Abstract
Introduction:The rate of cesarean sections has been continuously increasing in most industrialized countries in recent years. It has been observed that the rate of cesarean sections has increased in the last thirty years and is now between 0.4 and 65%. A significant percentage of women, ranging from 1-20%, request a caesarean section without a medical indication.
Aim:The aim of this study is to systematically review the available international literature concerning the phenomenon of tocophobia leading to woman`s desire for a caesarean section.
Methods: The methodology followed, included an advanced search in various scientific databases and retrieval of the relevant quantitative studies.
Results:We found a total of seven papers, all in English, which examined the correlation between tocophobia and women’s desire for a caesarean section.
Conclusions:One of the primary reasons behind women’s desire to give birth through a caesarean delivery is the pathological fear associated with the labor process, known under the scientific term “tocophobia”. According to the findings of this review, the prevalence of tocophobia ranged between 7-25% among primiparous women and 7.7-16.25% among multiparous ones. Approximately 7-18.6% of women with tocophobia asked for an elective cesarean section without any medical indication. Clinical treatment of tocophobia is required when the condition has a negative impact on the pregnant woman’s quality of life and her bond with the embryo, as well as when it affects her decision regarding the method of childbirth.
Keywords:tocophobia, fear of birth, desire for caesarean section, childbirth.
INTRODUCTION
Vaginal childbirth is the most appropriate way to give birth, while cesarean section (CS) is a risky procedure, being therefore reserved for clinical cases where serious medical contraindications for a vaginal birth are present. However, over the past few years an increased preference for CS has been documented, as shown by the equal increase in couples' requests for a CS, despite the absence of any medical indication for this procedure (1-3).
In recent years, the rate of cesarean sections has been continuously increasing in most industrialized countries (4-6). Since 1985, the World Health Organization set the ideal rate of cesarean sections between 10% and 15% (7). The rate of cesarean sections has constantly risen in the last three decades and is now largely varying between 0.4% and 40% (8). Due to maternal request without medical indication, the rate of caesarean sections is 1-2% of all births in the United Kingdom, 3% in the USA and 20% in China (9).
Greece continues to hold the lead in caesarean sections due to the percentage of caesarean sections performed, which is estimated to be around 50-65% (10). The main reasons behind this phenomenon are the various childbirth challenges that are often unnecessarily endured by women and existence of previous births via caesarean section. Notably, the corresponding percentage is 30% in the US, while the European average is 25% (10). It has been determined that physicians were motivated to perform CSs for financial and convenience incentives (10).
The most common factors that may lead a pregnant woman to request a CS for non-medical reason include the belief that, by undergoing this procedure, the baby will suffer less, the existence of a previous experience of birth via CS and the fear of pain induced by vaginal delivery (1, 11-13).
The feeling of fear is quite usual during pregnancy, with an estimated percentage of 80% of pregnant women showing signs of stress with regard to labor pain but also to the safety and health risks of the process (1, 14). These types of fear do stand to reason and the majority of women are able to express and control these feelings by being well-informed about the birth process, discussing their worries with other women who have already experienced childbirth and seeking advice from a midwife or doctor (1). In some cases, however, fear results in tocophobia and it is estimated that 3% of women develop post-traumatic stress disorder (PTSD) after childbirth (1). This rate increases in women at high risk of developing psychological problems and postpartum PTSD symptoms may include the revival of childbirth and nightmares of the event (1, 15).
Tocophobia is a type of particular phobia – a stress disorder in which people suffer from an unjustified fear of a particular object or situation. Its symptoms can involve sleeping disorders, panic attacks, nightmares, depression and persistence in having a CS (1). Feelings of fear of the unknown, losing control, losing their privacy, previous sexual abuse, fear of pain and fear for the baby's health are reasons that may trigger the onset of tocophobia (1).
In most cases, women who choose to give birth via CS appear to suffer from tocophobia, which is the fear of giving birth (11, 15). The majority of those who suffer from this form of phobia express a pathological fear of giving birth. Often, they do not wish to get pregnant, regardless of the fact that they want to build a family, and they express their option for CS in order to avoid giving birth naturally. Tocophobia can be either primary, occurring in women who have never gone into labor, or secondary, in women who have had a previous traumatic birth experience (1, 11-13).
