Abstract
Purpose:
Most published systematic reviews have focused on the use of virtual reality (VR)/augmented reality (AR) technology in ophthalmology as it relates to surgical training. To date, this is the first review that investigates the current state of VR/AR technology applied more broadly to the entire field of ophthalmology.
Methods:
PubMed, Embase, and CINAHL databases were searched systematically from January 2014 through December 1, 2020. Studies that discussed VR and/or AR as it relates to the field of ophthalmology and provided information on the technology used were considered. Abstracts, non–peer-reviewed literature, review articles, studies that reported only qualitative data, and studies without English translations were excluded.
Results:
A total of 77 studies were included in this review. Of these, 28 evaluated the use of VR/AR in ophthalmic surgical training/assessment and guidance, 7 in clinical training, 23 in diagnosis/screening, and 19 in treatment/therapy. 15 studies used AR, 61 used VR, and 1 used both. Most studies focused on the validity and usability of novel technologies.
Conclusions:
Ophthalmology is a field of medicine that is well suited for the use of VR/AR. However, further longitudinal studies examining the practical feasibility, efficacy, and safety of such novel technologies, the cost-effectiveness, and medical/legal considerations are still needed. We believe that time will indeed foster further technological advances and lead to widespread use of VR/AR in routine ophthalmic practice.
Keywords: augmented reality, ophthalmology, patient care, training, virtual reality
In 1962, Morton Heiling created what is considered to be the first true virtual reality (VR) system, the “sensorama”.1 This 3D film allowed users to feel as if they were riding a motorcycle through Brooklyn by engaging 4 of the 5 senses.2 Ivan Sutherland’s 1968 interactive head-mounted 3D display (HMD) took this one step further and created both an immersive and an interactive environment, what we define as a true modern-day VR experience.3
The goal of VR is to simulate a real environment using computer technology. Although there is no one unified definition of VR, three commonly agreed-upon components of all VR systems include immersion, sensory feedback, and interaction. Whereas VR has no real-life elements and is fully virtual, augmented reality (AR), on the other hand, supplements a pre-dominantly real environment with virtual elements. Meaning, AR can be defined as an interactive experience, overlaying virtual elements in the user’s perspective of the real world. One can better conceptualize their relationship using the reality-virtuality continuum coined by Milgram et al.4 As illustrated in Figure 1, this continuum displays the relationship between a completely real environment on one end and a completely virtual one (VR) on the other. Mixed reality is the space in between the 2 extremes.
FIGURE 1.
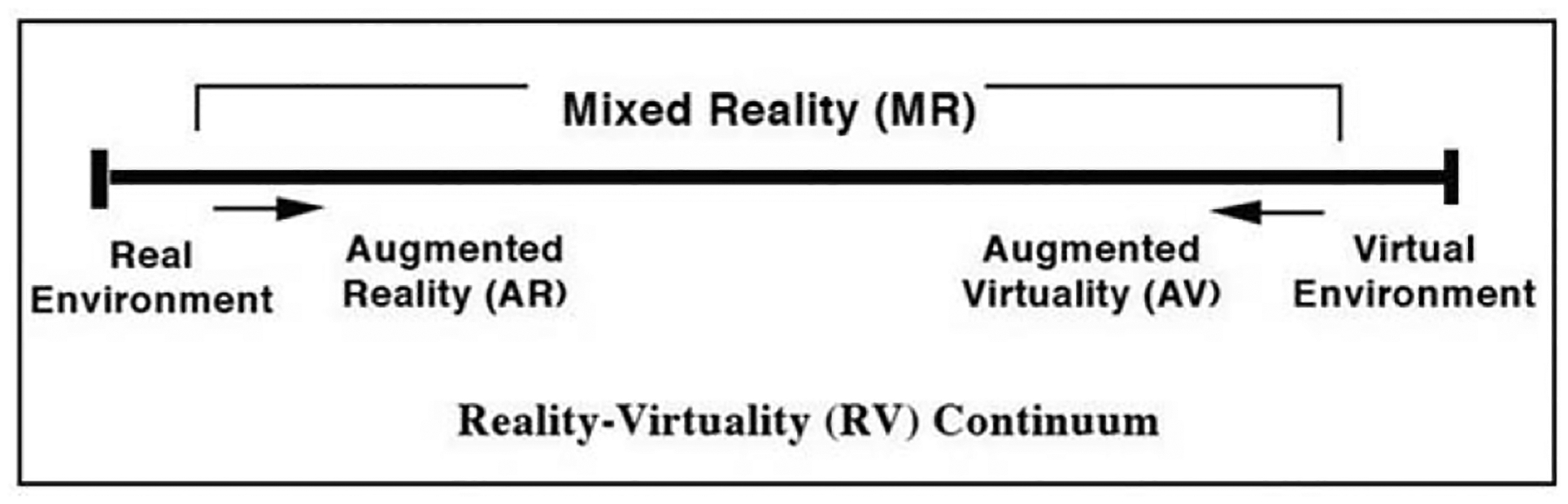
This continuum displays the relationship between a completely real environment on one end, and a completely virtual one (VR) on the other. Mixed reality is the space in between the 2 extremes.
Keeping in mind these definitions, ophthalmology is a field of medicine that lends itself well to the implementation of VR/AR technology. Not only is there a heavy emphasis on multimodal diagnostic testing that can be made efficient and portable with VR technology, but also VR simulators such as the Eyesi (VRmagic, Mannheim, Germany) and MicroVisTouch (ImmersiveTouch, Chicago, Illinois) are already commonly used training tools for the fine microsurgical procedures involved in most ophthalmic education programs.
To date, there have only been systematic reviews that examine VR/AR simulation–based training and surgical assessment in ophthalmology.5–7 In contrast, this is the first paper, to our knowledge, that provides a more comprehensive systematic review on the use of VR and AR in the broader field of ophthalmology. We will examine how VR/AR technology is used not only in ophthalmology for surgical training, assessment, and guidance, but also in the domains of clinical training, diagnosis, and treatment/therapy. We will conclude with a discussion on the limitations and the future trends of virtual environments associated with ophthalmology.
METHODS
Search Strategy
We performed a systematic review to identify the applications of VR and AR in ophthalmology according to the guidelines for reporting systematic reviews [Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)]. The protocol for our review was registered before the review started (PROSPERO: CRD42020216509). Literature searches were performed in the PubMed, Embase, and CINAHL databases from January 2014 through December 1, 2020, using keywords and MeSH terms for virtual reality, augmented reality, and ophthalmology. Language and publication limits were not applied. Full search details can be seen in appendix 1, http://links.lww.com/APJO/A97. Two reviewers screened 1190 abstracts, with a third reviewer available to resolve conflicts, after which 285 were chosen for full-text review. References of studies selected for full-text review were reviewed for possible inclusion. A total of 77 articles were subsequently chosen for inclusion (Fig. 2).
