Abstract
Background
This study assessed the diagnostic performance of the 0-hour/1-hour (0/1-h) algorithm to rule in and rule out acute myocardial infarction (MI) in patients presenting to the emergency department (ED) for suspected acute coronary syndrome without ST-segment elevation, as recommended in the 2015 European Society of Cardiology (ESC) guideline.
Methods and Results
Following the Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy (PRISMA-DTA) guidelines, a systematic review was conducted using the PubMed database from inception to March 31, 2020. We included any article published in English investigating the diagnostic performance of the ESC 0/1-h algorithm for diagnosing MI in patients with chest pain visiting the ED. Of 651 studies identified as potentially available for the study, 7 studies including 16 databases were analyzed. A meta-analysis of the diagnostic accuracy of the 0/1-h algorithm using high-sensitivity cardiac troponin I (hs-cTn) with 6 observational databases showed a pooled sensitivity of 99.3% (95% confidence interval [CI] 98.5–99.7%) and a pooled specificity of 90.1% (95% CI 80.7–95.2%). A meta-analysis of the diagnostic accuracy of 10 observational databases of the ESC 0/1-h algorithm using hs-cTn revealed a pooled sensitivity of 99.3% (95% CI 96.9–99.9%) and a pooled specificity of 91.7% (95% CI 83.5–96.1%).
Conclusions
Our results demonstrate that the ESC 0/1-h algorithm can effectively rule in and rule out patients with non-ST-segment elevation MI.
Key Words: 0/1-h algorithm, High-sensitivity troponin, Pooled sensitivity, Pooled specificity, Suspected NSTEMI
Cardiac troponin is a biochemical parameter with well-established validity for the diagnosis of acute myocardial infarction (AMI).1,2 The clinical use of troponin has been studied extensively, and the timing of the measurement of high-sensitivity troponin (hs-Tn) has been well investigated.3,4 Exclusion of myocardial infarction (MI) among patients with chest pain requires serial negative troponin tests conducted at 3- to 6-h intervals. The resulting delay in diagnosing MI affects patient outcomes, while the time required to exclude MI results in emergency department (ED) overcrowding.5,6 The development of hs-Tn assays has led to a shorter time interval until the second assessment of cardiac troponin. This substantially reduces the delay to diagnosis, shortens the length of the ED stay, and lowers costs.7
Among the proposed troponin-based strategies using high-sensitivity cardiac troponin (hs-cTn) testing, the 0-hour/1-hour (0/1-h) algorithm recommended by the European Society of Cardiology (ESC) is widely used to manage chest pain patients without persistent ST-segment elevation.8 The algorithm combines the value of hs-cTn at initial ED presentation and the change in hs-cTn values between 0 and 1 h to triage patients in the ED. The high sensitivity of the ESC 0/1-h algorithm enables physicians to rule out non-ST-segment elevation myocardial infarction (NSTEMI), and its use allows patients to be discharged earlier. This allows healthcare professionals to achieve appropriate resource allocation in the ED. Although several studies have investigated the effectiveness of this algorithm for safely ruling out MI in chest pain patients without ST-segment elevation,9,10 the demographics of the patients in each of the studies differed. Therefore, it is crucial to summarize the current evidence related to the ESC 0/1-h algorithm to examine its effectiveness in the real world.
We conducted a systematic review and meta-analysis of previous studies evaluating the diagnosis of AMI using hs-cTn levels to assess the diagnostic performance of the 2015 ESC guidelines for acute coronary syndrome (ACS) in patients without ST-segment elevation using the 0/1-h algorithm to rule in and rule out AMI at the time of patient presentation to the ED.
Methods
The Japan Resuscitation Council (JRC) ACS Task Force was established to create the JRC 2020 guidelines, and was organized by the Japanese Circulation Society, the Japanese Association of Acute Medicine, and the Japanese Society of Internal Medicine.11 Together, we conducted this review to create a statement related to the 0/1-h algorithm in the JRC guideline. A systematic review and meta-analysis of studies on the diagnosis of AMI in adult patients were performed following the recommendations of the Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy (PRISMA-DTA) guidelines.12
Participants
Studies involving patients presenting to the ED with symptoms suggestive of ACS were included in the analysis.
Study Selection Criteria
Any study published in English investigating the accuracy of the 0/1-h algorithm in diagnosing AMI using hs-cTn was included in the review and meta-analysis, with the exception of case reports/series, comments, animal studies, and studies without original data.
