Abstract
Background:
Younger patients who sustain anterior cruciate ligament (ACL) ruptures are at high risk for reinjury after ACL reconstruction. Restoring muscle strength before return to sports (RTS) is regarded as an important factor in reducing the reinjury risk, and quadriceps and hamstring strength assessment is commonly included in RTS testing. However, it is not clear whether reduced strength is a risk factor for subsequent graft rupture in this patient population.
Purpose:
To investigate the association between quadriceps and hamstring strength at 12 months after primary ACL reconstruction and ACL graft rupture in young patients.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
The cohort consisted of 210 patients (100 men and 110 women) who were younger than 20 years at the time of primary ACL reconstruction with a hamstring tendon autograft and who had no previous contralateral ACL injury. Isokinetic strength testing (60 and 180 deg/s) of knee flexors and extensors was performed at 12 months postoperatively, and the limb symmetry index (LSI) for each strength outcome was calculated. RTS rates and the incidence of further ACL graft ruptures were recorded.
Results:
Measures of central tendency (mean and median) of LSI values ranged from 88 to 98. The percentage of patients with LSI ≥90 was 57% to 69% for quadriceps strength and 45% to 47% for hamstring strength. Overall, 19 patients (9%) sustained an ACL graft rupture. No significant differences were found between the patients who sustained an ACL graft rupture and those who did not in terms of quadriceps and hamstring strength at 12 months. No significant associations were found between achieving LSI ≥90 for quadriceps peak torque and subsequent ACL graft rupture.
Conclusion:
In young patients who underwent an ACL reconstruction, no association was noted between quadriceps and hamstring strength at 12 months postoperatively and subsequent graft ruptures. The role of strength testing as part of the RTS criteria after ACL reconstruction, and specifically the use of limb symmetry thresholds, warrants further investigation and clarification.
Keywords: anterior cruciate ligament (ACL), strength testing, young patients, reinjury, graft rupture, contralateral injury, return to sport (RTS)
The incidence of anterior cruciate ligament (ACL) injuries and surgical reconstruction in young patients is increasing. 33,45 A further ACL injury after primary ACL reconstruction is a well-recognized and devastating complication. Young age at the time of surgery has been shown to be a risk factor for further injury, with reported reinjury rates of up to 40% in younger patients. 2,6,10,20,24,32,38,41 It appears that the risk of second ACL injury is greatest within the first 2 years after ACL reconstruction for young athletes returning to pivoting and cutting sports. 12,27,30,32,41
Restoration of strength in the quadriceps and hamstring muscle groups is generally accepted as an important component of rehabilitation after ACL reconstruction, not only to allow recovery of function and return to sports (RTS) but also to reduce the risk of reinjury. One way of assessing the recovery of strength is to compare the strength of the operated limb to that of the contralateral limb using the limb symmetry index (LSI). 12,25,34 Typically, LSI >80 to 90 is regarded as reflecting a satisfactory recovery of strength. 1,3,14,26,28,29 Achieving this level of symmetry has been proposed as a criterion to be met before RTS on the basis that this reduces the risk of reinjury. 8,12,22
A limited number of studies have specifically assessed recovery of strength and the relationship between strength and second ACL injuries, particularly in a young, high-risk population. Two studies reported that patients who had decreased quadriceps strength symmetry after ACL reconstruction had an increased risk of further knee reinjuries, including ACL graft ruptures. 12,22 In comparison, Beischer et al 4 recently concluded that there were no associations between achieving symmetrical muscle function or quadriceps strength and sustaining a subsequent ACL injury. These 3 studies entailed large variations in the time from surgery to strength testing and in the testing protocols used. In addition, a variety of graft types were used, and patient populations were not specifically a younger age group.
The aim of the current study was therefore to investigate the recovery of quadriceps and hamstring strength in a large cohort of young patients after primary ACL reconstruction using a hamstring tendon autograft and to explore the association between the recovery of quadriceps and hamstring strength and the rate of ACL graft ruptures. We hypothesized that there would be satisfactory recovery of quadriceps and hamstring muscle strength but no association between quadriceps or hamstring strength and ACL graft rupture rates in this young cohort of patients.
