Abstract
BACKGROUND:
Fetal effects of radiation are associated with the gestational week of exposure, dose, and duration of exposure, but the perception of risk of radiation in expecting mothers is greater than the actual risk of physical effects.
OBJECTIVES:
Evaluate the overestimation of the teratogenic risk in women exposed to radiation and the role of teratological counseling in minimizing preconceptions.
DESIGN:
Analytical, cross-sectional.
SETTING:
Tertiary care center, genetic diseases diagnosis center.
PATIENTS AND METHODS:
Out of 10 784 people who applied for teratological consultation between 2009 and 2018, pregnant women meeting inclusion criteria and exposed to radiation were selected as the study group; pregnant women without radiation exposure were selected as the control group. Two subgroups of the study group based on the week and dose of exposure were also analyzed.
MAIN OUTCOME MEASURES:
Abortion rate, termination recommendation rates before and after teratological counseling.
SAMPLE SIZE::
461 pregnant exposed to radiation; 213 pregnant women without radiation exposure.
RESULTS:
Preterm birth and termination rates differed significantly between cases and controls (P=.038, P=.019, respectively). Termination recommendation at the first examination was more frequent for both the week of exposure overall and dose subgroups comparing cases and controls (P<.001). In the comparison of subgroups by week of exposure, only the miscarriage rate was statistically significant (P=.007). After teratological counseling termination decision rates were significantly decreased (P<.001).
CONCLUSION:
Subjective perceptions about the risks of radiation may lead to the termination of an otherwise wanted pregnancy. Teratological counseling is crucial for the prevention of termination of pregnancy, clarifying misinformation, and minimizing anxiety.
LIMITATIONS:
With the exception of measurable values as calculated doses of radiation, the conclusions are mostly derived from medical records and subjective responses of pregnant women. The termination rates in our study probably do not reflect the whole population.
CONFLICT OF INTEREST:
None.
INTRODUCTION
Agents that cause structural and functional disorders in the fetus are called teratogens. Teratogenic agents can be physical, chemical, biological, infectious, and genetic. Radiation is a common and a well-known physical teratogen.1 It was only after the Hiroshima and Nagasaki disasters that the fetal effects of radiation drew attention. The effect on the fetus is often based on animal studies and the data from survivors of the atomic bombings.2,3
Studies have demonstrated that the effect of radiation on the fetus is associated with the week of gestation of the exposure, the dose, and the duration of exposure. The first month of gestation (0-4 weeks) is called the “all-or-none period” meaning an exposure will either result in fetal loss or have no obvious effect on embryonic development.3 The weeks following the first month are considered the organogenesis period in which anomalies are seen. Although some animal studies have claimed otherwise,4-6 teratogens generally do not cause fetal anomalies in humans during this first month of gestation.7,8 Radiation exposure to the gravid uterus is better avoided, but up to 50 mGy is considered to be a negligible dose by the United States National Council for Radiation Protection (USNR).9 Acute exposure has mostly immediate effects while chronic exposure has delayed effects; the radiation effect seems to be higher in acute exposures. The frequency of fetal abnormalities and abortion tend to increase at doses of 100-150 mGy and above.10 The dose in diagnostic X-rays is far below these values. During pregnancy, the fetus may be exposed to up to 5 mGy dose of radiation under normal conditions.2
Pregnant women are often exposed to radiation due to radiodiagnostic procedures, not knowing that they are pregnant. More than 3.5 billion radiodiagnostic procedures are performed annually worldwide.11 In Turkey, about 80 million radiodiagnostic procedures were performed in 2018, according to Ministry of Health data.12 Women of reproductive age reportedly make up to 22% of society and 45% to 51% of pregnancies are unplanned.13 The public, especially pregnant women, tend to exaggerate the risk of radiation. The the advice of primary health care specialists on the fetal effects of radiation exposure often does not coincide with the scientific facts,14-17 which may lead to misconceptions among pregnant women. An exaggerated perception of the harm of radiation can increase the number of terminations of otherwise wanted pregnancies.7 Teratological counseling is a practical, low-cost, and convenient public health service in relieving the concerns and anxiety of pregnant women and preventing unnecessary termination after diagnostic radiation exposure.7
There are numerous studies on the fetal effects of high-dose radiation. To the best of our knowledge, this is the first study evaluating the perception of the effects of radiation exposure, the effects of diagnostic radiation exposure on the fetus and the role of teratological counseling in a Turkish population. The aim of the study was to evaluate the subjective risk perception of radiation in Turkish women exposed to radiation, pregnancy outcomes, and the role of teratological counseling in minimizing this perception.
