Abstract
BACKGROUND:
The most important cause of mortality due to long bone fractures in the elderly patients are femoral fractures that require total hip arthroplasty (THA). THA surgeries may cause severe postoperative pain, long hospital stays, a need for transfusion and mortality.
OBJECTIVE:
Compare outcomes of spinal anesthesia (SA) versus combined sciatic nerve/lumbar plexus block (CSLPB).
DESIGN:
Retrospective cohort trıal.
SETTING:
University hospital in Turkey.
PATIENTS AND METHODS:
We selected patients from the electronic medical records by date of surgery (most recent first) and compared demographic and pre- and postoperative clinical characteristics including the amount of opioid use within the first 48 postoperative hours, 30-day mortality rates, length of hospital stay, intraoperative oxygen saturation (SpO2) and mean arterial pressure (MAP) values, duration of the surgery, and blood transfusion need.
MAIN OUTCOME MEASURE:
Opioid use within the first 48 postoperative hours.
SAMPLE SIZE:
204, 102 patients in each group with overall median (IQR) age of 82 (10.2) years.
RESULTS:
There was no significant difference between the groups in terms of the amount of opioid use within the postoperative 48 hours, 30-day mortality rates, intensive care need, duration of the surgery, blood transfusion need, and length of hospital stay. While the intraoperative SpO2 value was lower in the CSLPB group (P=.03), MAP values were lower in the SA group (P=.046). Preoperative American Society of Anesthesiology score (ASA) scores (P=.039) and the number of comorbidities were higher in the CSLPB group.
CONCLUSION:
We prefer CSLPB used with standardized sedation protocols for anesthesia in THA surgery in elderly patients.
LIMITATIONS:
Retrospective design and single-centered.
CONFLICT OF INTEREST:
None.
INTRODUCTION
A pproximately 1.66 million hip fractures happen in a year worldwide. About 95% of these fractures happen in individuals older than 60 years.1 Total hip arthroplasty (THA) is one of the common orthopedic surgical procedures that have been used to treat hip fracture since the 1960's.2 THA is the treatment of choice for hip arthritis and will probably continue to be the treatment of choice in the future. Both cemented and uncemented implants can provide good fixation, resulting in positive long-term results.3 However, the postoperative pain in particular, pulmonary complications due to venous thromboembolism and late mobilization4 and intraoperative bleeding due to intraoperative and postoperative risk factors, which increase with age, can occur.5 Allogenic blood transfusion that has to be performed in patients due to bleeding can cause potential risks as well.6 Hypothermia, long hospital stays and mortality especially due to prolonged surgical procedures during the intraoperative period are among the problems that can occur in the patients undergoing THA.7 Recently, the number of THA surgeries has increased up to two fold — the rate of diabetes mellitus in these patients has increased from 10.5% to 24.2% and the rate of obesity from 4% to 10.1% during the preoperative period. Complications after THA such as infection, venous thromboembolism, acute myocardial infarction, and pneumonia are also during the preoperative period.8
The search for an optimal method for intraoperative anesthesia especially in THA surgeries of high-risk patients still continues; however, neuraxial anesthesia (NA) and general anesthesia stand out as the main anesthetic methods that are currently used. Although various regional anesthesia techniques are used, combined sciatic nerve/lumbar plexus block (CSLPB) is the method that is still commonly used today.9 Studies assert that although there is no difference between general anesthesia and spinal anesthesia (SA) methods in terms of total blood loss, occurrence of deep vein thrombosis and postoperative mortality in THA surgeries performed on patients over 65 years of age, SA is more advantageous in terms of nausea and length of hospital stay.10 While methods such as SA, general anesthesia and epidural anesthesia are still used for intraoperative anesthesia in THA surgeries, regional nerve block methods are generally preferred for postoperative analgesia. Despite this preference for NA, the complications related to SA are still a concern in high-risk patients.11
This study aimed to compare the CSLPB block used for patients at high risk of complications, to SA, the most commonly used anesthesia method in THA surgeries.
