Abstract
Purpose
We aimed to review existing evidence on nutrition associations with gestational diabetes mellitus (GDM) development and management among Iranian women.
Methods
Web of Science, PubMed, Scopus, SID, and Magiran were searched up to August 2020. Observational studies on associations between circulatory markers of vitamins and minerals, dietary intakes, and GDM and clinical trials of the effects of nutritional supplementations or dietary modifications on management or prevention of GDM among Iranian women were selected.
Results
We reviewed 49 publications. Pooled analyses revealed that GDM women had lower serum vitamin D (-8.31 nmol/l (95% CIs= -14.4, -2.19), higher serum iron (26.2 μg/dl (95% CIs= 2.52, 49.8), ferritin (24.1 ng/ml (95% CIs= 15.0, 33.4), and haemoglobin (1.14 g/dl (95% CIs: 0.32, 1.96) levels than non-GDM women. Single studies found the inverse associations of the Mediterranean diet, dietary approaches to stop hypertension diet, plant-based dietary index, and the direct associations of dietary acid load and dietary inflammatory index with the odds of GDM. Vitamin D supplementation early in pregnancy prevented GDM in two clinical trials. In two studies, iron supplementation’s effect on GDM in non-anemic women was inconsistent. Pooled analyses of probiotic supplementation in women with GDM showed no significant impact on maternal glycemia.
Conclusions
Vitamin D supplementation early in pregnancy may reduce the incidence of GDM. There is no compelling evidence that vitamin D or probiotics can help with GDM management. There is currently inadequate data to recommend a specific dietary pattern to prevent GDM in Iranian women.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40200-021-00944-7.
Keywords: Gestational diabetes mellitus, Nutrition, Dietary modifications, Nutritional supplementation, Pregnancy, Birth weight
Introduction
The prevalence of gestational diabetes mellitus (GDM) varied by country, with the Middle East and North Africa (MENA) region having the highest rate (median (interquartile range): 12.9% (8.4-24.5%)) and Europe having the lowest rate (5.8% (1.8-22.3% )). [1, 2]. Regardless of the disparities in frequency, the number of GDM-affected pregnancies is increasing internationally [3]. Since GDM endangers maternal and neonatal health [4], its prevention is the first step toward lowering the burden of this obstetric problem. A systematic review of observational studies published in English, suggested a higher risk of GDM with substituting carbohydrates with fat, high cholesterol intake, heme iron, red and processed meat, and eggs. However, the current evidence is dominated by findings of studies conducted among western countries [5]. Given that nutrition challenges and dietary behaviors differ by culture, identifying nutritional determinants of GDM in a particular population is critical to successful GDM prevention in that society.
Maternal glycemic control is crucial to reducing the adverse effects of GDM on pregnancy outcomes and the risk of developing chronic diseases [6, 7]. The first approach to GDM is nutrition therapy and physical exercise, and medications are administered when this lifestyle modification fails to control glycemia adequately. Different nutritional interventions, either in the form of dietary or supplemental interventions, are recommended to increase the success of nutritional management of GDM and reduce the need for drug medication [8, 9]. However, there is no worldwide consensus on a standard recommendation for the nutritional management of GDM as different countries and organizations have different evidence-based dietary recommendations [10].
There has been no prior systematic review that summarized the relationship of nutrition with the development and management of GDM in Iranian women, a community with a high incidence of GDM and particular dietary habits. This review identifies which dietary interventions are beneficial in the management of GDM in Iranian women, which may aid in the development of guidelines for this nation. Therefore, in this study, we attempted to summarize all available findings from observational or interventional studies examining nutrition associations with the development and management of GDM among Iranian women. We aimed to review the differences in blood circulatory vitamin and mineral markers in women with and without GDM, the association of nutrients, foods, and dietary patterns with the development of GDM, and the effects of nutritional interventions on the development and management of GDM.
Materials and methods
This systematic review and meta-analysis study was conducted by the following methods recommended in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11].
Information sources and search strategy
A comprehensive literature search was carried out on the English-electronic databases of Web of Science, PubMed, Scopus, and Persian-electronic databases of SID, and Magiran from the inception of each database up to 23 August 2020. Three search domains using the appropriate keywords for GDM and nutrition and considering Iran as affiliation were combined with the Boolean operator of “AND” and modified in every database based on their system differences. There were no language restrictions. Full electronic search strategy for PubMed was provided in Supplementary file 1. Relevant reviews were also manually checked to find further eligible studies.
Study selection
The search results were saved and managed in the EndNote. After excluding the duplicated articles, two investigators (NM and FRS) independently screened all records based on their titles and abstracts, and full texts of studies that met the inclusion criteria were retrieved. All original studies with either observational or interventional designs on nutritional factors and GDM development and management among Iranian women were considered potentially eligible. Studies with an observational design if provided information on comparisons of dietary intakes or circulatory markers for vitamins and minerals among women with/without GDM or their associations with risk of GDM development were included. Studies with an interventional design if examined the effects of nutrition modifications or supplementation on the development or management of GDM were also included. The population, intervention/exposure, comparison, outcomes, and study design (PICOS) of this study are shown in Table 1. Letters, case-reports, brief-communications, meeting abstracts, reviews, animal studies, diagnostic accuracy studies, clinical trials with less than four weeks, drug/educational interventions, and studies that did not report the related information were excluded.
Table 1.
Population, intervention/exposure, comparison, outcomes and study design (PICOS) criteria for inclusion of the studies in this systematic review and meta-analysis
| Parameter | Definition |
|---|---|
| Population | Iranian women with gestational diabetes mellitus (GDM) |
| Intervention/exposure |
• Any nutritional factors (including dietary intakes or their biomarkers) as exposure • Nutrition modifications or supplementations |
| Comparison |
• Non-GDM women • GDM women on placebo or control diet |
| Outcomes |
• Development of GDM • Management of GDM considering any maternal and neonatal outcomes related to GDM |
| Study design |
• Observational studies • Interventional studies |
Data extraction
Two independent investigators reviewed all included articles and extracted data into pre-designed forms of variables in excel sheets (FRS and FT). The third investigator also checked the extracted data (NM). Data items for the first author name, publication year, number of participants, the mean and standard deviation of maternal age, description of the exposure/ intervention, time of exposure/intervention, duration of the intervention (interventional studies), and data about outcomes were extracted. For clinical trials on the management of GDM, the outcomes of interest were categorized as maternal outcomes for glycemic, lipid profiles, inflammatory/anti-oxidant variables and neonatal outcomes of birth weight, and macrosomia risk.
Quality assessment
The quality of observational studies was assessed using the Newcastle–Ottawa quality assessment scale (NOS) [12]. The NOS score ranges between 0 (highest risk of bias, lowest quality) and 9 (lowest risk of bias, highest quality), and a score of ≥7 was defined as being of high quality. The methodological quality of clinical trials was also assessed using the original Cochrane RoB tool, considering selection (random sequence generation and allocation concealment), performance, detection, attrition, and reporting bias [13]. The total score of the RoB tool ranges from 0 (highest risk of bias, lowest quality) to 6 (lowest risk of bias, best quality) by counting the number of items with low risk of bias. Two researchers (FRS and FT) independently evaluated the quality of the studies, and a third researcher confirmed the assessments (NM).
Synthesis of results
The weighted mean difference (WMD) and 95% confidence intervals (CIs) between the two groups of women with GDM and non-GDM were estimated using a random-effects model. We summarized mean differences in final (post-intervention) values in interventional studies. The odds ratio (OR) and 95%CIs were determined for binary outcomes. The I2 measure and Cochran’s Q test were used to analyze study heterogeneity; significant heterogeneity was defined as I2 ≥ 50%. To assess publication bias, Egger’s regression test was used. The significance criterion for heterogeneity and publication bias was set at P <0.10. If heterogeneity was high and at least four studies were available, an influence analysis was done to determine which study (s) had a substantial impact on the pooled effect size. Statistical analyses were done using Stata, version 12.0 (Stata Corp, College Station, TX).
Results
Study characteristics
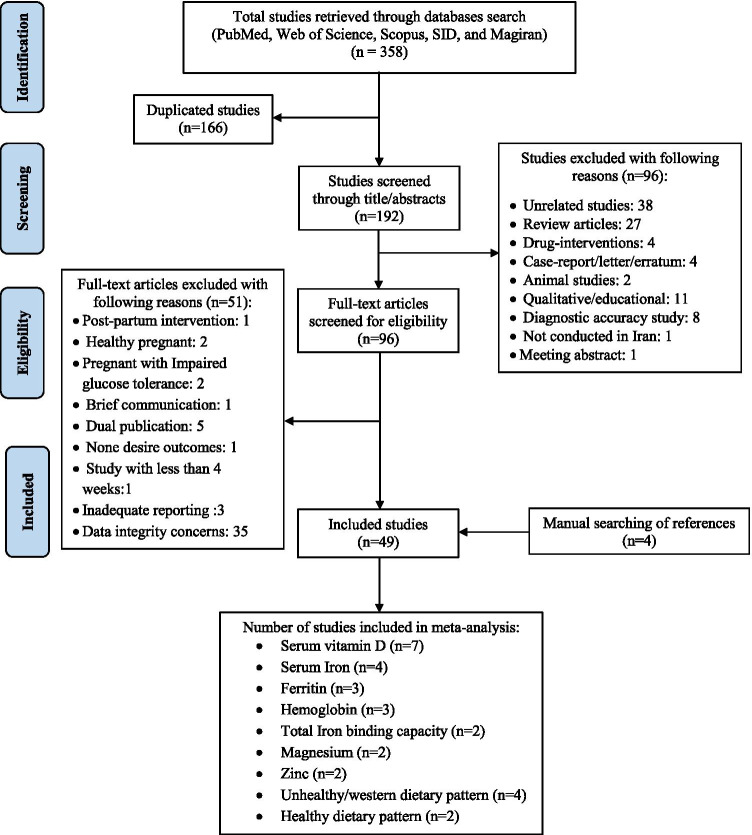
Forty-five out of 358 articles retrieved through searching the databases were found to be eligible. Adding four items found through manual searching [14–17], 49 articles were included in this systematic review (Fig. 1). Four studies were published in Persian [18–21], and the others were published in English. The designs of the studies were mainly case-control [14, 16, 18–36], seven were prospective [37–43], three were cross-sectional [44–46], and seventeen were clinical trials [15, 17, 47–61]. One study consisted of two phases: a case-control study followed by an open trial [62]. Seven trials investigated the effects of a specific intervention on the development of GDM in healthy pregnant women [17, 47, 52, 54, 56, 57, 60], while eleven trials examined the impact of a particular intervention on the management of GDM [15, 48–51, 53, 55, 58, 59, 61, 62]. Characteristics of the studies are summarized in Tables 2 and 3.
