Abstract
Infectious disease epidemics have become more frequent and more complex during the 21st century, posing a health threat to the general public and leading to psychological symptoms. The current study was designed to investigate the prevalence of and risk factors associated with depression, anxiety and insomnia symptoms during epidemic outbreaks, including COVID-19. We systematically searched the PubMed, Embase, Web of Science, OVID, Medline, Cochrane databases, bioRxiv and medRxiv to identify studies that reported the prevalence of depression, anxiety or insomnia during infectious disease epidemics, up to August 14th, 2020. Prevalence of mental symptoms among different populations including the general public, health workers, university students, older adults, infected patients, survivors of infection, and pregnant women across all types of epidemics was pooled. In addition, prevalence of mental symptoms during COVID-19 was estimated by time using meta-regression analysis. A total of 17,506 papers were initially retrieved, and a final of 283 studies met the inclusion criteria, representing a total of 948,882 individuals. The pooled prevalence of depression ranged from 23.1%, 95% confidential intervals (95% CI: [13.9–32.2]) in survivors to 43.3% (95% CI: [27.1–59.6]) in university students, the pooled prevalence of anxiety ranged from 25.0% (95% CI: [12.0–38.0]) in older adults to 43.3% (95% CI: [23.3–63.3]) in pregnant women, and insomnia symptoms ranged from 29.7% (95% CI: [24.4–34.9]) in the general public to 58.4% (95% CI: [28.1–88.6]) in university students. Prevalence of moderate-to-severe mental symptoms was lower but had substantial variation across different populations. The prevalence of mental problems increased over time during the COVID-19 pandemic among the general public, health workers and university students, and decreased among infected patients. Factors associated with increased prevalence for all three mental health symptoms included female sex, and having physical disorders, psychiatric disorders, COVID infection, colleagues or family members infected, experience of frontline work, close contact with infected patients, high exposure risk, quarantine experience and high concern about epidemics. Frequent exercise and good social support were associated with lower risk for these three mental symptoms. In conclusion, mental symptoms are common during epidemics with substantial variation across populations. The population-specific psychological crisis management are needed to decrease the burden of psychological problem and improve the mental wellbeing during epidemic.
Subject terms: Psychiatric disorders, Psychology
Introduction
The explosive spread of coronavirus disease 2019 (COVID-19) across the world has once again brought infectious disease epidemics into public attention [1]. In fact, several infectious disease epidemics occurred during the 21st century, including severe acute respiratory syndrome (SARS), influenza A subtype H5N1, Zika, Ebola, and Middle East respiratory syndrome coronavirus (MERS-CoV) [2, 3]. These epidemics posed a general public health threat requiring prevention of their spread, promoting public awareness, and educating the public about the diseases.
Facing these large-scale infectious public health events and enormous disruptions to daily life, people are under unprecedented pressure and can experience severe psychological problems, such as depression, anxiety and insomnia [4, 5]. Accumulating studies have investigated the prevalence of mental health problems during infectious disease epidemics in different populations, typically focusing on the general public [6], healthcare workers [7, 8], university students [9], infected survivors [10], and the pregnant women [11]. Recent published meta-analyses also pointed the existence of high prevalence of mental symptoms during COVID-19 among populations including general public and health workers [12, 13]. However, most of these studies included small samples that focused on early stage of COVID-19 rather than the pandemic, and did not investigate the change in mental symptoms as the pandemic progressed.
The risk of psychological symptoms was associated with demographic characteristics, medical conditions, epidemic-related factors, experiencing public health interventions like quarantines, and concern and understanding of the COVID-19 pandemic [14–16]. Recent studies have reported that female and self-perceived illness severity were significantly associated with symptoms of depression, anxiety and insomnia [6]. Participants whose families or friends were confirmed or suspected COVID-19 patients or who experienced quarantine had a higher risk of having symptoms of depression, anxiety, insomnia and acute stress [14]. Decreased physical exercise also was associated with worse mental health during the pandemic [17]. However, the magnitude of the relationship between these factors and the risk of mental health problems generally varies substantially across studies.
Understanding the mental health problems related to infectious disease epidemics and identifying associated risk factors would help to set priorities for public health policies and to implement effective health care interventions [18, 19]. To our knowledge, a comprehensive systematic review of studies investigating the prevalence and factors associated with mental health problems among multiple different populations during epidemics has not been published. Based on these considerations, the current study conducted a systematic review and meta-analysis to examine the prevalence of mental health symptoms across varying populations including the general public, health workers, university students, older adults, infected patients, survivors of infection, and pregnant women. Moreover, we intend to explore potential risk factors associated with mental health problems particularly in relation to anxiety, depression and insomnia.
Methods
This systematic review and meta-analysis followed the Meta-Analyses of Observational Studies in Epidemiology (MOOSE) guidelines [20] (Supplementary Table 1) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21] (Supplementary Table 2). The review protocol was registered in PROSPERO and is available online (CRD42020219530).
Search strategy and selection criteria
We systematically searched the PubMed, Embase, Web of Science, OVID, Medline, Cochrane databases, bioRxiv and medRxiv to identify studies that reported the prevalence of depression, anxiety or insomnia during infectious disease epidemics, including SARS, H1N1, poliomyelitis, Ebola, Zika, Nipah, MERS-CoV, H5N1, and COVID-19 (Supplement 1). The literature search was updated to August 14, 2020. Additionally, we also scanned reference lists of retrieved papers and recent reviews for additional studies that might met the inclusion criteria.
