Abstract
Background:
Percutaneous transcatheter angioplasty (PTA) and carotid artery stenting (CAS) are often performed repeatedly for in-stent restenosis (ISR) after CAS. Only a few reports describe the treatment for repeated ISR. Furthermore, only a few reports describe carotid endarterectomy (CEA) after CAS; thus, the evidence for this procedure is insufficient.
Case Description:
Herein, we describe a case in which CEA with stent removal was performed in a patient with repeated ISR after CAS. A 78-year-old man presented with dysarthria and slight left limb weakness. CAS was performed for the right internal carotid artery stenosis. ISR occurred again and PTA and stenting were performed. After the second CAS, ISR occurred again. CEA with stent removal was performed. After the CEA with stent removal, the patient experienced no restenosis or other complications.
Conclusion:
CEA with stent removal can be a good option for treating repeated ISR after CAS.
Keywords: Carotid artery stent, Carotid endarterectomy, In-stent restenosis, Internal carotid artery stenosis, Neointimal hyperplasia

INTRODUCTION
The rates of in-stent restenosis (ISR) after carotid artery stenting (CAS) are between 3% and 10% and ISR is associated with ipsilateral cerebral infarction.[17] Percutaneous transcatheter angioplasty (PTA) and CAS are often repeated for the reoccurrence of ISR after CAS.[19] However, the treatment of patients with repeated ISR and carotid endarterectomy (CEA) after CAS is not well known. We report the case of a patient who underwent CEA with stent removal for repeated ISR after CAS with good clinical results.
CASE REPORT
A 78-year-old man with hypertension, Type 2 diabetes mellitus, and dyslipidemia presented with dysarthria and slight left limb weakness. Diffusion-weighted imaging revealed multiple small cerebral infarctions spreading cortically and a watershed area in the right brain hemisphere [Figure 1a]. Magnetic resonance angiography revealed severe stenosis of the right internal carotid artery [Figure 1b]. We diagnosed atherosclerotic embolism caused by severe right internal carotid artery stenosis. Carotid echography showed a peak systolic velocity (PSV) of 354 cm/s for the stenosis lesion. Cervical magnetic resonance imaging revealed an unstable plaque with a T1-weighted image (black-blood method) of high intensity. Angiography showed that the stenosis rate was 90%, according to the method used in the North American Symptomatic CEA Trial [Figure 1c]. Dual antiplatelet treatment (aspirin 100 mg and clopidogrel 75 mg/day) and statin were initiated. We planned the best medical treatment in the acute phase and revascularization in the chronic phase.
Figure 1:
(a) Diffusion-weighted imaging at initial presentation showing a right frontal infarction. (b) Magnetic resonance angiography showing severe stenosis on the right side. (c) Preoperative angiography showing severe right internal carotid stenosis. (d) Angiography after carotid artery stenting.
CAS was performed 1 month after symptom onset. Although a staged CAS was planned, plaque protrusion occurred just after PTA; therefore, we deployed a closed-cell stent (Carotid WallStent 10 × 24 mm, Boston Scientific, Marlborough, MA, USA) [Figure 1d]. Due to concerns about the possibility of hyperperfusion syndrome, we did not perform poststenting PTA. In our institutes, 50% diluted contrast medium is used to evaluate plaque protrusion. The procedure was finished after confirming that there was no plaque protrusion. Postoperative carotid echography revealed no plaque protrusion and the PSV was 83 cm/s [Figure 2a]. Four months after CAS, a carotid echography revealed that the PSV was over 300 cm/s [Figure 2b]. A second CAS for ISR was performed 7 months after the first CAS. An open cell stent (Precise 6 × 30 mm, Cordis, Dublin, OH, USA) was deployed and poststenting PTA was performed [Figures 2c and d]. After confirming that there was no plaque protrusion, procedure was finished.