Fig. 1.
Flowchart diagram for studies selection
Table 2.
Summary of studies on nutrition associations with gestational diabetes among Iranian women
| Author (ref); year | City | Study design | Sample size; NO. of GDM | Mean maternal age ± SD | Exposure/intervention | Time of exposure/ intervention † | Significant association adjusted for confounders |
|---|---|---|---|---|---|---|---|
| Vitamin D | |||||||
| Maghbooli [44]; 2008 | Tehran | Cross-sectional | 579; 52 |
GDM:30.2±5.7 Non-GDM: 25.1 ± 4.4 |
Serum vitamin D | First half of the pregnancy |
• Lower serum vitamin D in GDM compared to non-GDM (16.5 ± 10.4 vs. 22.9 ± 18.3 nmol/l; p=0.001). • Serum D < 25 nmol/l was 86.5% in the GDM and 71% in non-GDM • Serum D <12.5 nmol/l was 44.2% in GDM and 23.5% in non-GDM |
| Soheilykhah [22]; 2010 | Yazd | Case-control | 165; 54 | 27.39 ± 5.08 | Serum vitamin D | 24-28 |
• Lower serum vitamin D in GDM compared to non-GDM (median (IQR): 9.62 (8.26) vs. 12.9 (14.3); p=0.03). • Prevalence of vitamin D deficiency (<20 ng/ml) was higher in GDM than non-GDM women (83.3% vs. 71.2%; p=0.03). • Odds serum vitamin D<15 ng/ml was 2.66 (1.26, 5.6) higher in GDM compared to non-GDM women |
| Akhlaghi [18]; 2014 | Mashhad | Case-control | 130; 61 |
GDM: 27.5 ± 5.54 control: 28.6±6.19 |
Serum vitamin D | 24-28 | • Lower serum vitamin D in GDM compared to non-GDM ( 8.06 ± 3.85 ng/ml vs 17.75 ± 5.38 ; p <0.001) |
| Sobhani [19]; 2016 | Rasht | Case-control | 154; 77 |
GDM: 27.1±5.7 Healthy 26.8 ± 5.0 |
Serum vitamin D | First half of the pregnancy |
• Lower serum vitamin D in GDM compared to non-GDM (13.4 ±6.8 vs. 17.8 ±11.1 nmol/l; p=0.003). • Inverse association between serum vitamin D and odds of GDM (OR=0.95 (95%CIs=0.91-0.99; p=0.021). |
| Haidari [26]; 2016 | Ahvaz | Case-control | 90; 45 |
GDM: 29.33 ± 4.31 NGT: 27.51 ± 4.87 |
Serum Vitamin D | 20-30 |
• Serum vitamin D was significantly lower in GDM than non-GDM women (13.46 ± 5.18 vs. 16.97 ± 5.56 ng/ml; p-adjusted: 0.034). • Vitamin D status was not significantly different between the two groups. |
| Shahgheibi [17]; 2016 | Sanandaj | Randomized clinical trial |
I:46 P: 44 |
I: 31.3 ± 6.4 P: 29.0 ±6.2 |
5000 unit/week vitamin D | From first trimester till gestational week 26 th | • Lower incidence of diabetes in the intervention group compared to the placebo (11.4 vs. 34.8%; p=0.009). |
| Rostami [54]; 2018 | Shushtar and masjed soleiman | Field trial | 900 control and 900 intervention | 18-40 | Vitamin D supplementation with different doses based on the status of vitamin D |
initiated 4 to 8 days after the first prenatal visit |
• Lower odds of GDM in the vitamin D supplemented group vs. non-supplemented women (OR=0.5; 95%CI= 0.34-0.88). |
| Mostali [20]; 2018 | Tehran | Case-control | 96; 48 | 30.1± 5.67 | Serum vitamin D | 24-28 | • No significant difference in serum vitamin D between GDM and non-GDM women ( 21.4±41.5 vs. 18.2±21.2 nmol/l; p=0.21) |
| Hosseini [21]; 2018 | Tehran | Case-control | 164; 82 |
GDM: 29.4±4.8 Non-GDM: 29.6±4.8 |
Serum vitamin D | 24-28 | • Lower serum vitamin D in GDM women than non-GDM (24.2 ± 13.3 vs. 29.4 ± 19 nmol/l; p=0.042) |
| Iron | |||||||
| Afkhami-Ardekani [14]; 2009 | Yazd | Case-control | 68; 34 | NA | ferritin, serum iron, TIBC, Hb, MCV | 24-28 |
• Higher serum iron (100 ±22.1 vs. 56.9±23.0 μg/dl), Hb (13.4 ±1.1 vs. 11.8 ± 1.43 g/dl), ferritin (73.3 ±31.7 vs. 41.6 ± 28.3 ng/ml), transferrin saturation (26.5 ± 5.94 vs. 12.8 ± 5.67%), and MCV (85.3±10.8 vs. 77.7 ± 6.46 fl) in GDM than non-GDM women. • Lower TIBC GDM than non-GDM women (383±30.6 vs. 458±58.2 μg/dl). |
| Ouladsahebmadarek [47]; 2011 | Tehran | Randomized clinical trial |
I: 410 P:372 Non-iron deficient , non-anemic women |
I:26.3±5.25 P:25.5±4.96 |
30 mg elemental iron | from 13 weeks of pregnancy | • No significant difference in frequency of GDM in iron-supplemented women compared to the placebo (0.5 vs. 0.8%; p=0.67). |
| Behboudi-Gandevani [37]; 2013 | Tehran | prospective | 1,033, 72 | 27.6±4.84 | Serum /dietary Iron | 14-20 |
• Higher serum iron in GDM vs. non-GDM women (143.8 ±48.7 vs. 112.5 ±69.4 μg/dl; p<0.001) • Higher odds of GDM (adjusted OR=1.006, 95 % CI 1.002 to 1.009; P=0.001) for serum iron levels in early pregnancy • No significant difference in dietary intakes of iron between the two groups (101.1 ±74 in GDM vs. 120.1 ±101 mg/day in non-GDM; p>0.05) |
| Nasiri Amiri [16]; 2013 | Babol | Case-control | 200; 100 |
Case: 25.7 ±5.33 Control: 25.0±5.33 |
Ferritin, serum iron | 24-28 |
• No significant difference in serum iron in GDM than non-GDM women (95.8 ± 41.1 vs. 91.5 ± 31.8 μg/dl; p=0.06) • Higher ferritin in GDM than non-GDM women (52.1 ± 47.2 vs. 30.4 ± 23.3 ng/ml; p=0.001) • No significant differences in TIBC between the two groups (355±40.5 vs. 353±51.1; p=0.1) |
| Javadian [23] ; 2014 | Tehran | Case-control | 102; 52 |
Case: 31.2±6.71 Control: 28.9 ± 6.58 |
Serum Ferritin and Hb | 34 | • Higher serum ferritin (31.22 ± 15.4 vs. 24.8 ± 63.2 ng/ml; p=0.012) and Hb (12.9 ± 0.72 vs. 12.2 ± 0.71; p=0.005) in GDM than non-GDM women |
| Didedar [31]; 2018 | Zabol | Case-control | 120; 60 |
Case: 34.9 ±8.10 Control: 33.9 ±7.96 |
Serum chromium, iron, and copper | 20-40 | • No significant differences in serum chromium (6.52±2.74 vs. 7.76 ±2.83 ng/dl; p=0.30), iron (0.55±0.14 vs. 0.60±0.10 μg/dl; p=0.14) and copper (0.83±0.22 vs. 0.97 ±0.22 μg/dl; p=0.50) in GDM and Non-GDM women |
| Taghavi [39]; 2018 | Bandar Abbas | Prospective | 120; 9 |
GDM: 24.6±5.92 Non-GDM: 24.3±7.27 |
Hb and dietary intakes iron |
Hb: first trimester and 24-28 Dietary intakes:6-10 and 16-20 |
• Higher Hb in GDM than non-GDM at the first trimester (11.1±3.63 vs. 10.1±5.71; p=0.05). • Higher Hb in GDM than non-GDM at gestational age of 24-28 (13.3±7.29 vs. 10.9±5.18 g/dl; p=0.001). • Higher dietary intake of iron in the GDM than non-GDM women at gestational age of 6-10 weeks (61.8±0.33 vs. 55 ± 0.32 mg/d; p=0.05) and 16-20 weeks (68.9±0.42 vs. 53.9±0.19; p=0.05) • Higher intake of iron from supplement in GDM than non-GDM women ( 61.8±0.33 vs.55±0.33 mg/d; p=0.05) |
| Asadi [57]; 2019 | Shiraz | non-randomized clinical trial | 90; 3 groups with 30 |
Group 1: 29.6 ± 16.1 Group 2: 29.6 ± 12.3 Group 3: 27.5 ± 8.3 |
A.Non-anemic women with prophylactic iron B. non-anemic women not receiving the supplementation C. anemic women with standard iron supplementation |
The first trimester | • Higher frequency of GDM in the group A compared to the other groups (16.7% vs. 0% in the two other groups). |
| Hajianfar [43]; 2020 | Isfahan | Prospective | 812 | 29.40 ± 4.84 | Heme and non-heme dietary iron intakes | 8–16 (first trimester) | • Higher odds of high FPG with higher intakes of heme iron (ORT2 = 052 (95%CIs= 0.32, 0.86), ORT3 = 0.72 (0.42, 1.2); p-trend=0.04) |
| Zinc | |||||||
| Rahimi Sharbaf [62]; 2008 | Tehran | Case-control | 70/35 (50%) |
Case: 28 ±12.5 Control: 28.2 ± 9.5 |
Serum zinc | 24-28 | • Lower serum zinc in GDM than non-GDM women (94.8±13.7 vs. 103±7.87mg/dl; p<0.001). |
| Behboudi-Gandevani [37]; 2013 | Tehran | prospective | 1,033, 72 | 27.6±4.84 | Serum /dietary zinc | 14-20 |
• No significant difference in serum zinc in GDM than non-GDM (84.8 ±44 vs. 83.5 ±44.4 μg/dl) • No significant difference in dietary intake of Zinc between the two groups • No significant association between serum zinc and odds of GDM |
| Parast [27]; 2017 | Isfahan | Case/control | 80; 40 |
Case: 29.4 ± 4.9 Non-control: 28.9 ± 5.2 |
Dietary zinc | 24-48 | • Lower dietary intake of zinc in GDM than non-GDM (7.4 ± 1.9 vs. 9.1 ± 1.7 mg/d; p<0.001) |
| Magnesium | |||||||
| Mostafavi[45]; 2015 | Tehran | Cross-sectional | 40 | 28.4 ±5.37 | Serum magnesium | 24-48 |
• Lower serum magnesium in GDM than non-GDM (0.75 ± 0.04 vs. 0.79 ± 0.08 mmol/l; p=0.05) • Obesity (relative risk = 20.6, p-value = 0.002), low-normal magnesium level (relative risk = 4.2, p-value = 0.009), and their interaction (p-value<0.001) were significant predictors of GDM. |
| Zarean [52]; 2017 | Isfahan | randomized controlled trial | 180; three groups of 60 | group A: 29.8±5.05 group B: 29.7±6.21 group C: 29.4±5.68 |
A.Normomagnesemia with one tablet multimineral till end of the pregnancy B.hypomagnesaemia receiving one tablet multimineral till end of the pregnancy C.hypomagnesaemia receiving one tablet multimineral till end of the pregnancy plus 200 mg effervescent magnesium tablet for one month |
