Abstract
Introduction:
During the COVID-19 pandemic, online video platforms became the primary mode of accessing substance use-focused mutual-help group meetings, which may persist after in-person meetings are available again. This study examined the characteristics (demographic, substance use and recovery, and mutual-help group use) of attendees of online recovery support meetings, and associations of online meeting attendance with substance use outcomes, using national data (without ensured representativeness) collected before the pandemic.
Methods:
Data were from the Peer Alternatives in Addiction (PAL) Study of attendees of 12-step groups (e.g., Alcoholics Anonymous), Women for Sobriety (WFS), LifeRing Secular Recovery (LifeRing), and SMART Recovery (SMART). The baseline sample, collected in 2015 (pre-pandemic), was 647 adults with lifetime alcohol use disorder who were surveyed online at baseline and 6-month (81%) and 12-month follow-up (83%).
Results:
At baseline, 62% (n=402) had attended an online mutual-help group meeting in their lifetime, and 36% (n=236) had done so in the past 30 days. Bivariate analyses found that online meeting attendance was more likely among women than men, younger than older participants, and participants with more recent alcohol and drug use, and less abstinence self-efficacy. In addition, online meeting attendance was more likely among respondents who attended two or more different types of mutual-help groups (rather than just one type), and whose primary group was 12-step or WFS rather than LifeRing or SMART. Longitudinal analyses found an interaction between online meeting attendance (yes or no) and time on the outcomes of alcohol and total abstinence such that, compared to those who did not attend online meetings, online meeting attendees were less likely to be abstinent at baseline but were about the same on abstinence at 12 months. However, the interaction effect was attenuated when the model adjusted for mutual-help use characteristics.
Conclusions:
The findings inform mutual-help groups, providers, and researchers’ efforts to sustain and expand this resource by suggesting that online meeting attendance may have appeal and be helpful to mutual-help group members who are earlier in their recovery.
Keywords: mutual-help groups, alcohol use disorder, online recovery resources
1. Introduction
In response to social distancing necessitated by the COVID-19 pandemic, meetings of substance use-focused mutual-help organizations have been taking place using online video platforms instead of in person (Bergman et al., 2021). Now that use of online recovery support meetings has become routine for many mutual-help group attendees, their use may persist post-pandemic. Examining the characteristics of attendees of online recovery support meetings, and potential benefits of online meeting attendance for recovery outcomes, may inform mutual-help groups, providers, and researchers’ efforts to sustain and expand this resource (Krentzman, 2021).
Before the pandemic, use of online and in-person services was not mutually exclusive. For example, in a nationally representative sample of US adults who resolved a substance use problem, among individuals who used online digital recovery support services (which include not only online video recovery support meetings, but also discussion boards, chat rooms, and social network sites), 48% also engaged with in-person recovery support services (Bergman et al., 2018). In the same study, 4.1% of the entire sample reported lifetime participation in at least one online recovery support meeting (Bergman et al., 2018). A randomized controlled trial examining SMART Recovery meeting attendance (online and/or in person) and an online cognitive-behavioral intervention for addiction found that among the entire sample, online SMART Recovery meeting attendance was related to improved percent days abstinent from baseline to 3-month follow-up (Campbell et al., 2016; Hester et al., 2013). Online SMART Recovery attendance, however, was unrelated to changes in other drinking outcomes during this time, and unrelated to changes in drinking outcomes between 3- and 6-month follow-ups. In a narrative review of digital recovery support services, Bergman and Kelly (2021) noted that no studies to date have examined attendance or effectiveness of online recovery support meeting attendance.
The present study used data from the Peer Alternatives in Addiction (PAL) Study, which conducted longitudinal surveys of attendees of 12-step groups (e.g., Alcoholics Anonymous [AA]) and of other prevalent mutual-help options for addiction including Women for Sobriety (WFS), SMART Recovery (SMART), and LifeRing Secular Recovery (LifeRing) (Zemore et al., 2017, 2018). All participants were required to report having attended at least one in-person meeting in the 30 days prior to baseline, as in-person attendance was also a study focus. The current study examined the baseline prevalence of any lifetime and past-30 day online mutual-help group meeting attendance in the PAL Study sample. It then examined baseline demographic, substance use and recovery, and mutual-help group factors associated with past-30 day online meeting attendance.
Regarding demographic and substance use and recovery characteristics of individuals who use online support services, studies of the use of electronic health (eHealth) services (which rely on the internet to deliver health information, data, or care) in large, representative samples in the US and Europe found that women of younger age without a partner, and with higher education and income, were more likely to use eHealth services (Kontos et al., 2014; Wynn et al., 2020). However, race/ethnicity did not significantly influence eHealth use (Kontos et al., 2014; Wynn et al., 2020). These findings are consistent with a qualitative study of SMART members’ views of potentially using a digital platform for routine outcome monitoring as a standard component of this mutual-help program (Gray et al., 2020). Participants described the platform as a good fit for the SMART program, but also expressed reservations, including that adopting the technology would be difficult for older members. In a survey of participants of an online recovery social network site, respondents generally endorsed the site as helpful, particularly with respect to self-efficacy and increased motivation for abstinence and recovery (Bergman et al., 2017). Individuals who had been abstinent for one or more years, compared to those who had been abstinent for less than one year, did not differ on engagement with site activities, and the two groups reported similar levels of perceived benefit from engagement.
In addition to background and other substance use and recovery-related factors that may be associated with online mutual-help group attendance, it is also critical to explore whether factors pertaining to how individuals use mutual-help groups may be associated with online attendance. Results from the baseline survey respondents in the PAL Study suggested differences across 12-step groups and their alternatives that may be relevant to understanding online meeting attendance (Zemore et al., 2017). Compared to respondents who identified a 12-step group as their primary affiliation, those whose primary group affiliation was a 12-step alternative had lower levels of in-person meeting attendance, but equivalent activity involvement and higher levels of satisfaction and cohesion (Zemore et al., 2017). These results suggest that questions such as whether online mutual-help group attendance varies depending on amount of in-person attendance or primary group affiliation, and the extent to which online mutual-help group attendance is associated with primary group involvement, satisfaction, or cohesion, are important to answer. However, to our knowledge, no prior studies have addressed these sorts of questions.
This present study examined bivariate associations between participants’ demographic, substance use and recovery, and mutual-help group use characteristics and online meeting attendance. It then retained significant predictors in a multivariate analysis to examine baseline correlates of any online meeting attendance. Finally, because the PAL Study collected data from participants at multiple timepoints (baseline and 6- and 12-month follow-ups), this study examined the association between online mutual-help group attendance and alcohol and total abstinence over time. This study was considered to be exploratory because it was secondary to the primary PAL Study objectives and literature was not available to guide hypotheses for all analyses. In light of suggestions that eHealth services defined broadly will continue to be a growing component of health care overall as pandemic-related restrictions are eased (Oesterle et al., 2020), the present study will inform efforts to optimize post-pandemic use of online mutual-help participation.
