Abstract
Objective
To determine and compare the incidence rate of (osteo)chondral lesions of the ankle in patients with acute and chronic isolated syndesmotic injuries.
Design
A literature search was conducted in the PubMed (MEDLINE) and EMBASE (Ovid) databases from 2000 to September 2021. Two authors independently screened the search results, and risk of bias was assessed using the MINORS (Methodological Index for Non-Randomized Studies) criteria. Studies on acute and chronic isolated syndesmotic injuries with pre-operative or intra-operative imaging were included. The primary outcome was the incidence rate with corresponding 95% confidence intervals (CIs) of (osteo)chondral lesions of the ankle in combined and separate groups of acute and chronic syndesmotic injuries. Secondary outcomes were anatomic distribution and mean size of the (osteo)chondral lesions.
Results
Nine articles (402 syndesmotic injuries) were included in the final analysis. Overall (osteo)chondral lesion incidence was 20.7% (95% CI: 13.7%-29.9%). This rate was 22.0% (95% CI: 17.1-27.7) and 24.1% (95% CI: 15.6-35.2) for acute and chronic syndesmotic injuries, respectively. In the combined acute and chronic syndesmotic injury group, 95.4% of the lesions were located on the talar dome and 4.5% of the lesions were located on the distal tibia. (Osteo)chondral lesion size was not reported in any of the studies.
Conclusions
This meta-analysis shows that (osteo)chondral lesions of the ankle are present in 21% of the patients with isolated syndesmotic injuries. No difference in incidence rate was found between the different syndesmotic injury types and it can be concluded that the majority of lesions are located on the talar dome.
PROSPERO Registration Number:
CRD42020176641
Keywords: ankle, osteochondral lesion, meta-analysis, isolated syndesmotic injuries, incidence rate
Introduction
Syndesmotic injuries are usually caused by external rotation and combined hyper-dorsiflexion of the ankle.1,2 During this high-force injury mechanism, external rotational forces are being impacted on the distal tibia and talar dome, potentially resulting in intra-articular pathologies, such as damage to the osteocartilaginous unit. There is also a growing body of evidence documenting a high incidence of intra-articular injuries following acute ankle fractures. Martijn et al. 3 published a recent meta-analysis having shown that osteochondral lesions in the ankle were frequently seen in patients with acute ankle fractures with a high incidence rate of around 45%. Two different studies by D’Hooghe et al. 4 and Rellensmann et al. 5 found cartilage damage of the talar dome in patients with isolated unstable syndesmotic injuries being present in 23% to 48% of the cases. Left untreated, cartilage damage to the talus may have a severe impact on the quality of life and function, emphasizing the necessity to create awareness among care providers as to the potentially high incidence rate of intra-articular (osteo)chondral lesions ((O)CL) in isolated syndesmotic injuries and acute ankle fractures. 6 From the current literature, it is unclear what the exact incidence rate is of (O)CLs in both acute (<6 weeks from trauma to diagnosis) and chronic (>6 weeks from trauma to diagnosis) isolated syndesmotic. Furthermore, it is unclear whether this incidence rate is higher in the chronic isolated syndesmotic group versus the acute isolated syndesmotic group. Moreover, lesion size and anatomic distribution of potentially present (O)CLs remain unknown. Understanding the incidence of (O)CLs in patients with isolated syndesmotic injuries will aid clinicians in the early recognition and treatment of these intra-articular pathologies and may prevent the progression of lesion size as well as cysts, the deterioration of subchondral bone, and, as such, may improve clinical outcomes. Moreover, the presence of (O)CLs in patients with syndesmotic injuries can justify the necessity for earlier diagnostic measures and the application of adjuvant (minimally invasive) arthroscopy for patients with isolated syndesmotic injuries undergoing a stabilization procedure in order to address concomitant complaints and prevent further deterioration of intra-articular damage.
It is therefore the primary aim of the present systematic review to determine and compare the incidence of (O)CLs in the ankle in patients with acute and chronic isolated syndesmotic injuries. The secondary aim of this study is to assess the size and the anatomic distribution of the (O)CLs in such injuries. Our primary hypothesis is that (O)CLs frequently occur in all types of isolated syndesmotic injuries irrespective of acuteness of the injury. Our secondary hypothesis is that lesion size is heterogeneous and that most lesions are located in the anterolateral talar dome which is known to be a more common location for post-traumatic (O)CLs of the ankle. 7
Materials and Methods
The PRISMA statement (Preferred Reporting Items for Systematic reviews and Meta-Analyses) was used as a guideline for the present study. 8 The protocol for our systematic review and meta-analysis was prospectively registered in the PROSPERO register with registration number CRD42020176641. 9
Search Strategy
PubMed (Medline) and EMBASE databases were used for a systematic search of the literature from 2000 to September 2021. A backward citation chaining strategy was used to identify additional eligible studies. The full literature search is provided in the Appendix.
Eligibility Criteria and Study Selection
Clinical studies investigating the treatment or diagnosis of acute and chronic isolated syndesmotic injury and reporting concomitant findings of potential presence of (O)CLs of the ankle were included. Isolated syndesmotic injuries were defined as purely ligamentous injuries, as suggested by the ESSKA-AFAS consensus statement by van Dijk et al. 10 Remaining in- and exclusion criteria are described in Table 1 . Independent screening of the title/abstract and full-text of included articles was carried out by 2 reviewers (J.D. and S.J.). If the reviewers disagreed, the 2 reviewers discussed the matter and aimed to come to a decision. However, if the disagreement remained, the judgment of a third investigator (G.K.) was decisive. Studies were not blinded for author, affiliation or source, and no limitation was put on publication status.