Our study primarily aimed to compare these methods in terms of the amount of opioid use within the postoperative 48 hours and secondarily compare them in terms of the 30-day mortality rates, length of hospital stays, intraoperative oxygen saturation (SpO2) and mean arterial pressure (MAP) values, duration of the surgery, and need for blood transfusion. The data was also expected to determine which preoperative factors affected anesthesiologist choice of anesthesia method.
PATIENTS AND METHODS
After the study was approved by the ethics committee of Nigde Omer Halisdemir University, Nigde, Turkey ((numbered 2021/16), we retrieved the records of 350 patients who had undergone THA for hip fracture between January 2019 and March 2021 (surgical procedure code, 612320). Patients included in the study were age of 65 or older; had undergone elective or emergent surgeries including primary arthroplasty of hip fractures; with unilateral femoral neck, intertrochanteric or subtrochanteric fractures who were scheduled to undergo surgery within 24-72 hours after the fractures. Exclusion criteria were peripheral nerve block within the last 24 hours, multiple trauma, multiple fractures, pathological fractures, pelvic fractures, femoral fractures, periprosthetic fracture and unsuccessful block. Unsuccessful block was defined as inadequate sensory and motor block after SA or CSLPB.
A minimum total sample size of 102 for each of the two groups was calculated based on the outcome, amount of opioid use within the postoperative 48 hours (type I error rate of 0.05, a power of 0.95 and effect size of 0.50). Sample size was based on the only other study that evaluated opioid use.12 Data was taken from electronic medical records and collected in Microsoft Excel.
Anesthesia
Patients in both groups received a standard sedation protocol. In the SA patients, spinal heavy bupivacaine in the range of 3-4 mL (15-20 mg) was administered in the sitting position or lateral decubitus position by different anesthesiologists. In the CSLPB patients, a 40 mL mixed solution consisting of 20 mL lidocaine hydrochloride 2% (20 mg/mL), 14 mL bupivacaine hydrochloride 0.5% (5 mg/mL), 5.8 mL saline solution, and 0.2 mL adrenaline tartrate (5 μg/mL) was prepared. A mean of 20 mL of the mixed solution was administered by the parasacral approach for sciatic nerve block and a mean of 20 mL was administered by the shamrock technique at the L2-3 or/and L3-4 level for the lumbar plexus nerve block by a single anesthesiologist (Figures 1). Drugs given routinely during the postoperative period included intravenous fentanyl (0.01 mg), intravenous hydromorphone (0.15 mg), intravenous meperidine IV (7.5mg), and intravenous tramadol (10 mg) using 1 mg morphine as a reference dose. Total consumption within 48 hours was recorded. All the records were converted to the equivalent doses of morphine. For the secondary results, the 30-day mortality rates, length of hospital stays, blood transfusion in the hospital, the duration between the first skin incision and the last skin suture, and mean SpO2 and MAP values in the same period of time were recorded.
Figure 1.
Sonography of the injection point for the lumbar plexus block (left) and the parasacral sciatic nerve block (right). ESM: erector spinae muscle, GM: gluteus maximus muscle, IVC: inferior vena cava, PM: psoas major muscle, QF: quadratus femoris muscle, QL: quadratus lumborum muscle, VB: vertebral body.
Statistical analyses
Statistical analyses were performed using the IBM SPSS for Windows version 22.0 (Armonk, New York, United States: IBM Corp). Numerical variables were summarized as mean and standard deviation. The independent samples t test was used in the comparison of normally distributed variables between the groups. The Mann-Whitney U test was used for the non-normally distributed variables. The intergroup changes in blood pressure and SpO2 values and their changes in time were assessed with the repeated measures analysis of variance. The Pearson chi-square test and the Fisher exact test were used in the assessment of statistical significance between categorical variables. The statistical significance level was P<.05. Multivariable logistic regression was used to assess associations of clinical factors with use of either CSLPB and SA. The enter method was used in variable selection.