FIGURE 2.
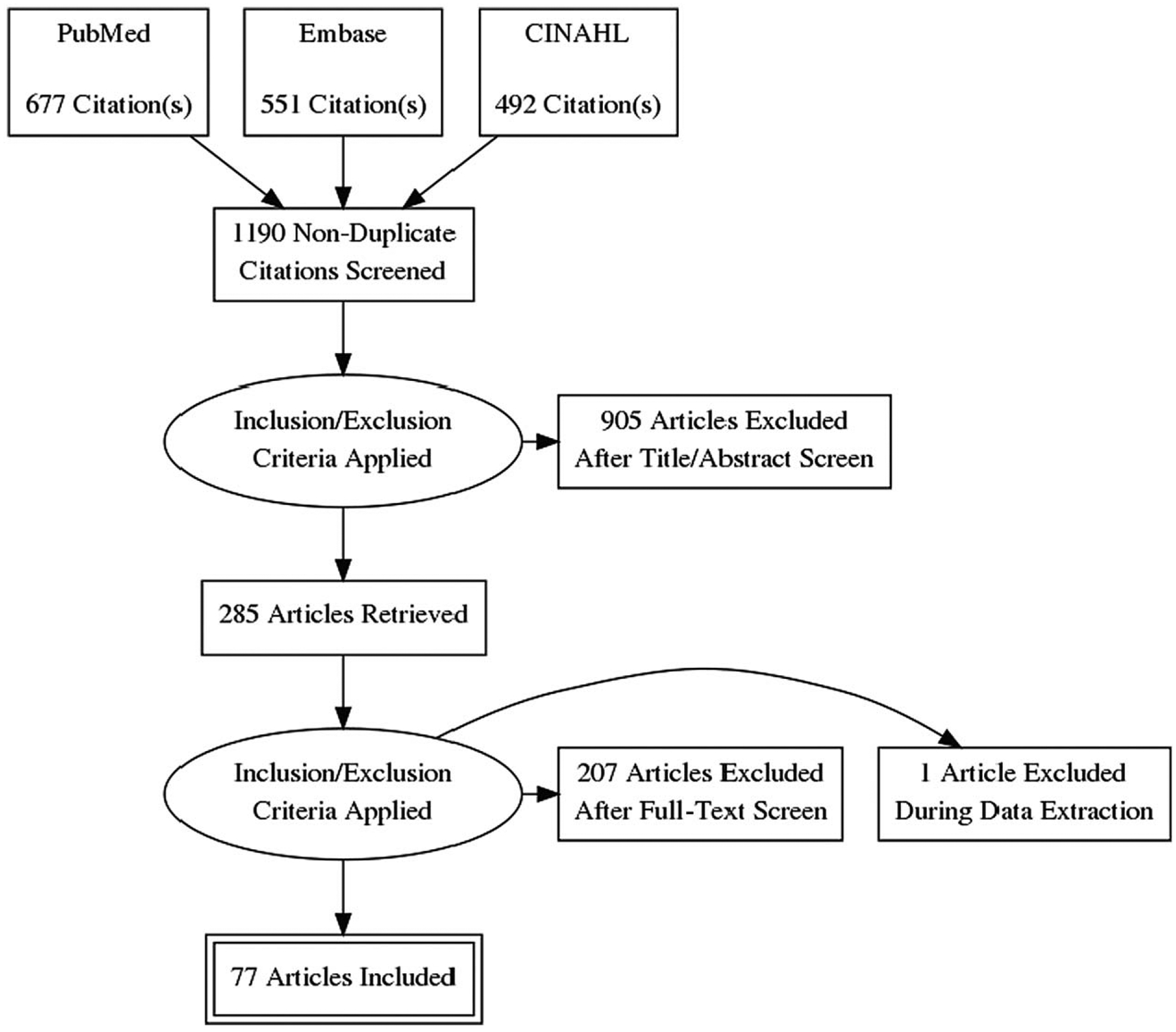
Search Strategy.
Eligibility Criteria
According to our eligibility criteria, we only included studies that had information available on the specific VR/AR technology used. The VR technology had to be immersive and interactive to be included. The technology was considered to be immersive if the device used a stereo/3D display, an HMD, or 2D screens in a manner that attempt to surround the participant. The technology was considered to be interactive if there was any potential for the participant to manipulate the virtual environment using a physical, device-based, or sensor-based interface. Letters to the editor and correspondences were excluded unless they reported on the applicability of VR/AR not found in other studies. Abstracts, non–peer-reviewed literature, review articles, qualitative studies, and studies with no English translation were excluded.
RESULTS
A total of 77 studies were included in this review, as shown in Figure 2.
Surgical Training/Assessment and Guidance
A total of 28 studies evaluated the use of VR and AR in surgical training/assessment and guidance as seen in Supplementary Digital Content, Table 1, http://links.lww.com/APJO/A93.
Augmented Reality
Two studies utilized AR for surgical training.8,9 Both demonstrated the feasibility of using their developed AR simulator with the HoloLens (Microsoft, US) to train vitreoretinal microsurgical skills.
Virtual Reality
Validation of Training Systems
Three studies investigated the validity of the Eyesi surgical simulator as a training and assessment tool for vitreoretinal surgery.10–12 Cissé et al10 studied the construct validity (whether a test actually measures what it claims to measure) of vitreoretinal modules on the Eyesi surgical simulator and showed that experienced surgeons achieved significantly higher median scores than novices in 4 modules (P values ranged from 0.01 to 0.04). Vergmann et al11 developed a vitreoretinal surgery training program on the Eyesi surgical simulator and found that in 4 (out of 6) vitreoretinal modules, the vitreoretinal surgeons had a better overall score than medical students (P < 0.01). Finally, Jaud et al12 designed a vitreoretinal surgery proficiency-based test on the Eyesi surgical simulator to establish a pass/fail score of 596.
In contrast, there were only 2 validiation studies that applied VR to cataract surgery training. One study designed a proficiency-based cataract surgery curriculum for novices13 and the other designed a test targeting experienced cataract surgeons.14
Skill Transfer
Several studies looked at whether skills learned on the Eyesi were transferable amongst surgical specialties, between training modules and ultimately to the operating room (OR).15–22 Thomsen et al15 found improved OR performance after Eyesi training for novice cataract surgeons (P = 0.008). Jacobsen et al16 similarly found a significant correlation between the Eyesi score and surgical performance (P = 0.003), and Ferris et al20 showed that the unadjusted rates of posterior capsule rupture before versus after Eyesi simulator training was 3.5% versus 2.6%. Roohipoor et al17 found a significant correlation between Eyesi scores of first-year ophthalmology residents and OR performance measured in the final year of residency (eg, forceps module P = 0.002 and navigation training module P = 0.013). At the very least, self-perceived difficulty scores on phacoemulsification procedures of residents without Eyesi training were significantly higher than reported difficulty scores of residents that did receive Eyesi training.18
Although simulator training can improve surgical performance, the converse has also been shown to be true. Sikder et al23 found that more experience in the OR improved MicroVisTouch simulator performance. Oflaz et al24 further showed a correlation between participants’ surgical experience and their scores on the capsulorhexis module on the Eyesi simulator. In reality, any form of practice, be it surgical or simulated, likely improves overall surgical skills. Deuchler et al25 even found that a warm-up session on the Eyesi simulator improved the average real surgery performance level of all surgeons, including surgeons with the most experience.
