Abstract
Objective:
We estimated the prevalence of diagnosed eating disorders, overall and by select demographics, among commercially-insured individuals identified as transgender in a national claims database.
Method:
From the 2018 IBM® MarketScan® Commercial Database, there were 10,415 people identifiable as transgender based on International Classification of Disease (ICD-10) codes and procedure codes, specific to gender affirming care, from inpatient and outpatient claims. Eating disorders were identified from ICD-10 codes and included anorexia nervosa, bulimia nervosa, binge eating disorder, eating disorder not otherwise specified, avoidant restrictive feeding and intake disorder, and other specified feeding and eating disorders. We estimated prevalence of specific eating disorders diagnoses by select patient characteristics.
Results:
Of individuals receiving some form of gender-affirming care, 2.43% (95% Confidence Interval 2.14%−2.74%) were diagnosed with an eating disorder: 0.84% anorexia nervosa, 0.36% bulimia nervosa, 0.36% binge eating disorder, 0.15% avoidant restrictive feeding and intake disorder, 0.41% other specified feeding and eating disorders, and 1.37% with an unspecified eating disorder. Among transgender-identifiable patients aged 12–15 years, 5.60% had an eating disorder diagnosis, whereas 0.52% had an eating disorder diagnosis in patients aged 45–64 years.
Discussion:
In patients identifiable as transgender, with receipt of gender affirming care, the prevalence of diagnosed eating disorders was low compared to extant self-reported data for eating disorder diagnosis in transgender individuals. Among this population, eating disorders were highest in adolescents and young adults. Clinically verified prevalence estimates for eating disorder diagnosis in transgender people with a history of gender affirming care warrant further investigation.
Keywords: transgender, eating disorders, gender identity, TGNC, disordered eating, healthcare claims
1. Introduction
In the United States, 1.4 million adults and ~150,000 youth aged 13–17 years identify as transgender (Flores et al., 2020; Conron, 2020). Transgender is a broad term that can be used to describe people whose gender identity is different from the gender assigned at birth. Some transgender people identify as neither a man nor a woman, or as a combination of male and female, and may use one or several terms to describe their gender identity. Often these individuals are referred to as gender diverse (National Center for Transgender Equality, 2018). Transgender and gender diverse individuals are more likely than cisgender individuals to develop a range of chronic physical and mental health conditions in their lifetime (Cicero et al., 2020; Dragon et al., 2017). This population additionally may face stigmatization based on others’ perceptions of their outward appearance, particularly among those who may physically present as what is perceived by an onlooker as visibly transgender (i.e., assumed to not be cisgender based on the onlooker’s ideas of what appearance constitutes identifying with a particular gender).
Both groups may experience social incongruence between gender and others’ perceptions of their gender conformity. Incongruence that is internalized and affects well-being is referred to as gender dysphoria (Zucker, Lawrence, & Kreukels, 2016). This incongruence, a discomfort with one’s physical body and a lack of body satisfaction, can increase vulnerability for the development of eating disorders (Diemer et al., 2018; Gordon et al., 2016; Grossman & D’Augelli, 2007). Those with eating disorders are characterized as having an excessive preoccupation with food, eating, and body image (American Psychological Association, 2021). People with eating disorders are at an elevated risk for suicide, hospitalization, and poor health outcomes–including but not limited to cardiac arrythmias, dehydration and electrolyte disorders, gastrointestinal issues, nutritional deficiencies, anemia, and amenorrhea (Casiero & Frishman, 2006; Sato & Fukudo, 2015; Bulik et al., 2008). In a multi-year, longitudinal study, Franko et al. (2013) reported a standardized mortality ratio of 7.7 in the first 10 years, among a sample of 246 (assumed cisgender) women with diagnosed anorexia nervosa and bulimia nervosa. While all eating disorders are associated with a high all-cause and suicide mortality, anorexia nervosa has the highest mortality rate among them (Franko et al., 2013; Arcelus et al., 2011; Chesney et al., 2014).
Despite a common desire among members of transgender and gender diverse populations to have their gender medically affirmed through hormone therapies and/or surgeries, many face barriers to both general and gender affirming care and may endure discrimination from health care providers (Forbes-Roberts, 2018; Hines et al., 2019). Many transgender and gender diverse people resort to unsafe methods, including disordered eating behaviors (Guss et al., 2017) to align their body with their gender identity and suppress secondary sex characteristics (Turan et al., 2015) largely through restrictive eating and overexercise, placing them at greater risk for developing eating disorders (Diemer et al., 2015; Gordon et al., 2016). Seventy-five percent of transgender and gender diverse college students with eating disorders reported attempted suicide in the last 12 months (Duffy et al., 2019), whereas ~42% of cisgender patients with eating disorders have attempted suicide (Suokas et al., 2014). Considering high all-cause and suicide mortality among cisgender individuals and transgender individuals, eating disorders pose a tremendous threat to the lives of those who suffer from them.
The current understanding of eating disorder prevalence in transgender populations is primarily based on medium size self-report studies from transgender youth and young, college age adults (White et al., 2011). Two studies that used data from the American College Health Association–National College Health Assessment II have reported similar prevalence of self-reported past year eating disorder diagnosis among two samples of self-identifying transgender and gender diverse students; Diemer et al. (2015) reported 15.8% (n=479) of transgender students and Duffy et al. (2019) reported 17.6% (n=678) of transgender students. Diemer et al. (2015) additionally found transgender students to be 4.6 times as likely to be diagnosed with an eating disorder as cisgender students. At the community level, one study leveraged self-report data from a cross-sectional study of transgender individuals over the age of 18 years (n=452) and found that 7.4% had ever been diagnosed with anorexia nervosa or bulimia nervosa. (Diemer et al., 2018) Among these individuals, 55% self-reported having accessed gender affirming medical services, which have been shown to reduce eating disorder symptomology (Jones et al., 2018; Testa et al., 2017; Uniacke et al., 2021; Algars et al., 2012).