12–14 till end of pregnancy | • Lower frequency of GDM in group C compared to group B; 8.3 % vs. 21.7%. |
| Musavi [46]; 2019 | Babol | cross-sectional |
GDM:96 Control: 122 |
GDM: 26.6±4.9 Control:26.4±6.0 |
Serum and RBC magnesium | 24-32 |
• Serum magnesium was not significantly different in GDM vs. control (0.71 ± 0.05 vs. 0.71 ± 0.04 mmol/l; p=0.9). • RBC-mg was significantly lower in GDM vs. control (1.93 ± 0.1 vs. 2.10± 0.07 mmol/l; p=0.001) |
| Antioxidant | |||||||
| Hekmat [24]; 2014 | Ahvaz | Case-control | 82 ; 41 |
Case: 29.4±4.68 Control:28.3±6.42 |
Serum retinol and α-tocopherol | ≥32 |
• Lower serum retinol in the GDM women than non-GDM (0.46 ± 0.19 vs. 0.59 ± 0.25 μg/dl; p<0.01). • No significant difference in α-tocopherol GDM women than non-GDM (6.21 ± 2.69 vs. 6.92 ± 2.43mg/dl; P=0.45) |
| Parast [27]; 2017 | Isfahan | Case-control | 80; 40 |
Case: 29.4 ± 4.9 Non-control: 28.9 ± 5.2 |
Serum TAC, dietary intakes of antioxidants including vitamin E, C, b-carotene, and Se | 24-28 |
• Lower serum TAC in GDM than non-GDM women ( 2.3 ± 0.7 vs. 3.7 ± 0.1 μmol/l; p<0.001) • Lower dietary intake of selenium GDM than non-GDM women (81 ± 26 vs. 95 ± 36 μg/d; p=0.037). • Lower dietary intake of vitamin E in GDM than non-GDM women (11.8 ± 3.1 vs. 16.2 ± 3.1 mg/d; p<0.001). • No significant difference in dietary intake of vitamin C between the two groups (223 ± 132 vs. 235 ± 122 mg/d; p=0.675) • No significant difference in dietary intake of β-carotene between the two groups (803 ± 512 vs. 1009 ± 635μg/d; p=0.114) |
| Protein, cholesterol, trans-fatty acid | |||||||
| Hezaveh [34]; 2019 | Tehran | Case-control | 320; 152 |
Case: 30.8±5.28 Control: 28.8±5.42 |
Total protein, vegetable protein, animal protein | 24-40 |
• No significant association between intakes of total protein, vegetable protein, protein intakes from red and process meat, poultry, seafood, and dairy, and odds of GDM. • Lower odds of GDM in women in the highest quartile of protein intake from egg than those in the lowest quartile (OR= 0.43 (95%CIs= 0.28, 0.89). |
| Milajerdi [32]; 2018 | Isfahan | Case-control | 463; 200 | 22-44 | Cholesterol | 5-28 | • No significant association between cholesterol intakes and odds of GDM |
| Alamolhoda [56]; 2019 | Tehran | Randomized controlled trial | 800 |
Intervention: 24.4±2.9 Control: 24.6 ±2.7 |
Intervention: Daily intake of trans-fatty acid content was less than1% | ≥7 |
• No significant effect on the development of GDM by Reducing the dietary intakes of trans-fatty acids • Frequency of GDM was 5% in the intervention group and 8% in the control group (p=0.08). |
| Food groups | |||||||
| Lamyian [38]; 2017 | Tehran | prospective | 1026; 71 | 26.7 ± 4.3 | total fast foods, French fries, hamburger, bologna, sausages, Pizza | ≤ 6 |
• Higher odds of GDM with higher consumption of fast food (p-trend: 0.03); odds of GDM in women in the highest vs. lowest quartile of fast food was 2.12 (95%CI: 1.12–5.43) • The odds of GDM in women in the highest quartile vs. lowest quartile of French fries was 2.18 (95%CI: 1.05, 4.70). • No significant association between odds of GDM and intakes of other fast food subtypes |
| Goshtasebi [40]; 2018 | Tehran | Prospective | 1,026; 71 | 26.7 ± 4.3 |
legumes, potatoes, and other starchy vegetables (corn, squash, green pea, and green lima beans) |
≤ 6 |
• No significant association between total starchy vegetable and other starchy vegetable and GDM • Inverse association between potato intakes and risk of GDM that became non-significant in the fully adjusted model • Higher legumes consumption associated with lower odds GDM; OR for those who consumed ≥ 3.3 servings/week (T3) was 0.33 (0.16 – 0.66); p-trend:0.002 |
| Milajerdi [32]; 2018 | Isfahan | Case-control | 463; 200 | 22-44 | egg | 5-28 | • The risk of GDM in the highest vs. lowest tertile of egg intakes were 41 lower (95% CIs: 0.35, 0.99; p=0.01). |
| Mirmiran [42]; 2019 | Tehran | Prospective | 1026; 71 | 26.7 ± 4.3 | Fruit and vegetables (combined and per se)/ dairy | ≤ 6 |
• Higher intakes of fruits and vegetables were associated with lower odds of GDM; (OR=0.85; 95%CI: 0.74-0.98) • Higher intakes of fruits were associated with lower odds of GDM (OR=0.82; 95%CI: 0.73-0.96). • Women in the highest quartiles of vegetable intakes had lower odds of GDM compared to those in the lowest quartiles (OR=0.46; 95%CI: 0.22-0.99). • Vegetable intakes as a continuous variable was not associated with GDM. • No significant association between dairy intake s and odds of GDM. |
| Periori dietary pattern | |||||||
| Izadi [25]; 2016 | Isfahan | Case-control | 460; 200 | 22-44 | Mediterranean & DASH diets | 5-28 |
• Odds of GDM in the tertile 3 of the MED diet was 0.20 (95% CIs= 0.50–0.70), compared to the lowest tertile. • Odds of GDM in the tertile 3 of the DASH diet was 0.29 (95%CIs: 0.17–0.48), compared to the lowest tertile. |
| Saraf-Bank [29]; 2017 | Isfahan | Case-control | 460; 200 | 22-44 | Dietary acid load (DAL): protein to potassium ratio (Pr/K) and potential renal acid load (PRAL) | 5-28 |
• Higher odds of GDM with higher score for pr/k; OR (95%CI) in tertile 3 vs.1 was 7.60 (3.43-16.84); p-trend<0.001. • Higher odds of GDM was higher with higher score for PRAL; OR (95%CI) in tertile 3 vs. 1 was 9.27 (4.00-21.46); p-trend<0.001. |
| Zamani [35]; 2019 | Isfahan | Case–control | 460; 200 | 22-44 |
overall plant-based dietary index (PDI), healthy plant-based diet (hPDI), and unhealthy plant-based diet index (uPDI) |
25-28 |
• The odds of GDM according to the tertiles of PDI was 0.79 (0.50, 1.25) and 0.47 (0.28, 0.78) in tertile 2 and 3 vs. 1 (p-trend: 0.004) in the fully adjusted model. • No significant associations between hPDI and uPDI and odds of GDM. |
| Shivappa [36]; 2019 | Tehran | Case-control | 388; 122 |
GDM: 29.76± 4.26 Control: 29.64± 4.52 |
Dietary inflammatory index | 24-28 |
• Odds of GDM was significantly higher in the tertile 3 vs. 1 of DII (OR: 2.10 (95%CIs: 1.02, 4.34) after adjusting for all potential variables. • No significant association was observed regarding DII as a continuous variable. |
| Posteriori dietary pattern | |||||||
| Sedaghat [28]; 2017 | Tehran | Case-control | 388; 122 |
Case: 29.76 ± 4.26 Control: 29.64 ± 4.52 |
Dietary pattern using PCA | 24-28 |
• The odds of GDM was higher in women with dietary scores for western diet above the median compare to below the median (OR (95%CI): 1.68 (1.04–2.72)). • No significant association between prudent diet and odds of GDM. |
| Zareei [30]; 2018 | Fasa | Case/control | 204; 104 |
GDM: 30.9 ±5.59 Control: 27.9±4.93 |
Dietary pattern using PCA | 24-28 |
• Odds of GDM was 2.84 (1.04, 7.75; p=0.042) in the quartile 4 vs. 1 of the unhealthy dietary pattern. • Odds of GDM was 0.28 (0.096, 0.84; 0.023) in the quartile 4 vs. 1 of healthy dietary pattern. |
| Hajianfar [41]; 2018 | Isfahan | Prospective | 812 | Aged 2-40 years | Dietary pattern using PCA | 8–16 | • Neither dietary patterns of healthy, western, and traditional were associated with odds of GDM. |
| Asadi [33]; 2019 | Yazd | Case-control | 278; 130 |
GDM: 29.0 ± 5.17 Control: 27.50 ± 4.92 |
Dietary pattern using PCA |
• No significant association between western diet and GDM. • The odds of GDM was significantly lower in tertiles 2 (OR: 0.38; 95%CI: 0.18-0.79) and 3 (OR: 0.88; 95%CIs: 0.44-0.99) compared to the tertile 1 in the prudent dietary pattern. |
|
| Probiotic | |||||||
| Asgharian [60]; 2020 | Tabriz | Randomized controlled trial | 64 in each group |
Probiotic: 29.5 ± 6.2 Conventional : 29.4 ± 5.5 |
Daily intake of 100 g probiotic yoghurt (intervention) and conventional yoghurt (control) |
from 24 weeks of gestation until delivery (4-weeks for FPG and GDM) |
• After 4- weeks, FPG (mean difference (95%CIs): -4.0 (-6.9, -1.1 mg/dl) and 2-h OGTT (-13.5 (-22.8, -5.0) were significantly lower in the probiotic vs. conventional yoghurt. • GDM was diagnosed in 9% of participants in the probiotic and 17% in the conventional yoghurt (p=0.184). • Intake of probiotic compared to conventional youghurt had no effects on odds of GDM (OR (95%CI): 0.5 (0.2, 1.5). |
†According to gestational weeks.