PATIENTS AND METHODS
From among 10 784 pregnant women who applied for teratological consultation and whose follow-up were completed, 2844 women exposed to radiation were chosen for the study. Information was gathered from the patient files and evaluated. Pregnant women who met the criteria were selected as the study group. The control group was selected among pregnant women who applied for teratological counseling and did not have a history of radiation and obvious teratogen exposure in pregnancy. The study was conducted in accordance with the principles expressed in the Declaration of Helsinki. The institutional review board approved the study protocol with the decision number 12.06.2020/2433. Signed informed consent was obtained from all participants at the time of teratological consultation.
The study group was selected from pregnant women referred to our center for teratological counseling, who were exposed to radiation for diagnostic purposes, but were not aware of their pregnancy at the time of exposure. Exclusion criteria were conditions with proven teratogenic effects such as exposure to high-dose radiation due to radiotherapy, I-131 used for therapeutic purposes, and the presence of any chronic disease (diabetes mellitus, hypertension, epilepsy, etc.), TORCH group infections, active and/or history of tobacco, alcohol, and substance use. Pregnant women using C, D, X risk group drugs (isotretinoin, warfarin, valproic acid, and others) according to the US Food and Drug Administration pregnancy risk category were also excluded from the study.
The study group was further evaluated by two subgroups according to the gestational week of radiation exposure (first month (0-4 weeks) and after the first month (4.1-28 weeks) and according to exposed dose (≤5 mGy and >5 mGy). Gestational age was determined by ultrasound imaging by an obstetrician-gynecologist. The fetal radiation dose of all subjects was calculated by a medical physicist in our hospital using the formula by Ozbayrak et al.18 Teratological consultation is given with a written report by a team of physicians specialized in medical genetics. This report consists of the information gathered from pediatric geneticist, medical geneticist, obstetrician-gynecologist, radiologist and physicist. The technical information required for fetal radiation dose calculations was obtained from the radiologist where the radiological screening was done. The babies were examined by a pediatric genetics specialist. The control group was selected from among healthy pregnant women who applied to our center either by the recommendation of their physician or by their own will. The control group may have been using pregnancy risk category A/B medications, or cosmetic procedures such as laser hair removal and who were not exposed to radiation for diagnostic or therapeutic purposes during pregnancy.
All statistical analyzes were performed using the IBM SPSS program (version 25.0 for Windows, (Armonk, New York, United States: IBM Corp). Continuous variables with normal distribution were expressed as mean and standard deviation, the chi-square test of independence was used in the analysis of categorical data. Percentages were used to express categorical values. The t test was used for the measurement of normally distributed numerical data. Results were considered statistically significant at a 95% confidence interval and with a P value of <.05.
RESULTS
Of the 2844 women who were exposed to radiation, we selected 461 pregnant women aged 17-47 years of age (mean [SD], 31.7 [5.6] years) for the study group. The control group consisted of 213 pregnant women aged 18-46 (31.6 [5.8]) years who had not been exposed to radiation. Most of the babies (56.7%) were delivered by cesarean section (Table 1). The gestational age at which pregnant women were exposed to radiation ranged from 2-182 days (mean [SD] 31.7 [21.4] days). The gestational age at the time of admission to the out-patient clinic was 24-206 days (mean [SD] 65.5 [27.3] days). Figure 1 shows the distribution of pregnant women in the study group according to the referring institute and location of the first-contact physician who made the referral with a suggestion or no suggestion of termination. Although the pregnant women who applied to our center referred from private clinics were the lowest in number (13%), they held the highest rate of termination recommendation (73.3%).
