Abstract
Objectives:
We assessed whether administering cannabidiol (CBD) before recalling the traumatic event that triggered their disorder attenuates anxiety in patients with post-traumatic stress disorder (PTSD). As an exploratory pilot analysis, we also investigated whether this effect depends on the nature of the event (sexual vs. nonsexual trauma).
Methods:
Thirty-three patients of both sexes with PTSD were recruited and randomized 1:1 into two groups. One group received oral CBD (300 mg), and the other received a placebo before listening to a digital audio playback of their previously recorded report of the trigger event. Subjective and physiological measurements were taken before and after recall. We analyzed the data in two subsamples: trigger events involving sexual and nonsexual trauma.
Results:
In the nonsexual trauma group, the differences between measurements before and after recall were significantly smaller with CBD than placebo; this held true for anxiety and cognitive impairment. However, in the sexual trauma group, the differences were non-significant for both measurements.
Conclusion:
A single dose of CBD (300mg) attenuated the increased anxiety and cognitive impairment induced by recalling a traumatic event in patients with PTSD when the event involved nonsexual trauma.
Keywords: Cannabidiol, post-traumatic, sexual trauma, anxiety, cognitive dysfunction
Introduction
Post-traumatic stress disorder (PTSD) is characterized by symptoms that include high levels of anxiety and intrusive memories of the traumatic event; these memories are distressing, recurrent, and involuntary. The condition is associated with symptoms of dissociation, flashbacks, and hypervigilance that are present for at least 30 days.1 PTSD also involves cognitive abnormalities in processing emotional information.2 The traumatic experience associated with PTSD must be related to exposure to a concrete episode, such as a death threat, serious injury, or sexual violation.1
Three types of medication – selective serotonin reuptake inhibitors, serotonin and noradrenaline reuptake inhibitors, and atypical antipsychotics – have been used to treat patients with PTSD, with limited results.3 Several studies have sought to assess the effect of different drugs on the subjective and physiological responses to recalling traumatic situations under controlled experimental conditions. A review of these studies suggests that some pharmacological interventions can alter responses to traumatic memories. The most studied drug is propranolol, but the diversity of experimental protocols and the small number of publications makes it challenging to reach solid conclusions.4 Therefore, new pharmacological therapeutic alternatives are needed.3
It seems reasonable to study cannabidiol (CBD) in this context. This component of the Cannabis sativa plant does not produce the typical effects induced by the consumption of the plant5 and has exhibited numerous therapeutic possibilities, including antiepileptic,6 antipsychotic,7 and anxiolytic applications.8 The anxiolytic effect of CBD, established by consistent results in animals, has also been demonstrated in humans under controlled experimental situations, using a single dose in healthy volunteers and patients with a social anxiety disorder.8 In this situation, CBD produces an inverted U-shaped dose-response curve, with significant anxiolytic results occurring at 300 mg.9,10 The anxiolytic action of CBD has also been observed in continuous administration over 4 weeks among frontline health care workers.11,12
Several studies have associated trauma type with the development and severity of PTSD. Sexual trauma is strongly associated with a diagnosis of PTSD,13,14 and these patients have a more symptoms than patients with other trigger types; these could be important factors in the therapeutic response to medication.15-18
This leads us to hypothesize that CBD could attenuate the subjective manifestations induced by recalling the trigger event in patients with PTSD. This effect could differ depending on the type of traumatic event that caused the disorder.15
This study assessed whether administering CBD to patients with PTSD before recalling the traumatic event can attenuate the subjective and physiological manifestations of anxiety induced by this recall. Considering that patients with PTSD due to sexual abuse are an important subgroup in terms of symptomatology,15 we also investigated, as an exploratory pilot analysis, whether the effects of CBD depend on the nature of the traumatic event.
Methods
Study design and participants
This study was a randomized, parallel-group, double-blind, placebo-controlled trial in patients diagnosed with PTSD. We estimated the sample size based on previous studies that used anxiety-eliciting stimuli to calculate the difference between mean Visual Analog Mood Scale (VAMS) scores in patients who received CBD vs. placebo.9,19 We estimated a sample size that would yield a significance level of 0.05 and a statistical power of 0.8.20 Thirty-three participants of both sexes were recruited and randomized by minimization 1:1 into two groups: the CBD group (n=17) and the placebo group (n=16). The groups were matched by sex, age, body mass index (BMI), and symptom severity by a researcher not involved in data collection and analysis.
To identify patients for recruitment, we analyzed the medical records of a large hospital and conducted an active search in outpatient clinics and social media. The inclusion criteria were age between 18 and 60 years and a diagnosis of PTSD according to the DSM-V. The exclusion criteria were: abuse or dependence on psychoactive drugs; the presence of other psychiatric disorders, except for depression and anxiety disorders; and the presence of organic brain syndromes.