RESULTS
Of 350 patients initially identified in the medical records, 6 who received SA and 5 who received CSLPB had an unsuccessful block and were excluded; 51 others were excluded for various reasons, leaving 175 in the SA group and 113 in the CSLPB group (Figures 2). We analyzed differences between 102 from each group using the date of surgery for selection (starting with most recent). There was a statistically significant difference between the groups in the preoperative ASA scores (Table 1). Peri- and postoperative outcomes differed only in peripheral oxygen saturation and mean arterial pressure during surgery (Table 2). The total number of comorbidities detected in patients during the preoperative period was significantly higher in the group CSLPB (P<.01). While heart diseases and arrhythmia (P<.01), respiratory system diseases (P<.01) and hypertension (P<.01) were significantly higher in the CSLPB group (Table 3). In the multivariate analysis, the number of comorbidities and the ASA score were associated with the type of anesthesia (Table 4). For the entire study population, the mortality rate was higher in males (24.1% versus 8.7%) (P<.01).
Figure 2.
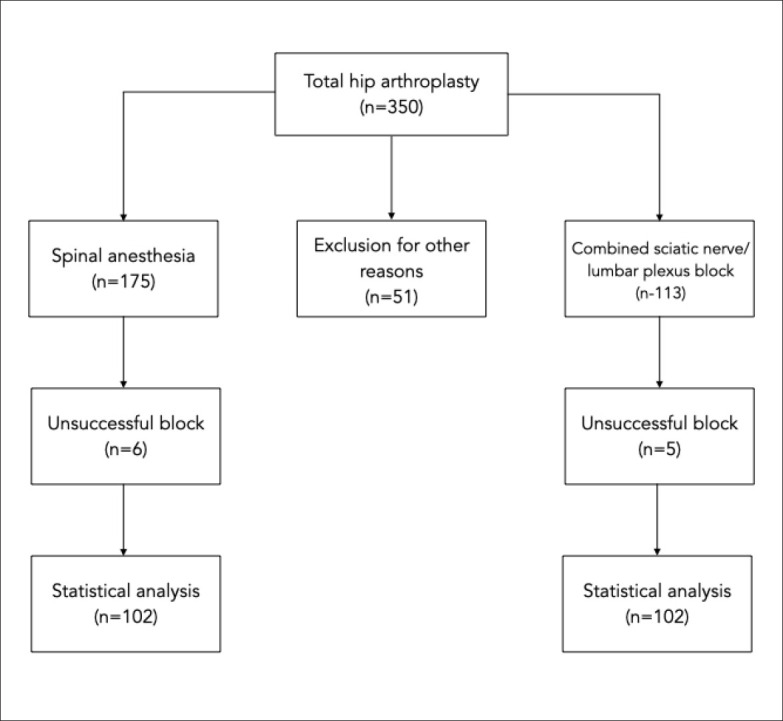
Study flow diagram.
Table 1.
Demographic and clinical features of the anesthesia groups (n=204).
| Lumbar plexus and sciatic nerve block (n=102) | Spinal anesthesia (n=102) | P | |
|---|---|---|---|
| Age (years) | 83 (10), 65–96 | 81 (10), 65–98 | .1383 |
| Sex | |||
| Male | 30 (45) | 37 (55) | .297 |
| Female | 72 (53) | 65 (47) | |
| ASA score | |||
| II | 10 (29) | 24 (71) | .039 |
| III | 57 (54) | 49 (66) | |
| IV | 35 (55) | 29 (45) | |
| Need for intensive care | |||
| Yes | 32 (57) | 24 (43) | .209 |
| No | 70 (47) | 78 (53) |
Data are number of patients (%) except age: median (IQR), range. ASA; American Society of Anaesthesiologists.
Table 2.
