Abstract
Objective
In a cohort assembled at the start of the pandemic in New York City, objectives of this longitudinal study were to ascertain whether perspectives about SARS-CoV-2 risks obtained at enrollment were associated with clinical course and vaccination intent obtained at follow-up with the advent of vaccines.
Methods
Patients with diverse rheumatologist-diagnosed diseases taking immunosuppressive medications were interviewed in April 2020 during the height of mortality-associated COVID-19 in New York City and were asked whether they perceived greater infection risk due to rheumatic diseases/medications. Patients were interviewed again when vaccines became available and asked about flares, medication changes, disease activity during the pandemic, and current disease status. They also reported SARS-CoV-2 testing, vaccination intent, and vaccination concerns.
Results
Ninety-six patients had follow-ups (January–March 2021; 83% women; mean age, 50 years). At enrollment, 53%/57% perceived much greater infection risk from autoimmune disease/medications; at follow-up, patients reported flares (63%), greater/unpredictable disease activity (40%), and more medications (44%). Current disease was excellent/very good/good (73%) and fair/poor (27%). Enrollment perspectives were not associated with follow-up status. Seventy percent had SARS-CoV-2 testing. Twenty-three percent would not/were hesitant about vaccination. In multivariable analysis, younger age, concern about effects on rheumatic disease, and distrusting vaccine information were main reasons for not intending/hesitancy to be vaccinated. Eighty-six percent did not report rheumatologists as sources of vaccine information.
Conclusions
Clinical status at follow-up and vaccination intent were not associated with perceived SARS-CoV-2 risk at the start of the pandemic. Concern about vaccine effects on rheumatic disease and distrust in vaccine information deterred patients from vaccination.
Key Words: COVID-19, perceived risk, flares, vaccine attitudes, distrust
The SARS-CoV-2 pandemic has had marked effects on physical and mental well-being among patients with rheumatic diseases.1–3 In addition to the impact on those infected, the virus has caused widespread disruptions in provisions of health care, medication regimens, and health-promoting behaviors.2–6 Vaccines offer potential additional defenses against the virus, but they are not universally accepted throughout the population and their long-term effectiveness is unknown, particularly in patients with underlying immunocompromised states.7,8
We assembled a cohort of patients with rheumatic diseases at the start of the pandemic in New York City to learn about patients' perceived risks of infection, medication modifications, and physical and mental well-being. The enrollment period coincided with peak mortality rates due to the virus in New York City in April 2020. Patients were interviewed in depth with open-ended questions and standard surveys, and a rich tableau of the pandemic's adverse effects on personal, social, professional, emotional, and physical health was assembled.9–12 Our plan was to track the clinical and personal impact of the unfolding pandemic longitudinally, and follow-up with patients at the time when a vaccine became available.
The goals of this study were to reinterview patients after several months to ascertain interval rheumatic disease status, such as flares and current disease activity, and their experiences with SARS-CoV-2, such as infection, testing, and attitudes toward vaccination. It was hypothesized that the deterioration in rheumatic disease status would be attributed to the pandemic and rheumatic disease–related issues obtained at enrollment would influence perspectives on vaccination.
METHODS
This study was approved by the institutional review board at the Hospital for Special Surgery, and all patients provided verbal consent. Patients were enrolled in April 2020 during the first surge of the pandemic and the height of COVID-19–related mortality in New York City. Patients with a rheumatologist-diagnosed rheumatic disease were eligible if they were taking immunosuppressive medications and had a telehealth visit during the study period or if they were recommended to the study by their rheumatologist. At enrollment, patients participated in a telephone interview, which asked about rheumatic disease medications, changes in medications due to the pandemic, psychosocial factors affected by the pandemic, and perceived risks of contracting the virus compared with the general population and due to immune-mediating medications (reported previously).9–12
For the follow-up, patients were interviewed again by telephone beginning in January 2021, coinciding with the initiation of SARS-CoV-2 vaccines for older patients and those with chronic conditions. This also coincided with the release of the American College of Rheumatology guidelines recommending vaccination for patients with rheumatic diseases.13 Patients were asked about clinical events since enrollment, including occurrence of typical or atypical flares and modifications in medications due to the pandemic or due to rheumatic disease symptoms. Medication changes were grouped as more disease-modifying antirheumatic drugs (DMARDs) (conventional or biologic) if doses were increased or if administration frequencies (ie, for injections/infusions) were shortened. Medication changes were grouped as less DMARDs if doses were decreased, if administration frequencies were lengthened, or if medications were discontinued. Reasons for medication changes were noted and grouped as due or not due to the pandemic. Patients rated their satisfaction with medications during the pandemic with options ranging from very satisfied to very dissatisfied and were asked about overall disease activity during the pandemic with response options of typical, more active, less active, or unpredictable. Patients also rated their current disease status with response options ranging from excellent to poor and reported any new physical or mental health diagnoses and related hospitalizations.
