Abstract
The effects of lower tidal volume ventilation (LTV) were controversial for patients with acute respiratory distress syndrome (ARDS). This systematic review and meta-analysis aimed to evaluate the use of LTV strategy in patients with ARDS. We performed a literature search on MEDLINE, CENTRAL, EMBASE, CINAHL, “Igaku-Chuo-Zasshi”, clinical trial registration sites, and the reference of recent guidelines. We included randomized controlled trials (RCTs) to compare the LTV strategy with the higher tidal volume ventilation (HTV) strategy in patients with ARDS. Two authors independently evaluated the eligibility of studies and extracted the data. The primary outcomes were 28-day mortality. We used the GRADE methodology to assess the certainty of evidence. Among the 19,864 records screened, 13 RCTs that recruited 1874 patients were included in our meta-analysis. When comparing LTV (4–8 ml/kg) versus HTV (> 8 ml/kg), the pooled risk ratio for 28-day mortality was 0.79 (11 studies, 95% confidence interval [CI] 0.66–0.94, I2 = 43%, n = 1795, moderate certainty of evidence). Subgroup-analysis by combined high positive end-expiratory pressure with LTV showed interaction (P = 0.01). Our study indicated that ventilation with LTV was associated with reduced risk of mortality in patients with ARDS when compared with HTV.
Trial registration: UMIN-CTR (UMIN000041071).
Subject terms: Respiratory distress syndrome, Translational research
Introduction
Acute respiratory distress syndrome (ARDS) is a life-threatening condition due to respiratory failure, often requiring mechanical ventilation for survival1. One of the most important aspects of ventilation management is minimizing pressure-related damage (barotrauma), capacity damage (volutrauma), and ventilator-induced lung injury (VILI)2–4.
Limiting the tidal volume is one of the strategies of lung protection that help in reducing adverse events due to mechanical ventilation4,5. Limiting the tidal volume results in lower levels of systemic inflammatory mediators6 and might prevent VILI by minimizing pressure-related and capacity damage7–9. On the contrary, lowering the tidal volume might also cause lung damage due to atelectasis, hypoxia, hypercapnia, patient discomfort, increased use of sedation, and cyclic atelectasis10.
Several randomized controlled trials (RCTs) that have analyzed the usefulness of lowering the tidal volume have shown inconsistent results11–16. The Cochrane Systematic Review of six trials that included 1297 patients with ARDS showed that 28-day mortality was significantly reduced by lung-protective ventilation, with a risk ratio (RR) of 0.74 (95% confidence interval [CI] 0.61–0.88)5. A recent systematic review of seven RCTs that included 1481 patients with ARDS demonstrated a trend towards lower risk of mortality, but the difference was insignificant (RR 0.87; 95% CI 0.70–1.08)17.
Lower tidal volume ventilation (LTV) has potentially relevant benefits; however, the certainty of evidence is imprecise. To develop the Japanese ARDS guidelines 2021, an updated systematic review is warranted. Therefore, this systematic review and meta-analysis aimed to evaluate the usefulness of the lower tidal volume ventilation strategy for patients with ARDS.
Methods
Protocol and registration
Our study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol for RCTs18. The review protocol was submitted to the University Hospital Medical Information Network Clinical Trial Registry (UMIN-CTR) on July 7, 2020, before data extraction was initiated (identifier: UMIN000041071).
Eligibility criteria
We included RCTs or cluster RCTs and excluded crossover trials, quasi-randomized, and non-randomized trials. The target population was intubated patients with ARDS (age ≥ 16 years). ARDS was defined according to the 1988 definition19, or the American-European Consensus Conference criteria20, or the Berlin definition21, or other authors’ definitions. We included studies that compared the LTV strategy with usual or higher tidal volume ventilation (HTV) strategy. We included a variety of tidal volume settings. For example, if there was a difference in the tidal volume between the two groups 24–72 h after the intervention due to differences in the method of setting tidal volume (specifying target tidal volume, a setting of the driving pressure, any protocol, or programmatic algorithms), we included them in this review (Additional File 1).
Data sources and searches
We performed a literature search on MEDLINE through PubMed, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Igaku-Chuo-Zasshi (Ichu-shi), a Japanese bibliographic database, from inception until July 2020. Our search strategies are described in an additional file (Additional File 1). We also performed searches for ongoing trials in the following trial registries: The World Health Organization International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/) and the United States National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov). We searched for references among the guidelines on the management of ARDS22–24 and the extracted articles. There were no language restrictions on any of the searches.
Study selection and data extraction
Titles and abstracts were assessed for potential relevance independently by two reviewers (YF, YK, SO, SW, SS, NS, and RY). We retrieved the full text of study reports or publications. Two assessors independently screened the full texts, identified studies for inclusion, and verified the reasons for the exclusion of ineligible studies. Differences were resolved by discussion and, where this failed, through arbitration by a third author (CN). We contacted the authors of these studies if necessary. We recorded the selection process with appropriate details to construct a PRISMA flow diagram18. Data extraction was carried out using standard data extraction forms by two authors independently. Differences in opinion regarding data collection were resolved using the same methods.
Type of outcome measures
The primary outcome was 28-day mortality. If 28-day mortality was not reported, then we used the mortality of the nearest 28 days at follow-up. The secondary outcomes were longest follow-up mortality, health-related quality of life (QOL), PaO2/FiO2 (P/F) ratio on day 1, ventilation-free day (VFD) up to 28 days, hospital length of stay (LOS), and barotrauma. Definitions of these outcomes are described in additional files (Additional File 1).
Assessment of risk of bias
Two review authors independently evaluated the risk of bias in the included studies using the Cochrane risk of bias assessment tool, version 125. These reviewers graded each potential source of bias as “high,” “low,” or “unclear.” Disagreements between the two reviewers regarding the risk of bias were resolved by discussion, with the involvement of a third reviewer (CN).