Most eating disorder literature in the general population has focused on youth and college age adults; to our knowledge, estimates of eating disorders among older transgender individuals do not exist. Jaworski et al. (2019) analyzed International Classification of Disease (ICD) – 10 codes for anorexia nervosa, atypical anorexia nervosa, bulimia nervosa, and atypical bulimia nervosa in a sample of (assumed cisgender) Polish men who received care through the National Health Fund between 2010–2017 and found that eating disorder prevalence dropped significantly among those older than 20 years of age. Another study that examined the prevalence of eating disorders among a nationally representative sample of (assumed cisgender) US adults found that the average age of onset for anorexia nervosa, bulimia nervosa and binge eating disorder ranged from 19–25 years, and the average current age of the same individuals with these conditions ranged from 39–45 (Udo & Grilo, 2018). In the same study, hazard ratios for all three conditions were inversely associated with age, relative to those 60 years and older, such that those between 18–29 years old were 3.86–5.81 times as likely to be diagnosed with an eating disorder as those 60 years of age and older, those 30–44 years were 2.77–5.45 times as likely and those 45–59 years were 2.37–2.52 times as likely. While eating disorders in assumed cisgender aging populations are much less common than in assumed cisgender youth, as evidenced here, they may persist into middle age and are as equally detrimental to the health of older adults as they are to others. Thus, we advocate that it is important to produce clinically validated estimates of prevalence of eating disorder diagnoses across all age groups in this population, as self-report studies report high numbers of transgender youth and adults with past year eating disorder diagnoses.
In addition to a paucity of estimates among an older cohort of transgender adults, clinically validated eating disorder prevalence estimates among large samples of transgender individuals do not exist. Within the United States, records of medical billing claims (i.e., billing for medical procedures and services provided to patients) are consolidated in several databases (Commercial, Medicaid, & Medicare Supplemental and Coordination of Benefits), which may be made accessible to researchers and institutions seeking to examine a range of health outcomes, cost of care, and care utilization among other areas of interest. While gender identity is not routinely recorded in these datasets, methods to identify transgender individuals through diagnostic and procedures codes have been developed (Proctor et al., 2016; Ewald et al., 2019; Dragon et al., 2017; Progovac et al., 2018). In this study, we have adapted these methods to provide estimates of the prevalence of specific eating disorder diagnoses and describe patient-level characteristics associated with having any diagnosed eating disorder among commercially insured transgender people receiving gender-affirming medical interventions.
2. Methods
2.1. Participants
We used the IBM® MarketScan® Commercial Database (2018). This data resource provides nationwide patient level data for a commercially insured population (health insurance provided to employees of a company, as well as their spouses and/or dependents, which are most often their children) (IBM Watson Health, 2019). The data resource allows linkages of medical billing claims across different settings and services (e.g., inpatient, outpatient, emergency room visits, prescription medications). Because these data are de-identified, this study was not considered human subjects research by the Institutional Review Board at the University of Massachusetts Chan Medical School.
Sample of transgender individuals
We identified 11,169 individuals with evidence of receipt of gender affirming care in inpatient (i.e., inpatient services; records that summarize information about a hospital admission, including up to 15 diagnosis codes and 15 procedure codes), and outpatient (up to 4 diagnosis and 1 procedure code) databases within the 2018 IBM® MarketScan® Commercial Database. This was the most recent year available to the research team. In accordance with prior literature, we used ICD-10 (International Classification of Disease) diagnosis codes for gender identity disorder: F64.0, F64.1 F64.2, F64.8, F64.9 and/or history of sex reassignment: Z87.890, as well as Procedure Coding System (ICD-10-PCS) and Healthcare Common Procedure Coding System (HCPCS) procedure codes for male to female bottom surgery: 0W4M070, 0W4M0J0, 0W4M0K0, 0W4M0Z0, 55970 and female to male bottom surgery: 0W4N071, 0W4N0J1, 0W4N0K1, 0W4N0Z1, 55980 (Proctor et al., 2016; Ewald et al., 2019; Dragon et al., 2017; Progovac et al., 2018). We excluded patients who lacked continuous coverage throughout 2018 and those who either lacked mental health coverage or whose mental health claims were not visible to the research team (n=313). The remaining 10,415 patients comprised the final transgender sample.
Individuals without continuous coverage were excluded because insured individuals are identified in the IBM® MarketScan® Commercial Database with an insurance enrollee identification number that may change when they change employers or when an abrupt change in status (such as disability) intervenes. Additionally, not all insurance plans cover mental health utilization on parity with physical health. Our choice to include only those with continuous coverage was in an effort to capture as many people with complete information as possible given these limitations.
2.2. Measures
Operational definition of eating disorders
Using all data included in the inpatient, inpatient services, and outpatient databases from 2018, we used ICD-10 diagnostic codes for eating disorders in any diagnosis field for anorexia nervosa (F50.0X), bulimia nervosa (F50.2X), binge eating disorder (F50.81), avoidant/restrictive food intake disorder (F50.82), other specified eating disorders (F50.89), and an overall eating disorders category that includes eating disorders (broadly), unspecified eating disorders, and eating disorder unspecified (F50.X, F50.8X (not including F50.81, F50.82, F50.89), F50.9X) (based on 5th ed.; DSM–5; American Psychiatric Association, 2013).