Psychological measures
The Portuguese version of the VAMS19,21,22 was used to analyze subjective manifestations of PTSD. This scale includes four factors: 1) anxiety (items: calm – agitated; tense – relaxed; worried – tranquil); 2) sedation (items: alert – sleepy; attentive – distracted); 3) cognitive impairment (items: difficult reasoning – perceptive; incapable – capable; agile – clumsy; confused – clear ideas; withdrawn – sociable; strong – weak; apathetic – dynamic) and; 4) discomfort (items: satisfied – dissatisfied; happy – sad; hostile – friendly; interested – disinterested).23
The SCID-V for the DSM-V was used to diagnose PTSD.24,25 The severity of PTSD symptoms was assessed using the Posttraumatic Stress Disorder Checklist (PCL-5).26,27
Physiological measures
Systolic and diastolic blood pressure (BP), heart rate (HR), and salivary cortisol concentrations were measured before and after traumatic event recall. The Salivette® device (Sarsted, Germany) was used to collect saliva samples. These devices consist of a tube containing a cylindrical cotton pad. The pad was chewed for at least 1 minute and then centrifuged in the tube. The results were determined with enzyme-linked immunosorbent assay (ELISA).
Trauma recall
Adapted from Pitman,28 the behavioral test for assessing subjective and physiological responses to recall of a traumatic event under controlled experimental conditions involved no editing of the recordings and did not include the neutral procedure. In the first experimental session, a digital audio recording was made of the patients as they described the traumatic event for 90 seconds. After recording, the participants were asked to imagine themselves in the traumatic situation, in the most vivid way possible, for 30 seconds. In the second experimental session, patients listened to their audio recording and then were asked to again imagine the trauma for 30 seconds. All participants received instructions prior to beginning the procedure and were advised that the recordings would be erased upon completion of the experiment.
Medication
CBD was supplied as a powder with 99.6% purity and no other cannabinoids (BioSynthesis Pharma Group; BSPG-Pharm, United Kingdom). The powder was then dissolved in corn oil and packed in gelatin capsules. Each capsule contained a 300 mg dose. The placebo consisted of corn oil packaged in identical capsules.
Procedure
The experimental protocol consisted of two sessions with a 1-week interval between them. In the first session, the informed consent form was signed, the measurements for matching the groups (sex, age, BMI, and PCL-5 score) were performed, and the participants recorded the traumatic event. In the second session, after adapting to the experimental setting (15 minutes), the patients were given CBD or placebo. Ninety minutes later, they underwent the recall procedure. The subjective and physiological measurements (BP, HR, CS, VAMS) were taken before and after the recall event. The study was conducted at the Laboratório de Psicofarmacologia, Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo em Ribeirão Preto. Table 1 summarizes the experimental protocol.
Table 1. Phases and procedures of the experimental session.
| Phase | Procedure |
|---|---|
| Day 0 | |
| Recruiting | Participants recruiting via social media or hospital outpatient. SCID-5 interview application and assessment of eligibility. |
| Day 1 | |
| Pairing | Calculation of BMI and application of PCL-5 |
| Behavioral trial (HCRP) | Recording the trauma report (90 seconds) |
| Imagine the traumatic event (30 seconds) | |
| Day 2 | Habituation (15 minutes) |
| Drug administration and behavioral trial (HCRP) | CBD or PLC (90 minutes) |
| BP, HR and SC, VAMS. | |
| Listening to the trauma report (90 seconds) | |
| Imagining the traumatic event (30 seconds) | |
| BP, HR and SC, VAMS. |
BMI = body mass index; BP = blood pressure; CBD = cannabidiol; HCRP = Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo; HR = heart frequency; PCL-5 = Posttraumatic Stress Disorder Checklist; PLC = placebo; SC = salivary cortisol; VAMS = Visual Analog Mood Scale.
Data analysis
Clinical and demographic data were analyzed, using the t-test for continuous data and Fisher’s exact test for nominal data. The remaining data were analyzed using three-way repeated measures analysis of variance (ANOVA). The factors were group (CBD x placebo), trauma (sexual x nonsexual), and phase (before and after the recall event). A significant difference in the phase-group-trauma interaction or phase-trauma interaction prompted an exploratory pilot analysis comparing the effects of CBD in two sub-samples, with and without sexual trauma. For this analysis, the differences (delta) between measurements performed before and after the recall in the CBD and placebo groups were compared using the t-test in each sub-sample. For all statistics, a p-value < 0.05 was considered statistically significant. SPSS version 26.0 was used for all statistical analyses.
Ethics statement
This study was approved by the research ethics committee of the Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (USP) (CAAE number: 2.405.299). Before enrollment in the study arms, informed consent was obtained from all participants.
Results
Table 2 shows the demographic characteristics of the study participants.
Table 2. Sociodemographic and clinical characteristics of the groups.
| Variable | CBD | PLC | Statistics |
|---|---|---|---|
| Group size (n – male/female) | 17 – 4/13 | 16 – 4/12 | X2 = 0.010; p = 0.922 |
| Age | 33.94 (11.55) | 32.50 (13.01) | t = 0.337; p = 0.738 |
| BMI | 25.69 (5.06) | 28.03 (6.57) | t = -1.14; p = 0.26 |
| PCL-5 | 52.47 (12.08) | 54.12 (9.21) | t = -0.44; p = 0.663 |
Data presented as mean (standard deviation), unless otherwise specified.