Analysis and results synthesis
We calculated measures of treatment effects using the Cochrane Statistical Package Review Manager 5 (Cochrane Collaboration, London, UK) for data synthesis and analysis. We analyzed dichotomous data (mortality, barotrauma) as RR with 95% CIs, and continuous data (such as QOL, VFD, LOS) as mean difference (MD) with 95% CI.
We planned to perform meta-analyses for separate comparisons because of the heterogeneity of the interventions. We pooled the following predefined comparisons:
Comparison of target tidal volumes 4–8 ml/kg predicted body weight (PBW) or ideal body weight (IBW) and above 8 ml/kg/PBW or IBW
Comparison of any (author-defined) LTV and normal or HTV strategies. To identify all RCTs that compared LTV and HTV, we did not specifically target tidal volume.
Comparison of very low tidal ventilation (less than 6 mL/kg PBW or IBW) and low tidal ventilation (6–8 mL/kg PBW).
Studies on extracorporeal membrane oxygenation (ECMO) were qualitatively integrated and reported separately.
We used a random-effects model for data synthesis because we assumed that clinical and methodological diversity exists and that intervention effects across studies are not entirely identical. We calculated the Chi2 test and the I2 statistic to measure heterogeneity. A P-value of less than 0.1 was considered statistically significant in the Chi2 test. To assess publication bias, we created a funnel plot and examined Egger’s test (P < 0.05, significant reporting bias) if each comparison included more than ten studies26,27.
Subgroup-analysis and sensitivity analysis
We planned subgroup analyses for primary outcomes to determine whether the results differed by one of the following: ARDS definition (the Berlin definition or not), open lung therapy (LTV plus higher positive end-expiratory pressure (PEEP) vs. HTV plus low PEEP), severity (P/F ≤ 200 mmHg or not), and control group target tidal volume (> 8 ml/kg vs 6–8 ml/kg). In sensitivity analyses, we included only studies with “low risk of bias” to assess the robustness of our conclusions for the primary outcomes. We performed another sensitivity analysis that compared LTV vs. HTV excluding studies where the average tidal volume was > 11 ml/kg on day 1 in the control group.
Post-hoc analysis
We conducted a post hoc meta-analysis of trials conducted since 2010 comparing any very low tidal volumes (author-defined) with any LTV (author-defined). In this analysis, we included trials that assessed the usefulness of LTV during ECMO for quantitative analysis.
Assessment of the certainty of evidence
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) considerations (risk of bias, consistency of effect, imprecision, indirectness, and publication bias) to evaluate the quality of the evidence based on the studies that contributed data to the meta-analyses for mortality and QOL, classifying the quality as “high,” “moderate,” “low,” or “very low”28. We used GRADEpro GDT software.
Results
Study selection
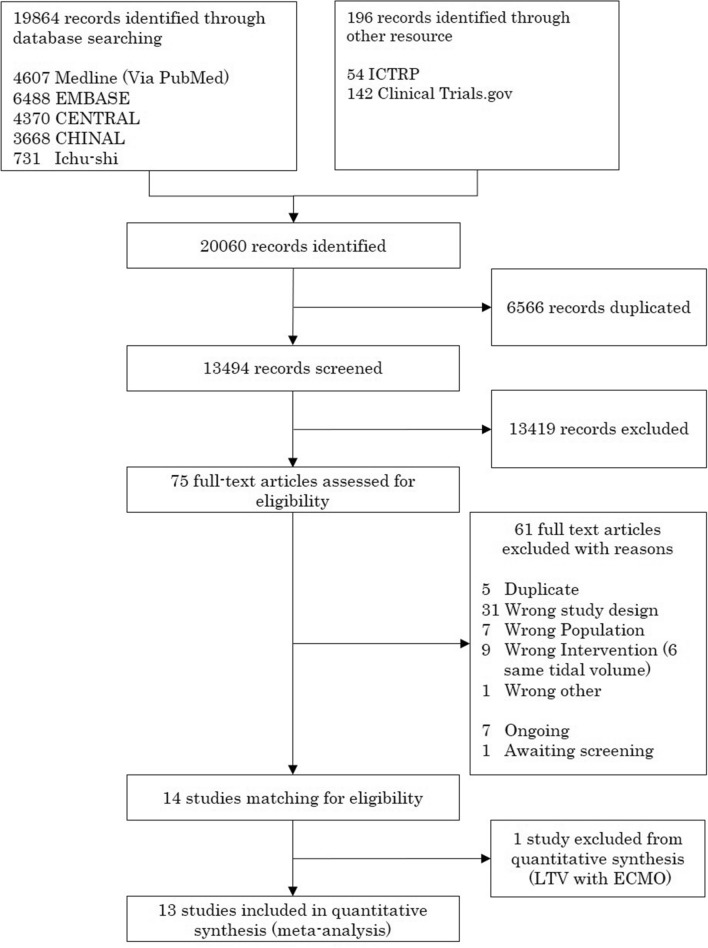
We identified 20,060 records through literature search. After removing duplicates and title and abstract screening, 75 studies were evaluated in detail and 61 were excluded (Fig. 1, Additional File 1; Supplementary Table 2). Fourteen RCTs met the eligibility criteria, and one trial assessed the usefulness of LTV during ECMO6,11–16,29–35. Therefore, 13 randomized trials that included 1874 patients were included in the quantitative synthesis for comparing LTV versus HTV.
Figure 1.
PRISMA flow diagram.
Study characteristics
The study characteristics are summarized in Table 1. For comparing LTV (4–8 ml/kg) versus HTV (> 8 ml/kg), we included 11 trials6,11–16,30–33. We added two trials comparing the small difference in targeting tidal volume for meta-analysis in comparison to any LTV versus any HTV34,35. Because one trial compared very low tidal volume ventilation with low tidal ventilation, we could not perform a meta-analysis on this comparison34. Tidal volumes at days 1, 3, and 7 are described in additional files (Supplementary Table 1).