Subspecialty skill transfer is another topic of extensive study. Although some have found no difference in simulator performance between surgical subspecialists, McCannel et al26 showed that residents that trained on the Capsulorhexis Intensive Training Curriculum had a higher portion of vitreous loss not associated with an errant capsulorhexis but not an overall lower rate of vitreous loss. These results imply that microsurgical training may be highly task-specific.
Beyond Training
Ophthalmologists are taking advantage of the Eyesi as a surgical simulator in numerous other innovative manners—from testing out the efficacy of robot-assisted surgery27 to understanding the impact that learning styles have on surgical performances.28
For example, several studies used simulators to study the impact of dexterity on surgical performance.29,30 Vieira et al29 found that 2 sequential training evaluations using the simulator showed improvement of microsurgery dexterity (increase in median score by 104 points; P < 0.001). Gonzalez-Gonzalez et al30 showed improved dexterity and overall score performance in both dominant (P < 0.05) and non-dominant (P < 0.001) hands after a structured Eyesi training. Additionally, Although the simulator training program led to significantly faster times in both dominant (P < 0.001) and non-dominant (P < 0.02) hands, the learning curve was steeper in the non-dominant hand (P < 0.01). This may be the first study to document this finding.
Two studies even used the simulators to assess the effect of distraction on surgical performance.31,32 Mellum et al31 found that lower simulated surgical performance was associated with auditory distraction (P = 0.0012), fasting (P = 0.02), sleep interruption (P = 0.02), and sleep deprivation (P = 0.0006). McGowan et al32 gave surgeons a cognitive task to perform simultaneously while using a surgical simulator to mimic real-time OR distractions and found that this increased the time of surgery (P = 0.028), while having no effect on the surgical task score.
Surgical Guidance
Unlike in other surgical fields, relatively few studies utilized AR for surgical guidance.33,34 DeLisi et al33 found that surgeons who used their video augmentation system experienced faster endoscopic procedural times than surgeons who did not use AR (P = 0.020). Pan et al34 developed and implemented a deep learning framework to accurately detect corneal contours for accurate suturing in deep anterior lamellar keratoplasty procedures. Although the technology has not been implemented in most surgical suites quite yet, novel VR programs are even being developed to display 3D interactive optical coherence tomography images to guide in real-time surgical visualization and execution.35
Clinical Training
Seven studies evaluated the use of VR and AR in clinical training as seen in Supplementary Digital Content, Table 2, http://links.lww.com/APJO/A94.32–38
Slitlamp Examination
Augmented Reality
One study examined slitlamp education for optometry students using an AR slitlamp prototype.36 The average success rate of the prototype based on user performance for a comprehensive simulation procedure was 83.8%, and the average user satisfaction score was 80.4%. The authors concluded that the AR slitlamp was a feasible method of education and that there was positive user feedback from the students.
Direct Ophthalmoscopy
Virtual Reality
Although there were no studies that have implemented AR technology into direct ophthalmoscopy training or usage, 3 studies examined the application of VR for direct ophthalmoscopy examination.37–39
One study validated the use of the Eyesi Direct Ophthalmoscope,37 and 2 studies described the usability of a prototype VR technology as a direct ophthalmoscope teaching tool.38,39 Wilson et al38 developed a 3D smartphone application combined with a VR headset to simulate direct ophthalmoscopy. Based on subjective user experience, the app was highly rated in questionnaires that assessed perceived usefulness and ease of use. Similarly, Nguyen et al39 conducted a preliminary usability study of a VR direct ophthalmoscope using an HTC VIVE VR headset and controller. The System Usability Questionnaire (SUS) score for this tool was 75.6, where a score above 68 was considered above average. The authors conclude that this is a cost-effective, immersive, and engaging educational tool for direct ophthalmoscopy.
Indirect Ophthalmoscopy
Augmented Reality
Three studies looked at the application of AR as it relates to indirect ophthalmoscopy training.40–42 Two of these studies demonstrated construct validity of the Eyesi Indirect Ophthalmoscope.40,41 Chou et al40 reported that medical students were outperformed by ophthalmology and optometry trainees on the simulator on all difficulty levels, and Rai et al41 similarly reported that vitreoretinal fellows outperformed residents (P < 0.001). Both these studies reported significantly faster mean examination times on the simulator by more advanced trainees.
Simulator training was also found to be a better method than conventional indirect ophthalmoscopy training. Rai et al41 found that residents who had trained only on the simulator outperformed those who had completed only traditional teaching (13.95 vs 9.09, P = 0.006), as measured by an evaluation module on the simulator. Leitritz et al42 on the other hand measured performance using an ophthalmoscopy training score, which was calculated by evaluation of an optic disc drawing done by participants after their respective training. The median score of those trained with the simulator was significantly greater (P < 0.0033) than the conventional method.
Diagnosis/Screening
Twenty-three studies evaluated the use of VR and AR in diagnosis/screening as seen in Supplementary Digital Content, Table 3, http://links.lww.com/APJO/A95.44–66
Visual Assessment
Augmented Reality
Two studies evaluated the use of AR to better determine visual function.43,44
Ong et al43 developed an HMD visual acuity test using the Epson Moverio BT350 smart glasses. They found their prototype overestimated vision in patients with poorer visual acuities [VA worse than 0.30 logMAR (6/12)], in which sensitivity was 63.6% and specificity was 81.0%. The authors did note, however, that the portability and automated nature of the visual acuity test were advantages over the traditional methods. Another study used AR to gain insight into how ophthalmic diseases affect functional vision.44 The authors used AR to simulate everyday difficulties caused by glaucoma, and found that participants with AR-simulated visual field loss had increased difficulties with visual mobility (P < 0.001). Interestingly, participants made more head movements (P = 0.017) and more eye movements when inferior visual field loss was simulated (P = 0.002) versus superior visual field loss.