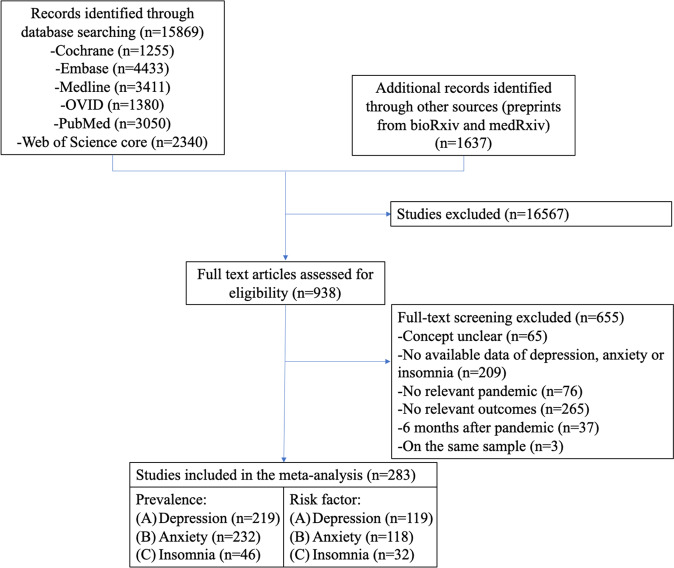
Three authors (Zheng YB, Wang YJ, and Liu XX) independently assessed the articles for their inclusion eligibility. Studies were included if they met the following criteria: (1) observational studies during the above list of infectious disease epidemics, (2) peer-reviewed articles without language restriction that reported the prevalence of depression, anxiety or insomnia symptoms during epidemics, or studies that provide odds ratios (ORs) or raw data that was available to calculate ORs for factors associated with depression, anxiety or insomnia symptoms during these epidemics. The following articles were excluded: (1) case reports, commentaries, conference abstracts, poster presentations, reviews, and dissertations; (2) studies that investigated the prevalence of mental problems more than sixth months after epidemics; (3) no available data to calculate prevalence or ORs of depression, anxiety or insomnia. If the same sample was used in more than one publication, then only the dataset with the most comprehensive information was included to avoid data duplication in the meta-analysis. The process of identifying eligible studies and reasons for exclusion are presented in Fig. 1.
Fig. 1.
The flow chart of study selection.
Data extraction and quality assessment
The following information was extracted from each study according to a prespecified protocol: first author, publication year, research site, type of infectious outbreak, study population, type of study, investigating time, sample size, male percentage, assessment instrument, and prevalence of mental problems (Supplementary Table 3). All data were independently extracted from the eligible studies by six of the authors (YBZ, YJW, YTH, YZ, MNJ, CWY) and subsequently double-checked by two authors (YBZ and YJW).
Four of the authors (YJW, WJL, MNJ and CWY) independently conducted Quality assessments of eligible studies using the Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI, https://jbi.global/critical-appraisal-tools). All discrepancies were resolved by group discussion and consensus. Detailed information on the study quality is shown in Supplementary Table 4.
Definitions
In this meta-analysis, we assessed prevalence of and risk factors associated with depression, anxiety and insomnia symptoms during infectious disease epidemics. Operational definitions of key terms including infectious disease epidemics, mental health problems, populations and risk factors used in the study are presented in Supplementary Table 5.
Data analysis
A random effects model was used to calculate pooled prevalence estimates of any or moderate-to-severe depression, anxiety and insomnia. Pooled prevalence estimates are expressed as mean estimates and 95% confidence intervals (CIs). We used an I2 statistic estimate of ≥50% as an indicator of large statistical heterogeneity. To explore potential sources of heterogeneity, subgroups and meta-regression analysis were conducted when possible using the following variables: population type (general public, health workers, university students, older adults, infected patients, survivors of infection, and pregnant women), type of infectious disease (SARS, COVID-19, and others types including H1N1, poliomyelitis, Ebola, Zika, Nipah, MERS-CoV, H5N1), and across different countries. We also conducted meta-regression analysis of depression, anxiety, and insomnia prevalence during the duration of COVID-19 among different populations.
We used inverse variance weighted random-effects models to pool the log-transformed ORs for factors associated with depression, anxiety, and insomnia. The following dichotomous factors were explored: 1) demographics: sex, age (>40 years vs <40 years), education, marriage, income level, living areas (rural area vs, urban area), smoking, drinking, living alone, emergency experience, 2) medical conditions: physical disorders, mental disorders, 3) epidemic-related factors: suspected or confirmed infected, colleagues or family members infected, frontline workers, close contact with infected patients, epidemic location (high vs low), exposure risk (high vs low), working status (working vs not working), being concerned about epidemics (highly vs not highly), quarantine, 4) potential protective factors: social support (good vs poor), exercise frequency (frequently vs less frequently), preventive behavior (frequently vs less frequently).