Table 1.
Characteristics of the included trials.
| Study | No. of center | Definition of ARDS/ALI | *Severity P/F ratio | Intervention | Control | Mortality Outcome |
|---|---|---|---|---|---|---|
| Comparison of lower tidal volume (6–8 ml/kg) versus higher tidal volume(> 8 ml/kg) | ||||||
| Amato 199811 | 2 | LISS | NA | Vt 6 ml/kg | Vt 12 ml/kg | ICU, 28-day, in-hospital |
| PEEP: preset at 2 cm of water above Pflex | PEEP: stepwise algorithm for PEEP increments | |||||
| PCV | ||||||
| Brochard 199812 | 25 | LISS | NA | Vt 6–10 ml/kg PBW, Pplat < 25 cm H2O | Vt 10–15 ml/kg PBW, peak airway pressure < 60 cm H2O | 30-day (from KM), 60-day |
| PEEP: increments of 5 cm H2O (from 0 to 15) during pure oxygen breathing to determine the optimal level | PEEP: increments of 5 cm H2O (from 0 to 15) during pure oxygen breathing to determine the optimal level | |||||
| VCV A/C | VCV A/C | |||||
| Stewart 199815 | 8 | Other author's definition | < 250 | Vt 8 ml/kg IBW, peak pressure < 30 cm H2O | Vt 10–15 ml/kg IBW, peak pressure < 50 cm of water | 30-day (from KM), in-hospital |
| PEEP: the range of 5 to 20 cm H2O was adjusted in increments of 2.5 cm H2O | PEEP: the range of 5 to 20 cm H2O was adjusted in increments of 2.5 cm H2O | |||||
| VCV A/C | VCV A/C | |||||
| Wu 199830 | 1 | Other author's definition | ≤ 300 | VT 7–10 ml/kg actual BW | VT 10–15 ml/kg | In-hospital |
| PEEP: titrated to PaO2 (range 3–12 cm H2O) | PEEP: titrated to PaO2 (range 3–12 cm H2O) | |||||
| AC and SIMV/PS | AC and SIMV/PS | |||||
| East 1999†31 | 10 | Other author's definition | < 200 | Vt 6 ml/kg IBW (titillated by computerized decision support) | Vt < 10 mL/kg IBW | In-hospital |
| PEEP: Computerized Protocol, A/C | PEEP: stepwise increments of PEEP, IMV | |||||
| Brower 199914 | 4 | AECC 1994 | ≤ 200 | Vt 5–8 mL/kg IBW, Pplat < 30 cm H2O | Vt 10–12 mL/kg IBW, Pplat < 55 cm H2O | In-hospital |
| PEEP: FiO2 table | PEEP: FiO2 table | |||||
| VCV A/C | VCV A/C | |||||
| Ranieri 19996 | 2 | AECC 1994 | < 200 | Vt 5 to 8 mL/kg IBW | No target, plateau airway pressure < 35 cm H2O | 28-day |
| PEEP: The PEEP was set at 2 to 3 cm H2O higher than the pressure at Pflex | PEEP: PEEP trial on 100% FiO2 was performed using incremental (3–5 cm H2O) levels from 3 to 15 cm H2O | |||||
| VCV | VCV, maintain PaCO2 35–40 mmHg | |||||
| ARDSnet 200013 | 10 | AECC 1994 | ≤ 300 | Vt 6 (4–8)ml/kg PBW, Pplat < 30 cm H2O PEEP: FiO2 table VCV A/C | Vt 12 ml/kg PBW, Pplat < 50 cm H2O PEEP: FiO2 table VCV A/C | 30-day (from KM), Death before a patient was discharged home |
| Orme 200332 | 1 | Other author's definition | ≤ 150 | Vt 4–8 ml/kg PBW, Pplat < 40 cm H2O | Vt 10–15 ml/kg PBW, Pplat < 70 cm H2O | In-hospital |
| PEEP: Computerized rules to maintain PaO2 above 55 | PEEP: Computerized rules to maintain PaO2 above 55 | |||||
| Villar 200616 | 8 | AECC 1994 | ≤ 200 | Vt 5–8 mL/kg PBW | Vt of 9–11 mL/kg PBW | ICU, in-hospital, 30-day (from KM) |
| PEEP: set on day 1 at Pflex + 2 cm H2O | PEEP: above 5 cm H2O, and an FiO2 ensuring arterial oxygen saturation 90% and PaO2 of 70–100 mm Hg | |||||
| VCV A/C | VCV A/C | |||||
| Sun 200933 | 1 | Other author's definition | ≤ 200 | Vt 4–6 ml/kg PBW | Vt < 12 ml/kg, Pplat < 30 | 28-day, in-hospital |
| PEEP: ARDSnet clinical trials | PEEP: ARDSnet clinical trials | |||||
| VCV | SIMV + PS or PS | |||||
| Comparison of any lower tidal volume versus any higher tidal volume | ||||||
| Pereira 202035 | 5 | Berlin Definition | P/F ≤ 300 | Vt 4–8 ml/kg PBW, driving pressure of 10 cm H2O | Vt 6 ml/kg PBW, Pplat below 30 cm H2O | 28-day, ICU, in-hospital |
| PEEP: ARDSNet low-PEEP table | PEEP: ARDSNet low-PEEP table | |||||
| VCV or PCV | VCV or PCV | |||||
| Agarwal 201334 | 1 | AECC 1994 | P/F ≤ 200 | Vt 6 mL/kg PBW, Pplat < 30–35 cm H2O | Percentage MV (%MV) | 30-day (from KM), in-hospital |
| PEEP: ARDSnet protocol | PEEP: ARDSnet protocol | |||||
| VCV | ASV | |||||
| Comparison of lower tidal volume versus higher tidal volume during ECMO | ||||||
| Thomas 2013 29 | 10 | AECC 1994 | P/F < 200 | Vt 3 ml/kg/PBW, assisted by avECCO2-R | Vt 6 ml/kg/PBW | In-hospital |
| PEEP: ARDSNet ‘‘high-PEEP/FiO2’’ table | PEEP: ARDSNet ‘‘high-PEEP/FiO2’’ table | |||||
ARDS Acute Respiratory Distress Syndrome, ALI Acute Lung Injury, P/F PaO2/FiO2, Int intervention, Cont control, PEEP positive end-expiratory pressure, Pflex lower inflection point of a pressure–volume curve, Pplat plateau pressure during inspiratory pause, Vt volume tidal, PBW predicted body weight, IBW ideal body weight, LISS The Lung Injury Severity Score, Dry BW Actual body weight minus the estimated weight gain due to salt and water retention, VCV volume-controlled ventilation, PCV pressure-controlled ventilation, A/C assist control, ASV adaptive support ventilation, MV mechanical ventilation, ICU intensive care unit, KM Kaplan–Meier.