Peri- and postoperative outcomes.
| Lumbar plexus and sciatic nerve block (n=102) | Spinal anesthesia (n=102) | P | |
|---|---|---|---|
| SpO2 (%) | 93.1 (2.6) | 94.2 (2.3) | .030 |
| Mean arterial pressure (nnmHg) | 85.3 (11.5) | 82.4 (9.4) | .046 |
| Opioid consumption (mg) | 19.9 (14.4) | 24.2 (21.4) | .397 |
| Length of stay (day) | 7.4 (3–25) | 7.13 (2–30) | .178 |
| Duration of surgery (min) | 72.1 (9.8) | 73.1 (10.3) | .281 |
| Blood transfusion (units) | 1.7 (0–7) | 1.8 (0–9) | .904 |
| Death (30-day mortality) | .385 | ||
| Yes | 14 (58) | 10 (42) | |
| No | 88 (49) | 92 (51) |
Data are mean (standard deviation), mean (range) for blood transfusion, and n (%) for death. SpO2: peripheral oxygen saturation
Table 3.
Diseases in the preoperative period.
| Lumbar plexus and sciatic nerve block (n=102) | Spinal anesthesia (n=102) | P | |
|---|---|---|---|
| Number of comorbidities (mean and range) | 2.43 (1–3) | 1.33 (0–3) | <.001 |
| 0 | 0 | 16 | |
| 1 | 8 | 54 | |
| 2 | 36 | 21 | |
| ≥3 | 58 | 11 | |
| Heart disease or arrhythmia | 57 | 14 | <.001 |
| Respiratory disease | 30 | 8 | <.001 |
| Hypertension | 73 | 27 | <.001 |
| Diabetes mellitus | 24 | 14 | .072 |
| Cerebrovascular diseases | 29 | 10 | <.001 |
| Cognitive diseases | 8 | 15 | .121 |
Table 4.
Multivariable regression analysis of association of clinical factors with use of lunnbar plexus and sciatic nerve block or spinal anesthesia (dependent variable) in patients who underwent prinnary total hip arthroplasty.
| OR | 95% Cl | P | |||
|---|---|---|---|---|---|
| Constant | −.124 | 1.607 | |||
| Duration of surgery | .022 | .020 | 1.02 | 0.98–1.06 | .289 |
| Sex | −.485 | .408 | 0.61 | 0.27–1.36 | .234 |
| ASA score | 1.229 | .416 | 3.41 | 1.51–7.72 | .003 |
| Need for intensive care | −.393 | .580 | 0.67 | 0.21–2.10 | .498 |
| Length of stay | −.002 | .042 | 0.96 | 0.91–1.08 | .960 |
| Connorbidity | −2.584 | .372 | 0.00 | 0.03–0.15 | <.001 |
| Death (30-day mortality) | .782 | .741 | 2.18 | 0.51–9.33 | .291 |
Model summary measures: deviance 170.064, Cox and Snell R square .425, Nagelkerke R square .566. Omnibus test of model coefficients P<.001
DISCUSSION
Although patients older than 65 years are considered the elderly population today, developing medical care and treatment standards have caused an increase in life expectancy. Major hip fractures have become more important risk factors for mortality in patients older than 75 years.13
Our study is the first comparing the effects of SA versus CSLPB for intraoperative anesthesia in THA. In another study, CSLPB decreased intraoperative pain, opioid needs and postoperative bleeding in the early postoperative period in the patients undergoing THA under general anesthesia,14 suggesting that the CSLPB could also be used to obtain maximum analgesic effect in the procedures such as hip arthroplasty.15 Moreover, although different study designs and methods were used, it has been asserted that CSLPB has an anesthetic effect equivalent to SA when a suitable technique and sufficient local anesthetics are used.16 In our study, the CSLPB was used for the intraoperative anesthesia of the patients undergoing THA and provided sufficient anesthesia for surgery with the standardized sedation protocol without requiring additional anesthesia. In addition, in our study, there was no significant difference between the groups in terms of the amount of opioid use within the postoperative 48 hours, the 30-day mortality rates, the need for intensive care, the duration of the operation, the need for blood transfusion, and the length of hospital stay. While intraoperative oxygen saturation value was lower in the CSLPB group, mean arterial pressure values were lower in the SA group. Preoperative ASA scores and number of comorbidities were higher in the CSLPB group.