Table 1.
Inclusion and Exclusion Criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| All clinical studies investigating patients with isolated stable or unstable syndesmotic injuries (acute and/or chronic) | <5 patients included |
| Necessity to mention whether pre-operatively or intra-operatively, a diagnosis of concomitant ankle (osteo)chondral injury is assessed | Patient overlap in different studies |
| All ages of the patients | Full-text article unavailable |
| Studies published in English | Level V evidence / review studies |
| Animal studies | |
| Cadaveric studies | |
| Conference abstracts | |
| Studies published before the year of 2000 |
Methodological Quality Assessment
The methodological quality of studies was assessed with the Methodological Index for Non-Randomized Studies (MINORS) tool and was scored by 2 independent reviewers (J.D. and S.J.). 11 The MINORS tool consists of 8 or 12 items for noncomparative or comparative nonrandomized studies, respectively. Maximum scores are 16 for non-comparative nonrandomized studies and 24 for comparative nonrandomized studies. An item was scored with a “0” when not reported, a “1” when inadequately reported, and a “2” when adequately reported. After independent evaluation, all disagreements were solved through discussion between the 2 independent reviewers. If the disagreement remained, the judgment of a third investigator (G.K.) was decisive.
Data Extraction
Data of included studies were extracted using Microsoft Excel (version 2020, macOS CATALINA) by 1 reviewer (J.D.) and cross-checked by a second author (S.J.). Standard study characteristics were retrieved as well as the following patient characteristics: number of patients and ankles, sex, age, method of diagnosis (magnetic resonance imaging (MRI), computed tomography (CT), arthroscopy, other), presence and number of (O)CLs, type of cartilage lesion (osteochondral or purely chondral), size of (O)CLs (diameter, surface area or volume), type of syndesmotic injury (acute, chronic) and associated grading system when available (e.g. West Point Grading System),4,12,13 and reported (in)stability of the syndesmotic injury. Additionally, anatomic distribution of (O)CLs was extracted.
Terminology
Many derivatives and combinations of chondral, cartilage, defect, lesions, and injury are currently used in the literature. Therefore, all reported osteochondral and purely cartilaginous lesions were considered an (O)CL and were referred to as an (osteo)chondral lesion in the results whenever not reported in sufficient detail, unless studies used an osteochondral classification system focusing separately on a subdivision of chondral versus osteochondral damage or when specifically qualitatively reported. 3 When cartilage damage was per-operatively assessed using arthroscopy, a lesion of the cartilage was defined as an (O)CL, because visualization of the subchondral bone is not always possible nor accurate during arthroscopy. Injuries were categorized into 2 groups based on the time period between initial trauma and diagnosis: (1) acute isolated syndesmotic up to 6 weeks after trauma and (2) chronic injuries diagnosed 6 weeks after the trauma.14-16 If the article in question did not mention the time from the injury to the time of diagnosis, it was chosen not to categorize the injury and it was marked as unknown: the incidence rate of (O)CLs in this subgroup was pooled as part of the overall incidence rate of (O)CLs in all types of isolated syndesmotic injuries, that is, acute and chronic combined (see statistical and data analysis below).
Statistical and Data Analysis
Concerning demographic data, in the case of categorical data, frequencies, and percentages were calculated. In the case of continuous data, weighted averages were calculated with the associated ranges of these averages. The primary outcome of the present study is the incidence rate of (O)CLs of the ankle in acute and chronic isolated syndesmotic injuries. Reported (O)CL incidence rates after syndesmotic injury were extracted from the original articles and pooled. If no (O)CL incidence percentage was reported, we calculated the (O)CL incidence by dividing the total number of (O)CLs by the total number of ipsilateral syndesmotic injuries reported in the article in question. First, an overall incidence rate in all isolated syndesmotic injury groups (that is, acute and chronic together) was calculated, and subsequently, a sub-analysis was performed to calculate the incidence rate of (O)CL in the acute isolated syndesmotic group and the chronic syndesmotic group. A log transformation was applied in order to calculate 95% confidence intervals for the incidence rates by means of random-effects model with inverse-variance weighting. 17 Subgroups with <5 observations (total included number of patients in 1 sub-group) were excluded due to a potential inclusion of a bias. Comparisons were made between the different groups in terms of time from injury to diagnosis and tested by use of Q-tests. Heterogeneity was quantified among studies (overall incidence group and separately analyzed subgroups) with the I2 statistic. 18 We chose an I2 <25% to represent low heterogeneity and a value >75% to indicate high heterogeneity. 18