*Severity used in inclusion criteria.
†Data extracted from Burns et al. and a subgroup with trauma-induced ARDS by McKinley et al.
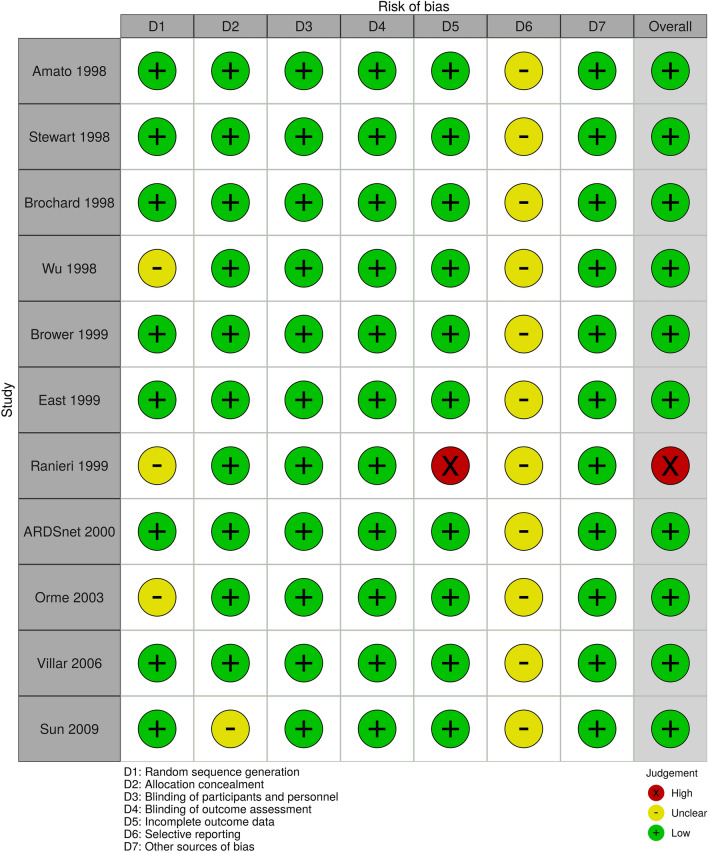
Risk of bias assessment
The risk of bias for mortality was low when comparing LTV (4–8 ml/kg) versus HTV (> 8 ml/kg) (Fig. 2). Masking was not performed due to the nature of the intervention in all studies, and we assessed objective outcomes such as mortality and P/F ratio as low risk of bias because it was not influenced by unmasking36. We evaluated subjective outcomes such as QOLs, VFD up to 28 days, LOS, and barotrauma as “unclear” risk of bias. With respect to incomplete outcomes, one study was found to have a high risk of bias because seven patients were excluded after randomization and complete-case analyses were performed for all outcomes6. All studies evaluated selection outcome reporting as “unclear” risk of bias because study protocols were not available. Funnel plots and Egger's test did not indicate the presence of publication bias (Egger's test p = 0.66; Supplementary Fig. 1). The risk of bias assessment of the other comparison was also similar (Additional file 1; Supplementary Figs. 2 and 3).
Figure 2.
Traffic light plot of the risk of bias.