Methods
Patient Population and Study Setting
Human research ethics committee approval was obtained for the study protocol, and all participants or their guardians gave informed consent to participate. The study was undertaken in a private orthopaedic clinic in Melbourne, Australia, at which data are collected prospectively for all patients undergoing an ACL reconstruction. The inclusion criteria for the study were age younger than 20 years at the time of surgery, a primary ACL reconstruction with a hamstring tendon autograft between January 2013 and April 2018, and routine follow-up attendance at 12 months postoperatively. Patients were excluded if they had previous contralateral surgery or ACL injury, contralateral graft harvest, multiligament surgery, a lateral extra-articular tenodesis procedure, or bilateral ACL reconstruction. Patients who underwent subsequent surgery that would affect strength testing or who sustained a graft rupture or contralateral ACL injury before their 12-month review were also excluded.
Surgical Technique and Rehabilitation
All ACL reconstructions were performed by 1 of 4 experienced knee surgeons using an arthroscopically assisted technique (J.A.F., T.S.W., B.M.D.). A 4-strand hamstring tendon autograft (semitendinosus/gracilis) was used in all cases. Both femoral and tibial tunnels were positioned within the anatomic footprint of the ACL, with the femoral tunnel being created via the anteromedial portal. An EndoButton CL Ultra (Smith & Nephew Endoscopy) was used to secure the proximal end of the graft; after cycling of the knee and tensioning of the graft, we used a cannulated interference screw to secure the distal portion of the graft with the knee in full extension.
The same postoperative rehabilitation protocol was provided to all patients, although individuals undertook their rehabilitation under supervision at their own discretion and using an allied health professional of their choice. Weightbearing as tolerated was encouraged from the outset, and no braces or splints were used unless a meniscal repair had been performed. Emphasis was placed on early restoration of active knee extension and quadriceps activation. Progression through the rehabilitation program was guided by the presence of pain and swelling. Participants progressed to riding a stationary bicycle as soon as they were comfortable (usually between 3 and 4 weeks) and typically commenced gymnasium-based exercises 5 to 6 weeks postoperatively. Running was permitted when there was no knee effusion and the quadriceps strength was satisfactory (typically between 12 and 16 weeks). Progression to sport-specific drills commenced at 4 months, and a graduated return to team training started around 6 months postoperatively, provided a participant had no effusion, essentially full range of motion, good quadriceps strength, and good control of lower limb stability. Formal RTS testing was not performed on a routine basis, but return to competition sport was permitted after at least 1 month of unrestricted full-contact training, typically from 11 to 12 months after surgery onward. The strength testing reported in this study was not used to determine readiness to RTS.
Data Collection Procedures
Participants’ characteristics, as well as information about the original injury, preinjury sports participation, and surgical details, were collated from the prospectively collected patient database.
All patients undergoing ACL reconstruction at the clinic are encouraged to return for a routine 12-month assessment. The assessment involves a questionnaire that includes standard patient-reported outcome measures (Marx activity rating scale, International Knee Documentation Committee–Subjective Knee Form, and single assessment numerical evaluation) as well as questions about further ACL injuries, further surgical procedures on the knee, and RTS. Possible responses to the RTS question were as follows: returned at the same or a higher level, returned at a lower level, returned to training only, or did not return to sport. Clinical examination of the knee is also undertaken (effusion, range of motion, and side-to-side difference in anterior knee laxity using the KT-1000 arthrometer at 134 N), as well as hop tests (single hop for distance and triple crossover hop for distance).
During the study period, all patients patients seen in the clinic who were younger than 20 years at the time of surgery were encouraged to undertake a strength assessment at the 12-month follow-up. Isokinetic strength testing was undertaken by trained clinical assessors (H.J.K.) using a HUMAC NORM Dynamometer (Computer Sports Medicine). The seat back was set at an angle of 85°, and the seat was adjusted to the length of the thigh. The thigh of the testing limb was secured via a strap, and the center of rotation of the dynamometer was aligned with the epicondylar axis of the knee. Isokinetic testing of the knee flexors and extensors was performed across the full range of motion at 2 different speeds: 60 and 180 deg/s. For each test, 2 warm-up trials were performed, followed by 3 and 5 trials at maximum effort for 60 and 180 deg/s, respectively. The nonoperated limb was tested first, followed by the operated limb. This protocol for testing knee flexor and extensor strength has shown good to excellent reliability, with intraclass correlation coefficient values ranging from 0.74 to 0.89 for knee tests. 13 The highest peak torque from the 3 trials was collected for each limb and used to calculate the LSI for both quadriceps and hamstring strength (LSI = [Injured Leg Value ÷ Uninjured Leg Value] × 100). As a secondary strength outcome, we also calculated peak torque as a percentage of body weight for the operated limb.
