Abstract
Purpose
Evidence has shown that 50% of patients, including type 2 diabetes mellitus (DM), are non-adherent to the prescribed antidiabetic medication regimen. Some barriers lead to nonadherence in people with DM type 2. The study aimed to identify factors related to adherence in patient with DM and to assess the correlation between barriers to adherence type 2 DM patients.
Methods
The cross-sectional study was conducted in 63 primary healthcare centers in Surabaya, Indonesia. Patients with DM type 2 were recruited between April and September 2019 using convenient sampling technique. Ethics approval was obtained (80/EA/KEPK/2019).
Results
A total of 266 patients with type 2 DM participated in this study. Of the respondents, 201 (75.2%) were female. Unwanted drug effects, changes in medication regimens, and refilling the prescription when the drugs run out were most reported factors that affected adherence. Spearman correlations and linear regression tests were used to examine the relationship between barriers to medication adherence, and education with medication adherence. A significant difference was observed between the level of education and adherence (p = 0.031). The results showed an association between barriers to medication and adherence to medication (r = 0.304; p < 0.001) which was confirmed in regression analysis (R = 0.309, R square = 0.095, p <0.001).
Conclusions
Barriers to adherence are common and affect adherence to therapy. It is essential to expand the roles of health care professionals in the community to include counseling, barrier-monitoring, education, and problem-solving to improve patient medication adherence.
Keywords: Diabetes mellitus, Chronic illness, Drug adherence, Patient compliance, Primary care
Introduction
Diabetes mellitus (DM) is characterized by chronic hyperglycemia, resulting in carbohydrate, fat, and protein metabolism [1]. With 10 million adults with diabetes, Indonesia ranks seventh in the prevalence of diabetes, after China, the United States, Brazil, Russia, and Mexico [2]. Other health complications are accelerated in presence of DM and is responsible for 77% of comorbidities and 88% of deaths in developing countries [2]. Patients with long-term DM may develop complications, such as retinopathy (which can cause blindness), nephropathy with potential renal failure, and neuropathy. Based on pathophysiology, type 1 DM, type 2 DM, and diabetes of other causes account for 5–10%, 90%, and 1–2% respectively, of all diabetes cases [3].
Adherence to treatment is crucial in treating chronic diseases, including DM. Adherence to a treatment regimen is generally defined by how a patient takes medication as determined by a healthcare provider [4]. Complying with therapy is crucial in the treatment of chronic diseases, including DM type 2. Nonadherence in patients with DM type 2 can result in increased blood sugar levels, causing microvascular and macrovascular complications, such as retinopathy, nephropathy, neuropathy, and other cardiovascular diseases [3]. However, evidence has shown that 50% of patients, including type 2 DM, are non-adherent to the prescribed antidiabetic medication regimen [5]. Moreover, rates of nonadherence were higher among ethnic minorities and patients with low socioeconomic status [6, 7].
Some barriers lead to nonadherence in people with DM type 2. Age, type of treatment, and copayment were the most decisive factors of poor adherence in DM type 2 patients [5]. A study conducted on 37,431 Medicaid-insured patients in the United States showed that only 15% of patients took their medications regularly [8]. Previous studies have demonstrated 10–78% poor oral DM type 2 medication adherence [9, 10]. The study’s findings in Qatar showed that nonadherence to medications among people with uncontrolled diabetes in the primary care setting is high [11]. Another study in Kenya found that medication adherence in 28.3% diabetes patients was low [12].
Nonadherence to treatment could be due to one or more of the following reasons: complexity of the therapeutic regimen, disregard for the physician’s advice, or the limited ability for self-management. Worldwide, nonadherence to therapeutic regimens is a significant issue for healthcare providers because of the consequences [13, 14]. To counter severe medical complications and minimize healthcare costs, patient adherence with antidiabetic drugs is a critical and principal factor. However, patient-healthcare provider relationships were the primary cause of poor adherence to antidiabetic medication [15]. Moreover, cultural- and gender-sensitive communication techniques for adapting healthcare goals for patients may ease healthcare professionals’ work [16].
The factors associated with nonadherence are complex, multilateral, and vary with patients, situation, and healthcare settings. Therefore, it is essential to know nonadherence to medication regimens in a particular individual with certain chronic conditions and evaluate its determinants. Various factors affect patient adherence to medication: patient-centered factors, therapy-related factors, healthcare system-related factors, socioeconomic factors, and disease-related factors [17]. Other factors described in a previous review by Sarayani in 2013 [18] explained that forgetfulness, lack of availability of medication, medication regimen complexity, and lack of symptoms were associated with nonadherence. A patient with DM type 2 and other complex conditions needs multiple drug therapies to control blood sugar levels and other complications. Optimal medication therapy for patients with DM requires multiple medications to achieve these goals that lead to higher rates of medication nonadherence [19, 20]. The prevalence of DM type 2 was 97.5% in a study conducted in Indonesia, and 67.9% of patients had poor control of DM type 2 (A1c:8.1 ± 2.0%) [21]. Due to the high prevalence rates of type 2 DM, and insufficient control of DM in Indonesia, evaluating the barrier to adherence is necessary to counter the disease. Considerable efforts including, assessing barriers to medication adherence, could improve patient adherence to achieve the desired outcomes in patients with type 2 DM.
Aim of the study
This study aimed to identify factors related to adherence in patients with DM type 2. This study also aimed to assess the correlation between barriers and medication adherence in patients with DM type 2 attending primary healthcare centers in Surabaya.