Table 1.
Characteristics of the pregnant women included in the study (n=674).
| Study group (n=461) | Control group (n=213) | P value | |
|---|---|---|---|
| Age (years), mean (standard deviation) | 31.7 (5.6) | 31.6 (5.8) | .773 |
| Pregnancy plan | |||
| Unplanned | 448 (97.2) | 203 (95.3) | .213 |
| Planned | 13 (2.8) | 10 (4.7) | |
| Assisted reproductive techniques | 10 (2.2) | 3 (1.4) | .764 |
| Type of deliverya | |||
| Cesarean delivery | 232 (56.7) | 127 (65.1) | .038 |
| Normal | 177 (43.3) | 66 (31) | |
| Recommendation of termination by first-contact physician | 240 (52.1) | 3 (1.4) | <.001 |
Data are number (%).
Denominator, number of live births (n=409 in study group and 195 in control group).
Figure 1.
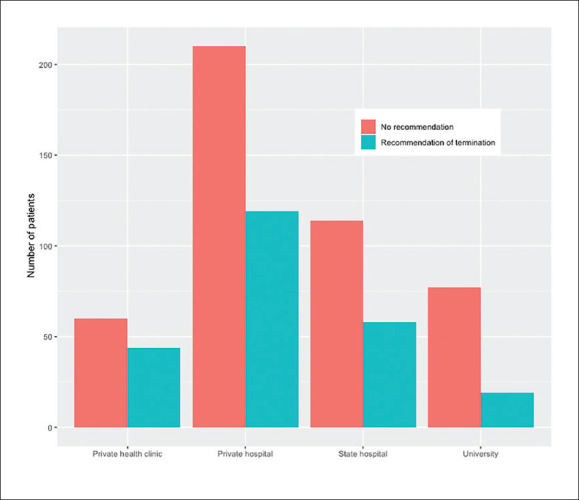
Distribution of referred pregnant women with and without recommendation of termination by referring institute (n=461).
The range and mean (SD) of calculated fetal doses was 0.1-10.3 mGy (0.68 [1.30]) for the study group. Twenty-three percent (n=106) had multiple radiological imagings. Termination advice according to imaging modalities is shown in Figure 2. Termination of pregnancy was suggested to 240 (52.1%) women exposed to radiation and 3 (1.4%) women in the control group at first examination (P<.001). The list of diagnostic radiological procedures is given in the Supplemental Table 1. While there was no statistically significant difference in the number of miscarriages, medical curettage and congenital anomalies between the study and the control groups, terminations (P=.019) and premature births (P=.039) were significant (Table 2). The distribution of the anomalies between the study and control groups is shown in Supplemental Figure 1.
Figure 2.
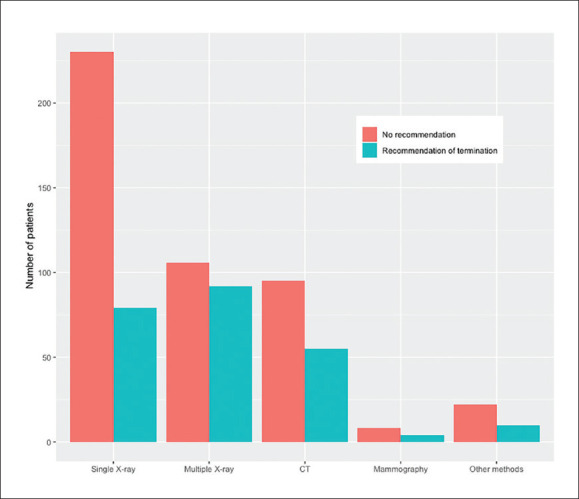
Termination rates per radiodiagnostic method with and without recommendation of termination.
Table 2.