Secondary outcomes were anatomical location distribution of the (O)CLs in the ankle joint and lesion size of the (O)CL. Anatomical location distribution of (O)CLs was described and classified according to the anatomical osseous location (i.e., talus or medial malleolus/ distal tibial plafond or lateral malleolus). If possible and reported, location was specified to more specified exact locations; e.g., anterior, medial, posterior, or lateral, and if possible subdivided into anterolateral, anteromedial, posterolateral, or posteromedial, or if possible in the 9-grid scale developed by Raikin et al. 19 In the case of lesion size reporting, lesion size was calculated by extracting individual diameter (antero-posterior, medio-lateral, and depth), surface area or volume of the separate lesion. Secondary outcomes were analyzed in a descriptive manner (numeric presentation and percentage presentation) and no between-group comparisons were made due to heterogeneity of reporting of data. Data analysis was conducted using Microsoft Excel (version 2020, macOS CATALINA) and R version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria) using the metaphor package. 20
Results
Search Results
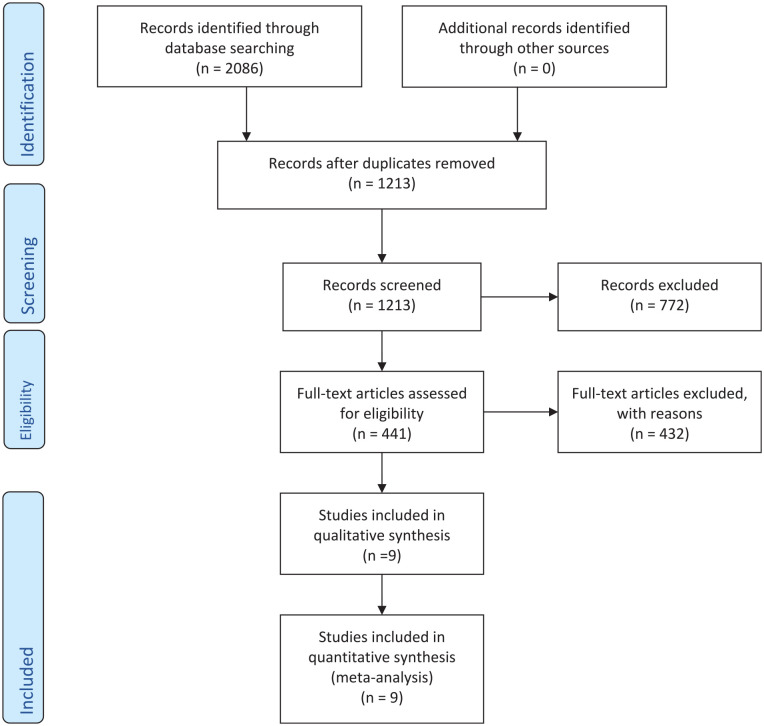
The selection of studies is shown in the PRISMA flow diagram ( Fig. 1 ). The literature search provided 1213 results. After screening the articles on title and abstract, and full-text screening, 9 articles were included – there was full agreement between the two independent authors on title, abstract, and full-text screening.4,5,21-27
Figure 1.
Literature selection algorithm—preferred reporting items for systematic reviews and meta-analyses (PRISMA).
Methodological Quality
For all cases, there was full agreement between the first 2 authors on the assessment of methodological quality of the studies. The overall methodological quality of the studies with the separate MINORS scores are to be appreciated in Table 2 . There was 1 comparative study, Han et al., 21 and its MINORS score was 14 out of 24 ( Table 2 ).
Table 2.
Study Characteristics and Patient Demographic Characteristics.
| Authors Journal | No. of Patients | Study Design | % Male | Mean Age | Pre-Operative Radiology Used | Grading System | Stable/Unstable | Author Definition of Acute/Chronic Definition | MINORS Score |
|---|---|---|---|---|---|---|---|---|---|
| D’Hooghe et al.
4
BJSM |
110 | Retrospective | 100% | 24.9 | MRI | West-Point IIB: 75, III: 35 |
All unstable (West-Point IIB and III) | All acute (<6 weeks from injury to diagnosis) | 10/16 |
| Han et al.
21
FAI |
20 | Prospective | 55% | 32.0 | MRI | N.R. | N.R. | Unclear definition of chronic syndesmotic injuries | 14/24 |
| Kent et al.
22
KSSTA |
116 | Retrospective | N.R. | N.R. | MRI | West-Point IIB: 204 |
All unstable (5.0mm blader through syndesmosis, all West-Point IIB) | Combination of acute and chronic (separate data available) | 7/16 |
| Mollon et al.
23
OJSM |
21 | Retrospective | 100% | 24.0 | MRI | N.R. | N.R. | Combination of acute and chronic (no separate data available)) | 7/16 |
| Rellensmann et al.
5
KSSTA |
18 | Retrospective | 78% | 33.7 | MRI | West-Point IIB: 13, III: 5, |
All unstable (West-Point IIB and III) | Combination of acute and chronic (no separate data available)) | 8/16 |
| Roemer et al.
24
AJSM |
53 | Prospective | N.R. | N.R. | MRI | N.R. | N.R. | All acute (<6 weeks from injury to diagnosis) | 8/16 |
| Sikka et al.
25
FAI |
36 | Retrospective | 100% | N.R. | MRI | Own system I: 4, II:5, III: 24, IV: 3 |
N.R. | All acute (<48 h from injury to diagnosis) | 10/16 |
| Takao et al.
26
AJSM |
17 | Retrospective | N.R. | N.R. | MRI | N.R. | N.R. | All chronic (>4 months from injury) | 9/16 |
| Zamzami et al.
27
FAS |
11 | Retrospective | 100% | 31.5 | MRI | N.R. | N.R. | All chronic (>2 years from injury) | 10/16 |
No. = number; MINORS = methodological index for non-randomized studies; MRI = magnetic resonance imaging; N.R. = not reported.
Evaluation of Characteristics of Included Studies
Articles included for final analysis totaled 402 syndesmotic injuries. The average age of the included patients was 26.9 (range of reported means, 24.0-33.7) years. In all, 52.4% of the affected ankles were on the right side, while 47.6% of the affected ankles were on the left side. Of the reported and extracted data, 94.0% was male and 6.0% was female. Pre-operatively, all patients underwent magnetic resonance imaging (MRI) of their injury. Other study, patient, and outcomes characteristics can be appreciated in Tables 2 and 3 .