Primary tocophobia usually develops during adolescence, notwithstanding the fact that it can also appear after a woman has become pregnant. It can be noticed in young girls and women who have been sexually assaulted or raped. In these cases, the recurrence of the trauma experience can be initiated during physical examinations performed during pregnancy and labor (14, 15). Secondary tocophobia is usually the result of previous traumatic labor experiences; however, it can also be noticed among women who have had previous unproblematic births, and also in those who have had either miscarriages or unsuccessful fertility treatments (13-15).
It is important for women with tocophobia to receive treatment to ensure that both the mother and child are healthy. Thus, it is essential that these women receive counselling from their midwife and doctor in collaboration with a psychologist or psychiatrist. It is believed that a psychologist or a psychiatrist will be able to assist these women to express their fear and acknowledge the reasons behind the development of the disorder (1, 15, 16).
As previously mentioned, it has been noticed that in the last few years the rate of cesarean sections has increased worldwide (9), which is mainly due to changes in the mother’s and fetus’ profiles and an increase in the number of pregnant women who choose CS as the preferable way to give childbirth without any medical implications (1, 11, 12).
Aim
The aim of the present study was to systematically review the available international literature concerning the association between the phenomenon of tocophobia and women`s desire for a caesarean section without any medical indication.
METHODS
Search and selection strategy
Papers included in the present review were limited to English and Greek publications, with restrictions for the publication year. Electronic databases of PubMed, Scopus, PsycINFO and CINAHL were searched from 2005 up to 2021. Only primary quantitative studies written in English were considered relevant to our review based on the following inclusion criteria: a) studies including samples of pregnant women with low risk and singleton pregnancy who requested a caesarean section for non-medical reasons; b) articles written in English; and c) time of publication between 2005 and 2021. We used the following search terms: ”tocophobia”, ”childbirth fear”, ”cesarean section on maternal request”, and ”cesarean section and elective cesarean section”.
Quality assessment of included studies
The quality of included studies was assessed by using the Effective Public Health Practice Project (EPHPP) quality assessment tool, including assessment of study design, selection and allocation bias, confounders, blinding, and methods of data collection, withdrawals/drop-outs and analysis (19). In addition, there was an overall quality rating assigned to each study: where no weak ratings were assigned, the quality was deemed to be ‘strong’; one weak rating was labelled ‘moderate’, and two or more weak ratings resulted in the paper being assessed as ‘weak’. Studies rated as ‘weak’ were excluded from analysis.
Data extraction and analysis
Data was extracted into causes and predisposing factors of tocophobia and a woman`s desire for a CS. Moreover, population characteristics as well as pregnancy and birth related aspects from the relevant studies were described.
RESULTS
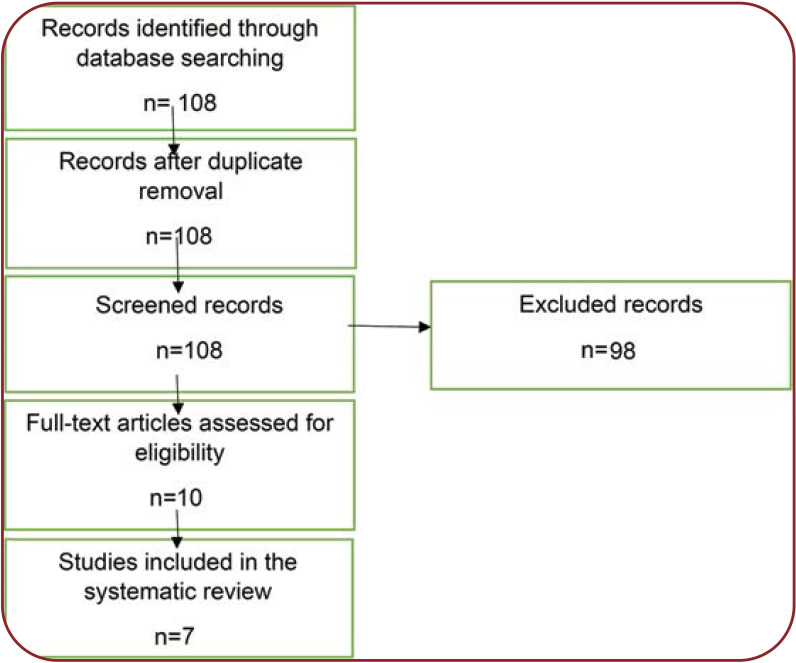
The initial search generated 108 titles. Titles and abstracts were examined for relevance to the review objective. After the assessment of titles and abstracts, 98 references were excluded because they were apparently not relevant to the objective of the present study. Finally, seven articles remained for inclusion (Figure 1).
