In pediatric rheumatology, patient access to certified providers is a troubling issue. The Arthritis Foundation estimates that approximately 300,000 children in the United States have juvenile idiopathic arthritis (JIA), but notes that there are fewer than 400 board-certified and practicing pediatric rheumatologists.1 There are presently 9 states (including Alaska, Idaho, Montana, New Hampshire, Oklahoma, South Dakota, Wyoming and West Virginia) that are without any full-time pediatric rheumatology providers (Fig. 1).2,3 The American Academy of Pediatrics Division of Workforce and Medical Education Policy notes that most pediatric subspecialists are working in urban areas, at academic centers, with median wait times that may exceed 2 weeks for some specialties.4 In pediatric rheumatology, this means that patients are traveling an average of 92 km (57 miles)5 to see their provider, compared with 40 km (25 miles) for patients followed in other pediatric subspecialties, and up to a quarter of adult rheumatologists care for pediatric patients with rheumatologic needs.6 This finding represents a considerable gap in access because most pediatric rheumatic diseases are chronic cyclic conditions. With respect to patient adoption of telemedicine, another study in pediatric rheumatology reported that, even though 28% of clinic patients traveled greater than 3 hours to see their pediatric rheumatology providers, most (95%) patients reported preference for in-person clinical visits rather than telemedicine visits. However, patient familiarity with telemedicine as a clinical tool did increase the preference for telemedicine visits.7 Before telemedicine practices can be adopted as a routine part of pediatric rheumatology care, providers and patients need to clearly understand its strengths and limitations as a tool for health care. For providers, this includes research that results in standardization of telemedicine practices, including (1) specification of patients appropriate for telemedicine follow-up, and (2) clinical guidelines for conducting appropriate and complete video examinations. For patients and their families, this may include education around telemedicine and planning for incorporating telemedicine as part of their routine chronic disease management.
Fig. 1.
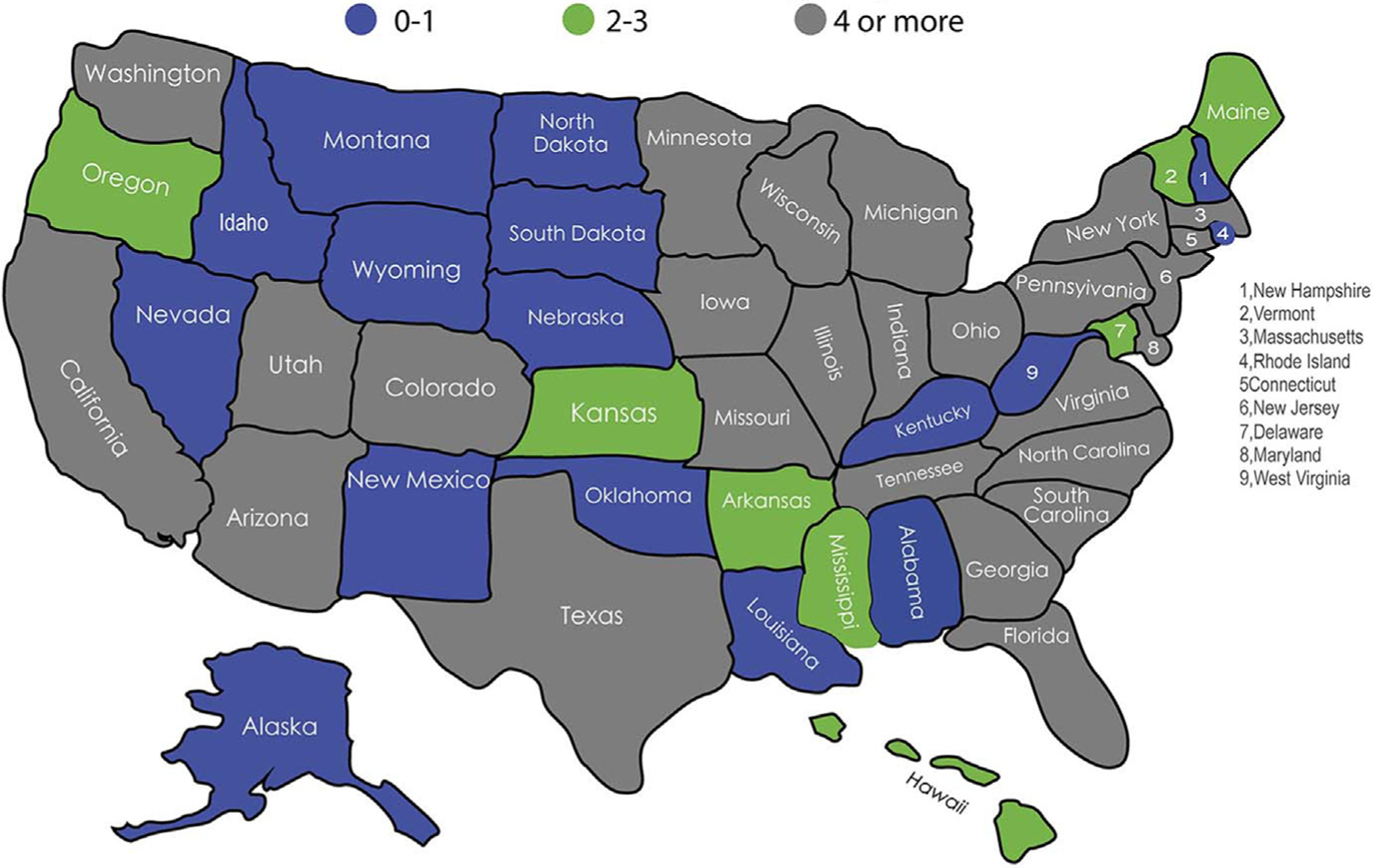
Number of pediatric rheumatologists by state.