All study patients were sent a questionnaire at a minimum of 2 years after surgery. This included the same questions from the 12-month questionnaire regarding RTS as well as further injuries or knee procedures. For the subsequent analysis, only ACL graft ruptures or contralateral ACL injuries that occurred before 3 years were included, given that beyond this time point, the relevance of a strength test at 12 months was questionable. It is worth reiterating that patients who sustained a graft rupture or contralateral ACL tear before the 12-month follow-up were not included.
Statistical Analysis
Measures of central tendency (mean, median) were calculated for each strength variable, and test of normality was performed. Patients were classified according to whether they had sustained a graft rupture, and between-group comparisons were performed for all strength variables using independent-samples t tests or the Mann-Whitney U test.
Patients were then grouped according to whether their LSI was ≥90 or <90. Contingency tables (2 × 2) were constructed, and the chi-square test was used to test for significant associations between achieving LSI ≥90 and reinjury.
All analyses were performed using IBM SPSS Statistics Version 27 (IBM Corp). A P value <.05 was considered statistically significant.
Results
During the study period, 421 patients younger than 20 years at the time of surgery underwent a primary ACL reconstruction. Of these patients, 265 met the eligibility criteria for this study. Reasons for exclusion are shown in Table 1. Of the 265 eligible patients, 221 had complete 12-month follow-up data, including strength testing. Of these patients, 11 patients did not have minimum 2-year follow-up and were therefore excluded, leaving a final study cohort of 210 patients. With this sample size, the current study had 80% power with an alpha level of .05 to detect a moderate to large effect when the number of patients sustaining graft ruptures was equivalent to 10% of those not sustaining a rupture.
Table 1.
Reasons for Exclusion From the Study a
| Reason for Exclusion | No. of Patients Excluded |
|---|---|
| Other graft source | 35 |
| Previous contralateral ACL reconstruction | 24 |
| Lateral extra-articular tenodesis | 10 |
| Graft rupture or contralateral ACL rupture before 12-mo follow-up | 26 |
| Further surgical procedure to the knee before 12-mo follow-up | 2 |
a ACL, anterior cruciate ligament.
The final population included 100 men and 110 women, and the average age at the time of surgery was 17 years (range, 10-19 years). The most common preinjury sports were Australian Rules football (34.8%), netball (27.6%), soccer (10.0%), and basketball (11.9%), together accounting for 84.3% of preinjury sports played by the cohort. The mean preinjury Marx activity score was 14.1 ± 2.3 (range, 4-16).
Concomitant meniscal and chondral findings at the time of ACL reconstruction are shown in Table 2, as are the graft diameters.
Table 2.
Surgical Details
| No. of Patients (%) | |
|---|---|
| Medial meniscal injury and treatment | |
| No tear | 161 (77) |
| Stable tear: no treatment | 15 (7) |
| Tear: partial resection | 10 (5) |
| Tear: repair | 23 (11) |
| Previous partial resection | 1 (0.5) |
| Lateral meniscal injury and treatment | |
| No tear | 141 (67) |
| Stable tear: no treatment | 23 (11) |
| Tear: partial resection | 34 (16) |
| Tear: repair | 12 (6) |
| Chondral injuries a | |
| Patellofemoral compartment | 9 (4) |
| Medial compartment | 9 (4) |
| Lateral compartment | 9 (4) |
| Graft diameter b | |
| 6-6.5 mm | 3 (1) |
| 6.6-7.0 mm | 28 (13) |
| 7.1-7.5 mm | 43 (21) |
| 7.6-8.0 mm | 58 (28) |
| 8.1-8.5 mm | 52 (25) |
| 8.6-9.0 mm | 21 (10) |
| 9.1-9.5 mm | 5 (2) |
a International Cartilage Repair Society grade ≥2.
b Calculated as (Proximal + Distal) ÷ 2.
The patient-reported outcome scores at 12-month follow-up are shown in Table 3. At 12 months, 75 patients (36%) had returned to the same or a higher level of sports compared with preinjury, 73 (35%) had returned to training, and 62 (30%) had not yet returned to any sport.
Table 3.
Patient-Reported Outcome Scores at 12 Months Postoperatively a
| Score | Mean | Median | Range | |
|---|---|---|---|---|
| Marx activity | 10.8 | 12 | 0-16 | |
| IKDC-SKF | 87.8 | 90.8 | 51.7-100 | |
| SANE | 90.0 | 90 | 7-100 |
a IKDC-SKF, International Knee Documentation Committee Subjective Knee Form; SANE, single assessment numerical evaluation.
