Abstract
Background
Nursing home staff have been adversely impacted throughout the COVID-19 pandemic, facing difficulties in providing patient care. The aim of this study was to explore health workers’ perception regarding their own care quality experience in nursing homes during the COVID-19 pandemic. Amidst the second wave of the pandemic, we investigated the relationships between fear of COVID-19 and care quality experiences in nursing homes with emotional exhaustion (EE) as a mediating role. We hypothesized that EE is associated with fear of COVID-19 and care quality experience among nursing home staff. Furthermore, we predicted that EE would mediate the relationships between fear of COVID-19 and care quality experience.
Methods
During the second wave of COVID-19 (October to December 2020), we administered surveys to a large sample of 129 French nursing home staff with a mean age of 38.47 ± 10.31 who were directly and repeatedly exposed to COVID-19. We assessed their emotional exhaustion (EE) and care quality experience in the workplace via subjective indicators using self-reported scales.
Results
In the context of COVID-19, low to severe emotional exhaustion levels were found among nursing home staff, and these levels were associated with care quality experience as well as fear of COVID-19. The groups with low and severe levels of EE reported the highest levels of fear of COVID-19. The groups with moderate and severe levels of EE reported the lowest levels of care quality experience. Lastly, the relationships between fear of COVID-19 and care quality experience were mediated by EE.
Conclusions
The findings made by the present study focused on the role of emotional coping responses to COVID-19. EE was associated positively with fear of COVID-19 and negatively with care quality experience. Furthermore, EE was found to mediate the relationship between fear of COVID-19 and care quality experience. We discuss these findings as they relate to palliative care issues in nursing homes and the manner in which emotional exhaustion ought to be addressed among nursing home staff.
Keywords: COVID-19, Care quality perception, Emotional exhaustion, Workplace, Nursing homes
1. Introduction
The outbreak of a global COVID-19 pandemic was declared in March 2020 (World Health Organization, 2020). Europe, and France in particular were severely impacted, counting more than two million infections and two hundred thousand deaths (Santé Publique France, 2020). The airborne SARS-CoV-2 virus produces a highly contagious infection in the general population. Dirst identified in late 2019 that SARS-CoV-2 causes in certain infected individuals a severe acute respiratory syndrome (SARS) which requires treatment in an intensive care unit, and that the virus is associated with an increased risk of infection and mortality compared to other airborne viruses (Horobet, et al., 2020). Due to its contagiousness, SARS-CoV-2 is associated with an omnipresent risk of becoming infected and contaminating others during one's daily activities, a factor which has wrought major mental health impacts on the general population. The main negative consequences of the virus include depression, anxiety, fear of COVID-19, trouble sleeping, obsession with COVID-19, and exhaustion (Di Blasi et al., 2021; Vindegaard, & Benros, 2020).
However, not everyone is equally affected by the virus; older people and health workers were particularly exposed and vulnerable to it. Nursing homes have been particularly afflicted (Mo & Shi, 2020), drastically more so than the rest of the population (El Haj et al., 2020; Pitkälä, 2020). Nursing homes are mostly peopled by vulnerable older people whose living conditions were greatly shaken up. Residents were isolated in their rooms, including during mealtime. All non-essential daily activities were durably put on hold (e.g., group activities, cognitive stimulation, family visits). The working conditions of health workers have been similarly upended by the risk of being contaminated by the virus and contaminating the older people they serve, curbing social interaction. The persistence of the pandemic over time appears to have had major impacts on the mental health of nursing home residents (e.g., depression, anxiety, trouble sleeping, loneliness) (Mo & Shi, 2020).
During the pandemic, nursing home staff cared around the clock for older people in long-term care, with major psychological consequences on residents. In addition, health workers suffered from a fear of COVID-19 related to the risk of being contaminated and contaminating residents, rampant COVID-19 case numbers, and related deaths (Fallon et al., 2020; Mo & Shi, 2020). The upheaval of working conditions in nursing homes is likely to have impacted well-being and mental health. Several studies have shown increased levels of depression, anxiety, and stress among health workers (Lai et al., 2020; Preti et al., 2020; Spoorthy, et al., 2020; Stuijfzand et al., 2020). Emotional exhaustion (EE) is defined as a psychological dimension characterized by a feeling of fatigue, emotional drain, and being overwhelmed (Maslach et al., 2001). EE can have an impact on care quality, a lesser-explored topic in the literature due notably to the difficulty in defining and measuring it. In nursing homes, care quality could be described as caregivers’ attitudes and behaviors in care practice towards residents (Mert Boga et al., 2020). In a recent literature review, Cleland et al. (2021) identified nine key themes characterizing care quality experience (e.g., skills and training of care staff, relationships between residents and care staff, supporting residents in making informed choices, etc.) and reported on care quality using clinical indicators.
