Abstract
Objective:
Veterans who served in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) commonly experience alcohol misuse and symptoms of posttraumatic stress disorder (PTSD) following deployment. We conducted a randomized clinical trial to evaluate the efficacy of a newly developed, eight-module, self-management Web intervention (VetChange) based on motivational and cognitive-behavioral principles to reduce alcohol consumption, alcohol-related problems, and PTSD symptoms in returning combat Veterans.
Methods:
Six hundred participants, recruited through targeted Facebook ads, were randomized to either an Immediate Intervention Group (IIG, n = 404) or a Delayed Intervention Group (DIG, n =196) that waited eight weeks for access to VetChange. Primary outcome measures were Drinks per Drinking Day, Average Weekly Drinks, Percent Heavy Drinking Days and PTSD symptoms. Intent-to-treat analyses compared changes in outcome measures over time between IIG and DIG, as well as within-group changes.
Results:
IIG participants demonstrated greater reductions in drinking (p < .001 for each measure) and PTSD symptoms (p = .009) between baseline and end-of-intervention than did DIG participants between baseline and the end of the waiting period. DIG participants showed similar improvements to those in IIG following participation in VetChange. Alcohol problems were also reduced within each group between baseline and three-month follow-up.
Conclusions:
Results indicate that VetChange is effective in reducing drinking and PTSD symptoms in OIF/OEF Veterans. Further studies of VetChange are needed to assess Web-based recruitment and retention methods and to determine VetChange’s effectiveness in demographic and clinical sub-populations of returning Veterans.
Keywords: Veterans, Alcohol abuse, PTSD, Web, Internet
Alcohol misuse is a major problem among men and women who served in Afghanistan (Operation Enduring Freedom; OEF) and Iraq (Operation Iraqi Freedom; OIF). For example, investigators report 12% to 36% of OEF/OIF Active Duty or National Guard and Reserve personnel are engaging in alcohol misuse following deployment (Burnett-Zeigler et al., 2011; Hoge et al., 2004; Milliken, Auchterlonie, & Hoge, 2007; Wilk et al., 2010). In addition, among Veterans seeking outpatient services at the Veterans Health Administration (VHA), one study found evidence of alcohol misuse among 6% of female and 23% of male Veterans (Hawkins, Lapham, Kivlahan, & Bradley, 2010), while another reported finding alcohol misuse in 40% of a sample of returning Veterans (Calhoun et al., 2008). Research also indicates that OEF/OIF military personnel with combat exposure may develop a range of new onset problem drinking behaviors (e.g., binge or weekly heavy drinking) following deployment (Jacobson et al., 2008).
Recent studies also provide evidence for high rates of posttraumatic stress disorder (PTSD), a potential psychological response to combat exposure (Weathers, Keane & Foa, 2009), among OEF and OIF Veterans following deployment. Estimated rates of PTSD among Active Duty, National Guard or Reserve personnel, and Veterans seeking services in the VHA range from 12% to 30% (Hoge et al., 2004; Seal et al., 2009; Thomas et al., 2010). Studies with previous generations of combat Veterans indicate that alcohol problems and PTSD are highly co-morbid (Keane & Kaloupek, 1997) and a similar pattern of co-morbidity is emerging in returning Veterans (McDevitt-Murphy et al., 2010; Thomas et al., 2010). It has been suggested that combat Veterans may use alcohol to diminish traumatic memories of war or alleviate other symptoms of PTSD (Jacobson et al., 2008; Keane & Kaloupek, 1997).
Many returning Veterans with alcohol or other mental health problems are not receiving the care that is needed to facilitate a full recovery from these problems (Hoge et al., 2004; Milliken et al., 2007). This is due in part to the reluctance of returning Veterans to seek services as a result of concerns about stigma, but is also related to logistical factors that can impede access to care (e.g., inconvenience of attending appointments or living in a remote geographical area with limited services [Burnett-Zeigler et al., 2011; Hoge et al., 2004; McLean, Steenkamp, Lev, & Litz, 2009; Milliken et al., 2007]). With nearly 2.3 million Veterans deployed during OEF/OIF/OND conflicts, there is an urgent need to find new ways to reach a new generation of combat Veterans who need services.
Web-based treatments offer a promising venue for both reaching and intervening with OEF and OIF Veterans. Web programs are able to address some of the most salient barriers to care reported by this population, offer standardized behavioral health care in locations where this is not available, and have the potential to reach a far greater number of Veterans than is feasible through in-person modalities (Amstadter et al., 2009; Bennett and Glasgow, 2009; Cucciare, Weingardt, & Humphreys, 2009; Hester et al., 2009).
Several controlled trials indicate that self-management Web interventions are effective for problem drinkers. Specifically, Web interventions based on motivational and cognitive-behavioral principles lead to greater reductions in drinking than online alcohol education (Riper et al., 2007), alcohol prevention programs (Pemberton et al., 2011), and wait list groups (Blankers, Koeter, & Schippers et al., 2011; Pemberton et al., 2011). A Web-based Moderate Drinking protocol added to online Moderation Management (MM) is also more effective in reducing drinking than MM alone (Hester, et al., 2009). Finally, results of a meta-analysis of nine randomized clinical trials confirm the effectiveness of self-management Web interventions for problem drinkers (Riper et al., 2011).