Covariates
Covariates included age, region of medical service within the United States, relationship to plan-holder, sex reported on claims, and type of insurance coverage. Our sample included all patients aged 64 years and younger, grouped into six age groups: <11, 12–15, 16–18, 19–24, 25–44, and 45–64 years to reflect a relatively small number of informative age groups. Patients were categorized based on their relationship to plan holder (i.e., the plan holder, their spouse, or a child/dependent of the plan holder). Sex categories, female and male, were maintained from the variable’s original format and reflect a mixture of sex at birth and current gender. Categories for the US region of service were also maintained from the region variable, in five categories: Northeast, North Central, South, West, or unknown. Race/ethnicity, education, and income are not available in the IBM® MarketScan® Commercial Database. Other demographics that were available, namely plan holder employment type (salary/hourly), unionization status, and employer industrial sector were not analyzed in this analysis due to excessive missingness and/or lack of relevance to the topic at hand.
2.3. Statistical analysis
2.3.1. Data Analysis
Analyses were conducted using SAS 9.4 (Cary, NC, 2011). Descriptive statistics for patient characteristics were calculated. Characteristics of transgender people receiving gender-affirming medical interventions were stratified by age and presence of any eating disorder and proportions were generated with 95% confidence intervals (CI).
3. Results
3.1. Descriptive statistics
Our sample consisted of 10,415 transgender-identified individuals. Almost sixty percent of the sample was described as female on claims (59.2%, which may be sex at birth or current gender), 63% were younger than 24 years old. Nearly one third (32.2%) were identified as being the primary plan holder, 62.6% were the child of a plan holder, 5.2% the spouses of the plan holder (Table 1).
Table 1.
Demographic characteristics of transgender people identified in a database of those with commercial insurance, 2018
| N=10,415 | |
|---|---|
| Percentage | |
| Sex reported on claims | |
| Male | 40.8 |
| Female | 59.2 |
| Age group (years) | |
| <11 | 2.5 |
| 12 to 15 | 10.8 |
| 16 to 18 | 18.1 |
| 19 to 24 | 31.6 |
| 25 to 44 | 26.0 |
| 45 to 64 | 11.1 |
| Plan Type | |
| Basic/ major medical/ comprehensive | 2.1 |
| Preferred provider organization | 49.9 |
| High-deductible/consumer-driven | 20.3 |
| All other health plans† | 25.8 |
| missing | 1.9 |
| Relationship to Plan Holder | |
| Self | 32.2 |
| Spouse | 5.2 |
| Child/other | 62.6 |
| US Region of Service | |
| Northeast | 21.4 |
| North Central | 24.1 |
| South | 31.3 |
| West | 22.8 |
| missing | 0.4 |
All other health plans include: exclusive provider organization, health maintenance organization, point-of-service.
3.2. Eating disorder prevalence
Among individuals identifiable as transgender from claims, we found that unspecified feeding and eating disorders (1.37%, 95% CI [1.16–1.62]) were the most commonly diagnosed eating disorders, followed by anorexia nervosa (0.84%, 95% CI [0.67–1.03]), other specified feeding and eating disorders (0.41%, 95% CI [0.30–0.56]), bulimia nervosa (0.36%, 95% CI [0.26–0.50]), binge eating disorder (0.36%, 95% CI [0.25–0.49]), and avoidant restrictive feeding and intake disorder (0.15%, 95% CI [0.09–0.25]) (Table 2). The median age of individuals with diagnosed eating disorders ranged from 15 for avoidant restrictive feeding and intake disorder to 22 for binge eating disorder.
Table 2.
Proportion and measures of the age distribution of specific eating disorder diagnoses among claims-identified transgender individuals, 2018
| Diagnoses | Number of patients | Proportion % (95% confidence interval) | Median age (25th – 75th percentile) |
|---|---|---|---|
| Anorexia nervosa | 87 | 0.84 (0.67–1.03) | 17 (16–20) |
| Bulimia nervosa | 38 | 0.36 (0.26–0.50) | 19 (16–23) |
| Binge eating disorder | 37 | 0.36 (0.25–0.49) | 22 (17–25) |
| Avoidant restrictive deeding and intake disorder | 16 | 0.15 (0.09–0.25) | 15 (14–20) |
| Other specified feeding and eating disorders | 43 | 0.41 (0.30–0.56) | 18 (15–22) |
| Unspecified feeding and eating disorders | 143 | 1.37 (1.16–1.62) | 17 (15–20) |
| Any eating disorder | 253 | 2.43 (2.14–2.74) | 18 (15–22) |
Those diagnosed with any eating disorder were more likely to be young, reported as female on claims; the proportion diagnosed with eating disorders was similar across all US geographic regions (Table 3). Figure 1 displays the prevalence of any diagnosed eating disorder for these patients identifiable as transgender, within 5-year age groups.
Table 3.
Prevalence of any eating disorder diagnosis across claims-identified transgender individuals
| Diagnoses | Number of patients with any eating disorder | Prevalence estimate (95% confidence interval) |
|---|---|---|
| Sex (on claims) | ||
| Male (n=4,252) | 73 | 1.72 (1.35–2.15) |
| Female (n=6,163) | 180 | 2.92 (2.51–3.37) |
| Age group (years) | ||
| 0–11 (n=256) | 1 | 0.39 (0.01–2.16) |
| 12–15 (n=1,125) | 63 | 5.60 (4.33–7.11) |
| 16–18 (n=1,883) | 74 | 3.93 (3.10–4.91) |
| 19–24 (n=3,287) | 77 | 2.34 (1.85–2.92) |
| 25–44 (n=2,709) | 32 | 1.18 (0.81–1.66) |
| 45–64 (n=1,156) | 6 | 0.52 (0.19–1.13) |
| Region of Service | ||
| Northeast (n=2,229) | 63 | 2.83 (2.18–3.60) |
| North central (n=2,509) | 69 | 2.75 (2.15–3.47) |
| South (n=2,377) | 65 | 2.00 (1.54–2.54) |
| West (n=2,377) | 54 | 2.27 (1.71–2.95) |
Figure 1.
