Abstract
Background
Worldwide, many countries have adopted colorectal cancer (CRC) screening programmes, often based on faecal occult blood tests (FOBTs). CRC screening aims to detect advanced neoplasia (AN), which is defined as CRC or advanced adenomas. FOBTs fall into two categories based on detection technique and the detected blood component: qualitative guaiac‐based FOBTs (gFOBTs) and faecal immunochemical tests (FITs), which can be qualitative and quantitative. Screening with gFOBTs reduces CRC‐related mortality.
Objectives
To compare the diagnostic test accuracy of gFOBT and FIT screening for detecting advanced colorectal neoplasia in average‐risk individuals.
Search methods
We searched CENTRAL, MEDLINE, Embase, BIOSIS Citation Index, Science Citation Index Expanded, and Google Scholar. We searched the reference lists and PubMed‐related articles of included studies to identify additional studies.
Selection criteria
We included prospective and retrospective studies that provided the number of true positives, false positives, false negatives, and true negatives for gFOBTs, FITs, or both, with colonoscopy as reference standard. We excluded case‐control studies. We included studies in which all participants underwent both index test and reference standard ("reference standard: all"), and studies in which only participants with a positive index test underwent the reference standard while participants with a negative test were followed for at least one year for development of interval carcinomas ("reference standard: positive"). The target population consisted of asymptomatic, average‐risk individuals undergoing CRC screening. The target conditions were CRC and advanced neoplasia (advanced adenomas and CRC combined).
Data collection and analysis
Two review authors independently screened and selected studies for inclusion. In case of disagreement, a third review author made the final decision. We used the Rutter and Gatsonis hierarchical summary receiver operating characteristic model to explore differences between tests and identify potential sources of heterogeneity, and the bivariate hierarchical model to estimate sensitivity and specificity at common thresholds: 10 µg haemoglobin (Hb)/g faeces and 20 µg Hb/g faeces. We performed indirect comparisons of the accuracy of the two tests and direct comparisons when both index tests were evaluated in the same population.
Main results
We ran the initial search on 25 June 2019, which yielded 63 studies for inclusion. We ran a top‐up search on 14 September 2021, which yielded one potentially eligible study, currently awaiting classification.
We included a total of 33 "reference standard: all" published articles involving 104,640 participants. Six studies evaluated only gFOBTs, 23 studies evaluated only FITs, and four studies included both gFOBTs and FITs. The cut‐off for positivity of FITs varied between 2.4 μg and 50 µg Hb/g faeces. For each Quality Assessment of Diagnostic Accuracy Studies (QUADAS)‐2 domain, we assessed risk of bias as high in less than 20% of studies. The summary curve showed that FITs had a higher discriminative ability than gFOBTs for AN (P < 0.001) and CRC (P = 0.004). For the detection of AN, the summary sensitivity of gFOBTs was 15% (95% confidence interval (CI) 12% to 20%), which was significantly lower than FITs at both 10 μg and 20 μg Hb/g cut‐offs with summary sensitivities of 33% (95% CI 27% to 40%; P < 0.001) and 26% (95% CI 21% to 31%, P = 0.002), respectively. Results were simulated in a hypothetical cohort of 10,000 screening participants with 1% CRC prevalence and 10% AN prevalence. Out of 1000 participants with AN, gFOBTs missed 850, while FITs missed 670 (10 μg Hb/g cut‐off) and 740 (20 μg Hb/g cut‐off). No significant differences in summary specificity for AN detection were found between gFOBTs (94%; 95% CI 92% to 96%), and FITs at 10 μg Hb/g cut‐off (93%; 95% CI 90% to 95%) and at 20 μg Hb/g cut‐off (97%; 95% CI 95% to 98%). So, among 9000 participants without AN, 540 were offered (unnecessary) colonoscopy with gFOBTs compared to 630 (10 μg Hb/g) and 270 (20 μg Hb/g) with FITs. Similarly, for the detection of CRC, the summary sensitivity of gFOBTs, 39% (95% CI 25% to 55%), was significantly lower than FITs at 10 μg and 20 μg Hb/g cut‐offs: 76% (95% CI 57% to 88%: P = 0.001) and 65% (95% CI 46% to 80%; P = 0.035), respectively. So, out of 100 participants with CRC, gFOBTs missed 61, and FITs missed 24 (10 μg Hb/g) and 35 (20 μg Hb/g). No significant differences in summary specificity for CRC were found between gFOBTs (94%; 95% CI 91% to 96%), and FITs at the 10 μg Hb/g cut‐off (94%; 95% CI 87% to 97%) and 20 μg Hb/g cut‐off (96%; 95% CI 91% to 98%). So, out of 9900 participants without CRC, 594 were offered (unnecessary) colonoscopy with gFOBTs versus 594 (10 μg Hb/g) and 396 (20 μg Hb/g) with FITs.
In five studies that compared FITs and gFOBTs in the same population, FITs showed a higher discriminative ability for AN than gFOBTs (P = 0.003).
We included a total of 30 "reference standard: positive" studies involving 3,664,934 participants. Of these, eight were gFOBT‐only studies, 18 were FIT‐only studies, and four studies combined both gFOBTs and FITs. The cut‐off for positivity of FITs varied between 5 µg to 250 µg Hb/g faeces. For each QUADAS‐2 domain, we assessed risk of bias as high in less than 20% of studies. The summary curve showed that FITs had a higher discriminative ability for detecting CRC than gFOBTs (P < 0.001). The summary sensitivity for CRC of gFOBTs, 59% (95% CI 55% to 64%), was significantly lower than FITs at the 10 μg Hb/g cut‐off, 89% (95% CI 80% to 95%; P < 0.001) and the 20 μg Hb/g cut‐off, 89% (95% CI 85% to 92%; P < 0.001). So, in the hypothetical cohort with 100 participants with CRC, gFOBTs missed 41, while FITs missed 11 (10 μg Hb/g) and 11 (20 μg Hb/g). The summary specificity of gFOBTs was 98% (95% CI 98% to 99%), which was higher than FITs at both 10 μg and 20 μg Hb/g cut‐offs: 94% (95% CI 92% to 95%; P < 0.001) and 95% (95% CI 94% to 96%; P < 0.001), respectively. So, out of 9900 participants without CRC, 198 were offered (unnecessary) colonoscopy with gFOBTs compared to 594 (10 μg Hb/g) and 495 (20 μg Hb/g) with FITs. At a specificity of 90% and 95%, FITs had a higher sensitivity than gFOBTs.
Authors' conclusions
FITs are superior to gFOBTs in detecting AN and CRC in average‐risk individuals. Specificity of both tests was similar in "reference standard: all" studies, whereas specificity was significantly higher for gFOBTs than FITs in "reference standard: positive" studies. However, at pre‐specified specificities, the sensitivity of FITs was significantly higher than gFOBTs.
Keywords: Humans, Adenoma, Adenoma/diagnosis, Colorectal Neoplasms, Colorectal Neoplasms/diagnosis, Early Detection of Cancer, Early Detection of Cancer/methods, Guaiac, Hemoglobins, Occult Blood, Prospective Studies, Retrospective Studies, Sensitivity and Specificity
Plain language summary
Which faecal blood test is more accurate in detecting bowel cancer and large polyps in population screening?
Background One of the most common types of cancer diagnosed is large bowel or colorectal cancer (CRC). Early detection, before symptoms appear, makes it easier to treat bowel cancer and increases the chance of survival. Taking part in a bowel cancer screening program can lead to early detection and removal of large or advanced polyps (advanced adenomas), which are considered to be a precursor to bowel cancer. Simple faecal tests are used to detect the presence of blood in stool, which could be an early sign of bowel cancer or polyps. Two types of faecal blood tests used in population screening are: guaiac‐based faecal occult blood tests (gFOBTs) and faecal immunochemical tests (FITs). Large, older studies have shown that screening with gFOBTs can reduce mortality. In a systematic review of the literature, we compared the accuracy of these two tests in order to assess which test gives the best results in population screening for bowel cancer, and, secondarily, for advanced neoplasia (which comprises bowel cancer and advanced polyps together).
Study characteristics We carried out a detailed search of online databases for studies that evaluated or compared (one of) these two tests in CRC screening. The review included only studies in average‐risk individuals over 40 years of age without symptoms. The reference standard to compare the test results with was a total endoscopic examination of the large bowel with a camera on a flexible tube passed through the anus (colonoscopy). We reviewed two types of studies: those in which all participants underwent both the stool test and colonoscopy; and those in which only participants with an unfavourable result on the stool test underwent colonoscopy (in these studies, participants who did not have a colonoscopy after the stool test were followed for at least one year to see if they would be diagnosed with colorectal cancer). The evidence is current until 25 June 2019. We ran a top‐up search on 14 September 2021, which yielded only one potentially eligible study, currently awaiting classification.
Test characteristics
The gFOBT 'screenees' – i.e. those who participate in screening – are instructed to collect two faecal samples from three consecutive bowel movements and to smear this on six stool panels. If there is blood in the stool, the panel changes colour. The number of coloured panels for referral to colonoscopy varies between screening programs. In most programs, a single coloured panel is sufficient for referral; however, in others, the number of panels is set at five out of six.
The FIT screenees are instructed to collect one faecal sample from one bowel movement, and to collect this with a brush or spatula into a tube. This tube is then send to a laboratory where the concentration of blood in the stool can be measured. Depending on the height of this concentration, above or below the so‐called cut‐off or threshold, the screenee is referred for colonoscopy. This cut‐off differs per screening program.
Key results We analysed 63 studies including almost 4 million individuals. The results of this review indicate that if, in theory, 10,000 people take part in screening with a faecal blood test and 100 people in this group have CRC:
‐ out of the 100 people with CRC, 24 will be missed in those being screened with FITs.
‐ out of the 100 people with CRC, 61 will be missed in those being screened with gFOBTs.
We also looked at participants with large polyps, CRC, or both. If, in theory, 10,000 people take part in screening with a faecal blood test and 1000 people in this group have large polyps, CRC, or both:
‐ out of the 1000 people with large polyps, CRC, or both, 850 will be missed in those being screened with gFOBTs.
‐ out of the 1000 people with large polyps, CRC, or both, 670 will be missed in those being screened with FITs.
In this theoretical group of 10,000 screenees:
‐ 594 people being screened with FITs will be offered an 'unnecessary' colonoscopy – unnecessary because they do not have CRC; and
‐ 594 people being screened with gFOBTs will be offered an 'unnecessary' colonoscopy.
From the results described above, we can see that FITs miss less CRC than gFOBTs, while an equal number of screenees from each type of blood test undergo an unnecessary colonoscopy.
How reliable are the results of the studies in this review? The results of the studies are reliable, as the included studies mostly met the quality criteria we specified before commencing the review.
Future research More research is needed to investigate whether, in the long term, FIT screening can reduce the number of bowel cancer cases and deaths, and to compare these findings with those from gFOBT screening.
Summary of findings
Summary of findings 1. Diagnostic accuracy of gFOBTs compared to FITs.
| Diagnostic accuracy of gFOBTs compared to FITs | ||||
| Participants/ population | Asymptomatic, average‐risk individuals over the age of 40 years undergoing colorectal cancer (CRC) screening | |||
| Prior testing | Only the results of the first screening round were included in this analysis | |||
| Settings | Population‐based colorectal cancer screening | |||
| Index test | Guaiac‐based faecal occult blood test (gFOBT) or faecal immunochemical test (FIT)* | |||
| Importance | Many screening programmes worldwide are currently changing from gFOBT‐ to FIT‐based screening | |||
| Reference standard | Colonoscopy is the reference standard for the diagnosis of colorectal cancer. If a colonoscopy was not completed, a CT‐colonography (or double‐contrast barium enema) was used as a surrogate. | |||
| Studies | Prospective and retrospective studies including average‐risk individuals invited for colorectal cancer screening "Reference standard: all": all screenees underwent both the index test and colonoscopy (n = 33) "Reference standard: positive": only screenees with a positive index test underwent colonoscopy and all screen negative participants were followed for at least one year (n = 30). |
|||
| Quality concerns | Due to strict inclusion criteria, most studies were of high quality. Few studies had an unclear risk of bias due to poor reporting of a pre‐specified cut‐off value. Only three studies had a high risk of bias regarding the selection of study population. For these studies, sensitivity analyses showed no significant differences in outcome when excluding these studies from analyses. | |||
| Test/subgroup* | ||||
| Studies (participants) |
Summary sensitivity (%, 95% CI) |
Summary specificity (%, 95% CI) |
Implications* | |
| "Reference standard: all" studies | ||||
| gFOBT advanced neoplasia |
11 (17,622) | 15 (12 to 20) | 94 (92 to 96) | Out of 1000 participants with AN, 850 will be missed. Among those without AN, 540 will be offered an (unnecessary) colonoscopy. |
| FIT** advanced neoplasia |
16 (49,081) | 33 (27 to 40) | 93 (90 to 95) | Out of 1000 participants with AN, 670 will be missed. Among those without AN, 630 will be offered an (unnecessary) colonoscopy. |
| gFOBT colorectal cancer |
9 (17,340) | 39 (25 to 55) | 94 (91 to 96) | Out of 100 participants with CRC, 61 will be missed. Among those without CRC, 594 will be offered an (unnecessary) colonoscopy. |
| FIT** colorectal cancer |
13 (42,335) | 76 (57 to 88) | 94 (87 to 97) | Out of 100 participants with CRC, 24 will be missed. Among those without CRC, 594 will be offered an (unnecessary) colonoscopy. |
| "Reference standard: positive" studies | ||||
| gFOBT colorectal cancer |
12 (1,349,890) | 59 (55 to 64) | 98 (98 to 99) | Out of 100 participants with CRC, 41 will be missed. Among those without CRC, 198 will be offered an (unnecessary) colonoscopy. |
| FIT** colorectal cancer |
10 (1,274,115) | 89 (85 to 92) | 94 (92 to 95) | Out of 100 participants with CRC, 11 will be missed. Among those without CRC, 594 will be offered an (unnecessary) colonoscopy. |
| Conclusion | FITs have a higher sensitivity and similar specificity for both AN and CRC compared to gFOBTs in an average‐risk population. In "reference standard: positive" participants, sensitivity for CRC was higher with FITs, but specificity was higher with gFOBTs. | |||
| CAUTION: the results in this table should not be interpreted in isolation from the results of the individual included studies contributing to each summary test accuracy measure. These are reported in the main body of the review. | ||||
| * In a hypothetical situation with prevalence of CRC of 1%, prevalence of AN of 10% and an assumed 100% participation rate in a population of n = 10,000 ** Results for a FIT cut‐off of 10 µg Hb/g faeces are shown | ||||
| AN = advanced neoplasia; CI = confidence interval; CRC = colorectal cancer; FIT = faecal immunochemical test; gFOBT = guaiac‐based faecal occult blood test; Hb = haemoglobin | ||||
Background
Based on the Wilson and Jungner criteria published in 1968 (Wilson 1968), and updated by the World Health Organization in 2008 (Andermann 2008), screening is justified when: (1) a disease is common and associated with significant morbidity or mortality; (2) screening tests are sufficiently accurate in detecting early stage disease, are acceptable to invitees, and are feasible in general clinical practice; (3) treatment after early detection by screening improves prognosis relative to treatment after usual diagnosis; and (4) the potential benefits outweigh the potential harms and costs of screening. Colorectal cancer (CRC) screening fulfils all of these criteria. CRC screening aims to detect advanced neoplasia (AN), which is defined as CRC or advanced adenomas. Advanced adenomas have a size of 10 mm or larger, and/or at least 25% villous histology, and/or high grade dysplasia. Risk factors for CRC include inflammatory bowel disease, a sedentary lifestyle, smoking, alcohol intake, and being overweight (Johnson 2013). While genetics seem to play a role in the development of CRC, most CRCs appear sporadic (Carethers 2015).
There are various methods for CRC screening. These vary in terms of the level of supporting evidence, effectiveness, test‐related burden, costs, and willingness of the target population to undergo screening. The screening modalities for CRC broadly fall into two categories: (a) faecal tests (i.e. faecal occult blood tests and faecal DNA testing); and (b) partial or full structural exams (i.e. flexible sigmoidoscopy, colonoscopy, and computed tomography (CT)‐colonography). Colonoscopy can be used as the reference standard for those with a positive screening test or as a primary CRC screening tool (Quintero 2012).
Stool blood tests are conventionally known as faecal occult blood tests (FOBTs), which are used as a two‐step testing approach in CRC screening (i.e. a positive test result requires further examination with visualisation of the colon, predominantly by means of colonoscopy). FOBT detects a higher proportion of CRCs and a lower proportion of advanced adenomas, since CRCs tend to have a more constant bleeding pattern and give rise to higher amounts of blood in stools than advanced adenomas, which are believed to bleed more intermittently (Van Roon 2011). In this way, FOBT screening identifies those individuals who are most likely to have advanced neoplasia. Therefore, after a positive FOBT, visualisation of the colon and rectum should follow. Colonoscopy is considered the reference standard for detection of AN with high sensitivity and specificity (both above 90%), and colonoscopy has the advantage that (adenomatous) polyps and early CRCs can be removed during the procedure. A meta‐analysis of the accuracy of colonoscopy (performed for various indications) reported that the pooled miss rate for adenomas of 10 mm or larger was 2%, for adenomas between 5 mm and 10 mm was 13%, and for adenomas between 1 mm and 5mm was 26% (Van Rijn 2006).
FOBTs fall into two categories based on the detected component of blood: guaiac‐based FOBTs (gFOBTs) and the more recently developed faecal immunochemical tests (FITs) for haemoglobin (Hb). These tests are described in detail at Index test(s).
To date, there are no long‐term prospective randomised data that demonstrate that FITs are superior to gFOBTs in terms of reducing CRC‐related mortality. However, a recent ecological study compared regions in Italy with and without population FIT screening. CRC‐specific mortality was 22% lower in areas with a FIT screening program compared with areas without a screening program (Zorzi 2015).
With this review, we aimed to compare the test accuracy measures of gFOBT and FIT screening in order to answer the question “Which FOBT is superior in population‐based CRC screening?”
Target condition being diagnosed
The target conditions were CRC and AN. FOBT screening primarily aims at early detection of bleeding colorectal neoplasia, since only bleeding lesions can be detected by stool blood tests. CRC screening in general aims at lowering CRC mortality by early detection of CRC and lowering CRC incidence by removal of this pre‐malignant lesion; that is, adenomatous polyps.
Index test(s)
Guaiac‐based faecal occult blood tests
Guaiac‐based FOBTs (gFOBTs) enable detection of occult blood in stool through the pseudo‐peroxidase activity of haem. Haem is an iron‐containing compound that forms the non‐protein part of Hb. However, peroxidase also reacts with non‐human haem present in red meat. Also, several fresh fruits and vegetables contain peroxidase activity, which may lead to false‐positive test results (Konrad 2010; Sinatra 1999). Vitamin C may block the peroxidase reaction, resulting in false‐negative test results. Guaiac FOBTs may detect bleeding from any site in the gastrointestinal tract, including the stomach, as haem remains relatively stable during transport through the gastrointestinal tract (Young 2009). The usual gFOBT protocol consists of three test cards, each containing two panels. The screenee – i.e. someone who participates in screening – is instructed to collect two faecal samples from three consecutive bowel movements yielding a total of six stool panels. Applying a hydrogen peroxide reagent to the faeces on the guaiac material in the panel leads to oxygenation of guaiac, which in turn leads to a blue colour change when haem is present. A panel is considered positive if such coloration appears (Kuipers 2013). The number of positive panels for referral to colonoscopy varies between screening programmes. In most programmes, a single positive panel is sufficient for referral; however, in others, the number of positive panels is set at five out of six. In this case, less than five positive panels imply renewed gFOBT testing. Prior to faecal sampling, individuals are asked to restrict their diet and medication as these might affect the number of false‐positive and false‐negative test results (Rockey 1999).
The sensitivity and specificity of gFOBT screening varies widely due to the variation in type of test (brand), instructions for stool collection, number of stool samples per screening round, the use of non‐hydrated or rehydrated stool samples, double reading of the test, the number of positive panels used to refer a screened person for colonoscopy, and the interval between successive screening rounds (Young 2015). In some trials, rehydrated gFOBT has been studied: rehydration reduces the false‐negative rate (improves sensitivity) while increasing the false‐positive rate (reduces specificity) (Liebermann 2001; Mandel 1993).
Guaiac‐based FOBTs are the only stool tests for which there is evidence of efficacy in terms of CRC‐related mortality reduction from prospective, randomised controlled trials (RCTs). These trials from the USA, United Kingdom, Denmark, and Sweden demonstrated that multiple rounds of annual or biennial gFOBT screening can reduce CRC‐related mortality by approximately 13% to 33% (Hardcastle 1996; Kronborg 1996; Lindholm 2008; Mandel 1993). The American trial, which used rehydrated gFOBT, also demonstrated a reduction in the incidence of CRC (Mandel 1993). A subsequent meta‐analysis reported a pooled 15% reduction in CRC‐related mortality among the three biennial screening trials with gFOBT compared to controls (Hewitson 2008). The American trial recently reported an overall reduction in CRC mortality of 27% after 30 years of follow‐up (Shaukat 2013). The efficacy of gFOBT screening in reducing CRC‐related mortality is limited due to a limited sensitivity for detecting CRC and low sensitivity for detection of advanced adenomas (Allison 1996). Furthermore, the process of analysing gFOBT is time consuming and is hampered by the possibility of inaccurate processing and evaluation (Young 2002).
Faecal immunochemical tests (FITs)
FITs have several technological advantages compared to guaiac‐based screening. FITs specifically target human globin, a protein that, along with haem, constitutes the Hb molecule (Young 2015). Therefore, FITs only detect human blood, in contrast to gFOBTs which can detect other substances, leading to false‐positive results. For this reason, FITs are less subject to interference from dietary factors and medication. In a meta‐analysis, use of oral anticoagulants, aspirin, or non‐steroidal anti‐inflammatory drugs was not associated with positive predictive value; therefore, there might be no need to withdraw these drugs before FIT screening (Nieuwenburg 2019). In addition, FITs are more specific for lower gastrointestinal tract bleeding since globin is degraded by digestive enzymes in the upper gastrointestinal tract. This improves their specificity for neoplasia in the colon and rectum (Young 2015). The sample collection for most FIT variants is less demanding than for gFOBT sampling, both in terms of requiring only a single sample and less direct handling of stool (smear cards for gFOBT versus brush/spatula for FIT testing). Furthermore, FIT screening does not require dietary restrictions. Both qualitative and quantitative FITs have been developed and are described below.
Qualitative FITs
Qualitative tests require a manual interpretation of test results as positive or negative. There is a range of such tests on the market. They often use immunochromatographic technology, and allow for simple office‐based analysis. Test performances may differ between brands, as qualitative FITs provide dichotomous test results and thresholds for a positive test result are different between brands (Chiang 2014a; Hundt 2009). Also, like gFOBTs, inter‐observer variations in interpretation of test results may influence performance (Freitas 2013).
Quantitative FITs
Quantitative FITs, on the contrary, can be analysed automatically and quantify the amount of Hb found in the stool sample. One advantage of quantitative FITs in CRC screening programmes is that the cut‐off level (i.e. the amount of Hb above which the test is considered positive and individuals are referred for follow‐up examination) can be adjusted (Young 2015). This allows the number of FIT‐positives to be matched with available resources for further investigation; in particular, colonoscopy capacity (Wilschut 2011). Quantitative FITs have further important advantages over qualitative FITs due to the use of automated analysis. This automation removes inter‐observer variation in interpretation of test results, improves reproducibility, and allows for high‐throughput testing (Young 2015). Nevertheless, studies suggest variable performance of different brands of quantitative FITs, even when the same standardised cut‐off is used (Chiang 2014a; Wieten 2020).
Clinical pathway
FOBT screening is based on the principle that a large proportion of colorectal neoplasia bleeds microscopically before any clinical signs or symptoms become noticeable. Bleeding tends to be intermittent, and blood is distributed unevenly in the stool. The concept of detecting CRC by testing for blood in the stool is based on the observation that cancers bleed because of disruption of the normal mucosa (Kuipers 2013). The amount of blood increases with the size of the polyp or the stage of the cancer, or both (Ciatto 2007; Edwards 2005; Levi 2007; Rozen 2006). In general, the amount of faecal Hb tends to be absent or low in those without neoplasia, higher for those with advanced adenomas, and highest for those with CRC (Van Doorn 2015).
Prior test(s)
There are no tests prior to gFOBT or FIT.
Role of index test(s)
The tests under evaluation are two FOBTs: gFOBTs and FITs. FITs can be both quantitative as well as qualitative; the qualitative test does not report individual faecal Hb concentrations. Both tests are intended for population‐based CRC screening.
Alternative test(s)
There are several alternative tests that can be used for CRC screening purposes. These tests vary in the level of supporting evidence, attendance, effectiveness, test‐related burden, and costs. Alternative screening modalities usually considered effective as CRC screening tools include: flexible sigmoidoscopy, colonoscopy, computed tomography‐colonography and, more recently, capsule endoscopy, faecal DNA testing, and serum molecular markers (Schreuders 2016; Spada 2014).
Rationale
Many countries in Europe, North America, and Australia have adopted a CRC screening program, often based on FOBT (Schreuders 2015). Screening by means of gFOBT has been proven to reduce CRC‐related mortality (Shaukat 2013). The results on accuracy of FIT screening and its subsequent effect on decreasing CRC‐related mortality are not yet available. The main explanation for this is that many countries have already implemented a CRC screening program. In addition, decisions on the optimal screening test have to be based on data about the sensitivity and specificity, existing RCT results, and modelling (Winawer 1997).
Screening aims to detect CRC and AN before symptoms occur, which leads to more early‐stage cancers with more treatment options and better survival. False‐positive results lead to unnecessary colonoscopies and false‐negative results may unjustly reassure individuals, leading to a delayed detection of CRC.
Objectives
To compare the diagnostic test accuracy of gFOBT and FIT screening for detecting advanced colorectal neoplasia in average‐risk individuals.
Methods
Criteria for considering studies for this review
Types of studies
We included two different types of studies in this review, and categorised them as follows.
"Reference standard: all": all accuracy studies in which all participants underwent both the index test and the reference standard. Diagnostic case‐control studies were considered inappropriate for this review because such studies are likely to overestimate diagnostic performance (Deeks 2013). Moreover, literature suggests that measures of accuracy may vary with the prevalence and stage‐distribution of the target condition (Leeflang 2009). For instance, the sensitivity of a test will often vary according to the severity of the detected disease (e.g. advanced CRCs are more easily detected with FOBTs than early‐stage tumours). For these reasons, we did not include case‐control studies in this review.
"Reference standard: positive": all accuracy studies in which all participants with a positive index test were referred for the reference standard and all participants with a negative index test were followed for at least one year to identify development of interval carcinomas. Only data from the first screening round were included for analysis.
We included studies irrespective of their publication status and language of publication, unless exclusion was explicitly justified. We did not include abstracts.
Participants
Asymptomatic average‐risk individuals aged 40 years and above were considered as representative for a CRC screening program. We chose an age restriction of 40 years and older as the risk of CRC increases with age. Therefore, most screening programmes target the population aged 50 years or older (Schreuders 2015). Study participants included people volunteering for a medical health check‐up (including CRC screening), as well as individuals identified from population registers, and general practitioner or managed care organisation records.
Index tests
The index test was either a gFOBT or FIT. Guaiac‐based FOBTs enable detection of occult blood in stool through the pseudo‐peroxidase activity of haem, whereas FITs targets human globin specifically. A FIT result can be qualitative (i.e. negative or positive) or it can be quantitative (i.e. reporting the concentration of Hb in the stool sample).
Comparator test
We included studies regardless of whether they made comparisons with other CRC screening modalities.
Target conditions
For "reference standard: all", we defined the target conditions as CRC and AN. We defined CRC as the invasion of malignant cells beyond the lamina muscularis mucosa. We classified people with an intramucosal carcinoma or carcinoma in situ as having high‐grade dysplasia (Lansdorp‐Vogelaar 2012). AN includes CRC and advanced adenomas. Adenomas with a greatest dimension of at least 10 mm, or with 25% or higher villous component, and/or with high‐grade dysplasia were classified as advanced adenomas (Lansdorp‐Vogelaar 2012). For each included study, we assessed whether these definitions were applied. If a study adopted another definition, we stated this in the Characteristics of included studies table.
For "reference standard: positive" studies, we defined only CRC as the target condition, as for these types of studies, only data on interval carcinomas are available (e.g. with the use of cancer registries).
Reference standards
We included studies for this review if colonoscopy was used as the primary reference standard. Only in case of an incomplete colonoscopy did we accept CT‐colonography or double‐contrast barium enema as reference standard. Furthermore, in "reference standard: positive" studies, participants with a negative index test result had to be followed for at least one year to assess the development of interval carcinomas. We defined interval carcinomas as CRC diagnosed in an FOBT‐negative screenee in the period between two successive FOBT screening rounds (Sanduleanu 2014).
Exclusion criteria
We excluded studies where more than 5% of the population consisted of high‐risk individuals. We defined high‐risk individuals as people: with a history of CRC; with a personal history of adenoma(s); scheduled for diagnostic colonoscopy because of hereditary CRC syndromes or a positive family history of CRC; with symptoms and complaints suspicious for CRC, such as rectal blood loss, changed bowel habits, or weight loss; or with a history of inflammatory bowel disease. We also excluded studies in which a positive gFOBT test result needed to be confirmed by a positive FIT test result or vice versa. We excluded studies in which less than 75% of the participants with a positive FOBT underwent colonoscopy (or, in case of an incomplete colonoscopy, underwent CT‐colonography or double‐contrast barium enema).
Search methods for identification of studies
Electronic searches
To identify appropriate studies, the Medical School Library of the Erasmus Medical Center (review author WB), in collaboration with the Trial Search Coordinator of the Cochrane Colorectal Cancer Group, conducted a literature search using the electronic databases Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 6) in the Cochrane Library, MEDLINE, Embase, BIOSIS, Science Citation Index Expanded, and Google Scholar on 25 June 2019 (Appendix 1, Appendix 2, Appendix 3, Appendix 4, Appendix 5, Appendix 6). The MEDLINE, Embase, and BIOSIS searches were run in Ovid. We placed no restrictions on date or language of the articles being reviewed. We performed a further top‐up search on 14 September 2021.
Searching other resources
We handsearched the references of all included studies for additional trials. In addition, we searched for relevant articles citing the studies included in the review. We defined relevant articles as any article published within the five years preceding our search. Furthermore, we examined the first 20 results from ‘PubMed Related Articles’ after sorting by publication date from newest to oldest.
Data collection and analysis
Selection of studies
Two review authors (EJG and EHS or PHW) independently assessed whether the titles and abstracts were eligible for further reading. Two review authors read the retrieved articles in their entirety to assess eligibility for inclusion. We resolved any disagreements about study inclusion through discussion with a third review author (AvR). Personal acquaintances and native speakers associated with our departments translated articles written in languages other than English. We listed all studies that did not meet the inclusion criteria, as ascertained by reading the full article, in a separate table with reasons for exclusion. We used the reference management software EndNote X7 (EndNote 2015) for the selection process (Bramer 2016).
Data extraction and management
We extracted data from those trials that fulfilled the inclusion criteria. The data extracted for both CRC and AN were:
positivity rate (PR; i.e. the proportion of participants having a positive index test result);
true positives (TP; i.e. participants having a positive index test result, followed by detection of AN by means of the reference standard);
false positives (FP; i.e. participants having a positive index test result, but no AN when assessed with the reference standard;
true negatives (TN; i.e. participants having a negative index test result, and no AN during colonoscopy for "reference standard: all" studies and no interval CRC identified during follow‐up for "reference standard: positive" studies;
false negatives (FN; i.e. participants having a negative index test result, and AN during colonoscopy for "reference standard: all" studies and interval CRC identified during follow‐up for "reference standard: positive" studies.
The analyses only include the main outcome measures sensitivity and specificity (which were derived from TP, FP, TN, FN). For CRC, we included data from both "reference standard: all" and "reference standard: positive" studies, and for AN we included data from "reference standard: all" studies only. For both study types, the extracted data were merged into separate 2 x 2 tables (containing TP, FP, FN, TN). We excluded non‐interpretable test results and FOBT‐positive participants who refused to undergo the reference standard from the 2 x 2 table and, in consequence, from the meta‐analysis. If data were lacking in a specific article, we contacted the principal investigators to ask for the original data, or tried to reconstruct the aforementioned cell frequencies from the information that was published, or both. If these efforts were unsuccessful, we excluded the study. We also contacted principal investigators of the included studies to clarify aspects of methods and results, and asked for any unpublished data concerning FOBT characteristics, when necessary. The numbers of participants analysed in our review are stated in the Characteristics of included studies table.
We extracted data for all possible cut‐offs. When multiple cut‐offs were available, we used a cut‐off of 10 µg Hb/g for analyses, unless specifically stated otherwise. Not all FITs use the same reporting units for the measured Hb concentration (e.g. ng Hb/mL). Therefore we transformed all cut‐offs into the internationally accepted unit of µg Hb/g faeces, as proposed by the Expert Working Group of the World Endoscopy Organization (Fraser 2012). Two review authors (EJG and EHS or PHW) independently extracted all data. In addition, we extracted data on the target population, country, age range, gender, inclusion and exclusion criteria, and definitions of AN. These are described in the Characteristics of included studies table. We entered the extracted data into Review Manager 2020. We did not use a piloted data collection form.
Assessment of methodological quality
Three review authors (EJG, EHS, PHW) independently assessed the quality of each study using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS and QUADAS‐2) tools (Whiting 2003; Whiting 2011). We included several items (questions) from the original QUADAS in the methodological quality assessment along with the QUADAS‐2 signalling questions (Appendix 7). We excluded some of the questions from the QUADAS‐2 tool because they were not applicable. Details of each study are described in Table 2 and Table 3. If data were not specified in the article, we mentioned this. When study authors did not respond, we contacted manufacturers, if necessary, to retrieve additional details about the test used.
1. Overview of test characteristics per study for "reference standard: all" studies.
| Study | Country | Test brand | gFOBT | FIT |
FIT quant./quali. |
FIT 10 µg | FIT 20 µg | AN | CRC | Other cut‐off | No. of stools |
| Ahlquist 2008a | USA | Hemoccult | + | + | + | 3 | |||||
| Ahlquist 2008b | Hemoccult Sensa | + | + | + | 3 | ||||||
| Aniwan 2015 | Thailand | SD Bioloine FOB | + | Qualitative | + | + | + | 50 ng Hb/mL = 10 µg/g | 1 | ||
| Aniwan 2017 | Thailand | OC‐Sensor | + | Qualitative | + | + | + | + | 1 | ||
| Brenner 2012 | Germany | HemoCARE (gFOBT) | + | + | + | 3 | |||||
| ImmoCARE‐C (FIT) | + | Qualitative | + | + | Unknown | 3 | |||||
| Brenner 2013 | Germany | Hemoccult | + | + | + | 1 | |||||
| Brenner 2018 | Germany | FOB‐Gold | + | Qualitative | + | + | + | + | 1 | ||
| Chang 2017 | Taiwan | OC‐Sensor | + | Qualitative | + | + | + | 1 | |||
| Chen 2014 | Taiwan | OC‐Light | + | Qualitative | + | + | + | 1 | |||
| Cheng 2002 | Taiwan | OC‐Hemodia | + | Qualitative | + | + | + | 1 | |||
| Chiu 2013 | Taiwan | OC‐Light | + | Qualitative | + | + | + | 1 | |||
| Chiu 2016a | Taiwan | OC‐Sensor | + | Qualitative | + | + | + | 1 | |||
| Cruz‐Correa 2007 | USA | Hemoccult II | + | + | ‐ | 3 | |||||
| De Wijkerslooth 2012 | Netherlands | OC‐Sensor | + | Quantitative | + | + | + | + | 1 | ||
| Graser 2009 | Germany | gFOBT brand not specified | + | + | + | 3 | |||||
| FOB‐Gold | + | Quantitative | + | + | 14 ng Hb/mL = 2.4 µg/g | 2 | |||||
| Haug 2011 | Germany | RIDASCREEN | + | Quantitative | + | + | + | + | 1 | ||
| Hernandez 2014 | Spain | OC‐Sensor | + | Quantitative | + | + | + | + | 1 | ||
| Hoepffner 2006 | Hemoccult | + | + | ‐ | 1 | ||||||
| Hb ELISA Immunodiagnostik | + | Unknown | + | + | ‐ | 10 µg/g | 1 | ||||
| Imperiale 2004 | USA | Hemoccult II | + | + | + | 3 | |||||
| Imperiale 2014 | Canada and USA | OC‐Sensor | + | Quantitative | + | + | + | 1 | |||
| Khalid‐de Bakker 2011 | Netherlands | OC‐Sensor | + | Quantitative | + | + | + | 1 | |||
| Kim 2017 | South Korea | OC‐Sensor | + | Qualitative | + | + | + | 1 | |||
| Levy 2014b | USA | Inverness Clearview | + | Qualitative | + | + | 50 µg/g faeces | 1 | |||
| Levy 2014c | Alere Clearview | + | Qualitative | + | + | 6 µg/g faeces | 1 | ||||
| Levy 2014a | Polymedco OC‐Light | + | Qualitative | + | + | + | 1 | ||||
| Levy 2014d | Quidel QuickVue | + | Qualitative | + | + | 50 µg/g faeces | 1 | ||||
| Liebermann 2001 | USA | Hemoccult II | + | + | + | 3 | |||||
| Nakama 2000 | Japan | Iatro Hemcheck | + | Qualitative | + | Not reported | 2 | ||||
| Nakazato 2006 | Japan | OC‐Hemodia | Quantitative | + | + | Not reported | 2 | ||||
| Omata 2011 | Japan | OC‐Micro | + | Quantitative | + | + | + | + | 1 | ||
| Park 2010 | South Korea | Hemoccult II | + | + | + | 3 | |||||
| OC‐Sensa | + | Quantitative | + | + | + | + | 3 | ||||
| Ribbing Wilen 2019 | Sweden | OC‐Sensor | + | Qualitative | + | + | + | 2 | |||
| Siripongpreeda 2016 | Thailand | ABON Biopharm | + | Qualitative | + | + | 6 µg/g faeces | 1 | |||
| Sohn 2005 | South Korea | OC‐Hemodia | + | Quantitative | + | + | 100 ng/mL = 20 µg/g faeces | 1 | |||
| Sung 2003 | China | Hemoccult II | + | + | + | 3 | |||||
| Wong 2014 | Hong Kong | Hemosure | + | Qualitative | + | + | 50 ng/mL = 50 µg/g faeces | 1 | |||
| Wu 2014 | Taiwan | ACON Laboratories | + | Qualitative | + | + | 50 ng/mL = 6 µg/g faeces | 1 |
Abbreviations: ng/mL: nanogram per millilitre; µg: microgram; g: gram; AN: advanced neoplasia; CRC: colorectal cancer; gFOBT: guaiac‐based faecal occult blood test; FIT: faecal immunochemical test
2. Overview of test characteristics per study for "reference standard: positive" studies.
| Study | Country | Test brand | gFOBT | FIT |
FIT quant./quali. |
FIT 10 µg | FIT 20 µg | Other cut‐off | CRC | No. of stools |
| Arana‐Arri 2017a | Spain | OC‐Sensor Micro | + | Quantitative | + | + | 1 | |||
| Arana‐Arri 2017b | FOB‐Gold | + | Quantitative | + | + | 1 | ||||
| Blanks 2019 | England | Hemascreen | + | + | 3 | |||||
| Bouvier 1999 | France | Hemoccult II | + | + | not described | |||||
| Burón 2019 | Spain | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Castiglione 2007 | Italy | OC‐Hemodia | + | Quantitative | + | + | 1 | |||
| Chen 2016a | Taiwan | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Chiang 2014a | Taiwan | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Chiang 2014b | HM‐Jack | + | Quantitative | + | + | 1 | ||||
| Crotta 2012 | Italy | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Denters 2012a | Netherlands | OC‐Sensor Micro | + | Quantitative | + | + | 1 | |||
| Denters 2012b | Hemoccult II | + | + | 3 | ||||||
| Digby 2016 | Scotland | OC‐Sensor | + | Quantitative | 80 µg/g faeces | + | 1 | |||
| Faivre 2004 | France | Hemoccult II | + | + | 3 | |||||
| Giai 2014 | France | Hemoccult II | + | + | 3 | |||||
| Itoh 1996 | Japan | OC‐Hemodia | + | Qualitative | + | + | 1 | |||
| Jensen 2016 | USA | OC FIT‐CHEK | + | Quantitative | + | + | 1 | |||
| Juul 2018 | Denmark | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Kapidzic 2017 | Netherlands | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Kronborg 1987 | Denmark | Hemoccult II | + | + | 3 | |||||
| Launoy 2005 | France | Magstream | + | Quantitative | 20 ng/mL (67 µg Hb/g faeces) | + | 2 | |||
| Levi 2011a | Israel | Hemoccult Sensa | + | + | 3 | |||||
| Levi 2011b | OC‐Micro | + | Quantitative | 70 ng/mL (14 µg Hb/g faeces) | + | 3 | ||||
| McNamara 2014 | Ireland | OC‐Sensor | + | Quantitative | + | + | 2 | |||
| Nakama 1996 | Japan | Monohaem | + | Qualitative | + | 1 | ||||
| Paimela 2010 | Finland | Hemoccult | + | + | 3 | |||||
| Parente 2013 | Italy | HM‐Jack | + | Quantitative | 100 ng/mL (250 µg Hb/g faeces) | + | 1 | |||
| Parra‐Blanco 2010 | Spain | Hemofec | + | + | 3 | |||||
| Parra‐Blanco 2010 | OC‐Light | + | Qualitative | + | + | 1 | ||||
| Paszat 2016 | Canada | Hema‐Screen | + | + | 3 | |||||
| Robinson 1996 | England | Hemoccult | + | + | 3 | |||||
| Robinson 1996 | Hemeselect | + | Qualitative | + | 1 or 3 | |||||
| Sieg 2002 | Germany | Unknown | + | Quantitative | 1994 to 1998: 10 µg/g Nov 1998 to 2000: 5 µg/g |
+ | 1 | |||
| Steele 2009 | Scotland | Hema‐Screen | + | + | 3 | |||||
| Van Roon 2013 | Netherlands | OC‐Sensor | + | Quantitative | + | + | 1 | |||
| Zorzi 2018 | Italy | OC‐Hemodia | + | Quantitative | + | + | 1 |
AN: advanced neoplasia; CRC: colorectal cancer; g: gram; gFOBT: guaiac‐based faecal occult blood test; FIT: faecal immunochemical test; ng/mL: nanogram per millilitre; µg: microgram
Statistical analysis and data synthesis
Descriptive analysis
The descriptive analysis provides an overview of all available studies. Tables were split by gFOBT or FIT, and by "reference standard: all" or "reference standard: positive" studies. We obtained study‐specific estimates and exact 95% confidence intervals (CIs) of sensitivity and specificity, and displayed these in forest plots per test type. We used different symbols per test type, in order to create a clear overview of between‐test variability.
Inferential statistics
In statistical analyses, we compared the performance of gFOBTs versus FITs. We complied with the methods and techniques introduced and explained in Chapter 10 of the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy (Macaskill 2013). We initially explored the data by plotting the study‐specific sensitivities and specificities on coupled forest plots in RevMan software. Based on the available reported 2 x 2 data, we used the Rutter and Gatsonis hierarchical summary receiver operating characteristic (HSROC) model to explore differences between tests and identify potential sources of heterogeneity (Rutter 2001), and the bivariate hierarchical model to estimate sensitivity and specificity at common thresholds (when there were at least three studies) (Reitsma 2005; Van Houwelingen 2002). For studies that evaluated multiple stool tests in the same person, we allowed that these contributed an observation to both series of tests. Thus, we included these studies twice in the data set. When at least three studies were available in which both gFOBTs and FITs were evaluated in the same population, we performed direct comparisons.
For studies using different cut‐off points for test positivity, HSROC models were fitted using the 'proc nlmixed' command of SAS version 9.4 (Deeks 2013). From the model, we estimated sensitivities at specified specificities (90% and 95%) for "reference standard: all" and "reference standard: positive" studies separately. Investigations of heterogeneity and comparisons between tests considered differences in accuracy, threshold, and shape parameters; if there was no significant difference in shape, a common shape was assumed. For comparisons of tests, we investigated models allowing different variance terms for both tests, but these did not converge, so models were fitted with the assumption of common variance. We obtained P values from likelihood ratio (LR) tests comparing the significance of the difference between the two tests. For quantitative FITs where multiple cut‐offs were available, we used the cut‐off of 10 µg Hb/g faeces.
To obtain summary sensitivities and specificities with 95% confidence intervals from tests that used consistent cut‐offs, the bivariate model was fitted using the 'meqrlogit' command of Stata software. We analysed separately the two most commonly used cut‐offs for FITs (10 µg and 20 µg Hb/g faeces). We compared gFOBTs and FITs by adding test type as a covariate in the bivariate model, in addition to allowing for separate variances of the random effects for sensitivity and specificity of both tests. We derived P values comparing the absolute differences between sensitivities or specificities from the model. Model output provided confidence and prediction region parameters and summary estimates of test accuracy measures per test type (gFOBT or FIT).
Investigations of heterogeneity
The magnitude of observed heterogeneity was depicted graphically by the prediction ellipse. We planned to address heterogeneity by adding covariates of interest to the HSROC model. In our objectives, we described the factors that we aimed to include in our heterogeneity analyses. However, there are several caveats to keep in mind, as follows.
We assessed heterogeneity related to gender as percentage of male participants. Investigation of heterogeneities within other population characteristics was not feasible due to lack of information provided in individual studies. Nevertheless, only (studies with) average‐risk individuals, as defined in our protocol, were included. The well‐defined criteria resulted in homogenous studies, according to prediction ellipses. Investigation of heterogeneities within cancer stage, distribution, and cancer location was not feasible due to lack of information provided in individual studies.
We assessed heterogeneity related to the number of tests or the number of stools per screening round, or both.
We performed summary estimates of sensitivity and specificity for the two most common cut‐off levels to refer screenees for further evaluation by the reference standard (i.e. cut‐off value for FITs in µg/mL or the number of positive panels for gFOBTs). We assessed heterogeneity related to the quantitative or qualitative nature of FITs.
Sensitivity analyses
We performed sensitivity analyses in which the QUADAS‐2 items were used to identify studies that scored differently on risk of bias for one of the four QUADAS‐2 domains, to determine the effect of poor study quality on the overall results. We tested the impact of each study by removing each one from the analysis separately and recalculating the summary estimates.
Assessment of reporting bias
Investigation of publication bias in diagnostic test accuracy studies has proven to be problematic because many studies are done without ethical approval or study registration (Deeks 2005; Leeflang 2008; Song 2002). Therefore, identification of studies from registration until final publication of the results is not possible (Leeflang 2008). Thus, we have not assessed reporting bias in this review.
Other published versions of this review
This review is based on a published Cochrane protocol (Van Roon 2011). Additionally, previous versions of the review were published as part of two theses (Grobbee 2016; Schreuders 2016).
Summary of findings
In the summary of findings table, we simulate a hypothetical cohort of 10,000 screening participants. The prevalence of CRC is 1% and the prevalence of AN is 10% in this cohort. The results of screening with FITs, with 10 µg Hb/g faeces as cut‐off, or gFOBTs are depicted in this hypothetical cohort. The number of studies and total number of included participants in this meta‐analysis for each screening strategy are depicted, together with the summary sensitivity and summary specificity. We assessed confidence intervals (95%) for the outcomes for summary sensitivity and specificity. The implication column shows the number of participants in the hypothetical cohort with CRC or AN that would be missed with gFOBTs or FITs and the number of participants that would be offered an (unnecessary) colonoscopy.
Results
Results of the search
Initial searches
The search, up to date until 25 June 2019, identified 7305 records. We found an additional 12 records through other sources. After removal of duplicates, 4425 records remained. Of these, we excluded 3897 records, based on title and abstract. We retrieved full‐text articles for the remaining 528 records, and assessed these for eligibility. In total, we excluded 465 articles because they met one of the exclusion criteria (see Figure 1), as follows:
1.