BMI = body mass index; CBD = cannabidiol; PCL-5 = Posttraumatic Stress Disorder Checklist; PLC = placebo.
Patient sex, age, BMI, and PCL-5 score did not differ significantly between the placebo and CBD groups.
Psychological measures
Table 3 shows the results of three-way repeated measures ANOVA for the VAMS subsets before and after the recall challenge.
Table 3. VAMS factor scores before and after behavioral tests and the three-way repeated measures ANOVA results.
| VAMS factor/phase | Cannabidiol
(n=17) (mean [SD]) |
Placebo
(n=16) (mean [SD]) |
Interaction | |||
|---|---|---|---|---|---|---|
| Phase | Phase x group | Phase x trauma | Phase x group x trauma | |||
| Anxiety | F1,29 = 73.7 (p < 0.001)*
ηp 2 = 0.72 |
F1,29 = 0.38 (p = 0.54)
ηp 2 = 0.01 |
F1,29 = 1.03 (p = 0.32)
ηp 2 = 0.03 |
F1,29 = 3.60 (p = 0.07)*
ηp 2 = 0.11 |
||
| Before | 40.34 (14.55) | 36.77 (14.92) | ||||
| After | 54.94 (15.05) | 55.00 (12.57) | ||||
| Sedation | F1,29 = 28.6 (p < 0.001)*
ηp 2 = 0.50 |
F1,29 = 0.69 (p = 0.41)
ηp 2 = 0.02 |
F1,29 = 3.22 (p = 0.08)**
ηp 2 = 0.10 |
F1,29 = 0.29 (p = 0.60)
ηp 2 = 0.01 |
||
| Before | 58.52 (10.40) | 54.34 (14.53) | ||||
| After | 42.23 (14.82) | 42.03 (13.55) | ||||
| Cognitive impairment | F1,29 = 23.4 (p < 0.001)*
ηp 2 = 0.45 |
F1,29 = 4.28 (p = 0.048)**
ηp 2 = 0.13 |
F1,29 = 0.03 (p = 0.86)
ηp 2 = 0.001 |
F1,29 = 0.61 (p = 0.44)
ηp 2 = 0.02 |
||
| Before | 45.40 (11.69) | 43.36 (11.95) | ||||
| After | 49.15 (13.01) | 53.41 (15.78) | ||||
| Discomfort | F1,29 = 29.8 (p < 0.001)*
ηp 2 = 0.51 |
F1,29 = 0.14 (p = 0.72)
ηp 2 = 0.005 |
F1,29 = 0.12 (p =0.72)
ηp 2 = 0.004 |
F1,29 = 4.48 (p = 0.043)*
ηp 2 = 0.13 |
||
| Before | 37.71 (11.8) | 40.86 (11.81) | ||||
| After | 46.90 (12.21) | 49.84 (11.16) | ||||
ANOVA = analysis of variance; VAMS = Visual Analog Mood Scale.
p < 0,05;
p > 0.05 and < 0.1.
Significantly higher VAMS scores were observed for all factors after the patients recalled the traumatic event (phase). There was also a significant phase-group interaction in cognitive impairment factor, with a greater increase in scores after recall in the placebo group (10.50) than in the CBD group (3.75). The phase-group-trauma interaction was significant for the discomfort factor, and there was a trend towards significance in anxiety. Moreover, there was a significant phase-trauma interaction in the sedation factor.
Since there was a significant interaction between phase-group-trauma, we performed an exploratory analysis by dividing the sample into two sub-samples (sexual and nonsexual trauma). The PTSD-triggering event was sexual abuse in 14 patients and nonsexual trauma in 19. The nonsexual types of traumatic events included being threatened with firearms (nine patients), physical violence (four patients), indirect trauma (four patients), and accidents (two patients). In the sexual trauma subsample, seven participants received CBD and seven received placebo; in the nonsexual trauma subsample, 10 participants received CBD and nine received placebo. Table 4 shows the demographic characteristics of the groups in the two sub-samples.
Table 4. Sociodemographic and clinics characteristics of the samples and groups.