Patients were asked about symptoms, testing, and diagnosis of SARS-CoV-2 infection and whether they intended to be vaccinated at this time. Patients also were asked “do you have any concerns about the vaccine and, if so, what are those concerns.” Patients could volunteer as many concerns as they wished, and their responses were grouped into themes associated with hesitancy to be vaccinated as defined by other investigators (described later). Patients also were asked about the sources of their information about the vaccine.
Frequencies of responses to enrollment and follow-up questions were compared with demographic and clinical variables with χ2 tests. Based on themes from previous studies, apprehensions about the vaccine were grouped as concerns about development and distribution, distrust in information available, adverse effects, impact of the vaccine on rheumatic diseases and medications, and the necessity and impact of the vaccine on those previously infected with SARS-CoV-2.7,14 Patients were dichotomized as intending to be vaccinated or not intending/hesitant to be vaccinated (for the latter, if they responded no, not sure, or only if my physicians recommend it). Associations between the intention to be vaccinated (dependent variable) and demographic characteristics, clinical features, and concerns about the vaccine (independent variables) were assessed with χ2 tests. A multivariable logistic regression model was set up with the intention not to be vaccinated/hesitant as the dependent variable and demographic and clinical variables associated in bivariate analyses were included as independent variables. Independent variables were then retained after backward stepwise elimination if the p value was ≤0.05; no other variables were maintained in the model. Model performance was verified with the Wald χ2 test and the Hosmer-Lemeshow goodness-of-fit statistics. An additional model included diagnosis (ie, lupus vs rheumatoid arthritis) in a subanalysis.
RESULTS
Patients were enrolled between April 2 and April 21, 2020, and follow-ups were conducted between January 12 and March 3, 2021. The mean interval between enrollment and follow-up was 10 months (range, 9–11). Of the 112 patients enrolled, 96 participated in the follow-up, 7 agreed to participate but were unavailable to be interviewed during the follow-up period, 7 were not contacted, and 2 refused (one was dissatisfied with medical care and another was overwhelmed with her husband's new cancer diagnosis). There were no differences between the 96 participants and 16 nonparticipants with respect to age, sex, diagnosis, duration of disease, and rheumatic disease medications (p > 0.05 for all comparisons).
At enrollment, the 96 participants' mean age was 50 ± 15 years; 83% were women; 53% were married, 4% separated/divorced, 5% widowed, and 38% never married; 18% were non-White race and 13% were Latino ethnicity (all Latino patients reported White race) (Table 1). Of the 43% with major comorbidity, 21% had pulmonary conditions. Patients had a spectrum of rheumatic diseases and were taking diverse and often multiple medications, that is, 1 medication (38%), 2 (38%), 3 (20%), and 4 (3%) (Table 1). At enrollment, most patient perceived they were at somewhat to very much greater risk of contracting SARS-CoV-2 compared with the general population and perceived their medications definitely increased their risk.
TABLE 1.