Virtual Reality
Seven studies examined the use of VR to better understand how vision loss can affect function.44–50
Five of the seven used VR to evaluate the effect of glaucoma on several aspects of daily living.44–48 For example, Goh et al45 evaluated the efficacy of a smartphone-based VR device to assess activity limitation in glaucoma using 3 tests (stationary, moving ball, driving). They found that only the stationary test and moving ball test showed reasonable measurement. Lam et al46 evaluated the application of VR to identify vision-related disability. They found that the overall VR disability score was associated with the National Eye Institute 25-item Visual Function Questionnaire Rasch score (R2 = 0.207, P < 0.001), indicating that VR simulation is a useful method of evaluating vision-related disability. Finally, Jones et al44 and Daga et al47 found that participants with visual field loss had increased difficulties with visual search (P < 0.001) and wayfinding (P = 0.001) respectively.
Two other studies evaluated the effect of visual field loss on functional vision using VR.49,50 Gopalakrishnan et al,49 for example, found that normal vision subjects performed better than low vision subjects in everyday tasks in a VR environment. They demonstrated that VR performance scores in patients with peripheral field loss (56.65) and central field loss (63.25) were lower (P < 0.001) than normal vision subjects (87). Qiu et al50 validated VR as a method to evaluate peripheral field loss patients’ ability to avoid collision with other pedestrians. They also tested whether high-power prisms improve pedestrian detection, and found that they improved detection rates and response times, and supported reasonable judgment among participants.
Three studies used VR for more specialized visual testing.51–53 Pujol et al51 studied a VR prototype as a method of testing spherical refraction, Versek et al52 described a Neuro-Optical Diagnostic VR system (the NeuroDotVR), and Tatiyosyan et al53 developed and validated an optokinetic nystagmus (OKN)–based VR device to test contrast sensitivity. Finally, 3 additional studies used VR environments to better understand the concepts of self-motion and oscillopsia.54–56
Visual Field Testing
Virtual Reality
Four studies used VR technology to diagnose visual field deficits in glaucoma patients.57–60 All 4 of these studies compared the VR to the Humphrey Visual Field Analyzer. Tsapakis et al57 found that there was a high correlation coefficient (r = 0.808, P < 0.0001) between their VR visual field device and the Humphrey perimeter visual field. Alawa et al58 similarly demonstrated that the VR visual field device had good agreement and high correlation coefficient (R2 = 0.77) with the Humphrey Zeiss FDT, and that there was no statistically significant difference between the 2 devices (Mann-Whitney test, P > 0.05). Razeghinejad et al59 found that the mean sensitivity of the VR device and the Humphrey Field Analyzer correlated significantly both in healthy participants (r = 0.5, P = 0.001) and in glaucoma patients (r = 0.8, P < 0.001). Mees et al,60 on the other hand, reported that although their VR visual field device was highly sensitive and specific in identifying glaucoma subjects (AUROC = 0.77–0.86), the visual field deficits did not match that of the Humphrey Field Analyzer. Only 38% of patients with an 18 dB or worse deficit seen on the Humphrey field Analyzer were picked up by the VR device.
Strabismus and Amblyopia
Virtual Reality
Three studies assessed the use of VR for determining ocular misalignment in strabismus patients.61–63 The first study was a case series that tested the efficacy and feasibility of measuring ocular misalignment using an Oculus Rift VR headset.61 They compared the performance of the VR-based technique to the traditional Lees screen test, and found good agreement between the pattern of ocular deviation obtained using the 2 methods. Another study utilized a FOVEVR headset to test for ocular deviation.62 They compared the VR-based test results to the strabismologist’s measurements of ocular deviation, and similarly found that the results were agreeable using the VR test (mean difference less than 0.7°). The third study testing children with intermittent exotropia on a VR-based block building task, found larger horizontal (P < 0.001), vertical (P = 0.039), and 3D distance disparities (P < 0.001) compared to age-matched normal controls.63
Two studies examined the use of VR in the evaluation of amblyopia.64,65 Panachakel et al64 validated a new VR-based approach to quantify the severity of amblyopia by measuring suppression asymmetry during dichoptic image recognition tasks. Martin et al65 implemented a VR-based test for binocular imbalance. They found that this test was correlated with interocular acuity difference (r = 0.575, P < 0.0001), stereoacuity (r = 0.675, P < 0.0001), and with the Worth 4-dots test (r = 0.538, P < 0.0001).
Treatment/Therapy
Nineteen studies evaluated the use of VR and AR in treatment/therapy as seen in Supplementary Digital Content, Table 4, http://links.lww.com/APJO/A96.67–85
Low Vision Services
Augmented Reality
Six studies evaluated the use of AR-based treatment of patients with low vision and/or loss of visual field.66–71 All these studies examined ways in which AR can improve patients’ functional vision.
Huang et al66 utilized the Microsoft HoloLens to provide indoor wayfinding assistance for individuals with reduced vision, specifically through the AR device in identifying and enhancing signs and room numbers for the patients. They calculated a distance ratio for each participant and found that the mean distance ratio was significantly reduced for participants that used the AR device versus those that did not (0.36 vs 0.50, P < 0.001), indicating that participants in the AR group took more direct routes than those not using the AR device. The AR group also reported the device helpful for wayfinding (96% of participants preferred the AR trial for ease, 83% for comfort, and 92% for confidence). Hwang et al67 similarly used an AR device, the Google Glass, to enhance real-world information by overlaying edge information on the wearer’s real-world view. The authors found that all the subjects had significantly improved contrast sensitivity, which could potentially help them navigate better real-world scenarios. The Google Glass was also found to significantly improve visual field in a case report performed by Trese et al.68 Ho et al69 evaluated the use of AR glasses to simulate reduced acuity, contrast, and visual field to investigate the utility of prosthetic central vision. They found that reading speed decreased with increasing pixel size and with a reduced field of view (78°–12°). In the face recognition task, participants identified faces at over 75% of accuracy with 100 lm pixels and only 2 grayscale levels. In addition, both Sayed et al70 and Kinateder et al71 reported improved object recognition when participants used their respective AR device (P < 0.001 for both).
Virtual Reality
Virtual reality has also been used to improve functional vision in people with reduced vision. Because VR does not incorporate the real environment, it cannot be used as a tool to improve functional vision in a real-world setting as with AR. Rather it can be used for functional vision training,72,73 remapping,74–76 and magnifying images.77 Virtual reality has also been used to simulate treatments to low vision, specifically to elucidate the potential utility of retinal prosthesis.78–80
Amblyopia/Strabismus
Virtual Reality
Three studies were found that examined VR-based treatment of amblyopia.81–83 Herbison et al81 specifically looked at a VR-based therapy called the Interactive Binocular Treatment (I-BiT) system, which is the first VR-based computer system that employs dynamic stimuli with preferential stimulation of an amblyopic eye. They noted an average VA improvement of 0.07 logMAR for all their participants 6 weeks after treatment (P < 0.001). A VR-based amblyopia therapy has the advantage that it does not rely on visual occlusion, as is the current clinical standard in children.