Pregnancy outcomes.
| Study group (n=461) | Control group (n=213) | P value | |
|---|---|---|---|
| Live birthsa | 409 (88.7) | 195 (91.5) | .255 |
| Prematurity | 33 (7.2) | 6 (2.8) | .039 |
| Congenital anomaly | 19 (4.1) | 5 (2.3) | .351 |
| Miscarriage | 21 (4.8) | 10 (4.7) | .999 |
| Medical curettage | 7 (1.5) | 5 (2.3) | .657 |
| Termination | 24 (5.2) | 3 (1.4) | .019 |
Data are number (%).
Live births include prematurity and congenital anomalies.
Out of 461 women in the study group, 239 (51.8%) were exposed to radiation in weeks 0-4 of gestation and 222 (48.2%) were exposed after 4 weeks of gestation (4.1-28 weeks). When the exposed dose was considered, 330 women (71.6%) were exposed to ≤5 mGy dose and 131 (28.4%) were exposed to >5 mGy dose. No significant difference was found in number of births with congenital malformation, number of premature births, abortions, medical curettage, and termination (P>.05) between high-dose (> 5 mGy) vs low-dose (≤5 mGy) groups. While there was no difference in the first month of pregnancy (0-4 w) in terms of congenital malformation, medical curettage, premature birth, and termination (P>.05); a statistically significant difference was found in the frequency of miscarriage (P=.007). Termination recommendation at the first examination was significant for both of the exposed week and exposed dose subgroups (P<.001) (Table 3). In all cases to whom termination was suggested, the number of pregnant women who had termination after teratological counseling was significantly lower than the number of those who decided to continue the pregnancy (P<.001).
Table 3.
Subgroup (radiation-exposed week and dose) comparisons in the study group (n=461).
| Radiation exposed week | Radiation exposed dose | |||||
|---|---|---|---|---|---|---|
| 0-4 w (n=239) | 4.1-28 w (n=222) | P value | ≤5 mGy (n=330) | >5 mGy (n=131) | P value | |
| Live birth | 205 (85.8) | 204 (91.9) | .054 | 291 (88.2) | 118 (90.1) | .677 |
| Prematuritya | 14 (5.9) | 19 (8.6) | .346 | 22 (6.7) | 11 (8.4) | .653 |
| Congenital anomalyb | 11 (4.6) | 8 (3.6) | .761 | 12 (3.6) | 7 (5.3) | .567 |
| Miscarriage | 17 (7.1) | 4 (1.8) | .007 | 15 (4.5) | 6 (4.6) | 1.00 |
| Medical curettage | 3 (1.3) | 4 (1.8) | .716 | 6 (1.8) | 1 (0.8) | .679 |
| Termination | 14 (5.9) | 10 (4.5) | .657 | 18 (5.5) | 6 (4.6) | .882 |
| Recommendation of termination by first-contact physician | 105 (43.9) | 135 (60.8) | <.001 | 141 (42.7) | 99 (75.6) | <.001 |
Data are number (%).
Denominator, number of live births.
Discussion
The extent of radiation exposure that is hazardous depends on the radiation dose absorbed, the type of radiation, and the affected organ or tissue. The two general types of biological effects are either deterministic or stochastic. Teratogenic effects are deterministic and the severity is associated with the dose, duration and week of exposure.19 High-dose radiation exposure has been reported to cause an increase in the frequency of microcephaly, developmental delay, preterm birth, and abortion in the fetus.3,9 No effects of low-dose radiation have been observed in humans.19,20 Many health care providers have inadequate information regarding the teratogenic effects of radiation. Teratological counseling is of crucial importance and should be encouraged for supporting both maternal and neonatal wellbeing. To the best of our knowledge, this is the first study evaluating fetal outcomes of diagnostic radiation exposure, risk perception of both physicians and pregnant women, and the role of teratological counseling in minimizing this perception in the Turkish population.