Table 3.
(Osteo)Chondral Assessment.
| Authors, Journal | No of Patients | Diagnostic Method of (Osteo)Chondral Damage Assessment | (Osteo)Chondral or Osteochondral Definition | Classification System Used for (Osteo)Chondral Assessment | No of (O)CLs (Incidence Rate and 95% CI) | Anatomical Location Reported (Y/N), If Yes, Where | Size Reported (Y/N), If Yes How Large |
|---|---|---|---|---|---|---|---|
| D’Hooghe et al.
4
BJSM |
110 | Arthroscopy | (osteo)chondral | N.R. | 23 (20.9% 95% CI: 14.3-29.5) | Y: all talar (no further sub-specification on location) | N |
| Han et al.
21
FAI |
20 | Arthroscopy | (osteo)chondral | N.R. | 3 (15.0% 95% CI: 4.9-37.6) | Y: all talar (no further sub-specification on location) | N |
| Kent et al.
22
KSSTA |
116 | Arthroscopy | (osteo)chondral | N.R. | 22 (19.0% 95% CI: 12.8-27.1) | Y: all talar (no further sub-specification on location) | N |
| Mollon et al.
23
OJSM |
21 | MRI | Osteochondral | N.R. | 1 (4.8% 95% CI: 0.7-27.1) | N | N |
| Rellensmann et al.
5
KSSTA |
18 | Arthroscopy | (osteo)chondral | ICRS (8 grade II, 3 grade IV) | 11 (61.1% 95% CI: 37.9-80.2) a | Y: talar and tibial (9-grid scheme by Elias et al. 28 and Raikin et al. 19 ): 8 talar (1,2,3,1,1 lesions for zone 1,2,3,4 and 6, respectively) and 3 tibial lesions (1 medial, 1 lateral, 1 anterior) |
N |
| Roemer et al.
24
AJSM |
53 | MRI | Osteochondral | N.R. | 4 (7.5% 95% CI: 2.9-18.4) | Y: all talar (not further sub-specification on location) | N |
| Sikka et al.
25
FAI |
36 | MRI | Chondral | N.R. | 9 (25.0% 95% CI: 13.6-41.5) | N | N |
| Takao et al.
26
AJSM |
17 | MRI and arthroscopy | Osteochondral | Pritsch et al. 29 (no separate scores available) | 3 (17.6% 95% CI: 5.8-42.7) | N | N |
| Zamzami et al.
27
FAS |
11 | Arthroscopy | (osteo)chondral | N.R. | 3 (27.3% 95% CI: 9.0-58.6) | Y: all talar (not further sub-specification on location) | N |
CI = confidence interval; N.R. = not reported; MRI = magnetic resonance imaging; ICRS = international cartilage repair society score; (O)CL = (Osteo)Chondral Lesion.
Subgroups not analyzed due to <5 observations.
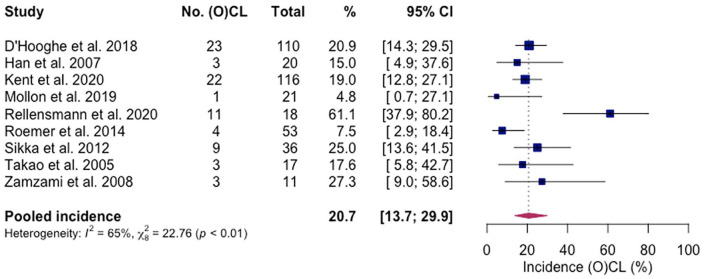
Overall Pooled Incidence Rate
The overall pooled incidence rate of (osteo)chondral lesions in the ankle joint in all isolated syndesmotic injuries—acute and chronic group combined—was 20.7% (95% CI: 13.7%-29.9%) as there were 79 reported lesions in a total of 402 patients (I 2 = 65%)4,5,21-27 ( Fig. 2 ).
Figure 2.
Forest plot of overall summarized incidence rate of (O)CLs of the ankle in all types of isolated syndesmotic injuries. CI = confidence interval; (O)CL = (Osteo)Chondral Lesion..
Anatomical location was reported in 6 studies4,5,21,22,24,27 (Table 3). There were 63 talar lesions (95.4%) and 3 tibial lesions (4.5%). One study 5 reported on a specified sub-localization distribution of the lesions, and these results can be appreciated in Table 3 . Lesion size was not reported in any of the studies.
A classification system for cartilage assessment was reported in 2 studies,5,26 comprising of the International Cartilage Repair Society score (ICRS) and the Pritsch et al. 29 classification system. Separate data on these lesions were extractable for the ICRS scores. Rellensmann et al. 5 concluded that there were 8 grade II and 3 grade IV lesions. A subgroup analysis on the distribution of chondral versus pure osteochondral injuries was not feasible due to the underreporting and heterogeneity of this outcome.
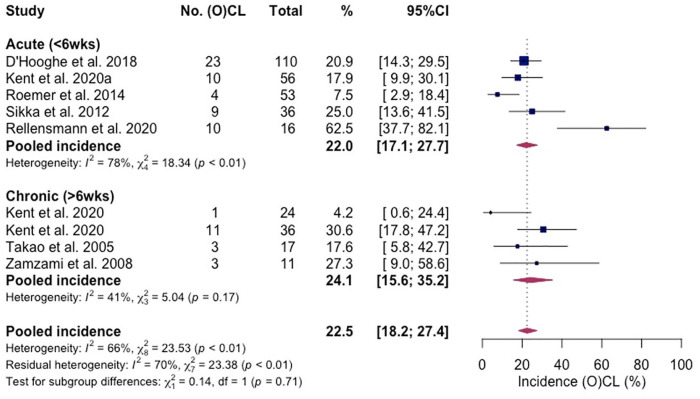
Acute Group
In the acute isolated syndesmotic group, there were 5 study groups included.4,5,22,24,25 Fifty-six (O)CLs in a total of 271 patients were found, having an associated (O)CL incidence rate of 22.0% (95% CI: 17.1-27.7%) (I2 = 78%) ( Fig. 3 ).
