Abstract
Introduction
Early defibrillation within minutes increases survival after in-hospital cardiac arrest (IHCA). However, early defibrillation is often not achieved even though automated external defibrillators (AEDs) are available. We aimed to investigate how AEDs were used and the barriers and facilitators for successful use.
Methods
We conducted unannounced, full-scale in-situ simulations of IHCAs in hospital wards with an AED. A debriefing followed the simulations. The simulations and debriefings were video recorded, and the debriefings were transcribed for subsequent qualitative analysis about the AED use.
Results
We conducted 36 unannounced in-situ simulations, and an AED was used in 98% of simulations. It was decided to collect an AED after a median of 62 (31; 123) seconds, the AED arrived after 99 (82; 146) seconds, were attached after 188 (150; 260) seconds, and the first shock were delivered after 221 (181; 301) seconds from time of cardiac arrest diagnosis. We identified three main domains related to barriers and facilitators of AED use: teamwork, knowledge, and transfer. Frequent reasons for successful use of an AED were recent resuscitation course, previous experience, and leadership. Reasons for unsuccessful use were doubt about responsibility, lack of knowledge, and lack of contextualized training.
Conclusion
During unannounced simulated IHCAs, time to defibrillation was often > 3 minutes. Most of the delay occurred after the AED was collected. Non-technical skills and contextualized training were among the main perceived barriers to AED usage. Facilitators for successful use included recent training, previous experience, and successful leadership.
Keywords: In-hospital cardiac arrest, In-situ simulation, Automated external defibrillator
Introduction
Survival after in-hospital cardiac arrest (IHCA) remains low at 20–30% and has remained unchanged over the last decade.1., 2., 3., 4., 5. Early defibrillation for shockable rhythm increases survival.6., 7., 8., 9. Automated external defibrillators (AEDs) may contribute to earlier defibrillation while awaiting the arrival of the cardiac arrest team and a manual defibrillator.10., 11. In Scandinavian countries, 90% of cardiac arrests occur outside of the intensive care unit where AEDs may be the only option for early defibrillation.12., 13. However, early defibrillation is often not achieved although AEDs are available.5., 6., 14. The reasons for the inadequate usage of AEDs are unknown.10., 15., 16.
Due to the unpredictability of time and place of cardiac arrests, it is difficult to investigate what happens during the first few minutes where an AED may be used. Simulations in a simulation center or planned in-situ simulations may not give an accurate assessment due to the artificial environment and the opportunity for preparation.17., 18. As such, the use of unannounced, full-scale in-situ simulations with debriefings provide an opportunity to investigate clinical practice during the first minutes of a cardiac arrest and the reasons for successful or unsuccessful use of an AED.
Accordingly, we aimed to investigate barriers and facilitators for successful use of AEDs during unannounced in-situ simulated cardiac arrests in hospital wards.
Material and methods
Study design
This study was a prospective, multicenter, observational study utilizing full-scale, unannounced in-situ simulated cardiac arrests to investigate clinical performance in a realistic setting using the clinical equipment.
Ethics
The Ethical Committee in the Central Denmark Region assessed the study and deemed it exempt from individual informed consent (j.no. 141/2017). The study was approved by the Danish Data Protection Agency (j.no. 1-16-02-367-18). Hospital administrations gave permission to conduct the study. All participants were given written information by e-mail before and during the study period and were informed that participation was voluntary, and that individual participation and performance would not be disclosed to the management. To ensure patient safety during simulations, we monitored emergency calls in the hospitals and canceled/interrupted the simulations in case of other emergencies or extraordinary activity.
Setting
The study was conducted in four hospitals in the Central Denmark Region. Simulations were performed during day (9.00–15.00) and night (16.00–00.00) seven days a week and were conducted in hospital wards with AEDs. A debriefing followed all simulations. We aimed to conduct four simulations in each department (workday daytime, workday night, weekend daytime, weekend night).
Participants were hospital ward staff on duty e.g., physicians, nurses, nurse assistants, and the cardiac arrest team. All hospitals used designated cardiac arrest teams with pre-allocated roles that generally consisted of at least a nurse anesthetist, an anesthesiologist, a physician (internal medicine/cardiologist), and two orderlies.19 There were no exclusion criteria regarding individuals as we aimed to reflect clinical practice. Hospital departments were eligible if the department had access to an AED. Intensive care, pediatric, and psychiatric departments were excluded. In case of more eligible departments at hospitals than needed for the study, departments were selected based on bed availability.
The in-situ simulations took place in a patient/examination room assigned by the nurse manager on the day. No other staff knew the time, location, or scenario. Research staff attempted to set up and prepare in the room quickly and quietly to minimize the risk of clinicians noticing. A full-body manikin (Resusci Anne QCPR AED with Airway Head, Laerdal Medical, Stavanger, Norway) was placed in a hospital bed. The manikin was dressed in patient garments and had an intravenous access.