Begg’s test was used to assess the possibility of publication bias. Sensitivity analyses were conducted to identify the influence of individual studies on the pooled estimates by excluding each of the studies from the pooled estimate. All of the analyses were calculated using the statistical packages for meta-analysis in Stata 12 software. Values of P < 0.05 were considered statistically significant for all tests.
Results
A total of 15,869 papers were initially retrieved through database searching, and additional 1637 records identified through other preprint resources. After screening titles and abstracts, 938 articles remained to review the full-text for eligibility. Among them, 655 were excluded after full-text screening. Finally, we included 283 eligible studies. Of these eligible studies, 219 studies assessed the prevalence of depression, 232 studies assessed the prevalence of anxiety, and 46 studies assessed the prevalence of insomnia. Moreover, the number of studies that provided data on factors associated with depression was 119, anxiety was 118, and insomnia was 32. An overview of the process of study selection is presented in Fig. 1.
Of the 283 included studies, a total of 948,882 individuals were included in the final analysis including 102 studies (627,452) for the general public, 87 studies (100,363) for health workers, 20 studies (65,495) for students, 10 studies (10,310) for older adults, 26 studies (46,606) for infected patients, 7 studies (1815) for survivors of infection, and 11 studies (15,399) for the pregnant. The number of individuals assessed during COVID-19, SARS, and other types of epidemics was 937,870 (255 studies), 5779 (18 studies), and 4128 (10 studies), respectively. This meta-analysis covered data from 45 countries on six continents, with 122 studies investigating the prevalence of mental problems in China, followed by Italy (n = 17), USA (n = 14), Turkey (n = 12), UK (n = 11), Iran (n = 9), Spain (n = 9), India (n = 8), Brazil (n = 5), Saudi Arabia (n = 5), Korea (n = 5), Germany (n = 4), Mexico (n = 4), Nepal (n = 4), Singapore (n = 4), Australia (n = 3), Canada (n = 3), Pakistan (n = 3), Colombia (n = 2), Greece (n = 2), Ireland (n = 2), Israel (n = 2), Jordan (n = 2), Oman (n = 2), and UAE (n = 2). Albania, Argentina, Austria, Bahrain, Bangladesh, Belgium, Cyprus, Ecuador, France, Guinea, Ibadan, Japan, Malaysia, Portuguesa, Russia, Sri Lanka, Switzerland, Thailand, Vietnam, Zimbabwe each had one study. Additionally, 7 studies performed surveys in multiple countries. The mental health symptoms were assessed based on scales in 280 studies, clinical diagnosis in 2 studies, and both scales and diagnosis in 1 study. Supplement Table 3 provides detailed information about these studies. Supplementary Table 4 presents the quality assessment of the included studies, with a score ranging from 4 to 9.
Prevalence of depression, anxiety and insomnia during epidemics across different populations
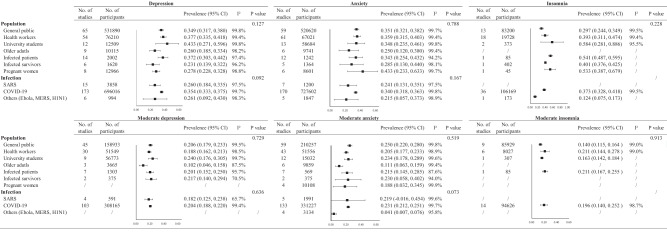
We pooled the prevalence of depression, anxiety and insomnia symptoms in different populations using a random model (Fig. 2 and Supplementary Fig. S1). Although there was no significant difference among different populations, there was some special features of prevalence for the three symptoms. For depression, university students reported the highest pooled prevalence (43.3%, 95% CI: [27.1–59.6]), followed by health workers (37.7%, 95% CI: [33.5–41.8]), infected patients (37.2%, 95% CI: [30.3–44.2]), the general public (34.9%, 95% CI: [31.7–38.0]), pregnant women (27.8%, 95% CI: [22.8–32.8]), and older adults (26.0%, 95% CI: [18.5–33.4]), survivors had the lowest prevalence (23.1%, 95% CI: [13.9–32.2]). For anxiety, pregnant women had highest anxiety during epidemic 43.3%, 95% CI: [23.3–63.3]), followed by health workers (35.9%, 95% CI: [31.5–40.3]), the general public (35.1%, 95% CI: [32.1–38.2]), university students (34.8%, 95% CI: [23.5–46.1]), infected patients (34.3%, 95% CI: [25.4–43.2]), and survivors (28.5%, 95% CI: [13.0–44.0]), older adults had the lowest anxiety (25.0%, 95% CI: [12.0–38.0]). For insomnia symptoms, university students (58.4%, 95% CI: [28.1–88.6]), infected patients (54.1%, 95% CI: [48.7–59.5]), and pregnant women (53.3%, 95% CI: [38.7–67.9]) reported higher insomnia during epidemic, followed by survivors (40.1%, 95% CI: [37.6–42.5]), and health workers (39.3%, 95% CI: [31.1–47.4]), the general public had the lowest insomnia symptoms (29.7%, 95% CI: [24.4–34.9]).
Fig. 2.
Prevalence of depression, anxiety, and insomnia across different populations and types of pandemic.