Methods
Study setting and design
A cross-sectional study was conducted in 63 primary healthcare centers in Surabaya, Indonesia. Convenience sampling was completed in a six-month period (from April to September 2019) to recruit patients with type 2 DM. Participants were recruited while waiting to receive their medications in the waiting rooms of the primary healthcare centers.
The sample size was calculated after a discussion with a statistician using a correlation sample size according to the following formula: N = [(Zα + Zβ) C]2 + 3 [22]. Considering the 95% confidence level, 80% test power, and expected correlation coefficient, the minimum required sample size was 194 [23].
Eligibility criteria
Patients were recruited if they were diagnosed with DM type 2, were using antidiabetic medication for at least three months, were aged ≥18 years, and could communicate in the Indonesian language. Patients diagnosed with DM type 2 recently (within less than a month) and those diagnosed with type 1 DM were excluded from the study.
Data collection
The researcher approached all eligible participants while participants were sitting in the waiting room, described the study, and requested written consent if they agreed to participate in the study. A standardized questionnaire based face-to-face interview was carried out on a one-to-one basis. An identical questionnaire was used at all primary health care centers. The questionnaire was divided into three parts. Part A comprised demographic section and data related to DM. This section included questions such as sex, age, Body Mass Index (BMI), education level, occupation, health insurance, family history of diabetes, exercise activity, and data on tobacco use (smoking). Part B comprised ten questions in the Identification of Medication Adherence Barriers (IMAB-Q). Part C comprised of 12 questions of Adherence to Refills and Medication Scale (ARMS) questionnaire.
Measurement
The authors of the IMAB-Q and ARMS questionnaire granted permission to use both questionnaires in this research. The IMAB-Q was used to assess medication adherence barriers in participants. The questionnaire contains ten theoretical domain framework questions about patients’ behavioral factors, patients’ beliefs, environmental factors, and social influences. The validity and reliability of the IMAB-Q for measuring obstructions to patient adherence have been tested [24]. The IMAB-Q consists of 10 questions: questions 1–5 relate to patients’ facilitators that lead to better adherence, and questions 6–10 relate to barriers that lead to poor adherence to medication. The assessment used a five-point Likert scale: for questions 1–5, 1 point = strongly agree and 5 points = strongly disagree, and for questions 6–10, 5 points = strongly agree and 1 point = strongly disagree. The author obtained the IMAB-Q score by adding the scores of each statement. For items, 1-4 is considered unintentional nonadherence, while items 5-10 can be seen as intentional nonadherence. Thus, the total IMAB-Q score ranged from 10 to 50, where a lower IMAB-Q score indicated a few barriers to adherence [24].
Patient adherence was measured using a self-reporting ARMS questionnaire. The ARMS questionnaire consists of 12 questions. The validity and reliability of the ARMS questionnaire in measuring adherence in patients with chronic diseases has been tested. Additionally, the ARMS questionnaire has two indicators: compliance to therapy and adherence to prescriptions. The lowest and highest total ARMS questionnaire scores are 12 and 48, respectively. A low total ARMS score indicates a high level of adherence [25]. Responses to each question are rated on a Likert scale: “never,“ “sometimes,“ “often,“ or “always,“ scored from 1 to 4 for questions 1–11; “always,“ “often,“ “sometimes,“ or “never,“ scored from 1 to 4 for question 12. A total ARMS score > 12 indicates some level of nonadherence [25]. All participants were asked to complete the demographic data, IMAB, and ARMS questionnaires.
The IMAB-Q and ARMS questionnaires were translated following the WHO guidelines [26]. The IMAB-Q and ARMS questionnaires were translated and adapted from English to Indonesian in four stages: forward translation, backward translation, pre-testing, and cognitive interviewing. From January to February 2019, four health sector professional translators (pharmacists and pharmacy academics) who were fluent English, worked on the forward and backward translation process. The results were then discussed by a panel of experts, who concluded that there was no difference in meaning for all questions in IMAB-Q and ARMS questionnaires. The process of pre-testing and cognitive interviewing was performed in individuals representing the target population. About 30 participants with DM type 2 were selected from primary health care centers. In the pre-testing and cognitive interview stage, we evaluated how words are used in each item of the questionnaire statement. Respondents were asked to respond to their understanding of the questionnaire so that researchers could determine the use of appropriate and easy-to-understand words. The results of the pre-testing and cognitive interviewing processes, combined with face validity, determined that all questions were easily understood and thus translated questionnaires were ready to be used.