| Variable | Comparison between samples | Comparison between groups | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Trauma | Sexual trauma (n=14) | Other trauma (n=19) | |||||||
| Sexual | Other | p-value | CBD | PLC | p-value | CBD | PLC | p-value | |
| Group size (n – male/female) | 14 (1/13) | 19 (7/12) | 0.10 | 7 (0/7) | 7 (1/6) | 1.00 | 10 (4/6) | 9 (3/6) | 1.00 |
| Age (mean [SD]) | 25.15 (6.00) | 39.21 (12.10) | < 0.001* | 23.57 (3.87) | 26.71 (7.50) | 0.34 | 41.2 (9.22) | 27.9 (14.90) | 0.47 |
| BMI (mean [SD]) | 25.18 (7.24) | 28.04 (4.45) | 0.17 | 22.52 (4.54) | 27.84 (8.75) | 0.18 | 27.9 (4.31) | 28.18 (4.86) | 0.90 |
| PCL-5 | 54.29 (11.50) | 52.53 (10.25) | 0.65 | 52.57 (13.63) | 56.00 (9.68) | 0.60 | 52.40 (11.65) | 52.67 (9.14) | 0.96 |
| Marital status | |||||||||
| Single | 5 (35.70) | 6 (31.60) | 1.00 | 3 (42.90) | 2 (28.60) | 1.00 | 2 (20.00) | 4 (44.40) | 0.35 |
| Cohabiting | 9 (64.30) | 13 (68.40) | 4 (57.10) | 5 (71.40) | 8 (80.00) | 5 (55.60) | |||
| Time since the trauma, years | |||||||||
| < 10 | 6 (42.90) | 16 (84.20) | 0.02† | 4 (57.10) | 2 (28.60) | 0.59 | 8 (80.00) | 8 (88.90) | 1.00 |
| ≥ 10 | 8 (57.10) | 3 (15.80) | 3 (42.90) | 5 (71.40) | 2 (20.00) | 1 (11.10) | |||
| Education, years | |||||||||
| < 11 | 4 (28.60) | 9 (47.40) | 0.31 | 1 (14.30) | 3 (42.90) | 0.56 | 6 (60.00) | 3 (33.30) | 0.37 |
| ≥ 11 | 10 (71.40) | 10 (52.60) | 6 (85.70) | 4 (57.10) | 4 (40.00) | 6 (66.70) | |||
| Employment | |||||||||
| Active | 5 (35.70) | 7 (36.80) | 1.00 | 3 (42.90) | 2 (28.60) | 1.00 | 2 (20.00) | 5 (55.60) | 0.17 |
| Inactive | 9 (64.30) | 12 (63.20) | 4 (57.10) | 5 (71.40) | 8 (80.00) | 4 (44.40) | |||
| Medication use | |||||||||
| Yes | 7 (50.00) | 9 (47.40) | 1.00 | 4 (57.10) | 3 (42.90) | 1.00 | 5 (50.00) | 4 (44.40) | 1.00 |
| No | 7 (50.0) | 10 (52.60) | 3 (42.90) | 4 (57.10) | 5 (50.00) | 5 (55.60) | |||
| Comorbidities | |||||||||
| Yes | 10 (71.40) | 12 (63.20) | 0.72 | 7 (100.0) | 3 (42.90) | 0.07** | 8 (80.00) | 4 (44.40) | 0.17 |
| No | 4 (28.60) | 7 (36.80) | 0 (0.0) | 4 (57.10) | 2 (20.00) | 5 (71.40) | |||
Data presented as n (%), unless otherwise specified.
BMI = body mass index; CBD = cannabidiol; PCL-5 = Posttraumatic Stress Disorder Checklist; PLC = placebo; SD = standard deviation.
p < 0.05;
p > 0.05 and < 0.1.
Patient sex, age, BMI, PCL-5 score, marital status, time since the trauma, education level, occupation, medication use, and comorbidities did not significantly differ between the placebo and CBD recipients in either subsample. However, there were sex differences between the sexual and nonsexual trauma subsamples in the CBD group (Fisher’s exact test = 6.5; p = 0.035). Moreover, patients with sexual trauma were younger and had a shorter time since the traumatic event than those with nonsexual trauma.
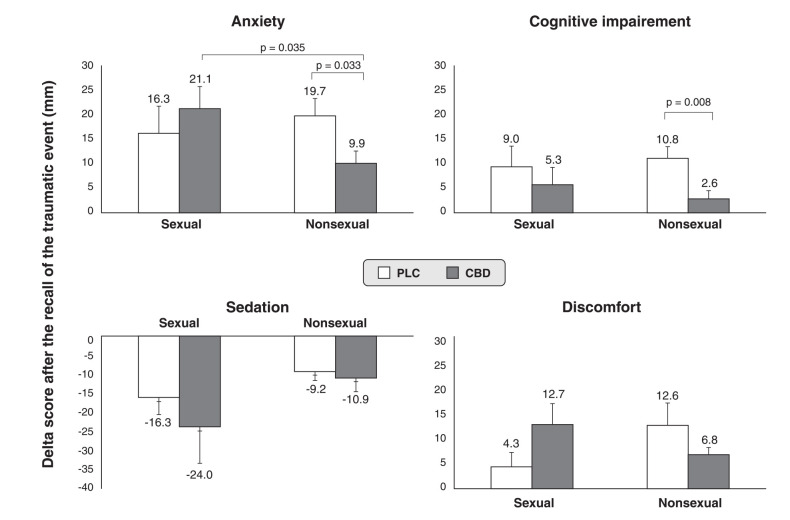
The differences between VAMS factor measurements before and after the recall event are shown in Figure 1.
Figure 1. Visual Analog Mood Scale delta scores after recalling the traumatic event in post-traumatic stress disorder patients with sexual and nonsexual traumas. In the nonsexual sample, the cannabidiol (CBD) group (n=10) had significantly lower anxiety and cognitive impairment than the placebo group (n=9). However, no significant differences were observed between CBD (n=7) and placebo (n=7) in the sexual sample.