The perception of radiation risk in expecting mothers is greater than its actual effects during pregnancy. In our study, according to the responses of pregnant women, termination of pregnancy was recommended at the first examination before the teratological consultation in 52.1% of the pregnant women in the study group. The high rate of termination recommendation to our study group at first examination may result from incorrect interpretation of the literature or inadequate information about the risk of radiodiagnostic procedures during pregnancy. Most of the termination suggestions were made for multiple images and for CT scans. This may be due to the physicians' tendency to avoid risks and engage in self-protective behavior to avoid malpractice. Although the number of pregnant women who applied to our center were referred from private clinics was the lowest, they had the highest rate of termination recommendation. After teratological consultation, the number of pregnant women who terminated their pregnancies (24 out of 240) were significantly lower than those who continued to their pregnancies. These results demonstrate the impact of teratological counseling.
Overestimating the radiation risk for pregnant women is a common problem among health care providers. According to published information, 40% of primary care physicians and 70% of obstetricians suggested termination.21 Another study states that 20% of the specialists and 30% of the primary care physicians had insufficient knowledge about radiation, and unfortunately, overestimated the risk by the following rates: for plain radiography; 38% of primary care physicians, 22.9% of obstetricians, and for CT scan; 63.2% of family physicians and 75.9% of obstetricians.14
The cesarean delivery rates in our study were similar to the data of the Turkish Ministry of Health12 in the whole group and were higher than that reported in the literature.22,23 The rates between groups were statistically significant (P=.038). Although there has been a fall in rates of unintended pregnancy in Europe and US,24 in our study, this rate was 97%, considerably higher than any reported to date.
When the pregnancy outcomes were compared between groups, there was a significant difference in premature births and termination rates. Previous studies have reported that the rate of termination was increased in pregnant women exposed to diagnostic radiation.19,20 The estimated rate of pregnancy termination between 2010-2014 was 35 per 1000 women ages 15 to 44,25 with lower rates in North America,26 northern and western Europe.27
According to World Health Organization, the rate of preterm birth ranges from 5% to 18% of babies born (https://www.who.int/news-room/fact-sheets/detail/preterm-birth). The rates differ by country.28 The results for our study for the rates of pregnancy termination and preterm birth were 1.4-5.2% and 2.8-7.2%, respectively. In the all-or-none period (0-4 w), a statistically significant difference was found in terms of miscarriages and termination recommendation at the first examination between the case and control groups. When the prenatal effects of diagnostic radiation were considered, there was an increase in spontaneous abortion rates, and this increase may be associated with the extent of follow-up periods and exposure to radiation in early pregnancy.20 When the pregnant women in exposed dose subgroups were analyzed, a statistically significant difference was found only in terms of termination recommendation (P<.001). The fetal dose calculated in the study group was 0.68 [1.30] mGy. This value is in the safe range according to USNR. No significant difference was observed between radiation subgroups in terms of congenital anomalies. The rate of anomalies in the group exposed to more than 5 mGy radiation is slightly higher than expected. Although these abnormalities are not related to radiation effects and this result is not statistically significant, previous literature indicate that some eye anomalies29 and reduced head circumference30 occurred following low-dose radiation exposure.
Studies have reported that fear and anxiety increase the risk of termination of an otherwise wanted pregnancy. The public, especially pregnant women, often tend to overestimate the risk associated with radiation. This tendency may have resulted from the “Pregnant women should not enter” warning sign on the entrance gate of the radiography rooms, contradictory information about radiation on the internet, and risk assessment incompatible with scientific facts at the first examination.14
In addition to the recommendation of the first contact physician for termination of pregnancy without any medical indication, factors such as an unplanned pregnancy, emotional pressure on pregnant women by close relatives, and unwillingness of spouses to take risks may also have a role in the termination decision. Termination rates increase due to the concern of birth defects in pregnant women exposed to diagnostic radiation.14 Most of the pregnant women who applied to our center had intense fear and anxiety for birth defects in their babies, regardless of common pregnancy concerns prior to counseling. Teratogenic risk perception was high even in safe exposures, and it is very difficult to change it even with solid evidence. However, after teratological counseling, the ratio of terminated pregnancies was statistically significantly lower compared to the rate of continued pregnancies as reported in the literature.31,32 Teratological counseling is effective in preventing abortions based on groundless anxieties and risk assessment is necessary to understand the outcomes of teratogen exposure.33,34
The study has several strengths. First, compared to other observational studies demonstrating the effects of low-dose radiation, our study includes a control group. The other strength of our study is that the study group is evaluated together in terms of exposed dose and the week of exposure. The study addresses the correct management of the risk perception due to radiation exposure during pregnancy in healthcare professionals and pregnant women by ensuring the correct interpretation of dose and time dependent effects of radiation. The study also underscores the impact of proper teratological counseling to reduce risk preconception. The collaboration of healthcare professionals with genetic counselors in this regard will provide comprehensive care for pregnant women. A limitation of our study is that the information obtained from pregnant women is based on recall. The rates found in our study would not reflect the whole population.