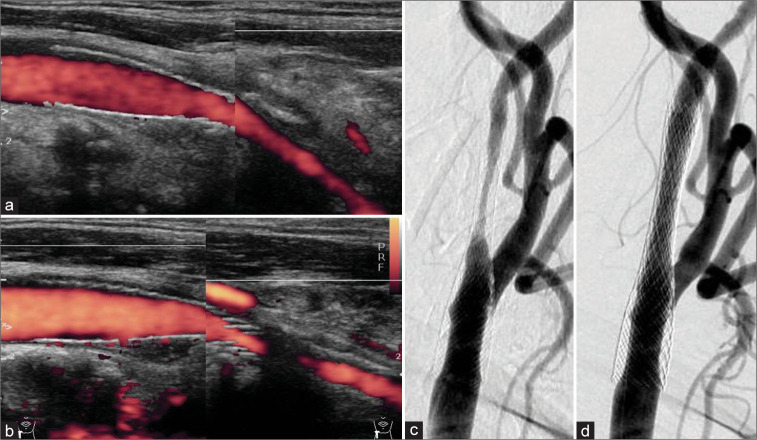
Figure 2:
(a) After carotid artery stenting (CAS), the postoperative carotid echography revealed no stenosis. The peak systolic velocity (PSV) was 62.3 cm/s. (b) A carotid echography 4 months after the first CAS showing in-stent restenosis (ISR). The PSV was over 300 cm/s. (c) Angiography showing ISR 4 months after the first CAS. (d) The angiography after percutaneous transcatheter angioplasty and a second CAS were performed.
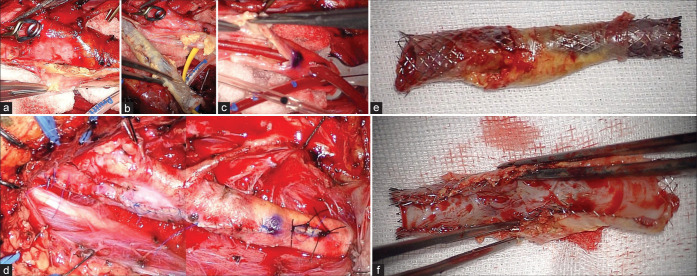
Six to 9 months after the second CAS, ISR again worsened; the carotid echography revealed a PSV of 139–317 cm/s [Figures 3a and b]. Angiography revealed severe ISR [Figures 3c-e]. ISR might have developed repeatedly in this patient, despite repeated CAS, and the thickness of the stent might cause ISR. Therefore, we decided to carry out CEA with stent removal. The procedure was performed 1 year after the second CAS. The proximal and distal ends of the stent were approached using normal techniques. Insertion of an internal shunt was needed because angiography showed that the collateral flow was inadequate. The space was not sufficient to insert the distal side of the internal shunt. To reduce the closure time, insertion of an internal shunt into the normal common carotid artery with a minimal incision was attempted. However, the shunt tube could not pass through the severe stenosis. Thus, the stent and plaque were removed first. A normal CEA could be performed because the boundary between the plaque (including stent) and the vessel wall was clear [Figures 4a and b]. After the plaque was removed, an internal shunt was inserted [Figure 4c]. The vessel wall was not damaged and could be sutured normally. The internal shunt was removed and the insertion portion was sutured [Figure 4d]. Although there was atherosclerotic plaque around the stent [Figure 4e], the ISR was caused by neointima formation inside the lumen of the stent, not by plaque protrusion or atherosclerotic change [Figure 4f]. The postoperative course was uneventful and postoperative carotid echography results were good. The postprocedural treatment included dual antiplatelet treatment, statin treatment, and diabetes mellitus control. At the 6-month follow-up, the patient was asymptomatic with no sign of recurrent restenosis.
Figure 3:
Worsening in-stent restenosis (ISR) after the second carotid artery stenting is shown. The carotid echography revealed peak systolic velocity changes from 139 cm/s (a) to 317 cm/s (b) 6 to 9 months after the second carotid artery stenting. (c and d) The angiography shows severe ISR. (e) The distal end of the stent location at the C2 level is shown.
Figure 4:
(a and b) The clear boundary between the plaque, including the stent, and the vessel wall is shown. Normal carotid endarterectomy was performed. (c) Insertion of an internal shunt after removed plaque is shown. (d) The vessel wall could be sutured as normal. (e and f) The stent and plaque are shown. Neointima formed inside the lumen of the stent, causing in-stent restenosis.