Scenario
A patient call for a nurse/nurse assistant was activated in the room. The arriving nurse/nurse assistant was briefed with a short patient story: 60-year-old (35-year-old in gynecology/obstetric and oncology departments and 85-year-old in the geriatric department) female patient, Anne, has been admitted to observation for [illness related to the department e.g., pneumonia]. She is not severely affected given the condition. However, she is now experiencing chest pain and called for help. After the outbreak of COVID-19, it was added that the patient had been tested for COVID-19 and did not have COVID-19. Participants were required to wear facemasks, but not full personal protective equipment.
The nurse/nurse assistant was instructed to act as in a real situation and access the patient. The manikin was unconscious with no breathing and presented with ventricular fibrillation when a defibrillator was connected. Ventricular fibrillation was present until the cardiac arrest team had delivered two shocks. There was sinus rhythm and return of spontaneous circulation at the subsequent rhythm analysis. The simulation ended when sinus rhythm was detected. If sinus rhythm was not detected, the simulation ended three minutes after sinus rhythm was achieved. In a few cases, sinus rhythm was achieved after one shock by the cardiac arrest team due to time constraints and long response time of the cardiac arrest team.
During the simulation, participants could access the patient record (printed version of electronic record) with a history, standard tests e.g., blood pressure, saturation, blood samples, electrocardiogram, and chest x-ray. Participants could perform actions as they would in a real situation, e.g., administering intravenous medication, intubating the manikin, and performing echocardiography (images and description then provided in printed version). Participants had to retrieve and use all their normal equipment and utilities, including the AED in the department. To allow defibrillation of the manikin, ShockLink (Laerdal Medical, Stavanger, Norway) was connected to the AED/defibrillator by a research assistant. Regular defibrillation electrodes were used. There was no help nor feedback during the simulations. However, if participants performed an action correctly and asked for the result e.g., checked for breathing and asked if the patient was breathing, they were given an answer e.g., the patient is not breathing.
Debriefing
After each in-situ simulation, we conducted a semi-structured debriefing for all participants lasting 15–25 minutes. The debriefing guide was based on PEARLS20., 21. and included themes related to AED use. The framework consisted of four phases: reaction, description, analysis, and summary. During the initial part of the analysis phase, we used plus-delta,22 and strived subsequently to use advocacy-inquiry23 where appropriate. The entire debriefing was conducted openly and allowed for emerging themes from participants.
Data collection
The in-situ simulations were video recorded from two angles. The cameras (GoPro Hero 5 Black, San Mateo, CA, USA) were placed in opposite corners of the room and captured 180-degree video. Data regarding actions performed were obtained from the video recordings. An extra camera was used during the debriefing to ensure sound quality. The camera was placed in a chest harness on a research assistant to alter position as needed. Afterward, the debriefing was transcribed verbatim for subsequent thematic analysis.
The starting point for time measurements was the time of diagnosis of cardiac arrest unless otherwise stated.6., 24. As previously described, electrode placement was assessed by placing a measuring tape forming an X-Y coordinate system on the manikin.25 Electrode placement was photographed and compared to the position recommended by the European Resuscitation Council.26 Correct placement of AED electrodes was defined as within 5 cm of the recommended position according to previous studies.25., 27., 28., 29. Distance to the AED was measured with a measuring wheel from the doorstep of the patient room to the location of the AED by the shortest possible route.
Outcomes measures
The primary outcome was ward staff’s perceived facilitators and barriers for the use/non-use of AED from the debriefings. Secondary outcomes were A) proportion of simulations with the use of an AED, B) time to decision to retrieve AED, C) time to arrival of AED, D) time to AED electrode attachment, E) time to first AED shock, F) safety during shock delivery, G) no-flow time during the use of AED, H) correct electrode placement.
Qualitative analysis
Debriefings were analyzed using a qualitative approach with the researchers as active interpreters with continued awareness of their own preconceptions and backgrounds.30 Using inductive thematic analysis, three researchers (MS, KGL, KK) independently coded six debriefings inductively to develop a coding framework by consensus. A single researcher (MS) used the coding framework to code remaining debriefings, constantly allowing emerging themes to the framework. Halfway through, three debriefings were coded by the same three researchers to ensure continued agreement. Subsequently, codes were merged and arranged into themes for further interpretation. Themes related in any way to the use or non-use of an AED and issues related to AEDs were extracted inductively for interpretive thematic analysis.31., 32.
Statistics
Normally distributed data are presented as mean (standard deviation), and non-normally distributed data are presented as median (1st quartile; 3rd quartile). Categorical data are presented as percentages (number). Normality was determined by histograms and QQ-plots. Data were analyzed using R-statistics (version 3.4.0, R Core Team 2017, R Foundation for Statistical Computing, Vienna, Austria). We did not perform a sample size calculation but intended to include 60 in-situ simulations.