In the process of searching through data bases and evaluating their content, seven articles were found to assess the correlation between tocophobia and women’s desire to have a CS (with no medical indication). We present them all below in a chronological order.
In 2006, Rouhe’s research team conducted a study regarding tocophobia, specifically looking at factors that play a role in its manifestation and in the choice of a particular mode of delivery. The sample consisted of 1 400 pregnant women who visited Helsinki University Hospital as outpatients. The authors used the Wijma Delivery Expectancy/ Experience Questionnaire (W-DEQ) as well as the visual analogue scale (VAS) to estimate the severity of childbirth fear. Their findings showed that tocophobia more commonly occurred among women who were going through their first pregnancy, with a median (range) score of 4.7 (0-10), which was significantly higher than that of parous women with the median score of 3.2 (0-10). Severe fear of childbirth (FOC) (W-DEC score ≥100) was observed in 7.0% of nulliparous women and in 7.7% of parous women. Cesarean section was the preferred mode of delivery for 8.1% of all subjects and these women scored higher on fear (W-DEC 87.6±26.5, VAS median 7.0) than those who preferred vaginal delivery (W-DEC 61.8±18.7, VAS median 2.7). Moreover, women with a previous CS scored higher on fear (W-DEC 73.2±23.5, VAS 5.1) than parous women without any previous CS (W-DEC 63.3±20.8, VAS 2.9) (20).
In 2006, Nieminen, Stephansson and Ryding looked at the relationship between tocophobia and the practice of CS on maternal request in a cross-sectional study with a sample of 1 635 Swedish women at various stages of pregnancy. Wijma's questionnaire was used for the calculation of tocophobia (W-DEQ). The study results showed that a small percentage of women (only 5.7%) had symptoms of pathological tocophobia (W-DEC ≥100), in addition to another 15.6% who reported intense fear (W-DEC ≥85) regarding the upcoming birth. A larger proportion of parous women (16.5%) showed intense fear (W-DEC ≥85) compared to nulliparous women (14.8%), but there was no correlation between the level of fear and gestational age. Results showed that parous women with a previous CS were more likely to have a higher mean W-DEQ score compared to women with a previous vaginal delivery (76.6 and 57.5, respectively). Additionally, women who had previously experienced either a vacuum extraction or forceps delivery were more afraid of their delivery than parous women with no experience in instrumental delivery (mean W-DEQ 65.6 and 59.5, respectively). Finally, the study results showed that 7.3% of pregnant women would prefer to give birth with a cesarean section; they had a higher mean W-DEQ score (88.8) than women who preferred vaginal delivery (W-DEQ score 60.6) (21).
In 2012, a retrospective case-control study conducted by Sydsjo et al investigated the obstetric outcomes for women with FOC who had received counseling during pregnancy comparatively to women without FOC. The study population included 17 969 pregnant women who attended the ANC (Swedish Antenatal Care) clinics during 2001-2007 and gave birth in Linkoping University Hospital. A total of 516 women who were referred for psychosocial obstetrics and gynecology to Linkoping University Hospital, after having been diagnosed with severe fear of childbirth based on DSM-IV, were first included in the index group; but after excluding women who were referred to Linkoping University Hospital but had given birth in other hospitals as well as those with late miscarriages, only 353 women with FOC remained in the index group. The reference group comprised 579 women without FOC who had given birth on the same day in Linkoping University Hospital. Antenatal and delivery records for all women were manually reviewed with respect to the following variables: age, civil status, occupation, body mass index, smoking habits, parity, pain relief methods and previous pregnancies and complications. The results showed that a CS was more commonly chosen by women who belonged to the group suffering from tocophobia (16.5%) comparatively to those without any significant FOC (9.6%) (22).