Standardizing telemedicine clinical practice in pediatric rheumatology still needs to be done to ensure appropriate and comprehensive care is given to patients with chronic disease, as well as providing standardized workflows that can support governmental initiatives and policies surrounding telehealth. In order to address the provider-specific issues related to telemedicine, the key issues that have limited its adoption as a part of pediatric chronic disease management have begun to be unpacked.
The pediatric rheumatology group at Stanford Children’s has already begun to study this problem and is in the first part of a multiphase pilot study that addresses the clinical gaps involved in pediatric rheumatology provider-patient video visits. Based on expert input, we have identified barriers to adoption of telemedicine that surround the components of the in-person clinic visit experience, including but not limited to (1) the rheumatologic physical examination, (2) the vital signs, (3) modes of communication between provider and patient, (4) the need for immediate laboratory work or imaging, and (5) the need for nursing or social work support. The first phase of the study used expert clinical opinion with modified Delphi methodology8 to establish what is standard of practice and essential to clinical practice in routine, follow-up, in-person appointments for patients with either JIA or systemic lupus erythematosus (SLE). The reason for selection for patients with these diagnoses is that (1) they are the most commonly treated diagnoses in pediatric rheumatology clinical practice, and (2) they differ in terms of clinical assessment of disease activity. For example, in SLE, a patient may not have overt clinical symptoms of active disease but may have laboratory features that suggest otherwise, whereas a patient with JIA may have completely normal laboratory tests but a large swollen knee. This process included independent ratings of a 16-item survey on present clinical practices by a panel of 4 attending pediatric rheumatologists at Stanford Children’s Health, followed by a face-to-face meeting to reach consensus regarding those survey items that did not reach at least 75% consensus (per item) in the written survey. Each item that had not reached consensus in the initial written survey was reviewed and discussed, and consensus for all survey items was reached in the first round of discussion. As shown in Box 1, immediate access to clinic resources such as laboratory, social work, nursing, and imaging is convenient to have but not necessary for most of our follow-up patients with JIA or SLE. Furthermore, the essential examination components that help determine disease activity, disease progression, or medication side effects vary depending on the diagnosis and characteristics of the individual patient’s disease. For example, a patient with known JIA and uveitis needs regular eye examinations. The slit-lamp examination is critical for monitoring uveitis activity; however, it is within routine practice for rheumatologists to conduct a basic ophthalmologic examination because chronic changes may be visible without slit-lamp. The essential components for a rheumatologic clinical examination are featured in Box 1.
Box 1. Necessary clinical components for pediatric rheumatology visits.
| Essential components for SLE follow-up visit |
| Vitals: temperature, blood pressure, weight |
| Examination: |
| Focused ear, nose, and throat examination |
| Lung examination |
| Cardiac examination |
| Abdominal examination |
| Skin examination |
| MSK/joint examination: general upper extremities and lower extremities |
| Laboratory tests: |
| Laboratory tests are necessary to determine level of disease activity |
| Laboratory tests are not necessary at the time of the clinical visit but are needed for that encounter |
| Imaging |
| Imaging is not required at time of the visit in greater than 50% of patients with SLE |
| Essential components for JIAa follow-up visit |
| Vitals: weight |
| Examination |
| Lung examination |
| Cardiac examination |
| Abdominal examination |
| MSK/joint examination including: |
| Temporomandibular joint |
| Spine/sacroiliac joints |
| Upper extremities |
| Lower extremities |
| Leg length |
| Gait |
| Ophthalmologic examinationb |
| Laboratory tests: |
| Laboratory tests are not necessary to determine level of disease activity |
| Laboratory tests are not necessary at the time of the clinical visit, but may be needed for that encounter (ie, drug toxicity monitoring) |
| Imaging |
| Imaging is not required at the time of the visit in more than 50% of patients with SLE |
Abbreviation: MSK, musculoskeletal.