Two studies looked at the use of the Oculus Rift headset to provide dichoptic visual training to anisometropic amblyopic adults.82,83 Both reported positive results, with visual acuity improving on average in the participants after the VR-based treatment. Ziak et al82 found that mean best-corrected visual acuity (BCVA) in the amblyopic eye improved significantly from a logMAR value of 0.58 ± 0.35 before VR training to 0.43 ± 0.38 post-training (P < 0.01). Halicka et al83 also found an improvement in BCVA after VR training, with an observed improvement of 0.1 BCVA from 0.48 to 0.58 Sloan table (P < 0.05).
A final study by Boon et al84 looked at VR as a treatment of convergence insufficiency. A VR intervention showed significant improvement in near point of convergence (F1,16 = 38.32, P < 0.0001), near positive fusional reserve break, and recovery (F1,16 = 21.94, P < 0.0001). Importantly, they found that not only did VR therapy improve convergence insufficiency, but it improved participants’ compliance to treatment (82% compliance to the VR game, 51% compliance to conventional treatment).
Limitations and Safety VR/AR
There are several limitations to the use of VR/AR. The weight and comfort of the VR/AR systems are one concern for its universal adoption. This is especially important when thinking of adopting HMD devices into the OR, or as a treatment/diagnostic method for patients. The Microsoft Hololens 2 AR headset weighs 1.248 pounds, and the Oculus Rift S VR headset weighs 1.1 pounds. Use for prolonged periods of time may put a strain on the neck and back. These devices may not be feasible for use by surgeons or patients who are injury-prone or for particularly long surgeries. Additional battery packs will also add bulk to the apparatus. Luckily, technological advancement almost always results in the reduction of the weight and size of hardware over time, and so one can predict that cumbersome and heavy VR/AR devices are likely not a long-term concern.
In addition, cybersickness (CS), which is a constellation of motion sickness–like symptoms,85 has been well documented as it relates to the virtual environment. A review done by Weech et al86 discussed multiple factors that are thought to contribute to CS including visual-vestibular mismatch and display characteristics such as low frame rate and higher field-of-view. Although the majority of the time CS symptoms stop upon termination of the exposure, there are reported long-lasting effects in some individuals.87 However, it should be noted that studies that applied VR/AR technologies addressed both the risk of motion sickness and the subsequent risk of falls and did not report any adverse outcomes.88 Further research is needed to elucidate the real risk of CS and sources of these motion sickness–like symptoms so that VR/AR developers can find ways to mitigate this.
Furthermore, long-term safety concerns need to be addressed particularly in children, as the product safety warnings on VR headsets ban their use with children under the age of 13. As young children are in a “critical period in visual development,” there is fear that these devices may affect future visual function. However, the evidence behind these claims is mixed. Tychsen et al89 studied the effects of 3D immersive HMD on the visuomotor function of 50 children after their exposure to two 30-minute VR gaming sessions and found no deleterious effects. Other studies reported transient refractive error, but no long-term effects on the vision of children or adolescents.90 Critics have also worried about the effects that prolonged screen time may have on the ocular surface or on myopia progression. In reality, a few studies have actually found increased lipid layer thickness, tear film stability, and increased choroidal thickening with VR headset wear in the general population, arguing against these concerns.91,92 Despite these findings, there is a need for more long-term standardized studies to be done before anything can be concluded on the ocular effects of VR/AR technology.
Future Scope of VR/AR in Ophthalmology
Adopting VR/AR into clinical practice and training poses unique challenges that must be addressed. Ultimately, lower costs, improved hardware, and validated studies are needed for this technology to be adopted and utilized more widely in ophthalmology programs. The fidelity and accuracy of the VR/AR technology is fundamental due to the high stakes and high precision nature of ophthalmology. Similarly, cost-effectiveness must be examined before implementing new technology in medicine. More research is needed in validity and analyzing cost-effectiveness to effectively incorporate reality technology into the field. Although several VR/AR projects remain at a preliminary stage of research in ophthalmology, rapid technological advancements in hardware and the integration of VR into the computer gaming industry, have generated a new impulse in reality technology research and published studies over recent years.93 Finally, to be accepted as more than a niche gimmick or a current transient fad, well-designed studies need to be highlighted at educational conferences and meetings. There needs to be more widespread dissemination of study results leading to greater awareness and better education across ophthalmology programs as to the use of VR/AR technologies.
VR/AR and COVID-19
During COVID-19, the impetus to adopt VR and AR into ophthalmology is now stronger than ever.94 The COVID-19 pandemic has momentously changed the landscape in which we practice medicine. As we adapt to what is the new “norm” surrounding social distancing and interpersonal contact, innovative ways to practice medicine are in high demand. As such, telemedicine and virtual visits have rightly spiked since the beginning of the pandemic. Kaur et al95 discuss the importance of the use of 3D heads-up displays in ophthalmic surgery in the COVID-19 era. The study points to the fact that this technology allows the adequate interpersonal distance between the surgeon and the patient. They additionally address the concern of aerosol production during phacoemulsification, and the potential hampered vision of the surgeon using face shields or goggles as a protective measure. The 3D heads-up displays may not require the use of these additional goggles or shields as the adequate distance is maintained from the surgical field. Likewise, the smaller and more compact of VR headsets makes them portable, transferable, and more hygienic. This applies to VR visual field devices as well. Finally, VR/AR devices are currently being studied for the feasibility of use by patients at home and during virtual visits.96 If future research validates their use in such a manner, they could be invaluable for the duration of the pandemic and in the future.
Limitations
Although we adhered closely to the PRISMA guidelines for systematic reviews, some limitations may affect the validity of our findings. Our review is susceptible to publication bias as grey literature was not included in this review. There could be VR/AR devices used in ophthalmology that did not publish results and therefore were excluded from our review (such as Eyesi Slit Lamp studies). Although comprehensive search terms were applied, reports using different terminology could have been missed. Similarly, studies published in technology journals would have been missed as we focused on health care databases for this review. Because of the heterogeneity in the methodologies and outcomes of the studies, quantitative analysis was not feasible for this review. Finally, as our review was limited to studies evaluating immersive and interactive VR/AR technology, articles regarding the cost-effectiveness, and legal/ethical and regulatory considerations of such novel techniques, were not in the scope of this article.
CONCLUSIONS
This systematic review is the first to comprehensively report on the application of VR and AR in the field of ophthalmology. With its dependence on imaging, highly precise microsurgical procedures, and tradition of being on the cutting edge of new technology, ophthalmology has seen the widespread introduction of VR and AR. As reality technologies improve in hardware and software, and approach their ultimate goal of making the user truly believe that the virtual is real, we are optimistic that ophthalmology will greatly benefit from the widespread adoption of this technology in practice.
Supplementary Material
Acknowledgments
Supported by Research to Prevent Blindness, New York, New York.