DISCUSSION
ISR is a complication that may occur after CAS. Cases of symptomatic or severe restenosis may require retreatment. The rate of cerebral infarction onset on the same side after CAS was 6.6%/3 years in the SAPPHIRE study,[11] 6.2%/4 years in the CREST study,[4] 11.1%/4 years in the EVA-3S study,[15] 9.5%/2 years in the SPACE study,[8] and 5.8%/6 years in the ICSS study.[3] ISR after CAS is often defined as more than 70% stenosis. The ISR occurrence was 6.0%/2 years in the CREST study,[14] 3.3%/3 years in the EVA-3S study,[1] 10.7%/2 years in the SPACE study,[8] and 10.6%/5 years in the ICSS study.[3] Dakour-Aridi et al. demonstrated an ISR occurrence of 9.4%/2 years after CAS,[6] and Pierre Clavel mentioned a 5.2%/1 year occurrence of ISR after CAS.[5] Reported risk factors for ISR after CAS include aging,[1,6,8,12] smoking,[2,23] diabetes mellitus and dyslipidemia,[14,23] women,[12,14,23] hostile neck,[5] and prior neck cancer.[22] Stent-related factors, such as the diameter,[24] length,[16] type of stents (closed or open cell stent),[16-18] and multiple stent use,[12] are also possible risk factors for ISR after CAS.
ISR has three primary causes. First, early postoperative stenosis with plaque protrusion or thrombus on the stent can cause ISR. Second, neointimal hyperplasia caused by non-specific inflammatory responses of blood vessels to the chronic mechanical stimulation of stents can cause ISR.[7] Third, an atherothrombotic clot can cause ISR. At present, standardized criteria and methods for treating ISR are not defined. According to Pourier’s review, PTA is the most common treatment for ISR after CAS, accounting for 57% of post-CAS ISR cases. The other common treatments for ISR after CAS include repeated CAS (21%) and CEA (16%).[19]
CONCLUSION
Conclusions about the optimal intervention for ISR cannot be made yet; however, CEA with stent removal is another good option.[9,19-21,25,26] Guo et al. reported a systematic review that showed no statistically significant differences between redo CAS and CEA in terms of safety, modality, and morbidity.[10] There are also no recommendations for the optimal treatment of repeated ISR case.
Our case required repeated treatment for ISR. After a careful discussion about the optimal treatment, we decided to perform CEA with stent removal after the third occurrence of ISR. If a third CAS had been performed, the lumen might have narrowed because of the thickness of the stent itself and ISR might have reoccurred. CEA was problematic for this patient, because of inadequate collateral flow, and insertion of an internal shunt was needed. The distal end of the stent was at the C2 level, and we were unsure if the space would be adequate for insertion of the internal shunt. As a result, CEA was carried out 13 months after the second CAS.
The structure between the intima and media is maintained because the carotid stent is located inside the intima. In earlier studies, a few perioperative technical difficulties for CEA with stent removal were reported.[9,20,26] The scarred tissue was difficult to dissect. Identifying the right cleavage plane for performing endarterectomy was difficult because the structure of the vessel wall was unclear after chronic inflammation caused by long-term compression.[13] Distal placement of the carotid stent in the internal carotid artery increased the technical difficulties. If repeated CAS is chosen for treating ISR, a repeated CAS with stenting at a high cervical level should be considered so the option for CEA is not eliminated. CEA for the ISR may be a good option to prevent restenosis. Learning the CEA technique for high cervical level lesions may facilitate high lesion ISR cases. CEA with stent removal may be a good option for treating repeated ISR after CAS.
Acknowledgments
The authors would like to thank Enago (www.enago.jp ) for the English language review.
Footnotes
How to cite this article: Takahashi Y, Higashida T, Uchida T, Watanabe S, Kanazawa R. Carotid endarterectomy with stent removal for recurring in-stent restenosis: A case report and literature review. Surg Neurol Int 2022;13:192.
Contributor Information
Yuichi Takahashi, Email: ptaka2013@gmail.com.
Tetsuhiro Higashida, Email: tets018@gmail.com.
Takanori Uchida, Email: tuchida6434@gmail.com.
Saiko Watanabe, Email: s.watanabe@nch.or.jp.