Results
We conducted 36 in-situ simulations from July 2018 to December 2020 of which 6 simulations were partial (interrupted due to emergency calls). Moreover, 30 attempted simulations were canceled: 8 due to COVID-19, 7 due to lack of capacity in wards, 12 due to acute patients, and 3 due to other reasons. Data collection was stopped prematurely due to the COVID-19 pandemic. Participants’ demographics are presented in the Appendix.
Quantitative data
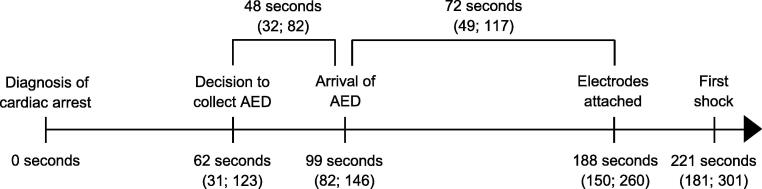
Ward staff used an AED before the arrival of the cardiac arrest team in 92% (n = 33) of simulations, an AED was used by the cardiac arrest team in 6% (n = 2) of the simulations, and an AED was not used at all in 1 simulation. The average distance to the AED was 31.9 (16.4) meters, and none of the AEDs were placed in a locked location. The AED models used were Lifepak CR+ (Physio-Control) in 17% (n = 6) of simulations, Lifepak CR2 (Physio-Control) in 53% (n = 19), Lifepak 1000 (Physio-Control) in 17% (n = 6), Lifepak 20 (Physio-Control) in AED mode in 11% (n = 4), and no AED in 3% (n = 1). The cardiac arrest team used a manual defibrillator in 81% (n = 29) of simulations. The median time to first shock was 221 (181; 301) seconds and the timeline for AED usage is shown in Fig. 1.
Fig. 1.
Data presented as median (Q1; Q3). For time measurements the starting point was time of diagnosis of cardiac arrest. The time measures presented above the timeline are median time interval between actions as marked. Time to first shock included time to first shock by either AED (n = 35) or manual defibrillator (n = 1).
The no flow time during electrode placement was 6 (0; 10) seconds. The right electrode was placed correctly in 47% (n = 17) simulations (median distance from recommended position: 5.1 (3.4; 10.1) cm), and the left electrode was placed correctly in 6% (n = 2) simulations (median distance from recommended position: 10.5 (8.0; 12.3) cm). Both electrodes were never placed correctly. The misplacement of the right electrode was too medial (22%, n = 8), too lateral (14%, n = 5), and/or too caudal (36%, n = 13), whereas the left electrode was placed too medial (72%, n = 26), too caudal (86%, n = 31), and/or too cranial (3%, n = 1).
In total, 148 rhythm analyses were performed, and 6 times the staff failed to defibrillate the manikin (5 times with an AED, 1 time with a manual defibrillator). Safety and no-flow time during rhythm analysis and defibrillation are presented in Table 1.
Table 1.
Safety and no-flow time during rhythm analysis and defibrillation.
|
AED (n = 112)a |
Manual defibrillator (n = 36)b | |
|---|---|---|
| Safety during shock delivery | ||
| Verbal warning | 82% (n = 88) | 89% (n = 31) |
| Visual warning (gestures) | 18% (n = 19) | 34% (n = 12) |
| Verifies all stand clearc | 25% (n = 27) | 71% (n = 25) |
| All stand clear | 85% (n = 91) | 100% (n = 35) |
| Oxygen kept at distance | 79% (n = 79)g | 86% (n = 30) |
| Chest compressions during charging (manual defibrillators) | – | 71% (n = 25) |
| Peri-shock pause (seconds) | 23 (20; 25) | 7 (5; 19) |
Data presented as percentages (n) or median (Q1; Q3).
Five rhythm analyses without subsequent defibrillation.
One rhythm analysis without subsequent defibrillation.
The person delivering shock looks to verify that all other staff stands clear when delivering shock.
Seven defibrillations without an oxygen supply.
Qualitative data
Analysis of the debriefings identified three domains related to the use/non-use of AEDs during the simulations: A) teamwork (including teaming [ad hoc team formation and teamwork]33) (Table 2), B) knowledge (Table 3), and C) transfer (Table 4). Each domain consisted of several themes.
Table 2.