Among those with nonsexual trauma, the change in VAMS anxiety before and after the recall event was significantly lower in the CBD group than the placebo group (mean difference = -9.82; p = 0.033; 95% confidence interval [95%CI] -18.74 to -0.91). The difference between the CBD and placebo subgroups was not significant among those with sexual trauma (mean difference = 5.00; p = 0.497; 95%CI -10.56 to 20.57). CBD led to significantly greater reductions in VAMS anxiety for nonsexual than sexual trauma (mean difference = 11.40; p = 0.035; 95%CI 0.90-21.89).
Regarding VAMS cognitive impairment before and after the recall event, those with nonsexual trauma had a significantly greater reduction in the CBD group than the placebo group (mean difference = -8.21; p = 0.008; 95%CI -13.94 to -2.47). This difference was not observed among those with sexual trauma (mean difference = -3.70; p = 0.524; 95%CI -16.00 to 8.60).
Regarding VAMS sedation, there was no significant difference in scores before and after the recall event among those with nonsexual (mean difference = -1.67; p = 0.713; 95%CI -11.10 to 7.75) or sexual trauma (mean difference = -7.72; p = 0.525; 95%CI -33.39 to 17.95). Similarly, there was no significant difference in VAMS discomfort among those with nonsexual (mean difference = -5.81; p = 0.202; 95%CI -15.03 to 3.42) or sexual trauma (mean difference = 8.28; p = 0.123; 95%CI -2.61 to 19.17).
Physiological measures
Table 4 shows the values and the three-way repeated measures ANOVA results for physiological measures taken before and after the recall event.
Table 5. Physiological measures and three-way repeated measures ANOVA results.
| Physiological measures/phase | Cannabidiol (n=17) (mean [SD]) | Placebo (n=16) (mean [SD]) | Interaction | |||
|---|---|---|---|---|---|---|
| Phase | Phase x group | Phase x trauma | Phase x group x trauma | |||
| Systolic blood pressure | F1,29 = 8.20 (p = 0.008)*
ηp 2 = 0.22 |
F1,29 = 0.38 (p = 0.54)
ηp 2 = 0.13 |
F1,29 = 0.67 (p = 0.42)
ηp 2 = 0.02 |
F1,29 = 0.11 (p = 0.74)
ηp 2 = 0.004 |
||
| Before | 119.88 (13.57) | 119.12 (14.12) | ||||
| After | 124.52 (15.65) | 126.87 (21.30) | ||||
| Diastolic blood pressure | F1,29 = 2.00 (p = 0.17)
ηp 2 = 0.07 |
F1,29 = 1.32 (p = 0.26)
ηp 2 = 0.04 |
F1,29 = 0.17 (p = 0.68)
ηp 2 = 0.006 |
F1,29 = 0.02 (p = 0.89)
ηp 2 = 0.001 |
||
| Before | 77.71 (10.31) | 76.44 (11.31) | ||||
| After | 78.06 (9.18) | 80.44 (13.07) | ||||
| Heart rate | F1,29 = 4.84 (p = 0.04)*
ηp 2 = 0.14 |
F1,29 = 0.37 (p = 0.55)
ηp 2 = 0.01 |
F1,29 = 6.64 (p = 0.015)*
ηp 2 = 0.19 |
F1,29 = 0.41 (p = 0.53)
ηp 2 = 0.01 |
||
| Before | 79.88 (10.36) | 81.62 (10.09) | ||||
| After | 82.05 (11.18) | 82.93 (11.18) | ||||
| Salivary cortisol | F1,29 = 0.39 (p = 0.54)
ηp 2 = 0.01 |
F1,29 = 0.79 (p = 0.38)
ηp 2 = 0.03 |
F1,29 = 0.03 (p = 0.86)
ηp 2 = 0.001 |
F1,29 = 0.24 (p = 0.63)
ηp 2 = 0.01 |
||
| Before | 0.19 (0.25) | 0.17 (0.17) | ||||
| After | 0.20 (0.18) | 0.14 (0.12) | ||||
ANOVA = analysis of variance; SD = standard deviation.
p < 0.05.
Both systolic BP and HR were significantly higher after recalling the traumatic event (phase). A phase-trauma interaction was observed in the HR results.
The delta scores of physiological variables before and after recall did not differ significantly in either trauma subsample in either group. In the sexual trauma subsample, the mean difference in salivary cortisol was 0.07 (p = 0.102; 95%CI -0.02 to 0.16), whereas it was 0.02 (p = 0.814; 95%CI -0.15 to 0.19) among those with nonsexual trauma. Among those with sexual trauma, the mean difference in systolic BP was -1.29 (p = 0.879; 95%CI -19.24 to 16.67), while among those with nonsexual trauma it was -4.27 (p = 0.398; 95%CI -14.68 to 6.13). Among those with sexual trauma, the mean difference in diastolic BP was -4.14 (p = 0.470; 95%CI -16.25 to 7.96), while among those with nonsexual trauma it was -3.22 (p = 0.397; 95%CI -11.05 to 4.60). Among those with sexual trauma, the mean difference in HR was 2.43 (p = 0.521; 95%CI -5.57 to 10.43), while among those with nonsexual trauma it was -0.07 (p = 0.974; 95%CI -4.25 to 4.11).