In 2015, Elsa Lena Ryding et al studied FOC and its relation to caesarean delivery. The researchers carried out a longitudinal cohort study using a sample of 6 422 pregnant women from Northern Europe, particularly Belgium, Iceland, Denmark, Estonia, Norway and Sweden. Tocophobia was measured using the Wijma questionnaire. The study revealed that pregnant women suffering from tocophobia were more likely to give birth by caesarian delivery. Particularly, a dose-response relationship between the level of FOC and CS was noticed. The likelihood of emergency CS increased with the level of FOC in both primiparous (adjusted OR 1.46 [95% CI 1.05.2.05]) and multiparous women. There was no difference in the prevalence of fetal distress, dystocia, breech presentation, exhausted mother, or other medical indications for cesarean delivery between women with or without severe fear of childbirth delivery. A total of 11.3% of primiparous women and 10.9% of multiparous ones had severe FOC (W-DEQ ≥85). The percentage of women with tocophobia who opted for a CS, without any medical indication for the procedure, was 16.7% among primiparous women and 31,7% among multiparous ones (23).
In 2015, Hege Therese Storksen et al conducted a cohort study investigating the fear of childbirth and its role as a predictive factor for women’s preference for elective CS. The sample consisted of 1 789 women from Norway and data was collected with the use of questionnaires filled out at 17 and 32 weeks of pregnancy and at eight weeks postpartum. The mean age of the women was 31 (range 18-45) years). Forty nine percent of women were primiparous and 99% were married or cohabiting with the father’s child. Eight percent of women showed symptoms of tocophobia with a Wijma questionnaire score of >85. In the study sample, 75% of women had a normal vaginal delivery, 11% instrumental vaginal delivery, while 9% delivered by emergency caesarean section and 5% by elective CS. Fear of childbirth was observed among 16% of women with poor social support, 33% of those with combined anxiety and depression and 28% of women with previous negative overall birth experience. In addition, among women with FOC, 32.8% had a preference for elective cesarean section and 12.7% delivered by elective CS. Fear of childbirth was strongly associated with preference for cesarean delivery, whereas the association with delivery by elective CS was weaker. Interestingly, women with a high educational level were less likely to have a preference for elective CS than those with a low to moderate educational level. Finally, the majority (87%, 117/134) of women with FOC did not undergo an elective CS (24).
In 2018, a study conducted by Henriksen, Borgen, Rislokken and Lukasse in Norway investigated FOC and its relation to women’s choices regarding their preferred method of delivery. Their cohort study included 2 145 Norwegian women and used the Wijma questionnaire. A cut–off >85 was used to define FOC. Among the total number of participants to the study, 258 (12%) reported fear of giving birth. In addition, those with FOC were less educated, more often smokers and more frequently reported symptoms of depression and prior experiences of abuse. Significantly, more women with fear of giving birth preferred CS when asked during pregnancy (18.6%) compared to those without FOC (5.2%). In conclusion, the study showed that 12% of subjects reported fear of giving birth and only 24.9% of participants who reported fear of giving birth had counselling at their hospital. (25).
Lastly in 2018, a cross-sectional study carried out by Demsar et al used a sample of 191 pregnant women of whom 90% were primiparous; also, 75% of all participants reported low to moderate levels of tocophobia, whereas 25% showed high or very high levels of FOC. Participants attended childbirth and parenting classes between June and September 2014 and were asked to fill out several questionnaires regarding depression (CES-D), anxiety (STAI X1 κατ X2), life satisfaction (SWLS) and delivery expectancy/experience (W-DEQ). Moderate FOC was present in more than half of all pregnant women (53.4%), high or very high fear in 23.1% and pathological fear in 1.6% of participants. Regarding the relationship between experiencing FOC and the preferred mode of delivery, the study showed that the majority of participants (86%) would choose vaginal delivery if they had a choice, 6% of subjects did not have a preferred mode of delivery, whereas 7% of those with the highest level of FOC wished to have a cesarean section (26).
DISCUSSION
The aim of our review was to study the contribution of tocophobia in women’s desire to have an elective CS when there was no medical indication for the procedure.
Childbirth is one of the most important periods in a woman’s life, considering the fact that it is a rather painful experience, and the process that surrounds the birth of a baby inevitably causes some stress to parturient women (26). However, when that stress transforms into intense fear it is capable of having a negative impact, not only on the woman’s mental state (27, 28) but also on the labor process itself (27, 28). According to the literature review conducted above, the primary reason for experiencing tocophobia is a CS on maternal request without it being necessary for medical reasons (20-26).
Caesarean section is a very important surgical procedure in the medical field of obstetrics, which is used when serious complications arise during either pregnancy or birth, and it is proven to be lifesaving for both the mother and fetus. Moreover, CS refinement has resulted in a significant reduction of perinatal mortality. However, in recent times the number of caesarean sections performed on maternal request has increased, despite not being medically necessary. There are various reasons behind this rise in caesareans, which are related to not only women’s social and cultural backgrounds but also differences between each country’s healthcare system (26, 28-30).