Outcome
The primary outcome was the diagnostic accuracy of the 0/1-h algorithm for AMI. The pooled sensitivity, specificity, and positive and negative likelihood ratios (LRs) were calculated with 95% confidence intervals (CIs).
Search Method to Identify Studies
We conducted a comprehensive electronic search of the PubMed database from its inception to March 31, 2020, using keywords that included “acute coronary syndrome,” “chest pain,” “angina,” “myocardial infarction,” “troponin,” and “emergency department”. The full search strategy is provided in Supplementary Appendixes 1,2. Full papers of studies published in English were searched for, and the reference lists of all eligible studies included in the present and previous systematic reviews were hand-searched to identify additional eligible articles. As relevant studies were identified, the reviewers checked for additional, relevant, and cited articles. Studies on both hs-cTnI and hs-cTnT were evaluated and the efficacy of both types of troponin were evaluated and compared.
Data Extraction
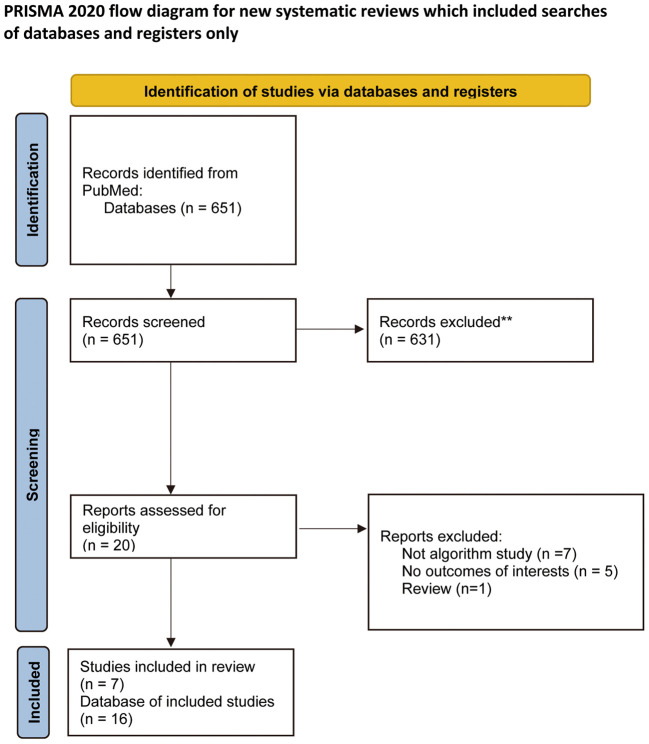
Two reviewers (O.N., K.H.) independently screened the titles and abstracts of all the retrieved bibliographic records. The inclusion and exclusion criteria were applied at each step of the screening process. When no abstract was available, the full text was obtained, unless the article could be confidently excluded based on its title alone. The full text of any article deemed questionable as to whether it should be excluded was examined in full to reduce the likelihood of incorrectly excluding relevant studies. The 2 reviewers independently retrieved the full text of potentially eligible studies (Figure 1).13
Figure 1.
Flowchart of the study selection process.
Decision Process
Two independent reviewers (O.N., K.H.) determined eligibility, assessed quality, and extraction data. Any discrepancies were resolved through discussion with or adjudication by a third reviewer (H.N.).
Quality Assessment
The included studies were assessed for their report quality based on the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 tool.14 According to this assessment tool, 4 domains, namely patient selection, index test, reference test, and flow and timing, were investigated for biases. Two separate investigators (O.N., K.H.) independently assessed the studies. The results of the QUADAS-2 scoring are shown in Figure 2.
Figure 2.
Summary of risk of bias and applicability concerns.
Strategy for Data Synthesis
The pooled sensitivity, specificity, positive and negative predictive values, and positive and negative LRs with 95% CIs were calculated. A bivariate model was used to derive summary effect estimates. A hierarchical summary receiver operating characteristic (HSROC) curve was constructed plotting sensitivity against specificity. The heterogeneity of the studies was graphically evaluated using forest plots. Statistical analysis and construction of the forest plot were performed using RevMan version 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark), and other statistical analyses were performed using MetaDTA: Diagnostic Test Accuracy Meta-Analysis version 2.15 All statistical tests were 2-sided, and P<0.05 was considered statistically significant.