Flow diagram of search and included studies
197 articles: only FOBT‐positive people had undergone the reference standard without follow‐up of FOBT‐negative people;
53 articles: did not focus on average‐risk persons;
40 articles: did not use colonoscopy as the first choice of reference standard;
19 articles: only provided data on cumulative mortality over multiple screening rounds, making it impossible to determine absolute numbers of advanced neoplasia detected per screening round;
13 articles: the full‐text was a letter or editorial;
13 articles: were reviews;
27 articles: encompassed the same cohort as an already included article;
14 articles: summarised the results of multiple screening rounds and separate data extraction of the first round was not possible;
7 articles: described case‐control studies;
4 articles: focused on digital FOBT where a stool sample was obtained by digital rectal examination;
35 articles: were excluded for various other reasons.
We have detailed those in the excluded studies table which needed further clarification for exclusion (see Characteristics of excluded studies).
Top‐up search
We performed a top‐up search on 14 September 2021, which identified 1522 records. Of these, we excluded 1489 based on title and abstract. We retrieved full‐text articles for the remaining 33 records. Of these, we identified one study that may be eligible for inclusion (Cheng 2021), and have listed this in Characteristics of studies awaiting classification. We excluded the other 32 records, adding any study that needed further clarification in order to assess eligibility to the Characteristics of excluded studies table.
Included studies
We included a total of 63 studies. We included the Faivre 2004 study after contacting the author. We included two additional studies that were included in a recent meta‐analysis (Imperiale 2019). Two included studies had study populations which partly overlapped (Brenner 2013; Haug 2011). Therefore, we combined these two studies for gFOBT and FIT results. Both studies analysed the same population of 3077 participants. The authors of the Haug 2011 study provided data for FIT cut‐offs 10 µg/g and 20 µg/g to allow direct comparison with other studies using the same cut‐offs. The original article excluded 15 cases for an analysis about left/right‐sided lesions, but we included these in our analysis. For studies that evaluated multiple stool tests in the same person, we allowed that these contributed an observation to both series of tests. Thus, we included these studies twice in the data set.
Studies using "reference standard: all"
We included a total of 33 "reference standard: all" studies: six were performed in the USA, of which one also included data from Canada; six in Germany; six in Taiwan; three in Japan; three in Thailand; three in South Korea; two in the Netherlands; and one study each in Spain, Sweden, China, and Hong Kong.
Six studies compared more than one test. Of those, in five studies, participants underwent more than one index test, resulting in a total of 23 separate tests in 104,640 participants. Overall, six gFOBT studies, 23 FIT studies, and four studies combining both gFOBT and FIT screening were included for this review.
The earliest study was published in 2000 (Nakama 2000), with the majority being published between 2008 and 2017. For all but one study (Nakama 2000), AN was the main outcome. Twenty‐six studies separately described the numbers of detected CRC and advanced adenoma. For 17 studies, we could retrieve data for a cut‐off of 10 μg Hb/g faeces, and for 13 studies, at a cut‐off of 20 μg Hb/g faeces. For all included gFOBT studies, a positivity criterion of at least one positive panel was used. All but three studies used a single stool sample for FIT testing, and for all but two gFOBT studies, three consecutive stools were used (Table 2).
Studies using "reference standard: positive"
We included a total of 30 "reference standard: positive" studies: four were performed in France; four in Italy; three in Spain; three in the Netherlands; two each in Japan, Taiwan, England, Scotland, and Denmark; and one study each in the USA, Canada, Israel, Ireland, Finland, and Germany.
Six studies compared more than one index test, with each participant undergoing one FOBT. Altogether, they reported on a total of 16 tests in 3,664,934 participants. Overall, we included nine gFOBT, 16 FIT, and five combination studies. Out of the studies combining gFOBTs and FITs, four studies randomised participants and one study performed both tests in all participants.
The earliest study was published in 1987 (Kronborg 1987), with the majority being published between 2002 to 2019. All studies had at least one year of follow‐up, with a maximum of four years of follow‐up. Nineteen of 30 included studies had exactly two years of follow‐up. For five studies, we could retrieve data with a cut‐off of 10 μg Hb/g faeces, and for ten studies (12 FITs), data with a cut‐off of 20 μg Hb/g faeces. All but two studies used a single stool sample for FIT testing, and for all but one gFOBT study, three consecutive stools were used (Table 3).
Methodological quality of included studies
All characteristics of included studies can be found in the Characteristics of included studies, Table 2, and Table 3.
Studies using "reference standard: all"
We have summarised the overall quality of the studies, as assessed using the QUADAS and QUADAS‐2 tools (see Appendix 7), in Figure 2 and Figure 3. We have included all studies in the final analyses.
2.

Studies using "reference standard: all". Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across studies
3.

Studies using "reference standard: all". Risk of bias and applicability concerns summary: review authors' judgement about each domain for each included study
Patient selection domain
Twenty‐nine (88%) studies included a representative spectrum of average‐risk participants, which reflects population‐based screening. For three studies, this spectrum was unclear because the studies were either retrospective or did not clearly describe exclusion criteria (Nakama 2000; Nakazato 2006; Omata 2011). However, all these studies were performed in an average‐risk CRC screening setting, and were therefore included in analysis. One study had a high risk of bias regarding the spectrum as it included participants referred for colonoscopy outside a screening setting (Cruz‐Correa 2007).
Index test domain
Twenty‐one (64%) of the studies had a low risk of bias concerning the index test. We assessed nine studies as unclear because either the method of collection was not clearly described or the positivity threshold was not described. Two studies (6%) had a high risk of bias since the study conducted the index test not as advised by the manufacturer or no threshold was described (Brenner 2013; Chiu 2016a). Unanalysable tests were only reported in six studies (18%).
Reference standard domain
Thirty studies (91%) had low concerns regarding applicability of the index test. We assessed three studies as unclear because they did not describe whether the threshold was pre‐specified (Aniwan 2015; Nakama 2000; Nakazato 2006). All studies had a low risk concerning the reference standard, with over 80% of the participants undergoing colonoscopy as the reference standard. However, many studies had missing values, and FOBT‐positivity rates were often lacking. The majority (88%) of studies had clear definitions of advanced adenomas; these were mainly defined as adenomas 10 mm or greater, adenomas with at least 25% villous component, and/or high grade dysplasia.
Flow and timing domain
Regarding flow and timing, we assessed 16% of the studies as having a high risk of bias. This was mainly due to lack of clarity about time between index test and the reference standard, and high proportions of unexplained excluded subjects.
Studies using "reference standard: positive"
We have summarised the overall quality of studies in Figure 4 and Figure 5. We have included all studies in the final analyses.
4.

Studies using "reference standard: positive". Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies
5.

Studies using "reference standard: positive". Risk of bias and applicability concerns summary: review authors' judgement about each domain for each included study
Patient selection domain
Twenty‐five studies (83%) clearly included a representative spectrum of participants with an average risk of developing advanced neoplasia. Two studies had a high risk of bias with regard to selection of participants: in one study (Itoh 1996), Japanese workers in a FIT‐based screening programme could have experienced gFOBT screening in previous years. In another study (Sieg 2002), the article stated that people below the age of 44 could also participate if they heard about the study, but when contacted, the authors stated this was not the case.
Index test domain
Risk of bias concerning the index test was potentially present if, in the manuscript, it was not specified how non‐interpretable or borderline test results had been handled. No studies had a high risk of bias in this domain and 13 (35%) had an unclear risk.
Reference standard domain
Of the included studies, 77% specified their reference standard as being colonoscopy. We assessed two studies as having a high risk of bias as it was unknown how many FIT‐positive screenees underwent colonoscopy because the final result of the colonoscopy, CRC, was retrieved via the national cancer registration (Chen 2016a; Paszat 2016). In one study, only 75% of FIT‐positive participants underwent colonoscopy (Jensen 2016). We assessed five studies as unclear because – while they used colonoscopy as the reference standard – it was unclear how many participants underwent CT‐colonography or double‐contrast barium enema in case of a failed colonoscopy.
Flow and timing domain
With regard to flow and timing, 37% of the studies had a low risk of bias. This was due to multiple reasons. All studies had a minimum follow‐up of one year, and most studies had two years of follow‐up. Of note, five studies had a follow‐up of three years, and one had a follow‐up of four years. Three studies followed participants until the next screening round, which was after approximately two years. In eight studies, a proportion of participants had a follow‐up duration of less than one year (Bouvier 1999; Castiglione 2007; Jensen 2016; Juul 2018; Kronborg 1987; Launoy 2005; Paimela 2010; Sieg 2002).
Findings
Studies using "reference standard: all"
Diagnostic accuracy for advanced neoplasia (AN)
Thirty‐one "reference standard: all" studies reported on AN as outcome. The median sample size was 1256 (interquartile range (IQR) 646 to 4404). Figure 6 shows the forest plot of the studies.
6.

Forest plot of gFOBT and FIT ("reference standard: all") for advanced neoplasia. For all FITs, a cut‐off of 10 µg Hb/g faeces was used, unless this cut‐off was unavailable.
Sensitivities between the studies ranged from 0% to 33% for gFOBTs and from 5% to 67% for FITs, while the corresponding specificities ranged from 79% to 98% and from 74% to 99%, respectively. The cut‐off for positivity of FITs varied between 2.4 µg to 50 µg Hb/g faeces. The summary curve estimated by the hierarchical summary receiver operating characteristic (HSROC) model for all "reference standard: all" studies can be found in Figure 7. FITs showed a higher discriminative ability for AN than gFOBTs (P < 0.001).
7.

Summary curve using the HSROC model for gFOBT and FIT ("reference standard: all") including multiple cut‐offs for advanced neoplasia. Scale of individual study points is based on sample size
Diagnostic accuracy for advanced neoplasia at different cut‐offs
In addition, we derived sensitivities and specificities from studies reporting on FIT screening at cut‐off values of 10 μg and 20 μg Hb/g faeces (Figure 8 and Figure 9). Analyses for a cut‐off of 10 μg Hb/g faeces contained both qualitative and quantitative FITs. The sensitivity of FIT screening varied between studies: between 5% to 67% at the 10 μg Hb/g cut‐off, and between 13% to 44% at the 20 μg Hb/g cut‐off. The summary sensitivity of gFOBT screening was 15% (95% confidence interval (CI) 12% to 20%), significantly lower than the 33% (95% CI 27% to 40%; P < 0.001) for FITs at the 10 μg Hb/g cut‐off, and the 26% (95% CI 21% to 31%; P = 0.002) for FITs at the 20 μg Hb/g cut‐off. Specificities of FIT screening varied between studies, from 87% to 97% and from 89% to 100% for FIT cut‐offs of 10 μg and 20 μg Hb/g, respectively. No significant differences in summary specificities were found between gFOBTs (94%; 95% CI 92% to 96%) and FITs at 10 μg Hb/g (93%; 95% CI 90% to 95%) and 20 μg Hb/g (97%; 95% CI 95% to 98%) cut‐offs.
8.

"Reference standard: all" gFOBT versus FIT (cut‐off 10 ug Hb/g) for AN
9.