Care quality experience can be derived from indicators obtained from residents, but also from structural and organizational indicators (e.g., staffing, available resources, leadership, etc.), objective indicators (e.g., communication and collaboration, teamwork, care hours per day, etc.), as well as subjective indicators such as work environment characteristics (e.g., relationships, values, etc.) (Thomas et al., 2019; Ryan et al., 2017; Oh et al., 2016; Burhans & Alliggod, 2010; Bayer & Baykal, 2018). Eltaybani et al. (2021) used objective indicators of care quality in long-term care units (e.g., rate of patients with pneumonia, patients with pressure ulcers, patients with urinary catheter, and patients on tube feeding). These authors reported nurse burnout and especially the EE burnout subscale to be pivotal determinants in care quality (Eltaybani et al., 2021). In the present study, we focused rather on subjective indicators.
Consequently, we focused in nursing homes on EE, care quality experience with subjective indicators, and fear of COVID-19 using self-reported assessment. Subjective indicators are self-assessments of overall lived perception of experience; they report the individual and personal viewpoints regularly employed in the social and psychological sciences. During the second pandemic wave, we studied EE and its relevant impacts on staff perceptions of their own care quality: care quality experience. Several studies have considered emotional exhaustion as the pivotal factor in health workers’ mental health during COVID-19. Similarly, high levels of EE were found in nurses exposed to COVID-19 over a lengthy period (Zhang et al., 2020). The prevalence of EE was found to be as high as 31.9%, and was higher in health workers exposed to COVID-19. According to Hwang et al. (2020), high levels of EE have had negative impacts during the pandemic across a variety of sectors (e.g., tourism, hotels, airlines, restaurants, and hospitals).
During the second pandemic wave, work environments were upended. In line with the recent literature on care quality in a COVID-19 context, we hypothesized that there are significant relationships between EE, care quality experience and fear of COVID-19, in particular, that the relationship between fear of COVID-19 and care quality experience is mediated by EE. In other words, fear of COVID-19 contributes to higher EE levels, in turn decreasing care quality perception.
2. Method
2.1. Study sample and procedure
A sample of 129 native French-speaking health workers was recruited from four nursing homes in France. Those health workers eligible to participate in the survey included physicians, psychologists, physiotherapists, dieticians, psychometricians, nurses, healthcare aides and nursing assistants. All health workers reported possession of a certificate or its equivalent validated by the French Health Ministry. All participants worked in a nursing home and were exposed directly and repeatedly to older people with COVID-19.
Following the consent of each nursing home, the recruitment process was carried out in compliance with the ethical principles of the Declaration of Helsinki and the agreement of the medical and administration authorities of the Hospital (Centre Hospitalier Gustave Dron, Tourcoing, France). The survey, taking the form of a paper questionnaire, was run during the second wave of COVID-19 (October to December 2020). Regular health workers (e.g., physicians, nurses, health officers or nursing assistants) were asked to fill out the questionnaire in their workplace. The respondent participation rate was 44%. All participants declared direct and multiple exposure to elderly people with COVID-19 during France's second coronavirus wave.
All individuals from the four nursing homes who gave their consent were invited to participate in the study. Questionnaires were made available to each staff member. A reminder was issued a month after the first distribution of the questionnaire. After being informed about the aims of the study and signing the free consent, all volunteers individually and anonymously completed the survey. Two questionnaires with missing data were not included in the study. No financial compensation was given. A reminder was made two weeks afterwards. The time needed to complete the questionnaire was between 15 and 20 min.
2.2. Measures
Socio-demographic variables. Socio-demographic data were collected including age, gender, occupational category (i.e., physicians, nurses, health officers and healthcare workers belonging to others professions), seniority, and working pattern (i.e., full-time or part-time).