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Regrebsubla N Determinants of Diffusion of Virtual Reality [Diploma Thesis]. GRIN: Chair of Technology and Management, Technical University of Berlin; 2015. [Google Scholar]
- 2.Boas YAGV Overview of virtual reality technologies. In: Proceedings of the Interactive Multimedia Conference, Bogotá, Colombia. 2013;2013. [Google Scholar]
- 3.Earnshaw RA. Virtual Reality Systems. Academic press; 1993, 2014. [Google Scholar]
- 4.Milgram P, Takemura H, Utsumi A, et al. Augmented reality: a class of displays on the reality-virtuality continuum. Paper presented at: Telemanipulator and telepresence technologies; 1995. [Google Scholar]
- 5.Thomsen ASS, Subhi Y, Kiilgaard JF, et al. Update on simulation-based surgical training and assessment in ophthalmology: a systematic review. Ophthalmology. 2015;122:1111–1130. [DOI] [PubMed] [Google Scholar]
- 6.Lee R, Raison N, Lau WY, et al. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye. 2020;34:1737–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rasmussen RC, Grauslund J, Vergmann AS. Simulation training in vitreoretinal surgery: a systematic review. BMC Ophthalmol. 2019;19:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ropelato S, Menozzi M, Michel D, et al. Augmented reality microsurgery: a tool for training micromanipulations in ophthalmic surgery using augmented reality. Simul Healthcare. 2020;15:122–127. [DOI] [PubMed] [Google Scholar]
- 9.Menozzi M, Ropelat S, Köfler J, et al. Development of ophthalmic microsurgery training in augmented reality. Klinische Monatsbl fAugenheilk. 2020;237:388–391. [DOI] [PubMed] [Google Scholar]
- 10.Cissé C, Angioi K, Luc A, et al. EYESI surgical simulator: validity evidence of the vitreoretinal modules. Acta Ophthalmol. 2019;97:e277–e282. [DOI] [PubMed] [Google Scholar]
- 11.Vergmann AS, Vestergaard AH, Grauslund J. Virtual vitreoretinal surgery: validation of a training programme. Acta Ophthalmol. 2017;95:60–65. [DOI] [PubMed] [Google Scholar]
- 12.Jaud C, Salleron J, Cisse C, et al. EyeSi Surgical Simulator: validation of a proficiency-based test for assessment of vitreoretinal surgical skills. Acta ophthalmologica. 2020. Published online October 3, 2020. doi: 10.1111/aos.14628. [DOI] [PubMed] [Google Scholar]
- 13.Spiteri A, Aggarwal R, Kersey T, et al. Development of a virtual reality training curriculum for phacoemulsification surgery. Eye. 2014;28:78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forslund Jacobsen M, Konge L, la Cour M, et al. Simulation of advanced cataract surgery–validation of a newly developed test. Acta Ophthalmol. 2020;98:687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomsen ASS, Bach-Holm D, Kjærbo H, et al. Operating room performance improves after proficiency-based virtual reality cataract surgery training. Ophthalmology. 2017;124:524–531. [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen MF, Konge L, Bach-Holm D, et al. Correlation of virtual reality performance with real-life cataract surgery performance. J Cataract Refract Surg. 2019;45:1246–1251. [DOI] [PubMed] [Google Scholar]
- 17.Roohipoor R, Yaseri M, Teymourpour A, et al. Early performance on an eye surgery simulator predicts subsequent resident surgical performance. J Surg Educ. 2017;74:1105–1115. [DOI] [PubMed] [Google Scholar]
- 18.Ng DSC, Sun Z, Young AL, et al. Impact of virtual reality simulation on learning barriers of phacoemulsification perceived by residents. Clin Ophthalmol (Auckland NZ). 2018;12:885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomsen ASS, Kiilgaard JF, Kjærbo H, et al. Simulation-based certification for cataract surgery. Acta Ophthalmol. 2015;93:416–421. [DOI] [PubMed] [Google Scholar]
- 20.Ferris JD, Donachie PH, Johnston RL, et al. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 6. The impact of EyeSi virtual reality training on complications rates of cataract surgery performed by first and second-year trainees. Br J Ophthalmol. 2020;104:324–329. [DOI] [PubMed] [Google Scholar]
- 21.Thomsen ASS, Kiilgaard JF, la Cour M, et al. Is there inter-procedural transfer of skills in intraocular surgery? A randomized controlled trial. Acta Ophthalmol. 2017;95:845–851. [DOI] [PubMed] [Google Scholar]
- 22.Thomsen ASS, Smith P, Subhi Y, et al. High correlation between performance on a virtual-reality simulator and real-life cataract surgery. Acta Ophthalmol. 2017;95:307–311. [DOI] [PubMed] [Google Scholar]
- 23.Sikder S, Luo J, Banerjee PP, et al. The use of a virtual reality surgical simulator for cataract surgical skill assessment with 6 months of intervening operating room experience. Clin Ophthalmol (Auckland NZ). 2015;9:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oflaz AB, Köktekir BE, Okudan S. Does cataract surgery simulation correlate with real-life experience? Turkish J Ophthalmol. 2018;48:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deuchler S, Wagner C, Singh P, et al. Clinical efficacy of simulated vitreoretinal surgery to prepare surgeons for the upcoming intervention in the operating room. PloS One. 2016;11:e0150690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCannel CA. Continuous curvilinear capsulorhexis training and non-rhexis related vitreous loss: the specificity of virtual reality simulator surgical training (an American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc. 2017;115:T2. [PMC free article] [PubMed] [Google Scholar]
- 27.Forslund Jacobsen M, Konge L, Alberti M, et al. Robot-assisted vitreoretinal surgery improves surgical accuracy compared with manual surgery: a randomized trial in a simulated setting. Retina (Philadelphia Pa). 2020;40:2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Modi N, Williams O, Swampillai AJ, et al. Learning styles and the prospective ophthalmologist. Med Teacher. 2015;37:344–347. [DOI] [PubMed] [Google Scholar]
- 29.Vieira IV, Sakaya BN, Soares LVdB, et al. Use of virtual reality equipment to assess the manual dexterity of applicants for ophthalmology residency. Arquivos Brasileiros Oftalmol. 2020;83:294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gonzalez-Gonzalez LA, Payal AR, Gonzalez-Monroy JE, et al. Ophthalmic surgical simulation in training dexterity in dominant and nondominant hands: results from a pilot study. Journal of Surg Educ. 2016;73:699–708. [DOI] [PubMed] [Google Scholar]
- 31.Mellum ML, Vestergaard AH, Grauslund J, et al. Virtual vitreoretinal surgery: effect of distracting factors on surgical performance in medical students. Acta Ophthalmol. 2020;98:378–383. [DOI] [PubMed] [Google Scholar]
- 32.McGowan G, Jawaheer L, Young D, et al. QUIET PLEASE! Effect of distraction on simulated posterior segment surgical performance. Graefes Arch Clin Exp Ophthalmol. 2018;256:519–523. [DOI] [PubMed] [Google Scholar]