"Reference standard: all" gFOBT versus FIT (cut‐off 20 ug Hb/g) for AN
Diagnostic accuracy for advanced neoplasia at pre‐specified specificities
We calculated the sensitivity of FITs and gFOBTs for advanced neoplasia at pre‐specified specificities. These calculations showed a higher sensitivity for FITs compared to gFOBTs at a specificity of 90% and 95% (Table 4).
3. Sensitivity at pre‐specified specificities for advanced neoplasia.
| Test | Sensitivity at 90% specificity | Sensitivity at 95% specificity | Difference in accuracy (LR test, P value) |
| gFOBT | 0.21 (0.17, 0.27) | 0.14 (0.11, 0.18) | < 0.0001 |
| FIT | 0.36 (0.32, 0.41) | 0.26 (0.22, 0.29) |
FIT: faecal immunochemical test; gFOBT: guaiac‐based faecal occult blood test; LR: likelihood ratio
Diagnostic accuracy for colorectal cancer
Twenty‐nine "reference standard: all" studies reported on CRC; the median sample size was 2235 (IQR 779 to 4404). Figure 10 shows the forest plot of the studies.
10.

Forest plot of gFOBT and FIT ("reference standard: all") for colorectal cancer. For all FITs, a cut‐off of 10 µg Hb/g faeces was used, unless this cut‐off was unavailable
Sensitivity in the included studies ranged from 13% to 100% for gFOBTs, and from 0% to 100% for FITs. Specificity ranged from 80% to 98% for gFOBTs and from 71% to 99% for FITs. The cut‐off for positivity of FITs varied between 2.4 µg to 50 µg Hb/g faeces. The summary curve estimated by the HSROC model for CRC is depicted in Figure 11. FITs showed a higher discriminative ability compared to gFOBTs (P < 0.004).
11.

Summary curve using the HSROC model for gFOBT and FIT ("reference standard: all") including multiple cut‐offs for colorectal cancer. Scale of individual study points is based on sample size
Diagnostic accuracy for colorectal cancer at different cut‐offs
We also derived sensitivities and specificities from studies where FIT cut‐offs of 10 μg and 20 μg Hb/g faeces were reported (Figure 12 and Figure 13). Sensitivity ranged between studies: from 13% to 100% for gFOBTs; from 0% to 100% for a FIT cut‐off of 10 μg Hb/g; and from 9% to 100% for a cut‐off of 20 μg Hb/g. Summary sensitivity of gFOBTs was 39% (95% CI 25% to 55%), which was significantly lower than the 76% (95% CI 57% to 88%; P = 0.001) for FITs at the 10 μg Hb/g cut‐off and 65% (95%; CI 46% to 80%; P = 0.035) for FITs at the 20 μg Hb/g cut‐off. Specificity for FITs ranged between studies: from 87% to 99% and from 88% to 96% for FITs at the 10 μg and 20 μg Hb/g cut‐offs respectively. No significant differences in summary specificities were found between gFOBTs (94%; 95% CI 91% to 96%), and FITs at 10 μg Hb/g (94%; 95% CI 87% to 97%) and 20 μg Hb/g (96%; 95% CI 91% to 98%) cut‐offs.
12.

"Reference standard: all" gFOBT versus FIT (cut‐off 10 ug Hb/g) for CRC
13.

"Reference standard: all" gFOBT versus FIT (cut‐off 20 ug Hb/g) for CRC
Diagnostic accuracy for colorectal cancer at pre‐specified specificities
We calculated the sensitivity of gFOBTs and FITs at pre‐specified specificities, finding a higher sensitivity for FITs at a specificity of 90% and 95% (Table 5).
4. Sensitivity at pre‐specified specificities for colorectal cancer.
| Test | Sensitivity at 90% specificity | Sensitivity at 95% specificity | Difference in accuracy (LR test, P value) |
| gFOBT | 0.57 (0.39, 0.73) | 0.37 (0.22, 0.54) | <0.004 |
| FIT | 0.81 (0.71, 0.88) | 0.65 (0.54, 0.75) |
FIT = faecal immunochemical test; gFOBT = guaiac‐based faecal occult blood test; LR = likelihood ratio
Linked receiver operating characteristic (ROC)
Five studies compared FITs and gFOBTs in the same population (Brenner 2012; Brenner 2013 and Haug 2011 combined; Graser 2009; Hoepffner 2006; Park 2010). The cut‐off for positivity of FITs varied between 2.4 µg to 10 µg Hb/g faeces. The summary curve estimated by the HSROC model for linked "reference standard: all" studies for AN can be found in Figure 14. FITs showed a higher discriminative ability for AN than gFOBTs (P = 0.003).
14.

Linked‐HSROC curve of studies ("reference standard: all") with outcome advanced neoplasia (including: Brenner 2012, Brenner 2013 and Haug 2011 combined, Graser 2009, Hoepffner 2006, Park 2010). Scale of individual study points is based on sample size
We calculated sensitivities of gFOBTs and FITs for AN at pre‐specified specificities. These calculations showed a higher sensitivity of FITs at a specificity of 90% and 95% (Table 6).
5. Sensitivity at pre‐specified specificities for advanced neoplasia in studies using FIT and gFOBT in the same population.
| Test | Sensitivity at 90% specificity | Sensitivity at 95% specificity | Difference in accuracy (LR test, P value) |
| gFOBT | 0.23 (0.10, 0.42) | 0.12 (0.07, 0.22) | 0.003 |
| FIT | 0.47 (0.29, 0.66) | 0.30 (0.18, 0.46) |
FIT = faecal immunochemical test; gFOBT = guaiac‐based faecal occult blood test; LR = likelihood ratio
Heterogeneity analyses
There was no significant difference in HSROC curves between studies using a quantitative or a qualitative FIT for AN (P = 0.655) or CRC (P = 1.000). We did not perform heterogeneity analyses for the number of stools per screening round or gender as there was insufficient heterogeneity between the studies.
Sensitivity analyses
For the analyses including all cut‐offs, we undertook a sensitivity analysis for each QUADAS‐2 domain by excluding studies that yielded a high risk of bias (Ahlquist 2008a; Ahlquist 2008b; Chiu 2016a; Cruz‐Correa 2007; Graser 2009; Nakama 2000; Nakazato 2006; Omata 2011; Park 2010; Siripongpreeda 2016; Sohn 2005; Wong 2014; Wu 2014), or an unclear risk of bias (Aniwan 2015; Aniwan 2017; Brenner 2012; Brenner 2018; Chang 2017; Graser 2009; Imperiale 2004; Khalid‐de Bakker 2011; Kim 2017; Nakama 2000; Omata 2011; Park 2010; Siripongpreeda 2016; Sohn 2005; Wong 2014), following the QUADAS assessment. After excluding these studies, all analyses for each specific QUADAS‐2 domain showed that FITs remained significantly superior in the detection of AN and CRC compared to gFOBTs.
Studies using "reference standard: positive"
Diagnostic accuracy for colorectal cancer
Thirty "reference standard: positive" studies reported on CRC as a separate outcome; their median sample size was 30,789 (IQR 4936 to 141,045). Figure 15 shows the forest plot of included studies reporting on CRC.
15.

Forest plot of gFOBT and FIT ("reference standard: positive") for colorectal cancer. For all FITs, a cut‐off of 10 µg Hb/g faeces was used, unless this cut‐off was unavailable
Sensitivity ranged between studies, from 10% to 67% for gFOBTs, and from 49% to 100% for FITs. Specificities ranged from 96% to 99% for gFOBTs, and from 88% to 98% for FITs. The cut‐off for positivity of FITs varied between 5 µg to 250 µg Hb/g faeces. The summary curve estimated by the HSROC model can be found in Figure 16. FITs showed a higher discriminative ability for CRC than gFOBTs (P < 0.001).
16.

Summary curve using the HSROC model for gFOBT and FIT ("reference standard: positive") including multiple cut‐offs for colorectal cancer. Scale of individual study points is based on sample size
Diagnostic accuracy for colorectal cancer at different cut‐offs
We derived sensitivity and specificity from studies where FIT cut‐offs of 10 μg Hb/g and 20 μg Hb/g faeces were used. Sensitivity varied between studies: from 75% to 100% and from 63% to 94% at cut‐offs of 10 μg and 20 μg Hb/g, respectively. Summary sensitivity of gFOBTs was 59% (95% CI 55% to 64%), which was significantly lower compared to 89% (95% CI 80% to 95%; P < 0.001) and 89% (95% CI 85% to 92%; P < 0.001) for FITs at cut‐offs of 10 μg and 20 μg Hb/g, respectively. Summary specificity of gFOBTs was 98% (95% CI 98% to 99%), which was higher compared to 94% (95% CI 92% to 95%; P < 0.001) and 95% (95% CI 94% to 96%) for FITs at 10 μg and 20 μg Hb/g, respectively.
Diagnostic accuracy for colorectal cancer at pre‐specified specificities
We calculated the sensitivity of gFOBTs and FITs for CRC at pre‐specified specificities, finding a higher sensitivity of FITs at a specificity of 90% and 95% (Table 7).
6. Sensitivity at pre‐specified specificities for colorectal cancer.
| Test | Sensitivity at 90% specificity | Sensitivity at 95% specificity | Difference in accuracy (LR test, P value) |
| gFOBT | 0.80 (0.67, 0.89) | 0.73 (0.63, 0.80) | 0.009* |
| FIT | 0.97 (0.95, 0.98) | 0.89 (0.86, 0.91) | |
| * HSROC curves have different shape parameters | |||
FIT = faecal immunochemical test; gFOBT = guaiac‐based faecal occult blood test; HSROC = hierarchical summary receiver operating characteristic; LR = likelihood ratio
Heterogeneity analyses
There was no significant difference in HSROC curves between studies using a quantitative or a qualitative FIT at all cut‐offs for the outcome CRC (P = 1.000). We did not perform heterogeneity analysis related to the number of stools per screening round for gFOBTs since all studies used three stools. For the following covariates, analyses were not possible due to convergence difficulties: gender for FITs, and number of stools for FITs.
Sensitivity analyses
For the analyses including all cut‐offs, we undertook a sensitivity analysis for each QUADAS‐2 domain by excluding the studies that yielded a high risk of bias following the QUADAS assessment (Chen 2016a; Giai 2014; Itoh 1996; Jensen 2016; Nakama 1996; Parra‐Blanco 2010; Sieg 2002; Robinson 1996). For the 'patient selection domain', two studies yielded a high risk of bias (Itoh 1996; Sieg 2002). For the 'reference standard domain', three studies yielded a high risk of bias (Chen 2016a; Jensen 2016; Paszat 2016). For the 'flow and timing domain', five studies yielded a high risk of bias (Chen 2016a; Giai 2014; Parra‐Blanco 2010; Paszat 2016; Robinson 1996). We also excluded studies that yielded an unclear risk of bias (Arana‐Arri 2017a; Arana‐Arri 2017b; Blanks 2019; Bouvier 1999; Castiglione 2007; Chiang 2014a; Chiang 2014b; Digby 2016; Faivre 2004; Juul 2018; Kronborg 1987; Launoy 2005; Nakama 1996; Paimela 2010; Steele 2009; Zorzi 2018). After excluding these studies, all analyses for each specific QUADAS‐2 domain showed that FITs remained significantly superior to gFOBTs in the HSROC model. FITs also remained significantly superior to gFOBTs when studies were excluded that did not describe the proportion of index test positives that underwent the reference standard (i.e. colonoscopy) (Chen 2016a; Giai 2014; Nakama 1996; Paszat 2016).
Discussion
Summary of main results
We have presented the main results in the Table 1. For this review, we chose to include two types of studies and report the results separately, as they differ in design and yield different results. We included 33 "reference standard: all" studies and 30 "reference standard: positive" studies.
Of the 33 "reference standard: all" studies, six evaluated the diagnostic accuracy of gFOBTs, 23 studies evaluated FITs, and four studies assessed both gFOBTs and FITs. Twenty‐one studies evaluated the diagnostic accuracy for AN and nineteen studies evaluated the diagnostic accuracy for CRC. FITs showed a higher discriminative ability than gFOBTs as assessed by the HSROC curve for both AN (P < 0.001) and CRC (P = 0.004). As "reference standard: all" studies allowed the use of multiple FIT cut‐offs within one study population, we analysed separately the two cut‐offs most commonly used worldwide (10 μg and 20 μg Hb/g faeces), and these results did not change our conclusion. Lastly, we compared sensitivities for pre‐specified specificities, showing that at the same specificity, of 90% and 95% respectively, FITs consistently had a higher sensitivity compared to gFOBTs.
Of the 30 "reference standard: positive" studies included, nine studies evaluated the diagnostic accuracy of gFOBTs, 16 studies evaluated FITs, and five studies combined both. In "reference standard: positive" studies, FITs also showed a higher discriminative ability than gFOBTs as assessed by the HSROC curve for CRC (P < 0.003).
The results of this systematic review demonstrate that one‐round FITs have a higher sensitivity and similar specificity for both AN and CRC compared to one‐round gFOBTs in an average‐risk population. Furthermore, most FITs are quantitative tests, which allows for the use of different cut‐offs to tailor for screening resources and colonoscopy capacity. Finally, studies have consistently shown that FIT screening is associated with a higher uptake than gFOBT screening (Hol 2009; Tinmouth 2015). This is important to reach a high coverage of the target population (i.e. cumulative uptake).
Strengths and weaknesses of the review
Strengths
The results of this review are based on a strict and thorough search without any language or date restrictions. The use of diagnostic test accuracy or randomised controlled trial filters may lead to the loss of some studies (Doust 2005); for this reason, we have not used any filters. Two independent review authors identified studies and extracted data from them, thus decreasing inaccuracies related to single‐person data extraction (Buscemi 2006). All included studies reported the results for average‐risk, asymptomatic individuals aged 40 years or older, making our results reflective of a screening population. Also, by contacting study authors, we obtained data for different cut‐offs, where these data had not already been reported in original publications. These additional data allowed sub‐analyses with the two most commonly used cut‐offs for the majority of the studies. We converted these cut‐offs to the internationally used measuring standard of μg Hb/g faeces (Fraser 2012). To avoid potential bias caused by the use of an inappropriate reference standard (e.g. barium enema or sigmoidoscopy), we restricted included studies to those with colonoscopy as the reference standard. As mentioned above, we included two types of studies in this review and analysed them separately. The inclusion of "reference standard: all" studies allowed for evaluating both AN and CRC as outcomes of FOBT‐based screening. AN is of special importance because, by removing adenomas, development of CRC (Winawer 1993), CRC deaths (Zauber 2012,) might be prevented. In "reference standard: positive" studies, we calculated sensitivity and specificity with the use of interval carcinomas identified through adequate follow‐up as a surrogate for the reference standard, colonoscopy. The different characters of "reference standard: all" and "reference standard: positive" studies may explain the observed differences in sensitivity and specificity. The use of interval carcinomas as endpoint in "reference standard: positive" studies may underestimate the true proportion of false negatives, as by definition, only those cancers that had become clinically evident during the observation period were reported. It therefore gives an overestimation of the sensitivity. On the other hand, "reference standard: positive" studies are more reflective of an FOBT‐based screening programme in a general population. In these studies, willingness to undergo FOBT as a primary screening tool was assessed, whereas in "reference standard: all" studies, participants had to be willing to undergo a full colonoscopy irrespective of the FOBT result. For this reason "reference standard: positive" studies are also often performed in larger populations. Combining both types of studies provides insight on both settings, and results in a broad evaluation of FOBT diagnostic test accuracy in CRC screening. "Reference standard: all" studies give insight into test sensitivity, whereas "reference standard: positive" studies give insight into program sensitivity. The overall quality of included studies was high, supporting the validity of the results of our analyses.
We conducted the search in June 2019, making the search possibly outdated. However, we performed a top‐up search on 14 September 2021, yielding only one new study potentially eligible for inclusion; it uses FIT in a "reference standard: all" study (Cheng 2021). We believe that this study, including 1411 screenees, will not influence the main conclusions of our systematic review, as it is a relatively small study compared to the other included studies, and it only included two participants with CRC.
Most previously published meta‐analyses have evaluated the test accuracy of FITs for CRC but not AN, and did not compare these results to the performance of gFOBTs (Imperiale 2019; Lee 2014). One recent meta‐analysis did include FIT sensitivity and specificity for both CRC and AN (Imperiale 2019). They found a summary sensitivity of FITs for CRC at 10 µg/g of 91% at specificity of 90% and at 20 µg/g, a sensitivity of 75% at a specificity of 95%. For AN, the summary sensitivity at 10 µg/g was 31% with a specificity of 91%, and at 20 µg/g, sensitivity was 25% with a specificity of 95%. This meta‐analysis did not include a comparison with gFOBTs. Another systematic review has compared the diagnostic test accuracy of gFOBTs and FITs (Launois 2014). The highest summary sensitivity of FIT (OC‐Sensor, Eiken, Japan) in this review was 87% and specificity was 93%, and for gFOBT (Hemoccult), the summary sensitivity was 47% and summary specificity was 95%. Even though the Launois 2014 review included a wide range of study types, its search strategy was very limited, yielding only 761 hits and 22 inclusions. Of note, Launois 2014 only included three brands of FOBTs in their review. In their meta‐analysis, the diagnostic accuracy of FITs was higher than in our meta‐analysis. This could be explained by the fact that they did not distinguish between studies in which all screenees underwent the reference test (i.e. "reference standard: all") and studies in which only FOBT‐positive screenees underwent the reference standard (i.e. "reference standard: positive"). Also, Launois 2014 included case‐control studies, which can possibly lead to underestimation of specificity or overestimation of sensitivity and specificity (Deeks 2013). Lastly, for some included studies, data from the same study were included more than once, as these data were published in multiple publications. Including several publications of the same study within a systematic review gives inappropriate weight to the duplicated data and might lead to duplicate publication bias (Fairfield 2017). A recent meta‐analysis focused on "reference standard: positive" studies and included studies after one or multiple screening rounds (Wieten 2019). This review demonstrated an increased risk for interval carcinoma after a negative gFOBT compared to after a negative FIT, which is in line with our results. Including both studies with a single screening round and those with multiple rounds may influence the observed effect, because it is known that the risk of interval carcinoma drops significantly after multiple negative tests compared to one negative test (Zorzi 2018).
Limitations
This systematic review was designed to evaluate the diagnostic test accuracy of two types of FOBTs commonly used for CRC screening. Even though diagnostic test accuracy is of major importance in screening, the usability of the test and participation (e.g. the willingness of participants to undergo the screening test) are also very relevant. One major limitation of this review is that it has not taken these latter points into account as they do not involve diagnostic test accuracy. Yet, these factors are also of importance when estimating screening efficacy at population level (programme sensitivity and specificity). The ultimate purpose of screening programmes is a decrease in CRC‐related mortality. However, diagnostic test accuracy can only be used as a surrogate in estimating mortality decrease after screening. Unfortunately, results of previously published, large, prospective gFOBT‐based screening trials could not be included in this review as their main outcome was mortality. Mortality rates could not be converted into contingency tables to calculate sensitivity and specificity. We excluded non‐interpretable test results and FOBT‐positive participants who refused to undergo the reference standard from the 2 x 2 table, and in consequence, from the meta‐analysis. Missing FOBT results are likely to be completely random (incidental missing data) and will not lead to biased estimates of test accuracy. Because only the participants who received the reference standard were included in the "reference standard: all" studies analysis (complete case analysis), and positive participants who did not receive the reference standard in the "reference standard: positive" studies were excluded from analysis, estimates of the accuracy of the diagnostic tests could be biased (Naaktgeboren 2016). We report the percentage of participants that did not undergo colonoscopy in Characteristics of included studies. Because of the large size of the studies, we believe that excluding these participants for whom the reference standard result is missing is mostly at random and will not bias the results but will only decrease precision.
Another limitation of the review was our inability to explore the sources of heterogeneity concerning age, gender, ethnicity, adenoma type, tumour localisation and stage distribution, because of limited information in the included studies. This problem was more prominent in "reference standard: positive" studies, as these studies often comprise retrospective descriptions using data from national databases of hospitals or cancer registries. A direct comparison was only possible for a limited number of studies, as most studies did not perform both tests in the same participants. This could be a limitation, as results from non‐comparative studies may differ from comparative studies (Takwoingi 2013). However, in this review, conclusions from the comparative studies did not differ from the overall results. Finally, many test brands are available and differences in quality between FOBT brands might influence the diagnostic performance of these tests. However, we could not perform sub‐analyses of these brands due to limited data and the use of different sub‐types of the same brand.
Applicability of findings to the review question
All participants included in this review were asymptomatic, average‐risk individuals who were over the age of 40 years and invited for CRC screening, which makes the findings of this review extremely relevant for CRC screening programmes. We included two types of studies. "Reference standard: all" studies are more homogenous than "reference standard: positive" studies, yet may be less representative of an FOBT‐based screening population. This is due to the fact that all screenees had to be willing to undergo colonoscopy. For "reference standard: positive" studies, false negatives were identified through interval carcinomas diagnosed during follow‐up. This might give an overestimation of test sensitivity, yet is appropriately representative of FOBT population‐based screening programmes. Sensitivities and specificities obtained from the "reference standard: positive" studies apply to the first, single, screening round. Since screenees will be invited for multiple screening rounds during a specific age range, sensitivity will increase per round (CRC generally grows slowly and can be detected during the next screening round before they become symptomatic). As almost all studies were performed in high‐income countries, the applicability of our findings extends to these countries.
Authors' conclusions
Implications for practice.
Faecal immunochemical tests (FITs) have a superior sensitivity compared to guaiac‐based faecal occult blood tests (gFOBTs) at equal sensitivity, so in terms of diagnostic test accuracy, FITs are superior to gFOBTs. We did not evaluate test usability and participation for the purpose of this review. It should also be noted that our initial search for studies occurred in June 2019. We ran a top‐up search on 14 September 2021, yielding only one additional small study which may be eligible for inclusion and is currently awaiting classification. The summary of findings table should be interpreted in light of these points. The quantitative nature of some FITs allows for the use of different cut‐offs, tailoring to screening resources and colonoscopy capacity (Wilschut 2011). Based on this review, no guidance can be provided as to which cut‐off should be chosen, since the results appear to show that the two most commonly‐used cut‐offs in the included studies (10 μg Hb/g and 20 μg Hb/g faeces) perform quite similarly in both sensitivity and specificity. Furthermore, it should be noted that several studies consistently reported higher rates of participation for FIT than for gFOBT screening (Hol 2009; Van Rossum 2008). Both gFOBTs and FITs have lower sensitivity for colorectal cancer than colonoscopy as reference standard. However, when combining test accuracy with participation, FIT‐based screening in many populations results in a higher diagnostic yield of advanced neoplasia compared to other CRC screening methods (Kuipers 2013; Schreuders 2015).
Implications for research.
Future studies should be conducted in a prospective manner, mimicking population‐based CRC screening and targeting average‐risk populations. We encourage authors to systematically report data on participation, cut‐off in µg Hb/g faeces, positivity rate, and colonoscopy adherence. New studies on higher cut‐offs are expected in the future and may guide which cut‐off should be used. For AN, we encourage authors to describe advanced adenomas separately. Also, future studies should report a clear definition of interval carcinomas. In the included studies, definitions of interval carcinomas were often vague or completely missing. The ultimate purpose of CRC screening is decreasing mortality, so future studies should be conducted to compare long‐term follow‐up on mortality between gFOBT‐ and FIT‐based CRC screening programmes.
What's new
| Date | Event | Description |
|---|---|---|
| 13 January 2022 | Feedback has been incorporated | Revisions incorporated |
| 14 September 2021 | New search has been performed | Top‐up search 14 September 2021 |
History
Protocol first published: Issue 8, 2011
Acknowledgements
The authors would like to thank the members of the Cochrane Colorectal Cancer Group (CCCG), especially Marija Barbateskovic for helping us to compose and conduct the literature searches. We would also like to thank the Medical School Library of the Erasmus MC for help in obtaining some of the articles. We also thank the many authors of individual papers who kindly went back to their original data to provide us with very relevant information for sub‐analyses.
Sign‐off Editor (final editorial decision): Nicole Skoetz, Cochrane Network Editor
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to authors, edited the article): Colleen Ovelman, Cochrane Central Editorial Service
Editorial Assistant (conducted editorial policy checks and supported editorial team): Leticia Rodrigues, Cochrane Central Editorial Service
Copy Editor (copy editing and production): Faith Armitage, Copy Edit Support team
Peer‐reviewers (provided comments and recommended an editorial decision): Rodrigo Jover, Servicio de Medicina Digestiva, Hospital General Universitario de Alicante (clinical review); Nastazja Dagny Pilonis, MD, PhD Department of Gastroenterological Oncology National Institute of Oncology Warsaw (clinical review); Catherine Dube, Clinical Associate Professor, University of Ottawa (clinical review); Dulce Estêvão, Faro, Portugal (consumer review); the Diagnostic Test Accuracy Editorial Team, Cochrane (methods review); Robin Featherstone, Cochrane Central Editorial Service (search review).
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
#1 exp Colorectal Neoplasms/
#2 (colorect* or colon* or rect* or anal* or anus* or intestin* or bowel*) adj3 (carcinom* or neoplas* or adenocarcinom* or cancer* or tumor* or tumour* or sarcom* or polyp* or adenom*).mp.
#3 1 or 2
#4 exp Occult Blood/
#5 (occult blood).mp.
#6 4 or 5
#7 (faecal or fecal or feces or faeces or stool*).mp.
#8 6 and 7
#9 (FOBT* or FIT* or gFOBT*).mp.
#10 8 or 9
#11 (immunohistochem* or immunochem* or immunol* or guaiac*).mp.
#12 exp Immunochemistry/
#13 exp Guaiac/
#14 11 or 12 or 13
#15 10 and 14
#16 (fecal immunochemical test* or faecal immunochemical test* or fecal immunochemistry test* or faecal immunochemistry test* or ColoScreen* or Hema‐Screen* or Hemdetect* or Hemoccult* or SENSA* or Hema‐Check* or HemaCheck* or hemoCARE* or Peroheme* or ColoCare* or Lifeguard* or Fecatwin* or HemaWipe* or Instaccult* or Monohaem* or Okokit* or Seracult* or Dencoccult* or Early detector* or Fe Cult* or Feca EIA* or Hemo FEC* or Hexagon* or SureScreen* or Hemaprompt* or Hemdetect* or Camco PAK* or Colocheck* or Cecogenics* or Hematest* or Dencocult* or Fecatest* or Hemofecia* or Quick‐CULT*).mp.
#17 15 or 16
#18 3 and 17
Appendix 2. Embase (Ovid) search strategy
#1 exp Large intestine tumor/
#2 (colorect* or colon* or rect* or anal* or anus* or intestin* or bowel*) adj3 (carcinom* or neoplas* or adenocarcinom* or cancer* or tumor* or tumour* or sarcom* or polyp* or adenom*).mp.
#3 1 or 2
#4 exp Occult Blood/
#5 (occult blood).mp.
#6 4 or 5
#7 (faecal or fecal or feces or faeces or stool*).mp.
#8 6 and 7
#9 (FOBT* or FIT* or gFOBT*).mp.
#10 8 or 9
#11 (immunohistochem* or immunochem* or immunol* or guaiac*).mp.
#12 exp Immunochemistry/
#13 exp Guaiac/
#14 11 or 12 or 13
#15 10 and 14
#16 (fecal immunochemical test* or faecal immunochemical test* or fecal immunochemistry test* or faecal immunochemistry test* or ColoScreen* or Hema‐Screen* or Hemdetect* or Hemoccult* or SENSA* or Hema‐Check* or HemaCheck* or hemoCARE* or Peroheme* or ColoCare* or Lifeguard* or Fecatwin* or HemaWipe* or Instaccult* or Monohaem* or Okokit* or Seracult* or Dencoccult* or Early detector* or Fe Cult* or Feca EIA* or Hemo FEC* or Hexagon* or SureScreen* or Hemaprompt* or Hemdetect* or Camco PAK* or Colocheck* or Cecogenics* or Hematest* or Dencocult* or Fecatest* or Hemofecia* or Quick‐CULT*).mp.
#17 15 or 16
#18 3 and 17
Appendix 3. Cochrane Library search strategy
#1 MeSH descriptor Colorectal neoplasms explode all trees
#2 (colorect* or colon* or rect* or anal* or anus* or intestin* or bowel*) near/3 (carcinom* or neoplas* or adenocarcinom* or cancer* or tumor* or tumour* or sarcom* or polyp* or adenom*)
#3 1 or 2
#4 MeSH descriptor Occult Blood explode all trees
#5 (occult blood)
#6 4 or 5
#7 (faecal or fecal or feces or faeces or stool*)
#8 6 and 7
#9 (FOBT* or FIT* or gFOBT*)
#10 8 or 9
#11 (immunohistochem* or immunochem* or immunol* or guaiac*)
#12 MeSH descriptor Immunochemistry explode all trees
#13 MeSH descriptor Guaiac explode all trees
#14 11 or 12 or 13
#15 10 and 14
#16 (fecal‐immunochemical‐test* OR faecal‐immunochemical‐test* OR fecal‐immunochemistry‐test* OR faecal‐immunochemistry‐test* OR ColoScreen* OR Hema‐Screen* OR Hemdetect* OR Hemoccult* OR SENSA* OR Hema‐Check* OR HemaCheck* OR hemoCARE* OR Peroheme* OR ColoCare* OR Lifeguard* OR Fecatwin* OR HemaWipe* OR Instaccult* OR Monohaem* OR Okokit* OR Seracult* OR Dencoccult* OR Early‐detector* OR Fe‐Cult* OR Feca‐EIA* OR Hemo‐FEC* OR Hexagon* OR SureScreen* OR Hemaprompt* OR Hemdetect* OR Camco‐PAK* OR Colocheck* OR Cecogenics* OR Hematest* OR Dencocult* OR Fecatest* OR Hemofecia* OR Quick‐CULT*)
#17 15 or 16
#18 3 and 17
Appendix 4. BIOSIS Citation Index (Ovid) search strategy
#1 exp Oncology/ or exp "Neoplasms ‐ Pathology, clinical aspects and systemic effects"/
#2 (colorect* or colon* or rect* or anal* or anus* or intestin* or bowel*) adj3 (carcinom* or neoplas* or adenocarcinom* or cancer* or tumor* or tumour* or sarcom* or polyp* or adenom*).mp.
#3 1 or 2
#4 exp Laboratory Techniques/ or exp "Methods and Techniques"/ or exp Biochemistry studies – General/ or exp Neoplasms ‐ Diagnostic methods/
#5 (occult blood).mp.
#6 4 or 5
#7 (faecal or fecal or feces or faeces or stool*).mp.
#8 6 and 7
#9 (FOBT* or FIT* or gFOBT*).mp.
#10 8 or 9
#11 (immunohistochem* or immunochem* or immunol* or guaiac*).mp.
#12 10 and 11
#13 (fecal immunochemical test* or faecal immunochemical test* or fecal immunochemistry test* or faecal immunochemistry test* or ColoScreen* or Hema‐Screen* or Hemdetect* or Hemoccult* or SENSA* or Hema‐ Check* or HemaCheck* or hemoCARE* or Peroheme* or ColoCare* or Lifeguard* or Fecatwin* or HemaWipe* or Instaccult* or Monohaem* or Okokit* or Seracult* or Dencoccult* or Early detector* or Fe Cult* or Feca EIA* or Hemo FEC* or Hexagon* or SureScreen* or Hemaprompt* or Hemdetect* or Camco PAK* or Colocheck* or Cecogenics* or Hematest* or Dencocult* or Fecatest* or Hemofecia* or Quick‐CULT*).mp.
#14 12 or 13
#15 3 and 14
Appendix 5. Science Citation Index Expanded search strategy
#1 ts=((colorect* or colon* or rect* or anal* or anus* or intestin* or bowel*) and (carcinom* or neoplas* or adenocarcinom* or cancer* or tumor* or tumour* or sarcom* or polyp* or adenom*))
#2 ts=(occult blood)
#3 ts=(faecal or fecal or feces or faeces or stool*)
#4 #3 AND #2
#5 ts=(FOBT* or FIT* or gFOBT*)
#6 #5 OR #4
#7 ts=(immunohistochem* or immunochem* or immunol* or guaiac*)
#8 #7 AND #6
#9 ts=(fecal immunochemical test* or faecal immunochemical test* or fecal immunochemistry test* or faecal immunochemistry test* or ColoScreen* or Hema‐Screen* or Hemdetect* or Hemoccult* or SENSA* or Hema‐Check* or HemaCheck* or hemoCARE* or Peroheme* or ColoCare* or Lifeguard* or Fecatwin* or HemaWipe* or Instaccult* or Monohaem* or Okokit* or Seracult* or Dencoccult* or Early detector* or Fe Cult* or Feca EIA* or Hemo FEC* or Hexagon* or SureScreen* or Hemaprompt* or Hemdetect* or Camco PAK* or Colocheck* or Cecogenics* or Hematest* or Dencocult* or Fecatest* or Hemofecia* or Quick‐CULT*)
#10 #9 OR #8
#11 #10 AND #1
Appendix 6. Google Scholar Search Stratetgy
"colorectal|colon|colonic|rectal|anal|anus carcinoma|neoplasm|neoplasms|adenocarcinoma|cancer|tumor|tumors" "occult blood"
faecal|fecal|feces|faeces|stool|FOBT|FIT|gFOBT
Appendix 7. QUADAS
Assessment of methodological quality table QUADAS (based on original QUADAS (Whiting 2003), as published in original protocol (Van Roon 2011).
1. Was the spectrum of invitees representative of the individuals who will be invited in a nationwide CRC screening program in practice?
2. Is the reference standard likely to classify the target condition correctly?
3. Is the time between reference standard and index test short enough to be reasonably sure that the target condition did not change between the two tests?
4. Did the whole sample, or a random selection of the sample, receive verification using the intended reference standard?
5. Did screened persons receive the same reference standard irrespective of the index test result?
6. Were the reference standard results interpreted without knowledge of the results of the index test?
7. Were the same clinical data available when test results were interpreted as would be available when the test is used in practice?
8. Were non‐interpretable test results reported for the index test?
9. Were withdrawals from the study explained?
10. Did the study provide a clear definition of what was considered to be a 'positive' index test result?
11. Was the study free of commercial funding?
Assesment of methodological quality table QUADAS‐2 (Whiting 2011)
| DOMAIN | PATIENT SELECTION | INDEX TEST | REFERENCE STANDARD | FLOW AND TIMING |
| Description | Describe methods of participant selection: explain selection of invitees (identified from general practitioner records or population registers Describe included patients (prior testing, presentation, intended use of index test and setting) |
Describe the index test and how it was conducted and interpreted | Describe the reference standard and how it was conducted and interpreted. Describe if definition of advanced neoplasia is according to Cochrane Review protocol | Describe enrolment of study participants, randomisation (if applicable). Describe any participants who were excluded from the 2 x 2 table: describe the time interval between index test(s) and reference standard |
|
Signalling questions (yes/no/unclear) |
Was a consecutive or random sample of patients enrolled? | If a threshold was used, was it pre‐specified? | Were the reference standard results interpreted without knowledge of the results of the index tests? | Was there an appropriate interval between index test and reference standard? |
| Was a case‐control design avoided? | Were non‐interpretable test results reported for the index test? | Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Were all participants included in the analysis? | |
| Did the study avoid inappropriate exclusions? | Were withdrawals from the study explained? | |||
| Was the spectrum of invitees representative of CRC screening? (e.g. avoid not‐average‐risk participants) | Did screened persons receive the same reference standard irrespective of index test result? | |||
| Risk of bias: high/low/unclear | Could the selection of participants have introduced bias? | Could the conduct or interpretation of the index test have introduced bias? | Could the reference standard, its conduct, or its interpretation have introduced bias? | Could the participant flow have introduced bias? |
| Concerns regarding applicability: high/low/ unclear | Are there concerns that the included participants do not match the review question? | Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Are there concerns that the target condition as defined by the reference standard does not match the review question? |
Anchoring statements for quality assessment of CRC
| Question |
Response and weighting |
Explanation |
| Patient selection | ||
| Was case‐control design avoided? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
Diagnostic case‐control studies were considered inappropriate for this review because such studies are likely to overestimate diagnostic performance (Deeks 2013). Moreover, literature suggests that measures of accuracy may vary with the prevalence and stage‐distribution of the target condition (Leeflang 2009). For instance, the sensitivity of a test will often vary according to the severity of the detected disease (e.g. advanced CRCs are more easily detected with FOBTs than early‐stage tumours). This item was scored as YES if case‐control design was avoided, NO if the study was clearly a case‐design study or if this was mentioned in the article, and UNCLEAR if design of the study was unclear. |
| Did the study avoid inappropriate exclusions? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
Inappropriate exclusions may lead to a potential bias; for example, overoptimistic estimates of diagnostic accuracy. Therefore, a study should preferably enrol all consecutive, or a random sample of, eligible participants with suspected disease. |
| Was the spectrum of invitees representative of CRC screening? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
It was determined how invitees were recruited from the general population and whether this was representative for a nationwide CRC screening program. The item was scored as YES if the spectrum of invitees and the method of recruitment of study participants fulfilled the pre‐stated requirements which were described under the subheading 'Participants' in the Methods section. Studies were still eligible for inclusion and scored as YES if high‐risk individuals or screened participants aged < 40 years represented the minority of participants examined (i.e. < 5%), or if they formed an identifiable subset that could be excluded during data extraction. The item was scored as NO if the spectrum of invitees did not fulfil the pre‐stated requirements which are described under the subheading 'Participants' in the Methods section. The item was scored as UNCLEAR when there was insufficient information available to make a judgement either about the spectrum of invitees or the method of recruitment. |
| Index test | ||
| If a threshold was used, was it pre‐specified? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
Selecting the test threshold to optimise sensitivity or specificity, or both, may lead to overoptimistic estimates of test performance, which is likely to be poorer in an independent sample of participants in whom the same threshold is used (Leeflang 2008). |
| Were non‐interpretable test results reported for the index test? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
A FOBT may, for example, be non‐interpretable because the stool was applied erroneously to the test cards, or because the time between faecal sampling and arrival of the test at the laboratory was too long. Usually, in that case, a new test set will be sent to participants. This item was scored as YES if the number of non‐interpretable test results was stated, or if the number of index test results reported was in accordance with the number of participants. This item was scored as NO if it was stated that non‐interpretable test results occurred or were excluded, and if it was not reported how many. This item was scored as UNCLEAR if it was not possible to work out whether non‐interpretable test results occurred. |
| Reference standard | ||
| Were the reference standard results interpreted without knowledge of the results of the index test? |
No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
It could be hypothesised that knowing the index test result may have implications for more or less extensive searching for advanced neoplasia when the reference standard is being performed. This might positively influence the sensitivity of the index test and therefore diagnostic review bias may occur. Therefore, this item was scored as YES if the study clearly stated that the reference standard results were interpreted blind to the results of the index test. This item was scored as NO if it was clear that the reference standard was performed with knowledge of the index test. This was per definition the case for all included "reference type: positive" studies in which only screened individuals with a positive test result were referred for the reference standard. This item was scored as UNCLEAR if this information was not reported by the study. |
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? |
No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
The availability or absence of participant information and screenee characteristics such as age, gender, family history, presence or severity of symptoms, may influence the performance of the reference standard. Therefore, this item was scored as YES if it was clearly described that clinical data concerning the screened individual were available to the physician during performance of the reference standard. This item was scored as NO if clinical data were withheld or if more information than normally available was provided. This item was scored as UNCLEAR if this information about the availability of clinical data was not stated. |
| Flow and timing | ||
| Was there an appropriate time between index test(s) and reference standard to be sure that the target condition did not change? |
No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
With a polyp dwell time (i.e. defined as the average time for the transformation from a small adenomatous polyp to cancer) of approximately 10 years, CRC is generally a slow‐growing tumour (Winawer 1997). Therefore, disease progression bias is not likely to occur in a screening setting. The item was scored as YES if the delay between the performance of the index test and reference standard was on average 3 months, with a maximum of 12 months, and if for "reference type: positive" studies (detection of interval carcinomas for those with a negative index test), the follow‐up time after a negative test result was at least 12 months. The item was scored as NO if the time period between the performance of the index test and the reference standard was sufficiently long (i.e. more than 12 months) to assume that the disease status may have changed between the performance of the two tests or in case of "reference type: positive" studies, if the follow‐up time after a negative test result was shorter than 12 months. This item was scored as UNCLEAR if it was not clearly stated what the time period was between the reference standard and index test. |
| Did screened persons receive the same reference standard irrespective of index test result? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
This item was scored as YES if the same reference standard was used in all screened individuals irrespective of the FOBT result. We scored this item as NO if the choice of reference standard varied between individuals. This is per definition the case for all included "reference type: positive" studies in which only individuals with a positive test index test were referred for the reference standard, and index negative screenees were followed by interval carcinomas. This item was scored as UNCLEAR if this information was not reported by the study. |
| Were all participants included in the analysis? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
Not including a number of participants for analysis in the 2 x 2 table could potentially lead to bias. When participants that were not included differ systematically from those that were analysed, diagnostic test accuracy may differ. |
| Were withdrawals from the study explained? | No = high risk of bias Yes = low risk of bias Unclear = unclear risk of bias |
Withdrawals included participants who dropped out from the study before the results of either the index test or reference standard were known, or when they were lost to follow‐up in case of verification of test results by interval carcinomas. This item was scored YES when it was clear what happened to all individuals from the moment of invitation until the results of the reference standard were available. This item was scored as NO when it appeared that some of the participants who entered the study did not complete the study, and these participants were not accounted for. This item was scored as UNCLEAR if it was not clear how many participants entered and, hence, if there were withdrawals. |
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
1. Test.