Today, ultrasonography is widely used for imaging subcutaneous tissues, muscles, peripheral nerves, vessels and bones.17,18 In our study, we used a nerve stimulator under USG guidance in the CSLPB group. Ahamed et al19 reported groups consisting of 25 individuals each that the first occurrence of analgesic need was later in patients receiving lumbar plexus block compared with the patients receiving SA, that a lower amount of analgesic was used in these patients and that they had more stable hemodynamic parameters. However, a sciatic nerve block was not combined with the lumbar plexus block in that study. Amiri et al20 obtained similar results in their study assessing the intraoperative effects of lumbar plexus block. In our study, the postoperative opioid need was lower in the CSLPB group but no statistically significant difference was noted versus the SA group. Pu et al21 reported in their meta-analysis on studies comparing SA and general anesthesia in THA that SA shortened the length of hospital stay and decreased postoperative nausea, but there was no difference between the groups in terms of blood transfusion need and incidence of deep vein thrombosis. In our study, the length of hospital stay and postoperative blood transfusion need were similar in both groups but patients in the CSLPB group had higher ASA scores and a higher number of comorbidities. Chen et al22 reported that epidural or spinal anesthesia was more effective in decreasing the 30-day mortality rate and reducing in-hospital mortality by decreasing acute respiratory failure in hip arthroplasty compared with general anesthesia. They also observed that regional anesthesia was associated with the improved preoperative results. Chen et al also observed that regional anesthesia was associated with the improved preoperative results; however, until more comprehensive comparisons are performed it is possible that the preference may return to peripheral nerve blocks.
Nearly all of the studies comparing anesthesia methods in hip fractures have compared general anesthesia, spinal anesthesia, or combined or epidural anesthesia methods. Gremillet et al23 reported in their study of patients in a large Swedish registry that only 16% of THAs were performed under general anesthesia but the anesthesia technique had no effect on the 30-day mortality rate. They also reported that factors mostly associated with a lower 30-day mortality rate were increasing age, ASA classification and male gender. In our study, there was no significant difference between the two groups in the 30-day mortality rate and length of hospital stay. Moreover, we observed that mortality rates were significantly higher in males (P<.01). These results were consistent with the findings of the study by Gremillet et al.23 Additionally, there was no difference in the mortality rate and length of hospital stay despite high ASA score and a high number of comorbidities.
The important factor in the selection of anesthesia method to the anesthesiologist is the expectation of fewer postoperative complications. Therefore, neuraxial (NA) is preferred in elderly patients and patients with critical preoperative condition if there is no contraindication.24 In addition to this preference for spinal or epidural anesthesia over general anesthesia, the belief that the CSLPB is potentially an alternative to NA is becoming more common today. Gabriel et al25 investigated factors affecting the use of NA in a registry study of more than 100 000 THA patients. They reported that the use of NA was low in university hospitals, in cases where surgery was expected to last long, in cases that did not include an assistant, in patients with high ASA scores, and in surgeries that included anesthesia methods without board certification for the regional anesthesia. Low use of NA in cases with high ASA scores and a high number of comorbidities was also interesting. However, although this study included a large number of patients, it involved clinics where traditional anesthesia methods were preferred; in addition, the number of certified personnel for NA was limited in these clinics. This result suggests that an increase in the use of NA by anesthesiologists will require an increase in their desire to learn new methods. In our study, the most important reasons why CSLPB was preferred were the higher number of comorbidities, higher ASA scores and the presence of an anesthesiologist experienced in this field. The need for intensive care, length of hospital stay, gender, and duration of the surgery were not related to the preferred anesthesia method.
Petchara et al26 asserted that CSLPB in patients undergoing THA could be more efficient and safer and could be used alone in patients with severe preoperative conditions and in patients with a contraindication for NA. However, that study was performed on 70 patients and did not include a control group. In our study, there were patients with severe preoperative conditions and high ASA scores in the CSLPB group. While the number of patients with pulmonary disease was 30 in the CSLPB group, in the SA group only 8 patients had pulmonary disease. Intraoperative SpO2 values were lower in the CSLPB group, which suggests that the low SpO2 values were caused by pulmonary disease independently of the anesthesia method used for patients.