In conclusion, the association between radiation exposure and the termination decision of otherwise wanted pregnancies is a public health problem. The most important concern of the parents is having a baby with serious birth defects. The obstetrician's concerns are the patient's well-being, reducing the risk for the patient, and avoiding malpractice. Teratological counseling will act as an interface to reduce this pressure on the physician and family in avoiding misconceptions and unnecessary terminations. Societal norms, fear of having a diseased child, defensive medicine, and poor knowledge of teratogenicity are a societal problem. Increasing the number of centers for teratological counseling, training physicians, and also increasing the knowledge of the public by providing fact sheets or informative meetings and by using telemedicine will be among steps to take in the future. We believe that increasing the awareness of teratogenic effects of radiation in developing countries is of paramount importance.
ACKNOWLEDGMENTS
We thank Dr. Selcuk Sozer Tokdemir, Dr. Selcuk Dasdemir, Dr. Bugrahan Duz, and Dr. Atıl Yuksel for their valuable contributions.
SUPPLEMENTS
Table S1.
Diagnostic radiological procedures.
| Diagnostic radiological procedures | n=461 (%) |
|---|---|
| Multiple x-ray views | 106 (23) |
| Chest x-ray | 93 (20.2) |
| Abdominal x-ray | 41 (9) |
| Cranial CT | 39 (8.4) |
| Dental x-ray | 31 (6.7) |
| Extremities x-ray | 26 (5.6) |
| Abdominal CT | 18 (3.9) |
| Lumbar x-ray | 17 (3.7) |
| Paranasal sinus CT | 17 (3.7) |
| Maxillary sinus graphy | 15 (3.3) |
| Thorax CT | 10 (2.2) |
| Mammography | 8 (1.7) |
| Cervical x-ray | 7 (1.5) |
| Pelvic CT | 6 (1.3) |
| Temporal CT | 5 (1.1) |
| Other methods | 22 (4.7) |
Figure S1.
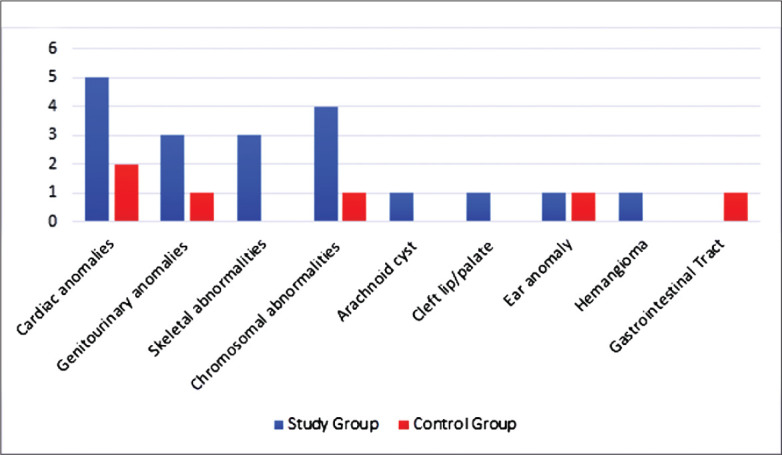
The distribution of anomalies in the study and control groups
Funding Statement
None.