The prevalence of moderate-to-severe depression (24.0%, 95% CI: [17.6–30.6]) was highest in the university students and lowest in health workers at 18.8% (95% CI: [16.2–21.3]). The general public had the highest prevalence of moderate-to-severe anxiety (25.0%, 95% CI: [23.0–28.0]), while the older adults had the lowest prevalence (11.1%, 95% CI: [6.3–15.9]). Moderate-to-severe insomnia had the largest prevalence in the health workers (21.1%, 95% CI: [14.4–27.8]) and infected patients (21.1%, 95% CI: [16.7–25.5]). Finally, the pooled prevalence of depression, anxiety and insomnia in different types of epidemics also showed no significant difference (Fig. 2 and Supplementary Fig. 2).
Time and regional distribution of prevalence of mental problems during the COVID-19 epidemic
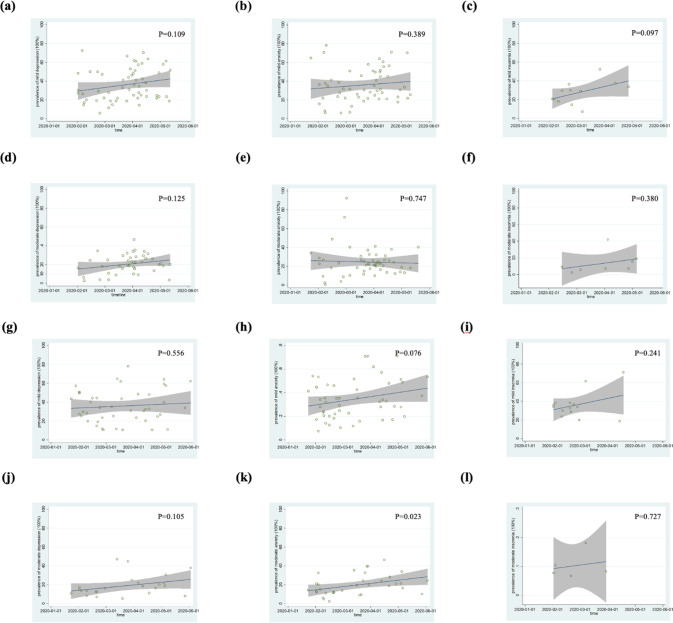
The prevalence of depression, anxiety and insomnia rose during the COVID-19 epidemic among the general public (Fig. 3a–f), health workers (Fig. 3g–i) and university students (Supplementary Fig. S3a–d). In contrast, the prevalence of depression and anxiety symptoms decreased during the COVID-19 epidemic among the infected patients (Supplementary Fig. S3e–h). Although meta-regression analysis showed no statistical significance.
Fig. 3. Meta-regression analysis of prevalence of general public’s and health worker’s depression, anxiety, and insomnia during COVID-19 estimated by time.
General public: (a) depression, (b) anxiety, (c) insomnia, (d) moderate-to-severe depression, (e) moderate-to-severe anxiety, (f) moderate-to-severe insomnia; Health worker: (g) depression, (h) anxiety, (i) insomnia, (j) moderate-to-severe depression, (k) moderate-to-severe anxiety, (l) moderate-to-severe insomnia.
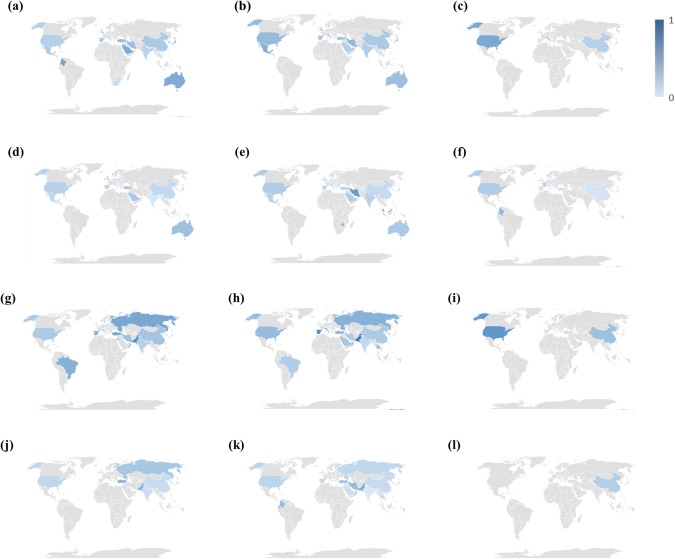
The prevalence of depression, anxiety, and insomnia during the COVID-19 epidemic across these populations within the different countries is presented in Fig. 4 (general public and health workers) and Supplementary Fig. S4 (university students, older adults, infected patients, survivors and the pregnant women). Overall, the prevalence of mental health problems during COVID-19 epidemics varied from countries to countries.
Fig. 4. Prevalence of general public’s and health worker’s depression, anxiety, and insomnia during pandemics across countries.