Statistical analysis
Descriptive analysis was used to assess the demographic characteristics of the participants. Data normality was evaluated to determine the type of statistical analysis required. Cross-tabulation testing was performed to determine the frequency of adherent and non-adherent patients using the IMAB and ARMS questionnaires. Pearson chi-square or Fisher’s exact test and Mann-Whitney U test were used to determine the significant difference between patients’ demographics and barriers and adherence levels. Spearman correlations and linear regression tests were used to examine the relationship between barriers to medication adherence and adherence and education. All data were analyzed using IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
Results
Demographic characteristics
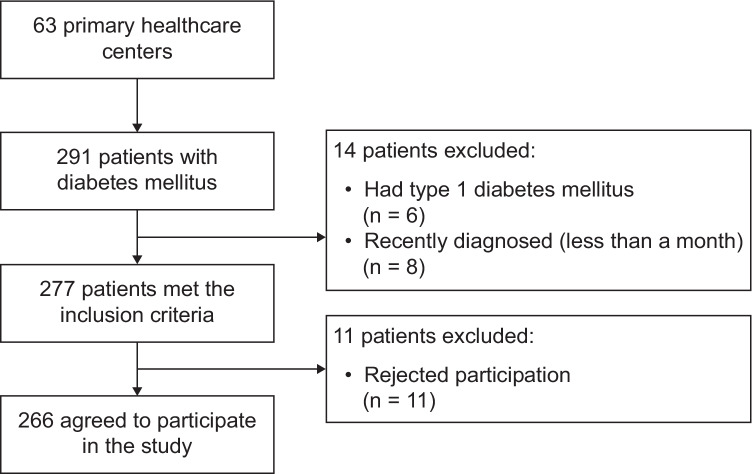
A total of 291 patients with DM type 2 were approached, and 266 agreed to participate in the study; 25 patients were excluded (Fig. 1). The demographic characteristics of the participants are shown in Table 1. The mean age of respondents was 61 years, and the majority (75.6%, n=201) were female. Most participants (52.2%) were of normal weight. Most of the participants had an elementary education (28%), and most were housemakers (n=223). Nearly 60% of the participants had no family history of DM type 2. Most of the respondents were diagnosed with DM and took oral antidiabetic drugs for four years. Most of the patients (n=259) had health insurance.
Fig. 1.
Participant recruitment flowchart
Table 1.
Demographic characteristics of participants with type 2 diabetes mellitus (n = 266)
| Patient characteristic | Frequency (%) |
|---|---|
| Sex | |
| Male | 65 (24.4) |
| Female | 201 (75.6) |
| Mean age (year) | 61.3131± 9.45 |
| BMI | 24,44 (16.00-38.70) |
| Underweight (<18.5 kg/m2) | 10 (3.8) |
| Normal weight (18.5–24.9 kg/m2) | 139 (52.2) |
| Overweight (25.0–29.9 kg/m2) | 91 (34.2) |
| Obesity (>30.0 kg/m2) | 26 (9.8) |
| Education | |
| No formal education | 52 (19.6) |
| Elementary | 77 (28.9) |
| Junior high school | 64 (24.1) |
| Senior high school | 51 (19.2) |
| Diploma | 7 (2.6) |
| Undergraduate/Postgraduate | 15 (5.6) |
| Occupation | |
| Housemaker | 223 (83.8) |
| Civil employee | 4 (1.5) |
| Self-employed | 21 (7.9) |
| Private | 14 (5.2) |
| Others | 4 (1.5) |
| Health insurance | |
| BPJS | 248 (93.2) |
| Non-BPJS | 11 (4.1) |
| No insurance | 7 (2.7) |
| Family history of diabetes mellitus | |
| Father | 25 (9.4) |
| Mother | 35 (13.2) |
| Grandparents | 7 (2.6) |
| Siblings | 21 (7.9) |
| None | 157 (59) |
| No information | 21 (7.9) |
| Smoking | |
| Always | 1 (0.4) |
| Never | 251 (94.4) |
| 1–5 years | 4 (1.5) |
| More than 5 years | 10 (3.8) |
| Exercise | |
| Yes | 202 (75.9) |
| No | 64 (24.1) |
| Comorbid conditions (hypertension, cardiovascular disease, asthma, others) | 154 (57.9) |
| Taking regular medications | 144 (54.1) |
BMI, body mass index; BPJS, Badan Penyelenggara Jaminan Sosial
Patient characteristics with adherence barriers and medication adherence are shown in Table 2. Most of the male (51,78.5%), and the female patients (140, 69.7%), reported low adherence barriers. Among the male respondents, 16 (24.6%) and 49 (74.4%) were adherent and non-adherent, respectively. Most of the female respondents (136, 67.7%) were non-adherent to therapy. Many of the normal-weight patients (n=95, 68.3%) had some degree of nonadherence to medication. Only 81 (30.5%) were entirely adherent to DM type 2 therapy based on the ARMS questionnaire scores. A total of 154 (57.9%) participants had comorbidities, such as hypertension, cardiovascular disease, and asthma. More than 70% of participants undertook regular sports activities, such as gymnastics, walking, cycling, and jogging, at least once a week. A total of 251 (94.3%) participants had never smoked. A significant difference between patients’ education and adherence level was observed (p = 0.031) (Table 2).
Table 2.