"Reference standard: all" gFOBT AN
2. Test.

"Reference standard: positive" gFOBT CRC
3. Test.

"Reference standard: all" FIT10 AN
4. Test.

"Reference standard: all" FIT20 AN
5. Test.

"Reference standard: all" gFOBT CRC
6. Test.

"Reference standard: all" FIT CRC
7. Test.

"Reference standard: all" FIT10 CRC
8. Test.

"Reference standard: all" FIT20 CRC
9. Test.

"Reference standard: all" gFOBT_Hemoccult_II_AN
10. Test.

"Reference standard: all" gFOBT_Hemoccult_Sensa_AN
11. Test.

"Reference standard: all" gFOBT_Hemoccult_II_CRC
12. Test.

"Reference standard: all" gFOBT_Hemoccult_Sensa_CRC
13. Test.

"Reference standard: all" gFOBT_Hemoccult_AN
14. Test.

"Reference standard: all" FIT_Iatro_Hemcheck_CRC
15. Test.

"Reference standard: all" FIT AN
16. Test.

"Reference standard: all" gFOBT_Hemoccult_CRC
17. Test.

"Reference standard: all" FIT_OC_Sensor_50_AN
18. Test.

"Reference standard: all" FIT_OC_Sensor_50_CRC
19. Test.

"Reference standard: all" FIT_OC_Sensor_100_AN
20. Test.

"Reference standard: all" FIT_OC_Sensor_100_CRC
21. Test.

"Reference standard: all" FIT_OC_Light_50_AN
22. Test.

"Reference standard: all" FIT_OC_Light_100_AN
23. Test.

"Reference standard: all" FIT_OC_Light_100_CRC
24. Test.

"Reference standard: all" FIT_OC_Light_50_CRC
25. Test.

"Reference standard: all" FIT_OC_Sensa_100_CRC
26. Test.

"Reference standard: all" FIT_OC_Sensa_50_CRC
27. Test.

"Reference standard: all" FIT_OC_Sensa_100_AN
28. Test.

"Reference standard: all" FIT_OC_Sensa_50_AN
29. Test.

"Reference standard: all" FIT_OC_Micro_50_AN
30. Test.

"Reference standard: all" FIT_ELISA_Immunodiagnostik
31. Test.

"Reference standard: all" FIT_RIDASCREEN_50_AN
32. Test.

"Reference standard: all" FIT_RIDASCREEN_50_CRC
33. Test.

"Reference standard: all" FIT_RIDASCREEN_100_AN
34. Test.

"Reference standard: all" FIT_RIDASCREEN_100_CRC
35. Test.

"Reference standard: all" FIT_OC_Hemodia_AN
36. Test.

"Reference standard: all" FIT_OC_Hemodia_CRC
37. Test.

"Reference standard: positive" FIT CRC
38. Test.

"Reference standard: positive" FIT_OC_Hemodia_CRC
39. Test.

"Reference standard: positive" FIT 50 CRC
40. Test.

"Reference standard: positive" FIT 100 CRC
41. Test.

"Reference standard: positive" gFOBT_Hemoccult_II_CRC
42. Test.

"Reference standard: positive" gFOBT_Hemoccult_Sensa_CRC
43. Test.

"Reference standard: positive" FIT_OC‐Micro_CRC
44. Test.

"Reference standard: positive" gFOBT_Hemoccult_CRC
45. Test.

"Reference standard: positive" FIT_OC_Sensor_CRC
46. Test.

"Reference standard: positive" FIT_Hemeselect_CRC
47. Test.

"Reference standard: positive" FIT_Magstream_CRC
48. Test.

"Reference standard: positive" gFOBT_Hema‐screen_CRC
49. Test.

"Reference standard: positive" FIT_HM‐Jack_CRC
50. Test.

"Reference standard: positive" FIT_Monohaem_CRC
51. Test.

"Reference standard: all" FIT_OCHEMCHECK_100_CRC
52. Test.

"Reference standard: all" FIT_OCHEMCHECK_100_AN
53. Test.

"Reference standard: all" FIT_Hemosure_50_AN
54. Test.

"Reference standard: all" FIT_Hemosure_50_CRC
55. Test.

"Reference standard: all" FIT_FOBGold_AN
56. Test.

"Reference standard: all" FIT_FOBGold_CRC
57. Test.

"Reference standard: all" FIT_InvernessClearview_AN
58. Test.

"Reference standard: all" FIT_InvernessClearview_CRC
59. Test.

"Reference standard: all" FIT_AlereClearview_AN
60. Test.

"Reference standard: all" FIT_AlereClearview_CRC
61. Test.

"Reference standard: all" FIT_ Quidel _QuickVue_AN
62. Test.

"Reference standard: all" FIT_ Quidel _QuickVue_CRC
63. Test.

"Reference standard: all" FIT_ImmoCARE‐C_AN
64. Test.

"Reference standard: all" FIT_ImmoCARE‐C_CRC
65. Test.

"Reference standard: all" gFOBT_HemoCARE_AN
66. Test.

"Reference standard: all" gFOBT_hemoCARE_CRC
67. Test.
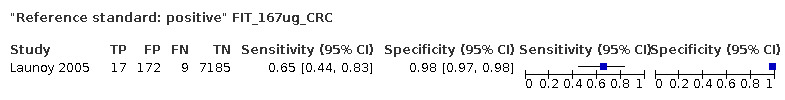
"Reference standard: positive" FIT_167ug_CRC
68. Test.

"Reference standard: positive" FIT_250ug_CRC
69. Test.

"Reference standard: all" FIT_OC_Micro_50_CRC
70. Test.

"Reference standard: all" FIT_OC_Micro_100_AN
71. Test.

"Reference standard: all" FIT_OC_Micro_100_CRC
72. Test.

"Reference standard: positive" gFOBT_Hemofec_CRC
73. Test.

"Reference standard: all" Linked‐ROC FIT AN
74. Test.

"Reference standard: all" Linked‐ROC gFOBT AN
75. Test.

"Reference standard: positive" FIT_OC_FIT_FIT‐CHEK_CRC
76. Test.

"Reference standard: positive" FIT_FOBGOLD
77. Test.

"Reference standard: all" linked‐ROC gFOBT CRC
78. Test.

"Reference standard: all" linked‐ROC all FIT CRC
79. Test.

"Reference standard: positive" linked‐ROC gFOBT CRC
80. Test.