Results
Application of the inclusion and selection criteria to the 651 studies identified as being potentially eligible for the study yielded 7 studies suitable for inclusion, including a total of 16 databases for complete analysis (Figure 1; Tables 1,2).
Table 1.
Characteristics of the 5 Studies Evaluating the Performance of High-Sensitivity Troponin I
| Study | Year | Sample size |
Age (years) |
Prevalence (%) |
Marker | Cut-off | Diagnostic performance (95% CI) |
|---|---|---|---|---|---|---|---|
| Jaeger et al21 | 2016 | 750 | 60 (median) |
13 | Dimension Vista 1500 immunoassay (Siemens Diagnostics) |
Baseline level 5 ng/L and an absolute change within 1 h of 2 ng/L |
Sen: 100% (96.3–100) NPV: 100% (96.1–100) Spe: 95.6% (93.7–97) PPV: 70.4% (60.3–79.2) |
| Pickering et al17 |
2016 | 2,222 | 60 (mean) |
11 | ARCHITECT High Sensitive STAT Troponin I (Abbott Laboratories) |
ESC 0-h/1-h algorithm | Sen: 98.8% (96.4–99.7) NPV: 99.8% (99.3–99.9) Spe: 95.0% (94.0–95.9) PPV: 68.1% (62.6–73.2) |
| Boeddinghaus et al22 |
2017 | 2,828 | 62 (median) |
16 | ARCHITECT High Sensitive STAT Troponin I (Abbott Laboratories) |
ESC 0-h/1-h algorithm | Sen: 98.4% (96.8–99.2) NPV: 99.5% (99–99.8) Spe: 61.3% (59.3–63.2) PPV: 32.5% (30.1–35.1) |
| Boeddinghaus et al16 |
2018 | 1,019 (young) |
ND | 9 | ARCHITECT High Sensitive STAT Troponin I (Abbott Laboratories) |
ESC 0-h/1-h algorithm | Sen: 100% (91.4–100) NPV: 100% (98.5–100) Spe: 93.5% (90.8–95.5) PPV: 58.5% (46.3–69.6) |
| 836 (middle- aged) |
ND | 23 | Sen: 97.9% (92.6–99.4) NPV: 98.5% (94.6–99.6) Spe: 88.9% (85.0–91.9) PPV: 69.6% (60.6–77.1) |
||||
| 973 (old) |
ND | 24 | Sen: 99.3% (96.0–99.9) NPV: 98.9% (94.2–99.8) Spe: 85.8% (82.1–88.8) PPV: 65.3% (57.9–72.0) |
||||
| Twerenbold et al18 |
2018 | 445 (renal disease) |
79 (median) |
32 | ARCHITECT High Sensitive STAT Troponin I (Abbott Laboratories) |
ESC 0-h/1-h algorithm | Sen: 98.6% (95.0–99.8) NPV: 97.4% (90.5–99.4) Spe: 84.4% (79.9–88.3) PPV: 70.8% (64.8–76.2) |
| 2,504 (normal) |
58 (median) |
13 | Sen: 98.5% (96.5–99.5) NPV: 99.7% (99.2–99.9) Spe: 91.7% (90.5–92.9) PPV: 60.7% (57.1–64.2) |
CI, confidence interval; ESC, European Society of Cardiology; ND, not documented; NPV, negative predictive value; PPV, positive predictive value; Sen, sensitivity; Spe, specificity.
Table 2.