Proportion of patients with type 2 diabetes mellitus reporting barriers to adherence using IMAB-Q score, and medication adherence as per ARMS (n = 266)
| Patients’ characteristics | IMAB-Q score | ARMS score | ||||
|---|---|---|---|---|---|---|
| Low barriers, n (%) | High barriers, n (%) | P-value | Adherent, n (%) | Non-adherent, n (%) | P-value | |
| Sex | ||||||
| Male | 51 (78.5) | 14 (21.5) | 0.170 | 16 (24.6) | 49 (75.4) | 0.279 |
| Female | 140 (69.7) | 61 (30.3) | 65 (32.3) | 136 (67.7) | ||
| BMI | ||||||
| Underweight (<18.5 kg/m2) | 8 (80) | 2 (20) | 0.204 | 4 (40) | 6 (60) | 0.662 |
| Normal weight (18.5–24.9 kg/m2) | 106 (76.3) | 33 (23.7) | 44 (31.7) | 95 (68.3) | ||
| Overweight (25.0–29.9 kg/m2) | 58 (63.7) | 33 (36.3) | 24 (26.4) | 67 (73.6) | ||
| Obesity (>30.0 kg/m2) | 19 (73.1) | 7 (26.9) | 9 (34.6) | 17 (65.4) | ||
| Education | ||||||
| No formal education | 40 (76.9) | 12 (23.1) | 0.183 | 25 (48.1) | 27 (51.9) | 0.031 |
| Elementary | 54 (70.1) | 23 (29.9) | 20 (26) | 57 (74) | ||
| Junior high school | 48 (75) | 16 (25) | 20 (31.3) | 44 (68.8) | ||
| Senior high school | 35 (68.6) | 16 (31.4) | 12 (23.5) | 39 (76.5) | ||
| Diploma | 2 (28.6) | 5 (71.4) | 0 | 7 (100) | ||
| Undergraduate/Postgraduate | 12 (80) | 3 (20) | 4 (26.7) | 11 (73.3) | ||
| Occupation | ||||||
| Housemaker | 159 (71.3) | 64 (28.7) | 0.940 | 69 (30.9) | 154 (69.1) | 0.127 |
| Civil employee | 2 (50) | 2 (50) | 0 | 4 (100) | ||
| Self-employed | 15 (71.4) | 6 (28.6) | 7 (33.3) | 14 (66.7) | ||
| Private | 11 (78.6) | 3 (21.4) | 2 (14.3) | 12 (85.7) | ||
| Others | 4 (100) | 0 | 3 (75) | 1 (25) | ||
| Health insurance | ||||||
| BPJS | 178 (71.8) | 70 (28.2) | >0.05 | 72 (29) | 176 (71) | 0.128 |
| Non-BPJS | 8 (72.7) | 3 (27.3) | 6 (54.5) | 5 (45.5) | ||
| No insurance | 5 (71.4) | 2 (28.6) | 3 (42.9) | 4 (57.1) | ||
BMI, body mass index; IMAB-Q, Identification of Medication Adherence Barriers Questionnaire; BPJS, Badan Penyelenggara Jaminan Social; ARMS, Adherence to Refills and Medications Scale
Profiles of barriers and medication adherence
Table 3 summarizes participant responses to the IMAB-Q. Table 4 lists patients’ responses to the medication adherence statements. Table 5 illustrates the correlation among barriers to adherence, education, and medication adherence. The analysis showed a significant relationship between barriers to medication adherence and adherence to treatment in patients in primary health centers in Surabaya (r = 0.304; p < 0.001), while patient’s education and adherence has no significant association (p = 0.064). Linear regression analysis in Table 6 showed that barrier to medication adherence affects medication adherence (R = 0.309, R square = 0.095, p < 0.001). Our results indicate that 9.5% of medication nonadherence is affected by adherence barriers, and the rest is affected by other factors. The study found that education had no significant impact on medication adherence.
Table 3.
IMAB-Q responses of participants with type 2 diabetes mellitus (n = 266)
| Domain | Statements | Strongly Agree, n (%) | Agree, n (%) | Neither Agree or Disagree, n (%) | Disagree, n (%) | Strongly Disagree, n (%) |
|---|---|---|---|---|---|---|
| Patient’s behavioral factors | (1) I know how to take medicine | 116 (43.6%) | 143 (53.8%) | 3 (1.1%) | 4 (1.5%) | 0 (0%) |
| (2)I can consume medicines that are given without the help of others | 108 (40.6%) | 139 (52.3%) | 9 (3.4%) | 9 (3.4%) | 1 (0.4%) | |
| (3)I remember to take medication as prescribed | 114 (42.9%) | 139 (52.3%) | 12 (4.5%) | 1 (0.4%) | 0 (0%) | |
| (4)I can get prescribed medicines easily | 110 (41.4%) | 154 (57.9%) | 2 (0.8%) | 0 (0%) | 0 (0%) | |
| Patient’s beliefs | (5)I feel sure about all aspects of management | 93 (35%) | 156 (58.6%) | 12 (4.5%) | 4 (1.5%) | 1 (0.4%) |
| (6)I am worried about unwanted effects | 15 (5.6%) | 55 (20.7%) | 23 (8.6%) | 143 (53.8%) | 30 (11.3%) | |
| Environmental Factors | (7) Taking medicines as prescription is a burden for me | 14 (5.3%) | 28 (10.5%) | 12 (4.5%) | 174 (65.4%) | 38 (14.3%) |
| (8) My life keeps me from taking medicine | 4 (1.5%) | 33 (12.4%) | 9 (3.4%) | 174 (65.4%) | 46 (17.3%) | |
| (9)I do not think I can cope with it if medicines keep changing | 8 (3%) | 42 (15.8%) | 27 (10.2%) | 158 (59.4%) | 31 (11.7%) | |
| Social Influences | (10)I worry what other people think of me if they know I’m taking medication | 5 (1.9%) | 23 (8.6%) | 7 (2.6%) | 167 (62.8%) | 64 (24.1%) |
IMAB-Q, Identification of Medication Adherence Barriers Questionnaire
Table 4.