One of the primary reasons behind women’s desire to give birth through a caesarean delivery is the pathological fear associated with the labor process, known under the scientific term of “tocophobia”. According to the findings of the present review, the prevalence of tocophobia ranged between 7-25% among primiparous women and 7.7-16.25% among multiparous ones. Approximately 7-18.6% of women with tocophobia ask for an elective CS without a medical indication. It was also found that FOC was more commonly occurred among primiparous women (20-26).
In 2008, Rouche et al explored the correlation between overall mental health of women likely to show signs of intense tocophobia. The authors found that those who showed symptoms of intense fear regarding childbirth had twice as many mental health issues as the remaining subjects and were more likely to express the desire of giving birth via CS (20). The results of the cited research revealed that tocophobia was an issue more commonly seen among women going through their first pregnancy, specifically during its last stage. Moreover, women who had a CS with their previous pregnancy were at higher risk of developing tocophobia. Finally, the results of their study showed that women who suffered from intense FOC were more likely to request a CS (20).
Another study that looked into the correlation between the manifestation of tocophobia and the co-existence of other mental disorders showed that fear of labor process was often associated with other individual symptoms of perinatal anxiety such as fear of potential complications during delivery, fear of lack of a supportive environment during birth and doubt in the woman’s capability to carry out a vaginal birth (1).
Another issue that has been of great interest to many researchers has to do with the factors that lead to the manifestation of intense tocophobia in certain women. The study conducted by Stoll et al in 2017 revealed that one of women’s main concerns regarding natural childbirth, which could potentially lead to symptoms of tocophobia, regarded the circumstances under which vaginal deliveries were carried out. Moreover, women are worried about losing control of their own body during delivery, especially since it is a common notion that the labor process is a rather painful experience. Women tend to request a CS with the aim of avoiding such circumstances (31).
Perhaps the most important reason for the manifestation of tocophobia lies behind women’s fear of the pain that is associated with the labor process. Pain is a subjective condition, which seems to be perceived in different ways by each individual. It has been proven that fear of pain is capable of affecting the way in which a woman experiences labor pains in each stage of the labor process and therefore, the choice or demand of a pregnant woman to have a CS is a completely personal decision (32-36). Besides, each woman’s experience of the labor process is in itself subjective: some women see it as an accomplishment of which they are proud, whereas for others it is a traumatic experience characterized by trauma, loss of control, fear, pain and anxiety (37-40). The way in which a woman experiences the labor process has to do with her unique personality. Specifically, women with lower self-esteem are afraid that a vaginal delivery will have a negative impact on their body and view labor as a degrading process (20-26, 29); they are also more likely to resort to having a CS. In contrast, women with a more assertive personality are more likely to insist on a vaginal delivery, since they would be more willing to withstand the pain and all that it involves (23, 41-45).
Finally, Handelzalts et al (2011) looked into the psychological and demographic factors that related to the tendency of some women to request giving birth via CS. The only factors that were found to be associated with a higher percentage of women requesting a CS included age, the method of conception and fear of the labor process. In particular, older age, use of assisted reproductive technologies and experience of symptoms of tocophobia were found to be associated with a higher percentage of caesarean sections (32).
Clinical treatment of tocophobia is required when the condition has a negative impact on the pregnant woman’s quality of life and her bond with the embryo as well as when it affects her decision regarding the method of childbirth (21, 32, 33, 46-51).
CONCLUSIONS
In our review we found that one of the primary reasons behind women’s desire to give birth through a caesarean delivery was the pathological fear associated with the labor process, known under the scientific term of “tocophobia”. According to the findings of this review, the prevalence of tocophobia ranged between 7-25% among primiparous women and 7.7-16.25% among multiparous ones. Approximately 7-18.6% of women with tocophobia asked for an elective CS without a medical indication. Overall, it should be noted that medical professionals must clearly explain to women all consequences that are involved in each of the options (vaginal delivery /cesarean section), so that the final decision would be made to the benefit of both the mother and child. Clinical treatment of tocophobia is required when the condition has a negative impact on the pregnant woman’s quality of life and her bond with the embryo as well as when it affects her decision regarding the method of childbirth.
Conflict of interests: none declared.