2. Material and method
2.1. Sample and procedure
Baseline respondents (n=647) were recruited in 2015 (Zemore et al., 2017). Recruitment was conducted in collaboration with the leadership of WFS, LifeRing, and SMART. In addition, 12-step group attendees were recruited, consented, and screened by publicizing the study via paid advertisements on IntheRooms, an online meeting hub for those in recovery with a 12-step focus. All participants were required to be at least 18 years old and a US resident, and report having attended at least one in-person 12-step, WFS, LifeRing, or SMART meeting for alcohol and/or drug use in the past 30 days, and a lifetime alcohol use disorder (AUD). Lifetime AUD was determined using a subset of CIDI items that were selected to address each of the DSM-5 criteria (see Zemore et al., 2017). Only participants who were screened and met these criteria had access to the baseline online survey. Follow-up surveys were conducted 6 months (81% response rate) and 12 months (83%) later. Minor baseline differences were identified between participants who were followed or not followed at 6- and 12-month follow-ups (Zemore et al., 2018). Specifically, participants with a higher lifetime AUD symptom count were more likely to be followed at 6 months. In addition, in comparison to White participants, Black participants were less likely, and Latino/Hispanic participants were more likely, to be followed at 12 months. Further, unemployed participants were less likely to be followed at 12 months than participants in other employment categories.
2.2. Measures
2.2.1. Mutual-help group meeting attendance
All participants were asked to report whether they had attended any online meetings, and whether they had attended any in-person meetings, for the groups of 12-step, SMART, LifeRing, and WFS, for an alcohol or drug problem of their own. The reports were asked with regard to participants’ lifetime (baseline survey only) and in the past 30 days (all assessments). Questions also solicited the number of online mutual-help meetings, and the number of in-person mutual-help meetings, participants attended (if any) for both lifetime and the past 30 days. Responses were used to create indicators of any (and number of) online and in-person mutual-help group meetings attended lifetime and in the past 30 days.
2.2.2. Demographic characteristics
Respondents’ demographic characteristics assessed at baseline were gender, age, race/ethnicity (white, Black/African-American, Latino/Hispanic, other), marital status (not married or married/partnered), education (high school graduate, college graduate, post-college), employment status (unemployed, student or otherwise not in the workforce, employed), annual household income, and urbanicity (urban, suburban, rural). Demographic characteristics of the sample are in Table 1. The sample was predominantly female, white, married or partnered, college educated, employed, and suburban. The mean age was 51.3 years old (SD=12.2; range = 21–80).
Table 1.
Full sample baseline demographic characteristics and correlates of online mutual-help group attendance in the past 30 days
| Full sample | Any online attendance | |||
| n (%) | n (%) | X2 (p) | ||
|
|
|
|||
| Gender | 15.86 (<.001) | |||
| Female | 418 (64.8) | 176 (42.1) | ||
| Male | 228 (35.2) | 60 (26.3) | ||
| Race/Ethnicity | 6.94 (.074) | |||
| White | 593 (92.2) | 211 (35.6) | ||
| Black/African-American | 12 (1.9) | 7 (58.3) | ||
| Hispanic | 25 (3.9) | 14 (56.0) | ||
| Other | 13 (2.0) | 4 (30.78) | ||
| Marital Status | .638 (.424) | |||
| Not married | 310 (48.1) | 118 (38.1) | ||
| Married/partnered | 334 (51.9) | 117 (35.0) | ||
| Education | 2.62 (.269) | |||
| High school graduate | 192 (29.8) | 74 (31.5) | ||
| College graduate | 255 (39.5) | 98 (38.4) | ||
| Post-college | 198 (30.7) | 63 (31.8) | ||
| Employment status | 2.34 (.309) | |||
| Unemployed | 51 (7.9) | 23 (45.1) | ||
| Student, not in workforce | 199 (30.9) | 67 (33.7) | ||
| Employed | 395 (61.2) | 146 (37.0) | ||
| Annual income | 4.62 (.201) | |||
| $30,000 or less | 159 (25.6) | 62 (39.0) | ||
| $30,001–$60,000 | 156 (25.1) | 64 (41.0) | ||
| $60,001–$100,000 | 131 (21.1) | 45 (34.3) | ||
| $100,000 or more | 176 (28.3) | 54 (30.7) | ||
| Urbanicity | 4.17 (.124) | |||
| Urban | 237 (36.7) | 83 (35.0) | ||
| Suburban | 289 (44.8) | 99 (34.3) | ||
| Rural | 119 (18.5) | 53 (44.5) | ||
| Full sample | Any online attendance | No online attendance | ||
| M (SD) | M (SD; n=236) | M (SD; n=410) | t (p) | |
| Age | 51.3 (12.2) | 48.56 (12.79) | 52.88 (11.60) | 4.38 (<.001) |
Note: Chi-square and t-test statistics report comparisons of participants with or without any online mutual-help group attendance in the past 30 days at baseline.
2.2.3. Substance use and recovery characteristics
These baseline characteristics include recency of alcohol and drug use, alcohol recovery goal, alcohol use severity, alcohol problems, and alcohol abstinence self-efficacy. Descriptive statistics for the full sample are in Table 2.
Table 2.
Full sample baseline substance use and recovery characteristics and correlates of online mutual-help group attendance in the past 30 days
| Full sample | Any online attendance | |||
| n (%) | n (%) | X2 (p) | ||
|
|
|
|||
| Recency of alcohol use | 14.22 (.003) | |||
| Within past 30 days | 145 (22.5) | 64 (44.1) | ||
| 30 days to 1 year ago | 161 (25.0) | 71 (44.1) | ||
| 1 to 5 years ago | 171 (26.5) | 51 (29.8) | ||
| 5 or more years ago | 168 (26.1) | 50 (29.7) | ||
| Recency of drug use | 15.78 (.003) | |||
| Within past 30 days | 64 (9.9) | 25 (39.1) | ||
| 30 days to 1 year ago | 110 (17.1) | 55 (50.0) | ||
| 1 to 5 years ago | 148 (23.0) | 59 (39.9) | ||
| 5 or more years ago | 240 (37.3) | 71 (29.6) | ||
| Never | 82 (12.7) | 25 (39.5) | ||
| Alcohol recovery goal | .12 (.726) | |||
| Total abstinence forever | 388 (60.9) | 144 (37.1) | ||
| Drink alcohol after abstinent period or occasionally | 249 (39.1) | 89 (35.7) | ||
| Full sample | Any online attendance | No online attendance | ||
| M (SD) | M (SD; n=236) | M (SD; n=410) | t (p) | |
| Alcohol: | ||||
| Use severity | 3.56 (4.4) | 4.76 (4.61) | 2.86 (4.09) | −5.43 (<.001) |
| Problems | .33 (.40) | .42 (.40) | .27 (.37) | −4.85 (<.001) |
| Self-efficacy | 78.6 (22.0) | 74.01 (24.02) | 81.24 (20.32) | 4.06 (<.001) |
Note: Chi-square and t-test statistics report comparisons of participants with or without any online mutual-help group attendance in the past 30 days at baseline.