Figure 3.
Forest plot of the separate incidence rates of (O)CLs of the ankle in acute and chronic isolated syndesmotic injuries. CI = confidence interval; (O)CL = (Osteo)Chondral Lesion.
Four studies reported on anatomical location reporting of the lesions.4,5,22,24 The majority was located on the talar bone (94%), while a minority was located on the distal tibial bone (6%). Rellensmann et al. 5 used the 9-grid scheme by Elias et al. 28 and Raikin et al. 19 to describe the sub-localization distribution of the lesions on the distal tibial plafond and the talar dome. Seven lesions were found on the talus (1,2,2,1,1 lesions for zones 1, 2, 3, 4, and 6, respectively) and 3 on the tibia (1 medial, 1 lateral, 1 anterior). A subgroup analysis on the distribution of chondral versus pure osteochondral injuries was not feasible due to the underreporting and heterogeneity of this outcome.
Chronic Group
In the sub-group, 3 studies and 4 study groups were included,22,26,27 totaling 88 patients with 18 (O)CLs (incidence rate of 24.1%; 95% CI: 15.6-35.2) (I 2 = 41%) ( Fig. 3 ). Two studies22,27 reported the specific location distribution: All lesions were located on the talar dome. A subgroup analysis on the distribution of chondral versus pure osteochondral injuries was not feasible due to the underreporting and heterogeneity of this outcome.
Subgroup Comparisons
(O)CLs were not significantly more common in acute versus chronic isolated syndesmotic injuries (P = 0.71) ( Fig. 3 ).
Discussion
The present study shows that (O)CLs of the ankle are present in 21% of the patients with isolated syndesmotic injuries. The incidence rates of (O)CLs of the ankle were 22% in the acute group and 24% in the chronic isolated syndesmotic injuries group. These findings are of high clinical importance as it aids clinicians in the early recognition and treatment of these intra-articular pathologies and may prevent the progression of a lesion. Furthermore, the present study raises awareness among clinicians to (O)CLs in patients with acute and chronic syndesmotic injuries.
The prevalence of (O)CLs among patient with isolated syndesmotic injuries may be due to the position of the ankle mortise at the time of syndesmotic injury. The most likely mechanism is external rotation movement through the foot and the ankle with the ankle in dorsiflexion and the foot being pronated.1,30 Another mechanism that may cause a syndesmotic injury is a combination of external rotation and supination. 31 During both injury mechanisms, the axial load in combination with the previously described rotatory component of the injury may cause damage to the (osteo-)cartilaginous unit of the ankle joint. This is the same principle as the mechanism of (osteo) chondral injury in acute lateral ankle sprains or ankle fractures.32-35 This evidence is further underscored with a recent article by Tampere and D’Hooghe 35 comparing the ankle syndesmosis pivot shift to the trauma mechanism of the anterior cruciate ligament.
The incidence rate of 21% found in this study may be an underrepresentation of the actual incidence rate as not all included publications in this meta-analysis used arthroscopy to assess the (osteo)chondral damage. Three studies23-25 included in our analysis used magnetic resonance imaging (MRI) with a combined intra-operative arthroscopic assessment of concomitant (osteo)chondral damage. The intraoperative arthroscopic assessment of (osteo)chondral damage may have a higher sensitivity and specificity rate in comparison to the sole usage of MRI.34,36 Furthermore, the majority of the studies did not assess the incidence of (O)CLs as their primary outcome, but rather reported these as concomitant injuries during surgical procedures for isolated syndesmotic injuries. It may therefore be that the pooled incidence of ankle (O)CLs found in the present study underestimates the true incidence of (O)CLs, as exemplified by the high incidence found by Rellensmann et al. 5 having accurately and thoroughly performed the inspection of the total ankle joint with a specific focus on identifying the presence of intra-articular pathologies. In this context, it is not surprising that the incidence rate may be comparable to a recently published systematic review by Martijn et al. 3 on the incidence of (O)CLs in acute ankle fractures which reported 3 an incidence of 45% from a total of 1707 patients with acute ankle fractures directly after trauma.
It was found that there were no significant differences between the O(CL) incidence rates of the acute isolated syndesmotic (less than 6 weeks) injury group, and the chronic isolated syndesmotic (more than 6 weeks) injury group ( Fig. 3 ). It was hypothesized that chronic isolated syndesmotic injuries would yield a higher incidence of (O)CLs than in the acute isolated syndesmotic injury group. Chronic insufficiency together with concomitant deltoid insufficiency may lead to a talar shift thereby causing a decrease of the tibiotalar contact surface subsequently causing (osteo) cartilaginous damage to the ankle joint.37-43
Due to the heterogeneity of reported incidence rates, it was not possible to compare incidence rates between stable and unstable isolated syndesmotic injuries. D’Hooghe et al. 4 included solely unstable isolated syndesmotic ankle injuries in male professional football players and found that cartilage injury was significantly more common in West-Point Grade III syndesmotic injuries versus West-Point Grade IIB injuries (40% versus 12%, respectively). 44 Future research should study the relation between higher grades and the severity of cartilage damage in the ankle joint (lesion size, osteochondral nature versus solely cartilaginous nature, and relation to localization). This is in line with the previously published study by Martijn et al. 3 having demonstrated higher incidence rates in rotational type ankle fractures than non-rotational type ankle fractures.