There is also a growing evidence base for the effectiveness of Web interventions for PTSD, including among Veterans. For example, Litz, Engel, Bryant, & Papa (2007) compared the efficacy of a cognitive-behavioral (CBT) Web intervention (including exposure therapy and therapist contact) to Web-based supportive counseling (SC) in a sample of Department of Defense (DOD) service members with PTSD related to the Pentagon attack on 9/11 and OEF and OIF military personnel with PTSD. Although both interventions led to a reduction in PTSD symptoms, there was a sharper decline in symptoms following the CBT than the SC condition.
While investigators are making progress in developing effective Web interventions, a significant limitation of existing programs is that they do not sufficiently address common co-morbidities (Amstadter, 2009). It may be especially important to address the co-occurring nature of alcohol problems and PTSD among OEF/OIF Veterans (Thomas et al., 2010) in order to help them reduce drinking. Integrated treatments for co-morbid alcohol misuse and PTSD are widely accepted in the treatment community and may optimize treatment outcomes (Najavits et al., 2009).
In this paper, we report results of the first randomized clinical trial to evaluate the efficacy of a newly developed Web intervention (VetChange) for OEF and OIF Veterans with problem drinking. Our primary aim was to determine whether a self-management Web intervention, tailored specifically to the returning Veteran population and their post-deployment experiences, would lead to reductions in drinking. As we expected that many Veterans would have PTSD symptoms associated with recent combat exposure, we were also interested in intervening with and examining the impact of the intervention on PTSD symptoms.
Consistent with other empirically supported interventions for problem drinkers (Finney, Wilbourne, & Moos, 2007; Hester et al., 2009), VetChange provided skills training to improve coping with a broad range of potential high risk situations for drinking, including symptoms of PTSD. We designed our Web intervention as a fully computer-automated intervention in order to maximize our potential to reach a large population of returning Veterans, some of whom might not be connected to a health care system (Bennett & Glasgow, 2009). Similar to pragmatic controlled trials, the study was designed to maximize recruitment of a sample of Veterans highly representative of the larger, diverse Veteran population (Zwarenstein et al., 2008). Finally, we selected two important outcomes related to long-term morbidity and mortality in returning Veterans, alcohol consumption and PTSD, to determine the significance of our outcomes for this new cohort of combatVeterans.
Methods
Participants
Six hundred OEF and OIF Veterans were randomized into the study. Eligibility criteria included: (a) self-reported status as OEF or OIF veteran, (b) age between 18 and 65 years, (c) score on the Alcohol Use Disorders Identification Test (AUDIT; Babor, de la Fuente, Saunders, & Grant, 1992; Bradley et al., 2003) between 8 and 25 for men and 5 and 25 for women, (d) drinking above guidelines for safer drinking during the 30 days prior to screening based on the Quick Drink Screen (no more than 4 drinks per occasion or 14 drinks per week for men and no more than three drinks per occasion or seven drinks per week for women; Dawson, Grant, & Li, 2005; USDHHS & USDA, 2010), and (e) willing to provide an email address for reminders and incentives.
Recruitment and Randomization
We recruited participants through targeted Facebook advertising. Due to high rates of attrition in Web interventions (Eysenbach, 2005) we set a recruitment goal of 600 participants to ensure sufficient power for significance tests. Over 46 recruiting days, approximately 11,000 individuals visited the Website, approximately 3,500 were assessed for eligibility, approximately 1,340 were determined to be eligible, and 617 participants were randomized (Figure 1). If participants were eligible, they provided informed consent prior to randomization using an IRB approved Web consent form. Ten participants were excluded following randomization in response to protocols designed to detect likely-invalid enrollments1, and seven were excluded due to incomplete baseline data. For more details on strategies to minimize misrepresentation in VetChange enrollment see Kramer, Rubin, Coster, et al. (in press).
Figure 1.