ARMS responses of participants with type 2 diabetes mellitus (n=266)
| Domain | ARMS statements | Never, n(%) | Sometimes, n(%) | Often, n(%) | Always, n(%) |
|---|---|---|---|---|---|
| Compliance to taking medication | (1) How often do you forget to take medication? | 165 (62%) | 90 (33.2%) | 10 (3.8%) | 1 (0.4%) |
| (2) How often do you decide not to take medicine? | 184 (69.2%) | 70 (12%) | 12 (4.5%) | 0 (0%) | |
| (5) How often do you skip taking medication before going to the doctor? | 188 (70.7%) | 71 (26.7%) | 7 (2.6%) | 0 (0%) | |
| (6) How often you don’t take medication when you feel better? | 190 (71.4%) | 62 (23.3%) | 14 (5.3%) | 0 (0%) | |
| (7) How often do you skip medication while still feeling sick? | 216 (81.2%) | 46 (17.3%) | 3 (1.1%) | 1 (0.4%) | |
| (8) How often do you skip medication when you are less concerned about your condition? | 218 (82%) | 43 (16.2%) | 5 (1.9%) | 0 (0%) | |
| (9) How often do you change your dosage? | 221 (83.1%) | 43 (16.2%) | 2 (0.8%) | 0 (0%) | |
| (10) How often do you forget to take medicines you should take more than one time? | 200 (75.2%) | 62 (23.3%) | 4 (1.5%) | 0 (0%) | |
| Adherence to prescriptions | (3) How often do you forget to redeem a recipe? | 211 (79.3%) | 47 (17.7%) | 7 (2.6%) | 1 (0.4%) |
| (4) How often do you run out of drugs? | 209 (78.6%) | 50 (18.8%) | 6 (2.3%) | 1 (0.4%) | |
| (11) How often you don’t redeem a recipe for paying too much? | 242 (91%) | 19 97.1%) | 2 (0.8%) | 2 (1.1%) | |
| (12) How often do you plan to redeem prescriptions before drugs run out? | 47 (17.7%) | 29 910.9%) | 44 (16.5%) | 146 (54.9%) |
ARMS, Adherence to Refills and Medications Scale
Table 5.
Correlation between total IMAB-Q score with total ARMS score and education with adherence level
| Variables | r | Sig.(2-tailed) | |
|---|---|---|---|
| IMAB-Q | ARMS score | 0.304** | <0.001 |
| Education | 0.114 | 0.064 | |
** Correlation is significant at the 0.01 level (2-tailed)
Table 6.
Regression analysis between total IMAB-Q score and ARMS score, and between education and adherence level
| Predictors | Dependent variable | R | R square | Std. Error | P-value |
|---|---|---|---|---|---|
| IMAB-Q score | ARMS score | 0.309 | 0.095 | 4.009 | <0.001 |
| Education | 0.061 | 0.004 | 4.207 | 0.320 |
Discussion
This research determined common barriers to adherence to treatment in patients with type 2 DM, as measured using the IMAB-Q. Of the items in IMAB-Q that most patients in our study perceived, concern regarding the side effects of the drug as barrier to medication adherence was common, which was also reported in previous studies [27–29]. Another study indicated that adverse events are a significant barrier to medication adherence [30]. A high percentage of patients in our study also identified “taking medication as a burden” as a barrier, and a higher number of medications led to nonadherence to therapy. Our results contrasted with a prior study that stated that patients with many medications showed good adherence to treatment [31]. However, our findings suggest that there is still room for improvement in terms of pro-active intervention to optimize the adherence of patients with diabetes.
Good adherence to a medication regimen is a vital dimension of the quality of healthcare. The adherence level in patients with type 2 DM in this study was measured using the ARMS questionnaire. In this study, only 81 (30.5%) participants were fully adherent to DM therapy based on the ARMS questionnaire. The ARMS scores lower than the previous study in which 39% of patients showed good adherence [32], and higher (22.7%) than the study conducted in Brazil [33]. Difference by the sex of patients was evident from the fact that male patients were non- adherent toward therapy as compared to female patients. The previous research showed contrast results compared to the current study that the female gender is more likely to skip medication, take less than prescribed medication, and delay filling the prescriptions [33, 34].
The results of the 12 question items in ARMS questionnaire showed that not having a plan to refill the medication prescription was the most frequent form of nonadherence. This could be since the patients did not have time to fill their prescriptions and lacked information about the harmful effects of stopping the medication. Other forms of nonadherence are forgetting to take the medicines, not wanting to take the drug, or believing that the treatment causes them to feel unwell, as reported in prior studies [18, 27]. Patients (23.3%) sometimes don’t take medication when they feel better, supported by Sarayani et al. [18] that described that lack of symptoms or feeling well leads to medication nonadherence in diabetic patients.
The study also evaluated the relationship between adherence barriers and medication adherence in patients with type 2 DM, showing a positive correlation between the IMAB and ARMS total scores, which means that the higher the total IMAB-Q score, the higher the total ARMS score. In other words, the lower the barrier to adherence, the more likely patients are to be adherent to their medication therapy. The degree of correlation was moderate (r=0.304), suggesting room for other factors to affect medication adherence, such as duration of treatment, frequency of medication use, the taste of the drug, and failure to understand the importance of the therapy [35].
Regression analysis showed that adherence barriers impact drug adherence, as supported by previous studies [36]. Other studies have also demonstrated that barriers such as multiple therapies, changing the dosage regimen, and a complex therapeutic regimen affect therapy adherence [37–39]. Insurance, adverse outcomes, and short-use medications also affect medication adherence [40, 41]. In this study, an association between patient education level and medication adherence was lacking. The results are consistent with a study in Ethiopia that found no relationship between education and adherence in diabetic patients [42]. However, a previous study conducted in Poland on diabetic patients concluded that patients with tertiary education have more self-care management on adherence than patients with low education levels [43]. Another review study on poor medication adherence recorded low education level as a crucial factor responsible for poor adherence to DM type 2 therapy [44].