Increased incidence of cartilage damage or osteochondral damage in the ankle in those patients with higher grades of injury or when associated with specific trauma mechanisms may introduce specific profiles for “high-risk” patients that have an increased chance of a concomitant injury to the (osteo)chondral unit in the ankle. This is a highly clinically relevant topic of discussion being of interest for future research as well as clinical interventions as it may introduce a cost-effective manner of concomitant (osteo)chondral damage assessment in “high-risk” profiles with immediate (evidence-based) treatment in the acute setting. Future applications and developments that may be suitable for this include the use of minimally invasive smaller arthroscopy techniques. A 2-mm bendable needle arthroscope has recently been developed, and in a recent study it was concluded that this novel system can safely and effectively be utilized for the visualization and surgical reach of the ankle joint thereby holding the potential to make ankle arthroscopy less invasive and more accessible.45,46 These novel innovations may be effective in helping to provide both a diagnostic and therapeutic protocol for high-risk patients with syndesmotic injuries to the ankle who could potentially have intra-articular (O)CLs present in the ankle joint.
With regard to the distribution of anatomical location of (O)CLs in the ankle joint, we conclude there was inadequate reporting of the anatomic localization of the lesions among included studies. The present study shows that for the summarized isolated syndesmotic injury group, the majority of the lesions were located on the talar bone (i.e., 95%), as opposed to 5% for the distal tibial bone. A more extensive in-depth analysis of anatomical location distribution of the (osteo)chondral damage in the isolated syndesmotic injury group was not reported nor performed in the included studies with the exception of Rellensmann et al. 5 specifically focusing on the distribution of the (osteo)chondral damage among the ankle joint. This study reported on the distribution of the lesions on the distal and the talar dome. The 9-grid scheme by Elias et al. 28 and Raikin et al. 19 was used and the study concluded that the majority of the lesions were located on the anterior talar dome with a higher incidence rate on the anterolateral talar dome. This finding is in contrast to the findings of a recently performed meta-analysis by van Diepen et al. 7 who found that 59% of the osteochondral lesions of the talus were located on the posterior side of the talar dome with the most commonly reported anatomical location being the centromedial zone (31%). As the publication by van Diepen et al. 7 consisted of mostly chronic osteochondral lesions and because of the fact that there is evidence that (antero)lateral lesions are potentially predominantly caused by traumatic events, it can be stated that the finding of the anteriorly located (O)CLs in the isolated syndesmotic injury group follows the specific evidence currently available on location distribution. The size of the lesions was not reported in any of the included studies. Further research projects may focus on accurately reporting concomitant (O)CLs in patients with isolated syndesmotic injuries, their distribution and localization, lesion characteristics, and lesion size.
This is the first study to assess the incidence rate of (O)CLs in ankles with acute and chronic isolated syndesmotic injuries. A strength of this study was the strict in- and exclusion criteria and the thorough selection of articles concerning the selection process. Specifically, articles were only included if assessment of intra-articular (O)CLs was performed and specifically reported in the methods section. Another strength of the present study is the usage and application of a random-effects model with an inverse variance weight statistic for pooling the data as this was chosen to be the most appropriate statistical method to summarize the results. This was chosen because the true effect size varied from study to study within the present meta-analysis thereby obviating the need for a random-effect model. 17
This study is, however, not without its limitations. First, the level of evidence of the included studies are considered of moderate quality as shown by the MINORS scores, and it should be stated that considerable heterogeneity was summarized. No sub-analyses were possible to compare the incidence rates of stable versus unstable isolated syndesmotic injuries, nor was it possible to compare the incidence rates of (O)CLs among different West-Point Grades. It was not possible to compare the incidence rates of osteochondral versus purely chondral lesions amongst the different isolated syndesmotic injury groups. Another limitation of the present study is that it was not reported whether the (O)CLs were symptomatic.
Conclusion
This meta-analysis shows that (osteo)chondral lesions of the ankle are present in 21% of the patients with isolated syndesmotic injuries. There was no significant difference in the incidence rate between the acute isolated syndesmotic injuries (22%) and the chronic isolated syndesmotic (24%). These findings are of high clinical importance as it aids clinicians in the early recognition and treatment of these intra-articular pathologies and may prevent the progression of a lesion. Furthermore, the present study raises awareness amongst clinicians to (O)CLs in patients with acute and chronic syndesmotic injuries.