Demographic Characteristics, Clinical Variables, and Perceived Risk of Contracting SARS-CoV-2 at Enrollment
| Variable | Value, % |
|---|---|
| Women | 83 |
| Age, mean, (range), y | 50 (22–87) |
| Race | |
| Asian | 8 |
| Black | 10 |
| White | 82 |
| Latino | 13 |
| Major comorbiditya | 43 |
| Diagnosis | |
| Systemic lupus erythematosus | 28 |
| Rheumatoid arthritis | 27 |
| Undifferentiated connective tissue disorder | 7 |
| Psoriatic arthritis | 7 |
| Sjögren syndrome | 4 |
| Mixed connective tissue disorder | 3 |
| Otherb | 23 |
| Duration of diagnosis, mean (range), y | 11 (.5–57) |
| Medications for rheumatic disease | |
| Conventional disease modifying anti‐rheumatic drugs | |
| Hydroxychloroquine | 50 |
| Glucocorticoids | 49 |
| Methotrexate | 16 |
| Azathioprine | 9 |
| Mycophenolate mofetil | 5 |
| Biologic disease modifying anti‐rheumatic drugs | |
| Tumor necrosis factor inhibitor | 17 |
| Interleukin inhibitor | 11 |
| B-cell activating factor inhibitor | 11 |
| B-cell CD20 monoclonal antibody | 9 |
| T-cell costimulatory signal inhibitor | 3 |
| Janus kinase (JAK) inhibitor | 3 |
| Perceive risk of contracting SARS-CoV-2 compared with general population | |
| Very much greater risk | 53 |
| Somewhat greater risk | 35 |
| Little more risk or not increased risk | 8 |
| Less risk or do not know | 3 |
| Perceive medications increase risk of contracting SARS-CoV-2 | |
| Definitely | 57 |
| Probably | 5 |
| Not really | 20 |
| Protective | 9 |
| Do not know | 9 |
aAccording to the Charlson Comorbidity Index.
bSpondyloarthritis, polymyalgia rheumatica, antiphospholipid syndrome/SLE, ankylosing spondylitis, small vessel vasculitis, scleroderma, Churg-Strauss syndrome, Still disease, overlap syndromes.
At the follow-up, patients reported that since enrollment they had typical (40%), worse (23%), or no flares (37%). Flares were more common in women than men (68% vs 38%; odds ratio [OR], 3.5; 95% CI, 1.1–10.6; p = 0.02), and 83% of those with flares had informed their rheumatologists about their symptoms. Patients reported their overall rheumatic disease activity had been typical (36%), more active or unpredictable (40%), or less active (24%) (Table 2). Compared with enrollment, 45% of patients were taking the same medications, 11% were taking less, and 44% were taking more medications defined as higher doses or more frequent dosing intervals (ie, 24% more prednisone, 12% more other conventional DMARDs, and 22% more biologics). In addition, 11% reported their medications had changed specifically due to the pandemic, mainly decreasing medications because of missed infusions and stopping medications before vaccination or when exposed to someone who was COVID-19 positive. At the follow-up, men were more likely than women to be taking the same medications (69% vs 40%; OR, 3.3; 95% CI, 1.1–10.4; p = 0.04), and patients were more likely to be taking prednisone if they were younger (44 vs 52 years; p = 0.04) and had been taking prednisone at enrollment (32% vs 14%; OR, 2.8; 95% CI, 1.0–7.7; p = 0.04). Overall, 71% were very satisfied or satisfied with the management of their medications during the pandemic and 32% rated their current condition as excellent or very good, 41% good, and 27% fair/poor. Satisfaction with medications and current disease activity were not associated with enrollment characteristics. New major health conditions requiring hospitalization were reported by 14%, including new pregnancy (3%) and new or advancing cancer (4%), including 1 new B-cell lymphoma in a patient taking adalimumab and azathioprine.
TABLE 2.