For recency of alcohol use and of drug use (i.e., illegal drugs, legal drugs not taken as prescribed, marijuana), response options were: within the past 30 days, 30 days to 1 year ago, 1 to 5 years ago, and more than 5 years ago. Drug use recency included the response option of never. As seen on Table 2, about one-quarter of the sample had used alcohol within the past 30 days, from 30 days to 1 year ago, from 1 to 5 years ago, and more than 5 years ago. Most of the respondents had not used drugs for at least one year.
Current alcohol recovery goal was assessed using a single item (Hall et al., 1991) asking respondents to select one recovery goal among five that was most true for them, ranging from total lifetime abstinence to controlled use. Responses were dichotomized into two categories: endorsement of total lifetime abstinence (“I want to quit using alcohol once and for all, to be totally abstinent, and never use alcohol ever again for the rest of my life”) or another goal. The majority of participants had a recovery goal of lifetime abstinence from alcohol (Table 2).
Alcohol use severity was assessed using an adaptation of the alcohol section of the CIDI (World Health Organization, 1993) comprised of 18 items addressing the 11 criteria for a DSM-5 AUD diagnosis (American Psychiatric Association, 2013). The DSM-5 assumes a single, unidimensional construct. Scores of 2–3 symptoms indicate mild AUD, 4–5 moderate AUD, and 6 or more severe AUD. The mean alcohol use severity score was 3.56 (SD=4.4; range = 0 to 11).
The Short Index of Alcohol Problems (SIP; Feinn et al., 2003) was derived from the Drinker Inventory of Consequences (DrInc; Alterman et al., 2009; Miller et al., 1995) assessing physical, intrapersonal, interpersonal, social role, and impulse control problems (α=.88). Respondents were provided 15 events that people who drink alcohol sometimes experience, and reported whether each event had ever happened to them (no or yes). The number of events that occurred was averaged. The mean SIP score was .33 (SD=0.40).
Alcohol abstinence self-efficacy was assessed with the Brief Situational Confidence Questionnaire (Annis & Graham, 1988; Breslin et al., 2000) (BSCQ). For each of 8 situations, respondents rated their confidence in being able to resist drinking heavily (0=not at all confident; 100= totally confident; α=.92); item responses were averaged. The full sample’s mean was 78.6 (SD=22.0; range=0 to 100).
2.2.4. Mutual-help group use characteristics
The baseline survey assessed characteristics related to how participants used mutual-help groups in the past 30 days. Sample statistics on these characteristics are on Table 3.
Table 3.
Full sample baseline mutual-help group use characteristics and correlates of online mutual-help group attendance in the past 30 days
| Full sample | Any online attendance | |||
| n (%) | n (%) | X2 (p) | ||
| Use of mutual-help groups: | 15.82 (<.001) | |||
| 1 type | 464 (72.3) | 146 (31.45) | ||
| 2 or more types | 178 (27.7) | 86 (48.3) | ||
| Primary group | 32.07 (<.001) | |||
| 12-Step | 208 (32.2) | 101 (48.6) | ||
| LifeRing | 98 (15.2) | 21 (21.4) | ||
| SMART Recovery | 166 (25.7) | 43 (25.9) | ||
| Women for Sobriety | 174 (26.9) | 71 (40.8) | ||
| Full sample | Any online attendance | No online attendance | ||
| M (SD) | M (SD; n) | M (SD; n) | t (p) | |
| No. in-person mtgs | 10.1 (18.3) | 11.50 (18.41) | 9.22 (18.18) | −1.53 (.127) |
| Primary group | ||||
| Involvement | .64 (.28) | .60 (.30) | .66 (.25) | 2.66 (.008) |
| Satisfaction | 8.61 (1.9) | 2.05 (8.43) | 8.71 (1.72) | 1.82 (.069) |
| Cohesion | 4.2 (.8) | 4.12 (.90) | 4.24 (.75) | 1.76 (.077) |
Note: Chi-square and t-test statistics report comparisons of participants with or without any online mutual-help group attendance in the past 30 days at baseline.
Number of in-person meetings.
Participants who attended various types of mutual-help groups were asked how many in-person meetings they attended in the past 30 days. The number of meetings attended was tallied across different group types (12-step, LifeRing, SMART, WFS) to create a variable representing the total number of in-person meetings attended (Mean=10.1, SD=18.3, Range=0–290).
Use of two or more mutual-help groups in the past 30 days.
Based on respondents’ reports regarding how many meetings they had attended (in-person or online) in the past 30 days, an indicator was created of whether participants had attended only one type of group or 2 or more different types of groups. In the full sample, most attended only one type of group (Table 3).
Primary group.
The study collected information on participants’ primary mutual-help group. For participants who reported in-person attendance at only one group, that group was coded as their primary group. For participants who attended multiple groups in person, the survey requested that they identify their primary group. In the full sample (see Table 3), respondents’ primary group was 12-step (32.2%), WFS (26.9%), SMART Recovery (25.7%), and LifeRing (15.2%).
Primary group involvement.
The survey collected information on how involved participants were with their primary group (Humphreys et al., 1998). Participants completed four yes/no questions measuring involvement, with different wording for 12-step groups and the alternatives, e.g., “home group” (12-step) or “regular group” (alternative). An aggregate, 5-item measure of primary group involvement was created by averaging across activities (recoding yes=1 and no=0) and meeting attendance (recoded using group-specific quartile splits, where cut-points were drawn from the attendance distribution for those indicating that group as their primary group). Baseline α’s=.90-.93 across groups. The mean involvement score was .64 (SD=.28; range = 0 to 1).
Primary group satisfaction.
Satisfaction with the primary group was assessed with a single item that respondents rated on a scale from 0 (not at all satisfied) to 10 (completely satisfied) as to how satisfied they were with their experiences in their primary group. The mean satisfaction score was 8.6 (SD=1.9; range=0 to 10).
Primary group cohesion.
Perceived cohesion in the primary group was assessed using the Cohesion Subscale of the Curative Climate Instrument (CCI), with slight wording changes to ensure applicability to mutual-help groups (Fuhriman et al., 1986; Yalom, 1975). Participants reported, on a 1 (not at all) to 5 (extremely) scale, the extent to which they felt, for example, that they belonged to and were valued by the group. Responses were averaged (mean=4.2, SD=0.8, range=1 to 5, baseline α=.93).
Longitudinal outcomes
Alcohol and total abstinence.
Each survey asked when the respondent had last used alcohol, and when the respondent had last used drugs (illegal drugs, legal drugs not taken as prescribed, marijuana or cannabis). Respondents who had not used alcohol during the past 30 days were classified as abstinent from alcohol; 77.4%, 80.8%, and 83.0% were abstinent from alcohol at baseline, 6-month follow-up, and 12-month follow-up, respectively. Respondents who had not used alcohol or drugs during the past 30 days were classified as having total abstinence; 72.6%, 77.8%, and 79.1% were totally abstinent at baseline, 6-month follow-up, and 12-month follow-up, respectively.