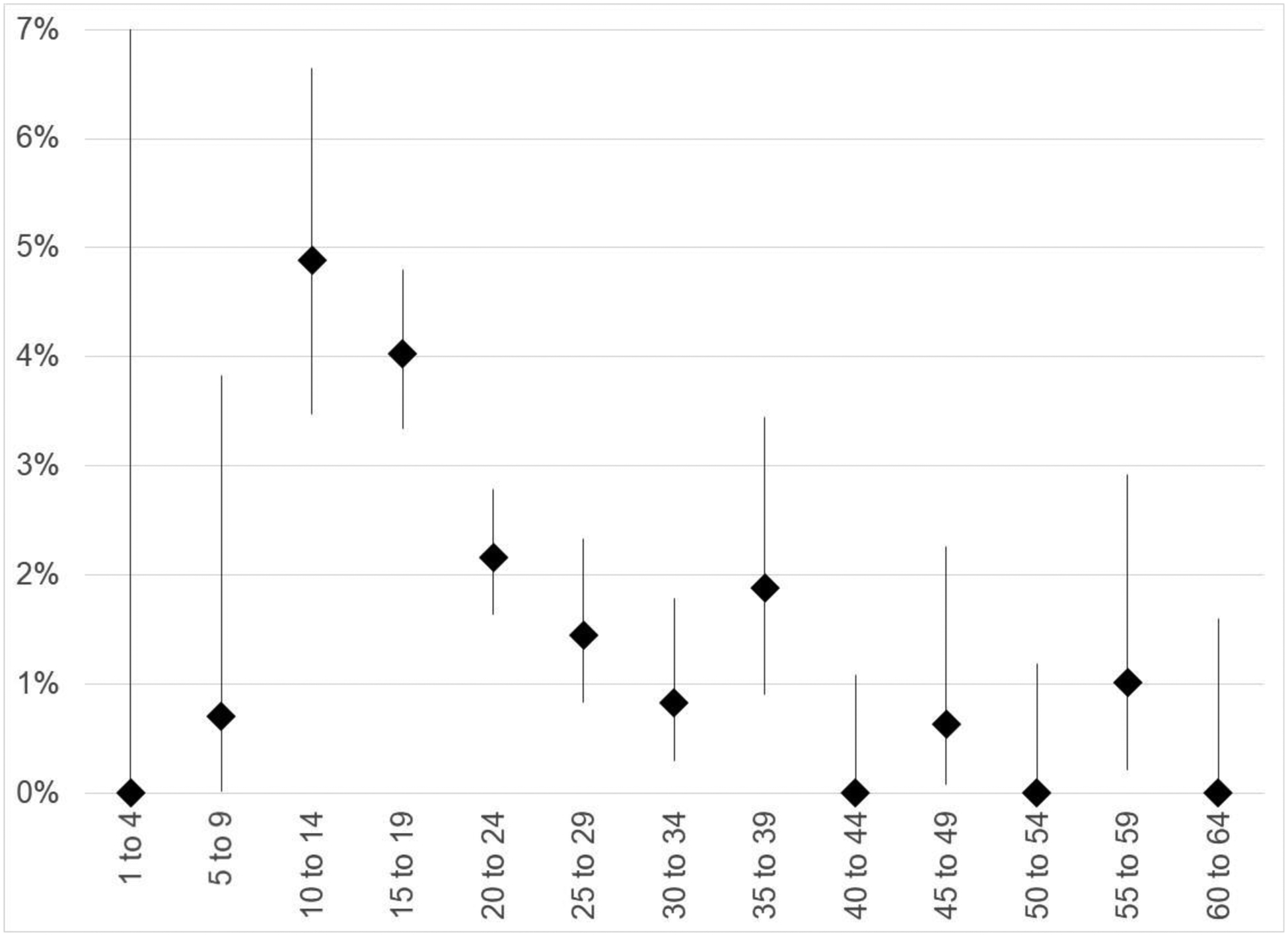
Prevalence and 95% confidence interval for any diagnosed eating disorder among patients identifiable as transgender in the IBM® MarketScan® 2018 database, by 5-year age groups.
Point estimates for any diagnosed eating disorder shown as black diamonds. 95% confidence intervals shown as vertical lines. The upper confidence limit for the 11 patients aged 1 to 4 is truncated from 28.5%
4. Discussion
Our study is the first to provide contemporary national estimates of clinically diagnosed eating disorders among US transgender individuals. Using national claims data from individuals, covering a diversity of insurers, providers, and commercially insured individuals, we found that 2.43% of transgender individuals had a diagnosis of an eating disorder in 2018. The prevalence of any eating disorder was highest among those younger than 24 years of age, and among patients coded as female on claims.
Our estimate of the prevalence of clinically diagnosed eating disorders is lower than previous reports of any eating disorder among transgender individuals. Prior studies have reported that that 7.4–17.6% of transgender individuals self-reported eating disorders (Diemer et al., 2015; Diemer et al., 2018; Duffy et al., 2019). We found that the highest prevalence of eating disorders was in those aged 12–15 years (5.60%) and 16–18 years (3.93%). These findings are consistent with general population age trends that highlight a greater prevalence of onset of disordered eating among those between the ages of 15–21 (Hudson et al., 2007; Keski-Rahkonen et al., 2007; Isomaa et al., 2009). We additionally found that 0.84% of our sample was clinically diagnosed with anorexia nervosa and 0.36% with bulimia nervosa. These estimates are lower than previous reports. In a survey of almost 500 transgender adults, Nagata et al. (2020) found that 4.1% of transgender women and 4.2% of transgender men reported being told by a clinician that they had anorexia nervosa, closely followed by 2.9% and 3.2% with bulimia nervosa.