- 33.DeLisi MP, Mawn LA, Galloway Jr. Image-guided transorbital procedures with endoscopic video augmentation. Med Phys. 2014;41:091901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan J, Liu W, Ge P, et al. Real-time segmentation and tracking of excised corneal contour by deep neural networks for DALK surgical navigation. Computer Methods Prog Biomed. 2020;197:105679. [DOI] [PubMed] [Google Scholar]
- 35.Maloca PM, de Carvalho JER, Heeren T, et al. High-performance virtual reality volume rendering of original optical coherence tomography point-cloud data enhanced with real-time ray casting. Transl Vision Sci Technol. 2018;7:2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wei L, Najdovski Z, Nahavandi S, et al. Towards a haptically enabled optometry training simulator. Network Model Anal iHealth Inform Bioinform. 2014;3:1–8. [Google Scholar]
- 37.Borgersen NJ, Skou Thomsen AS, Konge L, et al. Virtual reality-based proficiency test in direct ophthalmoscopy. Acta Ophthalmol. 2018;96:e259–e261. [DOI] [PubMed] [Google Scholar]
- 38.Wilson AS, O’Connor J, Taylor L, et al. A 3D virtual reality ophthalmoscopy trainer. Clin Teacher. 2017;14:427–431. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen M, Quevedo-Uribe A, Kapralos B, et al. An experimental training support framework for eye fundus examination skill development. Computer Methods Biomech Biomed Eng: Imag Visual. 2019;7:26–36. [Google Scholar]
- 40.Chou J, Kosowsky T, Payal AR, et al. Construct and face validity of the Eyesi indirect ophthalmoscope simulator. Retina (Philadelphia Pa). 2017;37:1967–1976. [DOI] [PubMed] [Google Scholar]
- 41.Rai AS, Rai AS, Mavrikakis E, et al. Teaching binocular indirect ophthalmoscopy to novice residents using an augmented reality simulator. Canad J Ophthalmol. 2017;52:430–434. [DOI] [PubMed] [Google Scholar]
- 42.Leitritz MA, Ziemssen F, Suesskind D, et al. Critical evaluation of the usability of augmented reality ophthalmoscopy for the training of inexperienced examiners. Retina (Philadelphia Pa). 2014;34:785–791. [DOI] [PubMed] [Google Scholar]
- 43.Ong SC, Pek LCI, Cheng TLC, et al. A novel automated visual acuity test using a portable head-mounted display. Optometry Vision Sci. 2020;97:591–597. [DOI] [PubMed] [Google Scholar]
- 44.Jones PR, Somoskeöy T, Chow-Wing-Bom H, et al. Seeing other perspectives: evaluating the use of virtual and augmented reality to simulate visual impairments (OpenVisSim). NPJ Digital Med. 2020;3:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goh RL, Kong YXG, McAlinden C, Liu J, et al. Objective assessment of activity limitation in glaucoma with smartphone virtual reality goggles: a pilot study. TranslVision Sci Technol. 2018;7:10–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lam AK, To E, Weinreb RN, et al. Use of virtual reality simulation to identify vision-related disability in patients with glaucoma. JAMA Ophthalmol. 2020;138:490–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daga FB, Macagno E, Stevenson C, et al. Wayfinding and glaucoma: a virtual reality experiment. Invest Ophthalmol Visual Sci. 2017;58:3343–3349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Diniz-Filho A, Boer ER, Gracitelli C, et al. Visually Induced Postural Reactivity in Glaucoma. Investig Ophthalmol Visual Sci. 2015;56:4765–14765. [Google Scholar]
- 49.Gopalakrishnan S, Jacob CES, Kumar M, et al. Comparison of visual parameters between normal individuals and people with low vision in a virtual environment. Cyberpsychol Behav Soc Network. 2020;23:171–178. [DOI] [PubMed] [Google Scholar]
- 50.Qiu C, Jung JH, Tuccar-Burak M, et al. Measuring pedestrian collision detection with peripheral field loss and the impact of peripheral prisms. Transl Vision Sci Technol. 2018;7:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pujol J, Ondategui-Parra JC, Badiella L, et al. Spherical subjective refraction with a novel 3D virtual reality-based system. J Optometry. 2017;10:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Versek C, Rissmiller A, Tran A, et al. Portable system for neuro-optical diagnostics using virtual reality display. Military Med. 2019;184(supp 1): 584–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tatiyosyan SA, Rifai K, Wahl S. Standalone cooperation-free OKN-based low vision contrast sensitivity estimation in VR-a pilot study. Restor Neurol Neurosci. 2020;38:119–129. [DOI] [PubMed] [Google Scholar]
- 54.Randall D, Fox SL, Fenner JW, et al. Using VR to investigate the relationship between visual acuity and severity of simulated oscillopsia. Curr Eye Res. 2020;45:1611–1618. [DOI] [PubMed] [Google Scholar]
- 55.Brin TA, Tarita-Nistor L, González EG, et al. Vection responses in patients with early glaucoma. J oGlaucoma. 2019;28:68–74. [DOI] [PubMed] [Google Scholar]
- 56.Kim J, Chung CY, Nakamura S, et al. The Oculus Rift: a cost-effective tool for studying visual-vestibular interactions in self-motion perception. Front Psychol. 2015;6:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tsapakis S, Papaconstantinou D, Diagourtas A, et al. Visual field examination method using virtual reality glasses compared with the Humphrey perimeter. Clin Ophthalmol (Auckland NZ). 2017;11:1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alawa KA, Nolan RP, Han E, et al. Low-cost, smartphone-based frequency doubling technology visual field testing using a head-mounted display. Br J Ophthalmol. 2021;105:440–444. [DOI] [PubMed] [Google Scholar]
- 59.Razeghinejad R, Gonzalez-Garcia A, Myers JS, et al. Preliminary report on a novel virtual reality perimeter compared with standard automated perimetry. J Glaucoma. 2021;30:17–23. [DOI] [PubMed] [Google Scholar]
- 60.Mees L, Upadhyaya S, Kumar P, et al. Validation of a head-mounted virtual reality visual field screening device. J Glaucoma. 2020;29:86–91. [DOI] [PubMed] [Google Scholar]
- 61.Nesaratnam N, Thomas P, Vivian A. Stepping into the virtual unknown: feasibility study of a virtual reality-based test of ocular misalignment. Eye. 2017;31:1503–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miao Y, Jeon JY, Park G, et al. Virtual reality-based measurement of ocular deviation in strabismus. Computer Methods Progr Biomed. 2020;185:105132. [DOI] [PubMed] [Google Scholar]
- 63.Chung SA, Choi J, Jeong S, et al. Block-building performance test using a virtual reality head-mounted display in children with intermittent exotropia. Eye. 2021;35:1758–1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Panachakel JT, Ramakrishnan AG, Manjunath KP. VR glasses based measurement of responses to dichoptic stimuli: a potential tool for quantifying amblyopia? Paper presented at: 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC); 2020. [DOI] [PubMed] [Google Scholar]