"Reference standard: positive" linked‐ROC all FIT CRC
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahlquist 2008a.
| Study characteristics | |||
| Patient Sampling |
Design: prospective, blinded, multicenter, cross‐sectional study Setting: invitation through health care systems |
||
| Patient characteristics and setting |
Population: asymptomatic, age 50 to 80 years, 48% male Country: USA Time period: 2001 to 2007 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult Sensa Method of collection: 3 consecutive stools, collected by using plastic buckets in toilet seat. After collection, performance of test. Multiple tests were conducted on the same group of individuals. Execution: interpretation by trained technicians. Rehydration not mentioned. Positivity threshold: 1/6 panels |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy performed by: experienced endoscopists % that underwent colonoscopy: 100 Definition advanced neoplasia: curable stage colorectal cancer, high‐grade dysplasia, adenomas >1 cm |
||
| Flow and timing |
Enrolment and exclusions: 4482 enrolled. Excluded: 477 because of protocol violations, 171 because of incomplete colonoscopy, 68 stool not collected within 120 days, 2 distant metastasis CRC Number analysed: 3764 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Ahlquist 2008b.
| Study characteristics | |||
| Patient Sampling |
Design: prospective, blinded, multicentre, cross‐sectional study Setting: invitation through health care systems |
||
| Patient characteristics and setting |
Population: asymptomatic, age 50 to 80 years, 48% male Country: USA Time period: 2001 to 2007 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult Method of collection: 3 consecutive stools, collected by using plastic buckets in toilet seat. After collection, performance of test. Multiple tests were conducted on the same group of individuals. Execution: interpretation by trained technicians. Rehydration not mentioned. Positivity threshold: 1/6 panels |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy performed by: experienced endoscopists % that underwent colonoscopy: 100 Definition advanced neoplasia: curable stage colorectal cancer, high‐grade dysplasia, adenomas >1 cm |
||
| Flow and timing |
Enrolment and exclusions: 4482 enrolled. Excluded: 477 because of protocol violations, 171 because of incomplete colonoscopy, 68 stool not collected within 120 days, 2 distant metastasis CRC Number analysed: 3764 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Aniwan 2015.
| Study characteristics | |||
| Patient Sampling |
Design: cross‐sectional study Setting: participants of health promotion program performed FIT before screening colonoscopy in a university hospital |
||
| Patient characteristics and setting |
Population (including mean age, % men): asymptomatic participants aged 50 to 75 years, mean age 61 years, 35% males Country: Bangkok, Thailand Time period: February 2013 to July 2014 Number analysed: 948 |
||
| Index tests |
Index test: qualitative FIT Brand: SD Bioline FOB, Standard Diagnostics Method of collection: participants collected a one‐time stool sample at home within 3 days before colonoscopy and returned the stool container on the day of colonoscopy. Execution: the FIT was interpreted by the medical laboratory scientist, who was blinded to the colonoscopy result Positivity threshold: 50 ng/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists (> 1000 colonoscopies), blinded to FIT results % that underwent colonoscopy: 100% of analysed population Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: of the 963 eligible participants, 6 were excluded because of missing FIT and 9 because of poor bowel preparation. Number analysed: 948 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Aniwan 2017.
| Study characteristics | |||
| Patient Sampling |
Design: cross‐sectional study. Setting: participants of health promotion program performed FIT before screening colonoscopy in six university hospitals |
||
| Patient characteristics and setting |
Population (including mean age, % men): asymptomatic participants aged 50 to 75 years, mean age 60 years, 38% males Country: Bangkok, Thailand Time period: December 2014 to June 2016 Number analysed: 1479 |
||
| Index tests |
Index test: qualitative FIT Brand: OC‐Sensor (Eiken, Japan) Method of collection: participants collected a one‐time stool sample at home within 3 days before colonoscopy and returned the stool container on the day of colonoscopy. No diet restrictions Execution: the FIT was analysed within 7 days after collection. The FIT was interpreted by the medical laboratory scientist, who was blinded to the colonoscopy result. Positivity threshold: multiple thresholds are reported |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy performed by: experienced endoscopists (> 1000 colonoscopies) % that underwent colonoscopy: 100% of analysed population Definition of advanced neoplasia: adenoma with high‐grade dysplasia, or villous adenoma (> 25 %), or > 10 mm size or CRC |
||
| Flow and timing |
Enrolment and exclusions: of 1580 screened, 60 were excluded due to age > 75 years, missed stool collection and poor bowel preparation. Number analysed: 1520 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Arana‐Arri 2017a.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cohort study Setting: Basque Colorectal Cancer Screening Programme |
||
| Patient characteristics and setting |
Population: participants aged 50 to 69 and resident. Mean age and % male not given for complete cohort Country: Spain (Basque Country) Time period: 2009 to 2012 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Micro and FOB‐Gold in the first screening round. Afterwards only OC‐Sensor Method of collection: not specified Execution: processed and analysed in centralised public laboratories under strict total quality management systems Positivity threshold: 20 µg Hb/g faeces for both tests |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: expert specialists in referral public hospitals % that underwent colonoscopy: 94.7% of positive participants |
||
| Flow and timing |
Enrolment and exclusions: 296,378 participants participated in screening, with 18,273 positive tests. 17,304 of 18,273 (94.7%) screen‐positive participants had colonoscopy. 1441 FIT‐positive participants underwent colonoscopy in FOB‐Gold group Number analysed: 295,409. 17,304 FIT‐positive participants underwent colonoscopy, of which 1441 in the FOB‐Gold group Identification of interval cancers: interval cancers, defined as CRC prior to a subsequent invitation, were identified from linkage to hospital discharges and population‐based cancer registries and pathology systems. Also, information provided about interval CRC within one or two years after negative test. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Arana‐Arri 2017b.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cohort study Setting: Basque Colorectal Cancer Screening Programme |
||
| Patient characteristics and setting |
Population: participants aged 50 to 69 and resident. Mean age and % male not given for complete cohort Country: Spain (Basque Country) Time period: 2009 to 2012 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Micro and FOB‐Gold in the first screening round. Afterwards only OC‐Sensor Method of collection: not specified Execution: processed and analysed in centralised public laboratories under strict total quality management systems Positivity threshold: 20 µg Hb/g faeces for both tests |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: expert specialists in referral public hospitals % that underwent colonoscopy: 94.7% of positive participants |
||
| Flow and timing |
Enrolment and exclusions: 296,378 participants participated in screening, with 18,273 positive tests. 17,304 of 18,273 (94.7%) screen‐positive participants had colonoscopy. 1441 FIT‐positive participants underwent colonoscopy in FOB‐Gold group Number analysed: 295,409. 17,304 FIT‐positive participants underwent colonoscopy, of which 1441 in the FOB‐Gold group Identification of interval cancers: interval cancers, defined as CRC prior to a subsequent invitation, were identified from linkage to hospital discharges and population‐based cancer registries and pathology systems. Also, information provided about interval CRC within one or two years after negative test Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Blanks 2019.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based screening study Setting: National Health Service (NHS) bowel cancer screening program in England |
||
| Patient characteristics and setting |
Population: women aged 60 to 74 and resident in England and registered in NHS. Mean age not given for complete cohort. 0% men Country: England Time period: 1 December 2006 to 31 March 2012 |
||
| Index tests |
Index test: qualitative gFOBT Brand: Hemascreen Method of collection: three separate stools deliver two small faecal samples each. In total six windows are tested. Execution: no dietary restrictions Positivity threshold: > 4 out of 6 windows positive is considered positive. When 1 to 4 windows are positive, a second (and third) test is offered. If at least 1 window is positive in this second or third collection, follow‐up evaluation is offered. |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test (default), flexible sigmoidoscopy and radiological investigations. In > 97% of FOB+ participants, colonoscopy is considered as most appropriate first follow‐up evaluation. Performed by: not specified % that underwent colonoscopy: 87% of positive participants (7911 out of 9133 participants) |
||
| Flow and timing |
Enrolment and exclusions: 628,976 participants participated in the first round of screening. 1222 of 9133 screen‐positive participants had no colonoscopy. Number analysed: 627,754. 628,976 participants participated in the first round of screening. 7911 of 9133 positive participants underwent colonoscopy. Identification of interval cancers: interval cancers, defined as CRC within two years of a negative result, were identified from the national cancer registry. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | No | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Bouvier 1999.
| Study characteristics | |||
| Patient Sampling |
Design: prospective population‐based study Setting: 1st round of screening in six areas of department of Calvados, France. Invitation via general practitioners and occupational doctors |
||
| Patient characteristics and setting |
Population: 165,000 people, aged 45 to 74 years, 51.1% male Country: France Time period: April 1991 to December 1994 |
||
| Index tests |
Index test: gFOBT Brand: Haemocullt II Method of collection: no dietary or drug restrictions were required Execution: all tests were mailed to a single centre and were processed without rehydration Positivity threshold: 1/6 panels |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy and in case of incomplete colonoscopy, DCBE, or follow‐up Performed by: not specified % that underwent colonoscopy: 63.2%. A total of 2020 positive tests, 1603 had a colonoscopy and DCBE (79.4%, of which 1277 had only colonoscopy (63.2%). |
||
| Flow and timing |
Enrolment and exclusions: all inhabitants of selected department, no exclusions. 22 cancers were excluded because of missing data; not clear if this is only from participants with negative test or also from non‐participants / reference group. 71,307 completed the test (43.3%). Number analysed: 71,307 Identification of interval cancers: recorded by the local digestive cancer registry Definition of interval cancers: all the cancers diagnosed between 1991 and 1995 in people living in the department, whether they occurred in a person participating in the screening or not. Follow‐up time: at least 12 months for all and 24 months for 90.5% |
||
| Comparative | |||
| Notes | Only 63% colonoscopy, additional 16% had DBCE Calculated incidence based on FU |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Brenner 2012.
| Study characteristics | |||
| Patient Sampling |
Design: observational study in 13 gastroenterological centres Setting: recruited participants who requested screening colonoscopy |
||
| Patient characteristics and setting |
Population: asymptomatic population, mean age 62 years, 50.3% male Country: Germany Time period: 2008 to 2009 |
||
| Index tests |
Index test: qualitative FIT and gFOBT (participants underwent both tests) Brand: immoCARE‐C (FIT) hemoCARE (gFOBT) Method of collection: both tests were performed on three different stool samples; for the FIT test, three test sticks were given Execution: not specified Positivity threshold: not specified |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: 13 gastroenterology physician practices % that underwent colonoscopy: 100% Definition advanced neoplasia: adenomas > 10 mm, villous adenoma or carcinoma |
||
| Flow and timing |
Enrolment and exclusions: 925 participants; 279 excluded because of missing data on colonoscopy or stool test results. Maximum of 310 days between index test and colonoscopy Number analysed: 646 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Brenner 2013.
| Study characteristics | |||
| Patient Sampling |
Design: prospective study Setting: participants of a screening colonoscopy study (Blitz) in Germany, invited for additional stool tests |
||
| Patient characteristics and setting |
Population: asymptomatic first‐time participants aged 50 to 79 years, mean age 63 years, 49% male Country: Germany Time period: 2005 to 2009 |
||
| Index tests |
Index test: gFOBT (+3 brands of FIT) Brand: HemOccult (Beckman Coulter, Krefeld Germany) Method of collection: no dietary restrictions, stool from one bowel movement, apply to 2 windows of 1 gFOBT test card Execution: by practice personnel, on average 4 days after stool collection and storage at room temperature. Rehydration not mentioned Positivity threshold: 1/2 windows of 1 slide (index test not conducted as usual: only one stool and only one of 3 cards used) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not specified % that underwent colonoscopy: 98% Definition advanced neoplasia: CRC + advanced adenoma (advanced adenoma not defined ) |
||
| Flow and timing |
Enrolment and exclusions: 2414 first‐time participants of screening colonoscopy for whom results of gFOBT, FIT, and colonoscopy were available. 102 excluded because stool sample on day of/after colonoscopy, 77 with histologically undefined polyps. Number analysed: 2235 |
||
| Comparative | |||
| Notes | FIT data from this article not included in review as these data are included in the article by Haug 2011 Multiple tests were conducted on the same group of individuals in these studies (Haug 2011, Brenner 2013) |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Brenner 2018.
| Study characteristics | |||
| Patient Sampling |
Design: prospective study Setting: participants of a screening colonoscopy study (Blitz) in Germany, invited for additional stool tests |
||
| Patient characteristics and setting |
Population: asymptomatic first‐time participants aged 50 to 79 years, mean age 60 years, 49% male Country: Germany Time period: January 2012 and June 2016 |
||
| Index tests |
Index test: FIT Brand: FOB Gold (Sentinel, Italy) Method of collection: no dietary restrictions, stool sample from one bowel movement done by the screenee and sent by mail. Execution: stool sample was send by mail and kept at 2 to 8 degrees Celcius and analysed in an accredited laboratory (Labor Imbach, Heidelberg, Germany), described according to FITTER guidelines. Positivity threshold: multiple thresholds are shown, including the threshold recommended by the manufacturer |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not specified % that underwent colonoscopy: 100% (of included participants) Definition advanced neoplasia: CRC or a non‐serrated adenoma with any of the following features: > 1 cm in size, tubulovillous or villous components or high‐grade dysplasia |
||
| Flow and timing |
Enrolment and exclusions: 4193 study participants were recruited, of which 170 did not meet the age criteria, 41 had a history of CRC or IBD, 270 had a colonoscopy in the past 5 years, 472 had an inadequate bowel preparation, 29 had an incomplete colonoscopy. Number analysed: 3211 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Burón 2019.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based screening study Setting: Barcelona Early Detection for Colon and Rectum Cancer programme |
||
| Patient characteristics and setting |
Population: people aged 50 to 69. Mean age not given for complete cohort. 52.8% of target population and 55.8 of participation population were women. Country: Spain Time period: 2010 to 2013 |
||
| Index tests |
Index test: qualitative FIT Brand: OC‐Sensor Method of collection: not specified Execution: not specified Positivity threshold: 20 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: not specified % that underwent colonoscopy: total number of positive tests and total number of performed colonoscopies not stated in article |
||
| Flow and timing |
Enrolment and exclusions: 79,922 participants. 4974 positive tests. 4182 positive participants underwent colonoscopy (84.1%). 251 screen‐detected CRC diagnosed and 47 interval cancers (IC) after 2‐year follow‐up. Number analysed: 79,130 Identification of interval cancers: interval cancers, defined as CRC within two years of a negative result, were identified after notification in the Barcelona Early Detection for Colon and Rectum Cancer programme or after crossing the programme, hospital and Catalonia Minimum Basic Data set. Follow‐up time: 2 years (separate results for number of interval cancers after 1 year) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Castiglione 2007.
| Study characteristics | |||
| Patient Sampling |
Design: national screening program Setting: participants living in 19 municipalities in the Province of Florence attending FOBT screening |
||
| Patient characteristics and setting |
Population: participants aged 50 to 70 years, 48% male Country: Italy Time period: January 2000 to December 2002 |
||
| Index tests |
Index test: quantitative FIT (latex agglutination test) Brand: OC‐Hemodia, developed with the OC‐Sensor Method of collection: not described Execution: not described Positivity threshold: 100 ng Hb/mL (20 µg Hb/g faeces) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up Performed by: not specified % that underwent colonoscopy: out of 1097 positives, 959 (87%) accepted further workup with colonoscopy. In 171 cases, colonoscopy was incomplete; in 166 of these DCBE was performed. So 72% total underwent colonoscopy. |
||
| Flow and timing |
Enrolment and exclusions: 24,913 participants performed 27,503 FITs; they were excluded in case of positive FIT and no colonoscopy and cancer after more than 1 year Number analysed: 27,365 Identification of interval cancers: through linkage to Tuscany cancer registry Definition ofinterval cancers: all cancers after negative FIT or positive FIT with negative colonoscopy Follow‐up time: 1 to 2 years (2000 to 2003) |
||
| Comparative | |||
| Notes | 24,913 participants, performed 27,503 tests; 2590 extra tests are unexplained | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Chang 2017.
| Study characteristics | |||
| Patient Sampling |
Design: prospective Setting: screening colonoscopies and FITS at the Health Management Center of National Taiwan University Hospital |
||
| Patient characteristics and setting |
Population: asymptomatic participants (only ethnic Chinese), mean age 59 years (SD 7.0 years), 51% male Country: Taiwan Time period: August 2010 to November 2014 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor (Eiken, Japan) Method of collection: no dietary restrictions, stool from one bowel movement Execution: by screenees at home 2 days before the colonoscopy using the collecting stick, and to refrigerate the samples until colonoscopy. Samples were sent the same day to the clinical laboratory Positivity threshold: 100 ng Hb/mL (20 µg Hb/g faeces) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists ( > 5000 colonoscopies performed) % that underwent colonoscopy: 100% Definition advanced neoplasia: only adenomas included, advanced was defined as > 1 cm in size, tubulovillous or villous components and high‐grade dysplasia (WHO criteria) |
||
| Flow and timing |
Enrolment and exclusions: 36,720 screenees received a screening colonoscopy during the study period, the majority (n = 21,605) had received a screening colonoscopy in the past 5 years. People with family or personal history of CRC, those younger than 50 years, those who did not submit a stool sample, those with an incomplete colonoscopy or those with invasive cancer (n = 3) were excluded. Number analysed: 6198 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Chen 2014.
| Study characteristics | |||
| Patient Sampling |
Design: retrospective analysis of prospectively enrolled population Setting: asymptomatic Taiwanese population that underwent health checkup |
||
| Patient characteristics and setting |
Population: asymptomatic population, 40 years or older, mean age 53.6 years old, 56% men. Country: Taiwan Time period: 2008 to 2009 |
||
| Index tests |
Index test: qualitative FIT Brand: OC‐Light (Eiken, Japan) Method of collection: one stool sample Execution: automated analysis Positivity threshold: 10 µg Hb/g faeces (50 ng/mL buffer) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists % that underwent colonoscopy: 100% Definition of advanced neoplasia: same as protocol |
||
| Flow and timing |
Enrolment and exclusions: 8258 consecutively enrolled, 2162 excluded. Exclusion criteria: under 40 years old (n = 1584), incomplete or missing information (n = 578), CRC, IBD, visible rectal bleeding or menstruation during time of stool collection. Number analysed: 6096 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Chen 2016a.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based screening study Setting: bowel cancer screening programme in Taiwan |
||
| Patient characteristics and setting |
Population: participants aged ≥ 20 years participating in a standard medical screening program. % males not reported. Country: Taiwan Time period: 1994 to 2007 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: not specified Execution: not specified Positivity threshold: 100 ng/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: gastroenterologists % that underwent colonoscopy: unknown; colonoscopy outcome retrieved by contacting national cancer registration |
||
| Flow and timing |
Enrolment and exclusions: in total 512,066 participants underwent FIT testing and follow‐up via cancer registration. 141,045 participants were above 50 years old, of which 8583 tested positive. It is not known how many positive participants underwent colonoscopy. Number analysed: 141,405 Identification of interval cancers: interval cancers, defined as CRC within two years of a negative result, were identified from the National Cancer Registry. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Cheng 2002.
| Study characteristics | |||
| Patient Sampling |
Design: cross‐sectional analysis of voluntary screening program Setting: asymptomatic adults who underwent colonoscopy in a health screening program |
||
| Patient characteristics and setting |
Population: asymptomatic adults, mean age 47 years (we used sub‐analysis of participants 40+ years old), 81% male Country: Taiwan Time period: 1997 to 2000 |
||
| Index tests |
Index test: qualitative FIT Brand: OC‐Hemodia Method of collection: diet instructions for 3 days, stool collection on day of colonoscopy Execution: not specified Positivity threshold: not specified (qualitative test so pre‐specified) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: well‐trained and board‐certified gastroenterologists % that underwent colonoscopy: 100% Definition advanced neoplasia: advanced neoplasm: polyp larger than 1 cm, polyps with villous or severe dysplastic features and cancer |
||
| Flow and timing |
Enrolment and exclusions: 7617 examined: 206 excluded because of exclusion criteria, 7411 examined for study. We used sub‐analysis of participants 40+ years old. Exclusion criteria: known history of colorectal cancer, IBD, rectal bleeding, recent changes in bowel habits, weight loss, anaemia, or positive FOBT on prior examinations. Individuals with a personal history of colonic polyps or a family history of colon cancer were not excluded. Number analysed: 5067 |
||
| Comparative | |||
| Notes | Data for participants > 40 years received from authors (n = 5067) CFOBB test results not extracted (= toluidine test, not guaiac) |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Chiang 2014a.
| Study characteristics | |||
| Patient Sampling |
Design: nationwide CRC screening program Setting: residents were invited for biennial FIT screening at 810 screening sites |
||
| Patient characteristics and setting |
Population: aged 50 to 69 years, mean age 58.42 (OC‐Sensor), 38.4% males Country: Taiwan Time period: 1 January 2004 to 31 December 2009 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: 1 test at home in 1 stool Execution: in one of the 125 qualified laboratories Positivity threshold: 20 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy and DCBE, or follow‐up Performed by: not described % that underwent colonoscopy: 86.2% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 747,076 participants underwent screening; exclusions not clearly described Number analysed: 747,076 Identification of interval cancers: Taiwan cancer registry Definition of interval cancers: invasive CRC diagnosed after a negative FIT and < 2 years to the next screen Follow‐up time: > 3 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Chiang 2014b.
| Study characteristics | |||
| Patient Sampling |
Design: nationwide CRC screening program Setting: residents were invited for biennial FIT screening at 810 screening sites |
||
| Patient characteristics and setting |
Population: aged 50 to 69 years, mean age 57.89 years (HM‐Jack), 38.4% males Country: Taiwan Time period: 1 January 2004 to 31 December 2009 |
||
| Index tests |
Index test: quantitative FIT Brand: HM‐Jack Method of collection: 1 test at home in 1 stool Execution: in one of the 125 qualified laboratories Positivity threshold: 20 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy and DCBE, or follow‐up Performed by: not described % that underwent colonoscopy: 86.2% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 208,929 participants underwent screening; exclusions not clearly described. Number analysed: 208,929 Identification of interval cancers: Taiwan cancer registry Definition of interval cancers: invasive CRC diagnosed after a negative FIT and < 2 years to the next screen Follow‐up time: > 3 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Chiu 2013.
| Study characteristics | |||
| Patient Sampling |
Design: prospective screening study Setting: asymptomatic adults invited for health checkup |
||
| Patient characteristics and setting |
Population: asymptomatic, age 50 years and older, mean age 59.8 years, 59% male Country: Taiwan Time period: 2005 to 2010 |
||
| Index tests |
Index test: qualitative FIT Brand: OC‐LIGHT V‐PC50 and V‐PH80 Method of collection: 1 stool sample 1 day before colonoscopy, no diet restrictions Execution: automated analysis with qualitative result at cut‐off of 50 ng Hb/mL Positivity threshold: 10 µg Hb/g faeces (50 ng Hb/mL) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists % that underwent colonoscopy: 100% Definition advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: target population was 33,263. Participants who were younger than 50 years old (n = 12.997), had CRC, and received colectomy (n = 96), did not submit faecal samples (n = 1555) or had incomplete colonoscopy (n = 319) were excluded. Number analysed: 18,296 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Chiu 2016a.
| Study characteristics | |||
| Patient Sampling |
Design: multicentre prospective study Setting: participants visiting bowel cancer screening centres or general medical outpatient clinics |
||
| Patient characteristics and setting |
Population: asymptomatic individuals aged > 40 years, mean age 57.8 years, 51% male. Participants had to fill out the Asia‐Pacific Colorectal Cancer Screening score and were divided in to low‐, medium‐, and high‐risk groups, according to the score. Country: 15 sites, including Australia, Brunei, China, Hong Kong, Japan, South Korea, Malaysia, Pakistan, Philipines, Singapore, Taiwan, and Thailand Time period: December 2011 to December 2013 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor (Eiken, Japan). However, the OC‐Sensor was not available in all countries; therefore, other available FIT kits were used. Method of collection: not described Execution: by screenees following the manual's instructions Positivity threshold: for OC‐Sensor, 20 µg Hb/g faeces; for other FIT kits, the cut‐off value as recommended by the manufacturer was used (not further specified in article) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: 100% Definition advanced neoplasia: CRC or adenomas which were > 1 cm in size, tubulovillous or villous components or high‐grade dysplasia (WHO criteria) |
||
| Flow and timing |
Enrolment and exclusions: exclusion criteria included history of colonic diseases that increase the risk of CRC; a CRC screening examination in the past 5 years; severe premorbid illness Number analysed: 5657 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Crotta 2012.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cohort study Setting: residents identified through regional health service register invited for screening |
||
| Patient characteristics and setting |
Population: asymptomatic, aged 50 to 74 years; mean age and male/female ratio not specified Country: Italy, Aosta Valley region Time period: 2001 to 2003 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor (Eiken, Japan) Method of collection: 1 sample of 1 bowel movement, without dietary restrictions Execution: automated analysis in 1 central laboratory Positivity threshold: 100 ng/mL (20 µg Hb/g faeces) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up Performed by: not specified, almost all performed in one hospital % that underwent colonoscopy: 93% of positives |
||
| Flow and timing |
Enrolment and exclusions: 2959 invited. General practitioners (GPs) were involved in the organisation of screening and were asked to exclude people with a personal history of polyps or CRC and inflammatory bowel disease. People reporting recent colorectal endoscopy (within the previous 5 years), or FOBT (within the previous 2 years), and people with terminal illness or unable to provide consent also were excluded. Number analysed: 1655 Identification of interval cancers: interval CRCs were identified through a record linkage of the study database with the regional hospital discharge records and with the archives of the Pathology Department of the Aosta Regional Hospital. Definition of interval cancers: interval cancers were defined as CRCs diagnosed within 2 years of a negative FIT. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Cruz‐Correa 2007.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cross‐sectional study Setting: university hospital, referred for colonoscopy |
||
| Patient characteristics and setting |
Population: asymptomatic people referred for colonoscopy, age 50 years and older, 37% male Country: USA Time period: 2002 to 2003 |
||
| Index tests |
Index test: 2x gFOBT Brand: EZ‐direct and Hemoccult II Method of collection: 2 consecutive bowel movements 1 week before colonoscopy, diet restrictions 3 days prior to test Execution: non‐rehydrated, interpretation by 2 investigators independently Positivity threshold: EZ‐direct: 1/3 cards; Hemoccult: 1/6 windows positive |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: endoscopists % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 207 analysed in study, only 126 screening participants used Number analysed: 126 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Denters 2012a.
| Study characteristics | |||
| Patient Sampling |
Design: RCT screening study (randomisation between gFOBT and FIT) Setting: population‐based screening pilot |
||
| Patient characteristics and setting |
Population: average risk, 50 to 74 years living in the catchment area of the screening program. Mean age 60 years, 43% male Country: the Netherlands Time period: 2008 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult II Method of collection: gFOBT: No dietary instructions. Participants were instructed to collect 2 samples of 3 consecutive bowel movements. Execution: gFOBT: cards were not rehydrated and read by 2 trained laboratory technicians. Positivity threshold: gFOBT: 1/6 windows |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up Performed by: experienced endoscopists % that underwent colonoscopy: 82% of positives Definition advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 10,054 invited, 4990 participants Number analysed: gFOBT: 2112 (FIT: 2824) Identification of interval cancers: interval cancers were identified through cross‐linkage of the screening pilot database with the Dutch cancer registry. Definition of interval cancers: defined as proportion of cancers diagnosed in first‐round participants (both guaiac FOBT and FIT) outside the screening protocol but within the screening interval. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Denters 2012b.
| Study characteristics | |||
| Patient Sampling |
Design: RCT screening study (randomisation between gFOBT and FIT) Setting: population‐based screening pilot |
||
| Patient characteristics and setting |
Population: average risk, 50 to 74 years living in the catchment area of the screening program. Mean age 60 years, 43% male Country: the Netherlands Time period: 2008 |
||
| Index tests |
Index test: quantitative FIT (participants were randomised to one of the tests) Brand: OC‐Sensor Method of collection: FIT: one sample of one bowel movement Execution: FIT: after arrival at the laboratory, tests were stored at 4°C and processed in batches by using an automated clinical analyser (OC‐Sensor Micro; Eiken). Positivity threshold: FIT: 10 µg Hb/g faeces (50 ng Hb/mL buffer) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up Performed by: experienced endoscopists % that underwent colonoscopy: 82% of positives Definition advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 10,054 invited, 4990 participants Number analysed: FIT: 2824 (gFOBT: 2112) Identification of interval cancers: interval cancers were identified through cross‐linkage of the screening pilot database with the Dutch cancer registry. Definition of interval cancers: defined as proportion of cancers diagnosed in first‐round participants (both guaiac FOBT and FIT) outside the screening protocol but within the screening interval. Follow up time: 2 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
De Wijkerslooth 2012.
| Study characteristics | |||
| Patient Sampling |
Design: prospective screening study Setting: invitation for colonoscopy screening, additional FIT performed before colonoscopy |
||
| Patient characteristics and setting |
Population: asymptomatic, age 50 to 75 years, median age 60 years, 51% male Country: the Netherlands Time period: 2009 to 2010 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Execution: automated analysis Method of collection: one stool sample 1 week before colonoscopy, no diet restrictions Positivity threshold: > 50 ng Hb/mL buffer |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: highly experienced endoscopists (> 1000 performed) % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 6600 invitees for colonoscopy screening, 1616 received colonoscopy intake, 130 excluded, 170 refused FIT, 58 refused colonoscopy, 1256 performed index test + reference standard. Number analysed in study: 1256 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Digby 2016.
| Study characteristics | |||
| Patient Sampling |
Design: prospective population‐based screening study Setting: two NHS Boards in the Scottish Bowel Screening Programme |
||
| Patient characteristics and setting |
Population: participants aged 50 to 74 and resident in National Health Service (NHS) Tayside and NHS Ayrshire & Arran. Both NHS Boards had offered screening previously, using a gFOBT/qualitative FIT but this was the first time that any participant had taken part in a quantitative FIT‐based CRC screening programme. Mean age and % male not given for complete cohort. Country: Scotland Time period: 1 July 2010 to 12 January 2011 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: not specified Execution: On OC‐Sensor‐Diana automated immunoturbidimetric analysers Positivity threshold: 80 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: not specified % that underwent colonoscopy: 86% of positive participants |