One of the most important side effects of SA in elderly patients is the drastic decrease in the cardiac output and blood pressure after the start of surgery. It has been reported that the main reason for this is not the decrease in the systemic vascular tonus but the decrease in stroke volume contrary to what is believed. This decrease can be observed independently of the local analgesic dose used for SA.27 In our study, MAP values measured during the intraoperative period were significantly lower in the SA group, including in patients with milder preoperative clinical conditions probably because the anesthesiologists preferred more SA in patients with milder preoperative conditions. In Roche et al28 the 30-day mortality rate was 9%, and the three or more comorbidities was the most important factor associated with mortality. Postoperative mortality was mostly caused by respiratory system problems (43%) and heart failure (45%) in patients older than 60 years (one comorbidity in 35%, two in 17% and three or more comorbidities in 7%). In our study, the 30-day mortality rate was 11.2%. However, our patient population was older than 65 years and only elective and emergent hip arthroplasties were included. While the number of patients with three or more comorbidities was 56% in the CSLPB group it was only 11% in the SA group.
Limitations of our study were the use of retrospective data from a single center. The data that were intraoperatively recorded were limited because of the duration of the surgery and SpO2 and MAP values that were obtained from the anesthesia follow-up form were not ideal as the study was not planned prospectively.
In conclusion, CSLPB was equivalent to NA block without affecting postoperative analgesic consumption, mortality rate and length of hospital stay in patients with a higher number of comorbidities and higher ASA scores. Therefore, we believe that CSLPB used with standardized sedation protocols is preferable to SA for the anesthesia in elderly patients undergoing THA. More comprehensive studies are needed to define CSLPB as the optimal peripheral nerve block method in THA patients.
Funding Statement
None.
REFERENCES
- 1.Gullberg B, Johnell O, Kanis JJOi. World-wide projections for hip fracture. 1997;7(5):407–413. [DOI] [PubMed] [Google Scholar]
- 2.Charnley J. Arthroplasty of the hip. A new operation. Lancet. May 27 1961;1(7187):1129–1132. [DOI] [PubMed] [Google Scholar]
- 3.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. Oct 27 2007;370(9597):1508–1519. [DOI] [PubMed] [Google Scholar]
- 4.Singh JA, Lewallen D. Predictors of pain and use of pain medications following primary Total Hip Arthroplasty (THA): 5,707 THAs at 2-years and 3,289 THAs at 5-years. BMC Musculoskelet Disord. May 13 2010;11:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saito K, Kaiho Y, Tamii T, Nakamura T, Kameyama E, Yamauchi M. Intraoperative hemorrhage in revision total hip arthroplasty: a retrospective single-center study. J Anesth. Jun 2019;33(3):399–407. [DOI] [PubMed] [Google Scholar]
- 6.Song K, Pan P, Yao Y, Jiang T, Jiang Q. The incidence and risk factors for allogenic blood transfusion in total knee and hip arthroplasty. J Orthop Surg Res. Aug 28 2019;14(1):273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frisch NB, Pepper AM, Rooney E, Silverton C. Intraoperative Hypothermia in Total Hip and Knee Arthroplasty. Orthopedics. Jan 1 2017;40(1):56–63. [DOI] [PubMed] [Google Scholar]
- 8.Maradit Kremers H, Visscher SL, Moriarty JP, et al. Determinants of direct medical costs in primary and revision total knee arthroplasty. Clin Orthop Relat Res. Jan 2013;471(1):206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang C, Wei J, Cai X, Lin W, Fan Y, Yang F. Efficacy and Safety of 3 Different Anesthesia Techniques Used in Total Hip Arthroplasty. Med Sci Monit. Aug 2 2017;23:3752–3759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pu X, Sun JM. General anesthesia vs spinal anesthesia for patients undergoing total-hip arthroplasty: A meta-analysis. Medicine (Baltimore). Apr 2019;98(16):e14925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ueshima H, Tanaka N, Otake H. Greater analgesic effect with intermittent compared with continuous mode of lumbar plexus block for total hip arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. Jun 2019;44(6):632–636. [DOI] [PubMed] [Google Scholar]