The discrepancy between our prevalence estimates based on clinically diagnosed eating disorders and estimates based on self-reported eating disorders may be explained by low rates of clinical diagnosis generally; only one in ten people living with eating disorders receive clinical treatment (Noordenbos, 2002). This may be because there are low levels of interaction with and potentially barriers to accessing care providers, perhaps especially for transgender individuals (Duffy et al., 2016). In the general population, low levels of diagnosis may be attributed to weight stigma (Hatzenbuehler et al., 2009), financial barriers and cost of care (National Eating Disorder Association Statistics, 2015; Evans et al., 2011), barriers caused by disparities and discrimination in healthcare settings due to racial, sexual and gender identity (Marques et al., 2011; Strother et al., 2012; Duffy et al., 2016). Within the sample we investigated, all individuals had received gender affirming care. Prior studies have shown that affirmation of gender identity can lead to a decrease in or lower disordered eating symptomology (Jones et al., 2018; Testa et al., 2017; Uniacke et al., 2021) and increased body image satisfaction (Owen-Smith et al., 2018). As such, the occurrence of eating disorders in this medically affirmed population is likely to be lower than in a general population of transgender people. Nevertheless, eating disorders may persist well beyond physical symptom remission and there is not yet consensus in the field regarding what qualifies as full recovery (Steinhausen, 2002; Vall & Wade, 2015). Those with eating disorders or those in recovery may take on new disordered eating behaviors; undergoing diagnostic crossover, especially on the path of recovery from one disorder (Eddy et al., 2008; Mortimer, 2019). Thus, the extent to which treatment of eating disorders provides attentive care that positively affirms their gender identity warrants further investigation.
Cross-sectional surveys of gender minority people tend to have a higher average age of transgender respondents than what was observed in the current study. Cross-sectional studies of transgender people are largely comprised of individuals over 25 years of age (Herman et al., 2017). Our study provides a rare look at the prevalence of clinically diagnosed eating disorders among older transgender adults as well as transgender youth. For transgender people, eating disorders may be a means to affirm their gender identity through the suppression of secondary sex characteristics (Ålgars, Santtila, & Sandnabba, 2010), coping with stress related to gender identity (Cohelo et al., 2019), body uneasiness (Bandini et al., 2013), objectification, and minority stress (Brewster, Velez, Breslow, & Geiger, 2019). Eating disorders, like in their cisgender peers, may serve as a path to rapidly attaining a socially desirable figure, gain social capital with peers of the gender they identify with, or attain a sense of control over one’s body and appearance when they lack a sense of control over the impact of puberty on their body (McGuire et al., 2016; Ålgars, Santtila, & Sandnabba, 2010, Murray et al., 2013). Non-conformity to cisgender norms as a by-product of seeking to affirm one’s gender presentation, can render transgender individuals vulnerable to scrutiny from family, peers, and strangers (Bradford, Reisner, Honnold, & Xavier, 2013; Fuller & Riggs, 2018). With societal pressures on young people to look a certain way and the added pressures that they may face from adults and peers if they are not cisgender, feeling comfortable about one’s body or appearance may be challenging, particularly for those experiencing gender dysphoria (Duffy, Henkel, & Earnshaw, 2016; Gordon et al., 2016; Nagata, Ganson, & Austin, 2020). Considering this, it is not surprising that most of our sample diagnosed with an eating disorder are in their teens (Ristori et al., 2019); when young people are coming into who they are as an individual.
Despite the use of a national claims data resource, our data were limited to those identifiable as transgender in claims data, likely reflective of receipt of gender-affirming care. Considering barriers to receiving gender-affirming care, it is not appropriate to generalize these findings to transgender people who are not receiving gender-affirming care. We have used a validated approach to identifying transgender individuals in claims data. Yet, the possibility of misclassification of individuals who prefer another gender identity than “transgender”, such as non-binary, gender queer, or two spirit among various other identities remains.
There are several explanations for why our estimates are lower than expected. First, in this claims dataset, diagnoses of eating disorders are likely driven by the receipt of health care for eating disorders, and thus under-reported relative to the actual prevalence in this population (Tkacz & Brady, 2021; Deloitte Access Economics, 2020). Providers may lack awareness of eating disorders among transgender individuals and fail to recognize these disorders, may prioritize treatment for gender dysphoria above disordered eating behaviors or may blame gender dysphoria as the cause of an eating disorder when it is being caused by trauma, issues with food texture, or bullying among a number of reasons. Patients receiving gender affirming care may be reluctant to disclose disordered eating behaviors either due to lack of time with providers or because of required mental health assessments before insurers authorize gender-affirming surgery.
Limitations
While we have produced findings that provide us insight regarding the scope of individuals with eating disorders who receive affirming medical care, overall and stratified by age, our cross-sectional analysis is limited to a single recent year of data, and may not reflect the age or diagnosis with eating disorders, merely their prevalence. Further, despite identifying a sample based on receipt of gender affirming care, we did not consider procedure codes for mammoplasty, orchiectomy, puberty blockers, and hormone replacement therapy, as these are all commonly used in the treatment of cisgender individuals. We recognize that in doing so, these findings must be interpreted within the context of those who have received particular types of gender affirming care. Additionally, we restricted our eligibility criteria to include only those with continuous health insurance coverage in 2018. Future research may lengthen the study period. This database does not collect information on race/ethnicity or socioeconomic status and thus individuals in this database are representative only of those insured by their employers, and these findings do not pertain to individuals who are covered under Medicare (i.e. older adults 65 years and older) and Medicaid (i.e., individuals with notably low income and disabled individuals). Lastly, females historically have been reported as the most affected by eating disorders and have been the focus of eating disorder treatment generally (Cohelo et al., 2019). Sex reported on claims in this study may be the sex of the individual at birth or the individual’s gender identity, and there is likely to be variation in coding practices between care sites. Thus, we caution against interpreting findings by sex.