REFERENCES
- 1.Calado AM, Dos Anjos Pires M. An overview of teratology. Methods in Molecular Biology. 2018;1797:3-32. [DOI] [PubMed] [Google Scholar]
- 2.Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstet Gynecol. 2017. Oct;130(4):e210-e216. [DOI] [PubMed] [Google Scholar]
- 3.Brent RL. Protection of the gametes embryo/fetus from prenatal radiation exposure. Health Phys. 2015;108(2):242-274. [DOI] [PubMed] [Google Scholar]
- 4.Pampfer S, Streffer C. Prenatal death and malformations after irradiation of mouse zygotes with neutrons or X-rays. Teratology. 1988;37(6):599-607. [DOI] [PubMed] [Google Scholar]
- 5.Pampfer S, Streffer C. Increased chromo-some aberration levels in cells from mouse fetuses after zygote X-irradiation. Int J Radiat Biol. 1989;55(1):85-92. [DOI] [PubMed] [Google Scholar]
- 6.Tang FR, Loke WK, Khoo BC. Low-dose or low-dose-rate ionizing radiation-induced bioeffects in animal models. J Radiat Res. 2017;58(2):165-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brent RL. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Am J Obstet Gynecol. 2009;200(1):4-24. [DOI] [PubMed] [Google Scholar]
- 8.Jain C. ACOG Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstet Gynecol. 2019;133(1):186. [DOI] [PubMed] [Google Scholar]
- 9.U.S.N.R. Commission. Backgrounder on biological effects of radiation, updated March 2017. Web site. http://www.Nrc.Gov/Reading-Rm/Doc-Collections/Fact-Sheets/Bio-Effects-Radiation.Html. (n.d.).
- 10.Gomes M, Matias A, Macedo F. Risks to the fetus from diagnostic imaging during pregnancy: review and proposal of a clinical protocol. Pediatr Radiol. 2015;45(13):1916-1929. [DOI] [PubMed] [Google Scholar]
- 11.Smith-Bindman R, Miglioretti DL, Johnson E, Lee C, Feigelson HS, Flynn M, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. Jama. 2012. Jun 13;307(22):2400-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Republic of Turkey Ministry of Health, Health Statistics YearBook 2018. Web site. https//Dosyasb.Saglik.Gov.Tr/Eklenti/36164,Siy2018en2pdf.Pdf?0 (Accessed January 21, 2020.).
- 13.Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect. 1998;30(1):24-46. [PubMed] [Google Scholar]
- 14.Ratnapalan S, Bona N, Chandra K, Koren G. Physicians' perceptions of teratogenic risk associated with radiography and CT during early pregnancy. AJR Am J Roentgenol. 2004;182(5):1107-1109. [DOI] [PubMed] [Google Scholar]
- 15.Bentur Y, Horlatsch N, Koren G. Exposure to ionizing radiation during pregnancy: perception of teratogenic risk and outcome. Teratology. 1991;43(2):109-112. [DOI] [PubMed] [Google Scholar]
- 16.Sadigh G, Khan R, Kassin MT, Applegate KE. Radiation safety knowledge and perceptions among residents: a potential improvement opportunity for graduate medical education in the United States. Acad Radiol. 2014;21(7):869-878. [DOI] [PubMed] [Google Scholar]
- 17.Harper-Hanigan K, Ross G, Sims T, Trotter K, Turman JE Jr.. Women's Perspectives of Needs Surrounding Adverse Birth Outcomes: A Qualitative Assessment of the Neighborhood Impact of Adverse Birth Outcomes. Matern Child Health J. 2017;21(12):2219-2228. [DOI] [PubMed] [Google Scholar]