Themes related to teamwork.
| Theme | |
|---|---|
| Responsibility | When AED use was delayed, there was often doubt about who was responsible for the use/attachment of the AED. “But I think, when it [AED] then got here, the responsibility sort of disappeared” (nurse D38-1) “Who is it, that has, eh, the responsibility of the AED?” (nurse D19-1) “If you arrive with the AED for a cardiac arrest, then perhaps it’s also a job to open it and attach it. Because it [AED] didn’t have anybody, there was no ownership of it [AED] there on the table.” (physician D40-1) |
| Leadership | The presence of a team leader who either took the responsibility of the AED or delegated this to another person facilitated the use of the AED. “I just think we were… again had a clear allocation of roles” (nurse D28-2) “Well, I brought it [the AED]. I was told to get the emergency cart - I got a clear order to do that - and I think it was nice to know straight away what I was supposed to do when I got here.” (nurse D33-2) Opposite the lack of a team leader who keeps the overview during the simulation resulted in ineffective use of an AED. [Debriefer: It [AED] beeps for a long time, you have to push the button] “Well, I didn’t notice it. But I think we lacked a person, who kept focus on it [the AED]” (nurse D38-2) |
| Communication | Lack of communication about AED arrival was mentioned as a reason for the delayed attachment of the AED. “Or say’now it [the AED] is here’ at least. The part about we should say something, just like when you get a message and say ‘now I’m doing it’, it [the AED] arrives, then we should say ‘I got it [the AED]’” (nurse D15-1) Loud and clear communication was mentioned as a positive factor during defibrillation. “I think it was good that [name of nurse] kept saying ‘All clear, oxygen clear’, well, she spoke loudly.” (nurse D6-4) |
Table 3.
Themes related to knowledge.
| Theme | |
|---|---|
| Organizational knowledge | Often, the cardiac arrest team members did not know the hospital had AEDs available to be used before the arrival of the manual defibrillator. “Do you have an AED here?!” (physician, A4-1) “I don’t think I’ve seen it [AED] before” (physician, D26-1) Both ward staff and the cardiac arrest team members described several challenges operating the AED. “Well, I fumbled with it [AED], and then ehmmmm, yeah, how did I open it? I think I was in doubt whether the whole box should just have been opened, and I panicked a little, and then I think I probably did not press ‘on’” (nurse, D12-3) “It took time before I realized that, ehm, I just had to pull out those wires…” (nurse, D20-5) |
| Training | Recently completed resuscitation courses or other forms of teaching or review of resuscitation procedures were often mentioned as a reason for effectively retrieving and applying an AED. “It hasn’t been that long ago since I been to a basic resuscitation course, and I just remember it [AED-use] from there” (nurse, D37-6) “I just think it was because we’ve talked about it [the AED]. We’ve talked about that we all know where the AED is, and if we are a couple of people, someone would pick up the AED, someone the emergency box, and someone calls the cardiac arrest team while someone is doing [chest compressions].” (nurse D14-4) |
| Transferable knowledge | Previous experience from clinical cardiac arrest and/or in-situ simulations caused an increased department-wise focus on using an AED effectively in the future. “I think it was because it was me who picked it [the AED] up. It’s because I’ve seen a cardiac arrest where I saw what they did, and I just thought maybe that’s what you need to start with, so I did it.” (nurse, D18-3) “I thought it has gone wrong earlier with it [the AED], so that [the AED] I need to use because of the previous feedback” (nurse B6-2) Lack of routine and experience with AED use was mentioned as a reason for ineffective AED use. “I think the keyword is ‘routine’. That we aren’t used to it [the AED].” (nurse B1-1) “It just demonstrates that I have spent too little time with such an AED.” (nurse D20-5) |
| Organizational design | A few mentioned new placement of the AED as a reason for delayed use due to unawareness of the new placement. “It is not an excuse, but before we didn’t have it on the emergency cart.” (nurse B1-3) Visible placement of the AED resulted in the staff being more aware and faster at retrieving the AED. “I kind of think ‘awareness’, because it [the AED] is located where it is on the ward. There is no one who is in doubt that you should take it [the AED] with you, whereas this one [emergency cart], it’s hidden quite well, you have to keep in mind, who gets the emergency cart, whereas the AED is located so everyone can see it.” (nurse, D18-4) Placement of the AED alongside other emergency equipment eased retrieval of equipment. “And then it [AED] is placed on our emergency cart, so we always bring it.” (nurse D33-2) |
| Application of knowledge | Despite being able to operate the AED, ward staff was unaware or in doubt about the order of actions. “Which order do we do it in?” (radiographer C1-1) |
Table 4.
Themes related to transfer.