CIs, confidence intervals; FPG, fasting plasma glucose; GDM, gestational diabetes mellitus; Hb, hemoglobin; 2-h OGTT, 2-hour oral glucose tolerance test; IQR, interquartile range; MCV, mean corpuscular volume; NA, not available; OR, odds ratio; PCA, principal component analysis; RBC, red blood cell; T, tertile; TIBC, total iron binding capacity.
Table 3.
Summary of clinical trials of the effect of nutritional interventions on management of gestational diabetes among Iranian women
| Author; year | Sample Size | Mean maternal age ±SD | Dose of intervention | Duration (weeks) |
Outcome of interest | |||
|---|---|---|---|---|---|---|---|---|
| Glycemic | Lipid profiles | Inflammatory/ anti-oxidant | Neonatal outcomes | |||||
| Vitamin D | ||||||||
|
Hosseinzadeh- Shamsi-Anar [15], 2012 |
I: 24 C:21 |
I: 30.7±6.2 C: 29.5±4 |
Intramuscular 300,000 IU of vitamin D |
12 | HbA1C ↔ | |||
| Yazdchi [49]; 2016 |
I:33 P:33 |
I:31.64±4.40 P:32.11±3.61 |
50,000 IU vitamin | 8 |
FPG↓ Insulin ↔ HbA1C ↓ HOMA-IR ↔ |
TC ↔ TG ↔ LDL ↔ HDL ↔ |
hs-CRP ↔ | - |
| Keshavarzi [51] ; 2017 | 192; three groups (n=64) |
I:27.9 P: 28.8 |
a) Low dose: 400 IU tablet once daily b) High dose: 50,000 IU daily c) Placebo |
a) until the 36th week of gestation b) At study baseline and 21 days after c) Similar to group b |
- | - |
BW ↔ Macrosomia↔ |
|
| Probiotic capsule | ||||||||
| Dolatkhah [48]; 2015 |
I:29 P: 27 |
I: 28.1±6.24 P:26.5 ± 5.23 |
> 4 × 109 CFU; 4 strains | 8 |
FPG ↓ fasting serum insulin↔ HOMA-IR↓ QUICKI↔ |
- | - | - |
| Jafarnejad [50]; 2016 |
I:41 P:41 |
I: 32.4 ± 3.1 P: 31.9 ± 4.0 |
112.5 × 109 CFU; 8 strains | 8 |
FPG↔ Fasting serum Insulin↓ HOMA-IR↓ HbA1C↔ |
- |
hs-CRP↓ IL-10↔ IFN-γ ↔ IL-6↓ TNF-α↓ |
- |
| Hajifaraji [55]; 2018 |
I:29 P:27 |
I:28.1±6.25 P:26.5±5.24 |
> 4 × 109 CFU;4 strains | 8 | - | - |
CRP↓ IL-6↔ TNF-α↓ TAC↔ MDA ↓ |
- |
| Yoghurt probiotic | ||||||||
| Sahhaf Ebrahimi [59]; 2019 |
I: 42 P:42 |
I: 31.64 ± 5.97 P: 31.61 ± 5.49 |
300 mg/d contained 106 (Lactobacillus acidophilus and Bifidobacterium Lactis) |
8 |
FPG↓ PG↓ HbA1C↓ |
- | - |
BW↓ Risk of macrosomia ↓ |
| Synbiotic | ||||||||
| Nabhani [53]; 2018 |
I:45 P:45 |
I:29.4±5.8 P:30.3±5.6 |
500 mg lactobacillus bacteria consisting 4 strain+38.5 mg fructooligosaccharide (FOS) | 6 |
FPG↔ insulin↔ HOMA-IR↔ QUICKI↔ |
TG↔ TC↔ LDL↔ HDL↔ |
TAC↔ | - |
| Zinc | ||||||||
| Rahimi Sharbaf [62]; 2008 |
I:30 C:30 |
NA | Zinc sulfate: 15 mg/day | 6-8 | - | - | - |
BW↓ Risk of macrosomia↓ |
| Other supplementation | ||||||||
| Aslfalah [58]; 2018 |
I:30 P:30 |
I: 30.96 ± 0.93 P: 31.10 ± 0.92 |
Alpha-lipoic acid: 100 mg/d | 8 |
FPG↓ Insulin↔ HOMA-IR↓ QUICKI↑ |
MDA/TAC↓ | - | - |
| Hajimoosayi [61]; 2020 |
I: 37 P: 33 |
I: 29.68± 5.05 P:31.15± 5.26 |
Ginger: dose of 1500 mg including three tablets of ginger or placebo daily in three meals |
6 |
FBS↓ Insulin↓ HOMA-IR↓ PG↔ |
- | - | - |
BW, birth weight; C, control group; CFU, colony forming units; FPG, fasting plasma glucose; HbA1C; glycosylated hemoglobin; HDL, high density lipoprotein; hs-CRP, high sensitive C-reactive protein; HOMA-IR; homeostatic model assessment of insulin resistance; I, intervention group; IFN-γ, Interferon gamma; IU, international unit; IL-6, interleukin-6; LDL, low density lipoprotein; MDA, Malondialdehyde ; NA, not available; P, placebo group; PG, post-prandial blood glucose; QUICKI, Quantitative Insulin Sensitivity Check Index; TAC, total antioxidant capacity; TC, total cholesterol; TNF-α, tumor necrosis factor-𝛼. ↓ Final values were significantly lower in the intervention group compared to the placebo/control group. ↑ Final values were significantly higher in the intervention group compared to the placebo/control group. ↔ No significant differences in final values between the two groups
Quality assessment
All six prospective studies were scored as a high quality (Supplementary Table 1). The quality score for case-control studies was ranged from 5 to 8; 54.5% of the studies had a high score ≥ of 7 [14, 16, 18, 20–22, 24, 26, 27, 33, 34, 62]. None of the studies provide a statement on the non-response rate. Apart from non-respondents, case representative was also the main concern for the case-control studies. Studies assessing dietary intakes did not explain the blindness to case/control status [25, 27–30, 32–36] and therefore lost one score for the item (Supplementary Table 2). Cross-sectional studies were scored between 3 and 4 (Supplementary Table 3).
Five clinical trials scored as a low risk of bias for all six items of the Cochrane tool [49, 53, 59–61]. In most studies, random sequence generation was either at low risk [15, 17, 48–56, 59–62] or unclear [47, 58]; nine studies described the concealment method adequately[47–50, 53, 55, 59, 61]. In four studies, participants and personnel were not blinded to the assigned groups [15, 52, 54, 62], and four studies did not clarify this point [47, 51, 56, 57]. One studies were at high risk of bias [62], and six were unclear regarding the blinding of outcomes [47, 51, 52, 56–58]. Except for one study that did not address adequately [51], the other study has a low risk of bias for incomplete outcome data. Compared to the registered protocol, two studies were at high risk of bias [48, 55], and three were unclear for selective reporting [17, 50, 62] (Supplementary Table 4).
Comparative analysis of circulatory vitamins and minerals in women with and without GDM
Serum vitamin D
Seven observational studies compared serum vitamin D in women with and without GDM [18–22, 26, 44]. Except for a case-control study that reported no significant difference in serum vitamin D [20], in the other six studies, serum vitamin D was significantly lower in women with GDM compared to non-GDM [18, 19, 21, 22, 26, 44]. Meta-analysis of the 7 studies, including 419 GDM-women and 959 non-GDM (Table 4), suggested a lower serum vitamin D in GDM women than in non-GDM women (WMD=-8.31 nmol/l (95% CIs= -14.4, -2.19); I2: 91.9%, Pheterogeneity<0.001). There was no publication bias by Egger’s test (P=0.954). Influence analysis showed a reduction in the estimated MD (WMD =-5.70 nmol/l (95%CIs =-7.47, -3.92)) after the exclusion of a study [18] (supplementary Table 5). In two studies [22, 44], vitamin D deficiency was higher in GDM-women than in non-GDM (22, 44), while one study suggests no significant difference in vitamin D status between the two groups [26].
Table 4.
Weighted mean differences in serum micronutrients and iron status markers in women with and without gestational diabetes according to observational studies
| Variables | No. of studies | No. of participants† | Weighted mean difference (95%CIs) | I2 (%) | Pheterogeneity | Egger’s test |
|---|---|---|---|---|---|---|
| Serum vitamin D (nmol/l) | 7 | 419/959 | -8.31 (-14.4, -2.19) | 91.9 | <0.001 | 0.954 |
| Serum iron (µg/dl) | 4 | 266/1155 | 19.3(-1.90, 40.4) | 96.6 | <0.001 | 0.154 |
| Ferritin (ng/ml) | 3 | 186/184 | 24.2 (15.0, 33.4) | 12.9 | 0.317 | 0.742 |
| Hemoglobin (g/dl) | 3 | 86/84 | 1.14 (0.32, 1.96) | 72.9 | 0.025 | 0.545 |
| Total iron binding capacity (µg/dl) | 2 | 134/134 | -36.0 (-111, 38.7) | 97.1 | <0.001 | - |
| Serum zinc (µg/dl) | 2 | 107/996 | -4.60 (-13.6, 4.44) | 60 | 0.114 | - |
| Serum magnesium (mmol/l) | 2 | 113/185 | -0.02 (-0.06, 0.02) | 85.3 | 0.009 | - |
† No. of women with gestational diabetes/ No. of women without gestational diabetes. § A study with extremely lower serum iron was excluded
Iron status markers
Six observational studies were conducted to assess the iron status of women with and without GDM [14, 16, 23, 31, 37, 39]. Two investigations found that serum iron levels were significantly higher in women with GDM at gestational ages of 14-20 [37] or 24-28 [14], but the other two studies did not identify a significant difference [16, 31]. A meta-analysis of the four studies showed no significant differences in serum iron between women with and without GDM (Table 4). However, influence analysis indicated a significant difference in serum iron after the exclusion of the Didedar et al. study [31] (WMD=26.2 µg/dl (95%CIs=2.52, 49.8); supplementary Table 6). Serum ferritin [14, 16, 23] and hemoglobin [14, 23, 39] levels in women with GDM were consistently greater than in non-GDM women, according to the findings of the research. Pooling the data from the studies, serum ferritin was estimated to be 24.2 ng/ml higher (95%CIs= 15, 33.4; I2= 12.9%, Pheterogeneity=0.317), and hemoglobin was 1.14 g/dl higher (95%CI= 0.32, 1.96; I2= 72.9%, Pheterogeneity=0.545) in GDM women compared to non-GDM women. In a case-control study, TIBC was significantly lower in women with GDM [14]. The other case-control study showed no significant difference in TIBC between the two groups of women [16]. A meta-analysis of the two studies found no statistically significant variations in TIBC between them (Table 4).