Meta-analyses of the results
LTV (4–8 ml/kg) versus HTV (> 8 ml/kg)
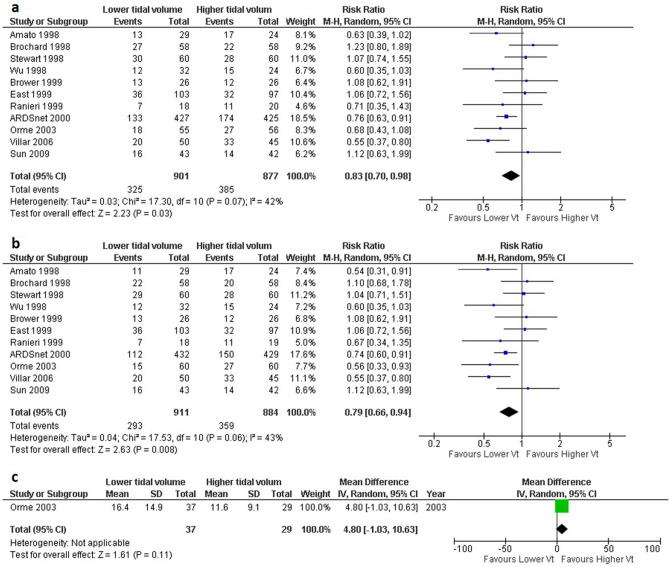
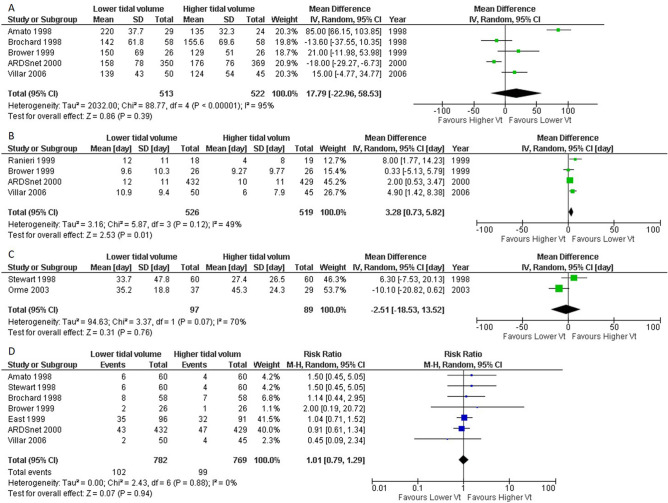
Regarding 28-day mortality and longest-follow-up mortality, the pooled RRs were · 0.79 (11 studies, 95% CI 0.66–0.94, I2 = 43%, n = 1795, Fig. 3A) and 0.83 (11 studies, 95% CI 0.70–0.98, I2 = 43%; n = 1778; Fig. 3B). Regarding QOL, only one study investigated the sickness impact profile28, MD was 4.80 (95% CI − 1.03–10.63, n = 66, Fig. 3C). The results of the meta-analysis for other secondary outcomes are summarized in Fig. 4. The VFD up to 28 days in the LTV group was significantly increased compared to that in the HTV group (4 studies, MD 3.28 days, 95% CI 0.73–5.82, I2 = 49%, n = 1045, Fig. 4B). For the other secondary outcomes, there were no significant differences between the LTV group and the HTV group (Fig. 4A, C, D).
Figure 3.
Forest plot showing the comparison of low tidal volume ventilation (LTV; 4–8 ml/kg) versus high tidal volume ventilation (HTV; > 8 ml/kg) for mortality and QOL. (a) 28-day mortality. Data extracted from the Kaplan–Meier curve at 28 days; Brochard 1998, Stewart 1998, ARDSnet 2000, and Villar 2006, in-hospital mortality; Wu 1998, East 1999, Brower 1999, and Orme 1999, 28-day mortality; the other studies. (b) the longest follow-up mortality. Data extracted from the Kaplan–Meier curve at 28 days; Villar 2006, 28-day mortality; Ranieri 1999, Sun 2009, 60-day mortality; Brochard 1998, 1-year mortality; Orme 2003. In-hospital mortality; other studies (c) quality of life (sickness impact profile) CI confidence interval; M–H Mantel–Haenszel method, IV inverse variance, QOL quality of life.
Figure 4.
Forest plot showing the comparison of low tidal volume ventilation (LTV; 4–8 ml/kg) versus high tidal volume ventilation (HTV; > 8 ml/kg) for secondary outcomes. (a) PaO2/FiO2 ratio on day 1. (b) Ventilator-free days up to 28 days. (c) Length of hospital stay, (d) Barotrauma CI confidence interval, IV inverse variance, M–H Mantel–Haenszel method.
Any (author-defined) LTV versus any HTV
We added two trials comparing the small difference in targeting tidal volume for the comparison of LTV versus HTV34,35. Actual tidal volumes at days 1, 3, and 7 are described in additional files (Supplementary Table 1). Thirteen studies were identified which evaluated the impact on mortality. The meta-analysis showed that 28-day mortality had an RR of 0.84 (13 studies, 95% CI 0.70–1.00, I2 = 49%, n = 1874, Supplementary Fig. 4A), and the longest follow-up mortality had an RR of 0.86 (13 studies, 95% CI 0.73–1.01, I2 = 45%, n = 1857, Supplementary Fig. 4B). Regarding other outcomes, there was no significant difference between any LTV and any HTV (Supplementary Fig. 4C and Supplementary Fig. 5).
Subgroup and sensitivity analyses
Pre-planned subgroup analyses for the comparison of LTV (4–8 ml/kg) versus HTV (> 8 ml) for mortality by the definition of ARDS (Berlin vs. other), open lung therapy (LTV plus higher PEEP vs. HTV plus low PEEP), and severity of inclusion criteria (P/F ratio ≤ 200 vs. > 200) were performed. The subgroup defining ARDS could not be reported. A subgroup analysis of 11 studies reporting 28-day mortality6,11–16,26–29 by open lung therapy demonstrated a significant reduction in mortality (test for subgroup differences: Chi2 = 6.42, P for interaction 0.01; Supplementary Fig. 6A). The subgroup analysis for nine studies reporting 28-day mortality according to the severity of inclusion criteria did not show any subgroup interaction (test for subgroup differences: Chi2 = 0.00, P for interaction 0.98; Supplementary Fig. 6B).
In comparison to any LTV vs any HTV, subgroup analysis for 13 studies reporting 28-day mortality according to the control group target tidal volume (> 8 ml/kg vs 6–8 ml/kg) showed a significant subgroup interaction (test for subgroup differences: Chi2 = 0.05, P for interaction 0.02; Supplementary Fig. 7).
We performed the sensitivity analysis exploring the impact of influence of high risk of bias on the comparison of LTV (4–8 ml/kg) versus HTV (> 6 ml/kg) and found similar results (Supplementary Fig. 8). To explore the impact of influence of tidal volume of control groups, we performed another sensitivity analysis that compared LTV vs. HTV excluding studies where average tidal volume was > 11 ml/kg on day 1 in the control group. Regarding 28-day mortality and longest-follow-up mortality, the pooled RRs were 0.84 (3 studies, 95% CI 0.54–1.33, I2 = 73%, n = 331; Supplementary Fig. 9A) and 0.89 (3 studies, 95% CI 0.54–1.46, I2 = 79%; n = 331; Supplementary Fig. 9B).