| Theme | |
|---|---|
| Contextualized training | Equipment during training was not identical to the equipment available in the department e.g., different AED models, AED placed in an unfamiliar bag, AED unpacked and opened during training. [Debriefer: Did you train with this AED-model?], “No, we have not” (physician D26-1), “It is another one” (nurse D26-2) “Well, and then it was just about getting it opened correctly, because that, [during] CPR-course it had been opened in advance. I didn’t know how to open it correctly!” (nurse D5-3) When the equipment was recognizable, it facilitated the use. “Is it a long shot, but we are trained in this one [manual defibrillator] at the courses and not that one [AED]” (physician A3-1) [Debriefer: So, you recognize this one [manual defibrillator]?] “Yes” (multiple participants A3) |
| Electrode placement | There was widespread doubt about how to attach the defibrillation electrodes during ongoing chest compressions, including doubt about whether to pause chest compressions or not. “There were some doubts about whether to continue or not there, with the chest compressions.” (nurse D37-1) A few participants expressed doubt regarding electrode placement recommendations. “So, should it [electrode] have been further down and the other [electrode] further out on the side?” (nurse D32-6) “Well, I don’t know, was it, should we… well they [electrodes] are placed wrong for sure.” (physician D33-1) |
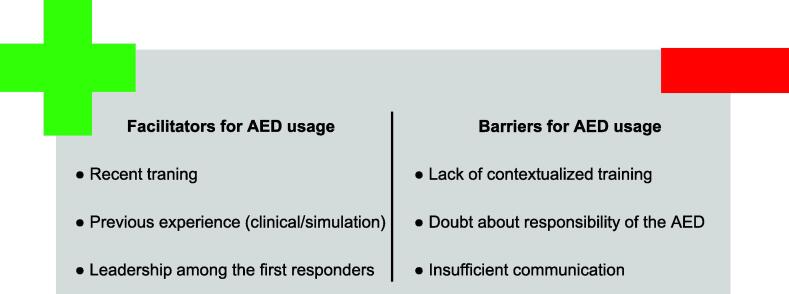
There were barriers related to AED usage within all three domains. The most frequently mentioned barrier to AED use were doubt about who was responsible for attaching and operating the AED, which led to delays in using the AED (Table 2). Further, lack of verbalization of the arrival of the AED caused delays. Both the cardiac arrest team and ward staff experienced challenges in operating the AED e.g., trying to “manually charge” the AED, trouble turning on the AED, and doubt about how to attach the electrodes (Table 3). Often it was described that resuscitation courses were not sufficiently contextualized e.g., used different AED models, or did not train how to unpack and turn on the AED (Table 4). Finally, the ward staff was often unaware of the priority of the AED, causing them to prioritize e.g., bag-mask ventilation and preparation of medication over the use of the AED.
The most frequently described facilitators for AED use were recently completed resuscitation course, previous experience with AED use from clinical situations or simulations, highly visual placement of the AED as a reminder to use it, placement on/next to the emergency cart (Table 3), leadership by a nurse or other person in the initial phase caused effective delegation of tasks including AED use, and finally, clear and loud communication facilitated the use of an AED (Table 2).
Discussion
We found that AEDs were often used during unannounced in-situ simulated IHCA. However, the first shock was not delivered until after 3.5 minutes mainly due to delays in deciding to collect the AED and applying the AED upon arrival. We found several challenges in operating the AED. The main reasons for ineffective AED use were limited responsibility for the AED use, lack of knowledge, and lack of contextualized training (Fig. 2).
Fig. 2.
Facilitators and barriers for AED usage.
AEDs were used in almost every simulated cardiac arrest in our study. Previous studies on AED usage did not find that AEDs were used this frequently for IHCAs.10., 15., 16. A reason for this is that IHCAs occurs in locations without AEDs. The proximity of the AEDs in our study may be one of the reasons for the frequent AED use.34 Also, our participants described visual placement of the AED, recent training, discussion, and reflection about the AED as factors contributing to the use of the AED.
Importantly, we found delays in the use of an AED and rhythm analysis in < 3 minutes were only achieved in less than 25% of cases, potentially contributing to lower survival after IHCA.6., 7., 8. Clinical data report delayed defibrillation in only 30% of cases,6., 7., 8. and faster time to rhythm analysis35., 16. than our findings. This may be due to a selected population in our study, i.e., departments with AEDs and exclusion of intensive care units etc., and due to inaccuracies in time registration in databases.36., 37., 38. Often, the delay in using an AED was due to a combination of spending > 1 minute to decide to collect the AED and the notable delay of more than a minute before using the AED upon arrival on site. The most frequently described reason for this was doubt about who had the responsibility of operating and attaching the AED once it was in the room. This is likely because there was no pre-defined role allocation for the ward staff being the first responders resulting in confusion and delays unless leadership and role-allocation were quickly established. Further, it was frequently observed and described that there was no verbalization about the AED arriving in the room causing people to continue cardiopulmonary resuscitation without using the AED as it arrived. This led to delays until another staff member asked about the AED only to discover the AED in the room. The staff described the need for verbalization about the arrival of the AED to clearly switch the responsibility from the person retrieving the AED to another person who could attach and operate the AED in case the person retrieving it felt insecure about doing this. Basic life support courses for nurses/nurse assistants are often provided without specific training on leadership, teamwork, and communication.39 However, our findings, as well as other findings, suggest that non-technical skills are just as important for basic life support skills as for advanced life support skills.19., 39., 40.