Serum Zinc
In a case-control study, the serum zinc of pregnant women at gestational age between 24 and 28 was significantly lower in GDM than in non-GDM women [62]. However, a prospective study of 1033 women, at the gestational age of 14-20 weeks, showed no significant difference in serum zinc in women with GDM and non-GDM [37]. When the two observational studies were combined, there was no significant difference in serum zinc levels between women with and without GDM (Table 4).
Serum/plasma magnesium
A research recruited two groups of pregnant women with and without abdominal obesity to assess plasma magnesium concentrations dependent on the presence of GDM. In the research, plasma magnesium was slightly lower in women with GDM than in women without GDM (0.75 ± 0.04 vs. 0.79 ± 0.08 mmol/l; P-value =0.05), and women with low plasma magnesium were more likely to develop GDM (relative risk=4.2; p=0.009) [45]. A case-control study found no significant difference in serum magnesium levels between GDM and non-GDM women, but the mean magnesium concentration in red blood cells was significantly lower in GDM women (1.93 ± 0.1 vs. 2.10 ± 0.07 mmol/l; p = 0.001) [46]. When the data from the two investigations were combined, there was no significant difference in serum magnesium levels between the two groups of women with and without GDM (Table 4).
Antioxidant markers
A case-control study of pregnant women at gestational age > 32 weeks found that women with GDM had significantly lower retinol concentrations than non-GDM women (0.46 ± 0.19 vs. 0.59 ± 0.25 µg/dl; p<0.01), but serum tocopherol levels were not different (6.21 ± 2.69 vs. 6.92 ± 2.43 mg/dl; P = 0.45) [24]. Serum total antioxidant capacity (TAC) was also lower in GDM than in non-GDM (2.3 ± 0.7 vs. 3.7 ± 0.1 µmol/l; P<0.001) in another case-control study consisting of 40 GDM women at gestational ages between 24 and 28 weeks [27].
Nutrition and development of GDM
Dietary intake of protein, cholesterol, and antioxidants
A case-control study consisting of 152 women with GDM did not find any significant associations between total protein, vegetable protein, or animal protein intakes and the odds of GDM [34]. According to the findings of a case-control study, cholesterol intake was also not related to the odds of GDM [32]. A case-control study aiming to compare dietary intake of antioxidants including vitamin E, vitamin C, beta-carotene, selenium, and zinc reported lower dietary intake of vitamin E (11.8±3.1 vs. 16.2±3.1 mg/d; p<0.001), selenium (81±26 vs. 95±36 µg/d; p=0.037), and zinc (7.4±1.9 vs. 9.1±1.7 mg/d; p<0.001) in women with GDM than in healthy pregnant women. However, dietary intake of vitamin C and beta-carotene did not significantly differ between the two groups [27].
Dietary intake of iron and iron supplementation
Three prospective studies reported the association between dietary intake of iron and GDM occurrence [37, 39, 43]. In one study [37], the dietary intake of iron, in 72 women with GDM was similar to that of 961 individuals without GDM, while the other studies showed that dietary intake of iron at the gestational age of 6-10 weeks and 16-20 weeks was significantly higher in women with GDM than non-GDM [39]. In a study, dietary intake of heme iron in the first trimester was associated with higher odds of high fasting blood sugar after adjusting for body mass index, physical activity, age, economic status, and energy intake (ORtertile 2 = 0.52 (95%CIs= 0.32, 0.86), ORtertile 3 = 0.72 (0.42, 1.2); P-trend=0.04) [43].
Two clinical studies investigated whether iron supplementation reduces the incidence of GDM in pregnant women who are not anemic [47, 57]. One study found that the incidence of GDM was not substantially greater in non-anemic women who received 30 mg elemental iron starting at gestational age 13 compared to those who received a placebo [47]. The other study found that the frequency of GDM was significantly higher in non-anemic women supplemented with prophylactic iron from the first trimester compared to both non-anemic women who did not receive the supplementation and anaemic women who received standard iron supplementation (16.7% vs. 0% in the two other groups) [57].
Food and food groups
A higher egg intake was related with a decreased risk of GDM in a case-control study [32]. The associations of several food groups, such as fast foods, fruits, vegetables, legumes, and dairy, with the risk of developing GDM were explored prospectively in three papers, utilizing the same dietary data of 1026 pregnant women at gestational age six weeks obtained using the 168-item FFQ [38, 40, 42]. After controlling for possible confounders, higher intakes of total fast foods and French fries were related with increased chances of GDM [38], whereas inverse associations were identified for intakes of potatoes, legumes, fruit, and vegetables and risks of GDM [40, 42].
A priori dietary pattern
Four case-control studies examined the association between a priori dietary patterns and the odds of GDM [25, 29, 35, 36]. Findings from these studies suggested inverse associations for the Mediterranean diet and Dietary Approaches to Stop Hypertension diet (DASH; n=1), and total plant-based dietary pattern (PDI; n=1), and direct associations for adherence to the dietary acid load (DAL; n=1), and dietary inflammatory index after adjusting for potential covariates [25, 29, 35, 36]. The two indices of healthy PDI and unhealthy PDI were not individually associated with the odds of GDM [35].
A posteriori dietary pattern
Four studies used principal component analysis (PCA) to investigate the relationship between main food patterns and the risk of GDM [28, 30, 33, 41]. Except for one study reporting three major dietary patterns [41], the other studies derived two patterns [28, 30, 33]. All of the studies discovered a dietary pattern with essentially identical features (e.g., a high intake of fast foods, processed meats, mayonnaise, salty snacks, and sugar-sweetened drinks) that was labeled as either unhealthy or a Western eating pattern. Based on fully-adjusted model of these studies, we could not find any significant association between the unhealthy/western dietary pattern and odds of GDM (pooled OR highest versus lowest category of the pattern = 1.39 (95%CI= 0.78, 2.48) but there was substantial heterogeneity between the studies (I2=59.7%, Pheterogeneity =0.059). After omitting Hajianfar et al. study, influence analysis demonstrated a significant higher OR of GDM in highest vs. lowest adherence of the pattern (pooled OR=1.75 (95%CIs=1.21-2.53); Supplementary Table 7). Two studies identified a healthy pattern with high intakes of vegetables, fruits, nuts, fish, poultry, and olive oil. A more adherence to the healthy dietary pattern was not related to the odds of GDM (pooled OR highest vs. lowest group= 0.57(95%CIs= 0.16, 2.05); I2= 72.4%, Pheterogeneity =0.057).
Dietary interventions
Two studies examined diet interventions on the development of GDM, one aimed at reducing trans-fatty acid consumption and the other at increasing probiotic intake [56, 60]. In a randomized clinical trial, daily intakes of trans-fatty acids designed to be less than 1% from gestational age of 7 weeks in a group of pregnant women (as an intervention group; n=393), while no adjustments in dietary intakes were made in another group (as a control group; n=407). The study’s findings revealed that lowering trans-fatty acid consumption in the diet had no effect on the risk of GDM. [56].
The impact of probiotic yoghurt vs. ordinary yoghurt on plasma glucose of overweight and obese pregnant women with no diabetes at 24 weeks gestation was studied in a randomized controlled clinical study. In the study, pregnant women who consumed 100 g probiotic yoghurt daily for four weeks (until the gestational age of 28 weeks) had lower fasting plasma glucose (FPG) and 2-hour oral glucose tolerance test (2-hOGTT) results as compared to pregnant women who consumed conventional yoghurt. However, probiotic yoghurt intake had no influence on the likelihood of developing GDM [60].
Vitamin D supplementation
Two interventional trials looked at the impact of vitamin D supplementation on the development of GDM in healthy pregnant women [17, 54]. In a randomised placebo-controlled trial, the development of GDM was considerably lower in pregnant women given 5000 unit/week of vitamin D from the first trimester to the 26th week of gestation compared to those given a placebo (11.4% vs. 34.8%; p=0.009) [17]. A field trial also examined the effect of different doses of vitamin D supplementation on the development of GDM in 1800 healthy pregnant women. Supplementation was initiated 4-8 days after the first prenatal visit in 900 pregnant women aged 18-40 years; the dosages and durations of supplementation were varied based on the maternal vitamin D status. The study’s finding showed that vitamin D supplementation could reduce the odds of GDM by 50% (95%CI: 0.34-0.88). The study underlines the need of screening for vitamin D deficiency and correcting it early in pregnancy to avoid obstetric complications [54].
Magnesium supplementation
A randomized controlled trial examined the effect of magnesium supplementation on the development of GDM in pregnant women at the gestational age of 12-14 weeks. The study groups were as follows: (A) women with serum magnesium >1.9 mg/d who received one multimineral tablet per day until the end of pregnancy; (B) women with serum magnesium <1.9 mg/d who received one multimineral tablet per day until the end of pregnancy; (C) women with serum magnesium <1.9 mg/d who received one multimineral tablet per day until the end of pregnancy plus 200 mg effervescent magnesium for one month. The multimineral supplement contained 100 mg magnesium. The number of women with GDM was significantly lower in group C than group B (8.3 vs. 21.7%) [52].
Nutritional interventions and management of GDM
Vitamin D supplementation
Three studies examined the impact of vitamin D supplementation on GDM management [15, 49, 51]. A high dose of vitamin D (300,000 IU) administered intramuscularly for 12 weeks enhanced serum vitamin D but had no effect on glycated haemoglobin (HbA1C) compared to the control group (5.58±12 in the intervention vs. 5.21±0.52% in control; P=0.2) [15]. Vitamin D capsules at a dose of 50,000 IU every two weeks for eight weeks could increase the serum vitamin D concentrations and improved its status and reduced FPG and HbA1C in 33 women with GDM compared to those receiving the placebo. The supplementation had no significant effects on insulin, homeostatic model assessment of insulin resistance (HOMA-IR), lipid profiles, and inflammatory markers of high-sensitivity C-reactive protein (hs-CRP) [49]. According to one research, the birth weight and incidence of macrosomia in neonates of mothers with low serum vitamin D supplemented with vitamin D were not statistically different from women with normal serum vitamin D receiving the placebo [51].