Healthcare providers and diabetes educators should pay special attention to the vulnerable population that is non-adherent to antidiabetic medication. Therefore, the role of healthcare professionals is crucial. Educating people regarding the consequences of nonadherence is an urgent need. Healthcare providers, such as physicians, clinical pharmacists, community pharmacists, and nurses play a vital role in improving adherence to therapy. Pharmacists in primary healthcare centers, for instance, can play a role in improving patient medication adherence. Activities such as conducting health promotions (e.g., providing brochures and pamphlets to patients) to help patients understand their disease and treatment are warranted. Additionally, monitoring and maintaining patient health by providing tools such as medication reminder charts that patients can see every time they refill and take the medication are also helpful. Other barriers to adherence may include the cost of medicines, lack of health insurance, and access to a pharmacy [45].
The government should provide health insurance to the population with a low economic status. This population cannot afford purchasing medications, which often leads to nonadherence and discontinuation of therapy. Providing information and education during counseling sessions, especially to patients with chronic diseases, such as DM, may reduce medication adherence barriers. Health care practitioners, including pharmacists, must assess patients’ knowledge regarding the aim of therapy and educate patients to fill the gaps in knowledge [46]. This study also provides healthcare providers with information for screening patients, identifying risk factors associated with adherence, designing interventions to remove the barriers, and improving medication adherence in diabetes patients. Moreover, because of the high percentage of nonadherence in patients with type 2 DM, health care practitioners must discuss the importance of adherence supported by a healthy lifestyle, including physical activity and diet [47].
One of the shortcomings of this study may be the evaluation of only patient-related factors affecting adherence. Based on the literature, many factors affect medication adherence, such as healthcare provider-related and drug-related factors. As this study only included those who could communicate in the Indonesian language (Bahasa), we may have excluded eligible individuals who could not participate in the study because of linguistic differences. In such individuals, unfamiliarity with the local language may also become a barrier to medication adherence. Therefore, further studies are needed to explore other factors that may affect adherence.
Conclusions
In conclusion, our findings in primary healthcare settings show considerable barriers to medication adherence in patients with type 2 DM. Unwanted drug effects, changing the medication regimen, failure to refill the prescription when the medication runs out and thinking about how other people feel about one’s medication use are some of the barriers that lead to nonadherence. Female participants, participants with normal weight, and those with health insurance had the lowest level of adherence.
A future study targeting barriers in adherence focusing on the perspectives of both healthcare professionals and patients is warranted. Educational interventions by healthcare providers and assistance solving other barriers to adherence, such as pharmacy access, may significantly improve adherence to therapy in vulnerable populations.
Acknowledgements
The authors would like to thank the Faculty of Pharmacy, Universitas Airlangga, and the Lembaga Penelitian dan Pengabdian Masyarakat (LPPM) Universitas Airlangga for the support and facilities provided during the study. We also thank the research assistants involved in this study: Ms. Yenni Desilia Indahsari, Ms. Edlia Fadilah and Ms. Yerlita El Girath.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Indonesian Ministry of Education and Culture [DRPM – PDUPT 2019-2021]. The funder had no role in the study design; in the collection, and analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Data availability
All data generated or analyzed in this study are included in this article.
Declarations
Ethics approval
Informed consent was obtained from all participants in this study and all procedures were approved by the Human Research Ethics Committee of the Faculty of Public Health, Universitas Airlangga, Surabaya, Indonesia (approval number: 80/EA/KEPK/2019).
Research involving human participants
This study was approved by The Human Research Ethics Committee of Faculty of Public Health at Universitas Airlangga, Surabaya, Indonesia.
Informed consent
All participants provided written informed consent to participate in this study.
Conflict of interest
The authors declare that there is no conflict of interest.
Footnotes
Impact on practice statement
• Barriers to adherence exist in patients with type 2 diabetes mellitus in Indonesia.
• Socioeconomic factors and education level of these patients impacts adherence.
• The role of pharmacists in the community should be expanded to counter this issue.
• Changes in medication regimens and failure to refill medicine also impact adherence.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Diabetes Association Diabetes advocacy. Diabetes Care. 2017;40(Suppl 1):128–9. doi: 10.2337/dc17-S018. [DOI] [Google Scholar]
- 2.Karuranga S, Malanda B, Saeedi P, Salpea PIDF, Diabetes Atlas. International Diabetes Federation. https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf. Accessed 1 Apr 2020.