Appendix
MEDLINE (OVID)
Database(s): Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, and Other Non-Indexed Citations and Search Strategy.
| # | Searches |
|---|---|
| 1 | (syndesmos* or syndesmotic or tibiofibular* or tibio fibular* or high ankle or AITFL or PITFL).ti, ab,kw. and (“Sprains and Strains”/ or Rupture/) |
| 2 | ((syndesmos* or syndesmotic or tibiofibular* or tibio fibular* or high ankle or AITFL or PITFL) adj3 (injur* or sprain* or instabilit* or unstable or rupture* or disruption* or tear* or torn)).ti, ab,kw. |
| 3 | 1 or 2 |
| 4 | letter/ or editorial/ or comment/ or (letter or editorial or comment).ti. |
| 5 | 3 not 4 |
EMBASE (OVID)
Database(s): Embase Classic + Embase Search Strategy.
| # | Searches |
|---|---|
| 1 | (syndesmos* or syndesmotic or tibiofibular* or tibio fibular* or high ankle or AITFL or PITFL).ti, ab,kw. and (exp sprain/ or ankle instability/ or rupture/) |
| 2 | ((syndesmos* or syndesmotic or tibiofibular* or tibio fibular* or high ankle or AITFL or PITFL) adj3 (injur* or sprain* or instabilit* or unstable or rupture* or disruption* or tear* or torn)).ti, ab,kw. |
| 3 | 1 or 2 |
| 4 | limit 3 to conference abstract status |
| 5 | 3 not 4 |
| 6 | letter/ or editorial/ or comment/ or exp conference paper/ or (letter or editorial or comment).ti. |
| 7 | 5 not 6 |
Footnotes
Author Contributions: All authors substantially contributed to the design (J.D., J.S., N.H., B.L., I.S., S.S., J.K., J.C., C.D., and G.K.). Data collection and analysis was performed by J.D. and J.S. Overall improvements were made by all authors for the final version of this manuscript.
Acknowledgments and Funding: The authors would like to thank F.S. van Etten-Jamudin of the Amsterdam UMC Medical Library for her help with the literature search.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: No ethical approval was requested nor necessary as the present study was a systematic review and meta-analysis of the literature.
Level of Evidence: Level IV, systematic review and meta-analysis.
ORCID iD: Jari Dahmen  https://orcid.org/0000-0002-6849-1008
https://orcid.org/0000-0002-6849-1008
References
- 1. Xenos JS, Hopkinson WJ, Mulligan ME, Olson EJ, Popovic NA. The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77:847-56. [DOI] [PubMed] [Google Scholar]
- 2. Beumer A, Valstar ER, Garling EH, Niesing R, Ginai AZ, Ranstam J, et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77:531-40. [DOI] [PubMed] [Google Scholar]
- 3. Martijn HA, Lambers KTA, Dahmen J, Stufkens SAS, Kerkhoffs G. High incidence of (osteo)chondral lesions in ankle fractures. Knee Surg Sports Traumatol Arthrosc. 2021;29:1523-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. D’Hooghe P, Grassi A, Alkhelaifi K, Calder J, Baltes TPA, Zaffagnini S, et al. Return to play after surgery for isolated unstable syndesmotic ankle injuries (West Point grade IIB and III) in 110 male professional football players: a retrospective cohort study. Br J Sports Med. 2020;54:1168-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rellensmann K, Behzadi C, Usseglio J, Vosseller JT, Böcker W, Polzer H, et al. Acute, isolated and unstable syndesmotic injuries are frequently associated with intra-articular pathologies. Knee Surg Sports Traumatol Arthrosc. 2021;29:1516-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vopat ML, Vopat BG, Lubberts B, DiGiovanni CW. Current trends in the diagnosis and management of syndesmotic injury. Curr Rev Musculoskelet Med. 2017;10:94-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Diepen PR, Dahmen J, Altink JN, Stufkens SAS, Kerkhoffs G. Location distribution of 2,087 osteochondral lesions of the talus. Cartilage. 2021;1344S-1353S. doi: 10.1177/1947603520954510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chien PF, Khan KS, Siassakos D. Registration of systematic reviews: PROSPERO. BJOG. 2012;119:903-5. [DOI] [PubMed] [Google Scholar]
- 10. van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, Ciuffreda M, et al. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24:1200-16. [DOI] [PubMed] [Google Scholar]
- 11. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-6. [DOI] [PubMed] [Google Scholar]
- 12. Switaj PJ, Mendoza M, Kadakia AR. Acute and chronic injuries to the syndesmosis. Clin Sports Med. 2015;34:643-77. [DOI] [PubMed] [Google Scholar]
- 13. Lubberts B, D’Hooghe P, Bengtsson H, DiGiovanni CW, Calder J, Ekstrand J. Epidemiology and return to play following isolated syndesmotic injuries of the ankle: a prospective cohort study of 3677 male professional footballers in the UEFA Elite Club Injury Study. Br J Sports Med. 2019;53:959-64. [DOI] [PubMed] [Google Scholar]
- 14. Espinosa N, Smerek JP, Myerson MS. Acute and chronic syndesmosis injuries: pathomechanisms, diagnosis and management. Foot Ankle Clin. 2006;11:639-57. [DOI] [PubMed] [Google Scholar]
- 15. Valkering KP, Vergroesen DA, Nolte PA. Isolated syndesmosis ankle injury. Orthopedics. 2012;35:e1705-10. [DOI] [PubMed] [Google Scholar]
- 16. Scranton PE, Jr, McDermott JE, Rogers JV. The relationship between chronic ankle instability and variations in mortise anatomy and impingement spurs. Foot Ankle Int. 2000;21:657-64. [DOI] [PubMed] [Google Scholar]
- 17. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97-111. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Raikin SM, Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28:154-61. [DOI] [PubMed] [Google Scholar]