Characteristics of the 5 Studies Evaluating the Performance of High-Sensitivity Troponin T
| Study | Year | Sample size |
Age (years) |
Prevalence (%) |
Marker | Cut-off | Diagnostic performance (95% CI) |
|---|---|---|---|---|---|---|---|
| Pickering et al17 |
2016 | 2,222 | 60 (mean) |
9.7 | Fifth-generation High Sensitivity Troponin T (Roche Diagnostics) |
ESC 0-h/1-h algorithm | Sen: 97.1% (94.0–98.8) NPV: 99.5% (99.0–99.8) Spe: 94.6% (93.4–95.5) PPV: 63.4% (57.5–68.9) |
| Mokhtari et al19 | 2017 | 1,167 | 61 (mean) |
19.5 | Roche Cobas e602 (Roche Diagnostics) |
ESC 0-h/1-h algorithm | Sen: 98.3% (94.1–99.8) NPV: 99.5% (98.3–99.9) Spe: 47.7% (44.4–51.0) |
| Shiozaki et al20 | 2017 | 413 | 72 (median) |
13.8 | Fifth-generation High Sensitivity Troponin T (Roche Diagnostics) |
ESC 0-h/1-h algorithm | Sen: 100% (88.0–100) NPV: 100% (96.8–100) Spe: 66.3% (60.2–72.0) PPV: 33.1% (25.1–41.9) |
| Twerenbold et al18 |
2018 | 487 (renal disease) |
79 (median) |
31 | Fourth-generation Elecsys High Sensitivity Troponin T (Roche Diagnostics) |
ESC 0-h/1-h algorithm | Sen: 100.0% (97.6–100.0) NPV: 100.0% (N/A) Spe: 88.7% (84.8–91.9) PPV: 76.5% (70.6–81.6) |
| 2,767 (normal renal function) |
58 (median) |
13 | Sen: 99.2% (97.6–99.8) NPV: 99.8% (99.5–100.0) Spe: 96.5% (95.7–97.2) PPV: 77.1% (73.1–80.7) |
||||
| Boeddinghaus et al16 |
2018 | 1,122 (young) |
45 (median) |
6 | Fourth-generation Elecsys High Sensitivity Troponin T (Roche Diagnostics) |
ESC 0-h/1-h algorithm | Sen: 100% (94.9–100) NPV: 100% (99.6–100) Spe: 97.0% (95.8–97.9) PPV: 66.3% (56.2–75.1) |
| 935 (middle- aged) |
62 (median) |
15 | Sen: 99.3% (96.0–99.9) NPV: 99.8% (99.1–100) Spe: 96.1% (94.5–97.2) PPV: 78.0% (70.5–84.1) |
||||
| 1,066 (older) |
78 (median) |
27 | Sen: 99.3% (97.5–99.8) NPV: 99.4% (97.7–99.8) Spe: 92.7% (90.7–94.3) PPV: 79.0% (73.8–83.5) |
CI, confidence interval; ESC, European Society of Cardiology; N/A, not applicable; NPV, negative predictive value; PPV, positive predictive value; Sen, sensitivity; Spe, specificity.
A meta-analysis of the diagnostic accuracy of the 0/1-h algorithm using hs-cTnI including 6 observational databases (n=7,235 patients in total)16–20 showed a pooled sensitivity of 99.3% (95% CI 98.5–99.7%) and a specificity of 90.1% (95% CI 80.7–95.2%). With an assumed prevalence of AMI of 10% (assuming a maximum number of false positives), the false positive rate was 89 per 1,000 patients (95% CI 43–174) and, assuming a prevalence of 30% (assuming a maximum number of false negatives), the false negative rate was 2 per 1,000 patients (95% CI 1–4; Figure 3 Upper).
Figure 3.
Summary of forest plots.
A meta-analysis of the diagnostic accuracy including 10 observational databases (n=9,188 patients in total)16,17,21,22 showed that the pooled sensitivity and specificity of the ESC 0/1-h algorithm using hs-cTnT were 99.3% (95% CI 96.9–99.9%) and 91.7% (95% CI 83.5–96.1%), respectively. When the prevalence was assumed to be 10% (assuming a maximum of false positives), the false positive rate was 75 per 1,000 patients (95% CI 35–148) and, when the prevalence was assumed to be 30% (assuming a maximum of false negatives), the false negative rate was 2 per 1,000 patients (95% CI 0–9; Figure 3 Lower).
Discussion
This systematic review and meta-analysis evaluated the diagnostic performance of the ESC 0/1-h algorithm with both troponin T and troponin I, and showed that the algorithm could effectively rule in or rule out AMI patients. The most important finding of this report is that the diagnostic performance of the ESC 0/1-h algorithm was extremely high (i.e., both sensitivity and specificity were >90%), indicating the excellent applicability of this algorithm in the real world, especially considering the fact that there is often a trade-off between sensitivity and specificity in clinical diagnostic tests. The ESC 0/1-h algorithm relies on the high sensitivity of troponin assays that detect an increase in troponins 1 h from first blood sampling among patients with NSTEMI. Conversely, very low baseline troponin levels, or the combination of low baseline levels and the absence of a significant increase within 1 h, rule out NSTEMI.8 Therefore, using the ESC 0/1-h algorithm improves the clinical management of patients with suspected NSTEMI and reduces ED crowding and treatment costs due to the associated shortening of the length of ED stay. Furthermore, we found that the diagnostic performance of the algorithm using troponin I was comparable to that of the troponin T algorithm. Although the diagnostic performance between troponin I and T was similar, the numbers of the studies and participants included in the meta-analysis were larger in the case of troponin T. This indicates that using troponin T was more common in the emergency care of patients with chest pain. A previous report showed that the hs-cTnT assay is able to identify the patient group with worse outcomes among patients who tested positive for cTnI.23 Although the availability of troponin T or troponin I depends on the testing resources of each institution, the similar diagnostic performance of both parameters is a desirable result in terms of the standardization of medical services.