Financial support: none declared.
FIGURE 1.
Flow-diagram of the search and selection process
Contributor Information
Dimitrios KANELLOPOULOS, Department of Midwifery, University of West Attica, Greece.
Kleanthi GOUROUNTI, Department of Midwifery, University of West Attica, Greece.
References
- 1.Mylonas I, Friese K. Indications for Risks of Elective Cesarean Section. Deutch Arztebl Int. 2015;122:489–495. doi: 10.3238/arztebl.2015.0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quinlivan JA, McGowan L. How do we help women become less fearful of birth? J Psychosom Obstet Gynaecol. 2019;40:175. doi: 10.1080/0167482X.2019.1604354. [DOI] [PubMed] [Google Scholar]
- 3.Long Q, Kingdon C, Yang F, et al. Prevalence of and reasons for women's, family members', and health professionals' preferences for cesarean section in China: a mixed-methods systematic review. PLoS Med. 2018;15:e1002672. doi: 10.1371/journal.pmed.1002672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moran PS, Normand C, Gillen P, et al. Economic implications of reducing caesarean section rates – analysis of two health systems. PLoS One. 2020;15:e0228309. doi: 10.1371/journal.pone.0228309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ionescu CA, Ples L, Banacu M, et al. Present tendencies of elective caesarean delivery in Romania: Geographic, social and economic factors. J Pak Med Assoc. 2017;67:1248–1253. [PubMed] [Google Scholar]
- 6.Handelzalts JE, Fisher S, Sadan O et al. Object relations, unconscious defences and fear of childbirth, as reflected in maternal-request caesarean section. J Reprod Infant Psychol. 2017;35:91–102. doi: 10.1080/02646838.2016.1253832. [DOI] [PubMed] [Google Scholar]
- 8.Althabe F, Sosa C, Belizán JM, et al. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth. 2006;33:270–277. doi: 10.1111/j.1523-536X.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- 9.Blustein J, Liu J. Time to consider the risks of caesarean delivery for long term child health. BMJ. 2015;350:h2410. doi: 10.1136/bmj.h2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mossialos E, Allin S, Karras K, et al. An investigation of Caesarean sections in three Greek hospitals: the impact of financial incentives and convenience. Eur J Public Health. 2005;15:288–295. doi: 10.1093/eurpub/cki002. [DOI] [PubMed] [Google Scholar]
- 11.Dodd JM, Crowther CA, Grivell RM, et al. Elective repeat caesarean section versus induction of labour for women with a previous caesarean birth. Cochrane Database Syst Rev 2017. [DOI] [PMC free article] [PubMed]
- 12.Eide KT, Morken NH, Bærøe K. Maternal reasons for requesting planned cesarean section in Norway: a qualitative study. BMC Pregnancy Childbirth. 2019;19:102. doi: 10.1186/s12884-019-2250-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pontiki G, Drakopoulou M, Apostolara P. Scheduled Caesarean section as a method of childbirth: a descriptive review. Hellenic Magazine of Nursing Science. 2017;10:15–20. [Google Scholar]
- 14.Karlström A. Women's self-reported experience of unplanned caesarean section: Results of a Swedish study. Midwifery. 2017;50:253–258. doi: 10.1016/j.midw.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Olieman RM, Siemonsma F, Bartens MA, et al. The effect of an elective cesarean section on maternal request on peripartum anxiety and depression in women with childbirth fear: a systematic review. BMC Pregnancy Childbirth. 2017;17:195. doi: 10.1186/s12884-017-1371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindstad Løvåsmoen EM, Nyland Bjørgo M, et al. Women's preference for caesarean section and the actual mode of delivery – comparing five sites in Norway. Sex Reprod Health. 2018;16:206–212. doi: 10.1016/j.srhc.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 17.Schantz C, de Loenzien M, Goyet S, et al. How is women's demand for caesarean section measured? A systematic literature review. PLoS One. 2019;14:e0213352. doi: 10.1371/journal.pone.0213352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kingdon C, Downe S, Betran AP. Women's and communities' views of targeted educational interventions to reduce unnecessary caesarean section: a qualitative evidence synthesis. Reprod Health. 2018;15:130. doi: 10.1186/s12978-018-0570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rouhe H, Salmela-Aro, K, Halmesmäki E, et al. Fear of childbirth according to parity, gestational age, and obstetric history. BJOG: An International Journal of Obstetrics & Gynaecology. 2008;116:67–73. doi: 10.1111/j.1471-0528.2008.02002.x. [DOI] [PubMed] [Google Scholar]
