Chen J-X (2020). Prevalence and socio-demographic correlates of psychological health problems in chinese adolescents during the outbreak of Covid-19. European Child & Adolescent Psychiatry. doi: 10.1007/s00787-020-01541-4 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.