Probiotic supplementation
The efficacy of probiotic supplementation on GDM control has been studied using probiotic capsules (n=3) [48, 50, 55], synbiotic capsules (n=1) [53] and yoghurt probiotics (n=1) [59].
Pooling the data from the trials revealed that at the end of the trial, none of the glycemic indicators of FPG, fasting insulin, HOMA-IR, and TAC were substantially different in women taking probiotics compared to the control group (Table 5). Based on influence analysis, one research was determined to have a significant influence on the pooled effect size for FPG (supplementary Table 8). Inflammatory markers of women receiving probiotic was 1.33 mg/l lower (95% -2.31, -0.35); I2= 34%) for hs-CRP and 0.89 pg/ml lower (95%CIs= -1.17, -0.61; I2=0) for IL-6 compared to women in the placebo group (Table 5). A trial looked at the neonatal effects of probiotic supplementation in mothers with GDM [59].The study’s findings imply that neonates of GDM mothers who consume 300 mg/d yoghurt probiotic have a lower birth weight and a reduced risk of macrosomia than women who get ordinary yoghurt [59].
Table 5.
Weighted mean differences in final values of maternal outcomes after probiotic supplementation
| Maternal outcomes | No. of studies † | No. of participants | Duration (weeks) |
Weighted mean difference (95%CIs) |
I2 (%) |
Pheterogeneity | Egger’s test |
|---|---|---|---|---|---|---|---|
| Fasting plasma glucose (mg/dl) | 4 | 153/149 | 6-8 | -1.61 (-5.46, 2.25) | 88.6 | <0.001 | 0.641 |
| HbA1C (%) | 2 | 79/77 | 8 | -0.09(-0.37, 0.19) | 51.9 | 0.149 | - |
| Insulin (µIU/mL) | 3 | 111/107 | 6-8 | -2.73(-5.79, 0.33) | 85.6 | 0.001 | 0.412 |
| HOMA-IR | 3 | 111/107 | 6-8 | -0.54(-1.10, 0.02) | 75.3 | 0.017 | 0.542 |
| Total antioxidant capacity (mmol/l) | 2 | 74/72 | 6-8 | 0.03 (-0.06, 0.28) | 21.6 | 0.259 | - |
| hs-CRP (mg/l) | 2 | 66/62 | 8 | -1.33(-2.31, -0.35) | 34.2 | 0.218 | - |
| IL-6 (pg/ml) | 2 | 66/62 | 8 | -0.89(-1.17, -0.61) | 0 | 0.601 | - |
† No. of women with gestational diabetes/ No. of women without gestational diabetes
Other supplementation
In a non-blind randomized clinical study, daily supplementation with 15 mg zinc sulphate in 30 women with GDM reduced neonatal birth weight and macrosomia rate when compared to control women (63).
A research revealed the benefits of alpha-lipoic acid (ALA), an anti-oxidant short-chain fatty acid, at a dosage of 100 mg/d for eight weeks on glycemic indices in women with GDM. At the end of 8-week, FPG, HOMA-IR, and MDA/TAC reduced, and quantitative insulin sensitivity check index (QUICKI) increased in the ALA group compared to the placebo [58].
After six weeks of supplementation, FPG, insulin, and HOMA-IR were considerably lower in the ginger group than in the placebo group, according to a research assessing the effects of daily intakes of 1500 mg ginger in the form of a tablet in women with GDM.Furthermore, postprandial blood glucose was lowered within the intervention group, although there were no significant differences between the two groups in terms of postprandial glucose [61].
Discussion
In this study, the findings of 49 publications from different types of researches on nutritional factors and GDM prevention/management among Iranian women were reviewed. Regarding markers for vitamins and minerals, associations between serum vitamin D and body iron status with GDM were mostly examined. Limited studies also reported associations between serum zinc, magnesium, retinol and α-tocopherol, and serum TAC. Nutritional interventions for the prevention/management of GDM were mostly based on nutritional supplementations, and in this regard, probiotic supplementation was predominant.
Based on the data of 7 observational studies (6 case-control and one cross-sectional) [18–22, 26, 44], including 419 women with GDM and 959 non-GDM women, a mean difference of -8.31 nmol/l (95%CIs; -14.4, -2.12) was estimated in serum vitamin D in women with GDM versus non-GDM women. The findings showed that serum vitamin D at the time of GDM diagnosis was lower in GDM women than non-GDM. Two trials consistently suggested the reduced risk of GDM development in women receiving vitamin D supplementation in the first trimester compared to non-supplemented women [17, 54]. World health organization (WHO) provided low-certainty evidence based on the findings of five trials, including 1744 pregnant women suggesting that vitamin D supplementation may reduce the risk of developing GDM by 50% (95%CIs= 12-72%). Currently, WHO has no general recommendation for vitamin D supplementation in all pregnant women, but in women with low serum vitamin D, a daily intake of 200 IU (5 µg) has been suggested [63]. A dose-response meta-analysis of 9 observational studies recently suggests a reduction of 2% in the risk of GDM per 10 nmol/l increments in circulatory vitamin D [64]. Since the prevalence of vitamin D insufficiency is high in pregnant women in Iran [65], assessing the vitamin D status in early prenatal visits and supplementation with vitamin D should be considered a cost-effective strategy that may prevent GDM. Whether vitamin D supplementation has beneficial effects on maternal and neonatal outcomes in Iranian women with GDM cannot be demonstrated due to the scarcity of studies. In 2019, a meta-analysis of 5 randomized clinical trials (RCTs) including 173 vitamin D-supplemented women suggested a significant mean reduction of 0.46 mmol/l (95%CIs= -0.68, -0.25) for FPG, 0.37% (95%CIs= -0.65, -0.08) for HbA1C, and 4.10 µIU/ml (95%CIs= -5.50, -2.71) for serum insulin [66]. Therefore, based on available studies either in Iran or worldwide, there is no strong evidence supporting the efficacy of vitamin D in the management of GDM.
We estimated a mean difference of 19.3 µg/dl (95%CIs= -1.90, 40.4) for serum iron, 24.2 ng/ml (95%CIs=15.0, 33.4) for ferritin, and 1.14 g/dl (95%CIs=0.32, 1.96) for hemoglobin in women with GDM compared to non-GDM women. A study reported a higher iron status in women with GDM than non-GDM from the first trimester [39]. To prevent maternal anemia and supply iron demand of fetus, WHO is recommended daily oral iron supplementation with 30-60 mg elemental iron for all pregnant women [67]. However, a concern is currently rising about the possible harm of iron supplementation in iron-sufficient pregnant women [68]. Hemoglobin and ferritin measurements early in pregnancy before iron supplementation may reduce the unfavorable effects of iron supplementation in those who may not benefit from the supplementation. In 2017, a meta-analysis based on the data of two prospective studies conducted in the USA suggested a higher risk of GDM in women with higher intakes of heme-iron (Relative risk=1.65; 95CIs= 1.28, 2.12) [69]. There is insufficient data to conclude the association between dietary iron intake and GDM in Iranian pregnant women. Further prospective studies are warranted to determine whether higher intakes of heme-iron pre-pregnancy or during pregnancy increase the risk of GDM in Iranian women.
Studies examining the effects of probiotics added to yogurt or capsule on glycemic parameters of women with GDM did not report consistent findings [48, 50, 53, 55, 59]. No significant impact on FPG, HbA1c, fasting insulin, and HOMA-IR were observed when we pooled their results; however, probiotics’ anti-inflammatory effects have been suggested. Findings of the current studies conducted in Iran could not support the beneficial effects of probiotics on the prevention of GDM or better management of glycemia in women with GDM. Two meta-analyses of RCTs showed that probiotic supplementation improved glycemic control in pregnant women, but the effects depend on GDM status [70, 71]. The probiotic glucose-lowering effect was suggested for only non-GDM women in the earlier study [70] and only GDM women in the later study [71].
Studies evaluating associations between priori dietary patterns and odds of GDM reported inverse associations for adherence to the Mediterranean and DASH diets, and plant-based dietary index, and positive associations for DAL and DII [25, 29, 35, 36]. Findings of the studies on associations between major dietary patterns derived by PCA and GDM were inconsistent [28, 30, 33, 41]. The evidence is currently not sufficient to recommend a specific dietary pattern to prevent GDM. However, adopting a healthy dietary pattern rich in fruits, vegetables, whole grains, legumes, low-fat dairy and reduce intakes of red and processed meats, fast-foods, sugar-sweetened beverage, and high-fat foods pre-pregnancy and during the period is encouraging to mitigate the risk of GDM.
This is a comprehensive review of the literature on nutrition and GDM targeting Iranian women. Searching Persian-databases and including studies published in Persian, in addition to English-databases and studies published in English, is a study strength that increases the number of eligible studies. This study has some limitations. The majority of the observational studies reviewed were case-control, which means they could not demonstrate a cause-and-effect relationship. The representative and non-response rate were the main concerns for the case-control studies. Besides, studies assessing dietary intakes as exposures did not provide any information to show whether blindness to case/control status had been done. Allocation concealment and blinding of participants and personnel (either as a high risk of bias or unclear) were the main concerns for clinical trials. Data from clinical trials could not be used for meta-analysis due to variable interventions and a small number of trials in each intervention. The interventions for the management of GDM were generally eight weeks long, which was rather short.
In conclusion, in Iranian women with GDM, serum vitamin D was lower, and iron status markers, including serum iron, ferritin, and hemoglobin, were higher than those of non-GDM women. Vitamin D and iron status assessments in women early in pregnancy help decide whether vitamin D or iron supplementation is necessary to minimize adverse outcomes. The effects of vitamin D supplementation on maternal and neonatal outcomes of women with GDM are now unclear. The beneficial effects of probiotic supplementation on the prevention and management of GDM are not convincing and deserve further investigation. Some individual clinical trials suggest favorable effects of zinc, ALA, and ginger supplementation on maternal or neonatal outcomes, which need to be confirmed in further studies. Findings from the limited studies demonstrated the inverse associations of the Mediterranean and DASH diets, plant-based dietary index, healthy dietary patterns, and the direct associations of DAL and DII with the odds of GDM. Further prospective investigations are required to determine the nutritional risk factors for the onset of GDM among Iranian women. The studies provide fundamental findings to help design more effective interventions for the prevention and management of GDM.
Supplementary Information
(DOCX 126 KB)
Authors’ contributions
FA and NM contributed to the conceptual design of the study. PM supervised the study. NM developed the overall research plan and study oversight. FRS and NM conducted the research.