Clinical Characteristics During Study Period Reported by Patients at Follow-up
| Variable | Value, % |
|---|---|
| Rheumatic disease flares | |
| None | 37 |
| Typical | 40 |
| Worse | 23 |
| Rheumatic disease activity | |
| Typical | 35 |
| More active | 31 |
| Less active | 24 |
| Unpredictable | 9 |
| Medications modified due to pandemic | 11 |
| Medications compared with enrollment | |
| Same | 45 |
| More prednisonea | 24 |
| Less prednisoneb | 4 |
| More conventional DMARDsa,c | 12 |
| Less conventional DMARDsb,c | 8 |
| More biologic DMARDsa | 22 |
| Less biological DMARDsb | 5 |
| Satisfaction with management of rheumatic disease medications | |
| Very satisfied | 44 |
| Satisfied | 27 |
| Neutral | 17 |
| Dissatisfied | 9 |
| Very dissatisfied | 3 |
| Current status of rheumatic disease | |
| Excellent | 11 |
| Very good | 22 |
| Good | 41 |
| Fair | 21 |
| Poor | 6 |
| New major physical or mental health diagnosis | 14 |
aIncludes increased dose and more frequent dosing interval.
bIncludes lower dose and less frequent dosing interval.
cNot including prednisone.
Most patients (70%) had been tested for SARS-CoV-2: 40% because of curiosity, 11% because it was required before a medical procedure, 10% because it was required for employment or because they were exposed to someone with COVID-19, and 9% because of symptoms (Table 3). Nine patients tested positive; 8 had symptoms (eg, cough, fever, loss of taste or smell) and 1 was asymptomatic. One patient was hospitalized for COVID-19; she was not intubated and was discharged after several days. Thirty-six percent were tested for SARS-CoV-2 antibodies and 4% were positive.
TABLE 3.
Variables Related to COVID-19
| Variable | Value, % |
|---|---|
| Had SARS-CoV-2 test | 70 |
| Positive result | 9 |
| Negative result | 61 |
| Reason for testing | |
| Not tested | 30 |
| Just curious | 40 |
| Before medical procedure | 11 |
| Required for job | 4 |
| Exposed to patient with COVID-19 | 4 |
| Before visiting others | 2 |
| Had COVID-19 symptoms | 9 |
| Plan to get vaccine | |
| Yes | 77 |
| No | 6 |
| Not sure | 11 |
| Only if MD recommends | 6 |
| Concerns about vaccine | |
| None | 32 |
| Development/distribution: developed too fast; new type of vaccine; requires special handling; which one is better; effectiveness against variants | 10 |
| Rheumatic disease–related: may impact compromised immune system; may trigger a flare; may interact with medications | 39 |
| Distrust: wait and see what happens to others; misinformation; too many unknowns | 15 |
| Adverse effects: short-term reaction; long-term sequelae; allergic to many things | 20 |
| Had COVID-19: may not be necessary; impact may be different compared with uninfected | 6 |
Vaccine availability based on older age and comorbidity started during the follow-up period, but scheduling appointments to be vaccinated was challenging. Overall, 77% stated they would definitely get the vaccine (28% already had received the first dose), 6% definitely would not, and the remaining 17% were hesitant (ie, unsure or wanted their physicians' opinions). Most patients (67%) reported they obtained information about the vaccine from 2 or more sources, including television news media (46%), the Internet (31%), daily briefings from local governments (19%), social network word of mouth (17%), rheumatologists (14%), other physicians (13%), employers/unions (10%), and hospital/rheumatic disease society newsletters (10%). Those who obtained information from medical sources (ie, physicians and hospital/society newsletters) reported these sources echoed uncertainty reported by other sources.
Patients were asked if they had concerns about the vaccine, and if so, what were those concerns. Nearly a third (32%) stated they had no concerns, 10% were concerned about the rapid development of this new type of vaccine and its special handling requirements, 39% were concerned about the unknown impact of the vaccine on their rheumatic disease and medications, 20% were concerned about short- and long-term adverse effects, and 15% were distrustful of available information about the vaccine. Only 2 patients reported they never receive vaccines. Among the 9 patients who had had COVID-19, 6 were concerned about the necessity of a vaccine and its impact on them compared with participants in clinical trials who were uninfected. There were no associations between types of concerns and clinical characteristics; however, distrust was a more frequent concern among Black patients compared with Asian and White patients (67% vs 9%; OR, 19.8; 95% CI, 4.1–94.5; p < 0.0001).