Discussion
We observed that patients with PTSD, when asked to recall their triggering event, experience significantly higher subjective anxiety, alertness, discomfort, and cognitive impairment. They also experience a significantly higher physiological response, e.g., systolic BP and HR. This demonstrates the adequacy of testing the effects of drugs on subjective and physiological parameters influenced by trauma recall.
The subjective effects of recalling a traumatic event on cognitive impairment were significantly lower in the CBD group than the placebo group. This could indicate that CBD interferes with aversive memory reconsolidation, as has been observed in preclinical studies.29 However, we did not test this hypothesis in our experiment.
The increase in subjective cognitive impairment after recalling a traumatic event may be associated with the cognitive interference of the event itself.30 The results of a previous study may support the lower cognitive impairment we observed in the CBD group: in healthy volunteers, CBD significantly increased VAMS “clear-headed” (opposite of “fuzzy”) and “quick-witted” (opposite of “mentally slow”) scores in healthy volunteers.5
Our post-hoc pilot analysis showed that CBD’s impact on the subjective effects of recalling a traumatic event depends on whether the trauma that triggered PTSD was of a sexual nature. In patients with nonsexual trauma, CBD significantly attenuated anxiety and cognitive impairment after recall. Regarding anxiety, our result is consistent with previous observations of this cannabinoid’s anxiolytic effects in preclinical studies, healthy volunteers, frontline healthcare workers, and patients with social anxiety disorders.8,11,12 Regarding cognitive impairment, our results are consistent with findings across the sample and discussed above. Unlike the phase-group interaction for anxiety and cognitive impairment, the physiological variables were not significantly attenuated in the trauma subsamples. This dissociation between subjective mood and physiological effects following acute administration of CBD is consistent with findings in healthy volunteers10,20 and patients with social phobia.31
The fact that CBD had no significant effect on the subjective effects of recalling a traumatic event in patients with sexual trauma could be related to the greater symptom severity associated with such trauma.15-18 Of the three commonly reported PTSD trauma types (sexual trauma, nonsexual physical violence, and the unexpected death of a loved one), sexual trauma is associated with a higher overall symptom score and longer symptom duration.15 Patients with sexual trauma-related PTSD may need a higher dose of CBD than that used in this study. We chose a 300-mg dose based on studies in healthy volunteers.9,10 However, studies in patients with social anxiety disorder show that anxiolytic effects are not observed until the dose reaches 600 mg.31 In line with this observation, a case report on a patient with sexual trauma reported that, although a single dose of CBD (300 mg) did not attenuate trauma recall-induced anxiety, improvement was noted after 1 week of daily administration.32 The finding that the response to CBD depends on the type of trauma that induced PTSD indicates the heterogeneity of this disorder.15
One limitation of the present study is that the mean patient age and time since the traumatic event were significantly lower among those with sexual trauma than nonsexual trauma, which could have influenced the non-attenuation of anxiety in the sexual trauma subsample. However, the regression analyses of a cross-sectional study showed that PTSD symptoms are not associated with patient age at the initial trauma.16 The sex difference between the subsamples in the CBD group, i.e., the predominance of women in the sexual trauma subgroup, is to be expected according to epidemiological data.33 In an exploratory analysis (data not shown), we found that patient sex had no influence on the effects of CBD. Another limitation is that the analysis was not corrected for multiple comparisons. However, the study’s primary measure was the VAMS, and, to the best of our knowledge, this correction has not been used in the literature to analyze this scale’s four factors. Finally, the small number of participants is another limitation and reflects the difficulty of recruiting patients with PTSD who are willing to recall their traumatic experiences.
In conclusion, this study shows that a single 300-mg dose of CBD attenuates the cognitive impairment induced by recalling the triggering event in patients with PTSD. A post-hoc experimental pilot analysis suggested that CBD’s impact on the subjective effects of recalling the event depend on the type of trauma that triggered PTSD. In nonsexual trauma, CBD attenuated the increased anxiety and cognitive impairment of recall. However, it failed to do so when the event was sexual in nature. More extensive double-blind chronic placebo-controlled clinical trials using higher doses of CBD are needed to confirm and expand the potential role of CBD in treating patients with PTSD.
Disclosure
JASC was a consultant and/or has received speaker fees and/or sits on the advisory board and/or receives research funding from Janssen-Cilag, Torrent Pharm, Prati-Donaduzzi, PurMed Global, and BSPG Pharm over the past 3 years. JASC, JECH, and AWZ are coinventors of the patent “Fluorinated CBD compounds, compositions and uses thereof. Pub. No.: WO/2014/108899. International Application No.: PCT/IL2014/050023,” Def. US number Reg. 62193296; July 29, 2015; INPI on August 19, 2015 (BR1120150164927; Mechoulam R, Zuardi AW, Kapczinski F, Hallak JEC, Guimarães FS, Crippa JAS, Breuer A). Universidade de São Paulo (USP) has licensed this patent to Phytecs Pharm (USP Resolution No. 15.1.130002.1.1) and has an agreement with Prati-Donaduzzi to “develop a pharmaceutical product containing synthetic CBD and prove its safety and therapeutic efficacy in the treatment of epilepsy, schizophrenia, Parkinson’s disease, and anxiety disorders.” JASC, JECH, and AWZ are coinventors of the patent “Cannabinoid-containing oral pharmaceutical composition, method for preparing and using same,” INPI on September 16, 2016 (BR 112018005423-2). The other authors report no conflicts of interest.