Post-hoc analysis
We performed a post hoc analysis of all trials conducted since 2010 comparing any very low tidal volumes (author-defined) with any LTV (author-defined)29,34,35. The analysis showed that 28-day mortality and longest-follow-up mortality were not significant, however, increase in mortality was observed in the very low tidal volume group than the LTV group (28-day mortality; RR 1.35, 95% CI 0.90–2.02, longest follow up mortality; RR 1.18, 95% CI 0.81–1.73; Supplementary Fig. 10). In addition, we described the relationship between target tidal volume and mortality in the intervention and control arms in all included studies (Supplementary Fig. 11).
Certainty of evidence
Certainty of evidence for mortality was downgraded by one level for inconsistency and considered moderate. The certainty of evidence for QOL was low because of the serious risk of bias and had very serious imprecision (Table 2; Supplementary Table 3).
Table 2.
Evidence tables of the systematic review. Comparison: (A) Lower tidal volume (6–8 ml/kg) compared to higher tidal volume (> 8 ml/kg) in patients with ARDS; (B) Any lower tidal volume compared to any higher tidal volume in patients with ARDS.
| Certainty assessment | No of patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Lower tidal volume (< 6 ml/kg) | Higher tidal volume (6-8 ml/kg) | Relative (95% CI) |
Absolute (95% CI) |
|
| Panel A | |||||||||||
| 11 | Randomized trials | Not serious | Seriousa | Not serious | Not serious | None | 293/911 (32.2%) | 359/884 (40.6%) |
RR 0.79 (0.66 to 0.94) |
85 fewer per 1000 (from 138 to 24 fewer) |
⨁⨁⨁◯ MODERATE |
| 11 | Randomized trials | Not serious | Seriousa | Not serious | Not serious | None | 325/901 (36.1%) | 385/877 (43.9%) |
RR 0.83 (0.70 to 0.98) |
75 fewer per 1000 (from 132 to 9 fewer) |
⨁⨁⨁◯ MODERATE |
| 1 | Randomized trials | Seriousb | Not serious | Not serious | Very seriousc | None | 37 | 29 | – |
MD 4.8 higher (1.03 lower to 10.63 higher) |
⨁◯◯◯ VERY LOW |
| Certainty assessment | No of patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Any lower tidal volume | Any higher tidal volume | Relative (95% CI) |
Absolute (95% CI) |
|
| Panel B | |||||||||||
| 13 | Randomized trials | Not serious | Seriousa | Not serious | Seriousd | None | 317/952 (33.3%) | 375/922 (40.7%) |
RR 0.84 (0.70 to 1.00) |
65 fewer per 1000 (from 122 to 0 fewer) |
⨁⨁◯◯ LOW |
| 13 | Randomized trials | Not serious | Seriousa | Not serious | Seriousd | None | 349/942 (37.0%) | 404/915 (44.2%) |
RR 0.86 (0.73 to 1.01) |
62 fewer per 1000 (from 119 fewer to 4 more) |
⨁⨁◯◯ LOW |
| 1 | Randomized trials | Seriouse | Not serious | Not serious | Very seriousd,f | None | 37 | 29 | – |
MD 4.8 higher (1.03 lower to 10.63 higher) |
⨁◯◯◯ VERY LOW |
CI Confidence interval, RR Risk ratio, MD Mean difference.
aDifferent directions of effect in the study.
bMost of the studies have a high risk of bias.
cThe wide confidence interval, sample size did not reach the Optimal Information Size.
dThe wide confidence interval.
eIncomplete outcome data.
fUnreached Optimal Information Size.
Discussion
Our systematic review and meta-analysis showed that LTV (4–8 ml/kg) reduces 28-day mortality, longest follow-up mortality, and increase in VFD up to 28 days for adult ARDS patients. There was no significant effect on P/F ratio, QOL, LOS, and barotrauma. When comparing any LTV versus any HTV, we found a similar trend towards lower mortality with any LTV (author’s definition) in ARDS. In addition, the post-2010 study used a lower tidal volume in the control group than in the pre-2010 study.
Previous systematic reviews have reported various results5,17,37,38. The potential reasons for the difference between our findings and past findings include studies6,15, searching methods, definition of LTV, and the use of a random-effects model. We included a trial that enrolled patients at risk of developing ARDS15. However, the inclusion criteria for the P/F ratio were below 250 mmHg in this trial; therefore, we considered this population to be ARDS. In the 2016 Japanese ARDS guidelines, only six studies were included. We searched the literature with no language restriction and searched the trial registration database and reference for guidelines, and included 13 RCTs in our systematic review.
Another significant contribution of this review is that we investigated a comparison of any LTV versus any HTV that was included in the 13 studies. The effect size tended to be smaller than that of LTV 4–8 ml/kg compared with HTV (> 8 ml/kg). This may be due to the small difference in tidal volume between the intervention and control groups34,35. In a meta-regression analysis, Walkey showed that the effect tended to be smaller when the difference in the ventilation rate between the two groups was smaller17. Recent studies have focused on limiting the tidal volume or pressure while avoiding high tidal volumes in the control group29,34,35.
Our study suggests with moderate certainty that limiting the tidal volume to 4–8 ml/kg is desirable in the ventilatory management of patients with ARDS. No significant increase in harm (such as increasing barotrauma or decreasing P/F ratio) was found, but the certainty of evidence was very low. However, given the low cost and simplicity of the intervention and the survival benefit, limited tidal volume might be considered routinely. This suggestion is similar to that reported in other guidelines22–24,39.