2.4. Analysis
To identify correlates of any online mutual-help group meeting attendance, baseline differences on demographic, substance use and recovery, and mutual-help group use characteristics between respondents who did or did not attend online meetings in the past 30 days were tested with chi-square tests and Student’s t-tests. Significant demographic, substance use and recovery, and mutual-help group use correlates of online attendance in the past 30 days were then examined in a simultaneous logistic regression model to assess the relative strength of these factors. Wald tests were used to examine the significance of categorical variables.
To examine the associations between online mutual-help group attendance in the past 30 days and both alcohol abstinence and total abstinence, the study used a generalized estimating equation (GEE) approach. This approach is commonly used in longitudinal data analysis because models can account for within-participant non-independence of observations (i.e., nesting or clustering) across multiple waves of data collection. Specifically, models first predicted alcohol and total abstinence by time point (categories of baseline [reference], 6-month, and 12-month interviews), online mutual-help group attendance in the past 30 days (yes or no), and the interaction of time point by online attendance. Time was modeled as a categorical rather than a continuous variable to more precisely identify when changes in abstinence occurred at follow-up. Then, the models included the same predictors while adjusting for the characteristics found to be associated with online mutual-help group attendance at baseline.
3. Results
At baseline, 62% (n=402) of the sample had attended an online mutual-help group meeting in their lifetime (mean number of meetings=92.9 and SD=465.3 among those who attended), and 36% (n=236) had done so in the past 30 days (mean number of meetings=14.1 and SD=29.6 among those who attended).
3.1. Demographic correlates of online mutual-help group meeting attendance
Tests conducted to examine bivariate associations of gender, race/ethnicity, marital status, education, employment status, income, and urbanicity with any online meeting attendance in the past 30 days found that online attendance was less likely among men than women (Table 1). In addition, respondents with online meeting attendance were younger than those without. Otherwise, respondents’ demographic characteristics were not associated with whether or not they attended mutual-help group meetings online.
3.2. Substance use and recovery correlates of online mutual-help group meeting attendance
Results of tests to examine baseline substance use and recovery characteristics associated with past-30-day online meeting attendance are on Table 2. Regarding recency of alcohol use, use within the past 30 days, and from 30 days to 1 year ago, were associated with higher odds of online meeting attendance in comparison to having used alcohol 1 to 5, and 5 or more, years ago. Regarding recency of drug use, use within the past 30 days to 1 year was associated with greater odds of online meeting attendance compared to having used drugs 5 or more years ago or never. In addition, use from 1 to 5 years ago was associated with greater odds of online meeting attendance compared to having used drugs 5 or more years ago. Alcohol recovery goal was unrelated to online meeting attendance. In comparison to those who did not attend online meetings, those who did had greater alcohol use severity and alcohol problems, and less alcohol abstinence self-efficacy.
3.3. Mutual help group use correlates
Use of multiple mutual-help groups was associated with increased odds of online meeting attendance. In addition, primary mutual-help group affiliation of 12-step and WFS was associated with increased odds of online attendance compared to primary group affiliation of LifeRing and SMART. Further, primary group involvement was lower among respondents with online meeting attendance. In contrast to these significant results, the number of in-person mutual-help group meetings, and primary group satisfaction and cohesion, were unrelated to likelihood of online meeting attendance.
3.4. Multivariate analysis
Baseline variables that were associated with online mutual-help group meeting attendance in the past 30 days (gender; age; recency of alcohol and of drug use; alcohol use severity, problems, and abstinence self-efficacy; use of multiple mutual-help groups; primary group, and primary group involvement) were entered in a simultaneous logistic regression model to assess their relative strength (Table 4). In this analysis, two mutual-help group use characteristics were associated with online meeting attendance: use of more than one type of mutual-help group, and primary group affiliation; that is, online attendance was more likely among 12-step than among 12-step alternative primary group affiliates.
Table 4.
Multivariable model examining correlates of online mutual-help group attendance in the past 30 days
| aOR | 95% CI | p | ||
|---|---|---|---|---|
|
|
||||
| Gender | ||||
| Female (Ref) | ||||
| Male | 0.73 | [0.47, 1.13] | 0.162 | |
| Age | 0.99 | [0.97, 1.01] | 0.179 | |
| Recency of Alcohol Use | ||||
| Within past 30 days | ||||
| 30 days to 1 year ago | 0.96 | [0.55, 1.67] | 0.877 | |
| 1 to 5 years ago | 1.02 | [0.40, 2.59] | 0.970 | |
| 5 or more years ago | 1.33 | [0.51, 3.46] | 0.557 | |
| Wald test | 0.830 | |||
| Alcohol Use Severity | 1.09 | [0.98, 1.22] | 0.122 | |
| Alcohol Problems | 0.93 | [0.21, 4.14] | 0.929 | |
| Recency of Alcohol Use | ||||
| Within past 30 days | ||||
| 30 days to 1 year ago | 1.53 | [0.75, 3.14] | 0.242 | |
| 1 to 5 years ago | 1.77 | [0.85, 3.69] | 0.124 | |
| 5 or more years ago | 0.95 | [0.47, 1.93] | 0.893 | |
| Never | 0.92 | [0.42, 2.01] | 0.836 | |
| Wald test | 0.146 | |||
| Abstinence self-efficacy | 1.00 | [0.99, 1.01] | 0.440 | |
| Use of Multiple (2 or more) Groups | 2.18 | [1.47, 3.22] | 0.000 | |
| Primary Group | ||||
| 12-Step (Ref) | ||||
| LifeRing | 0.25 | [0.13, 0.48] | 0.000 | |
| SMART | 0.32 | [0.20, 0.54] | 0.000 | |
| WFS | 0.58 | [0.36, 0.94] | 0.026 | |
| Wald test | <0.001 | |||
| Primary Group Involvement | 0.87 | [0.46, 1.62] | 0.654 | |
3.5. Longitudinal analysis
When GEE was used to predict alcohol abstinence from time, online mutual-help group meeting attendance (38% had attended online at 6 months, 32% at 12 months), and their interaction, there was a significant effect for online meeting attendance such that attendance was associated with a lower likelihood of abstinence from alcohol (see Table 5, Alcohol Model 1). In addition, there was a significant time by online attendance interaction showing that, at baseline, those with online attendance had a lower likelihood of alcohol abstinence than those without, and increased odds of abstinence from baseline to 6-month follow-up, but the two groups were comparable by the 12-month follow-up (see Figure 1). When the baseline mutual-help group use characteristics of multiple group types and primary group affiliation were also entered as predictors, the effect for online attendance held but the interaction did not (see Table 5, Alcohol Model 2). These findings were replicated when GEE was used to predict total abstinence (see Table 5, Total Model 1 and Total Model 2).