NM, FRS and FT independently screened all records based on their titles and abstracts. NM contributed to data analyses and interpretation. NM and FRS drafted the manuscript. FA, PM and FRT provided intellectual comments. All authors reviewed and approved the final version of the manuscript.
Funding
This study was supported by a grant by the Research Institute of Endocrine Sciences, Shahid Beheshti University Medical Sciences, Tehran, Iran.
Data availability
The data used and/ or analyzed during the current study available from the corresponding author on reasonable request.
Code availability
Not applicable.
Declarations
Conflict of interest
Authors declare no conflicts of interest.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Research Institute for Endocrine Sciences at the Shahid Beheshti University of Medical Sciences (IR.SBMU.ENDOCRINE.REC.1399.027).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diab Rep. 2016;16(1):7. doi: 10.1007/s11892-015-0699-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Badakhsh M, Daneshi F, Abavisani M, Rafiemanesh H, Bouya S, Sheyback M, et al. Prevalence of gestational diabetes mellitus in Eastern Mediterranean region: a systematic review and meta-analysis. Endocrine. 2019;65(3):505–514. doi: 10.1007/s12020-019-02026-4. [DOI] [PubMed] [Google Scholar]
- 3.Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Supplement 2):S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 4.Thomas AM, Duarte-Gardea M. Nutritional management for gestational diabetes. Nutrition in the Prevention and Treatment of Disease. Amsterdam: Elsevier; 2017. p. 709–29.
- 5.Schoenaker DA, Mishra GD, Callaway LK, Soedamah-Muthu SS. The role of energy, nutrients, foods, and dietary patterns in the development of gestational diabetes mellitus: a systematic review of observational studies. Diabetes Care. 2016;39(1):16–23. doi: 10.2337/dc15-0540. [DOI] [PubMed] [Google Scholar]
- 6.Association AD. 12. Management of diabetes in pregnancy. Diabetes Care. 2015;38(Supplement 1):S77-S9. doi: 10.2337/dc15-S015. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez TL, Brand-Miller JC. Nutrition therapy in gestational diabetes mellitus: time to move forward. Diabetes Care. 2018;41(7):1343–5. doi: 10.2337/dci18-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamamoto JM, Kellett JE, Balsells M, García-Patterson A, Hadar E, Solà I, et al. Gestational diabetes mellitus and diet: a systematic review and meta-analysis of randomized controlled trials examining the impact of modified dietary interventions on maternal glucose control and neonatal birth weight. Diabetes Care. 2018;41(7):1346–61. doi: 10.2337/dc18-0102. [DOI] [PubMed] [Google Scholar]
- 9.Jin S, Sha L, Dong J, Yi J, Liu Y, Guo Z, et al. Effects of nutritional strategies on glucose homeostasis in gestational diabetes mellitus: a systematic review and network meta-analysis. J Diabetes Res. 2020;2020(23):6062478. doi: 10.1155/2020/6062478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mustafa ST, Hofer OJ, Harding JE, Wall CR, Crowther CA. Dietary recommendations for women with gestational diabetes mellitus: a systematic review of clinical practice guidelines. Nutr Rev. 2021;79(9):988–1021. doi: 10.1093/nutrit/nuab005. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 12 Dec 2021.
- 13.Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7(1):1–11. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Afkhami-Ardekani M, Rashidi M. Iron status in women with and without gestational diabetes mellitus. J Diabetes Complicat. 2009;23(3):194–8. doi: 10.1016/j.jdiacomp.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Hosseinzadeh-Shamsi-Anar M, Mozaffari-Khosravi H, Salami M-A, Hadinedoushan H, Mozayan MR. The efficacy and safety of a high dose of vitamin d in mothers with gestational diabetes mellitus: a randomized controlled clinical trial. Iran J Med Sci. 2012;37(3):159. [PMC free article] [PubMed] [Google Scholar]
- 16.Amiri FN, Basirat Z, Omidvar S, Sharbatdaran M, Tilaki KH, Pouramir M. Comparison of the serum iron, ferritin levels and total iron-binding capacity between pregnant women with and without gestational diabetes. J Nat Sci Biol Med. 2013;4(2):302. doi: 10.4103/0976-9668.116977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shahgheibi S, Farhadifar F, Pouya B. The effect of vitamin D supplementation on gestational diabetes in high-risk women: Results from a randomized placebo-controlled trial. J Res Med Sci. 2016;21:2. doi: 10.4103/1735-1995.175148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akhlaghi F, Bonakdaran S, Fijan A. Comparative study on serum level of vitamin D in women with gestational diabetes and normal pregnant women. Med J Mashhad Univ Med Sci. 2014;57(1):429–35. [Google Scholar]
- 19.Sobhani A, Heidarnezhad Z, Salamat F. Association between vitamin D and gestational diabetes. J Guilan Univ Med Sci. 2016;25(98):45–50. [Google Scholar]
- 20.Mostali M, Etminan-Bakhsh M. Comparison of maternal plasma 25-Hydroxyvitamin D concentrations between pregnant women with GDM and without GDM at 24-28 weeks of gestation who referred to Azad University Hospitals in Tehran between 2016 and 2017. Med Sci J Islamic Azad Univ. 2018;28(3):239–44. [Google Scholar]
- 21.Hosseini MS, Bairamzadeh E, Dadashi AR, Fatahi S, Shiri Malekabad E. Relationship between serum vitamin D level and gestational diabetes mellitus in patients referring to Imam Hossein Hospital in Tehran, Iran, during 2015. Iran J Obstet Gynecol Infertil. 2018;21(10):7–12. [Google Scholar]
- 22.Soheilykhah S, Mojibian M, Rashidi M, Rahimi-Saghand S, Jafari F. Maternal vitamin D status in gestational diabetes mellitus. Nutr Clin Pract. 2010;25(5):524–7. doi: 10.1177/0884533610379851. [DOI] [PubMed] [Google Scholar]
- 23.Javadian P, Alimohamadi S, Gharedaghi MH, Hantoushzadeh S. Gestational diabetes mellitus and iron supplement; effects on pregnancy outcome. Acta Med Iran. 2014;52(5):385–9. [PubMed] [Google Scholar]
- 24.Hekmat K, Bagheri R, Abedi P, Tabesh H. The relationship of fat soluble antioxidants with gestational diabetes in Iran: A case-control study. J Matern-Fetal Neonatal Med. 2014;27(16):1676–9. doi: 10.3109/14767058.2014.892921. [DOI] [PubMed] [Google Scholar]
- 25.Izadi V, Tehrani H, Haghighatdoost F, Dehghan A, Surkan PJ, Azadbakht L. Adherence to the DASH and Mediterranean diets is associated with decreased risk for gestational diabetes mellitus. Nutrition. 2016;32(10):1092–6. doi: 10.1016/j.nut.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Haidari F, Jalali MT, Shahbazian N, Haghighizadeh MH, Azadegan E. Comparison of serum levels of vitamin D and inflammatory markers between women with gestational diabetes mellitus and healthy pregnant control. J Fam Reprod Health. 2016;10(1):1–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Parast VM, Paknahad Z. Antioxidant status and risk of gestational diabetes mellitus: a case-control study. Clin Nutr Res . 2017;6(2):81–8. doi: 10.7762/cnr.2017.6.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sedaghat F, Akhoondan M, Ehteshami M, Aghamohammadi V, Ghanei N, Mirmiran P, et al. Maternal dietary patterns and gestational diabetes risk: a case-control study. J Diabetes Res. 2017;2017:8. doi: 10.1155/2017/5173926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saraf-Bank S, Tehrani H, Haghighatdoost F, Moosavian SP, Azadbakht L. The acidity of early pregnancy diet and risk of gestational diabetes mellitus. Clin Nutr. 2018;37(6):2054–9. doi: 10.1016/j.clnu.2017.09.020. [DOI] [PubMed] [Google Scholar]
- 30.Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Rahimi M. Dietary pattern in pregnancy and risk of gestational diabetes mellitus (GDM) Diabetes Metab Syndr-Clin Res Rev. 2018;12(3):399–404. doi: 10.1016/j.dsx.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Didedar R, Rabaninia T, Barmaki B, Dahmardeh S, Nori F, Bagheri S, et al. Relation between chromium, iron and copper with gestational diabetes in Zabol, Iran. J Clin Diagn Res. 2018;12(11):BC15-BC18.