Strength at 12-month follow-up is summarized in Table 4. Measures of central tendency (mean and median) for both quadriceps and hamstring peak torque LSI ranged from 88 to 98, whereas the percentage of patients with LSI ≥90 was between 57% and 69% for quadriceps strength and 45% and 47% for hamstring strength. The distribution of LSI scores for hamstring strength showed marked deviation from a normal distribution (high positive skew and kurtosis >10). Quadriceps strength showed only mild deviation from a normal distribution (slightly positive skew for both speeds and kurtosis >3 for 180 deg/s). Peak torque of the operated limb as a percentage of body weight was normally distributed.
Table 4.
Measures of Central Tendency for Quadriceps and Hamstring Peak Torque and the Proportion of Patients With LSI ≥90 for Quadriceps and Hamstring Peak Torque a
| Quadriceps | Hamstring | |||
|---|---|---|---|---|
| 60 deg/s | 180 deg/s | 60 deg/s | 180 deg/s | |
| Peak torque LSI | ||||
| Mean ± SD | 91.4 ± 16.1 | 98.2 ± 20.7 | 92.4 ± 23.9 | 93.3 ± 34.8 |
| Median | 92.1 | 96.5 | 88.7 | 88.1 |
| % Patients with LSI ≥90 | 57 | 69 | 47 | 45 |
a LSI, limb symmetry index.
At minimum 2-year follow-up, 172 patients (81.9%) indicated that they had returned to their preinjury sports after surgery. A total of 19 patients (9%) had sustained an ACL graft rupture. A further 19 patients (9%) had sustained a contralateral ACL rupture. The median time from surgery to graft rupture was 23 months (11 months from strength testing) with a range from 13 to 36 months. A total of 4 patients sustained the graft rupture between 12 and 18 months from surgery; 6 patients, between 18 and 24 months; and the remainder, after 24 months. We noted that 2 of the ACL graft ruptures occurred in patients who reported that they had not returned to their preinjury sports at follow-up. However, both patients were playing sports when they sustained the graft rupture. In view of this as well as the generally high Marx scores of the patient cohort at 12 months and the high rate of return to preinjury sports (82%), comparison of strength measurements between those who sustained a graft rupture and those who did not was conducted using the whole cohort rather than only those who reported that they had returned to their preinjury sports.
We found no significant differences between the patients who sustained an ACL graft rupture and those who did not in terms of quadriceps and hamstring strength at 12 months. This was the case when strength was recorded as the LSI for peak torque measurements as well as when strength was reported as peak torque measurements adjusted for body weight (Table 5).
Table 5.
Comparison of Quadriceps and Hamstring Peak Torque (LSI and %BW) Between Patients Who Did and Did Not Sustain ACL Graft Rupture a
| Quadriceps | Hamstring | |||
|---|---|---|---|---|
| 60 deg/s | 180 deg/s | 60 deg/s | 180 deg/s | |
| Peak torque LSI | ||||
| No ACL graft rupture (n = 191) | 89.0 ± 22.5 | 97.1 ± 19.0 | 90.1 ± 19.4 | 91.4 ± 16.2 |
| ACL graft rupture (n = 19) | 94.2 ± 20.1 | 98.4 ± 19.3 | 93.6 ± 9.4 | 92.2 ± 16.0 |
| Peak torque, %BW | ||||
| No ACL graft rupture (n = 191) | ||||
| Operated | 195.0 ± 53.8 | 135.2 ± 43.3 | 103.8 ± 32.1 | 69.8 ± 27.4 |
| Nonoperated | 214.3 ± 55.5 | 140.4 ± 44.3 | 116.0 ± 35.3 | 77.0 ± 28.0 |
| ACL graft rupture (n = 19) | ||||
| Operated | 203.5 ± 53.8 | 136.8 ± 44.1 | 102.1 ± 25.4 | 73.6 ± 23.1 |
| Nonoperated | 225.8 ± 69.0 | 135.8 ± 42.8 | 109.0 ± 24.7 | 75.7 ± 24.0 |
a Data are reported as mean ± SD. No significant between-group differences were found in peak torque when assessed as LSI (P > .05, Mann-Whitney U test) and after adjustment for BW (P > .05, independent-samples t test). ACL, anterior cruciate ligament; BW, body weight, LSI, limb symmetry index.