Table 5.
Models predicting alcohol and total abstinence in the past 30 days
| Alcohol Model 1 | Alcohol Model 2 | |||||
| aOR | 95% CI | p | aOR | 95% CI | p | |
|
|
|
|||||
| Time | ||||||
| Baseline (Ref) | ||||||
| 6 months | .91 | .69,1.20 | .505 | 1.05 | .77,1.43 | .766 |
| 12 months | 1.11 | .84,1.47 | .448 | 1.26 | .91,1.73 | .159 |
| Online attendance | .62 | .44,.86 | .004 | .59 | .41,.85 | .039 |
| Interaction Time*Attendance | ||||||
| Baseline (Ref) | ||||||
| 6 months | 1.78 | 1.13,2.82 | .014 | 1.73 | 1.03,2.89 | .039 |
| 12 months | 1.58 | .98,2.56 | .061 | 1.44 | .83,2.50 | .196 |
| Wald test | .033 | .104 | ||||
| Use of >2 groups | 1.21 | .88,1.66 | .242 | |||
| Primary group | ||||||
| 12-step (Ref) | ||||||
| LifeRing | 1.00 | .58,1.72 | .990 | |||
| SMART | .50 | .34,.74 | .001 | |||
| WFS | .64 | .43,.96 | .030 | |||
| Wald test | .002 | |||||
| Total Model 1 | Total Model 2 | |||||
| aOR | 95% CI | p | aOR | 95% CI | p | |
|
|
|
|||||
| Time | ||||||
| Baseline (Ref) | ||||||
| 6 months | 1.00 | .77,1.30 | .997 | 1.15 | .85,1.54 | .364 |
| 12 months | 1.18 | .91,1.54 | .219 | 1.26 | .94,1.70 | .127 |
| Online attendance | .62 | .45,.85 | .003 | .62 | .44,.87 | .005 |
| Interaction Time*Attendance | ||||||
| Baseline (Ref) | ||||||
| 6 months | 1.75 | 1.12,2.72 | .013 | 1.61 | .99,2.63 | .057 |
| 12 months | 1.43 | .90,2.25 | .126 | 1.31 | .79,2.19 | .297 |
| Wald test | .041 | .125 | ||||
| Use of >2 groups | 1.17 | .309 | ||||
| Primary group | ||||||
| 12-step (Ref) | ||||||
| LifeRing | 1.19 | .72,1.96 | .503 | |||
| SMART | .59 | .41,.84 | .004 | |||
| WFS | .78 | .54,1.12 | .178 | |||
| Wald test | .008 | |||||
Figure 1.
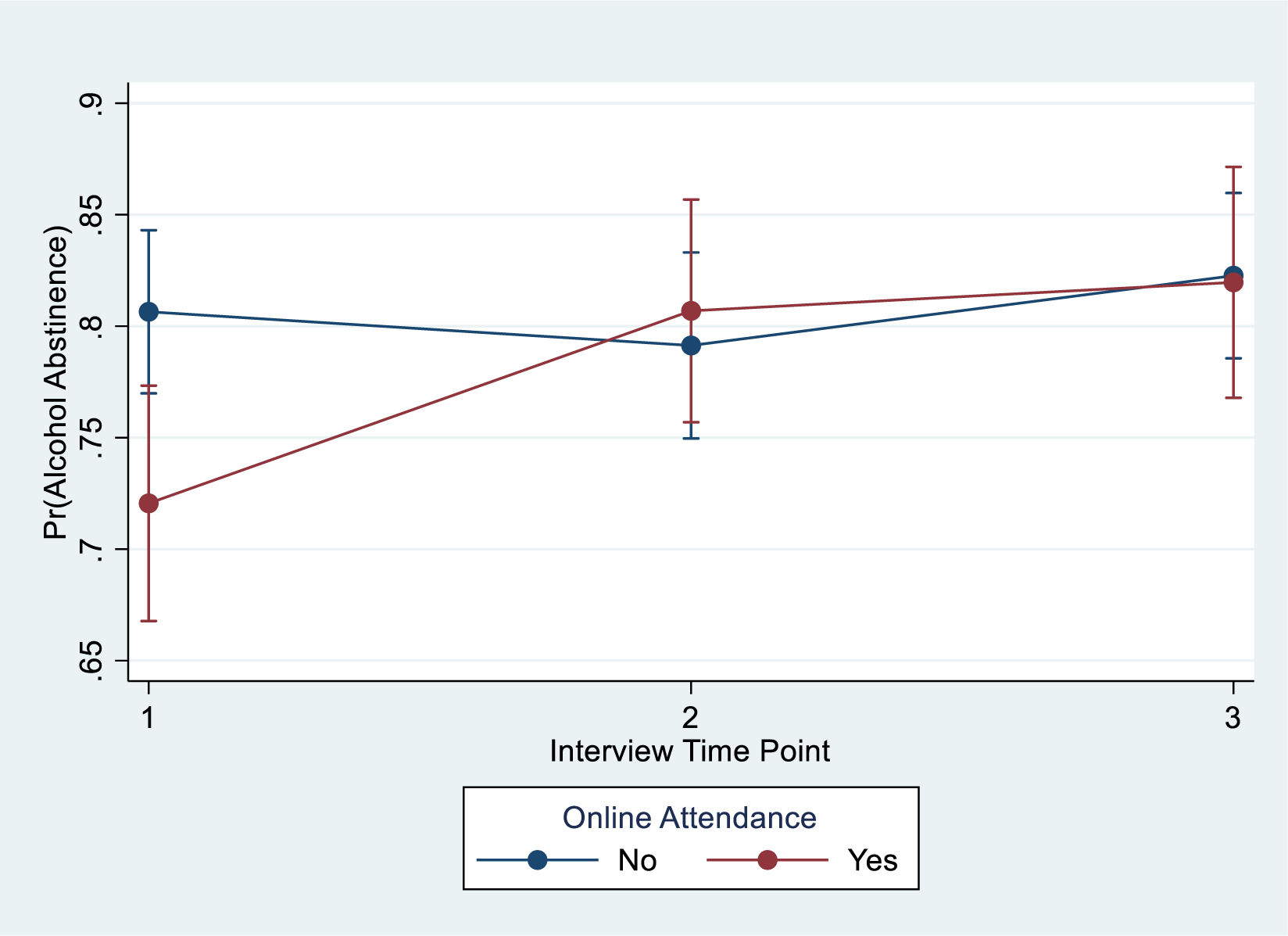
Alcohol Abstinence by Attendance over Time with 95% Cls
4. Discussion
This study found that, prior to the COVID-19 pandemic, online attendance at mutual-help groups was common among in-person attendees of these groups. About two-thirds of PAL Study participants, all of whom had attended mutual-help groups in person, had also attended meetings online prior to the baseline assessment, and about one-third had done so in the past month. Online meeting attendance was more likely among women and respondents who were younger (Gray et al., 2020; Kontos et al., 2014; Wynn et al., 2020), had used alcohol and drugs more recently, and whose alcohol use was more severe and problematic. Consistent with these results, online meeting attendees felt less efficacious at baseline about maintaining abstinence from alcohol use than those attending meetings only in person, and also used more than one type of mutual-help group for support. Also consistent with these results, longitudinal analyses that did not consider number and type of mutual-help group affiliation found that online meeting attendees were less likely to be abstinent at baseline, but were comparable to in-person-only attendees on abstinence up to one year later.