||
| Flow and timing |
Enrolment and exclusions: 30,893 participants participated in screening, with 30,140 participants screen‐negative. Of the 753 screen‐positive participants, 104 did not complete colonoscopy. Number analysed: 30,789 identification of interval cancers: interval cancers, defined as CRC within two years of a negative result, were identified from the Scottish Cancer Registry. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Faivre 2004.
| Study characteristics | |||
| Patient Sampling |
Design: prospective population‐based CRC screening trial Setting: biennial screening program for CRC for all residents in 12 administrative districts in Burgundy, France. Invitation by mail signed by their GPs. |
||
| Patient characteristics and setting |
Population: all residents in 12 administrative districts in Burgundy, France, born between 1914 and 1943. Mean age and male/female ratio not specified. Country: France Time period: 1988 and 1989 |
||
| Index tests |
Index test: gFOBT Brand: Hemocullt II Execution: processed without rehydration Method of collection: 2 samples of 3 consecutive stools, no diet restrictions Positivity threshold: not defined |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: gastroenterologists % that underwent colonoscopy: not described; full bowel exploration 85% (includes DCBE) |
||
| Flow and timing |
Enrolment and exclusions: invitation by sending an information letter, signed by the general practitioners (GPs) working in the screening areas, to each invited participant, along with a 4‐page information brochure. For participants who did not consult their GPs during the 4‐month period and those who did not complete the test, the co‐ordination centre subsequently mailed the test and, when necessary, a reminder letter 1 month later. Exclusions: people who died in the interval, moved from the region, clearly refused to receive any more screening material, or were excluded by GPs because of life‐threatening illness. Number analysed: 24,099 Identification of interval cancers: Burgundy Cancer Registry. Not clear if any of the interval cancers were in participants with positive FIT and no FU (15%) Definition of interval cancers: cancers diagnosed after a negative FOBT within the interval between 2 screenings and at any time for those who were not re‐screened. Follow up time: > 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Giai 2014.
| Study characteristics | |||
| Patient Sampling |
Design: prospective study, retrospective analysis Setting: population‐based screening program |
||
| Patient characteristics and setting |
Population: asymptomatic individuals, 50 to 74 years, living in the Isère department. Mean age 65 years, 62% male Country: France Time period: 2002 to 2006 Number analysed: 84,897 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult II Method of collection: two samples from each of three stools, diet not specified Execution: in analysis centre, (non)rehydration not specified Positivity threshold: not specified |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: not specified |
||
| Flow and timing |
Enrolment and exclusions: not specified. GP provided FOBT after checking for exclusion criteria. Exclusion criteria: personal or family history of CRC, history of adenomatous polyps, symptoms suggestive of cancer, colonoscopy in past 5 years. Number analysed: 86,750 Identification of interval cancers: via cancer registry database Definition of interval cancers: CRC diagnosed within 2 years of a negative test or a test that could not be analysed Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | Article only describes CRCs; data for 2x2 table received from authors | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Graser 2009.
| Study characteristics | |||
| Patient Sampling | Design: prospectiveSetting: not described | ||
| Patient characteristics and setting |
Population: average‐risk participants older than 50 years; not clear how consulted. 54.9% male Country: Germany Time period: not specified Number invited: 311 Number analysed: 276 |
||
| Index tests |
Index test: quantitative FIT and gFOBT (participants underwent both tests) Brand: FOBT‐Gold and for gFOBT not specified Method of collection: 2 FITs on 2 different parts from the same stool and gFOBT on 3 consecutive stools Execution: FIT automated analysis and gFOBT judged by staff Positivity threshold: FIT 14 ng Hb/mL (2.8 µg Hb/g faeces), the highest value of both tests was used. For gFOBT 1/3 samples |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy (and CT‐colonography) Performed by: six experienced gastroenterologists % that underwent colonoscopy: 100 Definition of advanced neoplasia: not defined, but characteristics of all polyps are listed |
||
| Flow and timing |
Enrolment and exclusions: 311 enrolled, 4 withdrawals, FIT results available for 258, gFOBT for 276 participants Number analysed: 285 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Haug 2011.
| Study characteristics | |||
| Patient Sampling |
Design: prospective colonoscopy‐screening study Setting: opportunistic colonoscopy screening |
||
| Patient characteristics and setting |
Population: asymptomatic, age 55 to 80 years, mean age and male/female ratio of total not specified Country: Germany Time period: 2006 to 2009 |
||
| Index tests |
Index test: quantitative FIT Brand: RIDASCREEN Execution: automated analysis Method of collection: stool from 1 bowel movement, without diet restrictions Positivity threshold: 10 µg Hb/g and 20 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 3077 consented to screening colonoscopy; 752 excluded, 15 excluded because advanced neoplasia in both left and right colon (these are re‐included in this analysis) Number analysed: 2310 |
||
| Comparative | |||
| Notes | 2x2 table received from authors including 15 excluded because of advanced neoplasia in both left and right colon Multiple tests were conducted on the same group of individuals in these studies (Haug 2011, Brenner 2013) |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | No | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Hernandez 2014.
| Study characteristics | |||
| Patient Sampling |
Design: multicentre, prospective, double‐blind study (COLONPREV study) Setting: average‐risk individuals submitted to screening colonoscopy in 3 tertiary hospitals in Spain |
||
| Patient characteristics and setting |
Population: average‐risk individuals aged 50 to 69 years, 49.6% males, mean age 57.5 years Country: Spain Time period: 1 January 2010 to 30 June 20111 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: 2 stool samples from 2 consecutive days the week before the colonoscopy was scheduled, without diet or medication restrictions. Execution: automated analysis. Faecal haemoglobin concentration was determined in the first sample (FIT1) and the highest level of both samples (FITmax). We only used results of FIT1. Positivity threshold: all, specified for 50 ng Hb/mL and 100 ng Hb/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not reported % that underwent colonoscopy: 94% (54 out of 851 did not complete colonoscopy) Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 851 were included and 779 were analysed (completed both FIT and colonoscopy) Number analysed: 779 |
||
| Comparative | |||
| Notes | Two stool samples from 2 consecutive days were collected; we only used results of the first sample (FIT1). | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Hoepffner 2006.
| Study characteristics | |||
| Patient Sampling | Design: prospective multicentre studySetting: participants referred for colonoscopy at 4 different centres | ||
| Patient characteristics and setting |
Population: participants referred for colonoscopy (both symptomatic as well as asymptomatic); only screened population used for this review (48% males) Country: Germany Time period: not specified |
||
| Index tests |
Index test: gFOBT, ELISA iFOBT and bedside test strip device Prevent ID CC (latter not used in review) (participants underwent all tests) Brand: Haemocullt and Hb ELISA (Immunodiagnostik) Execution: gFOBT non‐hydrated and iFOBT by automated analysis Method of collection: one stool sample Positivity threshold: 1/3 for gFOBT and 10 µg Hb/g stool for iFOBT |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists ('experienced' not defined) % that underwent colonoscopy: 100% Definition of advanced neoplasia: CRC + large adenomas (> 10 mm) |
||
| Flow and timing |
Enrolment and exclusions: 237 symptomatic participants and 150 healthy participants undergoing CRC screening were enrolled. 387 participants underwent 407 tests. All participants with repeat tests were known IBD cases, according to manuscript. Nevertheless, results for 156 screening participants given. Number analysed: 156 |
||
| Comparative | |||
| Notes | Authors did not respond to emails with request for clarification. Manufacturer of the iFOBT clarified the correct cut‐off (10 µg Hb/g stool instead of 10 g Hb/mL stool) | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Imperiale 2004.
| Study characteristics | |||
| Patient Sampling | Design: prospective multicentre study Setting: participants recruited from a total of 81 private‐practice and university‐based settings | ||
| Patient characteristics and setting |
Population: asymptomatic individuals older than 50 years undergoing screening colonoscopy; analysed subgroup 45% male, mean age 69.5 years Country: USA Time period: August 2001 and March 2003 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult II Method of collection: three cards for three stools, with dietary and medication modifications Execution: non‐hydrated analysis by the physician or a designee Positivity threshold: not specified |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: colonoscopists (not further specified) % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: a total of 5486 participants were enrolled, of whom 4404 could be fully evaluated. 2x2 table only extractable for analysed subgroup of 2507. Number analysed: 2505 (rectal carcinoid and cloacogenic cancer deleted) |
||
| Comparative | |||
| Notes | Authors did not respond to emails with request for data to extract 2x2 table on all study participants. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Imperiale 2014.
| Study characteristics | |||
| Patient Sampling |
Design: cross‐sectional prospective study Setting: 90 sites throughout the USA and Canada, including private practice and academic settings |
||
| Patient characteristics and setting |
Population: asymptomatic persons 50 to 84 years old were enrolled to undergo screening colonoscopy. Mean age of evaluable subgroup 64.2 years; 46.3% male. Country: Canada and USA Time period: June 2011 to November 2012 |
||
| Index tests |
Index test: quantitative FIT Brand: OC FIT‐CHECK (Polymedco) Method of collection: one stool sample before bowel preparation, collected in container. No diet restrictions. Execution: performed in stool from container according to manufacturer's instructions Positivity threshold: 100 ng Hb/mL (20 µg Hb/g faeces) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol plus sessile serrated polyps measuring 1 cm or more |
||
| Flow and timing |
Enrolment and exclusions: 12,776 were enrolled; 11,016 could be evaluated and 9989 had results that could be fully evaluated Number analysed: 9989 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Itoh 1996.
| Study characteristics | |||
| Patient Sampling |
Design: prospective study Setting: colorectal cancer screening program for Japanese workers |
||
| Patient characteristics and setting |
Population: Japanese workers > 40 years, 86% male. Most participants had experienced CRC screening by gFOBT between 1982 and 1990. Country: Japan Time period: 1991 to 1992 |
||
| Index tests |
Index test: FIT Brand: OC‐Hemodia, Eiken, Japan Method of collection: one sample from one bowel movement Execution: automatically analysed with OC‐Sensor analyser Positivity threshold: 10 µg Hb/g faeces (50 ng/mL) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: 81% |
||
| Flow and timing |
Enrolment and exclusions: 33,049 invited; 27,860 participated, 1490 positive test, 1207 underwent colonoscopy Identification of interval cancers: via health insurance claims because all medical expenses were incurred by a single health insurance organisation Definition of interval cancer: diagnosed with CRC within 2 years after negative test Follow‐up time: 2 years Number analysed: 27,577 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Jensen 2016.
| Study characteristics | |||
| Patient Sampling |
Design: retrospective cohort study Setting: population‐based screening in Kaiser Permanente Northern and Southern California (KPNC, KPSC) |
||
| Patient characteristics and setting |
Population: a total of 323,349 health plan members aged 50 to 70 years. 46.4% male Country: California, USA Time period: January 2007 to December 2013 |
||
| Index tests |
Index test: quantitative FIT Brand: OC FIT‐CHEK Method of collection: not specified Execution: OC‐Sensor‐Diana automated system (Polymedco) Positivity threshold: 20 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: the FIT results recorded within 1 year of each mail date, and colonoscopies performed and adenomas or CRC diagnosed within 1 year after FIT results were considered part of a single screening episode for the round when the FIT was distributed. Performed by: not described Percentage that underwent colonoscopy: out of 16,037 first‐round FIT‐positive participants, 12,112 underwent colonoscopy (75.5%) within one year of positive result |
||
| Flow and timing |
Enrolment and exclusions: population of 323,349. Follow‐up colonoscopy for 12,113 (out of 16,037) FIT positives. However, CRC results only reported for group consisting of 16,037 participants Number analysed: 319,424 Identification of interval cancers: colorectal adenocarcinomas and disease stage were obtained from the KPNC and KPSC cancer registries Follow‐up time: interval cancers after first round defined as CRC diagnosed within one year after FIT result |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Juul 2018.
| Study characteristics | |||
| Patient Sampling |
Design: historical population‐based cohort study Setting: 1st round of population screening in Denmark |
||
| Patient characteristics and setting |
Population: participants aged 50 to 74 years, 46.3% male Country: Denmark Time period: 1 March 2014 to 31 December 2014 |
||
| Index tests |
Index test: quantitative FIT Brand: unclear Method of collection: unclear Execution: unclear Positivity threshold: 100 µg Hb/L faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy (or alternatively CT‐colonography) Performed by: not specified % that underwent colonoscopy: 91.7% of positive participants (14,862/16,206) |
||
| Flow and timing |
Enrolment and exclusions: inhabitants of Denmark. Exclusions: not listed with general practice n = 4714; inactive civil registration number n = 49; individuals who died < 1 month after invitation to screening n = 417; individuals who lived outside Denmark n = 404; individuals with known gastrointestinal disease n = 8770. 245,299 of 376,198 individuals completed the test (65.2%) with 16,206 positive tests (6.6%) Number analysed: 244,015 Identification of interval cancers: Danish colorectal Cancer Screening Database (DCCSD) Definition of interval cancers: all the cancers diagnosed from day of invitation until one year following the screening invitation Follow‐up time: 12 months |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Kapidzic 2017.
| Study characteristics | |||
| Patient Sampling |
Design: prospective study Setting: population‐based screening pilot. Two randomly selected groups were invited for two rounds of either 1‐sample (n = 5007) or 2‐sample (n = 3197) FIT screening. |
||
| Patient characteristics and setting |
Population: asymptomatic participants aged 50 to 74 years old (n = 3197). 50% male. 1875 participated Country: the Netherlands Time period: 2006 to 2010 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: per round, participants received one or two identical FITs (OC‐Sensor, Eiken, Japan) to sample on one versus two consecutive bowel movements. Execution: automated analysis using OC‐Sensor Micro Positivity threshold: participants with a haemoglobin (Hb) level ≥ 10 μg Hb/g faeces in at least one test were referred for colonoscopy |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists Percentage that underwent colonoscopy: 94.1% |
||
| Flow and timing |
Enrolment and exclusions: 1875 participated (61.3%). 13 had unsuccessful colonoscopy Number analysed: 1862 Identification of interval cancers: linkage with the Dutch comprehensive Cancer Registry (unpublished data) Follow‐up time: at least 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Khalid‐de Bakker 2011.
| Study characteristics | |||
| Patient Sampling | Design: prospective single centre study Setting: employees of Maastricht University Medical Center were invited to participate | ||
| Patient characteristics and setting |
Population: employees of medical centre, aged 50 to 65 years, mean age 54.6 years, 39% male Country: the Netherlands Time period: not specified |
||
| Index tests |
Index test: iFOBT Brand: OC‐Sensor Method of collection: scrape different parts of stool from 1 bowel movement Execution: automated analysis Positivity threshold: 50 ng/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy: Performed by: four experienced endoscopists % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 1090 were invited, 447 participated, 329 underwent both tests Number analysed in this review: 329 |
||
| Comparative | |||
| Notes | No CRC; only advanced adenomas were found | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Kim 2017.
| Study characteristics | |||
| Patient Sampling |
Design: cross‐sectional study Setting: asymptomatic male participants in a comprehensive health screening program at Kangbuk Samsung Hospital |
||
| Patient characteristics and setting |
Population: asymptomatic male participants in a comprehensive health screening program, 100% male, mean age 41 years Country: South Korea Time period: 2010 to 2014 |
||
| Index tests |
Index test: qualitative FIT Brand: OC‐Sensor Method of collection: by participant from one stool, 3 days before colonoscopy Execution: automated analysis by OC‐Sensor‐Diana Positivity threshold: 20 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: 100% Definition of advanced neoplasia: adenoma with > 10 mm diameter, tubulovillous or villous structure, or high‐grade dysplasia or CRC |
||
| Flow and timing |
Enrolment and exclusions: 21,646 participated; 2013 were excluded; after colonoscopy, 1793 were excluded due to poor bowel preparation or lack of an adequate biopsy; furthermore, 603 were excluded due to age < 30 years. Number analysed: 17,237 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Unclear | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Kronborg 1987.
| Study characteristics | |||
| Patient Sampling |
Design: randomised controlled trial Setting: population‐based screening trial, random sample from central person register, national patient file was used to exclude people with known CRC, colorectal adenoma or distant spread from all types of cancer. |
||
| Patient characteristics and setting |
Population: average‐risk population 45 to 74 years; mean age and male‐female ratio not specified Country: Denmark Time period: August 1985 to September 1986 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult‐II Execution: no rehydration, two technicians developed all slides Method of collection: without dietary restrictions Positivity threshold: if one or more slides were positive |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: 84% of positives |
||
| Flow and timing |
Enrolment and exclusions: screening was offered to 30,767 persons and 20,695 performed the test. All participants with known CRC, colorectal adenomas, or distant spread of all types of malignant disease were excluded before randomisation, which was possible using the public registers in Denmark. Number analysed: 20,666 Identification of interval cancers: via national patient file, health office of the country, and all surgeons were asked to report cancers and adenomas to the screening centre. Definition of interval cancers: detected after a negative FOBT Follow‐up time: not specified (at least 11 months) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Launoy 2005.
| Study characteristics | |||
| Patient Sampling |
Design: prospective screening study Setting: 164 general practitioners invited patients to participate at the end of their regular consultations. |
||
| Patient characteristics and setting |
Population: people visiting general practitioner, 50 to 74 years old, 43% male Country: France Time period: 2001 to 2002 |
||
| Index tests |
Index test: quantitative FIT Brand: Magstream Method of collection: participants had to obtain 2 faecal samples on 2 different days using two test tubes. Execution: no dietary restrictions Positivity threshold: at least one test 20 ng/mL (67 µg Hb/g faeces) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: 84.3% of positives |
||
| Flow and timing |
Enrolment and exclusions: study population 7421 Number analysed: 7355 Identification of interval cancers: collected by general practitioners, gastroenterologists, and pathologists who were routinely contacted (over a 6‐month period) regarding occurrence, and by the local cancer registry. Definition of interval cancers: CRC detected after a negative test Follow‐up time: at least 12 months |
||
| Comparative | |||
| Notes | For 2x2 table of higher cut‐offs: interval CRCs include cancers not detected with this higher cut‐off point but detected by colonoscopy plus had occurred within the 2 years following the test. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Levi 2011a.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based study Setting: people from 9 primary care clinics were offered FIT or gFOBT according to randomisation by letter of invitation |
||
| Patient characteristics and setting |
Population: average‐risk people aged 50 to 75 years, mean age 61 years, 44% males Country: Israel Time period: not described |
||
| Index tests |
Index test: gFOBT & quantitative FIT (participants were randomised to one of the tests) Brand: Hemoccult Sensa (n = 2266 participants), OC‐Micro (n = 1224 participants) Method of collection: in 3 stool samples, gFOBT (with dietary instructions); FIT 3 samples of 3 stools, no dietary instructions Execution: gFOBT: hydration not described; FIT: automated analysis Positivity threshold: gFOBT if any of the 6 is positive, and FIT cutoff 14 µg Hb/g faeces (70 ng Hb/mL) (highest of 3 tests was used) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: 70% of positives |
||
| Flow and timing |
Enrolment and exclusions: 2266 performed gFOBT. 25 were excluded as they did not undergo colonoscopy Number analysed: 2241 Identification of interval carcinomas: linkage to cancer registry Definition of interval cancers: within 2 years after negative test Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Levi 2011b.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based study Setting: people from 9 primary care clinics were offered FIT or gFOBT according to randomisation by letter of invitation |
||
| Patient characteristics and setting |
Population: average‐risk people aged 50 to 75 years, mean age 61 years, 44% males Country: Israel Time period: not described |
||
| Index tests |
Index test: gFOBT & quantitative FIT (participants were randomised to one of the tests) Brand: Hemoccult Sensa (n = 2266 participants), OC‐Micro (n = 1224 participants) Method of collection: in 3 stool samples, gFOBT (with dietary instructions); FIT 3 samples of 3 stools, no dietary instructions Execution: gFOBT: hydration not described; FIT: automated analysis Positivity threshold: gFOBT if any of the 6 is positive, and FIT cutoff 14 µg Hb/g faeces (70 ng Hb/mL) (highest of 3 tests was used) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: 70% of positives |
||
| Flow and timing |
Enrolment and exclusions: 1224 performed FIT. 45 were excluded as they did not undergo colonoscopy. Number analysed: 1179 Identification of interval carcinomas: linkage to cancer registry Definition of interval cancers: within 2 years after negative test Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | Multiple tests were conducted on the same group of individuals | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Levy 2014a.
| Study characteristics | |||
| Patient Sampling |
Design: cohort study Setting: individuals who were scheduled for a screening, surveillance, or diagnostic colonoscopy at University of Iowa Healthcare, were invited to complete a FIT. Only data on screening colonoscopies used |
||
| Patient characteristics and setting |
Population: individuals aged 40 to 75, mean age 61 years, FIT group 45% male, gFOBT group 43% male. Country: USA Time period: January 2010 and November 2011 |
||
| Index tests |
Index test: qualitative FIT (participants underwent one test) Brand: due to issues with the FIT products, four different FIT manufacturers were used sequentially. ‐ Inverness Clearview ‐ Alere Clearview ‐ Polymedco OC‐Light ‐ Quidel QuickVue Method of collection: one sample prior to colonoscopy Execution: by two study team members according to manufacturer Positivity threshold: ‐ Inverness Clearview: 50 ng/mL; 50 µg/g faeces ‐ Alere Clearview: 50 ng/mL; 6 µg/g faeces ‐ Polymedco OC‐Light: 50 ng/mL; 10 µg/g faeces ‐ Quidel QuickVue: 50 ng/mL; 50 µg/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not specified % that underwent colonoscopy: 100% Definition of advanced neoplasia: CRC plus polyps with villous histology, serrated adenomas, high‐grade dysplasia, or any adenomatous polyp 10 mm or greater in diameter |
||
| Flow and timing |
Enrolment and exclusions: 2336 invited, 1140 consented, 1026 completed colonoscopy and FIT with valid result, n = 621 were screening participants. N = 217 with Polymedco OC‐Light. Exclusion criteria: having familial polyposis syndromes, ulcerative colitis, or Crohn’s disease, or active rectal bleeding. Number analysed for this review: 621. N = 217 with Polymedco OC‐Light |
||
| Comparative | |||
| Notes | Data of screening participants received from authors Multiple tests were conducted on the same group of individuals |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Levy 2014b.
| Study characteristics | |||
| Patient Sampling |
Design: cohort study Setting: individuals who were scheduled for a screening, surveillance, or diagnostic colonoscopy at University of Iowa Healthcare, were invited to complete a FIT. Only data on screening colonoscopies used |
||
| Patient characteristics and setting |
Population: individuals aged 40 to 75, mean age 61 years, FIT group 45% male, gFOBT group 43% male Country: USA Time period: January 2010 and November 2011 |
||
| Index tests |
Index test: qualitative FIT (participants underwent one test) Brand: due to issues with the FIT products, four different FIT manufacturers were used sequentially: ‐ Inverness Clearview ‐ Alere Clearview ‐ Polymedco OC‐Light ‐ Quidel QuickVue Method of collection: one sample prior to colonoscopy Execution: by two study team members according to manufacturer Positivity threshold: ‐ Inverness Clearview: 50 ng/mL; 50 µg/g faeces ‐ Alere Clearview: 50 ng/mL; 6 µg/g faeces ‐ Polymedco OC‐Light: 50 ng/mL; 10 µg/g faeces ‐ Quidel QuickVue: 50 ng/mL; 50 µg/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not specified % that underwent colonoscopy: 100% Definition of advanced neoplasia: CRC plus polyps with villous histology, serrated adenomas, high‐grade dysplasia, or any adenomatous polyp 10 mm or greater in diameter |
||
| Flow and timing |
Enrolment and exclusions: 2336 invited, 1140 consented, 1026 completed colonoscopy and FIT with valid result, n = 621 were screening participants. N = 44 with Inverness Clearview. Exclusion criteria: having familial polyposis syndromes, ulcerative colitis, or Crohn’s disease, or active rectal bleeding. Number analysed for this review: 621. N = 44 with Inverness Clearview |
||
| Comparative | |||
| Notes | Data of screening participants received from authors Multiple tests were conducted on the same group of individuals |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Levy 2014c.
| Study characteristics | |||
| Patient Sampling |
Design: cohort study Setting: individuals who were scheduled for a screening, surveillance, or diagnostic colonoscopy at University of Iowa Healthcare, were invited to complete a FIT. Only data on screening colonoscopies used |
||
| Patient characteristics and setting |
Population: individuals aged 40 to 75, mean age 61 years, FIT group 45% male, gFOBT group 43% male. Country: USA Time period: January 2010 and November 2011 |
||
| Index tests |
Index test: qualitative FIT (participants underwent one test) Brand: due to issues with the FIT products, four different FIT manufacturers were used sequentially: ‐ Inverness Clearview ‐ Alere Clearview ‐ Polymedco OC‐Light ‐ Quidel QuickVue Method of collection: one sample prior to colonoscopy Execution: by two study team members according to manufacturer Positivity threshold: ‐ Inverness Clearview: 50 ng/mL; 50 µg/g faeces ‐ Alere Clearview: 50 ng/mL; 6 µg/g faeces ‐ Polymedco OC‐Light: 50 ng/mL; 10 µg/g faeces ‐ Quidel QuickVue: 50 ng/mL; 50 µg/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not specified % that underwent colonoscopy: 100% Definition of advanced neoplasia: CRC plus polyps with villous histology, serrated adenomas, high‐grade dysplasia, or any adenomatous polyp 10 mm or greater in diameter |
||
| Flow and timing |
Enrolment and exclusions: 2336 invited, 1140 consented, 1026 completed colonoscopy and FIT with valid result, n = 621 were screening patients. N = 308 with Alere Clearview. Exclusion criteria: having familial polyposis syndromes, ulcerative colitis, or Crohn’s disease, or active rectal bleeding. Number analysed for this review: 621. N = 308 with Alere Clearview |
||
| Comparative | |||
| Notes | Data of screening participants received from authors Multiple tests were conducted on the same group of individuals |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Levy 2014d.
| Study characteristics | |||
| Patient Sampling |
Design: cohort study Setting: individuals who were scheduled for a screening, surveillance, or diagnostic colonoscopy at University of Iowa Healthcare, were invited to complete a FIT. Only data on screening colonoscopies used |
||
| Patient characteristics and setting |
Population: individuals aged 40 to 75, mean age 61 years, FIT group 45% male, gFOBT group 43% male Country: USA Time period: January 2010 and November 2011 |
||
| Index tests |
Index test: qualitative FIT (participants underwent one test) Brand: due to issues with the FIT products, four different FIT manufacturers were used sequentially: ‐ Inverness Clearview ‐ Alere Clearview ‐ Polymedco OC‐Light ‐ Quidel QuickVue Method of collection: one sample prior to colonoscopy Execution: by two study team members according to manufacturer Positivity threshold: ‐ Inverness Clearview: 50 ng/mL; 50 µg/g faeces ‐ Alere Clearview: 50 ng/mL; 6 µg/g faeces ‐ Polymedco OC‐Light: 50 ng/mL; 10 µg/g faeces ‐ Quidel QuickVue: 50ng/mL; 50 µg/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not specified % that underwent colonoscopy: 100% Definition of advanced neoplasia: CRC plus polyps with villous histology, serrated adenomas, high‐grade dysplasia, or any adenomatous polyp 10 mm or greater in diameter |
||
| Flow and timing |
Enrolment and exclusions: 2336 invited, 1140 consented, 1026 completed colonoscopy and FIT with valid result, n = 621 were screening patients. N = 52 with Quidel Quickview. Exclusion criteria: having familial polyposis syndromes, ulcerative colitis, or Crohn’s disease, or active rectal bleeding. Number analysed for this review: 621. N = 52 with Quidel Quickview |
||
| Comparative | |||
| Notes | Data of screening participants received from authors Multiple tests were conducted on the same group of individuals |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Liebermann 2001.
| Study characteristics | |||
| Patient Sampling | Design: retrospective analysis of prospective studySetting: average‐risk participants recruited from 13 Veterans' Affairs medical centres | ||
| Patient characteristics and setting |
Population: participants from 13 Veterans' Affairs medical centres, mean age 63 years, 97% male, 14% had a first‐degree relative with CRC Country: USA Time period: February 1994 to January 1997 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult II Execution: rehydrated and analysed by trained nurses Method of collection: 2 stool samples on consecutive days Positivity threshold: 1 out of 3 |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: the study investigators, who were selected because of their extensive experience with colonoscopy % that underwent colonoscopy: 92.4 Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 3196 invited, 2885 returned the FOBT and underwent a complete colonoscopic examination Number analysed in this review: 2885 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
McNamara 2014.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based Tallaght Hospital‐Trinity College Colorectal Cancer screening programme Setting: participants aged 50 to 75 years were obtained from local participating general practitioners and invited by mail |
||
| Patient characteristics and setting |
Population: population aged 50 to 75 years, 46% male Country: Ireland Time period: not described |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: 2‐day 2 sample collection, at home Execution: automated analysis Positivity threshold: 100 ng Hb/mL, at least 1 positive test |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: experienced colonoscopists % that underwent colonoscopy: 87% (of positives) |
||
| Flow and timing |
Enrolment and exclusions: 9863 were invited in the first round, 5063 participated. For 419 of 514 positives, colonoscopy results were available. Number analysed: 4968 Identification of interval cancers: not described Definition of interval cancers: number of cancers that occurred following a negative screening episode in the interval before the next invitation Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Nakama 1996.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cohort study Setting: screening study on 3365 residents of regions within Nagano, Japan |
||
| Patient characteristics and setting |
Population: mainly asymptomatic, first‐time screenees. 40 years and older. Mean age not mentioned, 48.6% male Country: Japan Time period: 1991 |
||
| Index tests |
Index test: qualitative FIT Brand: Monohaem (Nihon Pharmaceutical, Japan) Execution: non‐automated Method of collection: thin faecal smear on paper Positivity threshold: unknown |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: not specified % that underwent colonoscopy: not specified |
||
| Flow and timing |
Enrolment and exclusions: 3982 invited; 3365 participated. People who had already been screened were excluded. Number analysed: 3365 Identification of interval cancers: via cancer registry Definition of interval cancers: CRC diagnosed within one, two, or three years of a negative FIT Follow‐up time: 3 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Nakama 2000.
| Study characteristics | |||
| Patient Sampling | Design: retrospective analysisSetting: people participating in a medical check‐up as recommended by the companies with which they were employed | ||
| Patient characteristics and setting |
Population: asymptomatic individuals aged 40 to 60 years (age and gender not described) Country: Japan Time period: not described |
||
| Index tests |
Index test: iFOBT (qualitative) Brand: Iatro Hemcheck Execution: process described but not clear if manual or automated Method of collection: faecal smears were collected at the laboratory and tested immediately, 4 samples of 2 consecutive days' stool Positivity threshold: no agglutination within 1.5 minutes |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: not described Definition of advanced neoplasia: not described (only CRC described) |
||
| Flow and timing |
Enrolment and exclusions: poorly described Number analysed in this review: 17,664 |
||
| Comparative | |||