- 21.Nieminen K, Stephansson O, Ryding EL. Women’s fear of childbirth and preference for cesarean section – a cross-sectional study at various stages of pregnancy in Sweden. Acta Obstetricia et Gynecologica Scandinavica. 2009;88:807–813. doi: 10.1080/00016340902998436. [DOI] [PubMed] [Google Scholar]
- 22.Sydsjo G, Sydsjo A, Gunnervik A, et al. Obstetric outcome for women who received individualized treatment for fear of childbirth during pregnancy. Acta Obstetricia et Gynecologica Scandinavica. 2011;91:44–49. doi: 10.1111/j.1600-0412.2011.01242.x. [DOI] [PubMed] [Google Scholar]
- 23.Ryding EL, Lukasse M, Parys AS, et al. Fear of Childbirth and Risk of Cesarean Delivery: A Cohort Study in Six European Countries. Birth. 2015;42:48–55. doi: 10.1111/birt.12147. [DOI] [PubMed] [Google Scholar]
- 24.Størksen HT, Garthus-Niegel S, Adams SS, et al. Eberhard-Gran M. Fear of childbirth and elective caesarean section: a population-based study. BMC Pregnancy Childbirth. 2015;15:221. doi: 10.1186/s12884-015-0655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henriksen L, Borgen A, Risløkken J, et al. Fear of birth: Prevalence, counselling and method of birth at five obstetrical units in Norway. Women and Birth. 2018;33:97–104. doi: 10.1016/j.wombi.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Demšar K, Svetina, M, Verdenik I., et al. Tokophobia (fear of childbirth): prevalence and risk factors. Journal of Perinatal Medicine. 2018;46:151–154. doi: 10.1515/jpm-2016-0282. [DOI] [PubMed] [Google Scholar]
- 27.Jomeen J, Martin CR, Jones C, et al. Tokophobia and fear of birth: a workshop consensus statement on current issues and recommendations for future research. J Reprod Infant Psychol. 2021;39:2–15. doi: 10.1080/02646838.2020.1843908. [DOI] [PubMed] [Google Scholar]
- 28.Badaoui A, Kassm SA, Naja W. Fear and Anxiety Disorders Related to Childbirth: Epidemiological and Therapeutic Issues. Curr Psychiatry Rep. 2019;21:27. doi: 10.1007/s11920-019-1010-7. [DOI] [PubMed] [Google Scholar]
- 29.Sys D, Kajdy A, Baranowska B, et al. Women's views of birth after cesarean section [published online ahead of print, 2021 Oct 5]. J Obstet Gynaecol Res 2021. [DOI] [PubMed]
- 30.Striebich S, Mattern E, Ayerle GM. Support for pregnant women identified with fear of childbirth (FOC)/tokophobia – a systematic review of approaches and interventions. Midwifery. 2018;61:97–115. doi: 10.1016/j.midw.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 31.Stoll KH, Hauck YL, Downe S, et al. Preference for cesarean section in young nulligravid women in eight OECD countries and implications for reproductive health education. Reproductive Health. 2017;14:116. doi: 10.1186/s12978-017-0354-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Handelzalts JE, Fisher S, Lurie S, et al. Personality, fear of childbirth and cesarean delivery on demand. Acta Obstetricia et Gynecologica Scandinavica. 2011;91:16–21. doi: 10.1111/j.1600-0412.2011.01287.x. [DOI] [PubMed] [Google Scholar]
- 33.Asselmann E, Garthus-Niegel S, Martini J. Personality impacts fear of childbirth and subjective birth experiences: A prospective-longitudinal study. PLoS One. 2021;16:e0258696. doi: 10.1371/journal.pone.0258696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sioma-Markowska U, Żur A, Skrzypulec-Plinta V, et al. Causes and frequency of tocophobia - own experiences. Ginekol Pol. 2017;88:239–243. doi: 10.5603/GP.a2017.0045. [DOI] [PubMed] [Google Scholar]
- 35.Habek D. Tocophobia: Is It Being Treated Surgically? Psychiatr Danub. 2020;32:447–448. [PubMed] [Google Scholar]