- 20. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1-48. [Google Scholar]
- 21. Han SH, Lee JW, Kim S, Suh JS, Choi YR. Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int. 2007;28:336-42. [DOI] [PubMed] [Google Scholar]
- 22. Kent S, Yeo G, Marsland D, Randell M, Forster B, Lutz M, et al. Delayed stabilisation of dynamically unstable syndesmotic injuries results in worse functional outcomes. Knee Surg Sports Traumatol Arthrosc. 2020;28:3347-53. [DOI] [PubMed] [Google Scholar]
- 23. Mollon B, Wasserstein D, Murphy GM, White LM, Theodoropoulos J. High ankle sprains in professional ice hockey players: prognosis and correlation between magnetic resonance imaging patterns of injury and return to play. Orthop J Sports Med. 2019;7:2325967119871578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roemer FW, Jomaah N, Niu J, Almusa E, Roger B, D’Hooghe P, et al. Ligamentous injuries and the risk of associated tissue damage in acute ankle sprains in athletes: a cross-sectional MRI study. Am J Sports Med. 2014;42:1549-57. [DOI] [PubMed] [Google Scholar]
- 25. Sikka RS, Fetzer GB, Sugarman E, Wright RW, Fritts H, Boyd JL, et al. Correlating MRI findings with disability in syndesmotic sprains of NFL players. Foot Ankle Int. 2012;33:371-8. [DOI] [PubMed] [Google Scholar]
- 26. Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005;33:686-92. [DOI] [PubMed] [Google Scholar]
- 27. Zamzami MM, Zamzam MM. Chronic isolated distal tibiofibular syndesmotic disruption: diagnosis and management. Foot Ankle Surg. 2009;15:14-9. [DOI] [PubMed] [Google Scholar]
- 28. Elias I, Raikin SM, Schweitzer ME, Besser MP, Morrison WB, Zoga AC. Osteochondral lesions of the distal tibial plafond: localization and morphologic characteristics with an anatomical grid. Foot Ankle Int. 2009;30:524-9. [DOI] [PubMed] [Google Scholar]
- 29. Pritsch M, Horoshovski H, Farine I. Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1986;68:862-5. [PubMed] [Google Scholar]
- 30. Fritschy D. An unusual ankle injury in top skiers. Am J Sports Med. 1989;17:282-5; discussion 285-6. [DOI] [PubMed] [Google Scholar]
- 31. Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60:957-85. [PubMed] [Google Scholar]
- 32. Kerkhoffs GM, Kennedy JG, Calder JD, Karlsson J. There is no simple lateral ankle sprain. Knee Surg Sports Traumatol Arthrosc. 2016;24:941-3. [DOI] [PubMed] [Google Scholar]
- 33. Vuurberg G, Hoorntje A, Wink LM, van der Doelen BFW, van den Bekerom MP, Dekker R, et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018;52:956. [DOI] [PubMed] [Google Scholar]
- 34. Blom RP, Mol D, van Ruijven LJ, Kerkhoffs G, Smit TH. A single axial impact load causes articular damage that is not visible with micro-computed tomography: an ex vivo study on caprine tibiotalar joints. Cartilage. 2021;13:1490S-1500S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tampere T, D’Hooghe P. The ankle syndesmosis pivot shift “Are we reviving the ACL story? ” Knee Surg Sports Traumatol Arthrosc. 2021;29:3508-11. [DOI] [PubMed] [Google Scholar]
- 36. von Engelhardt LV, Lahner M, Klussmann A, Bouillon B, Dàvid A, Haage P, et al. Arthroscopy vs. MRI for a detailed assessment of cartilage disease in osteoarthritis: diagnostic value of MRI in clinical practice. BMC Musculoskelet Disord. 2010;11:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang DY, Jiao C, Ao YF, Yu JK, Guo QW, Xie X, et al. Risk factors for osteochondral lesions and osteophytes in chronic lateral ankle instability: a case series of 1169 patients. Orthop J Sports Med. 2020;8:2325967120922821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sugimoto K, Takakura Y, Okahashi K, Samoto N, Kawate K, Iwai M. Chondral injuries of the ankle with recurrent lateral instability: an arthroscopic study. J Bone Joint Surg Am. 2009;91:99-106. [DOI] [PubMed] [Google Scholar]
- 39. Bischof JE, Spritzer CE, Caputo AM, Easley ME, DeOrio JK, Nunley JA, II, et al. In vivo cartilage contact strains in patients with lateral ankle instability. J Biomech. 2010;43:2561-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58:356-7. [PubMed] [Google Scholar]
- 41. Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36:372-84. [DOI] [PubMed] [Google Scholar]
- 42. Mococain P, Bejarano-Pineda L, Glisson R, Kadakia RJ, Akoh CC, Chen J, et al. Biomechanical effect on joint stability of including deltoid ligament repair in an ankle fracture soft tissue injury model with deltoid and syndesmotic disruption. Foot Ankle Int. 2020;41:1158-64. [DOI] [PubMed] [Google Scholar]
- 43. Longo UG, Loppini M, Fumo C, Lanotte A, Trovato U, Risi Ambrogioni L, et al. Deep deltoid ligament injury is related to rotational instability of the ankle joint: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2021;29:1577-83. [DOI] [PubMed] [Google Scholar]
- 44. Calder JD, Bamford R, Petrie A, McCollum GA. Stable versus unstable grade ii high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy. 2016;32:634-42. [DOI] [PubMed] [Google Scholar]
- 45. Stornebrink T, Altink JN, Appelt D, Wijdicks CA, Stufkens SAS, Kerkhoffs G. Two-millimetre diameter operative arthroscopy of the ankle is safe and effective. Knee Surg Sports Traumatol Arthrosc. 2020;28:3080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stornebrink T, Emanuel KS, Shimozono Y, Karlsson J, Kennedy JG, Kerkhoffs G. A change in scope: redefining minimally invasive. Knee Surg Sports Traumatol Arthrosc. 2020;28:3064-5. [DOI] [PubMed] [Google Scholar]