Although findings will need to be confirmed post-pandemic, they suggest that online meeting attendance may be a beneficial adjunct to in-person mutual-help group attendance that is sought out by people who are newer to recovery and in more need of support. Similar to our findings at baseline, a study of Sober Grid, a recovery social network smartphone application (app), found that clients who used the check-in feature more often were more likely to have shorter sobriety lengths and a greater number of relapses; that is, were at greater risk and required more assistance (Ashford et al., 2020). Similar to online meeting attendance, check-ins allowed clients to provide feedback on how they were feeling, what they were doing for their recovery, and, in the circumstances of a relapse, describe emotional triggers they had experienced. On average, Sober Grid clients had less than a year of sobriety, suggesting digital recovery resources may be most engaging for those in early remission.
The same study also suggested that Sober Grid may foster social connection and reduce loneliness for female clients (Ashford et al., 2020), which is consistent with our finding that women were more likely than men to attend mutual-help group meetings online. In addition, PAL Study participants who affiliated primarily with WFS, the only active 12-step alternative that is exclusively for women (Zemore et al., 2017), were more likely to attend online meetings than those who affiliated primarily with LifeRing or SMART. A survey of US adults also found that women were more likely than men to have ever or recently engaged in health-seeking behaviors on the internet and to possess a health-related app, and concluded that women tend to approach health issues by using several sources, and often use the internet on the advice of healthcare providers, family, and friends (Escoffery, 2018). To widen the reach of online services, healthcare providers, researchers, and mutual-help group members could introduce and highlight the use of online recovery resources among men and among older persons in particular. Such endorsement could occur during in-person meetings, as we found comparable in-person meeting attendance between those who did and did not attend meetings online. Bergman and Kelly (2021) and Krentzman (2021) recommended that when making referrals to digital recovery support services or online recovery meetings, stakeholders should familiarize themselves with potential benefits (e.g., greater anonymity) and drawbacks (e.g., less social and emotional connection, technical difficulties) of such participation, based on empirical evidence. Additional studies are warranted to understand the specific needs of different demographic groups as to how to engage them in online recovery practices.
To guide future studies, Bergman and Kelly (2021) proposed a preliminary conceptual model of associations of utilization of social-online digital recovery support services with substance use outcomes over time. In the model, initial experiences with these services foster a sense of shared experience and hope (D’Agostino et al., 2017), which in turn encourages continued online participation. This participation then enables supportive social network changes and positive expectancies and skills, such as abstinence self-efficacy, which this study found to be relatively lacking among online meeting attendees at baseline. In turn, these mechanisms are associated with better substance use and health outcomes and overall well-being. In related work, an expansion of the PAL Study is now underway (funded by NIAAA, Dr. Zemore, PI) to test associations between online mutual-help group participation and substance use outcomes over time, identify causal mechanisms underlying the benefits of participation, and examine the moderating effects of primary group affiliation. The results will help to identify both online and in-person drivers of recovery that can be targeted in designing and testing interventions to help with alcohol use disorders.
4.1. Limitations
One limitation is that the study could not establish a baseline response rate and completely ensure the representativeness of the mutual-help group samples (Zemore et al., 2017). Because it was impossible to establish a baseline denominator or to compare baseline responders to non-responders, sample selection biases cannot be ruled out. The sample may be biased because all surveys were completed online, and the study used a 12-step sample that was recruited online (12-step traditions do not agree with direct participation in research). Thus, the sample may have been relatively knowledgeable about or comfortable with using online resources compared to mutual-help group members generally, which limits generalizability of the findings. Another concern was the fact that participants were combined across 12-step programs; members of these programs differ on demographic, clinical, and other characteristics, and the programs vary on size and meeting availability.
We chose to dichotomize online meeting attendance instead of examining the number of meetings attended. Any attendance versus none -- of mutual-help groups (e.g., Bergman et al., 2019; Glass JE et al., 2017) or of treatment (e.g., Dale et al., 2011; Milward et al., 2014) -- is a common outcome or predictor of outcome in substance use studies because dichotomization enables the identification of potentially modifiable factors to impact attendance and possibly improve outcomes. Even so, number of meetings attended online should be considered in future studies. In addition, longitudinal analyses controlled for correlates of online attendance rather than correlates of abstinence, and thus more research is needed to consider these sets of correlates of abstinence simultaneously. Finally, in order to inform referrals to online meetings, we conducted multiple statistical tests without adjustment in this exploratory study. Specifically, we did not apply a Bonferroni correction because, although it would control for false positive associations, it would also increase the risk of generating false null associations.
Together, these limitations again point to the need for additional studies to follow-up on these pre-pandemic observations, such as the PAL Study expansion. One purpose of the expansion study is to examine racial and ethnic differences in modes of mutual-help group participation and benefits, for which the present sample was not fully sufficient. Specifically, the “digital divide” affects individuals from racial and ethnic minorities who are already underserved, and were less likely to receive substance use care during the pandemic (Busch et al., 2021).
4.2. Conclusion
According to Bergman and Kelly (2021), emerging data suggest that when in-person treatment and recovery support services are limited, such as during the COVID-19 pandemic, providers and other stakeholders may refer individuals with current and remitted substance use disorders to digital recovery support services. The present study further suggests that online mutual-help group attendance, even when in-person meetings become available again, may appeal to and benefit people who are relatively early in recovery. Possibly, online meetings facilitate mutual-help group participation among those newer to recovery because they are convenient to attend (no travel required), facilitate “shopping around” different groups for those that fit, and enable more frequent attendance across more types of meetings. As noted by Kelly et al. (2021), although the infrastructure to deliver online meetings was further developed during the pandemic, as social distancing requirements are lessened, in-person mutual-help group meetings are returning. As in-person meetings return, the patterns and benefits of online meetings may differ depending on unique features of the mutual-help programs in which they are utilized (Oesterle et al., 2020). The present findings, along with the growing body of literature examining online resources use and outcomes, will assist in the development of clinical practice guidelines related to online, in-person, and hybrid services.
Figure 2.