Previous individual meta analysis indicated that the benefit of higher PEEP in ARDS patients receiving LTV40. However, this study did not examine the effect modification of higher PEEP on LTV. In our subgroup analysis, we found an effect modification when combined with a higher PEEP. This result is consistent with the results of a recent network meta-analysis41. Sud et al. showed that LTV combined with high PEEP was more effective than HTV, although the best effective strategy was LTV combined with prone positioning. In our study, we were unable to examine the effect modification of prone positioning on LTV due to a lack of data. The Alveolar Recruitment Trial (ART), which used very high levels of PEEP to recruit the lung showed increased mortality at 28 days42. If a very high PEEP is used, the effect modification on LTV may be small.
A comparison between a very low tidal volume and a lower tidal volume was not synthesized because there was only one study. Therefore, we added a post hoc analysis to compare any very low tidal volume with any low tidal volume. This meta-analysis showed that very low tidal volume tended to increase mortality compared with LTV, but this was not significant. Excessive ventilation limitations can lead to harm, but more studies are needed to verify how low tidal volumes are better. Similarly, there is a lack of evidence of LTV during ECMO.
Our study had several potential limitations. First, there was clinical heterogeneity due to differences in interventions: one study used a combined intervention with a recruitment maneuver (RM)11, and several studies did not describe whether they used RM6,14,15,31,32. Therefore, there might be heterogeneity due to RM, and there was heterogeneity because we included RCTs that examined the effect of LTV combined with high PEEP. Our subgroup analysis separately showed the effect of the combination of high PEEP and similar PEEP. Second, one study failed to complete the inclusion evaluation43. Chen compared pressure-limited ventilation (plateau pressure < 30 mmHg) with HTV (10–15 ml/kg), which might be included in our systematic review. However, because we could not identify the tidal volume after the intervention, this study was awaiting inclusion. Finally, in this systematic review, we performed many analyses. Caution should be exercised in the interpretation of results for secondary analyses, subgroup analyses, and sensitivity analyses.
Conclusions
This systematic review and meta-analysis demonstrated that ventilation using LTV was associated with reduced risk of mortality in patients with ARDS compared with HTV. Our study suggests with moderate certainty evidence that limiting the tidal volume to 4–8 ml/kg is desirable in the ventilatory management of patients with ARDS. More studies are needed to verify how low tidal volumes are better.
Supplementary Information
Acknowledgements
We thank all the members of the Japanese ARDS clinical practice guideline committee. We also appreciate Takaaki Suzuki, Nara Medical University Library and the librarian Kyoto Prefectural University of Medicine Medical Library) for developing a search strategy. We sincerely thank Dr. Takeaki Funamoto and Dr. Zhuan Jin for searching Chinese articles and translating Chinese. We would like to thank Editage (www.editage.com) for English language editing.
Author contributions
R.Y., C.N., and Y.N. contributed to the conception and design of the review. Y.F., Y.K., S.O., S.W., S.S., N.S., and R.Y. screened the title and abstract for eligible criteria, performed the full-text review, extracted the data, and assessed the risk of bias. R.Y. and S.O. performed data analysis and statistical analysis. R.Y. prepared the draft of the manuscript. All authors approved the final version of the manuscript.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The data and material used for this meta-analysis were obtained from the articles in our list of references.
Competing interests
The authors declare that they have no financial competing interests. This systematic review was performed as a part of developing ARDS guideline 2021. ARDS guideline committee has no role in the analysis and interpretation of the data.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-13224-y.
References
- 1.Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N. Engl. J. Med. 2017;377:1904–1905. doi: 10.1056/NEJMra1608077. [DOI] [PubMed] [Google Scholar]
- 2.Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am. Rev. Respir. Dis. 1988;137:1159–1164. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 3.Marini JJ. Lung mechanics in the adult respiratory distress syndrome. Recent conceptual advances and implications for management. Clin. Chest Med. 1990;11:673–690. doi: 10.1016/S0272-5231(21)00762-0. [DOI] [PubMed] [Google Scholar]
- 4.Hashimoto S, et al. The clinical practice guideline for the management of ARDS in Japan. J. Intensive Care. 2017;5:50. doi: 10.1186/s40560-017-0222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petrucci N, De Feo C. Lung protective ventilation strategy for the acute respiratory distress syndrome. Cochrane Database Syst. Rev. 2013;2:CD003844. doi: 10.1002/14651858.CD003844.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranieri VM, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: A randomized controlled trial. JAMA. 1999;282(1):54–61. doi: 10.1001/jama.282.1.54. [DOI] [PubMed] [Google Scholar]
- 7.Hickling KG, Henderson SJ, Jackson R. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med. 1990;16:372–377. doi: 10.1007/BF01735174. [DOI] [PubMed] [Google Scholar]
- 8.Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit. Care Med. 1994;22:1568–1578. doi: 10.1097/00003246-199422100-00011. [DOI] [PubMed] [Google Scholar]
- 9.Artigas A, et al. The American–European consensus conference on ARDS, Part 2. Ventilatory, pharmacologic, supportive therapy, study design strategies and issues related to recovery and remodeling. Intensive Care Med. 1998;24:378–398. doi: 10.1007/s001340050585. [DOI] [PubMed] [Google Scholar]
- 10.Roupie E, et al. Prevalence, etiologies and outcome of the acute respiratory distress syndrome among hypoxemic ventilated patients. SRLF Collaborative Group on Mechanical Ventilation. Société de Réanimation de Langue Française. Intensive Care Med. 1999;25:920–929. doi: 10.1007/s001340050983. [DOI] [PubMed] [Google Scholar]