General public: (a) depression, range: 12.5% (Israel)–66.7% (Jordan); (b) anxiety, range: 23.9% (Saudi Arabia)–71.0% (United Arab Emirates); (c) insomnia, range: 23.2% (China)–56.0% (USA); (d) moderate-to-severe depression, range: 3.5% (India)–36.3% (Australia); (e) moderate-to-severe anxiety, range: 10.9% (Japan)–72.1% (Malaysia); (f) moderate-to-severe insomnia, range: 5.7% (China)–42.0% (Columbia); Health worker: (g) depression, range: 22.5% (India)–78.0% (Jordan); (h) anxiety, range: 17.1% (India)–95.5% (Pakistan); (i) insomnia, range: 18.5% (Oman)–75.2% (Bahrain); (j) moderate-to-severe depression, range: 5.3% (Spain)–47.1% (Turkey); (k) moderate-to-severe anxiety, range: 1.5% (India)–53.5% (Pakistan); (l) moderate-to-severe insomnia, range: 8.3% (Italy)–24.4% (China).
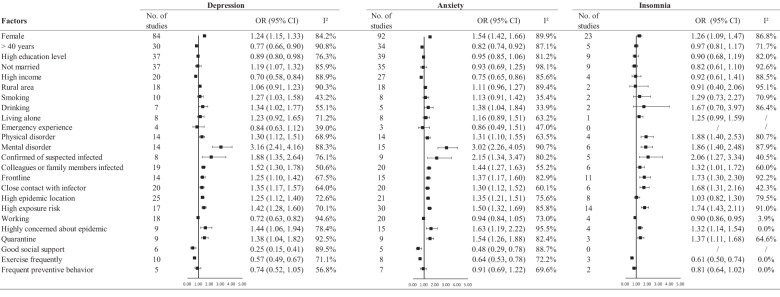
Factors associated with depression, anxiety and insomnia during epidemics
The factors associated with depression, anxiety and insomnia during epidemics are presented in Fig. 5 and Supplementary Fig. S5–7. Overall, females displayed a higher prevalence of all three mental health symptoms; participants who were less than 40 years old or in the high-income level had a lower prevalence of depression and anxiety; participants with a higher education level displayed a lower prevalence of depression, while participants who were not married or who had a habit of smoking had a higher prevalence of depression. In addition, participants who drank also displayed a higher prevalence of depression and anxiety. Other strong associations were found in participants with physical and mental disorders, with confirmed or suspected infection and their colleagues or family members or those having close contact with infected patients. More symptoms occurred in high epidemic rate locations. Remaining home rather than returning back to work during epidemics and quarantine experience were both associated with greater risk of mental health symptoms. Finally, good social support and high exercise frequency were both associated with fewer mental health symptoms.
Fig. 5.
Factors associated with depression, anxiety, and insomnia during pandemic.
Publication bias and sensitivity analysis
The results of the sensitivity analysis revealed that the direction of the results of the analysis did not change after excluding any single study in studies with number over ten (Supplementary Fig. S8). Supplementary Fig. S9 and Supplementary Table 6 showed significant publication bias for the following six areas: 1. moderate-to-severe insomnia in general public (p = 0.016), 2–4. moderate-to-severe depression (p = 0.029), anxiety (p = 0.019), and insomnia during COVID-19 (p = 0.012); 5. exposure risk (p = 0.014) and 6. frequency of exercise (p = 0.020) in the risk of depression. No significant publication bias was found for the other reported risk associations.
Discussion
This systematic review and meta-analysis provided comprehensive quantitative estimates of depression, anxiety and insomnia burdens of seven populations during large-scale infectious disease outbreaks, including the COVID-19 pandemic. To our knowledge, this is the largest and most wide-ranging analysis of its kind to date. Findings indicated that mental health problems were common and had substantial variation among the general public, health workers, university students, older adults, infected patients, infected survivors, and pregnant women. Furthermore, the different populations showed specific mental health problems, such as the main problem was depression and anxiety among university students and health workers, pregnant women had the highest anxiety rates, and university students and infected patients had higher insomnia rates during epidemics. We further explored the risk factors for the three mental health problems and found associations of all three mental health symptoms with being female, and having physical disorders, psychiatric disorders, infection, colleagues or family members infected, experience of frontline work, close contact with infected patients, high exposure risk, highly concerned about epidemics, and quarantine experience. Frequent exercise and good social support were associated with lower risk for all three mental symptoms. Our study indicated specific mental health problems for different populations and suggested aspects of a prevention strategy based on the risk factors analysis.
Different populations such as the general public, health workers, university students, older adults, infected patients, infection survivors, and pregnant women had a tendency but not statistically significant difference in mental health problems, suggesting these psychological problems are frequent during epidemics and should be addressed. Overall, about one third of the general public had the symptoms of depression, anxiety and insomnia in this meta-analysis. Our results were consistent with findings among several large sample cross-sectional studies that investigated risk factors for mental health symptoms during COVID-19 [7, 14, 22–24], SARS [25–27], and other 21st century epidemics [28–30]. Since we found significant emotional distress occurs during public health crises, the importance of preventing and treating mental health problems during the COVID-19 outbreak is clear.
Compared with the general public, health workers had a higher risk for overall depression, anxiety and insomnia symptoms, but displayed a lower risk for moderate to severe depression and anxiety. These findings suggest that health workers are under greater stress during epidemics, but have good command of knowledge and coping strategies to help alleviate mental health problems. Infected patients and the general public shared a similar prevalence of mental problems, which seems paradoxical since most infected patients were late-middle-aged adults, perhaps the infected patients’ responses reflected our additional finding that ORs for mental symptoms were lower in the older than younger adults. In addition, a cohort effect may help explain the phenomenon, considering the prevalence of mental symptoms was ascending among the general public, while decreasing among infected patients, as effective treatments and questions about vaccine efficacy rapidly evolved during the period of this data collection about COVID-19. In this meta-analysis, university students were generally composed of young adults, who have been at high risk of mental health burdens generally during epidemics, and they reported the highest rates of depression, anxiety and insomnia among the seven types of populations. Thus, stratified strategies should be applied to treat different populations during epidemics [18, 31, 32].