- 65.Martín S, Portela JA, Ding J, et al. Evaluation of a Virtual Reality implementation of a binocular imbalance test. PloS One. 2020;15:e0238047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huang J, Kinateder M, Dunn MJ, et al. An augmented reality sign-reading assistant for users with reduced vision. PloS One. 2019;14:e0210630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hwang AD, Peli E. An augmented-reality edge enhancement application for Google Glass. Optometry Vision Sci. 2014;91:1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Trese MG, Khan NW, Branham K, et al. Expansion of severely constricted visual field using Google Glass. Ophthal Surg Lasers Imaging Retina. 2016;47:486–489. [DOI] [PubMed] [Google Scholar]
- 69.Ho E, Boffa J, Palanker D. Performance of complex visual tasks using simulated prosthetic vision via augmented-reality glasses. J Vision. 2019;19:22–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sayed AM, Shousha MA, Baharul Islam M, et al. Mobility improvement of patients with peripheral visual field losses using novel see-through digital spectacles. Plos One. 2020;15:e0240509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kinateder M, Gualtieri J, Dunn MJ, et al. Using an augmented reality device as a distance-based vision aid—promise and limitations. Optometry Vision Sci. 2018;95:727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bowman EL, Liu L. Individuals with severely impaired vision can learn useful orientation and mobility skills in virtual streets and can use them to improve real street safety. PLoS One. 2017;12:e0176534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jung JH, Castle R, Kurukuti NM, et al. Field expansion with multiplexing prism glasses improves pedestrian detection for acquired monocular vision. Transl Vision Sci Technol. 2020;9:35–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gupta A, Mesik J, Engel SA, et al. Beneficial effects of spatial remapping for reading with simulated central field loss. Invest Ophthalmol Visual Sci. 2018;59:1105–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sayed AM, Kashem R, Abdel-Mottaleb M, et al. Toward improving the mobility of patients with peripheral visual field defects with novel digital Spectacles. Am Jo Ophthalmol. 2020;210:136–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sayed AM, Abdel-Mottaleb M, Kashem R, et al. Expansion of peripheral visual field with novel virtual reality digital spectacles. Ame J Ophthalmol. 2020;210:125–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Deemer AD, Swenor BK, Fujiwara K, et al. Preliminary evaluation of two digital image processing strategies for head-mounted magnification for low vision patients. Transl Vision Sci Technol. 2019;8:23–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zapf MPH, Boon MY, Matteucci PB, et al. Towards an assistive peripheral visual prosthesis for long-term treatment of retinitis pigmentosa: evaluating mobility performance in immersive simulations. J Neural Eng. 2015;12:036001. [DOI] [PubMed] [Google Scholar]
- 79.Endo T, Hozumi K, Hirota M, et al. The influence of visual field position induced by a retinal prosthesis simulator on mobility. Graefes Arch Clin Exp Ophthalmol. 2019;257:1765–1770. [DOI] [PubMed] [Google Scholar]
- 80.Zapf MPH, Boon MY, Lovell NH, et al. Assistive peripheral prosthetic vision aids perception and mobility in outdoor environments: a virtual-reality simulation study. Paper presented at: 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); 2015. [DOI] [PubMed] [Google Scholar]
- 81.Herbison N, MacKeith D, Vivian A, et al. Randomised controlled trial of video clips and interactive games to improve vision in children with amblyopia using the I-BiT system. Br J Ophthalmol. 2016;100:1511–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Žiak P, Holm A, Halička J, et al. Amblyopia treatment of adults with dichoptic training using the virtual reality oculus rift head mounted display: preliminary results. BMC Ophthalmol. 2017;17:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Halička J, Sahatqija E, Krasňanský M, et al. Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia. Ceska Slovenska Oftalmol. 2020;76:24–28. [DOI] [PubMed] [Google Scholar]
- 84.Boon MY, Asper LJ, Chik P, et al. Treatment and compliance with virtual reality and anaglyph-based training programs for convergence insufficiency. Clin Exp Optometry. 2020;103:870–876. [DOI] [PubMed] [Google Scholar]
- 85.Stanney KM, Kennedy RS, Drexler JM. Cybersickness is not simulator sickness. In: Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 1997;41:1138–1142. [Google Scholar]
- 86.Weech S, Kenny S, Barnett-Cowan M. Presence and cybersickness in virtual reality are negatively related: a review. Front Psychol. 2019;10:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Weech S, Varghese JP, Barnett-Cowan M. Estimating the sensorimotor components of cybersickness. J Neurophysiol. 2018;120:2201–2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gunasekeran DV, Low R, Gunasekeran R, et al. Population eye health education using augmented reality and virtual reality: scalable tools during and beyond COVID-19. BMJ Innovations. 2021;7:278–283. [DOI] [PubMed] [Google Scholar]
- 89.Tychsen L, Foeller P. Effects of immersive virtual reality headset viewing on young children: visuomotor function, postural stability, and motion sickness. Am J Ophthalmol. 2020;209:151–159. [DOI] [PubMed] [Google Scholar]
- 90.Ha SG, Na KH, Kweon IJ, et al. Effects of head-mounted display on the oculomotor system and refractive error in normal adolescents. J Pediatr Ophthalmol Strabismus. 2016;53:238–245. [DOI] [PubMed] [Google Scholar]
- 91.Turnbull PR, Wong J, Feng J, et al. Effect of virtual reality headset wear on the tear film: a randomised crossover study. Contact Lens Anterior Eye. 2019;42:640–645. [DOI] [PubMed] [Google Scholar]
- 92.Turnbull PR, Phillips JR. Ocular effects of virtual reality headset wear in young adults. Scientific Rep. 2017;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Valmaggia LR, Latif L, Kempton MJ, et al. Virtual reality in the psychological treatment for mental health problems: a systematic review of recent evidence. Psychiatry Res. 2016;236:189–195. [DOI] [PubMed] [Google Scholar]
- 94.Hong Y-R, Lawrence J, Williams Jr. Population-level interest and telehealth capacity of US hospitals in response to COVID-19: cross-sectional analysis of Google search and national hospital survey data. JMIR Public Health Surveill. 2020;6:e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kaur M, Titiyal JS. Three-dimensional heads up display in anterior segment surgeries-Expanding frontiers in the COVID-19 era. Indian J Ophthalmol. 2020;68:2338–2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tsapakis S, Papaconstantinou D, Diagourtas A, et al. Home-based visual field test for glaucoma screening comparison with Humphrey perimeter. Clin Ophthalmol (Auckland NZ). 2018;12:2597–2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