Ryuzaburo Kanazawa, Email: r.kanazawa@nch.or.jp.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Arquizan C, Trinquart L, Touboul PJ, Long A, Feasson S, Terriat B, et al. Restenosis is more frequent after carotid stenting than after endarterectomy: the EVA-3S study. Stroke. 2011;42:1015–20. doi: 10.1161/STROKEAHA.110.589309. [DOI] [PubMed] [Google Scholar]
- 2.Bonati LH, Ederle J, McCabe DJ, Dobson J, Featherstone RL, Gaines PA, et al. Long-term risk of carotid restenosis in patients randomly assigned to endovascular treatment or endarterectomy in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): long-term follow-up of a randomised trial. Lancet Neurol. 2009;8:908–17. doi: 10.1016/S1474-4422(09)70227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonati LH, Gregson J, Dobson J, McCabe DJ, Nederkoorn PJ, van der Worp HB, et al. Restenosis and risk of stroke after stenting or endarterectomy for symptomatic carotid stenosis in the International Carotid Stenting Study (ICSS): Secondary analysis of a randomised trial. Lancet Neurol. 2018;17:587–96. doi: 10.1016/S1474-4422(18)30195-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brott TG, Hobson RW, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11–23. doi: 10.1056/NEJMoa0912321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clavel P, Hebert S, Saleme S, Mounayer C, Rouchaud A, Marin B. Cumulative incidence of restenosis in the endovascular treatment of extracranial carotid artery stenosis: A meta-analysis. J Neurointerv Surg. 2019;11:916–23. doi: 10.1136/neurintsurg-2018-014534. [DOI] [PubMed] [Google Scholar]
- 6.Dakour-Aridi H, Mathlouthi A, Locham S, Goodney P, Schermerhorn ML, Malas MB. Predictors of midterm high-grade restenosis after carotid revascularization in a multicenter national database. J Vasc Surg. 2020;71:1972–81. doi: 10.1016/j.jvs.2019.07.100. [DOI] [PubMed] [Google Scholar]
- 7.de Borst GJ, Ackerstaff RG, Mauser HW, Moll FL. Operative management of carotid artery in-stent restenosis: first experiences and duplex follow-up. Eur J Vasc Endovasc Surg. 2003;26:137–40. doi: 10.1053/ejvs.2002.1916. [DOI] [PubMed] [Google Scholar]
- 8.Eckstein HH, Ringleb P, Allenberg JR, Berger J, Fraedrich G, Hacke W, et al. Results of the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study to treat symptomatic stenoses at 2 years: A multinational, prospective, randomised trial. Lancet Neurol. 2008;7:893–902. doi: 10.1016/S1474-4422(08)70196-0. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez A, Drummond M, McCord S, Garrett HE., Jr Carotid endarterectomy for treatment of in-stent restenosis. J Vasc Surg. 2011;54:1167–9. doi: 10.1016/j.jvs.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Guo Z, Liu C, Huang K, Yu N, Peng M, Starnes BW, et al. Meta-analysis of redo stenting versus endarterectomy for in-stent stenosis after carotid artery stenting. J Vasc Surg. 2021;73:1282–9. doi: 10.1016/j.jvs.2020.07.102. [DOI] [PubMed] [Google Scholar]
- 11.Gurm HS, Yadav JS, Fayad P, Katzen BT, Mishkel GJ, Bajwa TK, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008;358:1572–9. doi: 10.1056/NEJMoa0708028. [DOI] [PubMed] [Google Scholar]
- 12.Khan MA, Liu MW, Chio FL, Roubin GS, Iyer SS, Vitek JJ. Predictors of restenosis after successful carotid artery stenting. Am J Cardiol. 2003;92:895–7. doi: 10.1016/s0002-9149(03)00912-3. [DOI] [PubMed] [Google Scholar]
- 13.King BN, Scher LA, Lipsitz EC. Refractory in-stent restenosis following carotid artery stenting: A case report and review of operative management. Vasc Endovascular Surg. 2009;43:306–11. doi: 10.1177/1538574408327572. [DOI] [PubMed] [Google Scholar]