The prevalence of mental health problems during COVID-19 were higher than SARS or other types of epidemics. The severe symptoms caused by COVID-19 as well as wide-spread epidemic information during COVID-19 may have led to the high prevalence of these psychological problems. In contrast to SARS and other epidemics, the COVID-19 virus also is more contiguous and spread faster resulting in more mental symptoms among all populations.
The prevalence of mental health symptoms rose during COVID-19 among the general public, health workers, and university students, while the prevalence of mental problems dropped among the infected patients. The increased prevalence of mental problems as COVID infections progressed could reflect the elevated number of infected patients as well as a latency in recognizing mental health problems, as the concerns about physical infection and their sequels become more evident. Moreover, increasing information about ongoing epidemics may largely affect individuals’ mental symptoms. The decreasing prevalence over time of mental symptoms among the infected patients might could be explained by their recovery. In the meantime, mental health problems were different among the different countries in this meta-analysis, which could be postulated by different cultures, severity of epidemic, and strategies applied across countries.
The present study identified several population groups who were likely to develop mental health symptoms. Participants who were infected, or having colleagues or family members infected had a higher risk for all mental health symptoms. The higher risk of mental health symptoms among infected patients during an epidemic may be attributable to their distressing circumstances, physical pain, and adverse effects of medications that are used to treat infections [33]. Participants with colleagues or family members infected experienced more grief [34, 35], and worry and concern about becoming infected themselves, may be quarantined, and may feel stigmatized, all of which may exacerbate psychological distress [36, 37].
Epidemic-related factors such as experience of frontline work, close contact with infected patients or having high exposure risk also increased risk for all three mental health symptoms. People who work in high-risk environments often report more fatigue, health worries, and fear [38]. Therefore, people may understandably feel a threat of becoming infected by being exposed to general patients, thereby affecting their psychological well-being [14, 39]. Being highly concerned about epidemics also increased the risk for all mental health symptoms in this meta-analysis. As earlier findings suggest, exposure to misinformation online can trigger psychological distress [40, 41]. Quarantine experiences were associated with all mental health problems, through hampered access to basic supplies, disrupted information flow, and increased fear and anxiety [15, 37, 42]. Additionally, quarantine experiences also lead to social isolation and a sense of loneliness, especially for geriatric populations who may be less comfortable using online tools [43–45]. All of these epidemic-related stressors might help explain quarantines association with increased mental health risk.
In contrast with the risk factors mentioned above, factors such as frequent exercise and good social support were associated with lower risk for depression and anxiety symptoms [16]. Frequent and high intensity exercise reduces inflammation, which may further help relieve mental health symptoms [46]. Perceived support from the social environment may help resist and effectively cope with the risk factors related to mental health [47]. Our results imply the necessity of exercise and good social support during epidemics, when they may have positive influences on mental health.
In addition, demographic characteristics and medical conditions were associated with mental health symptoms. Participants with a history of mental disorders displayed over three times higher risk for depression and anxiety, and nearly twice as high ORs for insomnia. The experience of epidemics, as a stress, may trigger or exacerbate an individuals’ mental health problems and result in the higher risk for all psychological symptoms [48]. The recent findings also found a bidirectional association between COVID-19 and psychiatric disorders [49], implicating the necessity of monitoring mental health in individuals with psychiatric disorders during epidemics [50]. Physical disorders also showed a higher risk for mental health problems, which could be explained by fundamental physical disorders and restriction of medical assistance during epidemics [51–53]. Also, demographic characteristics such as gender, age, income level, and drinking were associated with two or three mental health symptoms. The results implied stratified strategies should be developed to cope with mental health problems during epidemics.
The current findings also have several limitations. First, the electronic research was conducted before August 2020, and we excluded studies examining outcomes beyond 6-months after infection, thus we do not have findings reflecting after the acute epidemic resolved. Second, mental health symptoms were based on the respondents’ self-reports rather than clinical diagnoses. Third, we preferentially investigated three relatively common main outcomes during the pandemics, depression, anxiety, and insomnia; however, other symptoms such as psychotic or cognitive impairments from these stressful pandemics were not included.
Despite these limitations, this study provides useful information for improving mental health in the face of future epidemics. More immediately, COVID-19 is still a continuing threat for society, and several key actions are needed to reduce COVID-19-related mental health symptoms. First, the governments and authorities need to address mental health symptoms, especially for those who are vulnerable to pandemics. Second, proper public health education with scientific-based information should be advocated. As indicated in this meta-analysis, exercise and social support are both effective ways to reduce negative emotions. Third, community leaders and public health officials should maintain supervision on and provide medical services for physically and psychologically high-risk populations even after COVID-19 since long-lasting impacts of epidemics may exist [39, 54].