Acknowledgements
This study was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and by the Instituto Nacional de Ciência e Tecnologia Translational em Medicina (INCT-TM; CNPq/FAPESP; 2008/09009-2; 2016/01801-5; 2020/ 05416-4). The funders had no role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
JASC received a grant from the University Global Partnership Network (UGPN) – Global Priorities in Cannabinoid Research Excellence Program; and is a member of the International Advisory Board of the Australian Centre for Cannabinoid Clinical and Research Excellence (ACRE) – National Health and Medical Research Council (NHMRC). JASC, JEH, and AWZ are recipients of Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) research fellowships.
Footnotes
How to cite this article: Bolsoni LM, Crippa JAS, Hallak JEC, Guimarães FS, Zuardi AW. The anxiolytic effect of cannabidiol depends on the nature of the trauma when patients with post-traumatic stress disorder recall their trigger event. Braz J Psychiatry. 2022;44:298-307. http://dx.doi.org/10.1590/1516-4446-2021-2317
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Vasterling JJ, Arditte Hall KA. Neurocognitive and information processing biases in posttraumatic stress disorder. Curr Psychiatry Rep. 2018;20:99. doi: 10.1007/s11920-018-0964-1. [DOI] [PubMed] [Google Scholar]
- 3.Hoskins MD, Bridges J, Sinnerton R, Nakamura A, Underwood JF, Slater A, et al. Pharmacological therapy for post-traumatic stress disorder: a systematic review and meta-analysis of monotherapy, augmentation and head-to-head approaches. Eur J Psychotraumatol. 2021;12:1802920. doi: 10.1080/20008198.2020.1802920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolsoni LM, Zuardi AW. Pharmacological interventions during the process of reconsolidation of aversive memories: a systematic review. Neurobiol Stress. 2019;11:100194. doi: 10.1016/j.ynstr.2019.100194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zuardi AW, Shirakawa I, Finkelfarb E, Karniol IG. Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology (Berl) 1982;76:245–50. doi: 10.1007/BF00432554. [DOI] [PubMed] [Google Scholar]
- 6.Guimarães dos Santos R, Hallak JE, Zuardi AW, Crippa JA. Cannabidiol for treatment of epilepsy: an overview of possible mechanisms of action and preclinical and human studies. In: Preedy V, editor. Handbook of cannabis and related pathologies. Cambridge: Academic Press; 2017. pp. 795–801. [Google Scholar]
- 7.Zuardi AW, Crippa JA, Hallak JE, Bhattacharyya S, Atakan Z, Martin-Santos R, et al. A critical review of the antipsychotic effects of cannabidiol: 30 years of a translational investigation. Curr Pharm Des. 2012;18:5131–40. doi: 10.2174/138161212802884681. [DOI] [PubMed] [Google Scholar]
- 8.Zuardi AW, Crippa JA, Hallak JE, Campos AC, Guimarães FS. The anxiolytic effects of cannabidiol. In: Preedy V, editor. Handbook of cannabis and related pathologies. Cambridge: Academic Press; 2017. pp. e131–9. [Google Scholar]
- 9.Zuardi AW, Rodrigues NP, Silva AL, Bernardo SA, Hallak JE, Guimarães FS, et al. Inverted U-shaped dose-response curve of the anxiolytic effect of cannabidiol during public speaking in real life. Front Pharmacol. 2017;8:259. doi: 10.3389/fphar.2017.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linares I, Zuardi AW, Pereira LC, Queiroz RH, Mechoulam R, Guimarães FS, et al. Cannabidiol presents an inverted U-shaped dose-response curve in a simulated public speaking test. Eur Neuropsychopharmacol. 2016;26:S617. doi: 10.1016/S0924-977X(16)31702-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pacheco JC, Souza JD, Hallak JE, Osório FL, Campos AC, Guimarães FS, et al. Cannabidiol as a treatment for mental health outcomes among health care workers during the coronavirus disease pandemic. J Clin Psychopharmacol. 2021;41:327–9. doi: 10.1097/JCP.0000000000001405. [DOI] [PubMed] [Google Scholar]
- 12.Crippa JA, Zuardi AW, Guimarães FS, Campos AC, de Lima Osório F, Loureiro SR, et al. Efficacy and safety of cannabidiol plus standard care vs standard care alone for the treatment of emotional exhaustion and burnout among frontline health care workers during the COVID-19 pandemic: a randomized clinical trial. JAMA Netw Open. 2021;4:e2120603. doi: 10.1001/jamanetworkopen.2021.20603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit area survey of trauma. Arch Gen Psychiatry. 1998;55:626–32. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 14.Nöthling J, Simmons C, Suliman S, Seedat S. Trauma type as a conditional risk factor for post-traumatic stress disorder in a referred clinic sample of adolescents. Compr Psychiatry. 2017;76:138–46. doi: 10.1016/j.comppsych.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Smith HL, Summers BJ, Dillon KH, Cougle JR. Is worst-event trauma type related to PTSD symptom presentation and associated features? J Anxiety Disord. 2016;38:55–61. doi: 10.1016/j.janxdis.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Guina J, Nahhas RW, Sutton P, Farnsworth S. The influence of trauma type and timing on PTSD symptoms. J Nerv Ment Dis. 2018;206:72–6. doi: 10.1097/NMD.0000000000000730. [DOI] [PubMed] [Google Scholar]