Study Limitations
This study has some limitations. First, we used only the PubMed database and restricted the language to English due to the limited resources for this systematic review. Therefore, it is possible that this review missed other important reports on this topic that were written in languages other than English or listed in other databases, such as EMBASE and CENTRAL. Second, most of the studies included in this systematic review were from Western countries,23–25 and hence it is not clear whether these findings are applicable to EDs in Asian countries, such as Japan, where cardiologists sometimes provide the initial care. Therefore, further studies with ethnically diverse populations are needed. Hence, additional verification of the effectiveness of the 0/1-h algorithm in Japan is awaited. Finally, rapid test kits, called point-of-care tests, are used in some facilities to determine test results at the patient’s bedside. Although meta-analyses according to the kits used are required (because test accuracy varies depending on the kit product), there have not been sufficient studies to allow such a meta-analysis to be performed.26 At this stage, it is necessary to understand the diagnostic performance of the test adopted by each institution and then use them clinically.
Conclusions
This meta-analysis confirms the efficacy of the ESC 0/1-h algorithm in ruling in and ruling out AMI in patients with chest pain without ST-segment elevation.
Sources of Funding
Funding was provided by the JRC and the Japanese Circulation Society of Emergency and Critical Care Committee.
Disclosures
T. Matoba is a member of Circulation Reports’ Editorial Team. The other authors declare no conflicts of interest with regard to this article.
Author Contributions
All authors were involved in the study design. O.N. and K.H. identified the studies included in the meta-analysis and analyzed the data. O.N. and K.H. drafted the manuscript. M.K., T. Matoba, Y.T., and H.N. reviewed the manuscript. All authors were involved in data interpretation and discussion. All authors had full access to all the study data (including statistical reports and tables), take responsibility for the integrity of the data and the accuracy of the analysis, and read and approved the final manuscript.
Supplementary Files
Supplementary Appendix 1. Search Strategy Supplementary Appendix 2. PICOST
Acknowledgments
The authors thank Morio Aihara and the staff at the Japan Council for Quality Health Care (Minds Tokyo GRADE Center) for their help with the GRADE approach.
References
- 1. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al.. Fourth universal definition of myocardial infarction. Eur Heart J 2019; 40: 237–269. [DOI] [PubMed] [Google Scholar]
- 2. Danese E, Montagnana M.. An historical approach to the diagnostic biomarkers of acute coronary syndrome. Ann Transl Med 2016; 4: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al.. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients with Unstable Angina/Non-ST-elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol 2007; 50: e1–e157. [DOI] [PubMed] [Google Scholar]
- 4. Alpert JS, Thygesen K, Antman E, Bassand JP.. Myocardial infarction redefined: A consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J 2000; 21: 1502–1513. [DOI] [PubMed] [Google Scholar]
- 5. Sun BC, Hsia RY, Weiss RE, Zingmond D, Liang LJ, Han W, et al.. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med 2013; 61: 605–611.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hoot NR, Aronsky D.. Systematic review of emergency department crowding: Causes, effects, and solutions. Ann Emerg Med 2008; 52: 126–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al.. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009; 361: 858–867. [DOI] [PubMed] [Google Scholar]
- 8. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al.. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 267–315. [DOI] [PubMed] [Google Scholar]
- 9. Reichlin T, Schindler C, Drexler B, Twerenbold R, Reiter M, Zellweger C, et al.. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012; 172: 1211–1218. [DOI] [PubMed] [Google Scholar]