Conclusion
In conclusion, this systematic review and meta-analysis specifically focused on the pooled estimates of prevalence of mental health problems during large-scale infectious disease outbreaks. The prevalence of mental health symptoms was about one-third, and moderate-to-severe mental health symptoms was present in about one-fifth of the general public. Additionally, demographic characteristics and medical conditions (e.g., female, physical disorders, psychiatric disorders), as well as epidemic-related factors (e.g., infection, having colleagues or family members infected, experience of frontline work, close contact with infected patients, high exposure risk, highly concerned about epidemics, and quarantine experience) were associated with increased prevalence of all three mental health symptoms. In contrast, frequent exercise and good social support were associated with lower risk for mental health symptoms. Our findings may provide helpful information for policy making through recognition of high-risk populations, and a framework for designing for and improving population-specific strategies to address mental health in infectious disease outbreaks.
Supplementary information
Acknowledgements
GT acknowledges support from the National Institute for Health and Care Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust. GT is also supported by the UK Medical Research Council (UKRI) in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards.
Author contributions
LL, YPB, and YBZ designed the study. YBZ, KY, and YKS conducted data extraction, analysis, drafted the manuscript, and interpreted the results. YKS, YBZ, YMG, XXL, and YTH developed the search strategy and conducted data retrieval. YBZ, YJW, YTH, YZ, MNJ, and CWY screened the abstracts and conducted full-text screening. LL, YPB, TK, KY, and YKS supervised the meta-analysis, contributed to interpreting the results, and revised the manuscript. XC, SZS, NG, YLL, ZW, WJL, JYQ, YBY, AYZ, NZ, MVV, VP, SF, HM, GT, TTF, XL, WY, LS, and JS contributed to discussions. All authors approved the final proof.
Funding
This work was supported by the National Key Research and Development Program of China (Nos. 2021YFC0863700, 2019YFA0706200, and 2019YFC0118502), the National Natural Science Foundation of China [Nos. 81761128036, 81821092, 82171514, 82001404, and 81901345], and PKU-Baidu Fund (no. 2020BD011).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Kai Yuan, Yong-Bo Zheng, Yi-Jie Wang, Yan-Kun Sun.
Contributor Information
Thomas Kosten, Email: kosten@bcm.edu.
Yan-Ping Bao, Email: baoyp@bjmu.edu.cn.
Lin Lu, Email: linlu@bjmu.edu.cn.
Supplementary information
The online version contains supplementary material available at 10.1038/s41380-022-01638-z.
References
- 1.Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7:875–82. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bedford J, Farrar J, Ihekweazu C, Kang G, Koopmans M, Nkengasong J. A new twenty-first century science for effective epidemic response. Nature. 2019;575:130–6. doi: 10.1038/s41586-019-1717-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giesecke J. The truth about PHEICs. Lancet. 2019;S0140-6736:31566–1. doi: 10.1016/S0140-6736(19)31566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan K, Gong Y-M, Liu L, Sun Y-K, Tian S-S, Wang Y-J, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry. 2021;87:4982–98. [DOI] [PMC free article] [PubMed]
- 6.Morin CM, Bjorvatn B, Chung F, Holzinger B, Partinen M, Penzel T, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45. doi: 10.1016/j.sleep.2021.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr. 2020;33:e100259. [DOI] [PMC free article] [PubMed]
- 8.Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alyoubi A, Halstead EJ, Zambelli Z, Dimitriou D. The impact of the COVID-19 pandemic on students’ mental health and sleep in Saudi Arabia. Int J Environ Res Public Health. 2021;18:9344. doi: 10.3390/ijerph18179344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patabendige M, Gamage MM, Weerasinghe M, Jayawardane A. Psychological impact of the COVID-19 pandemic among pregnant women in Sri Lanka. Int J Gynaecol Obstet. 2020;151:150–3. doi: 10.1002/ijgo.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. doi: 10.1016/j.eclinm.2021.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Shi L, Que J, Lu Q, Liu L, Lu Z, et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry. 2021;26:4813–22. doi: 10.1038/s41380-021-01019-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu Y, Su S, Jiang Z, Guo S, Lu Q, Liu L, et al. Prevalence and risk factors of mental health symptoms and suicidal behavior among university students in Wuhan, China during the COVID-19 pandemic. Front Psychiatry. 2021;12:695017. doi: 10.3389/fpsyt.2021.695017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Creese B, Khan Z, Henley W, Corbett A, Vasconcelos Da Silva M, Mills K, et al. Loneliness, physical activity and mental health during Covid-19: a longitudinal analysis of depression and anxiety between 2015 and 2020. Int Psychogeriatr. 2021;33:505–14. [DOI] [PMC free article] [PubMed]
- 18.Yue JL, Yan W, Sun YK, Yuan K, Su SZ, Han Y, et al. Mental health services for infectious disease outbreaks including COVID-19: a rapid systematic review. Psychol Med. 2020;50:2498–513. doi: 10.1017/S0033291720003888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu Q, Liu L, Wang Y, Shi L, Xu Y, Lu Z, et al. Online survey on accessing psychological knowledge and interventions during the COVID-19 pandemic - China, 2020. China CDC Wkly. 2020;2:797–803. doi: 10.46234/ccdcw2020.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cai Q, Feng HL, Huang J, Wang MY, Wang QF, Lu XZ, et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J Affect Disord. 2020;275:210–5. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17:4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–92. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–12. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tang YM, Zhang YY, Li JG, Shen J, Xing YG. Characteristics of neuropsychiatric impairment symptoms in patients with severe acute respiratory syndrome. Chin J Clin Rehabil. 2005;9:208–9. [Google Scholar]