- 17.Çoban DA, Gündoğmuş İD. Comparison of post-traumatic stress disorder symptom profile according to sexual and nonsexual trauma types. Anadolu Psikiyatri Derg. 2019;20:470–6. [Google Scholar]
- 18.Kul AT, Gündogmus I. The effect of trauma type on the severity of Post-Traumatic Stress Disorder (PTSD) symptoms. Rev Psiquiatr Clin. 2020;47:135–9. [Google Scholar]
- 19.Zuardi AW, Cosme RA, Graeff FG, Guimarães FS. Effects of ipsapirone and cannabidiol on human experimental anxiety. J Psychopharmacol. 1993;7:82–8. doi: 10.1177/026988119300700112. [DOI] [PubMed] [Google Scholar]
- 20.Miot HA. Sample size in clinical and experimental trials. J Vasc Bras. 2011;10:275–8. [Google Scholar]
- 21.Norris H. The action of sedatives on brain stem oculomotor systems in man. Neuropharmacology. 1971;10:181–91. doi: 10.1016/0028-3908(71)90039-6. [DOI] [PubMed] [Google Scholar]
- 22.Zuardi AW, Karniol IG. Estudo transcultural de uma escala de auto-avaliação para estados subjetivos. J Bras Psiquiatr. 1981;30:403–6. [Google Scholar]
- 23.Parente AC, Garcia-Leal C, Del-Ben CM, Guimarães FS, Graeff FG. Subjective and neurovegetative changes in healthy volunteers and panic patients performing simulated public speaking. Eur Neuropsychopharmacol. 2005;15:663–71. doi: 10.1016/j.euroneuro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 24.First MB, Willians JB, Karg RS, Spitzer RL. Entrevista clínica e estruturada para os transtornos do DSM-V – SCID-5 – CV. Porto Alegre: Artmed; 2017. [Google Scholar]
- 25.Osório FL, Loureiro SR, Hallak JE, Machado-de-Sousa JP, Ushirohira JM, Baes CV, et al. Clinical validity and intrarater and test-retest reliability of the Structured Clinical Interview for DSM-5 – Clinician Version (SCID-5-CV) Psychiatry Clin Neurosci. 2019;73:754–60. doi: 10.1111/pcn.12931. [DOI] [PubMed] [Google Scholar]
- 26.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) [Internet] 2013. www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp [cited 2018 Apr 2]
- 27.Osório FL, da Silva TD, dos Santos RG, Chagas MH, Chagas NM, Sanches RF, Crippa JA. Post-traumatic stress disorder checklist for DSM-5 (PCL-5): transcultural adaptation of the Brazilian version. Arch Clin Psychiatry. 2017;44:10–9. [Google Scholar]
- 28.Pitman RK, Sanders KM, Zusman RM, Healy AR, Cheema F, Lasko NB, et al. Pilot study of secondary prevention of post-traumatic stress disorder with propranolol. Biol Psychiatry. 2002;51:189–92. doi: 10.1016/s0006-3223(01)01279-3. [DOI] [PubMed] [Google Scholar]
- 29.Stern CA, Gazarini L, Takahashi RN, Guimarães FS, Bertoglio LJ. On disruption of fear memory by reconsolidation blockade: evidence from cannabidiol treatment. Neuropsychopharmacology. 2012;37:2132–42. doi: 10.1038/npp.2012.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halligan SL, Michael T, Clark DM, Ehlers A. Posttraumatic stress disorder following assault: the role of cognitive processing, trauma memory, and appraisals. J Consult Clin Psychol. 2003;71:419–31. doi: 10.1037/0022-006x.71.3.419. [DOI] [PubMed] [Google Scholar]
- 31.Bergamaschi MM, Queiroz RH, Chagas MH, de Oliveira DC, De Martinis BS, Kapczinski F, et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naïve social phobia patients. Neuropsychopharmacology. 2011;36:1219–26. doi: 10.1038/npp.2011.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bolsoni LM, da Silva TD, Quintana SM, de Castro M, Crippa JA, Zuardi AW. Changes in cortisol awakening response before and after development of posttraumatic stress disorder, which cannot be avoided with use of cannabidiol: a case report. Perm J. 2019;23:18300. doi: 10.7812/TPP/18.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Douglas KA, Collins JL, Warren C, Kann L, Gold R, Clayton S, et al. Results from the 1995 National College health risk behavior survey. J Am Coll Health. 1997;46:55–66. doi: 10.1080/07448489709595589. [DOI] [PubMed] [Google Scholar]