| Notes | Methods are very limited, not clear what period, exclusion criteria, or uptake. No useful data for AN, data for CRC is entered in RevMan | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Unclear | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Nakazato 2006.
| Study characteristics | |||
| Patient Sampling | Design: cross‐sectional analysisSetting: asymptomatic adults | ||
| Patient characteristics and setting |
Population: asymptomatic individuals in a medical checkup. Age and gender not described Country: Japan Time period: July 1998 to July 2002 |
||
| Index tests |
Index test: iFOBT (qualitative) Brand: OC‐Hemodia Execution: two days before colonoscopy from two bowel samples before start of bowel preparation Method of collection: not described Positivity threshold: 16 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: not described Definition of advanced neoplasia: not described |
||
| Flow and timing |
Enrolment and exclusions: a large proportion underwent iFOBT only (80%) and were excluded. A large part underwent sigmoidoscopy only. Number analysed in this review: 7797 |
||
| Comparative | |||
| Notes | Test brand and threshold are not described in the article. These data were retrieved from the systematic review by Imperiale 2019. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Omata 2011.
| Study characteristics | |||
| Patient Sampling |
Design: retrospective analysis of cross‐sectional study Setting: consecutive participants who completed both full colonoscopy and FIT in a general health checkup clinic |
||
| Patient characteristics and setting |
Population: asymptomatic individuals participating in health checkup, mean age 64 years, 70% males. Included participants with increased risk, such as those with a history of colorectal neoplasia and family history of CRC in first‐degree relatives Country: Japan Time period: 1 May 2004 to 30 June 2008 |
||
| Index tests |
Index test: iFOBT (quantitative) Brand: OC‐Micro Execution: automated analysis Method of collection: most likely one stool sample (not described) Positivity threshold: for AA 25 ng/mL was chosen, for CRC 50 ng/mL was chosen |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: unclear % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 3194 invited, 2153 underwent colonoscopy. 973 were excluded because of previous colonoscopy, 11 because of incomplete colonoscopy, 84 because FIT results were unavailable. 1085 participants analysed. Number analysed in this review: 1085 |
||
| Comparative | |||
| Notes | Added data for CRC from calculated numbers, not real numbers. In manuscript, a total of 77 as well as 71 advanced neoplasia mentioned; 77 used. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | No | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Unclear | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Paimela 2010.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based screening program Setting: individuals were randomised in biennial screening or control groups in participating municipalities in Finland |
||
| Patient characteristics and setting |
Population: people aged 60 to 64 years, 49.5% male invitees, 44% male participants Country: Finland Time period: September 2004 to 2006 |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult Method of collection: 3 stool samples Execution: no rehydration Positivity threshold: not described; most likely according to manufacturer at least 1 positive |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: consultant gastroenterologists and GPs % that underwent colonoscopy: 90% of positives |
||
| Flow and timing |
Enrolment and exclusions: 52,998 invited; 37,514 participants; 81 of 806 positives did not undergo colonoscopy. Number analysed in this review: 37,433 Identification of interval carcinomas: linkage to Finnish Cancer registry Definition of interval cancers: CRC after negative test Follow‐up time: (mean) 23 months |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Parente 2013.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cohort study Setting: population‐based CRC screening program |
||
| Patient characteristics and setting |
Population: asymptomatic men and women 50 to 69 years old; participants 48.4% male Country: Italy, Lecco region Time period: 2005 |
||
| Index tests |
Index test: quantitative FIT Brand: HM‐Jack Execution: single laboratory without rehydration, using an automated reading technique Method of collection: one day FIT without dietary restriction Positivity threshold: 100 ng/mL (250 µg Hb/g faeces) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: expert endoscopist with > 10 years and > 4000 examinations experience % that underwent colonoscopy: 92% of positives |
||
| Flow and timing |
Enrolment and exclusions: residents identified using a Regional Health Service database and mailed letter of invitation to order/pickup test Number analysed: 38,353 Identification of interval cancers: via Lecco cancer screening centre database Definition of interval cancers: CRC detected in database within 2 years of negative test Follow‐up time: at least 2 years |
||
| Comparative | |||
| Notes | Missing variables were retrieved from Parente, 2009 | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Park 2010.
| Study characteristics | |||
| Patient Sampling | Design: prospective studySetting: participants from 4 centres undergoing screening colonoscopy | ||
| Patient characteristics and setting |
Population: asymptomatic individuals, aged 50 to 75 years, mean age 59 years, 51% male Country: South Korea Time period: December 2007 to November 2008 |
||
| Index tests |
Index test: quantitative FIT and gFOBT (participants underwent both tests) Brand: OC‐Sensa micro and Hemoccult II Method of collection: collection of FOBT 1 week before colonoscopy. 3 daily consecutive bowel movements, samples were stored at 4 degrees for 2 weeks Execution: gFOBT by trained staff and iFOBT by automated analysis Positivity threshold: FIT 100 ng/mL (20 µg Hb/g faeces) and 50 ng/mL (10 µg Hb/g faeces) and gFOBT any blue colouring |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: endoscopists % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: 1020 invited, 891 agreed to participate, 770 completed study Number analysed in this review: 770 for FIT, 760 for gFOBT |
||
| Comparative | |||
| Notes | Differing numbers of participants (770 for FIT, 760 FOR gFOBT) not explained | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Parra‐Blanco 2010.
| Study characteristics | |||
| Patient Sampling |
Design: prospective study Setting: random selection of inhabitants of Tenerife who received 2 FOBTs |
||
| Patient characteristics and setting |
Population: random sample of 2288 asymptomatic people aged 50 to 79 years, 34% males Country: Spain (Tenerife) Time period: January to August 2004 |
||
| Index tests |
Index test: gFOBT and qualitative FIT (participants underwent both tests) Brand: Hemofec and OC‐Light Method of collection: diet restrictions. gFOBT: three cards, 3 stools; and FIT: 1 stool. FIT taken from last stool of which gFOBT was taken Execution: gFOBT non‐hydrated; FIT automated analysis Positivity threshold: gFOBT positivity not described. For FIT, cut‐off 50 ng Hb/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: 4 experienced staff endoscopists % that underwent colonoscopy: FOBT positive: 93.7% and FOBT negative: 16.2% |
||
| Flow and timing |
Enrolment and exclusions: 1756 returned both FOBTs, FIT was correctly prepared in 1716, gFOBT in 1689. 143/143 FIT‐positives underwent colonoscopy versus 43/62 gFOBT‐positives. All were followed up 2 years later either with colonoscopy or by telephone in case of refusing colonoscopy (both FOBT‐positives and FOBT‐negatives were invited for colonoscopy). Number analysed: 3386 Identification of interval carcinomas: all participants with a negative FOBT or who refused colonoscopy were contacted by phone Definition of interval cancers: CRC after negative FOBT or who refused colonoscopy (for this review only after a negative test was used) Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Paszat 2016.
| Study characteristics | |||
| Patient Sampling |
Design: cohort study Setting: ColonCancer Check (CCC) is a provincial colorectal screening program managed by Cancer Care Ontario. Participants are offered biennial guaiac faecal occult blood testing. This study focuses on those invited between 1 April 2008 and 31 December 2009 and follows until 30 June 2014. |
||
| Patient characteristics and setting |
Population: people aged 50 to 74 without first‐degree relative with colorectal cancer. Exclusions were those with: billing claim for colonoscopy ≤ 5 years prior, or gFOBT ≤ 2 years prior and those with prior diagnosis of CRC. 45% male. Mean age not described. Country: Canada Time period: 1 April 2008 to 31 December 2009 |
||
| Index tests |
Index test: quantitative gFOBT Brand: Hema‐Screen (Immunostics Inc.) Method of collection: three stool collection cards. Participants were instructed to collect two samples per card, from 3 consecutively passed stools. Participants were advised to not restrict their diets except for eliminating vitamin C supplements and citrus fruits and juices for 3 days prior to and during stool collection; participants were advised to not discontinue taking aspirin (ASA) or nonsteroidal anti‐inflammatory drugs (NSAIDs). Execution: kits were processed at seven community laboratories in Ontario and in accordance with published Cancer Care Ontario gFOBT laboratory standards. Positivity threshold: not specified |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: not specified % that underwent colonoscopy: unknown (after contacting researchers) |
||
| Flow and timing |
Enrolment and exclusions: 307,456 participants participated in screening, with 294,329 participants screen‐negative. Unknown how many gFOBT participants underwent colonoscopic evaluation or other follow‐up examination Number analysed: 307,456 Identification of interval cancers: interval cancers, defined as CRC within two years of a negative result, were identified from the Ontario Cancer Registry (OCR). Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Unclear | ||
| Could the patient flow have introduced bias? | High risk | ||
Ribbing Wilen 2019.
| Study characteristics | |||
| Patient Sampling |
Design: national randomised controlled study (SCREESCO) Setting: population‐based |
||
| Patient characteristics and setting |
Population: people aged 60 years without previous colorectal cancer or a procto‐colectomy. 48% male Country: Sweden Time period: March 2016 to March 2017 |
||
| Index tests |
Index test: iFOBT Brand: OC‐Sensor Method of collection: two samples from two consecutive bowel movements Execution: by the screenee at home Positivity threshold: 10, 20, 40, 60, 80 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: a gastroenterologist, surgeon, or endoscopist nurse with at least 1000 procedures of experience % that underwent colonoscopy: 100% |
||
| Flow and timing |
Enrolment and exclusions: 1155 invited; 806 completed colonoscopy, FIT, and questionnaire Number analysed in this review: 806 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Robinson 1996.
| Study characteristics | |||
| Patient Sampling |
Design: prospectively enrolled population Setting: asymptomatic people aged 50 to 75 years in Brighton and Guildford, UK |
||
| Patient characteristics and setting |
Population: asymptomatic individuals participating. Mean age unknown. 40.4% male Country: England Time period: 1 February 1991 to July 1992 |
||
| Index tests |
Index test: gFOBT (Haemoccult FOBT, qualitative) and iFOBT (Hemeselect, qualitative). Participants underwent both tests Brand: Haemoccult gFOBT and Hemeselect iFOBT Execution: automated analysis Method of collection: Haemoccult group was tested for 3 consecutive days and participants were advised to eat a diet rich in salad, vegetables, and wholemeal bread. Also they were asked to avoid preparations containing vitamin C for 3 days prior to testing. Hemeselect group split for 3 days of testing (analysed at 1:32 fold dilution) or 1 day of testing (analysed at 1:8 fold dilution). Positivity threshold: test at 1:8 dilution for Hemeselect. |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: unclear % that underwent colonoscopy: 9.5% (142 of 1489 participants) |
||
| Flow and timing |
Enrolment and exclusions: 3984 invited; 1489 completed both tests Number analysed in this review: 1489 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Sieg 2002.
| Study characteristics | |||
| Patient Sampling |
Design: screening in four practices in Germany Setting: people older than 44 years who visited the clinic also had a FIT carried out |
||
| Patient characteristics and setting |
Population: people older than 44 years, mean age and male‐female ratio not described. People with abdominal complaints were excluded. Country: Germany Time period: 1994 to 2000 |
||
| Index tests |
Index test: FIT Brand: unknown Execution: Hb determined by luminescence immune assay Method of collection: two samples of one bowel movements, in one 1 mL container Positivity threshold: from 1994 to 1998: 10 g/g stool; from November 1998 to 2000: 5 µg/g stool |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: undefined % that underwent colonoscopy: 84% of positives |
||
| Flow and timing |
Enrolment and exclusions: 5332 participated, 273 positive, 229 colonoscopy Number analysed: 5288 Identification of interval cancers: through diagnosis lists of surrounding hospitals screened on CRC diagnosis and compared with study population Follow‐up time: 1 to 4 years after performing FIT |
||
| Comparative | |||
| Notes | People who visited the clinic, if under 44 years old and they have heard of the study, they were also able to participate. (% < 40 years old not clear; author emailed: says none) | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Siripongpreeda 2016.
| Study characteristics | |||
| Patient Sampling |
Design: prospective cohort study Setting: colonoscopy offered to healthy volunteers |
||
| Patient characteristics and setting |
Population: people between the age of 50 and 60 years with no medical history of colorectal cancer. 30.5% males, mean age 56.9 years Country: Thailand Time period: July 2009 and June 2010 |
||
| Index tests |
Index test: FIT Brand: Abon Biopharm Execution: rapid chromatographic immunoassay Method of collection: self‐collected from one bowel movement before the bowel preparation Positivity threshold: unclear, most likely 6 µg Hb/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: 99.6% Definition of advanced neoplasia: size > 1 cm, > 3 adenomas, tubulovillous or villous adenoma or high‐grade dysplasia, or CRC |
||
| Flow and timing |
Enrolment and exclusions: no exclusions are described Number analysed in this review: 1404 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Sohn 2005.
| Study characteristics | |||
| Patient Sampling |
Design: cohort study Setting: average‐risk screenees admitted to the National Cancer Centre for cancer prevention and detection |
||
| Patient characteristics and setting |
Population: screenees admitted to the National Cancer Centre, no age limits. 57% male. Mean age 48.9 years Country: South Korea Time period: May 2001 to November 2002 |
||
| Index tests |
Index test: FIT Brand: OC‐Hemodia Execution: on the OC‐Sensor analyser Method of collection: self‐collected from one bowel movement before the bowel preparation. No dietary restrictions Positivity threshold: 100 ng/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: not described % that underwent colonoscopy: 100% Definition of advanced neoplasia: high‐grade dysplasia, a 10 mm or greater adenoma, or with at least 25% villous component, or CRC |
||
| Flow and timing |
Enrolment and exclusions: no exclusions are described Number analysed in this review: 3794 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Steele 2009.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based screening Setting: people between 50 and 69 years were sent an FOBT by mail |
||
| Patient characteristics and setting |
Population: asymptomatic people, aged between 50 and 69 years, mean age not described, 49% male participants Country: Scotland Time period: 2000 to 2007 (3 rounds) |
||
| Index tests |
Index test: gFOBT Brand: Hema‐screen Method of collection: 2 samples per stool of 3 stools, no dietary restrictions Execution: rehydration not described. Positivity threshold: if 5 to 6 windows were positive (strong positive), if 1 to 4 windows positive than a further gFOBT with dietary restrictions was requested |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: endoscopists who attended evaluation sessions % that underwent colonoscopy: 85.5% of positives |
||
| Flow and timing |
Enrolment and exclusions: 304,245 invitations, 167,415 participants (55%). 3464 tested positive, 85.5% colonoscopy Number analysed: 166,913 Identification of interval cancers: linkage to Scottish Cancer Registry Follow‐up time: > 2 years |
||
| Comparative | |||
| Notes | Problem: different number of screen‐detected and interval cancers mentioned within and between articles Different number of people who underwent colonoscopy ‐ Emailed authors but no response ‐ Used numbers from 2009 article from table 7 |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Sung 2003.
| Study characteristics | |||
| Patient Sampling | Design: prospective studySetting: individuals were recruited by conducting health exhibitions at public places | ||
| Patient characteristics and setting |
Population: asymptomatic individuals aged older than 50 years, mean age 56 years, 44% male Country: China Time period: not specified |
||
| Index tests |
Index test: gFOBT Brand: Hemoccult II Method of collection: 3 consecutive stool samples collected before start of bowel preparation. Participants returned gFOBT on day of colonoscopy Execution: non‐hydrated Positivity threshold: 1 out of 3 positive |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced endoscopists % that underwent colonoscopy: 94.3 Definition of advanced neoplasia: moderate‐ to severe‐grade dysplasia, 25% or more villous component, adenomas > 1cm, or CRC |
||
| Flow and timing |
Enrolment and exclusions: 510 invited. 476 complete colonoscopy on 1st attempt, but 505 analysed (including 5 barium enema) Number analysed in this review: 505 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Van Roon 2013.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based FIT screening pilot Setting: randomly‐selected people were invited for CRC screening by mail |
||
| Patient characteristics and setting |
Population: average‐risk participants, median age 60 years, 50% male Country: the Netherlands Time period: 2006 to 2009 |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Sensor Method of collection: 1 stool without diet restrictions Execution: automated analysis Positivity threshold: 50 ng Hb/mL (10 µg Hb/g) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy or follow‐up (in case of negative test) Performed by: experienced gastroenterologists % that underwent colonoscopy: 96% of positives |
||
| Flow and timing |
Enrolment and exclusions: 7229 were invited, 4523 participated Number analysed: 4503 Identicification of interval carcinomas: linkage to Dutch Cancer Registration Definition of interval cancers: CRC detected after negative test and before next test Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Yes | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Wong 2014.
| Study characteristics | |||
| Patient Sampling |
Design: population‐based CRC screening Setting: primary care screening centre; participants were recruited via media invitations or referrals by physicians in clinic affiliated with the screening centre |
||
| Patient characteristics and setting |
Population: people aged 50 to 70 years and asymptomatic of CRC, mean age 58 years, 58% male Country: Hong Kong Time period: 2008 to 2012 |
||
| Index tests |
Index test: FIT (qualitative) Brand: Hemosure Method of collection: 1 stool 6 times poking, at home with applicator Execution: within 48 hours of receipt by trained professionals Positivity threshold: 50 ng/mL = 50 µg/g faeces |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: experienced colonoscopists % that underwent colonoscopy: not described (100%?) Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: multiple groups; unclear who went in which group for what reason. 4127 participants underwent both FIT and colonoscopy Number analysed in this review: 4127 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Wu 2014.
| Study characteristics | |||
| Patient Sampling |
Design: retrospective diagnostic cohort study Setting: Health promotion and Evaluation Center of Renai Brach, Taipei City Hospital |
||
| Patient characteristics and setting |
Population: asymptomatic health examinees aged 20 and over (96.8% were > 40 years), mean age 51.6, 58% male Country: Taiwan Time period: January 2010 to June 2011 |
||
| Index tests |
Index test: qualitative FIT Brand: unknown (ACON laboratories, San Diego, USA) Execution: no dietary instructions except for stopping anticoagulant drugs Method of collection: 1 stool sample before colonoscopy Positivity threshold: 50 ng Hb/mL |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy Performed by: specialised gastroenterologists % that underwent colonoscopy: 100% Definition of advanced neoplasia: according to protocol |
||
| Flow and timing |
Enrolment and exclusions: a total of 1007 participants were identified from January 2010 to June 2011. Exclusions are not described. Number analysed: 1007 participants underwent FIT and colonoscopy |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Unclear | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | Unclear | ||
| Did screened persons receive the same reference standard irrespective of index test result? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Zorzi 2018.
| Study characteristics | |||
| Patient Sampling |
Design: retrospective cohort study Setting: cohort of participants in first round of FIT screening in 5 regional programs (Belluno, Feltre, Alto Vicentino, Pieve di Soligo and Bussolengo) within Veneto region in northeastern Italy. |
||
| Patient characteristics and setting |
Population: people aged 50 to 69 and resident in Veneto region. Mean age and % male not given for complete cohort Country: Italy Time period: 2002 to 2015. First round started in 2002 to 2004. |
||
| Index tests |
Index test: quantitative FIT Brand: OC‐Hemodia latex agglutination test (developed with the OC‐Sensor Micro instrument) Method of collection: not specified Execution: automated instruments Positivity threshold: 20 µg Hb/g faeces (100 ng Hb/mL buffer) |
||
| Target condition and reference standard(s) |
Reference test: colonoscopy in case of positive test Performed by: Not specified % that underwent colonoscopy: unknown. Only the number of performed colonoscopies per screening round is mentioned in the manuscript. No information available regarding number of positive tests for each screening round. |
||
| Flow and timing |
Enrolment and exclusions: 123,347 individuals participated in screening. Number of positive tests = 7015 in first screening round. In total, 6419 participants underwent colonoscopy after positive test (91.5%). Number analysed: 6419 Identification of interval cancers: interval cancers, defined as CRC within two years of a negative result, were identified from the GISCoR (Italtian Group for Colorectal Screening), using hospital discharge records documenting possible CRC diagnosis. Follow‐up time: 2 years |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Was the spectrum of invitees representative of CRC screening? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Were non‐interpretable test results reported for the index test? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Were the same clinical data available when test results were interpreted as would be available when test is used in practice? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Were withdrawals from the study explained? | No | ||
| Did screened persons receive the same reference standard irrespective of index test result? | No | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
AA: advanced adenomas; AN: advanced neoplasia; DCBE: double‐contrast barium enema; CT: computed tomography; CRC: colorectal cancer; CT: computed tomography; FIT: faecal immunochemical test; FITTER: Faecal Immunochemical TesTs for haemoglobin Evaluation Reporting; FOBT: faecal occult blood test; gFOBT: guaiac‐based faecal occult blood test; FU; follow‐up; Hb: haemoglobin; IBD: inflammatory bowel disease; IC: interval cancer; NA: not applicable; WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Allison 1996 | Colonoscopy was not the reference standard for all participants. |
| Brenner 2010a | Data are from the same cohort as an already included article. |
| Brenner 2010b | Data are from the same cohort as an already included article. |
| Brenner 2014 | "Reference standard ‐ positive"; without follow‐up. |
| Castiglione 1996 | "Reference standard ‐ positive"; without follow‐up. |
| Castiglione 2000 | "Reference standard ‐ positive"; without follow‐up. |
| Chiu 2015 | Only cumulative mortality was described. |
| Crotta 2004 | "Reference standard ‐ positive"; without follow‐up. |
| Cubiella 2014 | Data are from the same cohort as an already included article. |
| Cummings 1986 | Colonoscopy was not the reference standard for all participants. |
| Dancourt 2008 | "Reference standard ‐ positive"; without follow‐up. |
| Elferink 2018 | Data are from the same cohort as an already included article. |
| Faivre 2012 | Colonoscopy was not the reference standard for all participants. |
| Fraser 2006 | "Reference standard ‐ positive"; without follow‐up. |
| Gies 2018 | Case‐control study. |
| Hardcastle 1996 | Colonoscopy was not the reference standard for all participants. |
| Hoff 2004 | "Reference standard ‐ positive"; without follow‐up. |
| Hol 2010 | "Reference standard ‐ positive"; without follow‐up. |
| Hundt 2009 | Data are from the same cohort as an already included article. |
| Jørgensen 2002 | Only cumulative mortality was described. |
| Ko 2003 | "Reference standard ‐ positive"; without follow‐up. |
| Libby 2018 | Only cumulative mortality was described. |
| Mandel 1993 | Only cumulative mortality was described. |
| Mandel 2000 | Only cumulative mortality was described. |
| Oort 2010 | Participants were not average‐risk. |
| Quintero 2012 | "Reference standard ‐ positive"; without follow‐up. |
| Scholefield 2002 | Only cumulative mortality was described. |
| Steele 2013 | "Reference standard ‐ positive"; without follow‐up. |
| Van Rossum 2008 | "Reference standard ‐ positive"; without follow‐up. |
| Winawer 1980 | Colonoscopy was not the reference standard for all participants. |
| Zorzi 2011 | Only cumulative mortality was described. |
Characteristics of studies awaiting classification [ordered by study ID]
Cheng 2021.
| Patient Sampling | Design: retrospective, single centre |
| Patient characteristics and setting |
Setting: asymptomatic people who received health checkup colonoscopy Characteristics: 1411 cases, 85 with positive FIT and 1326 with negative FIT. Male n = 711 (56.5%) |
| Index tests |
FIT: HM‐JACK (Kyowa Medex Co Ltd, Tokyo, Japan) Threshold: positive result was defined as equal to or more than 20 mg per gram of faeces. |
| Target condition and reference standard(s) |
Target condition: advanced adenoma (AA), defined as adenoma with 25% villous histology, high‐grade dysplasia or larger than 1 cm in size, and advanced colonic neoplasia (AN), defined as advanced adenoma or adenocarcinoma Reference standard: colonoscopy |
| Flow and timing | Participants provided FIT 6 months before colonoscopy |
| Comparative | not applicable |
| Notes |
FIT: faecal immunochemical test; NA: not applicable
Differences between protocol and review
We removed colorectal as a ‘brand name’ from the literature search strategy.
We searched Google Scholar for additional studies. We did not search the MEDION and ARIF reviews databases.
We updated the QUADAS items to QUADAS‐2 (Whiting 2011).
Positive predictive value (PPV), i.e. the proportion of participants with a positive index test result having advanced neoplasia, was not extracted from the included articles.
We investigated fewer sources of heterogeneity due to underreporting of these data in included studies. We planned to investigate the following sources, but did not undertake these analyses:
heterogeneity related to characteristics of the study population apart from gender (i.e. age limits, ethnicity, selection of invitees (identified from general practitioner records or population registers), tumour stage distribution, and tumour location;
heterogeneity related to average‐risk or high‐risk individuals, since only studies that comprised average‐risk individuals were included as per protocol;
heterogeneity related to number of screening rounds since only first‐round "reference type: positive" studies were included for analysis.
In terms of sensitivity analyses, we did not feel it necessary to remove each study, one by one, from the analyses as our review includes such a large number of studies, making it highly unlikely that one particular study would heavily skew the overall pooled estimates. We did remove the studies that had a potentially high risk of bias as assessed by QUADAS‐2.
Contributions of authors
All authors developed the study protocol. MCWS, IL‐V, and EJK obtained funding. AvR, LvD and the Trial Search Coordinator conducted the protocol and literature search strategy. EHS, EJG, WB, and the Trial Search Coordinator conducted the literature search. EHS, EJG, and PHW performed assessment of abstracts, performed the data extraction of identified articles, conducted the analyses and wrote the report. AvR contributed in case of disagreement between EHS and EJG. SB and JD conducted the statistical analyses. MCWS and EJK helped with the design of the study and with interpretation of the results. AGZ and IL‐V, together with all other co‐authors, provided critical revision for important intellectual content.
Sources of support
Internal sources
No sources of support provided
External sources
No sources of support provided
Declarations of interest
EG has no interests to disclose.
PW has no interests to disclose.
ES has no interests to disclose.
AR has no interests to disclose.
LD has no interests to disclose.
AZ has no interests to disclose.
IL was involved in a published overview paper on risk‐based CRC screening in The International Journal of Cancer and participated in The BMJ Rapid Recommendations on CRC screening.
WB has no interests to disclose.
SB has no interests to disclose.
JD has a Cochrane Diagnostic Test Accuracy (DTA) Editorial role but was not involved in the editorial process. JD was involved in published opinions in medical journals, the public press, broadcast, and social media relevant to the interventions in the work: eight podcasts, including Talk Evidence (BMJ), More or Less (Radio 4), Inside Science (Radio 4), and The Newscast (Radio 4); five opinion pieces in The Guardian, UnHerd and The BMJ; and numerous television, radio and mainstream media interviews giving substantial coverage of scientific issues related to test evaluation for COVID‐19. JD presented evidence to the House of Lords Select Committee, and the All Parliamentary Party Investigation on COVID‐19, and wrote two invited editorials on COVID‐19 for The BMJ.
ES received payment for a book: Clinical Prediction Models.
ML has no interests to disclose.
MS has no interests to disclose.
EK has no interests to disclose.
These authors contributed equally to this work.
These authors contributed equally to this work.
New
References
References to studies included in this review
Ahlquist 2008a {published data only}
- Ahlquist DA, Sargent DJ, Loprinzi CL, Levin TR, Rex DK, Ahnen DJ, et al.Stool DNA and occult blood testing for screen detection of colorectal neoplasia. Annals of Internal Medicine 2008;149(7):441-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahlquist 2008b {published data only}
- Ahlquist DA, Sargent DJ, Loprinzi CL, Levin TR, Rex DK, Ahnen DJ, et al.Stool DNA and occult blood testing for screen detection of colorectal neoplasia. Annals of Internal Medicine 2008;149(7):441-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aniwan 2015 {published data only}
- Aniwan S, Rerknimitr R, Kongkam P, Wisedopas N, Ponuthai Y, Chaithongrat S, et al.A combination of clinical risk stratification and fecal immunochemical test results to prioritize colonoscopy screening in asymptomatic participants. Gastrointestinal Endoscopy 2015;81(3):719-27. [DOI] [PubMed] [Google Scholar]
Aniwan 2017 {published data only}
- Aniwan S, Ratanachu Ek T, Pongprasobchai S, Limsrivilai J, Praisontarangkul OA, Pisespongsa P, et al.The optimal cut-off level of the fecal immunochemical test for colorectal cancer screening in a country with limited colonoscopy resources: a multi-center study from Thailand. Asian Pacific Journal of Cancer Prevention 2017;18(2):405-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arana‐Arri 2017a {published and unpublished data}
- Arana-Arri E, Idigoras I, Uranga B, Pérez R, Irurzun A, Gutiérrez-ibarluzea, et al.Population-based colorectal cancer screening programmes using a faecal immunochemical test: should faecal haemoglobin cut-offs differ by age and sex? BMC Cancer 2017;17(1):577. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arana‐Arri 2017b {published data only}
- Arana-Arri E, Idigoras I, Uranga B, Pérez R, Irurzun A, Gutiérrez-ibarluzea, et al.Population-based colorectal cancer screening programmes using a faecal immunochemical test: should faecal haemoglobin cut-offs differ by age and sex? BMC Cancer 2017;17(1):577. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blanks 2019 {published and unpublished data}
- Blanks R, Burón Pust A, Alison R, He E, Barnes I, Patnick J, et al.Screen-detected and interval colorectal cancers in England: associations with lifestyle and other factors in women in a large UK prospective cohort. International Journal of Cancer 2019;145(3):728-34. [DOI: 10.1002/ijc.32168] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouvier 1999 {published data only}
- Bouvier V, Launoy G, Herbert C, Lefevre H, Maurel J, Gignoux M.Colorectal cancer after a negative Haemoccult II test and programme sensitivity after a first round of screening: the experience of the Department of Calvados (France). British Journal of Cancer 1999;81(2):305-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brenner 2012 {published data only}
- Brenner G, Faure H, Heuer S, Reinholz J.Detection of colorectal findings for cancer prevention by immunochemical stool test with different sensitivity levels [Detektion von kolorektalen Befunden zur Darmkrebsprävention mit immunologischem Stuhltest in verschiedenen Empfindlichkeitsstufen]. Zeitschrift fur Gastroenterologie 2012;50(10):1083-8. [DOI] [PubMed] [Google Scholar]
Brenner 2013 {published data only (unpublished sought but not used)}
- Brenner H, Tao S.Superior diagnostic performance of faecal immunochemical tests for haemoglobin in a head-to-head comparison with guaiac based faecal occult blood test among 2235 participants of screening colonoscopy. European Journal of Cancer 2013;49(14):3049-54. [DOI] [PubMed] [Google Scholar]
Brenner 2018 {published data only}
- Brenner H, Qian J, Werner S.Variation of diagnostic performance of fecal immunochemical testing for hemoglobin by sex and age: results from a large screening cohort. Clinical Epidemiology 2018;10:381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burón 2019 {published and unpublished data}
- Burón A, Macià F, Andreu M, Pellisé M, Castells X, Grau J.Population-based colorectal cancer screening: interval cancers and relationship with the quantitative faecal immunological for hemoglobin. Medica Clinica 2019;152(8):303-6. [DOI] [PubMed] [Google Scholar]
Castiglione 2007 {published data only}
- Castiglione G, Visioli CB, Ciatto S, Grazzini G, Bonanomi AG, Rubeca T, et al.Sensitivity of latex agglutination faecal occult blood test in the Florence District population-based colorectal cancer screening programme. British Journal of Cancer 2007;96(11):1750-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2017 {published data only}
- Chang LC, Shun CT, Hsu WF, Tu CH, Tsai PY, Lin BR, et al.Fecal immunochemical test detects sessile serrated adenomas and polyps with a low level of sensitivity. Clinical Gastroenteroly and Hepatology 2017;15(6):872-9. [DOI] [PubMed] [Google Scholar]
Chen 2014 {published data only}