We also found several challenges in operating the AED, including failed shock delivery and inadequate placement of the electrodes. Both the ward staff and the cardiac arrest team experienced these challenges. Many of the challenges were related to insufficient training with different AED models compared to the AED available in the clinical setting and lacking training of opening and turning on the AED, i.e., contextual skills in operating the AED. These elements, not identical to the clinical setting, may have caused some form of negative learning i.e., acquiring a skill incorrectly, leading to confusion as seen during the in-situ simulations.41., 42., 43. This could very well also occur during an actual cardiac arrest.
Our finding of poor electrode placement is in line with previous studies28., 29., 44., 42. suggesting a need for faculty and course curricula development to increase the focus on correct electrode placement with ongoing chest compressions.
Our findings suggest a need for more training conducted in a realistic manner. Further, the training should focus on team formation, including leadership and communication as these non-technical skills proves as important for the ward staff as the cardiac arrest team. It is important that the training is contextualized e.g., training should also include the ad hoc delegation of tasks, use of equipment, and consist of a “team” instead of focusing on individual performance to avoid confusion and doubt during clinical emergencies. This can be trained through in-situ simulations, which can be a contextualized training method, that seems associated with improved survival after IHCA.45
Limitations
This is a simulation-based study. To reflect the clinical setting and clinical performance, we conducted full-scale, unannounced, in-situ simulations using the clinical equipment. Although the simulations were unannounced and the staff unaware of the scenarios, the staff may have detected the research staff entering the patient room in some cases. Further, some staff members participated in more than one in-situ simulation. However, use of daytime, evening, and nighttime with only a few simulations per department limited the amount of ward staff being exposed to more than one simulation. Due to the COVID-19 pandemic, surgical face masks and disinfection of hands were mandated. Although this reflects clinical practice during the pandemic, it may have caused slight delays in performance and have affected communication. Finally, this is an observational study. Due to the explorative nature of the study, it was not based on a sample size calculation, the sample size was limited, and data collection was stopped prematurely due to the COVID-19 pandemic.
Conclusion
During unannounced simulated IHCAs, time to defibrillation was often > 3 minutes. Most of the delay occurred after the AED was collected. Lack of non-technical skills and contextualized training were among the main perceived barriers to AED usage. Facilitators for successful use included recent training, previous experience, and successful leadership.
CRediT authorship contribution statement
Mathilde Stærk: Conceptualization, Methodology, Resources, Investigation, Writing – original draft, Writing – review & editing, Project administration. Kasper G. Lauridsen: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision. Julie Niklassen: Investigation, Writing – review & editing. Rasmus Philip Nielsen: Investigation, Writing – review & editing. Kristian Krogh: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision. Bo Løfgren: Conceptualization, Methodology, Resources, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank all participating hospitals, departments, and staff. A special thanks to Rikke Højbjerg, RN and Mette Qvortrup, RN for their contribution to include departments and conduct simulations. We thank Dung Thuy Nguyen, Camilla Thomsen Støtt, Josephine Johnsen, Signe Hedebo, Christian Gansted, Cecilie Budolfsen, Kathrine Mackenhauer, Marlice Zwanenburg, Maria Høybye, Stine Holst Bjerre Pedersen, Marine Sølling Ramsing, Alexandra Amalie Uglebjerg Pedersen, Sophie Fromholt, Martin Thomsen, Isabella Hangaard Rüdiger, Ida Norup, Marie Egebjerg Jensen, Louise Nørkjær, Kenneth Lavrsen, Reshaabi Srinanthalogen, Amalie Nicolaisen, and Mette Vold Hansen for their assistance in conducting simulations.
Funding
We thank Randers Regional Hospital, Aarhus University, Laerdal Foundation, the A.P. Møller Foundation for the Advancement of Medical Science (Fonden til Lægevidenskabens Fremme), the Health Foundation (Helsefonden), and Health Research Foundation of Central Denmark Region (Region Midtjyllands Sundhedsvidenskabelige Forskningsfond) for financial support. We thank Physio-Control for providing defibrillation electrodes for the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100257.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Nolan J.P., Soar J., Smith G.B., et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85:987–992. doi: 10.1016/j.resuscitation.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Kolte D., Khera S., Aronow W.S., et al. Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation. 2015;131:1415–1425. doi: 10.1161/CIRCULATIONAHA.114.014542. [DOI] [PubMed] [Google Scholar]
- 3.Ehlenbach W.J., Barnato A.E., Curtis J.R., et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. The New Engl J Med. 2009;361:22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandroni C., Nolan J., Cavallaro F., Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237–245. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 5.DANARREST. DANARREST - Registrering af hjertestop på hospital. Årsrapport 2018. 2019 May 2019.