Response to the question about intending to be vaccinated was dichotomized as yes, intending to be vaccinated, or no, not intending/hesitant. There were no differences in the percent of men and women intending to be vaccinated (87% vs 75%; OR, 2.3; 95% CI, 0.5–11.2; p = 0.29), but younger patients and Black patients were less likely to plan to be vaccinated (Figure). There were no differences based on Latino or non-Latino ethnicity (67% vs 79%; OR, 0.6, 95% CI, 0.2–2.0; p = 0.36) and, according to clinical characteristics measured at enrollment, including use of corticosteroids, other DMARDs or biologics, number of medications, comorbidity, and perceived risk of contracting SARS-CoV-2 (all p's > 0.1). In a subanalysis according to diagnosis, patients with lupus (n = 27) were less likely to intend to be vaccinated compared with patients with rheumatoid arthritis (n = 26) (59% vs 92%; OR, 0.1; 95% CI, 0.02–0.62; p = 0.01). Patients with lupus also were younger (43 vs 52, p = 0.02) but did not differ by race.
FIGURE.
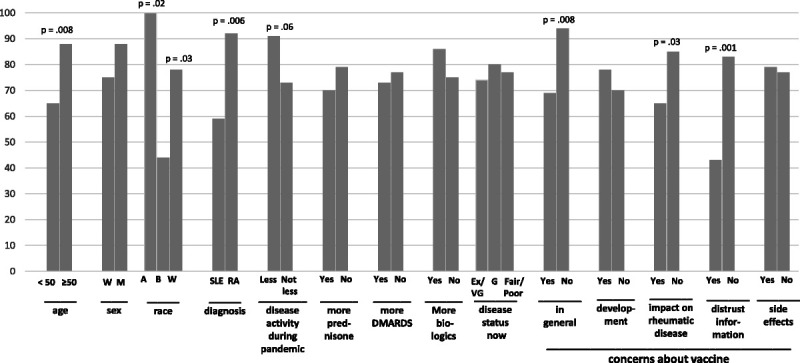
Percent of patients intending to get vaccine according to demographic variables, clinical characteristics, and categories of concerns about vaccine. Abbreviations: for sex: W, women; M, men; for race: A, Asian; B, Black; W, White; for diagnosis: SLE, systemic lupus erythematosus; RA, rheumatoid arthritis; for disease status now: Ex/VG, excellent/very good; G, good.
Willingness to be vaccinated did not vary according to clinical characteristics measured at follow-up, such as occurrence of typical flares, changes in medications since enrollment, current disease status, and satisfaction with medications (Figure). Patients who reported less disease activity during the follow-up period tended to be more likely to plan to be vaccinated compared with patients with the same, more, or unpredictable disease activity (91% vs 73%; OR, 4.0; 95% CI, 0.9–18.5; p = 0.06).
With respect to concerns about the vaccine, having no concerns was associated with a higher proportion intending to be vaccinated (94% vs 69%; OR, 6.4; 95% CI, 1.4–29.7; p = 0.008). Patients concerned about the impact of the vaccine on their rheumatic disease, however, were less likely to intend to be vaccinated (65% vs 85%; OR, 3.3; 95% CI, 1.1–8.0; p = 0.02). Similarly, patients distrustful of vaccine-related information were less likely to intend to be vaccinated (43% vs 83%; OR, 6.5; 95% CI, 1.9–21.6; p = 0.001). Concerns about development/distribution and adverse effects were not associated with intention to be vaccinated.
A multivariable logistic regression model was set up with the dependent variable being not intending/hesitant about vaccination, and independent variables being age younger than 50 years (ie, the mean), Black race, concern about vaccine effects on rheumatic disease/medications, and concern about inaccurate information/distrust. These were the only variables included in the model. After backward stepwise elimination, younger age, concern about effects on rheumatic disease/medications, and concern about inaccurate information/distrust remained associated (Table 4). In subanalysis comparing only patients with lupus or RA, variables that remained associated with not intending to be vaccinated were having lupus, concern about effects on rheumatic disease/medications, and concern about inaccurate information/distrust (p ≤ 0.01 for all comparisons).