- Chen YY, Chen TH, Su MY, Ning HC, Kuo CJ, Lin WP, et al.Accuracy of immunochemical fecal occult blood test for detecting colorectal neoplasms in individuals undergoing health check-ups. Advances in Digestive Medicine 2014;1:74-9. [Google Scholar]
Chen 2016a {published data only}
- Chen CH, Wen CP, Tsai MK.Fecal immunochemical test for colorectal cancer from a prospective cohort with 513,283 individuals: providing detailed number needed to scope (NNS) before colonoscopy. Medicine 2016;95(36):e4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheng 2002 {published and unpublished data}
- Cheng TI, Wong JM, Hong CF, Cheng SH, Cheng TJ, Shieh MJ, et al.Colorectal cancer screening in asymptomatic adults: comparison of colonoscopy, sigmoidoscopy and fecal occult blood tests. Journal of the Formosan Medical Association 2002;101(10):685-90. [PubMed] [Google Scholar]
Chiang 2014a {published data only}
- Chiang TH, Chuangs SL, Chen SL, Chiu HM, Yen AM, Chiu SY, et al.Difference in performance of fecal immunochemical tests with the same hemoglobin cutoff concentration in a nationwide colorectal cancer screening program. Gastroenterology 2014;147(6):1317-26. [DOI] [PubMed] [Google Scholar]
Chiang 2014b {published data only}
- Chiang TH, Chuangs SL, Chen SL, Chiu HM, Yen AM, Chiu SY, et al.Difference in performance of fecal immunochemical tests with the same hemoglobin cutoff concentration in a nationwide colorectal cancer screening program. Gastroenterology 2014;147(6):1317-26. [DOI] [PubMed] [Google Scholar]
Chiu 2013 {published data only}
- Chiu HM, Lee YC, Tu CH, Chen CC, Tseng PH, Liang JT, et al.Association between early stage colon neoplasms and false-negative results from the fecal immunochemical test. Clinical Gastroenterology and Hepatology 2013;11(7):832-8. [DOI] [PubMed] [Google Scholar]
Chiu 2016a {published data only}
- Chiu HM, Ching JY, Wu KC, Rerknimitr R, Li J, Wu DC, et al.A risk-scoring system combined with a fecal immunochemical test is effective in screening high-risk subjects for early colonoscopy to detect advanced colorectal neoplasms. Gastroenterology 2016;150(3):617-25. [DOI] [PubMed] [Google Scholar]
Crotta 2012 {published data only}
- Crotta S, Segnan N, Paganin S, Dagnes B, Rosset R, Senore C.High rate of advanced adenoma detection in 4 rounds of colorectal cancer screening with the fecal immunochemical test. Clinical Gastroenterology and Hepatology 2012;10(6):633-8. [DOI] [PubMed] [Google Scholar]
Cruz‐Correa 2007 {published data only}
- Cruz-Correa M, Schultz K, Jagannath S, Harris M, Kantsevoy S, Bedine M, et al.Performance characteristics and comparison of two fecal occult blood tests in patients undergoing colonoscopy. Digestive Diseases and Sciences 2007;52(4):1009-13. [DOI] [PubMed] [Google Scholar]
Denters 2012a {published data only}
- Denters MJ, Deutekom M, Bossuyt PM, Stroobants AK, Fockens P, Dekker E.Lower risk of advanced neoplasia among patients with a previous negative result from a fecal test for colorectal cancer. Gastroenterology 2012;142(3):497-504. [DOI] [PubMed] [Google Scholar]
Denters 2012b {published data only}
- Denters MJ, Deutekom M, Bossuyt PM, Stroobants AK, Fockens P, Dekker E.Lower risk of advanced neoplasia among patients with a previous negative result from a fecal test for colorectal cancer. Gastroenterology 2012;142(3):497-504. [DOI] [PubMed] [Google Scholar]
De Wijkerslooth 2012 {published data only}
- De Wijkerslooth TR, Stoop EM, Bossuyt PM, Meijer GA, Van Ballegooijen M, Van Roon AH, et al.Immunochemical fecal occult blood testing is equally sensitive for proximal and distal advanced neoplasia. American Journal of Gastroenterology 2012;107(10):1570-8. [DOI] [PubMed] [Google Scholar]
Digby 2016 {published data only}
- Digby J, Fraser CG, Carey FA, Lang J, Stanners G, Steele RJ.Interval cancers using a quantitative faecal immunochemical test (FIT) for haemoglobin when colonoscopy capacity is limited. Journal of Medical Screening 2016;23(3):130-4. [DOI] [PubMed] [Google Scholar]
Faivre 2004 {published data only}
- Faivre J, Dancourt V, Lejeune C, Tazi MA, Lamour J, Gerard D, et al.Reduction in colorectal cancer mortality by fecal occult blood screening in a French controlled study. Gastroenterology 2004;126(7):1674-80. [DOI] [PubMed] [Google Scholar]
Giai 2014 {published and unpublished data}
- Giai J, Exbrayat C, Boussat B, Poncet F, Bureau du ColombierP, Colonna M, et al.Sensitivity of a colorectal cancer screening program based on a guaiac test: a population-based study. Clinics and Research in Hepatology and Gastroenterology 2014;38(1):106-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Graser 2009 {published data only}
- Graser A, Stieber P, Nagel D, Schäfer C, Horst D, Becker CR, et al.Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut 2009;58(2):241-8. [DOI] [PubMed] [Google Scholar]
Haug 2011 {published data only}
- Haug U, Kuntz KM, Knudsen AB, Hundt S, Brenner H.Sensitivity of immunochemical faecal occult blood testing for detecting left- vs right-sided colorectal neoplasia. British Journal of Cancer 2011;104(11):1779-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hernandez 2014 {published data only}
- Hernandez V, Cubiella J, Gonzalez-Mao MC, Iglesias F, Rivera C, Iglesias MB, et al.Fecal immunochemical test accuracy in average-risk colorectal cancer screening. World Journal of Gastroenterology 2014;20(4):1038-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoepffner 2006 {published data only}
- Hoepffner N, Shastri YM, Hanisch E, Rösch W, Mössners J, Caspary WF, et al.Comparative evaluation of a new bedside faecal occult blood test in a prospective multicentre study. Alimentary Pharmacology and Therapeutics 2006;23(1):145-54. [DOI] [PubMed] [Google Scholar]
Imperiale 2004 {published data only}
- Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME.Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. New England Journal of Medicine 2004;351(26):2704-14. [DOI] [PubMed] [Google Scholar]
Imperiale 2014 {published data only}
- Imperiale TF, Ransohoff DF, Itzkowitz SH, Levin TR, Lavin P, Lidgard GP, et al.Multitarget stool DNA testing for colorectal-cancer screening. New England Journal of Medicine 2014;370(14):1287-97. [DOI] [PubMed] [Google Scholar]
Itoh 1996 {published data only}
- Itoh M, Takahashi K, Nishida H, Sakagami K, Okubo T.Estimation of the optimal cut off point in a new immunological faecal occult blood test in a corporate colorectal cancer screening programme. Journal of Medical Screening 1996;3(2):66-71. [DOI] [PubMed] [Google Scholar]
Jensen 2016 {published and unpublished data}
- Jensen CD, Corley DA, Quinn VP, Doubeni CA, Zauber AG, Lee JK, et al.Fecal immunochemical test program performance over 4 rounds of annual screening: a retrospective cohort study. Annals of Internal Medicine 2016;164(7):456-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Juul 2018 {published data only}
- Juul JS, Andersen B, Laurberg S, Carlsen AH, Olesen F, Vedsted P.Differences in diagnostic activity in general practice and findings for individuals invited to the Danish screening programme for colorectal cancer: a population-based cohort study. Scandinvian Journal of Primary Health Care 2018;36(3):281-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kapidzic 2017 {published data only}
- Kapidzic A, Van Roon AH, Van Leerdam ME, Van Vuuren AJ, Van Ballegooijen M, Lansdorp-Vogelaar I, et al.Attendance and diagnostic yield of repeated two-sample faecal immunochemical test screening for colorectal cancer. Gut 2017;66(1):118-23. [DOI] [PubMed] [Google Scholar]
Khalid‐de Bakker 2011 {published data only}
- Khalid-de Bakker CA, Jonkers DM, Sanduleanu S, Bruïne AP, Meijer GA, Janssen JB, et al.Test performance of immunologic fecal occult blood testing and sigmoidoscopy compared with primary colonoscopy screening for colorectal advanced adenomas. Cancer Prevention Research 2011;4(10):1563-71. [DOI] [PubMed] [Google Scholar]
Kim 2017 {published data only}
- Kim NH, Lee MY, Park JH, Park DI, Sohn CI, Choi K, et al.A combination of fecal immunochemical test results and iron deficiency anemia for detection of advanced colorectal neoplasia in asymptomatic men. Yonsei Medical Journal 2017;58(5):910-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kronborg 1987 {published data only}
- Kronborg O, Fenger C, Søndergaard O, Pedersen KM, Olsen J.Initial mass screening for colorectal cancer with fecal occult blood test. A prospective randomized study at Funen in Denmark. Scandinavion Journal of Gastroenterology 1987;2(6):677-86. [DOI] [PubMed] [Google Scholar]
Launoy 2005 {published data only}
- Launoy GD, Bertrand HJ, Berchi C.Evaluation of an immunochemical fecal occult blood test with automated reading in screening for colorectal cancer in a general average‐risk population. International Journal of Cancer 2005;115(3):493-96. [DOI] [PubMed] [Google Scholar]
Levi 2011a {published data only}
- Levi Z, Birkenfeld S, Vilkin A, Bar-Chana M, Lifshitz I, Chared M, et al.A higher detection rate for colorectal cancer and advanced adenomatous polyp for screening with immunochemical fecal occult blood test than guaiac fecal occult blood test, despite lower compliance rate. A prospective, controlled, feasibility study. International Journal of Cancer 2011;128(10):2415-24. [DOI] [PubMed] [Google Scholar]
Levi 2011b {published data only}
- Levi Z, Birkenfeld S, Vilkin A, Bar-Chana M, Lifshitz I, Chared M, et al.A higher detection rate for colorectal cancer and advanced adenomatous polyp for screening with immunochemical fecal occult blood test than guaiac fecal occult blood test, despite lower compliance rate. A prospective, controlled, feasibility study. International Journal of Cancer 2011;128(10):2415-24. [DOI] [PubMed] [Google Scholar]
Levy 2014a {published and unpublished data}
- Levy BT, Bay C, Xu Y, Daly JM, Bergus G, Dunkelberg J, et al.Test characteristics of faecal immunochemical tests (FIT) compared with optical colonoscopy. Journal of Medical Screening 2015;21(3):133-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2014b {published data only}
- Levy BT, Bay C, Xu Y, Daly JM, Bergus G, Dunkelberg J, et al.Test characteristics of faecal immunochemical tests (FIT) compared with optical colonoscopy. Journal of Medical Screening 2015;21(3):133-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2014c {published data only}
- Levy BT, Bay C, Xu Y, Daly JM, Bergus G, Dunkelberg J, et al.Test characteristics of faecal immunochemical tests (FIT) compared with optical colonoscopy. Journal of Medical Screening 2015;21(3):133-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2014d {published data only}
- Levy BT, Bay C, Xu Y, Daly JM, Bergus G, Dunkelberg J, et al.Test characteristics of faecal immunochemical tests (FIT) compared with optical colonoscopy. Journal of Medical Screening 2015;21(3):133-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liebermann 2001 {published data only}
- Lieberman DA, Harford WV, Ahnen DJ, Provenzale D, Sontag SJ, Schnell TG, et al.One-time screening for colorectal cancer with combined fecal occult-blood testing and examination of the distal colon. New England Journal of Medicine 2001;345(8):555-60. [DOI] [PubMed] [Google Scholar]
McNamara 2014 {published data only}
- McNamara D, Leen R, Seng-Lee C, Shearer N, Crotty P, Neary P, et al.Sustained participation, colonoscopy uptake and adenoma detection rates over two rounds of the Tallaght-Trinity College colorectal cancer screening programme with the faecal immunological test. European Journal of Gastroenterology and Hepatology 2014;26(12):1415-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nakama 1996 {published data only}
- Nakama H, Kamijo N, Abdul Fattah AS, Zhang B.Validity of immunological faecal occult blood screening for colorectal cancer: a follow up study. Journal of Medical Screening 1996;3(2):63-5. [DOI] [PubMed] [Google Scholar]
Nakama 2000 {published data only}
- Nakama H, Zhang B, Fattah AS, Zhang X.Colorectal cancer in iron deficiency anemia with a positive result on immunochemical fecal occult blood. International Journal of Colorectal Disease 2000;15(5-6):271-4. [DOI] [PubMed] [Google Scholar]
Nakazato 2006 {published and unpublished data}
- Nakazato M, Yamano H, Matsushita H, Sato K, Fujita K, Yamanaka Y, et al.Immunologic fecal occult blood test for colorectal cancer screening. Japan Medical Association Journal 2006;49:203-7. [Google Scholar]
Omata 2011 {published data only}
- Omata F, Shintani A, Isozaki M, Masuda K, Fujita Y, Fukui T.Diagnostic performance of quantitative fecal immunochemical test and multivariate prediction model for colorectal neoplasms in asymptomatic individuals. European Journal of Gastroenterology and Hepatology 2011;23(11):1036-41. [DOI] [PubMed] [Google Scholar]
Paimela 2010 {published data only}
- Paimela H, Malila N, Palva T, Hakulinen T, Vertio H, Jarvinen H.Early detection of colorectal cancer with faecal occult blood test screening. British Journal of Surgery 2010;97(10):1567-71. [DOI] [PubMed] [Google Scholar]
Parente 2013 {published data only}
- Parente F, Boemo C, Ardizzoia A, Costa M, Carzaniga P, Ilardo A, et al.Outcomes and cost evaluation of the first two rounds of a colorectal cancer screening program based on immunochemical fecal occult blood test in northern Italy. Endoscopy 2013;45(1):27-34. [DOI] [PubMed] [Google Scholar]
Park 2010 {published data only}
- Park DI, Ryu S, Kim YH, Lee SH, Lee CK, Eun CS, et al.Comparison of guaiac-based and quantitative immunochemical fecal occult blood testing in a population at average risk undergoing colorectal cancer screening. American Journal of Gastroenterology 2010;105(9):2017-25. [DOI] [PubMed] [Google Scholar]
Parra‐Blanco 2010 {published data only}
- Parra-Blanco A, Gimeno-Garcia AZ, Quintero E, Nicolas D, Moreno SG, Jimenez A, et al.Diagnostic accuracy of immunochemical versus guaiac faecal occult blood tests for colorectal cancer screening. Journal of Gastroenterology 2010;45(7):703-12. [DOI] [PubMed] [Google Scholar]
Paszat 2016 {published data only}
- Paszat L, Sutradhar R, Tinmouth J, Baxter N, Rabeneck L.Interval colorectal cancers following guaiac fecal occult blood testing in the Ontario ColonCancerCheck Program. Canadian Journal of Gastroenterology and Hepatology 2016;2016:[6 p.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ribbing Wilen 2019 {published data only}
- Ribbing Wilen H, Blom J, Hoijer J, Andersson G, Lowbeer C, Hultcrantz R.Fecal immunochemical test in cancer screening - colonoscopy outcome in FIT positives and negatives. Scandinavian Journal of Gastroenterology 2019;54(3):303-10. [DOI] [PubMed] [Google Scholar]
Robinson 1996 {published data only}
- Robinson MH, Marks CG, Farrands PA, Bostock K, Hardcastle JD.Screening for colorectal cancer with an immunological faecal occult blood test: 2-year follow-up. British Journal of Surgery 1996;83(4):500-1. [DOI] [PubMed] [Google Scholar]
Sieg 2002 {published data only}
- Sieg A, Wirth A, Luthgens K, Schmidt-Gayk H.Six years of screening for colorectal neoplasms with an immunological fecal occult hemoglobin test. Verdauungskrankheiten 2002;20:114-7. [Google Scholar]
Siripongpreeda 2016 {published data only}
- Siripongpreeda B, Mahidol C, Dusitanond N, Sriprayoon T, Muyphuag B, Sricharunrat T, et al.High prevalence of advanced colorectal neoplasia in the Thai population: a prospective screening colonoscopy of 1,404 cases. BMC Gastroenterology 2016;16:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sohn 2005 {published data only}
- Sohn DK, Jeong SY, Choi HS, Lim SB, Huh JM, Kim DH, et al.Single immunochemical fecal occult blood test for detection of colorectal neoplasia. Cancer Research and Treatment 2005;37(1):20-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steele 2009 {published data only}
- Steele RJ, McClements PL, Libby G, Black R, Morton C, Birrell J, et al.Results from the first three rounds of the Scottish demonstration pilot of FOBT screening for colorectal cancer. Gut 2009;58(4):530-5. [DOI] [PubMed] [Google Scholar]
Sung 2003 {published data only}
- Sung JJ, Chan FK, Leung WK, Wu JC, Lau JY, Ching J, et al.Screening for colorectal cancer in Chinese: comparison of fecal occult blood test, flexible sigmoidoscopy, and colonoscopy. Gastroenterology 2003;124(3):608-14. [DOI] [PubMed] [Google Scholar]
Van Roon 2013 {published data only}
- Van Roon AH, Goede SL, Van Ballegooijen M, Van Vuuren AJ, Looman CW, Biermann K, et al.Random comparison of repeated faecal immunochemical testing at different intervals for population-based colorectal cancer screening. Gut 2013;62(3):409-15. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wong 2014 {published data only}
- Wong MC, Ching JY, Chan VC, Shum JP, Lam TY, Luk AK, et al.Should prior FIT results be incorporated as an additional variable to estimate risk of colorectal neoplasia? A prospective study of 5,813 screening colonoscopies. PloS One 2014;9(12):e114332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2014 {published data only}
- Wu T, Kuo K, Wu Y, Lin K.Diagnostic accuracy of a single qualitative immunochemical fecal occult blood test coupled with physical measurements. Chinese Medical Journal 2014;127(24):4164-70. [PubMed] [Google Scholar]
Zorzi 2018 {published and unpublished data}
- Zorzi M, Hassan C, Capodaglio G, Narne E, Turrin A, Baracco M, et al.Divergent long-term detection rates of proximal and distal advanced neoplasia in fecal immunochemical test screening programs: a retrospective cohort study. Annals of Internal Medicine 2018;169(9):602-9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Allison 1996 {published data only}
Brenner 2010a {published data only}
- Brenner G, Faure H, Reinholz J.Comparison of the guaiac-based test (g-FOBT) and the immunochemical test (i-FOBT) with the results of the screening colonoscopy in an asymptomatic population. Verdauungskrankheiten 2010;28.
Brenner 2010b {published data only}
Brenner 2014 {published data only}
Castiglione 1996 {published data only}
- Castiglione G, Zappa M, Grazzini G, Mazzotta A, Biagini M, Salvadori P, et al.Immunochemical vs guaiac faecal occult blood tests in a population-based screening programme for colorectal cancer. British Journal of Cancer 1996;74(1):141-4. [DOI] [PMC free article] [PubMed]
Castiglione 2000 {published data only}
Chiu 2015 {published data only}
- Chiu HM, Chen SL, Yen AM, Chiu SY, Fann JC, Lee YC, et al.Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program. Cancer 2015;121(18):3221-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crotta 2004 {published data only}
Cubiella 2014 {published data only}
- Cubiella J, Castro I, Hernandez V, Gonzalez-Mao C, Rivera C, Iglesias F, et al.Diagnostic accuracy of fecal immunochemical test in average- and familial-risk colorectal cancer screening. United European Gastroenterology Journal 2014;2(6):522-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cummings 1986 {published data only}
- Cummings KM, Michalek A, Tidings J, Herrera L, Mettlin C.Results of a public screening program for colorectal cancer. New York State Journal of Medicine 1986;86(2):68-72. [PubMed]
Dancourt 2008 {published data only}
Elferink 2018 {published data only}
- Elferink MA, Toes-Zoutendijk E, Vink GR, Lansdorp-Vogelaar I, Meijer GA, Dekker E, et al.National population screening for colorectal carcinoma in the Netherlands: results of the first years since the implementation in 2014. Nederlands Tijdschrift voor Geneeskunde 2018;162:D2283. [PubMed] [Google Scholar]
Faivre 2012 {published data only}
Fraser 2006 {published data only}
Gies 2018 {published data only}
- Gies A, Cuk K, Schrotz-King, Brenner H.Direct comparison of diagnostic performance of 9 quantitative fecal immunochemical tests for colorectal cancer screening. Gastroenterology 2018;154(1):93-104. [DOI] [PubMed] [Google Scholar]
Hardcastle 1996 {published data only}
Hoff 2004 {published data only}
- Hoff G, Grotmol T, Thiis-Evensen E, Bretthauer M, Gondal G, Vatn MH.Testing for faecal calprotectin (PhiCal) in the Norwegian Colorectal Cancer Prevention trial on flexible sigmoidoscopy screening: comparison with an immunochemical test for occult blood (FlexSure OBT). Gut 2004;53(9):1329-33. [DOI] [PMC free article] [PubMed]
Hol 2010 {published data only}
Hundt 2009 {published data only}
Jørgensen 2002 {published data only}
- Jørgensen OD, Kronborg O, Fenger C.A randomised study of screening for colorectal cancer using faecal occult blood testing: results after 13 years and seven biennial screening rounds. Gut 2002;50(1):29-32. [DOI] [PMC free article] [PubMed]
Ko 2003 {published data only}
Libby 2018 {published data only}
- Libby G, Fraser CG, Carey FA, Brewster DH, Steele RJ.Occult blood in faeces is associated with all-cause and non-colorectal cancer mortality. Gut 2018;67(12):2116-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mandel 1993 {published data only}
- Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al.Reducing mortality from colorectal cancer by screening for fecal occult blood. New England Journal of Medicine 1993;328(19):1365-71. [DOI] [PubMed] [Google Scholar]
Mandel 2000 {published data only}
Oort 2010 {published data only}
- Oort FA, Terhaar Sive Droste JS, Van der Hulst RW, Van Heukelem HA, Loffeld RJ, Wesdorp IC, et al.Colonoscopy-controlled intra-individual comparisons to screen relevant neoplasia: faecal immunochemical test vs. guaiac-based faecal occult blood test. Alimentary Pharmacology and Therapeutics 2010;31(3):432-9. [DOI] [PubMed]
Quintero 2012 {published data only}
Scholefield 2002 {published data only}
- Scholefield JH, Moss S, Sufi F, Mangham CM, Hardcastle JD.Effect of faecal occult blood screening on mortality from colorectal cancer: results from a randomised controlled trial. Gut 2002;50(6):840-4. [DOI] [PMC free article] [PubMed]
Steele 2013 {published data only}
- Steele RJ, McDonald PJ, Digby J, Brownlee L, Strachan JA, Libby G, et al.Clinical outcomes using a faecal immunochemical test for haemoglobin as a first-line test in a national programme constrained by colonoscopy capacity. United European Gastroenterology Journal 2013;1(3):198-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Rossum 2008 {published data only}
Winawer 1980 {published data only}
Zorzi 2011 {published data only}
References to studies awaiting assessment
Cheng 2021 {published data only}
- Cheng WC, Chen PJ, Kang JW, Chen WY, Sheu BS.Age, male sex, smoking and metabolic syndrome as risk factors of advanced colorectal neoplasia for fecal immunochemical test negative patients. Journal of the Formosan Medical Association 2021;S0929-6646(21)00240-0.:Online ahead of print.. [DOI] [PubMed] [Google Scholar]
Additional references
Andermann 2008
- Andermann A, Blancquaert I, Beauchamp S, Dery V.Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bulletin of World Health Organization 2008;86:317-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bramer 2016
- Bramer WM, Giustini D, Jonge GB, Holland L, Bekhuis T.De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association : JMLA 2016;104(3):240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buscemi 2006
- Buscemi N, Hartling L, Vandermeer B, Tjosvold L, Klassen TP.Single data extraction generated more errors than double data extraction in systematic reviews. Journal of Clinical Epidemiology 59;7:697-703. [DOI] [PubMed] [Google Scholar]
Carethers 2015
- Carethers JM, Jung BH.Genetics and genetic biomarkers in sporadic colorectal cancer. Gastroenterology 2015;149(5):1177-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ciatto 2007
- Ciatto S, Martinelli F, Castiglione G, Mantellini P, Rubeca T, Grazzini G, et al.Association of FOBT-assessed faecal Hb content with colonic lesions detected in the Florence screening programme. British Journal of Cancer 2007;96:218-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2005
- Deeks JJ, Macaskill P, Irwig L.The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. Journal of Clinical Epidemiology 2005;58:882-93. [DOI] [PubMed] [Google Scholar]
Deeks 2013
- Deeks JJ, Bossuyt PM, Gatsonis C (editors).Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy, Version 1.0.0. The Cochrane Collaboration, 2013. Available from srdta.cochrane.org.
Doust 2005
- Doust JA, Pietrzak E, Sanders S, Glasziou PP.Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. Journal of Clinical Epidemiology 2005;58(5):444-9. [DOI] [PubMed] [Google Scholar]
Edwards 2005
- Edwards JB.Screening for colorectal cancer using faecal blood testing: varying the positive cut-off value. Pathology 2005;37:565-8. [DOI] [PubMed] [Google Scholar]
EndNote 2015 [Computer program]
- EndNote.Version X7. Thomson Reuters, 2015.
Fairfield 2017
- Fairfield CJ, Harrison EM, Wigmore SJ.Duplicate publication bias weakens the validity of meta-analysis of immunosuppression after transplantation. World Journal of Gastroenterology 2017;23(39):7198-7200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fraser 2012
- Fraser CG, Allison JE, Halloran SP, Young GP, Expert Working Group on Fecal Immunochemical Tests for Hemoglobin, Colorectal Cancer Screening Committee, World Endoscopy Organization.A proposal to standardize reporting units for fecal immunochemical tests for hemoglobin. Journal of the National Cancer Institute 2012;104(11):810-4. [DOI] [PubMed] [Google Scholar]
Freitas 2013
- Freitas BR, Nagasako CK, Pavan CR, Lorena SL, Guerrazzi F, Coy CS, et al.Immunochemical fecal occult blood test for detection of advanced colonic adenomas and colorectal cancer: comparison with colonoscopy results. Gastroenterology Research and Practice 2013;2013:[6 p.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hewitson 2008
- Hewitson P, Glasziou P, Watson E, Towler B, Irwig L.Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (Hemoccult): an update. Americal Journal of Gastroenterology 2008;103(6):1541-9. [DOI] [PubMed] [Google Scholar]
Hol 2009
- Hol L, Wilschut JA, Van Ballegooijen M, Van Vuuren AJ, Van der Valk H, Reijerink JC, et al.Screening for colorectal cancer: random comparison of guaiac and immunochemical faecal occult blood testing at different cut-off levels. British Journal of Cancer 2009;100(7):1103-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Imperiale 2019
- Imperiale TF, Gruber RN, Stump TE, Emmett TW, Monahan PO.Performance characteristics of fecal immunochemical tests for colorectal cancer and advanced adenomatous polyps: a systematic review and meta-analysis. Annals of Internal Medicine 2019;170(5):319-29. [DOI] [PubMed] [Google Scholar]
Johnson 2013
- Johnson CM, Wei C, Ensor JE, Smolenski DJ, Amos CI, Levin B, et al.Meta-analyses of colorectal risk factors. Cancer Causes Control 2013;24(6):1207-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Konrad 2010
- Konrad G.Dietary interventions for fecal occult blood test screening: systematic review of the literature. Canadian Family Physician 2010;56(3):229-38. [PMC free article] [PubMed] [Google Scholar]
Kronborg 1996
- Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O.Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet 1996;348:1467-71. [DOI] [PubMed] [Google Scholar]
Kuipers 2013
- Kuipers EJ, Rösch T, Bretthauer M.Colorectal cancer screening--optimizing current strategies and new directions. Nature Reviews Clinical Oncology 2013;10(3):130-42. [DOI] [PubMed] [Google Scholar]
Lansdorp‐Vogelaar 2012
- Lansdorp-Vogelaar I, Karsa L, International Agency for Research on Cancer.European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition--Introduction. Endoscopy 2012;44(Suppl 3):SE15-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Launois 2014
- Launois R, Le Moine JG, Uzzan B, Fiestas Navarrete LI, Benamouzig R.Systematic review and bivariate/HSROC random-effect meta-analysis of immunochemical and guaiac-based fecal occult blood tests for colorectal cancer screening. European Journal of Gastroenterology and Hepatology 2014;9:978-89. [DOI] [PubMed] [Google Scholar]
Lee 2014
- Lee JK, Liles EG, Bent S, Levin TR, Corley DA.Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Annals of Internal Medicine 2014;160(3):171-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leeflang 2008
- Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM.Systematic reviews of diagnostic test accuracy. Annals of Internal Medicine 2008;149:889-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leeflang 2009
- Leeflang MM, Bossuyt PM, Irwig L.Diagnostic test accuracy may vary with prevalence: implications for evidence-based diagnosis. Journal of Clinical Epidemiology 2009;62(1):5-12. [DOI] [PubMed] [Google Scholar]
Levi 2007
- Levi Z, Rozen P, Hazazi R, Vilkin A, Waked A, Maoz E, et al.A quantitative immunochemical fecal occult blood test for colorectal neoplasia. Annals of Internal Medicine 2007;146:244-55. [DOI] [PubMed] [Google Scholar]
Lindholm 2008
- Lindholm E, Brevinge H, Haglind E.Survival benefit in a randomized clinical trial of faecal occult blood screening for colorectal cancer. British Journal of Surgery 2008;95(8):1029-36. [DOI] [PubMed] [Google Scholar]
Macaskill 2013
- Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y.Chapter 10: Analysing and presenting results. In: Deeks JJ, Bossuyt PM, Gatsonis C (editors). Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy, Version 1.0.0. The Cochrane Collaboration, 2013. Available from srdta.cochrane.org.
Naaktgeboren 2016
- Naaktgeboren CA, Groot JA, Rutjes AW, Bossuyt PM, Reitsma JB, Moons KG.Anticipating missing reference standard data when planning diagnostic accuracy studies. BMJ 2016;352:i402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nieuwenburg 2019
- Nieuwenburg SA, Vuik FE, Kruip MJ, Kuipers EJ, Spaander MC.Effect of anticoagulants and NSAIDs on accuracy of faecal immunochemical tests (FITs) in colorectal cancer screening: a systematic review and meta-analysis. Gut 2019;68(5):866-72. [DOI] [PubMed] [Google Scholar]
Reitsma 2005
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH.Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. Journal of Clinical Epidemiology 2005;58:982‐90. [DOI] [PubMed] [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5).Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Rockey 1999
- Rockey D.Occult gastrointestinal bleeding. New England Journal of Medicine 1999;341:38-46. [DOI] [PubMed] [Google Scholar]
Rozen 2006
- Rozen P, Waked A, Vilkin A, Levi Z, Niv Y.Evaluation of a desk top instrument for the automated development and immunochemical quantification of fecal occult blood. Medical Science Monitor 2006;12:MT27-32. [PubMed] [Google Scholar]
Rutter 2001
- Rutter CM, Gatsonis CA.A hierarchical regression approach to meta‐analysis of diagnostic test accuracy evaluations. Statistics in Medicine 2001;20:2865‐2884. [DOI] [PubMed] [Google Scholar]
Sanduleanu 2014
- Sanduleanu S, le Clercq CM, Dekker E, Meijer GA, Rabeneck L, Rutter MD, et al.Definition and taxonomy of interval colorectal cancers: a proposal for standardising nomenclature. Gut 2015;64(8):1257-67. [DOI] [PubMed] [Google Scholar]
Schreuders 2015
- Schreuders EH, Ruco A, Rabeneck L, Schoen SE, Sung JJ, Young GP, et al.Colorectal cancer screening: a global overview of existing programmes. Gut 2015;64(10):1637-49. [DOI] [PubMed] [Google Scholar]
Shaukat 2013
- Shaukat A, Mongin SJ, Geisser MS, Lederle FA, Bond JH, Mandel JS, et al.Long-term mortality after screening for colorectal cancer. New England Journal of Medicine 2013;369(13):1106-14. [DOI] [PubMed] [Google Scholar]
Sinatra 1999
- Sinatra MA, St John DJ, Young GP.Interference of plant peroxidases with guaiac-based fecal occult blood tests is avoidable. Clinical Chemistry 1999;45(1):123-6. [PubMed] [Google Scholar]
Song 2002
- Song F, Khan KS, Dinnes J, Sutton AJ.Asymmetric funnel plots and publication bias in meta-analyses of diagnostic accuracy. International Journal of Epidemiology 2002;31:88-95. [DOI] [PubMed] [Google Scholar]
Spada 2014
- Spada C, Barbaro F, Andrisani G, Minelli Grazioli L, Hassan C, Costamagna I, et al.Colon capsule endoscopy: what we know and what we would like to know. World Journal of Gastroenterology 2014;20(45):16948-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stata [Computer program]
- Stata.Version 16. College Station, TX, USA: StataCorp, 2019. Available at www.stata.com.
Takwoingi 2013
- Takwoingi Y, Leeflang MM, Deeks JJ.Empirical evidence of the importance of comparative studies of diagnostic test accuracy. Annals of Internal Medicine 2013;158(7):544-54. [DOI] [PubMed] [Google Scholar]
Tinmouth 2015
- Tinmouth J, Lansdorp-Vogelaar I, Allison JE.Faecal immunochemical tests versus guaiac faecal occult blood tests: what clinicians and colorectal cancer screening programme organisers need to know. Gut 2015;64(8):1327-37. [DOI] [PubMed] [Google Scholar]
Van Doorn 2015
Van Houwelingen 2002
- Van Houwelingen HC, Arends LR, Stijnen T.Advanced methods in meta-analysis: multivariate approach and meta-regression. Statistics in Medicine 2002;21(4):589-624. [DOI] [PubMed] [Google Scholar]
Van Rijn 2006
- Van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, Van Deventer SJ, Dekker E.Polyp miss rate determined by tandem colonoscopy: a systematic review. American Journal of Gastroenterology 2006;101:343-50. [DOI] [PubMed] [Google Scholar]
Whiting 2003
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J.The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Medical Research Methodology 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al, QUADAS-2 Group.QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529-36. [DOI: 10.7326/0003-4819-155-8-201110180-00009] [DOI] [PubMed] [Google Scholar]
Wieten 2019
- Wieten E, Schreuders EH, Grobbee EJ, Nieboer D, Bramer WM, Lansdorp-Vogelaar I, et al.Incidence of faecal occult blood test interval cancers in population-based colorectal cancer screening: a systematic review and meta-analysis. Gut 2019;68(5):873-81. [DOI] [PubMed] [Google Scholar]
Wieten 2020
- Wieten E, Klerk CM, Lansdorp-Vogelaar I, Bossuyt PM, Dekker E, Spaander MC.A quarter of participants with advanced neoplasia have discordant results from 2-sample fecal immunochemical tests for colorectal cancer screening. Clinical Gastroenterology and Hepatology 2020;18(8):1805-11. [DOI] [PubMed] [Google Scholar]
Wilschut 2011
- Wilschut JA, Habbema JD, Van Leerdam ME, Hol L, Lansdorp-Vogelaar I, Kuipers EJ, et al.Fecal occult blood testing when colonoscopy capacity is limited. Journal of the National Cancer Institute 2011;103(23):1741-51. [DOI] [PubMed] [Google Scholar]
Wilson 1968
- Wilson JM, Jungner YG.Principles and practice of mass screening for disease. Public Health Papers 34 1968;65:281-393. [PubMed] [Google Scholar]
Winawer 1993
- Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, et al.Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. New England Journal of Medicine 1993;329:1977-81. [DOI] [PubMed] [Google Scholar]
Winawer 1997
- Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD, et al.Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 1997;112:594-642. [DOI] [PubMed] [Google Scholar]
Young 2002
- Young GP, St John DJ, Winawer SJ, Rozen P.Choice of fecal occult blood tests for colorectal cancer screening: recommendations based on performance characteristics in population studies: a WHO (World Health Organization) and OMED (World Organization for Digestive Endoscopy) report. American Journal of Gastroenterology 2002;97:2499-507. [DOI] [PubMed] [Google Scholar]
Young 2009
- Young GP.Population-based screening for colorectal cancer: Australian research and implementation. Journal of Gastroenterology and Hepatology 2009;24 Suppl 3:S33-42. [DOI] [PubMed] [Google Scholar]
Young 2015
- Young GP, Symonds EL, Allison JE, Cole SR, Fraser CG, Halloran SP.Advances in fecal occult blood tests: the FIT revolution. Digestive Diseases and Sciences 2015;60(3):609-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zauber 2012
- Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, Van Ballegooijen M, Hankey BF, et al.Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. New England Journal of Medicine 2012;366(8):687-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zorzi 2015
- Zorzi M, Fedeli U, Schievano E, Bovo E, Guzzinati S, Baracco S, et al.Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut 2015;64(5):784-90. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Grobbee 2016
- Grobbee EJ.From FIT to Future [PhD thesis]. Rotterdam (NL): Erasmus University Rotterdam, 2016. [Google Scholar]
Schreuders 2016
- Schreuders EH.Optimizing Colorectal Cancer Screening [PhD thesis]. Rotterdam (NL): Erasmus University Rotterdam, 2016. [Google Scholar]
Van Roon 2011
- Van Roon AH, Wilschut JA, Hol L, Van Ballegooijen M, Reijerink JC, 't Mannetje H, et al.Diagnostic yield improves with collection of 2 samples in fecal immunochemical test screening without affecting attendance. Clinical Journal of Gastroenterology and Hepatology 2011;9(4):333-9. [DOI] [PubMed] [Google Scholar]