Emotional Exhaustion. The Emotional Exhaustion (EE) subscale of the Maslach Burnout Inventory (MBI) was used to assess the level of EE in health workers (Maslach et al., 1986). The MBI was translated and validated in French by Dion & Tessier (1994) in a sample of nurses. This subscale was composed of a 9-item self-report measure (e.g., “I feel emotionally exhausted because of my work”) which assessed the frequency of EE symptoms using a 7-point Likert scale from 0 (“never”) to 6 (“everyday”). The higher the total score, the higher the level of EE. Cut-off scores for EE were proposed in nurses by Dion & Tessier (1994): a score below 18 indicates a low level of EE, a score between 19 and 27 indicates a moderate level of EE and a score over 28 indicates a severe level of EE. In our sample, the internal consistency for the scale was α= .90.
Care quality experience. Care quality experience was assessed with the Care Quality Perception Scale (CQPS) [“Grille d'autocontrôle de mes pratiques Professionnelles”], designed by the French National Authority for Health (HAS), an entity set up by the French government to improve the quality of patient care. The HAS organizes and assesses France's healthcare system. It developed the Care Quality Perception Scale (HAS, 2012), composed of 32-items (e.g., “I do not perform care because of lack of time”, “I have an infantilizing, humiliating attitude.”) and consists of a unidimensional self-report measure of care behaviors and attitudes held within a healthcare team and or an institution. A 5-point Likert-type scale (1= Always, 2= Often, 3= Sometimes, 4= Rarely, 5= never) was used to collect responses. The higher the total score, the greater the level of perception of care quality. The caregiver may also indicate “non-concerned” (0= non-concerned) when the caregiver cannot comment because the situation described is not encountered in their workplace or not correspond to their job. The number of responded items can vary from 12 to 32. For this reason, the use of scores proportioned to the number responded items for the CQPS is better adapted. To adjust for missing values, the use of an adjusted total score based on the number responded items for the CQPS is more suitable. In our sample, the internal consistency for the scale was α= .89.
Fear of COVID-19. Respondents’ level of fear of COVID-19 was assessed with the fear of COVID-19 scale (Ahorsu et al., 2020), a self-report measure of fear of COVID-19 composed of 7 items (e.g., “I am most afraid of coronavirus”) using a 5-point Likert scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). A total score is calculated by adding the scores of the 7 items (ranging from 7 to 35). As the score increases, so does the level of the fear of COVID-19. In our sample, the internal consistency for the scale was α= .89. This scale was translated and validated in French by Mailliez et al. (2020) with 316 French participants from the general population.
2.3. Statistical analysis
The data set was analyzed with JAMOVI® software version 1.6.18.00 (The Jamovi project, 2021). The statistical analyses were set to test the hypothesis in four steps. First, descriptive analyses were conducted on the whole sample. Second, correlation matrix was conducted. Third, the different groups of EE levels were determined using cut-off scores (Dion & Tessier, 1994). Fourth, χ2 test was conducted on the categorical variables, and Kruskal-Wallis non-parametric one-way analysis of variance was conducted for comparison of the three EE groups’ (Low EE, Moderate EE, Severe EE) care quality experience levels. Study data were not normally distributed (e.g., EE, fear of COVID-19, Care quality experience). For significant differences, the Dwass-Steel-Critchlow-Flinger post-hoc analysis method was applied for pairwise comparisons. Finally, mediational analysis with the GLM mediation model in the JAMM module (JAMOVI) was conducted to test mediational sequence with EE as a mediator in relationships between fear of COVID-19 and care quality experience.
3. Results
Means, standard deviations, median, Skewness, Kurtosis and Shapiro-Wilk for all study variables were reported in Table 1 . The sample included 107 females and 24 males with a mean age of 38.66 ± 10.34 years and a mean seniority of 14.53 ± 8.51. One hundred and eight of them had a full-time job and twenty-three worked part-time. All workers had been directly exposed to COVID-19 in nursing homes. Correlations among the study variables were reported in Table 2 . No significant correlation was found between age and the other study variables: EE, Fear of COVID-19 and Care quality perception. Significant correlations were found between EE and Fear of COVID-19 (r= .19, p= .30), and between EE and Care quality perception (r= -.36, p < .001). No significant correlation was found between Care quality perception and Fear of COVID-19 (Table 2).
Table 1.