Conclusion
In this population of individuals identifiable as transgender from claims indicating receipt of gender-affirming care, 2.43% were diagnosed with one or more eating disorders. This proportion is low compared to the self-reported prevalence of eating disorders from other sources. While we suspect diagnostic biases to be at play, our data do not allow us to explore this issue further. The health of transgender individuals is understudied, and these claims data provide insights for those receiving affirming care.
Nevertheless, we believe that the occurrence of eating disorders in transgender populations is likely undercounted, particularly in adolescent and young adult populations, who may be hindered in their ability to access care (Duffy et al., 2016) or avoid disclosing gender identity to providers due to fear of exile from family members and/or community, as well as fear of discrimination and microaggressions from providers. Despite that this population of transgender individuals already received care, more research is needed to understand potential issues around identifying eating disorders and ensuring that those providing care for eating disorders are aware of issues specific to mental wellness for transgender individuals. As with all clinicians, those treating eating disorders should 1) be educated around providing gender affirming care, 2) allow gender minority patients in their practice to identify themselves (i.e., gender identity, pronouns, preferred name) and use those identity markers, 3) affirm the gender identity of their gender minority patients, 4) develop treatment plans cognizant of their patients’ developing gender identities, and 5) seek resources to help them develop these skills, such as attending gender minority focused grand rounds at local universities and medical centers, educational trainings for providing treatment and affirming care to gender minority patients through local, state, and national transgender and gender diverse run mental health and advocacy organizations, 6) educate themselves on state level healthcare policies pertaining to gender minority individuals, and 7) network with peers who openly advocate for and provide gender inclusive mental health care.
Public Significance Statement:
The present study aims to provide clinically validated, contemporary prevalence estimates for diagnosed eating disorders among a medically affirmed population of transgender adults and children in the United States. We report low prevalence of having any eating disorder relative to prevalence estimates reported in prior literature without clinical validation. These findings may be explained by access to affirming care and medical care generally.
Acknowledgements and Conflicts of Interest:
The authors have no conflicts to declare. Ms. Ferrucci is a recipient of a pre-doctoral slot on an institutional NIH training grant (TL1TR001454 to Dr. Lapane). All authors identify as cisgender.
Availability of Data, Materials and Code:
We are unable to share data per the terms of the licensing agreement with the IBM® MarketScan® Commercial Database. The IBM® MarketScan® Commercial Database may be licensed and used for research with a Data Use Agreement. The SAS code used to generate the analyses will be made available on request.
References
- Ålgars M, Alanko K, Santtila P, & Sandnabba NK (2012). Disordered eating and gender identity disorder: a qualitative study. Eating disorders, 20(4), 300–311. 10.1080/10640266.2012.668482 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- American Psychological Association. (2021). What Are Eating Disorders? What are eating disorders? Retrieved December 5, 2021, from https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, & Nielsen S (2011). Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Archives of general psychiatry, 68(7), 724–731. 10.1001/archgenpsychiatry.2011.74 [DOI] [PubMed] [Google Scholar]
- Bachmann CL, Gooch B. LGBT in Britain: Health report [Internet]. London; 2018. Available from: stonewall.org.uk [Google Scholar]
- Bandini E, Fisher AD, Castellini G, Lo Sauro C, Lelli L, Meriggiola MC, Casale H, Benni L, Ferruccio N, Faravelli C, Dettore D, Maggi M, & Ricca V (2013). Gender identity disorder and eating disorders: similarities and differences in terms of body uneasiness. The journal of sexual medicine, 10(4), 1012–1023. 10.1111/jsm.12062 [DOI] [PubMed] [Google Scholar]
- Becker I, Nieder TO, Cerwenka S, Briken P, Kreukels BP, Cohen-Kettenis PT, Cuypere G, Haraldsen IR, & Richter-Appelt H (2016). Body Image in Young Gender Dysphoric Adults: A European Multi-Center Study. Archives of sexual behavior, 45(3), 559–574. 10.1007/s10508-015-0527-z [DOI] [PubMed] [Google Scholar]
- Bradford J, Reisner SL, Honnold JA, & Xavier J (2013). Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. American journal of public health, 103(10), 1820–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster ME, Velez BL, Breslow AS, & Geiger EF (2019). Unpacking body image concerns and disordered eating for transgender women: The roles of sexual objectification and minority stress. Journal of counseling psychology, 66(2), 131. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Thornton L, Pinheiro AP, Plotnicov K, Klump KL, Brandt H, … & Kaye WH (2008). Suicide attempts in anorexia nervosa. Psychosomatic Medicine, 70(3), 378–383. [DOI] [PubMed] [Google Scholar]
- Casiero D, & Frishman WH (2006). Cardiovascular complications of eating disorders. Cardiology in review, 14(5), 227–231. [DOI] [PubMed] [Google Scholar]
- Chesney E, Goodwin GM, & Fazel S (2014). Risks of all‐cause and suicide mortality in mental disorders: a meta‐review. World psychiatry, 13(2), 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coelho JS, Suen J, Clark BA, Marshall SK, Geller J, & Lam PY (2019). Eating disorder diagnoses and symptom presentation in transgender youth: a scoping review. Current psychiatry reports, 21(11), 1–10. [DOI] [PubMed] [Google Scholar]
- Conron KJ LGBT Youth Population in the United States. (September 2020). The Williams Institute, UCLA, Los Angeles, CA. [Google Scholar]