- 6.Chan P.S., Krumholz H.M., Nichol G., Nallamothu B.K. Delayed time to defibrillation after in-hospital cardiac arrest. New Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 7.Herlitz J., Aune S., Bång A., et al. Very high survival among patients defibrillated at an early stage after in-hospital ventricular fibrillation on wards with and without monitoring facilities. Resuscitation. 2005;66:159–166. doi: 10.1016/j.resuscitation.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 8.Skrifvars M.B., Rosenberg P.H., Finne P., et al. Evaluation of the in-hospital Utstein template in cardiopulmonary resuscitation in secondary hospitals. Resuscitation. 2003;56:275–282. doi: 10.1016/s0300-9572(02)00373-8. [DOI] [PubMed] [Google Scholar]
- 9.Sandroni C., Ferro G., Santangelo S., et al. In-hospital cardiac arrest: survival depends mainly on the effectiveness of the emergency response. Resuscitation. 2004;62:291–297. doi: 10.1016/j.resuscitation.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 10.Hanefeld C., Lichte C., Mentges-Schröter I., Sirtl C., Mügge A. Hospital-wide first-responder automated external defibrillator programme: 1 year experience. Resuscitation. 2005;66:167–170. doi: 10.1016/j.resuscitation.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Kloppe C., Jeromin A., Kloppe A., Ernst M., Mügge A., Hanefeld C. First responder for in-hospital resuscitation: 5-year experience with an automated external defibrillator-based program. J Emerg Med. 2013;44:1077–1082. doi: 10.1016/j.jemermed.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 12.Andersen L.W., Holmberg M.J., Lofgren B., Kirkegaard H., Granfeldt A. Adult in-hospital cardiac arrest in Denmark. Resuscitation. 2019;140:31–36. doi: 10.1016/j.resuscitation.2019.04.046. [DOI] [PubMed] [Google Scholar]
- 13.Hessulf F., Herlitz J., Rawshani A., et al. Adherence to guidelines is associated with improved survival following in-hospital cardiac arrest. Resuscitation. 2020;155:13–21. doi: 10.1016/j.resuscitation.2020.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Chan P.S., Nichol G., Krumholz H.M., Spertus J.A., Nallamothu B.K. Hospital variation in time to defibrillation after in-hospital cardiac arrest. Arch Internal Med. 2009;169:1265–1273. doi: 10.1001/archinternmed.2009.196. [DOI] [PubMed] [Google Scholar]
- 15.Wutzler A., Kloppe C., Bilgard A.K., Mugge A., Hanefeld C. Use of automated external defibrillators for in-hospital cardiac arrest : Any time, any place? Medizinische Klinik, Intensivmedizin und Notfallmedizin. 2019;114:154–158. doi: 10.1007/s00063-017-0377-7. [DOI] [PubMed] [Google Scholar]
- 16.Stærk M., Lauridsen K.G., Krogh K., Løfgren B. Distribution and use of automated external defibrillators and their effect on return of spontaneous circulation in Danish hospitals. Resuscitation Plus. 2022;9 doi: 10.1016/j.resplu.2022.100211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosen M.A., Hunt E.A., Pronovost P.J., Federowicz M.A., Weaver S.J. In situ simulation in continuing education for the health care professions: a systematic review. J Continuing Educ Health Professions. 2012;32:243–254. doi: 10.1002/chp.21152. [DOI] [PubMed] [Google Scholar]
- 18.Walker S.T., Sevdalis N., McKay A., et al. Unannounced in situ simulations: integrating training and clinical practice. BMJ Quality & Saf. 2013;22:453–458. doi: 10.1136/bmjqs-2012-000986. [DOI] [PubMed] [Google Scholar]
- 19.Lauridsen K.G., Krogh K., Müller S.D., et al. Barriers and facilitators for in-hospital resuscitation: A prospective clinical study. Resuscitation. 2021;164:70–78. doi: 10.1016/j.resuscitation.2021.05.007. [DOI] [PubMed] [Google Scholar]
- 20.Eppich W., Cheng A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthcare : J Soc Simulation Healthcare. 2015;10:106–115. doi: 10.1097/SIH.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 21.Eppich W.J., Mullan P.C., Brett-Fleegler M., Cheng A. “Let's talk about it”: translating lessons from health care simulation to clinical event debriefings and coaching conversations. Clin Pediatric Emergency Med. 2016;17:200–211. [Google Scholar]
- 22.Fanning R.M., Gaba D.M. The role of debriefing in simulation-based learning. Simul Healthcare : J Soc Simul Healthcare. 2007;2:115–125. doi: 10.1097/SIH.0b013e3180315539. [DOI] [PubMed] [Google Scholar]
- 23.Rudolph J.W., Simon R., Dufresne R.L., Raemer D.B. There's no such thing as “nonjudgmental” debriefing: a theory and method for debriefing with good judgment. Simul Healthcare : J Soc Simul Healthcare. 2006;1:49–55. doi: 10.1097/01266021-200600110-00006. [DOI] [PubMed] [Google Scholar]
- 24.Andersen L.W., Østergaard J.N., Antonsen S., et al. The Danish in-hospital cardiac arrest registry (DANARREST) Clin Epidemiology. 2019;11:397–402. doi: 10.2147/CLEP.S201074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Staerk M., Bodtker H., Lauridsen K.G., Lofgren B. Automated external defibrillation training on the left or the right side - a randomized simulation study. Open Access Emergency Medicine : OAEM. 2017;9:73–79. doi: 10.2147/OAEM.S140220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soar J., Nolan J.P., Bottiger B.W., et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult Adv Life Support Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 27.Nurmi J., Castren M. Layperson positioning of defibrillation electrodes guided by pictorial instructions. Resuscitation. 2005;64:177–180. doi: 10.1016/j.resuscitation.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Nurmi J., Rosenberg P., Castren M. Adherence to guidelines when positioning the defibrillation electrodes. Resuscitation. 2004;61:143–147. doi: 10.1016/j.resuscitation.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 29.Heames R.M., Sado D., Deakin C.D. Do doctors position defibrillation paddles correctly? Observational Study BMJ. 2001;322:1393–1394. doi: 10.1136/bmj.322.7299.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gadamer H-G, Weinsheimer J, Marshall DG. Elements of a Theory of Hermeneutic Experience. Truth and methods. 2. rev. ed. / translation revised by Joel Weinsheimer and Donald G. Marshall. New York: Continuum; 1989. p. 268-306.