Characteristics of 129 health workers and normality test
| All sample (n = 129) | ||||||
|---|---|---|---|---|---|---|
| mean (or percentage) (SD) | Median | Skewness | Kurtosis | Shapiro-Wilk | p value | |
| Age | 38.47 (10.31) | 34 | .334 | -1.19 | .930 | .001 |
| Gender (female) | .82 (.38) | 1 | -1.701 | .907 | - | - |
| Seniority in position | 14.41 (8.50) | 13 | .268 | -1.008 | .950 | .001 |
| Working pattern (full-time) | .83 (.38) | 1 | -1.773 | 1.160 | - | - |
| Emotional Exhaustion | 22.03 (12.90) | 19 | .359 | -.658 | .972 | .008 |
| Fear of COVID | 14.09 (6.14) | 13 | .702 | -.262 | .921 | .001 |
| Care quality perception | 104 (16.52) | 105,6 | -2.051 | 7.347 | .845 | .001 |
Gender (Female: 1, Male: 0), Working pattern (Full-time:1, part-time:0)
Gender and Working pattern are in %
Table 2.
Correlation matrix for age, EE, Fear of the COVID-19 and Care quality perception.
| n = 129 | Age | Emotional exhaustion | Fear of COVID-19 |
|---|---|---|---|
| Age | — | ||
| Emotional Exhaustion | -.03 (p= .778) | — | |
| Fear of COVID-19 | .06 (p= .470) | .19 (p= .030) | — |
| Care quality perception | .04 (p= .638) | -.36 (p< .001) | -.013 (p= .885) |
We classified our sample into three groups: 1- “Lower EE” group, 2- “Moderate EE” group and 3- “Severe EE” group using the cut-off scores of Dion & Tessier (1994). The results indicated that fifty-eight participants (44.96%) belonged to the lower EE group, twenty-nine (22.48%) to moderate EE, and the forty-two (32.56%) to the severe EE group (Table 3 ).
Table 3.
Characteristics of 129 health workers and comparison of three EE groups with the Kruskal-Wallis test.
| Low EE (n = 58) | Moderate EE (n = 29) | Severe EE (n = 42) | p-value | |
|---|---|---|---|---|
| (between groups) | ||||
| mean (or percentage) (SD) | mean (or percentage) (SD) | mean (or percentage) (SD) | ||
| Age | 38.66 (10.31) | 37.79 (10.56) | 38.69 (10.35) | .816 |
| Gender (female) | .76 (.43) | .93 (.26) | .83 (.38) | .137 (χ2) |
| Seniority in position | 13.09 (7.87) | 16.17 (8.76) | 15.02 (9.05) | .332 |
| Working pattern (full-time) | .81 (.39) | .82 (.38) | .86 (.35) | .828 (χ2) |
| Emotional Exhaustion | 10.60 a (5.45) | 22.66 b (3.15) | 37.38 c (6.68) | .001 |
| Fear of COVID | 14.12 a (5.46) | 11.55 b (4.50) | 15.81 c (7.40) | .039 |
| Care quality perception | 111.20 a (11.63) | 97.53 b (21.88) | 98.46 b (14.26) | .001 |
Note. n= 129. p < .05 using χ2 (gender, working pattern) or Kruskal-Wallis (age, emotional exhaustion, fear of COVID, care quality perception).
Gender (Female: 1, Male: 0), Working pattern (Fulltime:1, part-time:0) Gender and Working pattern are in % For each variable, means with different subscripts indicate a significant difference at p < .05 using χ2 or Kruskal-Wallis with Dwass-Steel-Crichtlow-Fligner post-hoc pairwise test.
Fear of COVID-19 (p = .039) was significantly different between the three EE groups (Table 3). Post-hoc pairwise comparison analysis for fear of COVID-19 reported that the low and severe EE groups rated higher than the moderate EE group. The severe EE group reported higher fear of COVID-19 than the low EE group (Table 3).
Care quality perception (p < .001) was significantly different between the three EE groups (Table 3). Post-hoc pairwise comparison analysis of care quality experience found that moderate and severe EE groups reported lower level of care quality experience than the low EE group. No difference was found between the moderate and severe EE groups (Table 3). In addition, no significant difference was found for age, gender, seniority, and working pattern between the three EE groups (Table 3).