- 11.Amato MBP, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N. Engl. J. Med. 1998;338:347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 12.Brochard L, et al. Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. The Multicenter Trail Group on Tidal Volume reduction in ARDS. Am. J. Respir. Crit. Care Med. 1998;158:1831–1838. doi: 10.1164/ajrccm.158.6.9801044. [DOI] [PubMed] [Google Scholar]
- 13.Acute Respiratory Distress Syndrome Network, Brower, R.G. et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med.342, 1301–1308 (2000) [DOI] [PubMed]
- 14.Brower RG, et al. Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit. Care Med. 1999;27:1492–1498. doi: 10.1097/00003246-199908000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Stewart TE, et al. Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and Volume-Limited Ventilation Strategy Group. N. Engl. J. Med. 1998;338:355–361. doi: 10.1056/NEJM199802053380603. [DOI] [PubMed] [Google Scholar]
- 16.Villar J, Kacmarek RM, Pérez-Méndez L, Aguirre-Jaime A. A high positive end-expiratory pressure, low tidal volume ventilatory strategy improves outcome in persistent acute respiratory distress syndrome: A randomized, controlled trial. Crit. Care Med. 2006;34:1311–1318. doi: 10.1097/01.CCM.0000215598.84885.01. [DOI] [PubMed] [Google Scholar]
- 17.Walkey AJ, et al. Low tidal volume versus non-volume-limited strategies for patients with acute respiratory distress syndrome. A systematic review and meta-analysis. Ann. Am. Thorac. Soc. 2017;14:S271–S279. doi: 10.1513/AnnalsATS.201704-337OT. [DOI] [PubMed] [Google Scholar]
- 18.Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G & PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann. Intern. Med.151, 264–269, W64 (2009) [PMC free article] [PubMed]
- 19.Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am. Rev. Respir. Dis. 1988;138:720–723. doi: 10.1164/ajrccm/138.3.720. [DOI] [PubMed] [Google Scholar]
- 20.Bernard GR, et al. The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am. J. Respir. Crit. Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 21.the Berlin Definition ARDS Definition Task Force, Ranieri, V.M. et al. Acute respiratory distress syndrome. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 22.Fan E, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 23.Griffiths MJD, et al. Guidelines on the management of acute respiratory distress syndrome. BMJ. Open Respir. Res. 2019;6:e000420. doi: 10.1136/bmjresp-2019-000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alhazzani W, et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus Disease 2019 (COVID-19) Crit. Care Med. 2020;48:e440–e469. doi: 10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins JP, et al. The Cochrane Collaboration. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 28.Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J. Clin. Epidemiol. 2011;64:380–382. doi: 10.1016/j.jclinepi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 29.Bein T, et al. Lower tidal volume strategy (≈ 3 ml/kg) combined with extracorporeal CO2 removal versus 'conventional' protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med. 2013;39:847–856. doi: 10.1007/s00134-012-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu G, Lu B. The application of low tidal volume pressure-controlled ventilation in patients with acute respiratory distress syndrome. Hunan Yi Ke Da Xue Bao. 1998;23:57–58. [PubMed] [Google Scholar]
- 31.East TD, et al. Efficacy of computerized decision support for mechanical ventilation: Results of a prospective multi-center randomized trial. Proc. AMIA. Symp. 1999;66:251–255. [PMC free article] [PubMed] [Google Scholar]
- 32.Orme J, Jr, et al. Pulmonary function and health-related quality of life in survivors of acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2003;167:690–694. doi: 10.1164/rccm.200206-542OC. [DOI] [PubMed] [Google Scholar]
- 33.Sun JJ, et al. Clinical effects of low-stretch ventilation on acute respiratory distress syndrome. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2009;21:609–612. [PubMed] [Google Scholar]
- 34.Agarwal R, Srinivasan A, Aggarwal AN, Gupta D. Adaptive support ventilation for complete ventilatory support in acute respiratory distress syndrome: A pilot, randomized controlled trial. Respirology. 2013;18:1108–1115. doi: 10.1111/resp.12126. [DOI] [PubMed] [Google Scholar]
- 35.Pereira Romano ML, et al. Driving pressure-limited strategy for patients with acute respiratory distress syndrome. A pilot randomized clinical trial. Ann. Am. Thorac. Soc. 2020;17:596–604. doi: 10.1513/AnnalsATS.201907-506OC. [DOI] [PubMed] [Google Scholar]
- 36.Wood L, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: Meta-epidemiological study. BMJ. 2008;336:601–605. doi: 10.1136/bmj.39465.451748.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burns KE, et al. Pressure and volume limited ventilation for the ventilatory management of patients with acute lung injury: A systematic review and meta-analysis. PLoS ONE. 2011;6:e14623. doi: 10.1371/journal.pone.0014623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moran JL, Bersten AD, Solomon PJ. Meta-analysis of controlled trials of ventilator therapy in acute lung injury and acute respiratory distress syndrome: An alternative perspective. Intensive Care Med. 2005;31:227–235. doi: 10.1007/s00134-004-2506-z. [DOI] [PubMed] [Google Scholar]
- 39.Papazian L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann. Intensive Care. 2019;9:69. doi: 10.1186/s13613-019-0540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Briel M, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: Systematic review and meta-analysis. JAMA. 2010;303:865–873. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 41.Sud S, et al. Comparative effectiveness of protective ventilation strategies for moderate and severe acute respiratory distress syndrome. A network meta-analysis. Am. J. Respir. Crit. Care Med. 2021;203:1366–1377. doi: 10.1164/rccm.202008-3039OC. [DOI] [PubMed] [Google Scholar]
- 42.Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators. Effect of Lung recruitment and titrated Positive End-Expiratory Pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: A randomized clinical trial. JAMA. 318, 1335–1345 (2017) [DOI] [PMC free article] [PubMed]
- 43.Haobo C. Inspiratory plateau pressure controlling mechanical ventilation on traumatic ARDS. Chin. J. Prim. Med. Pharm. 2004;11:144–145. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and material used for this meta-analysis were obtained from the articles in our list of references.