- 3.Palicka V. Pathophysiology of Diabetes Mellitus. EJIFCC. 2002;13(5):140–4. [PMC free article] [PubMed] [Google Scholar]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.Horvat O, Popržen J, Tomas A, Paut Kusturica M, Tomić Z, Sabo A. Factors associated with nonadherence among type 2 diabetic patients in primary care setting in eastern Bosnia and Herzegovina. Prim Care Diabetes. 2018;12(2):147–54. doi: 10.1016/j.pcd.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Nelson LA, Wallston KA, Kripalani S, LeStourgeon LM, Williamson SE, Mayberry LS. Assessing barriers to diabetes medication adherence using the Information-Motivation-Behavioral skills model. Diabetes Res Clin Pract. 2018;142:374–84. doi: 10.1016/j.diabres.2018.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinto DM, Santiago LM, Maurício K, Silva IR. Health profile and medication adherence of diabetic patients in the Portuguese population. Prim Care Diabetes. 2019;13(5):446–51. doi: 10.1016/j.pcd.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Dailey G, Kim MS, Lian JF. Patient compliance and persistence with antihyperglycemic drug regimens: evaluation of a medicaid patient population with type 2 diabetes mellitus. Clin Ther. 2001;23(8):1311–20. doi: 10.1016/s0149-2918(01)80110-7. [DOI] [PubMed] [Google Scholar]
- 9.Evans J, Donnan P, Morris AD. Adherence to oral hypoglycemic agents prior to insulin therapy in Type 2 diabetes. Diabet Med. 2002;19(8):685–8. doi: 10.1046/j.1464-5491.2002.00749. [DOI] [PubMed] [Google Scholar]
- 10.Donnan PT, MacDonald TM, Morris AD. Adherence to prescribed oral hypoglycaemic medication in a population of patients with Type 2 diabetes: a retrospective cohort study. Diabet Med. 2002;19(4):279–84. doi: 10.1046/j.1464-5491.2002.00689. [DOI] [PubMed] [Google Scholar]
- 11.Jaam M, Mohamed Ibrahim MI, Kheir N, Hadi MA, Diab MI, Awaisu A. Assessing prevalence of and barriers to medication adherence in patients with uncontrolled diabetes attending primary healthcare clinics in Qatar. Prim Care Diabetes. 2018;12(2):116–25. doi: 10.1016/j.pcd.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Waari G, Mutai J, Gikunju J. Medication adherence and factors associated with poor adherence among type 2 diabetes mellitus patients on follow-up at Kenyatta National Hospital, Kenya. Pan Afr Med J. 2018;29:82. doi: 10.11604/pamj.2018.29.82.12639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alves Peres H, Leira Pereira LR, Zangiacomine Martinez E, Viana CM, de Freitas MCF. Elucidating factors associated with nonadherence among Type 1 diabetes patients in primary care setting in Southeastern Brazil. Prim Care Diabetes. 2020;14(1):85–92. doi: 10.1016/j.pcd.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Wu J, Davis-Ajami ML, Noxon V, Lu ZK. Venue of receiving diabetes self-management education and training and its impact on oral diabetic medication adherence. Prim Care Diabetes. 2017;11(2):162–70. doi: 10.1016/j.pcd.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Schechter CB, Walker EA. Improving adherence to diabetes self-management recommendations. Diabetes Spectr. 2002;15(3):170–5. doi: 10.2337/diaspect.15.3.170. [DOI] [Google Scholar]
- 16.Pentzek M, Santos S, Wollny A, et al. Which patients with type 2 diabetes mellitus are perceived as ‘difficult’ by general practitioners? Prim Care Diabetes. 2019;13(4):353–9. doi: 10.1016/j.pcd.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: A review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–86. doi: 10.2147/TCRM.S1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sarayani A, Jahangard-Rafsanjani Z, Hadjibabaie M, Ahmadvand A, Javadi M, Gholami K. A comprehensive review of adherence to diabetes and cardiovascular medications in Iran; implications for practice and research. J Diabetes Metab Disord. 2013;12(1):1–9. doi: 10.1186/2251-6581-12-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rätsep A, Oja I, Kalda R, Lember M. Family doctors’ assessment of patient- and health care system-related factors contributing to nonadherence to diabetes mellitus guidelines. Prim Care Diabetes. 2007;1(2):93–7. doi: 10.1016/j.pcd.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Q, Zhao C, Davies MJ, Radican L, Seck T. Compliance and persistencewith concomitant statin and oral antihyperglycemic therapy. Am J Manag Care. 2011;17(11):746–52. [PubMed] [Google Scholar]
- 21.Soewondo P, Soegondo S, Suastika K, Pranoto A, Soeatmadji DW, Tjokroprawiro A. The DiabCare Asia 2008 study â Outcomes on control and complications of type 2 diabetic patients in Indonesia. Med J Indones. 2010;19(4):235–44. doi: 10.13181/mji.v19i4.412. [DOI] [Google Scholar]
- 22.Jeffrey JW. Designing clinical research: an epidemiologic approach, 2nd edition. Optometry and Vision Science, 78. 2001.
- 23.Baruel Okumura PC, Okumura LM, Reis WC, Godoy RR, Cata-Preta BO, de Souza TT, Favero ML, Correr CJ. Comparing medication adherence tools scores and number of controlled diseases among low literacy patients discharged from a Brazilian cardiology ward. Int J Clin Pharm. 2016;38:1362–6. doi: 10.1007/s11096-016-0390-6. [DOI] [PubMed] [Google Scholar]
- 24.Bhattacharya D. Final Report for the IMAB-Q Study: Validation and feasibility testing of a novel questionnaire to identify barriers to medication adherence. University of East Angila. http://pharmacyresearchuk.org/wp-content/uploads/2019/12/PG14_final_report_v2.pdf. Accessed 20 Aug 2019.
- 25.Kripalani S, Risser J, Gatti ME, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value Health. 2009;12(1):118–23. doi: 10.1111/j.1524-4733.2008.00400. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization (WHO). Process of translation and adaptation of instruments. 2016. Available at: http://www.who.int/substance_abuse/research_tools/translation/en/. Accessed 30 Oct 2018.