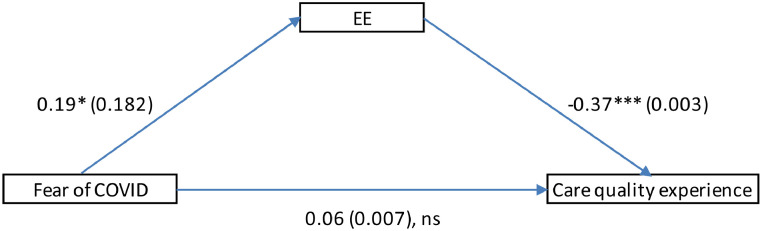
Mediation analysis supported the mediational role of EE in the relationships between fear of COVID-19 and care quality experience. Consistent with the mediational analyses reported in Fig. 1 , the indirect effect of fear of COVID-19 on care quality experience via EE (B= -0,07, S.E.= 0.003, 95% CI= [-0.383; -0.003]) was significant (p = 0.047). In addition, the direct effect of fear of COVID-19 on care quality experience was not significant (Fig. 1). In sum, the effect of fear of COVID-19 was completely mediated by EE (Rucker et al., 2011).
Fig. 1.
Mediating effects of EE between fear of COVID and care quality experience.
4. Discussion
Nursing homes staff were composed mostly of young females working full-time with moderate seniority (average 14 years). During the COVID-19 pandemic, more than half (55.04 %) of the nursing home healthcare workers in our sample reported moderate to severe emotional exhaustion.
Two points are worth noting regarding nursing home staff. First, EE is regularly found in said population, caused by the multitude of physical and psychological stress factors encountered in the workplace (Manzano Garcia & Ayala Calvo, 2012). In the literature, high prevalence of EE was reported, ranging from 22.1 and 68.6% (Dhaini et al., 2016; Tanaka et al., 2015; Costello et al., 2019). Second, EE was reported in the literature as the short-term consequence of repeated exposure to workplace stress factors (González-Gil et al., 2021). Our results were therefore concordant with the previous literature's findings concerning EE in nursing home staff.
In addition, EE was clearly related with fear of COVID-19 and care quality perception (Table 3). In fact, a significant, high level of fear of COVID-19 was found in the group with severe EE. Participants with higher risk of EE reported a higher level of fear of COVID-19, while significantly lower levels of care quality perception were found in two groups: severe and moderate level of EE. The relationships between EE and fear of COVID-19, and EE and care quality perception were not linear. The relationships between EE, fear of COVID-19 and care quality perception appear to be dynamic and more complex.
In order to focus on care quality perception through the prism of the emotional exhaustion of nursing home staff, we determined the impact of fear of COVID-19 and EE level on care quality perception in the workplace using a mediational hypothesis. First, a high level of EE was associated with the highest level of fear of COVID-19, and the lowest level of care quality perception in nursing home staff. Moderate level of EE was associated with the lowest level of fear of COVID-19 and the highest level of care quality perception. Second, fear of COVID-19, EE and care quality perception in nursing homes were associated in a mediational sequence. EE was reported as a mediator in relationships between fear of COVID-19 and care quality perception. In other words, fear of COVID-19 contributes to increased EE levels, in turn decreasing care quality perception. In agreement with Eltaybani et al. (2021), we found EE to be a pivotal factor in care quality experience in nursing homes.
The original contribution of our work was to highlight, during the second wave of COVID-19 in France, the relationships between fear of COVID-19, EE and care quality experience among staff in nursing homes, shining a light on the mediation role of EE. Our finding also reveals the pertinence of subjective or self-reported indicators reported by care staff in assessing workplace context, particularly in assessing care quality experience.
According to the literature, the context brought on by the COVID-19 pandemic contributed to an increase of EE in workplace (Zhang et al., 2020; Giusti et al., 2020). Many negative consequences related to COVID-19 were reported, as the atmosphere created by the pandemic caused considerable psychological and physical disorders such as increased depression, anxiety, insomnia or distress, stress, and emotional exhaustion (Lai et al., 2020; Preti et al., 2020; Spoorthy et al., 2020; Stuijfzand et al., 2020; Özdemir & Kerse, 2020; Hwang et al., 2020). EE is indeed regularly found to be present in nursing homes due to lack of time and inadequate human and material resources (Dhaini et al., 2016, Tanaka et al., 2015, Costello et al., 2019, White et al., 2019).