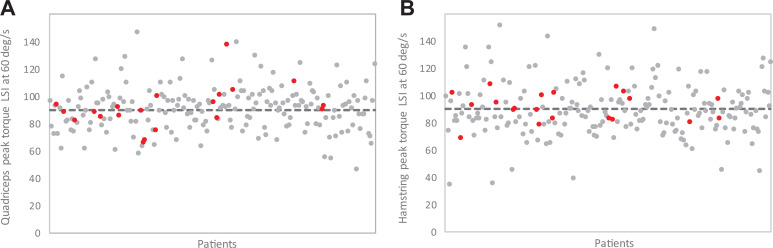
We also found no significant associations between achievement of LSI ≥90 for peak torque and subsequent ACL graft rupture, as shown in Table 6. Figure 1 shows scatterplots of all LSI scores for quadriceps and hamstring peak torque at 60 deg/s. We found no discernable pattern of LSI scores among patients who sustained an ACL graft rupture compared with those who did not.
Table 6.
Comparison of ACL Graft Rupture Rates Between Patients Who Did and Who Did Not Achieve Peak Torque LSI ≥90 for Quadriceps and Hamstring Strength a
| Graft Ruptures | ||
|---|---|---|
| LSI ≥90 | LSI <90 | |
| Quadriceps | ||
| 60 deg/s | 9/91 (10) | 10/119 (8) |
| 180 deg/s | 14/144 (10) | 5/66 (8) |
| Hamstring | ||
| 60 deg/s | 13/99 (13) | 6/111 (5) |
| 180 deg/s | 8/116 (7) | 11/94 (12) |
a Data are reported as No. of patients/total patients (%). No significant between-group differences were found (P > .05, Mann-Whitney U test). ACL, anterior cruciate ligament; LSI, limb symmetry index.
Figure 1.
Scatterplots of peak torque limb symmetry index (LSI) scores at 60 deg/s of all study patients for (A) quadriceps and (B) hamstring strength. Gray dots indicate patients with no anterior cruciate ligament (ACL) graft rupture; red dots indicate patients with ACL graft rupture. Dashed line indicates LSI = 90.
Discussion
This study revealed that in a large cohort of young athletes undergoing primary ACL reconstruction with hamstring tendon autograft, although there was an overall high level of quadriceps and hamstring strength recovery as judged via measures of central tendency (mean and median values) of the LSI, <70% of patients actually achieved LSI ≥90 at 12 months after surgery. Despite this, we found no association between quadriceps and hamstring strength at 12 months and ACL graft ruptures in the 2 years after strength testing. This potentially raises questions about the emphasis placed on quadriceps and hamstring strength assessment in decisions about returning to sports.
Restoring quadriceps and hamstring muscle strength and symmetrical function is considered a key aspect of ACL rehabilitation and has been regarded as an important factor in reducing the reinjury risk upon RTS. 8,12,22 Grindem et al 12 reported significantly higher rates of knee reinjury in patients with a quadriceps strength LSI <90 on routine testing at 6 and 12 months after ACL reconstruction versus those with LSI ≥90 (33% vs 13%, respectively). Similarly, Kyritsis et al 22 found that elite-level male athletes who did not meet all 6 discharge criteria, including quadriceps strength LSI ≥90, before returning to professional sports had a 4 times greater risk of ACL graft rupture than did those who passed the RTS criteria. However, quadriceps strength LSI <90 was not associated with an increased risk of ACL graft rupture. 22 In the current study, we found no association between ACL graft rupture and knee extensor or flexor strength.
The findings of the current study are consistent with those of Beischer et al, 4 who investigated a cohort of 157 patients with a mean age of 22 years and found no associations between sustaining a subsequent ACL injury and achieving symmetrical muscle function or quadriceps strength. Ithurburn et al 17 assessed strength of quadriceps and hamstring muscles at the time of clearance for RTS in a young patient group (mean age, 17 years) and found no differences between those who successfully resumed their preinjury sports participation and those who sustained a second ACL injury.
The discrepancies in the literature regarding the association between quadriceps strength and the risk of further ACL injury may be due in part to differences in the characteristics of the patient cohorts and the methods used in the relevant studies. For instance, Kyritsis et al 22 reported on a cohort of male professional athletes, whereas other studies included both male and female participants and entailed a wider range of sporting levels. 4,12,17 In addition, Kyritsis et al used ACL graft rupture as their outcome of interest, whereas Beischer et al 4 and Ithurburn et al 17 used further ACL injury, including contralateral ACL injuries. Grindem et al 12 reported on further knee injuries, although their data included both ACL graft ruptures and contralateral ACL injuries.