If systemic JIA, need blood pressure, temperature, and weight.
For known iritis, need documentation from ophthalmologist within last 3 months.
The next steps of this study are to use the clinical framework outlined in Box 1 and develop a checklist, that will be used to directly compare follow-up video visits and follow-up in-person visits in the Stanford Children’s pediatric rheumatology clinics. We hypothesize that 75% of the essential clinical standard practice (including examination) will be completed in the telemedicine visits. Ultimately, we will be able to measure these differences and understand the specific limitations of patient-provider video visits, such as effectiveness for urgent problems that come up unexpectedly. Understanding the differences between both types of clinical visits will (1) help determine solutions toward potential examination limitations, (2) provide a framework that can be used to standardize video visits, (3) understand the necessary education for patients around video visits, (4) improve provider clinical support and education regarding telemedicine visits, and (5) further governmental policy or insurance practices regarding telemedicine reimbursement.
If pediatric rheumatologists can better understand what is essential and nonessential in an in-person clinic visit, they can better understand the potential limitations in the use of telemedicine for chronic disease management and work toward solutions that continue to increase access and improve medical decision making in telemedicine.
The study described earlier and preliminary data show the need for additional research in telemedicine in pediatric rheumatology care. Only by understanding how to optimally use technologic tools can clinicians improve the delivery of medical care for patients with chronic disease. Telemedicine in pediatric rheumatology care can serve as a model for other pediatric subspecialties requiring chronic disease management. Studies could be conducted in other subspecialties, because the necessary clinical components for successful follow-up visits may vary widely. Telemedicine has the potential to be a critical component in pediatric chronic care, and it is the responsibility of clinicians to understand how best to use it for their patients.
KEY POINTS.
This article describes issues in patient access to pediatric rheumatologic care and the potential use of telemedicine in pediatric rheumatology. It also describes the necessary components of clinical exams in pediatric rheumatology.
ACKNOWLEDGMENTS
The authors acknowledge the following groups and individuals for their partnership and research guidance: Pediatric Rheumatology Department, Stanford Children’s Health, Health Research and Policy Department, Stanford University. C. Jason Wang MD PhD, Director of Center for Policy, Outcomes and Prevention, Stanford. Lee Sanders MD MPH, Associate Professor of Pediatrics, Lucile Packard Children’s Hospital, Stanford.
Footnotes
DISCLOSURE
The authors have nothing to disclose.
REFERENCES
- 1.Battafarano DF, Ditmyer M, Bolster MB, et al. 2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015–2030. Arthritis Care Res 2018. 10.1002/acr.23518. [DOI] [PubMed] [Google Scholar]
- 2.Available at: https://my.rheumatology.org/find-a-rheumatologist. Accessed February 8, 2020.
- 3.Pediatric Rheumatologists by State - Google Search. Available at: https://www.google.com/search?sxsrf=ACYBGNTlP4J_S2F5Xwu6dRtzTN9NClF1oQ%A1581483441235&source=hp&ei=sYVDXtL5C8XC-gSa0JyQCw&q=pediatric+rheumatologists+by+state&oq=pediatric+rheumatologists+by+state&gs_l=psyab.3..0i22i30.3159.8283..8461…3.0..0.107.2805.34j1. Accessed February 8, 2020.
- 4.Rimsza ME, Ruch-Ross HS, Clemens CJ, et al. Workforce Trends and Analysis of Selected Pediatric Subspecialties in the United States. Acad Pediatr 2018. 10.1016/j.acap.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Increase Access to Pediatric Rheumatologists. Available at: http://www.arthritis.org/advocate/our-policy-priorities/access-to-care/increase-access-to-pediatric-rheumatologists/. Accessed September 29, 2019.
- 6.Mayer ML, Mellins ED, Sandborg CI. Access to pediatric rheumatology care in the United States. Arthritis Rheum 2003. 10.1002/art.11462. [DOI] [PubMed] [Google Scholar]
- 7.Bullock DR, Vehe RK, Zhang L, et al. Telemedicine and other care models in pediatric rheumatology: An exploratory study of parents’ perceptions of barriers to care and care preferences. Pediatr Rheumatol 2017. 10.1186/s12969-017-0184-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilowite NT, Sandborg CI, Feldman BM, et al. Algorithm development for corticosteroid management in systemic juvenile idiopathic arthritis trial using consensus methodology. Pediatr Rheumatol 2012. 10.1186/1546-0096-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]