Our original contribution with this study was to highlight the care quality perception as reflected by EE in nursing home staff. A significant number of healthcare workers had a moderate or severe EE level, prompting a significant decrease in care quality perception during the second wave of COVID-19. The context underlying the pandemic (e.g., fear of COVID-19) increased usual EE levels and decreased care quality perception in caregivers. These results raise compelling questions about the personal and institutional strategies used to combat EE in nursing home staff.
Moreover, it seems that COVID-19 has substantially changed the work carried out and the care provided by health workers in nursing homes. Workers are performing greater amounts of medical care with limited time and resources, and if a resident is undergoing new care and treatment plans, caregivers need to assess how such plans fit the patient's needs. During COVID-19 crisis, caregivers’ activities became more focused on palliative care (e.g., making complex decisions about infected older people) and fighting the spread of COVID-19 within their nursing home (e.g., implementing new health and safety practices such as isolation, and explaining them to families) rather than providing the best wellness care to people nearing end-of-life (Wallace et al., 2020). More and more elderly were deprived of social support from their families, leaving them without any positive, life-affirming events to attend (Wu, 2020). Health workers in nursing homes were exposed to an increase in mortality among the elderly, which has impacted their ability to cope with death and triggered altered emotion regulation (EE being one of its impacts) (Kosar et al., 2021; Blanco-Donoso et al. 2022). We believe that nursing homes should provide intervention programs to support nursing home staffs in order to drive down demands at work and ward off EE. As a first step, there is a need to deploy specific short-term prevention interventions against EE with a view to developing coping strategies and programs to support health workers, especially in dealing with their emotions and feelings, to prevent long-term effects. A second step should consist of developing a commensurate long-term strategy against the types of EE prevalent in nursing homes by providing caregivers adequate time and resources.
Our study has some limitations. First of all, our sample is small and health workers were recruited from only four nursing homes. Second, the study specifically explored (using self-reporting measuring methods) only two dimensions of the work environment: emotional exhaustion and care quality experience. Third, the small number of each occupational category (e.g., physician, nurses, ) does not allow for their comparison. Regardless, this study is the first to assess the linkages between care quality experience in nursing home staff directly and repeatedly exposed to COVID-19.
In future research, it could be of interest to evaluate the long-term effect of COVID-19 exposure on the care experience of nursing home staff.
CRediT authorship contribution statement
Emin Altintas: Conceptualization, Formal analysis, Methodology, Project administration, Writing – original draft. Abdel-Halim Boudoukha: Writing – original draft, Writing – review & editing. Yasemin Karaca: Writing – review & editing. Andréa Lizio: Writing – review & editing. Marion Luyat: Writing – original draft, Writing – review & editing. Karim Gallouj: Conceptualization, Investigation, Supervision, Validation, Project administration. Mohamad El Haj: Resources, Supervision, Validation, Writing – review & editing.
Declaration of Competing Interest
All authors declare that there is no conflict of interest.
References
- Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/s11469-020-00270-8. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer N., Baykal U. Quality perception of nurses in the hospitals receiving quality certificate. Health Science Journal. 2018;12(4):578. doi: 10.21767/1791-809X.1000578. [DOI] [Google Scholar]
- Blanco-Donoso L.M., Moreno-Jiménez J., Gallego-Alberto L., Amutio A., Moreno-Jiménez B., Garrosa E. Satisfied as professionals, but also exhausted and worried!!: The role of job demands, resources and emotional experiences of Spanish nursing home workers during the COVID-19 pandemic. Health Social Care Community. 2022;30(1):e148–e160. doi: 10.1111/hsc.13422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhans L.M., Alligood M.R. Quality nursing care in the words of nurses. Journal of Advanced Nursing. 2010;66(8):1689–1697. doi: 10.1111/j.1365-2648.2010.05344.x. [DOI] [PubMed] [Google Scholar]