- 31.Braun V., Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101. [Google Scholar]
- 32.Fereday J., Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qualitative Methods. 2006;5:80–92. [Google Scholar]
- 33.Edmondson A.C., Schein E.H. 1st ed. Jossey-Bass; San Francisco: 2012. Teaming how organizations learn, innovate, and compete in the knowledge economy. [Google Scholar]
- 34.Sondergaard K.B., Hansen S.M., Pallisgaard J.L., et al. Out-of-hospital cardiac arrest: Probability of bystander defibrillation relative to distance to nearest automated external defibrillator. Resuscitation. 2018;124:138–144. doi: 10.1016/j.resuscitation.2017.11.067. [DOI] [PubMed] [Google Scholar]
- 35.DANARREST. DANARREST - Registrering af hjertestop på hospital Årsrapport 2020. 2021 June 17th 2021.
- 36.Kaye W., Mancini M.E., Truitt T.L. When minutes count–the fallacy of accurate time documentation during in-hospital resuscitation. Resuscitation. 2005;65:285–290. doi: 10.1016/j.resuscitation.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 37.Stewart J.A. Problems with time-interval data from In-hospital resuscitation records. Int J Cardiol. 2016;223:879–880. doi: 10.1016/j.ijcard.2016.07.300. [DOI] [PubMed] [Google Scholar]
- 38.Grundgeiger T., Albert M., Reinhardt D., Happel O., Steinisch A., Wurmb T. Real-time tablet-based resuscitation documentation by the team leader: evaluating documentation quality and clinical performance. Scand J Trauma, Resuscitation and Emergency Med. 2016;24:51. doi: 10.1186/s13049-016-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lauridsen K.G., Løfgren B., Brogaard L., Paltved C., Hvidman L., Krogh K. Cardiopulmonary resuscitation training for healthcare professionals: a scoping review. Simul Healthcare : J Soc Simul Healthcare. 2021 doi: 10.1097/SIH.0000000000000608. [DOI] [PubMed] [Google Scholar]
- 40.Nallamothu B.K., Guetterman T.C., Harrod M., et al. How do resuscitation teams at top-performing hospitals for in-hospital cardiac arrest succeed? A qualitative study. Circulation. 2018;138:154–163. doi: 10.1161/CIRCULATIONAHA.118.033674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bond W.F., Lammers R.L., Spillane L.L., et al. The use of simulation in emergency medicine: a research agenda. Acad Emergency Med. 2007;14:353–363. doi: 10.1197/j.aem.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 42.Stærk M., Vammen L., Andersen C.F., Krogh K., Løfgren B. Basic life support skills can be improved among certified basic life support instructors. Resuscitation Plus. 2021;6 doi: 10.1016/j.resplu.2021.100120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krogh K.B., Hoyer C.B., Ostergaard D., Eika B. Time matters–realism in resuscitation training. Resuscitation. 2014;85(8):1093–1098. doi: 10.1016/j.resuscitation.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Mattei L.C., McKay U., Lepper M.W., Soar J. Do nurses and physiotherapists require training to use an automated external defibrillator? Resuscitation. 2002;53(3):277–280. doi: 10.1016/s0300-9572(02)00023-0. [DOI] [PubMed] [Google Scholar]
- 45.Josey K., Smith M.L., Kayani A.S., et al. Hospitals with more-active participation in conducting standardized in-situ mock codes have improved survival after in-hospital cardiopulmonary arrest. Resuscitation. 2018;133:47–52. doi: 10.1016/j.resuscitation.2018.09.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.