TABLE 4.
Bivariate and Multivariable Analyses Associated With Not Intending to Get Vaccine
| Bivariate | Initial Multivariablea | Final Multivariablea | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% CI | p value | Odds Ratio | 95% CI | p value | Odds Ratio | 95% CI | p value |
| Age <50 y | 3.9 | 1.4, 11.1 | 0.01 | 2.7 | 0.9, 8.6 | 0.09 | 3.0 | 1.0, 9.3 | 0.06 |
| Black race | 5.2 | 1.3, 21.2 | 0.02 | 2.3 | 0.4, 14.2 | 0.39 | — | — | — |
| Concerned about vaccine's impact on rheumatic disease | 3.0 | 1.1, 8.0 | 0.03 | 4.1 | 1.3, 13.4 | 0.02 | 3.8 | 1.2, 12.2 | 0.02 |
| Concerned about misinformation about vaccine (distrust) | 6.5 | 1.9, 21.6 | 0.002 | 6.5 | 1.4, 29.6 | 0.02 | 8.6 | 2.2, 34.4 | 0.002 |
aModels were not adjusted for other variables.
DISCUSSION
In our longitudinal study assessing patients with rheumatic diseases and their perspectives on COVID-19, we enrolled patients during the first surge of the pandemic in New York City when mortality rates were highest, and conducted follow-ups when vaccines first became available. Our study increases knowledge of patients' experiences with COVID-19 by juxtaposing perspectives from the start of the pandemic with knowledge subsequently gained as the pandemic unfolded. These evolving perspectives directly impacted intention to be vaccinated.
We found that more than a third of patients reported that during the pandemic their condition had worsened or was unpredictable, that they were taking more medications, and their medications often were changed due to the pandemic. However, most patients were satisfied with the management of medications during the pandemic and most rated their current condition as excellent, very good, or good with only a quarter rating it as fair or poor. Except for associations with age and sex, we did not find clinical variables or perceived vulnerability to infection measured at enrollment to be associated with patient-reported clinical status at follow-up.
What new factors, therefore, emerged during the pandemic that influenced patients' perspectives at follow-up? There are several possibilities. First, although some patients reported physical setbacks during the pandemic, most did not, and instead reported a relatively typical course for their disease. Flares occurred but were treated with or without rheumatologists' input and did not result in urgent care or hospitalization for any patient. With respect to becoming infected with the virus, generally recommended protective measures were effective as most patients had no symptoms and were negative when self-referred for viral and antibody testing. Among those who tested positive, one was hospitalized and the rest treated themselves at home. In addition to these personal experiences, more information about the interaction of rheumatic diseases and medications and COVID-19 outcomes gradually became available and contributed to evolving perspectives.15–18
We conducted our follow-up to coincide with the advent of SARS-CoV-2 vaccines. We found most patients planned to or already had been vaccinated, and the intention to be vaccinated was not associated with perceptions of vulnerability and risk of infection obtained at the start of the pandemic. Instead, demographic characteristics and concerns about the vaccine itself, particularly unknown effects on rheumatic diseases and distrust of information, were the main reasons for reluctance to be vaccinated.
With respect to concerns about rheumatic disease, patients questioned the vaccine's effectiveness in the setting of their abnormal immunological state and the vaccine's potential to trigger flares and interact with medications. These findings are consistent with the few other studies specifically addressing vaccination hesitancy due to rheumatic diseases. For example, in 1 study conducted in India in March to April 2021, 280 patients with diverse rheumatic diseases were interviewed in person and asked about their perceptions about the vaccine.19 About half were willing to be vaccinated (54%). Among those uncertain or unwilling to be vaccinated, the main reasons were no need for vaccination, fear of adverse effects, and fear of worsening rheumatic disease symptoms. There were no differences among groups based on duration of disease or treatment. In another study conducted in the Netherlands in December 2020 with online questionnaires, 61% of over 1300 patients with diverse rheumatic diseases were willing to be vaccinated.14 Willingness was more common in older patients and was not associations with use of medications. Uncertainty and unwillingness to be vaccinated were associated with concerns about adverse effects and the potential to worsen autoimmune disease symptoms. Interestingly, most patients who were uncertain or unwilling reported they would change their opinion if specifically advised by a physician. Similar findings were reported in an international Web-based study, also conducted in December 2020, with over 1500 self-reported rheumatic disease patients that found 46% were unwilling to be vaccinated but most would reconsider if recommended by a specialist.20 Unlike these studies that found no associations with diagnosis, in our study, we found greater vaccination reluctance if patients had lupus versus rheumatoid arthritis (after controlling for age). This result, however, was based on a subanalysis, and the small sample size precluded controlling for other clinical variables.