- Cleland J., Hutchinson C., Khadka J., Milte R., Ratcliffe J. What defines quality of care for older people in aged care? A comprehensive literature review. Geriatrics and Gerontology International. 2021:1–14. doi: 10.1111/ggi.14231. [DOI] [PubMed] [Google Scholar]
- Costello H., Walsh S., Coope C., &Livingston G. A systematic review and meta-analysis of the prevalence and associations of stress and burnout among staff in long term care facilities for people with dementia. International Psychogeriatrics. 2019;31(8):1203–1216. doi: 10.1017/S1041610218001606. [DOI] [PubMed] [Google Scholar]
- Dhaini S.R., Zúñiga F., Ausserhofer D., Simon M., Kunz R., De Geest S., Schwendimann R. Care workers health in Swiss nursing homes and its association with psychosocial work environment: A cross-sectional study. International Journal of Nursing Studies. 2016;53:105–115. doi: 10.1016/j.ijnurstu.2015.08.011. [DOI] [PubMed] [Google Scholar]
- Di Blasi M., Gullo S., Mancinelli E., Freda M.F., Esposito G., Gioacchino Gelo O.M., et al. Psychological distress associated with the COVID-19 lockdown: A two-wave network analysis. Journal of Affective Disorders. 2021;284:18–26. doi: 10.1016/j.jad.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dion G., Tessier R. Validation de la traduction de l'Inventaire d'épuisement professionnel de Maslach et Jackson [Validation of a French translation of the Maslach Burnout Inventory (MBI)] Canadian Journal of Behavioural Science/Revue Canadienne des Sciences du Comportement. 1994;26(2):210–227. doi: 10.1037/0008-400X.26.2.210. [DOI] [Google Scholar]
- El Haj M., Altintas E., Chapelet G., Kapogiannis D., Gallouj K. High depression and anxiety in people with Alzheimer's disease living in retirement homes during the covid-19 crisis. Psychiatry Research. 2020;291 doi: 10.1016/j.psychres.2020.113294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eltaybani S., Yamamoto-Mitani N., Ninomiya A., et al. The association between nurses’ burnout and objective care quality indicators: A cross-sectional survey in long-term care wards. BMC Nursing. 2021;20(34):2–10. doi: 10.1186/s12912-021-00552-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallon A., Dukelow T., Kennelly S.P., O'Neill D. COVID-19 in nursing homes. QJM. 2020;113(6):391–392. doi: 10.1093/qjmed/hcaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giusti E.M., Pedroli E., D'Aniello G.E., Stramba Badiale C., Pietrabissa G., Manna C., et al. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Frontiers in Psychology. 2020;11:1684. doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Gil M.T., González-Blázquez C., Parro-Moreno A.I., Pedraz-Marcos A., Palmar-Santos A., Otero-García L., et al. Nurses’ perceptions and demands regarding COVID-19 care delivery in critical care units and hospital emergency services. Intensive and Critical Care Nursing. 2021;62 doi: 10.1016/j.iccn.2020.102966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haute Autorité de Santé (HAS) (2012). Grille d'autocontrôle de mes pratiques professionnelles [Care Quality Perception Scale - CQPS]. https://www.has-sante.fr/upload/docs/application/pdf/2012-10/bientraitance_-_grille_ceppral.pdf.
- Horobet A., Simionescu A.A., Dumitrescu D.G., Belascu L. Europe's war against COVID-19: A map of countries’ disease vulnerability using mortality indicators. International Journal of Environmental Research and Public Health. 2020;17(18):6565. doi: 10.1177/0969733020901830. 10.3390/ijerph17186565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang H., Hur W.M., Shin Y. Emotional exhaustion among the South Korean workforce before and after COVID-19. Psychology and Psychotherapy. 2020 doi: 10.1111/papt.12309. 10.1111/papt.12309. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosar C.M., White E.M., Feifer R.A., Blackman C., Gravenstein S., Panagiotou O.A., McConeghy K., Mor V. COVID-19 mortality rates among nursing home residents declined from March to November 2020. Health Affairs. 2021;40(4):655–663. doi: 10.1377/hlthaff.2020.02191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mailliez M., Griffiths M.D., Carre A. Validation of the French version of the fear of COVID-19 scale and its associations with depression. Anxiety and Differential Emotions. 2020 doi: 10.21203/rs.3.rs-46616/v1. 22 July 2020PREPRINT (Version 1) available at Research Square. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzano Garcia G., Ayala Calvo J.C. Emotional exhaustion of nursing staff: Influence of emotional annoyance and resilience. International Nursing Review. 2012;59:101–107. doi: 10.1111/j.1466-7657.2011.00927.x. [DOI] [Google Scholar]