- 27.Dixon BE, Alzeer AH, Phillips EOK, Marrero DG. Integration of provider, pharmacy, and patient-reported data to improve medication adherence for type 2 diabetes: A controlled before-after pilot study. JMIR Med Inform. 2016;4(1):e4. doi: 10.2196/medinform.4739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Danladi J, Falang KD, Barde RA, Jimam NS, Dangiwa DA, Jimoh HO. Pharmaceutical care and medication adherence in management of psychosis in a Nigerian tertiary hospital. J Res Pharm Pract. 2013;2(2):83–7. doi: 10.4103/2279-042X.117388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sweileh WM, Zyoud SH, Abu Nab’a RJ, et al. Influence of patients’ disease knowledge and beliefs about medicines on medication adherence: findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14:94. doi: 10.1186/1471-2458-14-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ownby RL, Hertzog C, Crocco E, Duara R. Factors related to medication adherence in memory disorder clinic patients. Aging Ment Health. 2006;10(4):378–85. doi: 10.1080/13607860500410011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases. J Gen Intern Med. 2006;21(12):1215–21. doi: 10.1111/j.1525-1497.2006.00591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tiv M, Viel JF, Mauny F, Eschwège E, Weill A, Fournier C, Fagot-Campagna A, Penfornis A. Medication adherence in type 2 diabetes: the ENTRED study 2007, a French Population-Based Study. PLoS One. 2012;7:e32412. doi: 10.1371/journal.pone.0032412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saraiva EMS, Coelho JLG, dos Santos Figueiredo FW, do Souto RP, Medication non-adherence in patients with type 2 diabetes mellitus with full access to medicines, J Diabetes Metab Disord, 19 (2020) 1105-1113. [DOI] [PMC free article] [PubMed]
- 34.Bhuyan SS, Shiyanbola O, Deka P, Isehunwa OO, Chandak A, Huang S, Wang Y, Bhatt J, Ning L, Lin WJ, Wyant D, Kedia S, Chang CF. The role of gender in cost-related medication nonadherence among patients with diabetes. J Am Board Fam Med. 2018;31:743–51. doi: 10.3122/jabfm.2018.05.180039. [DOI] [PubMed] [Google Scholar]
- 35.Hussar DA. Patient Compliance. In: Troy D, editor. editor Remington. The Science and Practice of Pharmacy. 21. Philapdelphia: Lippincott Williams & Wilkins; 2005. pp. 1782–95. [Google Scholar]
- 36.Vlasnik JJ, Aliotta SL, DeLor B. Medication adherence: factors influencing compliance with prescribed medication plans. Case Manag. 2005;16:47–51. doi: 10.1016/j.casemgr.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Tsai KT, Chen JH, Wen CJ, et al. Medication adherence among geriatric outpatients prescribed multiple medications. Am J Geriatr Pharmacother. 2012;10(1):61–8. doi: 10.1016/j.amjopharm.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 38.Mukhtar O, Weinman J, Jackson SH. Intentional nonadherence to medications by older adults. Drugs Aging. 2014;31(3):149–57. doi: 10.1007/s40266-014-0153-9. [DOI] [PubMed] [Google Scholar]
- 39.Kulkarni AS, Balkrishnan R, Anderson RT, Edin HM, Kirsch J, Stacy MA. Medication adherence and associated outcomes in medicare health maintenance organization-enrolled older adults with Parkinson’s disease. Mov Disord. 2008;23(3):359–65. doi: 10.1002/mds.21831. [DOI] [PubMed] [Google Scholar]
- 40.Hsu YH, Mao CL, Wey M. Antihypertensive medication adherence among elderly Chinese Americans. J Transcult Nurs. 2010;21(4):297–305. doi: 10.1177/1043659609360707. [DOI] [PubMed] [Google Scholar]
- 41.Lam P, Lum C, Leung M. Drug nonadherence and associated risk factors among Chinese geriatric patients in Hong Kong. Hong Kong Med J. 2007;13(4):284. [PubMed] [Google Scholar]
- 42.Kassahun T, Gesesew H, Mwanri L, Eshetie T. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: a cross-sectional survey. BMC Endocr Disord. 2016;16(1):1–1. doi: 10.1186/s12902-016-0114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krzemińska S, Lomper K, Chudiak A, Ausili D, Uchmanowicz I. The association of the level of self-care on adherence to treatment in patients diagnosed with type 2 diabetes. Acta Diabetol. 2021;58(4):437–45. doi: 10.1007/s00592-020-01628-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. 2016;10:1299–307. doi: 10.2147/PPA.S106821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacoepidemiol Drug Saf. 2009;18(8):672–81. doi: 10.1002/pds.1766. [DOI] [PubMed] [Google Scholar]
- 46.Machen S, Jani Y, Turner S, Marshall M, Fulop NJ. The role of organizational and professional cultures in medication safety: a scoping review of the literature. Int J Qual Health Care. 2019;31:G146–57. doi: 10.1093/intqhc/mzz111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Waheedi M, Awad A, Hatoum HT, Enlund H. The relationship between patients’ knowledge of diabetes therapeutic goals and self-management behaviour, including adherence. Int J Clin Pharm. 2017;39:45–51. doi: 10.1007/s11096-016-0375-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed in this study are included in this article.