- 36.Smith V, Gallagher L, Carroll M, et al. Antenatal and intrapartum interventions for reducing caesarean section, promoting vaginal birth, and reducing fear of childbirth: An overview of systematic reviews. PLoS One. 2019;14:e0224313. doi: 10.1371/journal.pone.0224313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhuk SI, Shchurevska OD. Maternal psychosocial stress and labor dystocia. Wiad Lek. 2020;73:1334–1338. [PubMed] [Google Scholar]
- 38.Takács L, Mlíková Seidlerová J, Čepický P. Souvisí postoje žen k těhotenství, porodu a mateřství s délkou porodu? [Are womens attitudes towards pregnancy, childbirth and motherhood associated with length of labour? ]. Ceska Gynekol. 2017;82:462–472. [PubMed] [Google Scholar]
- 39.Freedman SA, Reshef S, Weiniger CF. Post-traumatic stress disorder and postpartum depression and their reported association with recent labor and delivery: a questionnaire survey cohort. Int J Obstet Anesth. 2020;43:18–24. doi: 10.1016/j.ijoa.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 40.Goutaudier N, Bertoli C, Séjourné N, et al. Childbirth as a forthcoming traumatic event: pretraumatic stress disorder during pregnancy and its psychological correlates. J Reprod Infant Psychol. 2019;37:44–55. doi: 10.1080/02646838.2018.1504284. [DOI] [PubMed] [Google Scholar]
- 41.Hantoushzadeh S, Shariat M, Moradi R, et al. Personality traits of volunteer females of normal vaginal delivery or cesarean section based on HEXACO's personality model: a comparison study. Arch Gynecol Obstet. 2020;301:387–392. doi: 10.1007/s00404-019-05378-4. [DOI] [PubMed] [Google Scholar]
- 42.Khooban H, Asadi Yoonesi M. Comparing the Personality Traits and Childbirth-related Beliefs of Two Groups of Women undergoing Vaginal Delivery and Cesarean Section. Journal of Midwifery and Reproductive Health. 2021;9:2613–2620. [Google Scholar]
- 43.Schaal K, Fehm T, Helbig M, et al. The Influence of Personality and Anxiety Traits on Birth Experience and Epidural Use in Vaginal Deliveries – A Cohort Study. Women & Health. 2020;60:1141–1150. doi: 10.1080/03630242.2020.1802640. [DOI] [PubMed] [Google Scholar]
- 44.Field T. Postnatal anxiety prevalence, predictors and effects on development: A narrative review. Infant Behav Dev. 2018;51:24–32. doi: 10.1016/j.infbeh.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 45.Soh YX, Razak NKBA, Cheng LJ, et al. Determinants of childbirth self-efficacy among multi-ethnic pregnant women in Singapore: a structural equation modelling approach. Midwifery. 2020;87:102716. doi: 10.1016/j.midw.2020.102716. [DOI] [PubMed] [Google Scholar]
- 46.O'Connell MA, Khashan AS, Leahy-Warren P, et al. Interventions for fear of childbirth including tocophobia. Cochrane Database Syst Rev 2021. [DOI] [PMC free article] [PubMed]
- 47.Moghaddam Hosseini V, Nazarzadeh M, Jahanfar S. Interventions for reducing fear of childbirth: a systematic review and meta-analysis of clinical trials. Women Birth. 2018;31:254–262. doi: 10.1016/j.wombi.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 48.O'Connell MA, O'Neill SM, Dempsey EK, et al. Interventions for fear of childbirth (tocophobia). The Cochrane Database of Systematic Reviews 2019. [DOI] [PMC free article] [PubMed]
- 49.Webb R, Bond R, Romero-Gonzalez B, et al. Interventions to treat fear of childbirth in pregnancy: A systematic review and meta-analysis. Psychological Medicine. 2021;51:1964–1977. [Google Scholar]
- 50.Ahmadi L, Karami S, Faghihzadeh S, et al. Effect of couples counseling based on the problem-solving approach on the fear of delivery, self-efficacy, and choice of delivery mode in the primigravid women requesting elective cesarean section. Preventative Care in Nursing & Midwifery Journal. 2018;7:32–40. [Google Scholar]
- 51.Irmak Vural P, Aslan E. Emotional freedom techniques and breathing awareness to reduce childbirth fear: A randomized controlled study. Complementary Therapies in Clinical Practice. 2019;35:224–231. doi: 10.1016/j.ctcp.2019.02.011. [DOI] [PubMed] [Google Scholar]