- Maslach C., Jackson S.E. 2nd ed. Consulting Psychologists Press; Palo Alto, CA: 1986. Maslach burnout inventory manual. [Google Scholar]
- Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annual Review of Psychology. 2001;52(1):397. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- Mert Boğa S., Aydin Sayilan A., Kersu Ö., Baydemir C. Perception of care quality and ethical sensitivity in surgical nurses. Nursing Ethics. 2020;27(3):673–685. doi: 10.1177/0969733020901830. [DOI] [PubMed] [Google Scholar]
- Mo S., Shi J. The psychological consequences of the COVID-19 on residents and staff in Nursing homes. Work Aging and Retirement. 2020;6(4):254–259. doi: 10.1093/workar/waaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh H., Uhm D.C., Yoon Y.J. Workplace bullying, job stress, intent to leave, and nurses' perceptions of patient safety in South Korean Hospitals. Nursing Research. 2016;65(5):380–388. doi: 10.1097/NNR.0000000000000175. [DOI] [PubMed] [Google Scholar]
- Özdemir Ş., Kerse G. The effects of COVID 19 on health care workers: Analysing of the interaction between optimism, job stress and emotional exhaustion. International and Multidisciplinary Journal of Social Sciences. 2020;9(2):178–201. doi: 10.17583/rimcis.2020.5849. [DOI] [Google Scholar]
- Pitkälä K.H. COVID-19 has hit nursing homes hard. European Geriatric Medicine. 2020;11:889–891. doi: 10.1007/s41999-020-00411-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti E., Di Mattei V., Perego G., Ferrari F., Mazzetti M., Taranto P., et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Current Psychiatry Reports. 2020;22(8):43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucker D.D., Preacher K.J., Tormala Z.L., Petty R.E. Mediation analysis in social psychology: Current practices and new recommendations. Social and Personality Psychology Compass. 2011;5(6):359–371. [Google Scholar]
- Ryan C., Powlesland J., Phillips C., Raszewski R., Johnson A., Banks-Enorense K., et al. Nurses' perceptions of quality care. Journal of Nursing Care Quality. 2017;32(2):180–185. doi: 10.1097/NCQ.0000000000000211. [DOI] [PubMed] [Google Scholar]
- Santé Publique France (2020). COVID-19: Point épidémiologique en Hauts-de-France du 10 Septembre 2020. https://www.santepubliquefrance.fr/dossiers/coronavirus-covid-19/coronavirus-chiffres-cles-et-evolution-de-la-covid-19-en-france-et-dans-le-monde.
- Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-a review. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuijfzand S., Deforges C., Sandoz V., Sajin C.T.C.T., Jaques C., et al. Psychological Impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health. 2020;20:1230. doi: 10.21203/rs.3.rs-30156/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka K., Iso N., Sagari A., Tokunaga A., Iwanaga R., Honda S., et al. Burnout of long-term care facility employees: Relationship with employees' expressed emotion toward patients. International Journal of Gerontology. 2015;9:161–165. doi: 10.1016/j.ijge.2015.04.001. [DOI] [Google Scholar]
- The Jamovi Project (2021). Jamovi. (Version 1.6) [Computer Software]. Retrieved from https://www.jamovi.org.
- Thomas D., Newcomb P., Fusco P. Perception of caring among patients and nurses. Journal of Patient Experience. 2019;6(3):194–200. doi: 10.1177/2374373518795713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace C.L., Wladkowski S.P., Gibson A., White P. Grief during the COVID-19 pandemic: Considerations for palliative care providers. Journal of Pain and Symptom Management. 2020;60(1):e70–e76. doi: 10.1016/j.jpainsymman.2020.04.012. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White E.M., Aiken L.H., McHugh M.D. Registered nurse burnout, job satisfaction and missed care in nursing homes. Journal of the American Geriatrics Society. 2019;67(10):2065–2071. doi: 10.1111/jgs.16051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B. Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Global Health Research and Policy. 2020;5:27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Wang C., Pan W., Zheng J., Gao J., Huang X., et al. Stress, burnout, and coping strategies of frontline nurses during the COVID-19 epidemic in wuhan and shanghai, China. Frontiers in Psychiatry. 2020;11:1–9. doi: 10.3389/fpsyt.2020.565520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020). WHO COVID-19 Dashboard. Available online: https://covid19.who.int Accessed 28 June 2021.