- Cicero EC, Reisner SL, Merwin EI, Humphreys JC, & Silva SG (2020). The health status of transgender and gender nonbinary adults in the United States. PloS one, 15(2), e0228765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deloitte Access Economics. The Social and Economic Cost of Eating Disorders in the United States of America: A Report for the Strategic Training Initiative for the Prevention of Eating Disorders and the Academy for Eating Disorders. June 2020. Available at: https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/. [Google Scholar]
- Diemer EW, Grant JD, Munn-Chernoff MA, Patterson DA, & Duncan AE (2015). Gender identity, sexual orientation, and eating-related pathology in a national sample of college students. Journal of Adolescent Health, 57(2), 144–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diemer EW, White Hughto JM, Gordon AR, Guss C, Austin SB, & Reisner SL (2018). Beyond the binary: Differences in eating disorder prevalence by gender identity in a transgender sample. Transgender Health, 3(1), 17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragon CN, Guerino P, Ewald E, & Laffan AM (2017). Transgender Medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT health, 4(6), 404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy ME, Henkel KE, & Earnshaw VA (2016). Transgender clients’ experiences of eating disorder treatment. Journal of LGBT Issues in Counseling, 10(3), 136–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy ME, Henkel KE, & Joiner TE (2019). Prevalence of self-injurious thoughts and behaviors in transgender individuals with eating disorders: A national study. Journal of Adolescent Health, 64(4), 461–466. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, & Herzog DB (2008). Diagnostic crossover in anorexia nervosa and bulimia nervosa: implications for DSM-V. American Journal of Psychiatry, 165(2), 245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EJ, Hay PJ, Mond J, Paxton SJ, Quirk F, Rodgers B, Sawoniewska MA (2011). Barriers to help-seeking in young women with eating disorders: A qualitative exploration in a longitudinal community survey. Eating Disorders, 19(3), 270–285. https://doi-org.umassmed.idm.oclc.org/10.1080/10640266.2011.566152 [DOI] [PubMed] [Google Scholar]
- Ewald ER, Guerino P, Dragon C, Laffan AM, Goldstein Z, & Streed C Jr (2019). Identifying medicare beneficiaries accessing transgender-related care in the era of ICD-10. LGBT health, 6(4), 166–173. [DOI] [PubMed] [Google Scholar]
- Flores AR, Herman JL, Gates GJ, & Brown TN (2020, April 27). How many adults identify as transgender in the United States? Retrieved March 04, 2021, from https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/ [Google Scholar]
- Forbes-Roberts S (2018). Exploring Patient Satisfaction among Transgender and Non-Binary Identified Healthcare Users: The Role of Microaggressions and Inclusive Healthcare Settings. [Google Scholar]
- Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, & Herzog DB (2013). A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. American Journal of Psychiatry, 170(8), 917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller KA, & Riggs DW (2018). Family support and discrimination and their relationship to psychological distress and resilience amongst transgender people. International Journal of Transgenderism, 19(4), 379–388. [Google Scholar]
- Gordon AR, Austin SB, Krieger N, Hughto JMW, & Reisner SL (2016). “I have to constantly prove to myself, to `people, that I fit the bill”: Perspectives on weight and shape control behaviors among low-income, ethnically diverse young transgender women. Social Science & Medicine, 165, 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman AH, & D’Augelli AR (2007). Transgender youth and life-threatening behaviors. Suicide and life-threatening behavior, 37(5), 527–537. [DOI] [PubMed] [Google Scholar]
- Guss CE, Williams DN, Reisner SL, Austin SB, & Katz-Wise SL (2017). Disordered weight management behaviors, nonprescription steroid use, and weight perception in transgender youth. Journal of Adolescent Health, 60(1), 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Hasin DS. (2009). Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity, 17(11), 2033–2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman JL, Flores AR, Brown TN, Wilson BD, & Conron KJ (2017). Age of individuals who identify as transgender in the United States (pp. 1–13). eScholarship, University of California. [Google Scholar]
- Hines DD, Laury ER, & Habermann B (2019). They Just Don’t Get Me: A Qualitative Analysis of Transgender Women’s Health Care Experiences and Clinician Interactions. The Journal of the Association of Nurses in AIDS Care, 30(5), e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological psychiatry, 61(3), 348–358. 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Watson Health. IBM MarketScan Research Databases for Health Services Researchers. White Pap. Published online 2019:15. [Google Scholar]
- Isomaa R, Isomaa AL, Marttunen M, Kaltiala-Heino R, & Björkqvist K (2009). The prevalence, incidence and development of eating disorders in Finnish adolescents: a two-step 3-year follow-up study. European eating disorders review: the journal of the Eating Disorders Association, 17(3), 199–207. 10.1002/erv.919. [DOI] [PubMed] [Google Scholar]