- 18.Ozbayrak M, Cavdar I, Seven M, Uslu L, Yeyin N, Tanyildizi H, et al. Determining and Managing Fetal Radiation Dose from Diagnostic Radiology Procedures in Turkey. Korean J Radiol. 2015;16(6):1276-1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guilbaud L, Beghin D, Dhombres F, Blondiaux E, Friszer S, Ducou Le Pointe H, et al. Pregnancy outcome after first trimester exposure to ionizing radiations. Eur J Obstet Gynecol Reprod Biol. 2019;232:18-21. [DOI] [PubMed] [Google Scholar]
- 20.Cohen-Kerem R, Nulman I, Abramow-Newerly M, Medina D, Maze R, Brent RL, et al. Diagnostic radiation in pregnancy: perception versus true risks. J Obstet Gynaecol Can. 2006;28(1):43-48. [DOI] [PubMed] [Google Scholar]
- 21.Fink D, Glick S. Misinformation among physicians about dangers of fetal x-ray exposure. Harefuah. 1993;124(11):717-739. [PubMed] [Google Scholar]
- 22.Hamilton BE, Martin JA, Osterman MJ, Driscoll AK, Rossen LM. Births: Provisional Data for 2017 Nvss Vital Statistics Rapid Release. Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. 2018. https://www.cdc.gov/nchs/data/vsrr/report004.pdf. [PubMed]
- 23.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Births: Final data for 2018, Natl. Vital Stat. Reports. 2019;68:1980-2018. [PubMed] [Google Scholar]
- 24.Bearak J, Popinchalk A, Ganatra B, Moller AB, Tunçalp Ö, Beavin C, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990-2019. Lancet Glob Health. 2020;8(9):e1152-e1161. [DOI] [PubMed] [Google Scholar]
- 25.Sedgh G, Bearak J, Singh S, Bankole A, Popinchalk A, Ganatra B, et al. Abortion incidence between 1990 and 2014: global, regional, d subregional levels and trends. Lancet. 2016;388(10041):258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kortsmit K, Jatlaoui TC, Mandel MG, Reeves JA, Oduyebo T, Petersen E, et al. Abortion Surveillance - United States, 2018. MMWR Surveill Summ. 2020;69(7):1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gissler M, Fronteira I, Jahn A, Karro H, Moreau C, Oliveira da Silva M, Olsen J, Savona-Ventura C, Temmerman M, Hemminki, et al. ; REPROSTAT group. Terminations of pregnancy in the European Union. BJOG. 2012;119(3):324-32. [DOI] [PubMed] [Google Scholar]
- 28.Walani SR. Global burden of preterm birth. Int J Gynecol Obstet 2020;150:31-33. [DOI] [PubMed] [Google Scholar]
- 29.Jacobsen L, Mellemgaard L. Anomalies of the eyes in descendants of women, irradiated with small X-ray doses during age of fertility. Acta Ophthalmol (Copenh). 1968;46(3):352-354. [DOI] [PubMed] [Google Scholar]
- 30.Bohnen NI, Ragozzino MW, Kurland LT. Brief communication: effects of diagnostic irradiation during pregnancy on head circumference at birth. Int J Neurosci. 1996;87(3-4):175-80. [DOI] [PubMed] [Google Scholar]
- 31.Hancock RL, Koren G, Einarson A, Ungar WJ. The effectiveness of Teratology Information Services (TIS). Reprod Toxicol. 2007;23(2):125-132. [DOI] [PubMed] [Google Scholar]
- 32.De Santis M, Straface G, Cavaliere AF, Cinque B, Carducci B, Caruso A. Teratological risk evaluation and prevention of voluntary abortion. Minerva Ginecol. 2006;58(2):91-9. [PubMed] [Google Scholar]
- 33.Buharalioglu CK, Acar S, Erol-Coskun H, Küçüksolak G, Karadas B, Kaya-Temiz T, et al. Pregnancy outcomes after maternal betahistine exposure: A case series. Reprod Toxicol. 2018;79:79-83. [DOI] [PubMed] [Google Scholar]
- 34.De Santis M, Cesari E, Ligato MS, Nobili E, Straface G, Cavaliere A, et al. Prenatal drug exposure and teratological risk: one-year experience of an Italian Teratology Information Service. Med Sci Monit. 2008;14(2):PH1-8. [PubMed] [Google Scholar]