- 10. Twerenbold R, Boeddinghaus J, Mueller C.. Update on high-sensitivity cardiac troponin in patients with suspected myocardial infarction. Eur Heart J 2018; 20: 2–10. [DOI] [PubMed] [Google Scholar]
- 11. Welsford M, Nikolaou NI, Beygui F, Bossaert L, Ghaemmaghami C, Nonogi H, et al.. Part 5: Acute coronary syndromes: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2015; 132(Suppl 1): S146–S176. [DOI] [PubMed] [Google Scholar]
- 12. McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM, PRISMA-DTA Group, et al.. Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA 2018; 319: 388–396. [DOI] [PubMed] [Google Scholar]
- 13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al.. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al.. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155: 529–536. [DOI] [PubMed] [Google Scholar]
- 15. Patel A, Cooper N, Freeman S, Sutton A.. Graphical enhancements to summary receiver operating characteristic plots to facilitate the analysis and reporting of meta-analysis of diagnostic test accuracy data. Res Synth Methods 2021; 12: 34–44. [DOI] [PubMed] [Google Scholar]
- 16. Boeddinghaus J, Nestelberger T, Twerenbold R, Neumann JT, Lindahl B, Giannitsis E, et al.. Impact of age on the performance of the ESC 0/1 h-algorithms for early diagnosis of myocardial infarction. Eur Heart J 2018; 39: 3780–3794. [DOI] [PubMed] [Google Scholar]
- 17. Pickering JW, Greenslade JH, Cullen L, Flaws D, Parsonage W, Aldous S, et al.. Assessment of the European Society of Cardiology 0-hour/1-hour algorithm to rule-out and rule-in acute myocardial infarction. Circulation 2016; 134: 1532–1541. [DOI] [PubMed] [Google Scholar]
- 18. Twerenbold R, Badertscher P, Boeddinghaus J, Nestelberger T, Wildi K, Puelacher C, et al.. 0/1-Hour triage algorithm for myocardial infarction in patients with renal dysfunction. Circulation 2018; 137: 436–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mokhtari A, Lindahl B, Schiopu A, Yndigegn T, Khoshnood A, Gilje P, et al.. A 0-hour/1-hour protocol for safe, early discharge of chest pain patients. Acad Emerg Med 2017; 24: 983–992. [DOI] [PubMed] [Google Scholar]
- 20. Shiozaki M, Inoue K, Suwa S, Lee CC, Chikata Y, Ishiura J, et al.. Utility of the 0-hour/1-hour high-sensitivity cardiac troponin T algorithm in Asian patients with suspected non-ST elevation myocardial infarction. Int J Cardiol 2017; 249: 32–35. [DOI] [PubMed] [Google Scholar]
- 21. Jaeger C, Wildi K, Twerenbold R, Reichlin T, Gimenez MR, Neuhaus JD, et al.. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am Heart J 2016; 171: 92–102.e1–5. [DOI] [PubMed] [Google Scholar]
- 22. Boeddinghaus J, Nestelberger T, Twerenbold R, Wildi K, Badertscher P, Cupa J, et al.. Direct comparison of 4 very early rule-out strategies for acute myocardial infarction using high-sensitivity cardiac troponin I. Circulation 2017; 135: 1597–1611. [DOI] [PubMed] [Google Scholar]
- 23. Lee CC, Huang SS, Yeo YH, Hou YT, Park JY, Inoue K, et al.. High-sensitivity-cardiac troponin for accelerated diagnosis of acute myocardial infarction: A systematic review and meta-analysis. Am J Emerg Med 2020; 38: 1402–1407. [DOI] [PubMed] [Google Scholar]
- 24. Burgos LM, Trivi M, Costabel JP.. Performance of the European Society of Cardiology 0/1-hour algorithm in the diagnosis of myocardial infarction with high-sensitivity cardiac troponin: Systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care 2021; 10: 279–286. [DOI] [PubMed] [Google Scholar]
- 25. Chiang CH, Chiang CH, Lee GH, Gi WT, Wu YK, Huang SS, et al.. Safety and efficacy of the European Society of Cardiology 0/1-hour algorithm for diagnosis of myocardial infarction: Systematic review and meta-analysis. Heart 2020; 106: 985–991. [DOI] [PubMed] [Google Scholar]
- 26. Boeddinghaus J, Nestelberger T, Koechlin L, Wussler D, Lopez-Ayala P, Walter JE, et al.. Early diagnosis of myocardial infarction with point-of-care high-sensitivity cardiac troponin I. J Am Coll Cardiol 2020; 75: 1111–1124. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix 1. Search Strategy Supplementary Appendix 2. PICOST