Distrust about information was another main vaccination concern in our study. This also has been previously reported, particularly in large surveys among the general US population. For example, in the interview-based AmeriSpeak survey from April 2020 with over 900 individuals, 42% were unsure or did not intend to be vaccinated; for those who gave a reason, not trusting entities involved in the development and dissemination of the vaccine was a main reason.7 In the more recent Internet-based Understanding America Study from March 2021, 35% of the over 6000 surveyed individuals were hesitant about obtaining the vaccine and 3% cited distrust, particularly in governmental processes to ensure safety.8 Results of our study agree with these large US population–based studies finding that distrust was more prevalent among individuals who were Black and younger. Unlike other studies, however, we did not compare vaccination intent with other sociodemographic characteristics such as income and education.7,8,19
Finally, we found that rheumatologists and other physicians were not the main sources of information about vaccines. Instead, patients relied more on social media and social networks rather than on their physicians for information. This pattern also was reported in a Web-based study from early 2021 with over 700 patients with diverse rheumatic diseases in which most patients were undecided about the vaccine.21 Given that the impact of the vaccine on rheumatic disease was a major concern for vaccination in our study and the studies cited previously, rheumatologists should play an increasingly important future role in guiding patients about SARS-CoV-2 boosters and other vaccines.19 As more is learned about COVID-19 and vaccines in rheumatic diseases, more comprehensive and consistent messaging will be possible from health care providers which, in turn, may address issues of distrust and uncertainty.
This study has several limitations. First, it was conducted with patients from a tertiary care rheumatic disease center, and their perspectives may differ from patients in other settings. Also, patients with diagnoses that were not treated with immunosuppressive medications, such as osteoarthritis, were not included. Second, patients were continuously enrolled during the first surge of the pandemic, and recruitment ceased when rates of infection and morality began to decline. Thus, the sample size was restricted by the narrow duration of the enrollment period. Third, the follow-up period also was temporally restricted to coincide with when the vaccine first became available to patients based on age and comorbidity. Thus, patients who were not available to be interviewed during this period were not included. Fourth, to decrease response burden during follow-up interviews, we minimized questions about covariates that might have contributed to the understanding of some of our findings. Fifth, although most patients reported a relatively typical pattern of rheumatic disease symptoms during the pandemic, approximately one quarter had worse disease activity. Other aspects of physical and mental health that may have contributed to worse clinical status in this group were not assessed in subanalyses.