The current study involved a young cohort of patients, all younger than 20 years at the time of surgery and with a mean age of 17 years. The only other study with a similarly young cohort was that of Ithurburn et al. 17 It has been reported that quadriceps strength after ACL reconstruction decreases with age, 16,37 although this in itself would not explain the lack of association between quadriceps strength and further ACL injury in either the current study or the study of Ithurburn et al. The older age of the patient cohorts in the studies by Grindem et al, 12 Kyritsis et al, 22 and Beischer et al 4 may explain in part the lower reinjury rate in those studies, as young age is a known risk factor for second ACL injuries. 2,24,32,38,41
A further difference between the current study and others is that all patients in the current study received a hamstring tendon graft, whereas the populations in other studies received a mix of both hamstring tendon and patellar tendon grafts. 4,12,17,22 When studying a cohort of 53 similarly young patients who had undergone ACL reconstruction with a patellar tendon graft, Rauck et al 31 reported a graft rupture rate of 7.4%, which is not dissimilar to the finding of the current study. It is not clear whether their patients underwent strength testing. It has been reported that ACL reconstruction using a hamstring tendon graft results in better quadriceps strength compared with that using patellar tendon or quadriceps tendon grafts, 19,21 although once again this would not specifically explain the lack of association between quadriceps strength and further ACL injury in the current study.
The timing of strength testing after surgery also varies among studies. We performed routine strength testing at 12 months postoperatively, but this was not done as part of RTS testing. Other studies used strength testing at variable time points, although generally related to the time of RTS. 4,12,17,22 This resulted in a broader range of time points, such as 116 to 513 days in the study by Kyritsis et al. 22 It is possible that customizing the timing of strength testing relative to the stage of rehabilitation and the time of RTS may have influenced the findings with regard to an association between strength recovery and further injury. However, only half of the graft ruptures occurred within 12 months of strength testing, and less than a quarter occurred within 6 months. Presumably, the longer the time from strength testing to graft rupture, the less likely are the results of the testing to be associated with the risk of graft rupture.
The validity of using limb symmetry in RTS testing after ACL reconstruction has been questioned. Although an association between LSI ≥90 for hop tests and RTS has been reported, 39 it has also been shown that only 45% of a healthy young cohort was able to achieve LSI ≥90 for all tests in a battery of 4 hop tests. 11 Interestingly, the mean LSI for each hop test in the battery was >95. 11 Looking at the issue from another perspective, Wellsandt et al 44 compared quadriceps strength LSI and the results of 4 hop tests in the operated limb 6 months after ACL reconstruction with the results of the nonoperated limb at 6 months as well as preoperatively. Those investigators found that 57% of patients achieved at least 90% limb symmetry relative to the nonoperated limb at 6 months whereas only 29% achieved at least 90% of the preoperative performance of the nonoperated limb. However, this result was found when the analysis combined hop test results with the quadriceps strength results. For quadriceps strength in isolation, 87% (61/70) of patients achieved at least 90% limb symmetry of the nonoperated limb at 6 months compared with 83% (58/70) relative to the preoperative results of the nonoperated limb. 44 Whether testing at 12 months would have produced different results is unknown. Johnston et al 18 demonstrated a significant improvement in quadriceps strength in the operated limb between 6 and 12 months after ACL reconstruction with both hamstring and quadriceps tendon grafts; the investigators noted less improvement in the nonoperated limb, resulting in an increased LSI from 6 to 12 months. Clearly, further research is needed to fully understand the implications of LSI and its role in RTS testing.
Young patient cohorts can entail considerable heterogeneity in terms of height and weight given the effects of growth in this age group. Younger patients are more likely to RTS; as well, young patients are more likely to meet criteria that indicate a satisfactory functional recovery and that have been used to indicate readiness to RTS, 39 although few patients meet the threshold criteria for multiple tests. 4,7,36,40 It has been suggested that thresholds for RTS criteria might need to be adjusted in this age group, potentially using age-based normative data as a comparison. 23,39 In the current study, we used the LSI for peak torque as well as peak torque as a percentage of body weight. The latter was an attempt to account for some of the heterogeneity in the cohort in terms of patients’ body weight. Despite this, the findings based on body weight were similar to those based on LSI, in that there were no strength differences between those patients who had a graft rupture and those who did not.