- 27.Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J Trauma Stress. 2005;18:39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elizarraras-Rivas J, Vargas-Mendoza JE, Mayoral-Garcia M, Matadamas-Zarate C, Elizarraras-Cruz A, Taylor M, et al. Psychological response of family members of patients hospitalised for influenza A/H1N1 in Oaxaca, Mexico. BMC Psychiatry. 2010;10:104. doi: 10.1186/1471-244X-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee SM, Kang WS, Cho A-R, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123–7. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keita MM, Taverne B, Sy Savané S, March L, Doukoure M, Sow MS, et al. Depressive symptoms among survivors of Ebola virus disease in Conakry (Guinea): preliminary results of the PostEboGui cohort. BMC Psychiatry. 2017;17:127. doi: 10.1186/s12888-017-1280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhai Y, Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e22. doi: 10.1016/S2215-0366(20)30089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsang HW, Scudds RJ, Chan EY. Psychosocial impact of SARS. Emerg Infect Dis. 2004;10:1326–7.. doi: 10.3201/eid1007.040090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bromet EJ, Atwoli L, Kawakami N, Navarro-Mateu F, Piotrowski P, King AJ, et al. Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. Psychol Med. 2017;47:227–41. doi: 10.1017/S0033291716002026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang B, Liu X, Liu Y, Xue C, Zhang L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. 2014;14:623. doi: 10.1186/1471-2458-14-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Person B, Sy F, Holton K, Govert B, Liang A. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10:358–63. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018;60:248–57. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- 39.Zheng YB, Sun J, Liu L, Zhao YM, Yan W, Yuan K, et al. COVID-19 vaccine-related psychological stress among general public in China. Front Psychiatry. 2021;12:2241. doi: 10.3389/fpsyt.2021.774504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lu S, Reavley N, Zhou J, Su J, Pan X, Xiang Q, et al. Depression among the general adult population in Jiangsu Province of China: prevalence, associated factors and impacts. Soc Psychiatry Psychiatr Epidemiol. 2018;53:1051–61. doi: 10.1007/s00127-018-1568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The Lancet. Social media, screen time, and young people’s mental health. Lancet. 2019;393:611. doi: 10.1016/S0140-6736(19)30358-7. [DOI] [PubMed] [Google Scholar]
- 42.Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. 2020;4:347–9. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jawaid A. Protecting older adults during social distancing. Science. 2020;368:145. doi: 10.1126/science.abb7885. [DOI] [PubMed] [Google Scholar]
- 44.Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5:e62–70. doi: 10.1016/S2468-2667(19)30230-0. [DOI] [PubMed] [Google Scholar]
- 45.Zheng YB, Shi L, Lu ZA, Que JY, Yuan K, Huang XL, et al. Mental health status of late-middle-aged adults in China during the coronavirus disease 2019 pandemic. Front Public Health. 2021;9:643988. doi: 10.3389/fpubh.2021.643988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paolucci EM, Loukov D, Bowdish DME, Heisz JJ. Exercise reduces depression and inflammation but intensity matters. Biol Psychol. 2018;133:79–84. doi: 10.1016/j.biopsycho.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 47.Xu Q, Li S, Yang L. Perceived social support and mental health for college students in mainland China: the mediating effects of self-concept. Psychol Health Med. 2019;24:595–604. doi: 10.1080/13548506.2018.1549744. [DOI] [PubMed] [Google Scholar]
- 48.Shi L, Lu ZA, Que JY, Huang XL, Lu QD, Liu L, et al. Long-term impact of COVID-19 on mental health among the general public: a nationwide longitudinal study in China. Int J Environ Res Public Health. 2021;18:8790. doi: 10.3390/ijerph18168790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu L, Ni SY, Yan W, Lu QD, Zhao YM, Xu YY, et al. Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: a systematic review, meta-analysis and call for action. EClinicalMedicine. 2021;40:101111. doi: 10.1016/j.eclinm.2021.101111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–40. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Y, Duan Z, Ma Z, Mao Y, Li X, Wilson A, et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry. 2020;10:263. doi: 10.1038/s41398-020-00950-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Naser Moghadasi A. One aspect of coronavirus disease (COVID-19) Outbreak in Iran: high anxiety among MS patients. Mult Scler Relat Disord. 2020;41:102138. doi: 10.1016/j.msard.2020.102138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kosir U, Loades M, Wild J, Wiedemann M, Krajnc A, Roskar S, et al. The impact of COVID-19 on the cancer care of adolescents and young adults and their well-being: results from an online survey conducted in the early stages of the pandemic. Cancer. 2020;126:4414–22. doi: 10.1002/cncr.33098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao YM, Liu L, Sun J, Yan W, Yuan K, Zheng YB, et al. Public willingness and determinants of COVID-19 vaccination at the initial stage of mass vaccination in China. Vaccines. 2021;9:1172. doi: 10.3390/vaccines9101172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.