- 14.Lal BK, Beach KW, Roubin GS, Lutsep HL, Moore WS, Malas MB, et al. Restenosis after carotid artery stenting and endarterectomy: A secondary analysis of CREST, a randomised controlled trial. Lancet Neurol. 2012;11:755–63. doi: 10.1016/S1474-4422(12)70159-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mas JL, Chatellier G, Beyssen B, Branchereau A, Moulin T, Becquemin JP, et al. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355:1660–71. doi: 10.1056/NEJMoa061752. [DOI] [PubMed] [Google Scholar]
- 16.Megaly M, Alani F, Cheng CI, Ragina N. Risk factors for the development of carotid artery in-stent restenosis: Multivariable analysis. Cardiovasc Revasc Med. 2021;24:65–9. doi: 10.1016/j.carrev.2020.09.005. [DOI] [PubMed] [Google Scholar]
- 17.Miyata H, Nakahara I, Ishii A, Ohta T, Sadamasa N, Matsumoto S, et al. Predictors and stroke risk of restenosis after carotid artery stenting. J Neuroendovascular Ther. 2015;9:245–53. [Google Scholar]
- 18.Müller MD, Gregson J, McCabe DH, Nederkoorn PJ, van der Worp HB, de Borst GJ, et al. Stent design, restenosis and recurrent stroke after carotid artery stenting in the international carotid stenting study. Stroke. 2019;50:3013–20. doi: 10.1161/STROKEAHA.118.024076. [DOI] [PubMed] [Google Scholar]
- 19.Pourier VE, de Borst GJ. Technical options for treatment of in-stent restenosis after carotid artery stenting. J Vasc Surg. 2016;64:1486–96. doi: 10.1016/j.jvs.2016.07.106. [DOI] [PubMed] [Google Scholar]
- 20.Reichmann BL, van Laanen JH, de Vries JP, Hendriks JM, Verhagen HJ, Moll FL, et al. Carotid endarterectomy for treatment of in-stent restenosis after carotid angioplasty and stenting. J Vasc Surg. 2011;54:87–92. doi: 10.1016/j.jvs.2010.11.118. [DOI] [PubMed] [Google Scholar]
- 21.Setacci C, de Donato G, Setacci F, Chisci E, Cappelli A, Pieraccini M, et al. Surgical management of acute carotid thrombosis after carotid stenting: A report of three cases. J Vasc Surg. 2005;42:993–6. doi: 10.1016/j.jvs.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 22.Skelly CL, Gallagher K, Fairman RM, Carpenter JP, Velazquez OC, Parmer SS, et al. Risk factors for restenosis after carotid artery angioplasty and stenting. J Vasc Surg. 2006;44:1010–5. doi: 10.1016/j.jvs.2006.07.039. [DOI] [PubMed] [Google Scholar]
- 23.Texakalidis P, Tzoumas A, Giannopoulos S, Jonnalagadda AK, Jabbour P, Rangel-Castilla L, et al. Risk factors for restenosis after carotid revascularization: A meta-analysis of hazard ratios. World Neurosurg. 2019;125:414–24. doi: 10.1016/j.wneu.2019.02.065. [DOI] [PubMed] [Google Scholar]
- 24.Yamagami H, Sakai N, Matsumaru Y, Sakai C, Kai Y, Sugiu K, et al. Periprocedural cilostazol treatment and restenosis after carotid artery stenting: The retrospective study of in-stent restenosis after carotid artery stenting (ReSISteR-CAS) J Stroke Cerebrovasc Dis. 2012;21:193–9. doi: 10.1016/j.jstrokecerebrovasdis.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Yu LB, Yan W, Zhang Q, Zhao JZ, Zhang Y, Wang R, et al. Carotid endarterectomy for treatment of carotid instent restenosis: Long-term follow-up results and surgery experiences from one single centre. Stroke Vasc Neurol. 2017;2:140–6. doi: 10.1136/svn-2017-000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng J, Liu L, Cao Y, Zhang D, Wang R, Zhao J. Carotid endarterectomy with stent removal in management of in-stent restenosis: A safe, feasible, and effective technique. Eur J Vasc Endovasc Surg. 2014;47:8–12. doi: 10.1016/j.ejvs.2013.10.011. [DOI] [PubMed] [Google Scholar]