- Jaworski M, Panczyk M, Śliwczyński A, Brzozowska M, Janaszek K, Małkowski P, & Gotlib J (2019). Eating Disorders in Males: An 8-Year Population-Based Observational Study. American Journal of Men’s Health. 10.1177/1557988319860970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BA, Haycraft E, Bouman WP, Brewin N, Claes L, & Arcelus J (2018). Risk factors for eating disorder psychopathology within the treatment seeking transgender population: The role of cross‐sex hormone treatment. European Eating Disorders Review, 26(2), 120–128. [DOI] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Hoek HW, Susser ES, Linna MS, Sihvola E, Raevuori A, Bulik CM, Kaprio J, & Rissanen A (2007). Epidemiology and course of anorexia nervosa in the community. The American journal of psychiatry, 164(8), 1259–1265. [DOI] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen C, Fang A, Chosak A, & Diniz JB (2011). Comparative Prevalence, Correlates of Impairment, and Service Utilization for Eating Disorders across U.S. Ethnic Groups: Implications for Reducing Ethnic Disparities in Health Care Access for Eating Disorders. The International Journal of Eating Disorders, 44(5), 412–420. 10.1002/eat.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JK, Doty JL, Catalpa JM, & Ola C (2016). Body image in transgender young people: Findings from a qualitative, community based study. Body Image, 18, 96–107. [DOI] [PubMed] [Google Scholar]
- Mortimer R (2019). Pride before a fall: Shame, diagnostic crossover, and eating disorders. Journal of bioethical inquiry, 16(3), 365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray K, Rieger E, & Byrne D (2013). A longitudinal investigation of the mediating role of self-esteem and body importance in the relationship between stress and body dissatisfaction in adolescent females and males. Body image, 10(4), 544–551. 10.1016/j.bodyim.2013.07.011 [DOI] [PubMed] [Google Scholar]
- Nagata JM, Ganson KT, & Austin SB (2020). Emerging trends in eating disorders among sexual and gender minorities. Current Opinion in Psychiatry, 33(6), 562–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata JM, Murray SB, Compte EJ, Pak EH, Schauer R, Flentje A, et al. Community norms for the Eating Disorder Examination Questionnaire (EDE-Q) among transgender men and women. Eat Behav 2020. 3 27;101381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Eating Disorders Association (2015) Retrieved from http://www.nationaleatingdisorders.org/
- Noordenbos G, Oldenhave A, Muschter J, & Terpstra N (2002). Characteristics and treatment of patients with chronic eating disorders. Eating disorders, 10(1), 15–29. 10.1080/106402602753573531. [DOI] [PubMed] [Google Scholar]
- Owen-Smith AA, Gerth J, Sineath RC, Barzilay J, Becerra-Culqui TA, Getahun D, … & Goodman M (2018). Association between gender confirmation treatments and perceived gender congruence, body image satisfaction, and mental health in a cohort of transgender individuals. The journal of sexual medicine, 15(4), 591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Progovac AM, Cook BL, Mullin BO, McDowell A, Sanchez R MJ, Wang Y, … & Schuster MA (2018). Identifying gender minority patients’ health and health care needs in administrative claims data. Health Affairs, 37(3), 413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor K, Haffer SC, Ewald E, Hodge C, & James CV (2016). Identifying the transgender population in the Medicare program. Transgender Health, 1(1), 250–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ristori J, Fisher AD, Castellini G, Sensi C, Cipriani A, Ricca V, & Maggi M (2019). Gender dysphoria and anorexia nervosa symptoms in two adolescents. Archives of sexual behavior, 48(5), 1625–1631. [DOI] [PubMed] [Google Scholar]
- Strother E, Lemberg R, Stanford SC, & Turberville D (2012). Eating Disorders in Men: Underdiagnosed, Undertreated, and Misunderstood. Eating Disorders, 20(5), 346–355. doi: 10.1080/10640266.2012.715512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato Y, & Fukudo S (2015). Gastrointestinal symptoms and disorders in patients with eating disorders. Clinical journal of gastroenterology, 8(5), 255–263. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC (2002). The outcome of anorexia nervosa in the 20th century. American Journal of Psychiatry; 159:1284–93. [DOI] [PubMed] [Google Scholar]
- Vall E & Wade TD, (2015). Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. International Journal of Eating Disorders. 48:946–71. [DOI] [PubMed] [Google Scholar]
- Suokas JT, Suvisaari JM, Grainger M, Raevuori A, Gissler M, & Haukka J (2014). Suicide attempts and mortality in eating disorders: a follow-up study of eating disorder patients. General hospital psychiatry, 36(3), 355–357. [DOI] [PubMed] [Google Scholar]
- Testa RJ, Rider GN, Haug NA, & Balsam KF (2017). Gender confirming medical interventions and eating disorder symptoms among transgender individuals. Health Psychology, 36(10), 927. [DOI] [PubMed] [Google Scholar]
- Tkacz J, & Brady BL (2021). Increasing rate of diagnosed childhood mental illness in the United States: Incidence, prevalence and costs. Public Health in Practice, 2, 100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan Ş, Poyraz CA, & Duran A (2015). Prolonged anorexia nervosa associated with female-to-male gender dysphoria: A case report. Eating behaviors, 18, 54–56. [DOI] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and Correlates of DSM-5-Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biological psychiatry, 84(5), 345–354. 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Understanding transgender people: The basics. National Center for Transgender Equality. (2018, October 5). Retrieved December 5, 2021, from https://transequality.org/issues/resources/understanding-transgender-people-the-basics. [Google Scholar]
- Uniacke B, Glasofer D, Devlin M, Bockting W, & Attia E (2021). Predictors of eating-related psychopathology in transgender and gender nonbinary individuals. Eating behaviors, 42, 101527. 10.1016/j.eatbeh.2021.101527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S, Reynolds-Malear JB, & Cordero E (2011). Disordered eating and the use of unhealthy weight control methods in college students: 1995, 2002, and 2008. Eating disorders, 19(4), 323–334. [DOI] [PubMed] [Google Scholar]
- Zucker KJ, Lawrence AA, & Kreukels BP (2016). Gender dysphoria in adults. Annual Review of Clinical Psychology, 12, 217–247. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We are unable to share data per the terms of the licensing agreement with the IBM® MarketScan® Commercial Database. The IBM® MarketScan® Commercial Database may be licensed and used for research with a Data Use Agreement. The SAS code used to generate the analyses will be made available on request.