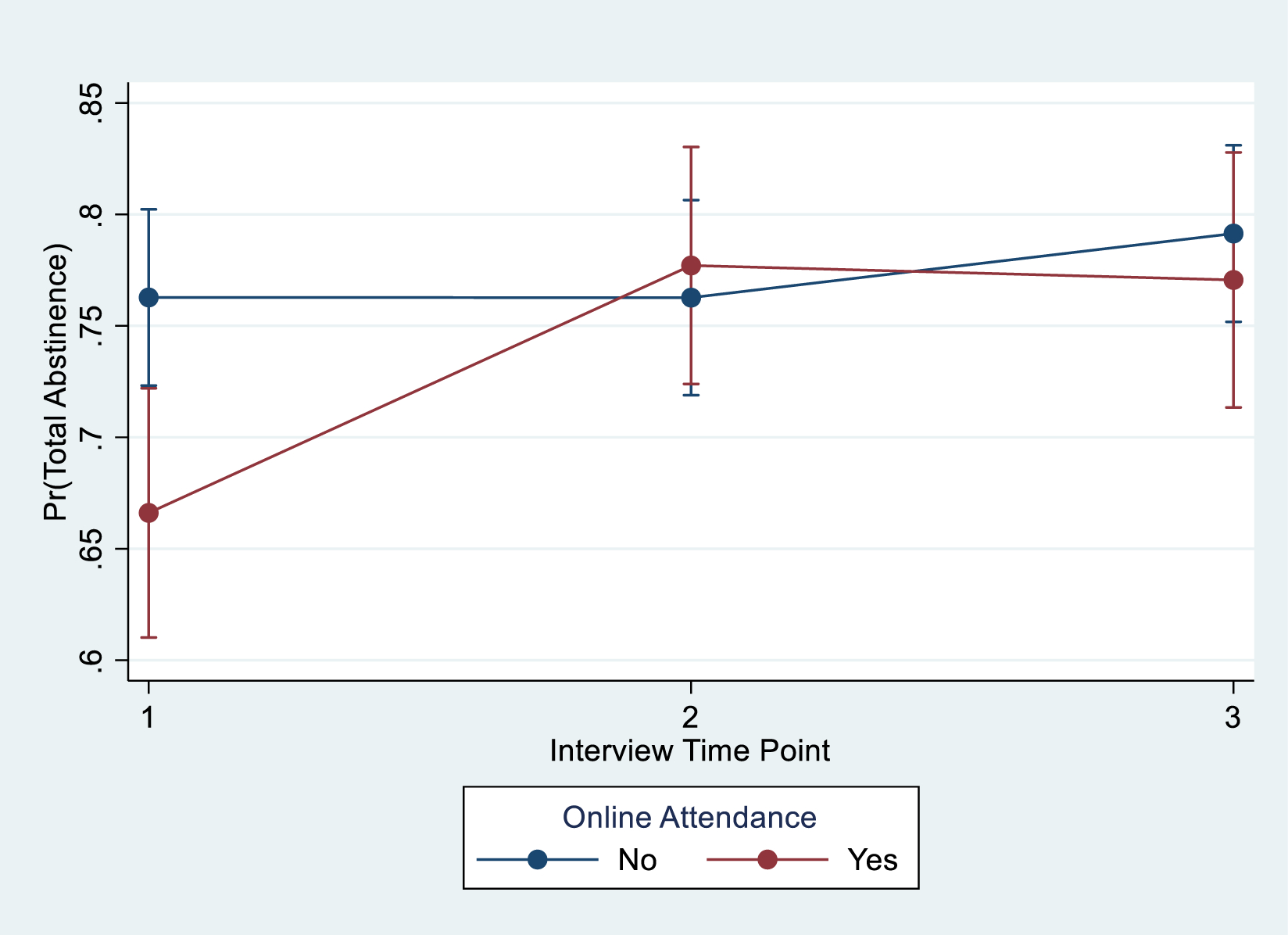
Total Abstinence by Attendance over Time with 95% Cls
Highlights.
Mutual-help members with alcohol use disorder were surveyed (baseline, follow-ups).
At baseline, online attendance was reported by 62% (lifetime) and 36% (past 30 days).
Women, younger, and new-recovery members were more likely to attend meetings online.
12-step and Women for Sobriety (vs. LifeRing, SMART) members attended online.
Online meeting attendance may beneficially assist in-person attendance post-pandemic.
Acknowledgements
We are very grateful for the important contributions of collaborators in implementing this research, including Becky Fenner (Executive Director for Women for Sobriety); Byron Kerr and Robert Stump (Board Chair and Executive Director of LifeRing, respectively); Tom Horvath and Shari Allwood (President and Executive Director of SMART, respectively); Ronald Tannebaum and Kenny Pomerance (Co-Founders of IntheRooms.com); Shelley Osborn and Deborah Krug (the project management team at ICF International), and Deidre Patterson (Research Associate of the Alcohol Research Group).
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health (R21AA022747 and R01AA027920 to Dr. Zemore) and by the Department of Veterans Affairs, Health Services Research and Development Service (RCS 00-001 to Dr. Timko). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Department of Veterans Affairs.
Footnotes
Conflicts of interest: None
CRediT author statement
Christine Timko: Conceptualization, Methodology, Writing – Original Draft, Writing – Review & Editing, Funding Acquisition, Supervision
Amy Mericle: Conceptualization, Methodology, Writing – Original Draft, Writing – Review & Editing, Formal Analysis
Lee Ann Kaskutas: Conceptualization, Methodology, Writing – Original Draft, Funding Acquisition
Priscilla Martinez: Conceptualization, Methodology, Project administration
Sarah Zemore: Conceptualization, Methodology, Writing – Original Draft, Writing – Review and Editing, Funding Acquisition, Project administration
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alterman AI, Cacciola JS, Ivey MA, Habing B, & Lynch KG (2009). Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. Journal of Studies on Alcohol and Drugs, 70, 304–307. 10.15288/jsad.2009.70.304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM- 5). 10.1176/appi.books.9780890425596 [DOI]
- Annis HM, & Graham JM (1988). Situational Confidence Questionnaire (SCQ-39) User’s Guide. Addiction Research Foundation. [Google Scholar]
- Ashford RD, Giorgi S, Mann B, Pesce C, Sherritt L, Ungar L, & Curtis B (2020). Digital recovery networks: Characterizing user participation, engagement, and outcomes of a novel recovery social network smartphone application. Journal of Substance Abuse Treatment, 109, 50–55. doi: 10.1016/j.jsat.2019.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman BG, Ashford RD, & Kelly JF (2019). Attitudes toward opioid use disorder medications: Results from a U.S. national study of individuals who resolved a substance use problem. Experimental and Clinical Psychopharmacology. 10.1037/pha0000325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman BG, Claire GM, Hoeppner BB, & Kelly JF (2018). Expanding the reach of alcohol and other drug services: Prevalence and correlates of US adult engagement with online technology to address substance problems. Addictive Behaviors, 87, 74–81. DOI: 10.1016/j.addbeh.2018.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman BG, & Kelly JF (2021). Online digital recovery support services: An overview of the science and their potential to help individuals with substance use disorder during COVID-19 and beyond. Journal of Substance Abuse Treatment, 120, 108152 doi: 10.1016/j.jsat.2020.108152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman BG, Kelly JF, Fava M, & Eden EA (2021). Online recovery support meetings can help mitigate the public health consequences of COVID-19 for individuals with substance use disorder. Addictive Behaviors,113, 106661. doi: 10.1016/j.addbeh.2020.106661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman BG, Kelly NW, Hoeppner BB, Vilsaint CL, & Kelly JF (2017). Digital recovery management: Characterizing recovery-specific social network site participation and perceived benefit. Psychology of Addictive Behaviors, 31, 506–512. doi: 10.1037/adb0000255. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Sobell LC, Sobell MB, & Agrawal S (2000). A comparison of a brief and long version of the Situational Confidence Questionnaire. Behavior Research and Therapy, 38, 1211–1220. doi: 10.1037/adb0000255 [DOI] [PubMed] [Google Scholar]
- Busch AB, Sugarman DE, Horvitz LE, & Greenfield SF (2021). Telemedicine for treating mental health and substance use disorders: Reflections since the pandemic. Neuropsychopharmacology, 46, 1068–1070. doi: 10.1038/s41386-021-00960-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell W, Hester RK, Lenberg KL, & Delaney HD (2016). Overcoming Addictions, a web-based application, and SMART Recovery, an online and in-person mutual help group for problem drinkers, part 2: Six-month outcomes of a randomized controlled trial and qualitative feedback from participants. Journal of Medical Internet Research, 18, e262. doi: 10.2196/jmir.5508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Agostino AR, Optican AR, Sowles SJ, Krauss MJ, Escobar LK, & Cavazos-Rehg PA (2017). Social networking online to recover from opioid use disorder: A study of community interactions. Drug and Alcohol Dependence, 181, 5–10. doi: 10.1016/j.drugalcdep.2017.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale V, Coulton S, Godfrey C, Copello A, Hodgson R, Heather N, Orford J, Raistrick D, Slegg G, & Tober G (2011). Exploring treatment attendance and its relationship to outcome in a randomized controlled trial of treatment for alcohol problems: Secondary analysis of the UK Alcohol Treatment Trial (UKATT). Alcohol and Alcoholism, 46, 592–599. Doi: 10.1093/alcalc/agr079 [DOI] [PubMed] [Google Scholar]