Limitations
The current study has several limitations. The cohort was recruited from a single, private, high-volume clinic, and only hamstring tendon grafts were used. As such, the results may not be generalizable to a more heterogeneous population. The strength testing was done as part of routine testing at 12 months after ACL reconstruction and not as part of an assessment of readiness to RTS. The assessment deliberately did not include hamstring to quadriceps strength ratios on the basis of our experience that this ratio can be difficult to interpret when patients have undergone ACL reconstruction using a hamstring tendon graft. Patients who had sustained a second ACL injury before 12 months could not be included because they did not undergo 12-month strength testing or strength testing before RTS and reinjury. This included 19 patients who sustained a graft rupture, which was the same number of graft ruptures after the 12-month strength assessment, albeit a lower percentage of the potentially eligible patient population compared with the percentage of eligible patients who sustained a graft rupture. It is unknown whether these patients had adequate or inadequate strength or strength asymmetries at the time of their graft rupture. Similarly, strength and LSI at the time of graft rupture were unknown in the patients in the eligible cohort. The minimum follow-up of the current study was 2 years, and it is possible that some patients may have sustained second ACL injuries at a later date but did not report these or received treatment elsewhere. Furthermore, as outlined earlier, because 2 graft ruptures occurred in patients who reported that they had not returned to their preinjury sports, we decided to include all patients in our analysis, regardless of RTS status. This may have potentially resulted in a bias to lower overall strength and LSI values in the group of patients who did not sustain a graft rupture. Finally, no account was made for other potential contributing factors that may affect function and performance and further explain the risk of second ACL injuries. These could include rehabilitation protocols, the treatment of concomitant injuries, social factors, and psychological factors.
Despite these limitations, the results of the current study raise questions about the emphasis placed on strength testing in the decision making regarding RTS after ACL reconstruction, particularly in a young patient cohort. It may be that other factors such as agility and balance testing, assessment of proprioception, and time since surgery may be more important or that a combination of tests would provide a better guide as to the safety of returning to sports. Nonetheless, restoration of quadriceps and hamstring strength is intuitively important for patients in order to RTS both safely and competently, but it is unclear whether a threshold level of strength or symmetry is required to minimize risk of further ACL injury. A recent review and meta-analysis reported that only 23% of patients passed the testing criteria before returning to sports after ACL reconstruction surgery. 42 Other studies have shown that as few as 20% to 60% of patients have LSI ≥85% for knee extensor strength at the time of RTS and that LSI <85% frequently persists for up to 2 years. 5,9,15,35,36,43 Despite the perceived importance of achieving strength symmetry, in a number of studies, only a minority of patients achieved this before returning to sports, particularly in the younger age group. 5,7,36
Conclusion
In young patients who underwent an ACL reconstruction, there was no association between quadriceps or hamstring strength at 12 months postoperatively and subsequent ACL graft ruptures. The role of strength tests as part of RTS testing after ACL reconstruction therefore warrants further investigation and clarification.
Footnotes
Final revision submitted March 22, 2022; accepted April 5, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.A.F. has received consulting fees from Smith & Nephew and is a paid associate editor for Orthopaedic Journal of Sports Medicine. B.M.D. has received speaking fees from Arthrex and Stryker. T.S.W. has received consulting fees from Medacta; speaking fees from Arthrex, Medacta, and Stryker; and royalties from Medacta. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Epworth HealthCare (study No. 57012).
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2(1):2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andernord D, Desai N, Bjornsson H, et al. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. [DOI] [PubMed] [Google Scholar]
- 3. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. [DOI] [PubMed] [Google Scholar]
- 4. Beischer S, Gustavsson L, Senorski EH, et al. Young athletes who return to sport before 9 months after anterior cruciate ligament reconstruction have a rate of new injury 7 times that of those who delay return. J Orthop Sports Phys Ther. 2020;50(2):83–90. [DOI] [PubMed] [Google Scholar]
- 5. Beischer S, Hamrin Senorski E, Thomee C, Samuelsson K, Thomee R. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1966–1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dekker TJ, Godin JA, Dale KM, et al. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 7. Ebert JR, Edwards P, Yi L, et al. Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2353–2361. [DOI] [PubMed] [Google Scholar]
- 8. Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–376. [DOI] [PubMed] [Google Scholar]
- 9. Fischer F, Fink C, Herbst E, et al. Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):418–425. [DOI] [PubMed] [Google Scholar]