- 12.Liang C, Wei J, Cai X, et al. Efficacy and safety of 3 different anesthesia techniques used in total hip arthroplasty. 2017;23:3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karademir G, Bilgin Y, Erşen A, et al. Hip fractures in patients older than 75 years old: Retrospective analysis for prognostic factors. 2015;24:101–104. [DOI] [PubMed] [Google Scholar]
- 14.Stevens RD, Van Gessel E, Flory N, Fournier R, Gamulin ZJTJotASoA. Lumbar plexus block reduces pain and blood loss associated with total hip arthroplasty. 2000;93(1):115–121. [DOI] [PubMed] [Google Scholar]
- 15.Jaffe JD, Morgan TR, Russell GBJJop, pharmacotherapy pc. Combined sciatic and lumbar plexus nerve blocks for the analgesic management of hip arthroscopy procedures: a retrospective review. 2017;31(2):121–125. [DOI] [PubMed] [Google Scholar]
- 16.de Visme V, Picart F, Le Jouan R, et al. Combined lumbar and sacral plexus block compared with plain bupivacaine spinal anesthesia for hip fractures in the elderly. 2000;25(2):158–162. [DOI] [PubMed] [Google Scholar]
- 17.Chang P-H, Chen Y-J, Chang K-V, Wu W-T, Özçakar L. Ultrasound measurements of superficial and deep masticatory muscles in various postures: reliability and influencers. Scientific reports. 2020;10(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han D-S, Wu W-T, Hsu P-C, Chang H-C, Huang K-C, Chang K-V. Sarcopenia Is Associated With Increased Risks of Rotator Cuff Tendon Diseases Among Community-Dwelling Elders: A Cross-Sectional Quantitative Ultrasound Study. Frontiers in medicine. 2021;8:566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahamed ZA, Sreejit MS. Lumbar Plexus Block as an Effective Alternative to Subarachnoid Block for Intertrochanteric Hip Fracture Surgeries in the Elderly. Anesth Essays Res. Apr-Jun 2019;13(2):264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amiri HR, Zamani MM, Safari S. Lumbar plexus block for management of hip surgeries. Anesth Pain Med. Aug 2014;4(3):e19407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pu X, Sun J-mJM. General anesthesia vs spinal anesthesia for patients undergoing total-hip arthroplasty: A meta-analysis. 2019;98(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen DX, Yang L, Ding L, Li SY, Qi YN, Li QJM. Perioperative outcomes in geriatric patients undergoing hip fracture surgery with different anesthesia techniques: A systematic review and meta-analysis. 2019;98(49). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gremillet C, Jakobsson JGJF. Acute hip fracture surgery anaesthetic technique and 30-day mortality in Sweden 2016 and 2017: A retrospective register study. 2018;7.1009:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White S, Moppett I, Griffiths RJA. Outcome by mode of anaesthesia for hip fracture surgery. An observational audit of 65 535 patients in a national dataset. 2014;69(3):224–230. [DOI] [PubMed] [Google Scholar]
- 25.Gabriel RA, Kaye AD, Jones MR, Dutton RP, Urman RDJTJoa. Practice variations in anesthetic care and its effect on clinical outcomes for primary total hip arthroplasties. 2016;31(4):918–922. [DOI] [PubMed] [Google Scholar]
- 26.Petchara S, Paphon S, Vanlapa A, Boontikar P, Disya KJMoj. Combined lumbar-sacral plexus block in high surgical risk geriatric patients undergoing early hip fracture surgery. 2015;9(3):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hofhuizen C, Lemson J, Snoeck M, Scheffer G-JJL, anesthesia r. Spinal anesthesia-induced hypotension is caused by a decrease in stroke volume in elderly patients. 2019;12:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roche J, Wenn RT, Sahota O, Moran CGJB. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. 2005;331(7529):1374. [DOI] [PMC free article] [PubMed] [Google Scholar]