- 32.Milajerdi A, Tehrani H, Haghighatdoost F, Larijani B, Surkan PJ, Azadbakht L. Associations between higher egg consumption during pregnancy with lowered risks of high blood pressure and gestational diabetes mellitus. Int J Vitam Nutr Res. 2018;88(3–4):166–75. doi: 10.1024/0300-9831/a000505. [DOI] [PubMed] [Google Scholar]
- 33.Asadi M, Shahzeidi M, Nadjarzadeh A, Hashemi Yusefabad H, Mansoori A. The relationship between pre-pregnancy dietary patterns adherence and risk of gestational diabetes mellitus in Iran: A case-control study. Nutr Diet. 2019;76(5):597–603. doi: 10.1111/1747-0080.12514. [DOI] [PubMed] [Google Scholar]
- 34.Hezaveh ZS, Feizy Z, Dehghani F, Sarbakhsh P, Moini A, Vafa M. The association between maternal dietary protein intake and risk of gestational diabetes mellitus. Int J Prev Med. 2019;10:197. [DOI] [PMC free article] [PubMed]
- 35.Zamani B, Milajerdi A, Tehrani H, Bellissimo N, Brett NR, Azadbakht L. Association of a plant-based dietary pattern in relation to gestational diabetes mellitus. Nutr Diet. 2019;76(5):589–96. doi: 10.1111/1747-0080.12512. [DOI] [PubMed] [Google Scholar]
- 36.Shivappa N, Hébert JR, Akhoundan M, Mirmiran P, Rashidkhani B. Association between inflammatory potential of diet and odds of gestational diabetes mellitus among Iranian women. J Matern-Fetal Neonatal Med. 2019;32(21):3552–8. doi: 10.1080/14767058.2018.1466275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Behboudi-Gandevani S, Safary K, Moghaddam-Banaem L, Lamyian M, Goshtasebi A, Alian-Moghaddam N. The relationship between maternal serum iron and zinc levels and their nutritional intakes in early pregnancy with gestational diabetes. Biol Trace Elem Res. 2013;154(1):7–13. doi: 10.1007/s12011-013-9703-y. [DOI] [PubMed] [Google Scholar]
- 38.Lamyian M, Hosseinpour-Niazi S, Mirmiran P, Moghaddam Banaem L, Goshtasebi A, Azizi F. Pre-pregnancy fast food consumption is associated with gestational diabetes mellitus among Tehranian women. Nutrients. 2017;9(3):216. doi: 10.3390/nu9030216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taghavi SA, Tehranian N, Jamhiri R, Aramesh S, Mosadegh M, Rezaee Z, et al. Relation between total Iron intake and gestational diabetes: a cohort study. Hormozgan Medical Journal. 2018;22(1):25–32. [Google Scholar]
- 40.Goshtasebi A, Hosseinpour-Niazi S, Mirmiran P, Lamyian M, Banaem LM, Azizi F. Pre-pregnancy consumption of starchy vegetables and legumes and risk of gestational diabetes mellitus among Tehranian women. Diabetes Res Clin Pract. 2018;139:131–8. doi: 10.1016/j.diabres.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 41.Hajianfar H, Esmaillzadeh A, Feizi A, Shahshahan Z, Azadbakht L. The association between major dietary patterns and pregnancy-related complications. Arch Iran Med. 2018;21(10):443–51. [PubMed] [Google Scholar]
- 42.Mirmiran P, Hosseinpour-Niazi S, Moghaddam-Banaem L, Lamyian M, Goshtasebi A, Azizi F. Inverse relation between fruit and vegetable intake and the risk of gestational diabetes mellitus. Int J Vitam Nutr Res. 2019;89(1-2):37–44. doi: 10.1024/0300-9831/a000475. [DOI] [PubMed] [Google Scholar]
- 43.Hajianfar H, Abbasi K. The association between maternal dietary iron intake during the first trimester of pregnancy with pregnancy outcomes and pregnancy-related complications. 2020;9(1):52–62. [DOI] [PMC free article] [PubMed]
- 44.Maghbooli Z, Hossein-nezhad A, Karimi F, Shafaei AR, Larijani B. Correlation between vitamin D3 deficiency and insulin resistance in pregnancy. Diabetes Metab Res Rev. 2008;24(1):27–32. doi: 10.1002/dmrr.737. [DOI] [PubMed] [Google Scholar]
- 45.Mostafavi E, Nargesi AA, Asbagh FA, Ghazizadeh Z, Heidari B, Mirmiranpoor H, et al. Abdominal obesity and gestational diabetes: the interactive role of magnesium. Magnes Res. 2015;28(4):116–24. doi: 10.1684/mrh.2015.0392. [DOI] [PubMed] [Google Scholar]
- 46.Musavi H, Mohammadi Tahroodi F, Fesahat F, Bouzari Z, Esmaeilzadeh S, Elmi F, et al. Investigating the relationship between magnesium levels and diabetes mellitus in pregnant women. Int J Mol Cell Med. 2019;8(3):223–31. doi: 10.22088/IJMCM.BUMS.8.3.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ouladsahebmadarek E, Sayyah-Melli M, Taghavi S, Abbasalizadeh S, Seyedhejazie M. The effect of supplemental iron elimination on pregnancy outcome. Pak J Med Sci. 2011;27(3):641–5. [Google Scholar]
- 48.Dolatkhah N, Hajifaraji M, Abbasalizadeh F, Aghamohammadzadeh N, Mehrabi Y, Abbasi MM. Is there a value for probiotic supplements in gestational diabetes mellitus? A randomized clinical trial. J Heatlh Popul Nutr. 2015;33:8. doi: 10.1186/s41043-015-0034-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yazdchi R, Gargari BP, Asghari-Jafarabadi M, Sahhaf F. Effects of vitamin D supplementation on metabolic indices and hs-CRP levels in gestational diabetes mellitus patients: A randomized, double-blinded, placebo-controlled clinical trial. Nutr Res Pract. 2016;10(3):328–35. doi: 10.4162/nrp.2016.10.3.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jafarnejad S, Saremi S, Jafarnejad F, Arab A. Effects of a multispecies probiotic mixture on glycemic control and inflammatory status in women with gestational diabetes: a randomized controlled clinical trial. J Nutr Metab. 2016;2016:8. doi: 10.1155/2016/5190846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keshavarzi F, Nankali A, Azizi F, Hematti M. Low-dose versus high-dose vitamin D supplementation and pregnancy outcome in gestational diabetes. World Fam Med. 2017;15(10):50–5. [Google Scholar]
- 52.Zarean E, Tarjan A. Effect of magnesium supplement on pregnancy outcomes: a randomized Control Trial. Adv Biomed Res. 2017;6:109. doi: 10.4103/2277-9175.213879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nabhani Z, Hezaveh SJG, Razmpoosh E, Asghari-Jafarabadi M, Gargari BP. The effects of synbiotic supplementation on insulin resistance/sensitivity, lipid profile and total antioxidant capacity in women with gestational diabetes mellitus: A randomized double blind placebo controlled clinical trial. Diabetes Res Clin Pract. 2018;138:149–57. doi: 10.1016/j.diabres.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 54.Rostami M, Tehrani FR, Simbar M, Bidhendi Yarandi R, Minooee S, Hollis BW, et al. Effectiveness of prenatal vitamin D deficiency screening and treatment program: a stratified randomized field trial. J Clin Endocrinol Metab. 2018;103(8):2936–48. doi: 10.1210/jc.2018-00109. [DOI] [PubMed] [Google Scholar]
- 55.Hajifaraji M, Jahanjou F, Abbasalizadeh F, Aghamohammadzadeh N, Abbasi MM, Dolatkhah N. Effect of probiotic supplements in women with gestational diabetes mellitus on inflammation and oxidative stress biomarkers: A randomized clinical trial. Asia Pac J Clin Nutr. 2018;27(3):581–91. doi: 10.6133/apjcn.082017.03. [DOI] [PubMed] [Google Scholar]
- 56.Alamolhoda SH, Simbar M, Mirmiran P, Mirabi P. The effectiveness of low trans-fatty acids dietary pattern in pregnancy and the risk of gestational diabetes mellitus. Casp J Intern Med. 2019;10(2):197–204. doi: 10.22088/cjim.10.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Asadi N, Vafaei H, Kasraeian M, Yoosefi S, Faraji A, Abbasi L. Effects of prophylactic iron supplementation on outcome of nonanemic pregnant women: A non-randomized clinical trial. J Chin Med Assoc. 2019;82(11):840–4. doi: 10.1097/JCMA.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 58.Aslfalah H, Jamilian M, Khosrowbeygi A. Elevation of the adiponectin/leptin ratio in women with gestational diabetes mellitus after supplementation with alpha-lipoic acid. Gynecol Endocrinol. 2019;35(3):271–5. doi: 10.1080/09513590.2018.1519795. [DOI] [PubMed] [Google Scholar]
- 59.Sahhaf Ebrahimi F, Homayouni Rad A, Mosen M, Abbasalizadeh F, Tabrizi A, Khalili L. Effect of L. acidophilus and B. lactis on blood glucose in women with gestational diabetes mellitus: A randomized placebo-controlled trial. Diabetol Metab Syndr. 2019;11:75. [DOI] [PMC free article] [PubMed]
- 60.Asgharian H, Homayouni-Rad A, Mirghafourvand M, Mohammad-Alizadeh-Charandabi S. Effect of probiotic yoghurt on plasma glucose in overweight and obese pregnant women: a randomized controlled clinical trial. Eur J Nutr. 2020;59(1):205–15. doi: 10.1007/s00394-019-01900-1. [DOI] [PubMed] [Google Scholar]
- 61.Hajimoosayi F, Sadatmahalleh SJ, Kazemnejad A, Pirjani R. Effect of ginger on the blood glucose level of women with gestational diabetes mellitus (GDM) with impaired glucose tolerance test (GTT): A randomized doubleblind placebo-controlled trial. BMC Compl Med Therapies. 2020;20(1):116. [DOI] [PMC free article] [PubMed]
- 62.Rahimi Sharbaf F, Mosavy Fakhr Z, Davari Tanha F. Serum zinc levels in gestational diabetes. Tehran Uni Med J. 2008;66(9):682–7. [Google Scholar]
- 63.WHO antenatal care recommendations for a positive pregnancy experience. Nutritional interventions update: Vitamin D supplements during pregnancy. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/9789240008120. Accessed 12 Dec 2021. [PubMed]
- 64.Sadeghian M, Asadi M, Rahmani S, Zanjani MA, Sadeghi O, Hosseini SA, et al. Circulating vitamin D and the risk of gestational diabetes: a systematic review and dose-response meta-analysis. Endocrine. 2020:1–12. [DOI] [PubMed]
- 65.Tabrizi R, Moosazadeh M, Akbari M, Dabbaghmanesh MH, Mohamadkhani M, Asemi Z, et al. High prevalence of vitamin D deficiency among Iranian population: a systematic review and meta-analysis. Iran J Med Sci. 2018;43(2):125. [PMC free article] [PubMed] [Google Scholar]
- 66.Ojo O, Weldon SM, Thompson T, Vargo EJ. The effect of vitamin d supplementation on glycaemic control in women with gestational diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials. Int J Environ Res Public Health. 2019;16(10):1716. doi: 10.3390/ijerph16101716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.WHO antenatal care recommendations for a positive pregnancy experience. Nutritional interventions update: Multiple micronutrient supplements during pregnancy. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/9789240007789. Accessed 12 Dec 2021. [PubMed]
- 68.Georgieff MK, Krebs NF, Cusick SE. The benefits and risks of iron supplementation in pregnancy and childhood. Annu Rev Nutr. 2019;39:121–46. doi: 10.1146/annurev-nutr-082018-124213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhao L, Lian J, Tian J, Shen Y, Ping Z, Fang X, et al. Dietary intake of heme iron and body iron status are associated with the risk of gestational diabetes mellitus: a systematic review and meta-analysis. Asia Pac J Clin Nutr. 2017;26(6):1092. doi: 10.6133/apjcn.022017.09. [DOI] [PubMed] [Google Scholar]
- 70.Peng T-R, Wu T-W, Chao Y-C. Effect of probiotics on the glucose levels of pregnant women: a meta-analysis of randomized controlled trials. Medicina. 2018;54(5):77. doi: 10.3390/medicina54050077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Łagowska K, Malinowska AM, Zawieja B, Zawieja E. Improvement of glucose metabolism in pregnant women through probiotic supplementation depends on gestational diabetes status: meta-analysis. Sci Rep. 2020;10(1):1–17. doi: 10.1038/s41598-020-74773-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 126 KB)
Data Availability Statement
The data used and/ or analyzed during the current study available from the corresponding author on reasonable request.
Not applicable.