- 10. Geffroy L, Lefevre N, Thevenin-Lemoine C, et al. Return to sport and re-tears after anterior cruciate ligament reconstruction in children and adolescents. Orthop Traumatol Surg Res. 2018;104(8 suppl):S183–S188. [DOI] [PubMed] [Google Scholar]
- 11. Greenberg E, Dabbous M, Leung A, et al. Less than half of youth athletes can achieve 90% limb symmetry on a battery of single leg hop tests. Orthop J Sports Med. 2019;7(3 suppl):2325967119S00052. [Google Scholar]
- 12. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Habets B, Staal JB, Tijssen M, van Cingel R. Intrarater reliability of the Humac NORM isokinetic dynamometer for strength measurements of the knee and shoulder muscles. BMC Res Notes. 2018;11(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Herbst E, Hoser C, Hildebrandt C, et al. Functional assessments for decision-making regarding return to sports following ACL reconstruction, part II: clinical application of a new test battery. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1283–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iriuchishima T, Shirakura K, Horaguchi T, et al. Age as a predictor of residual muscle weakness after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):173–178. [DOI] [PubMed] [Google Scholar]
- 17. Ithurburn MP, Longfellow MA, Thomas S, Paterno MV, Schmitt LC. Knee function, strength, and resumption of preinjury sports participation in young athletes following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2019;49(3):145–153. [DOI] [PubMed] [Google Scholar]
- 18. Johnston PT, Feller JA, McClelland JA, Webster KE. Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2022;30(4):1300–1310. [DOI] [PubMed] [Google Scholar]
- 19. Johnston PT, Feller JA, McClelland JA, Webster KE. Strength deficits and flexion range of motion following primary anterior cruciate ligament reconstruction differ between quadriceps and hamstring autografts. J ISAKOS. 2021;6:88–93. [DOI] [PubMed] [Google Scholar]
- 20. Kay J, Memon M, Marx RG, et al. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1019–1036. [DOI] [PubMed] [Google Scholar]
- 21. Kobayashi A, Higuchi H, Terauchi M, et al. Muscle performance after anterior cruciate ligament reconstruction. Int Orthop. 2004;28(1):48–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 23. Magill JR, Myers HS, Lentz TA, et al. Establishing age- and sex-specific norms for pediatric return-to-sports physical performance testing. Orthop J Sports Med. 2021;9(8):23259671211023101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Magnussen RA, Pedroza AD, Donaldson CT, Flanigan DC, Kaeding CC. Time from ACL injury to reconstruction and the prevalence of additional intra-articular pathology: is patient age an important factor? Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2029–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Muller U, Kruger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3623–3631. [DOI] [PubMed] [Google Scholar]
- 26. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. [DOI] [PubMed] [Google Scholar]
- 27. Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47(2):221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Neeter C, Gustavsson A, Thomee P, et al. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(6):571–580. [DOI] [PubMed] [Google Scholar]
- 29. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. [DOI] [PubMed] [Google Scholar]
- 30. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rauck RC, Apostolakos JM, Nwachukwu BU, et al. Return to sport after bone-patellar tendon-bone autograft ACL reconstruction in high school-aged athletes. Orthop J Sports Med. 2021;9(6):23259671211011510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. [DOI] [PubMed] [Google Scholar]
- 33. Shaw L, Finch CF. Trends in pediatric and adolescent anterior cruciate ligament injuries in Victoria, Australia 2005-2015. Int J Environ Res Public Health. 2017;14(6):599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–1805. [DOI] [PubMed] [Google Scholar]
- 35. Thomee R, Neeter C, Gustavsson A, et al. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1143–1151. [DOI] [PubMed] [Google Scholar]
- 36. Toole AR, Ithurburn MP, Rauh MJ, et al. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther. 2017;47(11):825–833. [DOI] [PubMed] [Google Scholar]
- 37. Ueda Y, Matsushita T, Araki D, et al. Factors affecting quadriceps strength recovery after anterior cruciate ligament reconstruction with hamstring autografts in athletes. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3213–3219. [DOI] [PubMed] [Google Scholar]
- 38. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 39. Webster KE, Feller JA. Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sports Med. 2018;6(8):2325967118788045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Webster KE, Feller JA. Who passes return-to-sport tests, and which tests are most strongly associated with return to play after anterior cruciate ligament reconstruction? Orthop J Sports Med. 2020;8(12):2325967120969425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 42. Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med. 2019;49(6):917–929. [DOI] [PubMed] [Google Scholar]
- 43. Wells L, Dyke JA, Albaugh J, Ganley T. Adolescent anterior cruciate ligament reconstruction: a retrospective analysis of quadriceps strength recovery and return to full activity after surgery. J Pediatr Orthop. 2009;29(5):486–489. [DOI] [PubMed] [Google Scholar]
- 44. Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2017;47(5):334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Werner BC, Yang S, Looney AM, Gwathmey FW, Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447–452. [DOI] [PubMed] [Google Scholar]