- Escoffery C (2018). Gender similarities and differences for e-health behaviors among U.S. adults. Telemedicine and e-Health, 24. doi: 10.1089/tmj.2017.0136 [DOI] [PubMed] [Google Scholar]
- Feinn R, Tennen H, & Kranzler HR (2003). Psychometric properties of the short index of problems as a measure of recent alcohol-related problems. Alcoholism, Clinical and Experimental Research, 27, 1436–41. doi: 10.1097/01.ALC.0000087582.44674.AF [DOI] [PubMed] [Google Scholar]
- Fuhriman A, Drescher S, Hanson E, Henrie R, & Rybicki W (1986). Refining the measurement of curativeness: an empirical approach. Small Group Behavior, 17, 186–201. 10.1177/104649648601700204 [DOI] [Google Scholar]
- Gray RM, Kelly PJ, Beck AK, Baker AL, Deane FP, Neale J, Treloar C, Hides L, Manning V, Shakeshaft A, Kelly J, Argent A, & McGlaughlin R (2020). A qualitative exploration of SMART Recovery meetings in Australia and the role of a digital platform to support routine outcome monitoring. Addictive Behaviors, 101. 10.1016/j.addbeh.2019.106144 [DOI] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, & Wasserman DA (1991). Effects of commitment to abstinence, positive moods, stress, and coping on relapse to cocaine use. Journal of Consulting and Clinical Psychology, 59, 526–532. 10.1037/0022-006X.59.4.526 [DOI] [PubMed] [Google Scholar]
- Hester RK, Lenberg KL, Campbell W, & Delaney HD (2013). Overcoming Addictions, a Web-based application, and SMART Recovery, an online and in-person mutual help group for problem drinkers, part 1: Three-month outcomes of a randomized controlled trial. Journal of Medical Internet Research, 15, e134. doi: 10.2196/jmir.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, Kaskutas LA, & Weisner C The Alcoholics Anonymous Affiliation Scale: Development, reliability, and norms for diverse treated and untreated populations. Alcoholism: Clinical and Experimental Research, 22, 974–978. DOI: 10.1111/j.1530-0277.1998.tb03691.x [DOI] [PubMed] [Google Scholar]
- Kelly PJ, McCreanor K, Beck AK, Ingram I, O’Brien D, King A, McGlaughlin R, Argent A, Ruth M, Hansen BS, Andersen D, Manning V, Shakeshaft A, Hides L, & Larance B (2021). SMART Recovery International and COVID-19: Expanding the reach of mutual support through online groups. Journal of Substance Abuse Treatment, 108568. doi: 10.1016/j.jsat.2021.108568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontos E, Blake KD, Chou W-YS, & Prestin A (2014). Predictors of eHealth usage: Insights on the digital divide from the Health Information National Trends Survey 2012. Journal of Medical Internet Research, 16, e172. doi: 10.2196/jmir.3117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krentzman AR (2021): Helping clients engage with remote mutual aid for addiction recovery during COVID-19 and beyond. Alcoholism Treatment Quarterly. 10.1080/07347324.2021.1917324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, & Longabaugh R (1995). The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. [Google Scholar]
- Milward J, Lynskey M, & Strang J (2014). Solving the problem of non-attendance in substance abuse services. Drug and Alcohol Review, 33, 625–636. 10.1111/dar.12194 [DOI] [PubMed] [Google Scholar]
- Oesterle TS, Bhanuprakash K, Risma CJ, Breitinger SA, Rakocevic DB, Loukianova LL, Hall-Flavin DK, Gentry MT, Rummans TA, Chauhan M, & Gold MS (2020). Substance use disorders and telehealth in the COVID-19 pandemic era: A new outlook. Mayo Clinic Proceedings, 95, 2709–2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1993). Composite International Diagnostic Interview. World Health Organization. [Google Scholar]
- Wynn R, Oyeyemi SO, Budrionis A, Marco-Ruiz L, Yigzaw KY, & Billikacle JG (2020). Electronic health use in a representative sample of 18,497 respondents in Norway. JMIR Medical Informatics, 8, e13106. doi: 10.2196/13106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yalom ID (1975). The theory and practice of group psychotherapy. Basic Books. [Google Scholar]
- Zemore SE, Kaskutas LA, Mericle A, & Hemberg J (2017). Comparison of 12-Step groups to mutual help alternatives for AUD in a large, national study: Differences in membership characteristics and group participation, cohesion, and satisfaction. Journal of Substance Abuse Treatment, 73, 16–26. doi: 10.1016/j.jsat.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Lui C, Mericle A, Hemberg J, & Kaskutas LA (2018). A longitudinal study of the comparative efficacy of Women for Sobriety, LifeRing, SMART Recovery, and 12-step groups for those with AUD. Journal of Substance Abuse Treatment, 88, 18–26. doi: 10.1016/j.jsat.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]