In this longitudinal study, we found that patients' perspectives of increased risk for SARS-CoV-2 infection due to rheumatic diseases obtained during the first surge of the pandemic were not associated with subsequent assessments of clinical status and change in medications obtained several months later when vaccines first became available. In addition, perspectives regarding risk of infection and assessments of clinical status and medication change were not associated with willingness to be vaccinated. Instead, hesitancy to be vaccinated was associated with concerns about the effects of the vaccine on rheumatic disease symptoms and distrust in vaccine information. Rheumatologists and other physicians were not the main sources of information about the vaccine. Our study reflects the evolving nature of patients' perspectives regarding COVID-19, as well as the need for rheumatologists to identify and treat patients who deteriorate clinically, and counsel all patients regarding vaccination.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Antonelli A Fallahi P Elia G, et al. Effect of the COVID-19 pandemic on patients with systemic rheumatic diseases. Lancet Rheumatol. 2021;3:e675–e676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kapteyn A Angrisani M Bennett D, et al. Tracking the effect of the COVID-19 pandemic on American households. Survey Res Methods. 2020;14:179–186. [Google Scholar]
- 3.Hausmann JS Kennedy K Simard JF, et al. Immediate effect of the COVID-19 pandemic on patient health, health-care use, and behaviours: results from an international survey of people with rheumatic diseases. Lancet Rheumatol. 2021;3:e707–e714. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leese J Backman CL Ma JK, et al. Experiences of self-care during the COVID-19 pandemic among individuals with rheumatoid arthritis: a qualitative study. Health Expect. 2021. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adnine A Soussan I Nadiri K, et al. Patients with rheumatic diseases overlooked during COVID-19 pandemic: how are they doing and behaving. Curr Rheumatol Rev. 2021;17:318–326. [DOI] [PubMed] [Google Scholar]
- 6.Garrido-Cumbrera M Marzo-Ortega H Christen L, et al. Assessment of impact of the COVID-19 pandemic from the perspective of patients with rheumatic and musculoskeletal diseases in Europe: results from the REUMAVID study (phase 1). RMD Open. 2021;7:e001546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher KA Bloomstone SJ Walder J, et al. Attitudes toward a potential SARS-CoV-2 vaccine. Ann Intern Med. 2020;173:964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daly M, Jones A, Robinson E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020 to March 29, 2021. JAMA. 2021;325:2397–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duculan R Jannat-Khah D Mehta B, et al. Variables associated with perceived risk of contracting SARS-CoV-2 infection during the COVID-19 pandemic among patients with systemic rheumatic diseases. J Clin Rheumatol. 2021;27:120–126. [DOI] [PubMed] [Google Scholar]
- 10.Mancuso CA Duculan R Jannat-Khah D, et al. Modifications in systemic rheumatic disease medications: patients' perspectives during the height of the COVID-19 pandemic in New York City. Arthritis Care Res (Hoboken). 2021;73:909–917. [DOI] [PubMed] [Google Scholar]
- 11.Mancuso CA Duculan R Jannat-Khah D, et al. Rheumatic disease–related symptoms during the height of the COVID-19 pandemic. HSS J. 2020;16(Suppl 1):S36–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang XA, Duculan R, Mancuso CA. Coping mechanisms mitigate psychological stress in patients with rheumatologic diseases during the COVID-19 pandemic. J Clin Rheumatol. 2021. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.ACR COVID-19 Vaccine Clinical Guideline Task Force . COVID-19 vaccine guidance summary for patients with rheumatic and musculoskeletal diseases. American College of Rheumatology. February 8, 2021. Available at: https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf. Accessed October 12, 2021. [Google Scholar]
- 14.Boekel L Hooijberg F van Kempen ZLE, et al. Perspective of patients with autoimmune diseases on COVID-19 vaccination. Lancet Rheumatol. 2021;3:e241–e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed S, Zimba O, Gasparyan AY. COVID-19 and the clinical course of rheumatic manifestations. Clin Rheum. 2021;40:2611–2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monti S Balduzzi S Delvino P, et al. Clinical course of COVID-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis. 2020;79:667–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gianfrancesco MA, Robinson P. Changing COVID-19 outcomes in patients with rheumatic disease—are we really getting better at this? Lancet Rheumatol. 2021;3:E88–E90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jorge A D'Silva KM Cohen A, et al. Temporal trends in severe COVID-19 outcomes in patients with rheumatic disease: a cohort study. Lancet Rheumatol. 2021;3:e131–e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaur P, Agrawat H, Shukla A. COVID-19 vaccine hesitancy in patients with systemic autoimmune rheumatic disease: an interview-based survey. Rheumatol Int. 2021;41:1601–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Felten R Dubois M Ugarte-Gil MF, et al. Vaccination against COVID-19: expectations and concerns of patients with autoimmune and rheumatic diseases. Lancet Rheumatol. 2021;3:e243–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yurttas B Poyraz BC Sut N, et al. Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in Turkey: a web-based survey. Rheumatol Int. 2021;41:1105–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]