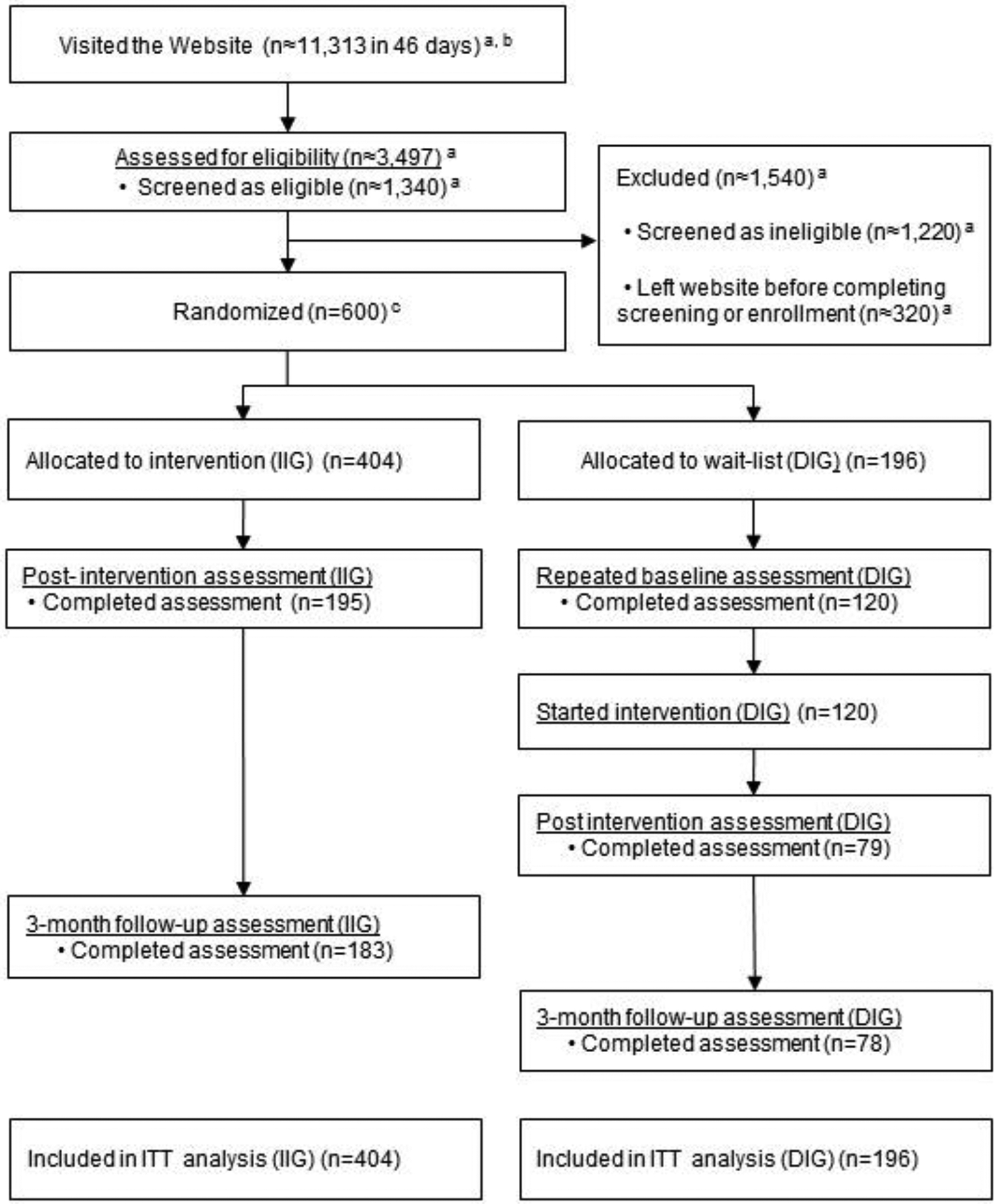
Flowchart of participants through the trial
a Approximate figures derived from web analytics estimates. Subject data records not created until study enrollment. b Most web visitors (N ≈ 7,816) left without initiating eligibility screening. c A total of 617 subjects were randomized, but 17 were excluded from analysis as potentially fraudulent (n=10) or incomplete baselines (n=7).
A final sample size of 600 included 404 participants randomized to an Initial Intervention Group (IIG), which had immediate access to the intervention and 196 participants to a Delayed Intervention Group (DIG), which had access to Vetchange after an eight week delay. Based on their IP addresses, we determined that our participants included OEF and OIF Veterans from across the United States (primarily) and a small number of Veterans from overseas locations where military bases are located.
Randomization was stratified by gender to ensure an equal number of women across groups. Twice as many participants were assigned to IIG as DIG so that we could offer immediate access to the Web intervention to as many participants as possible within the shortest period of time. This was done both for ethical reasons (Helsinki Accords, World Medical Association, 2008) and to enhance participation.
General Procedures
The Institutional Review Boards (Boston University and VA Boston Healthcare System) approved all study procedures. IIG participants completed three assessments: 1) at baseline prior to randomization, 2) at the end of the intervention, and 3) at three months post-intervention. DIG participants completed four assessments: 1) at baseline prior to randomization, 2) at the end of the eight week waiting period (repeated baseline assessment), 3) at the end of the intervention, and 4) at three months post-intervention (Figure 2). Participants received Amazon gift codes via email of $20 for each of the assessments and a bonus of $25 for completing all assessments. All assessments were administered on the Web. Automated email reminders were sent to participants throughout the study to improve retention and encourage completion of assessments. Participants could receive up to 31 (IIG) or 36 (DIG) emails during the study for various reasons (e.g., acknowledgment of completion of a module or as a reminder of a pending assessment).
Figure 2.
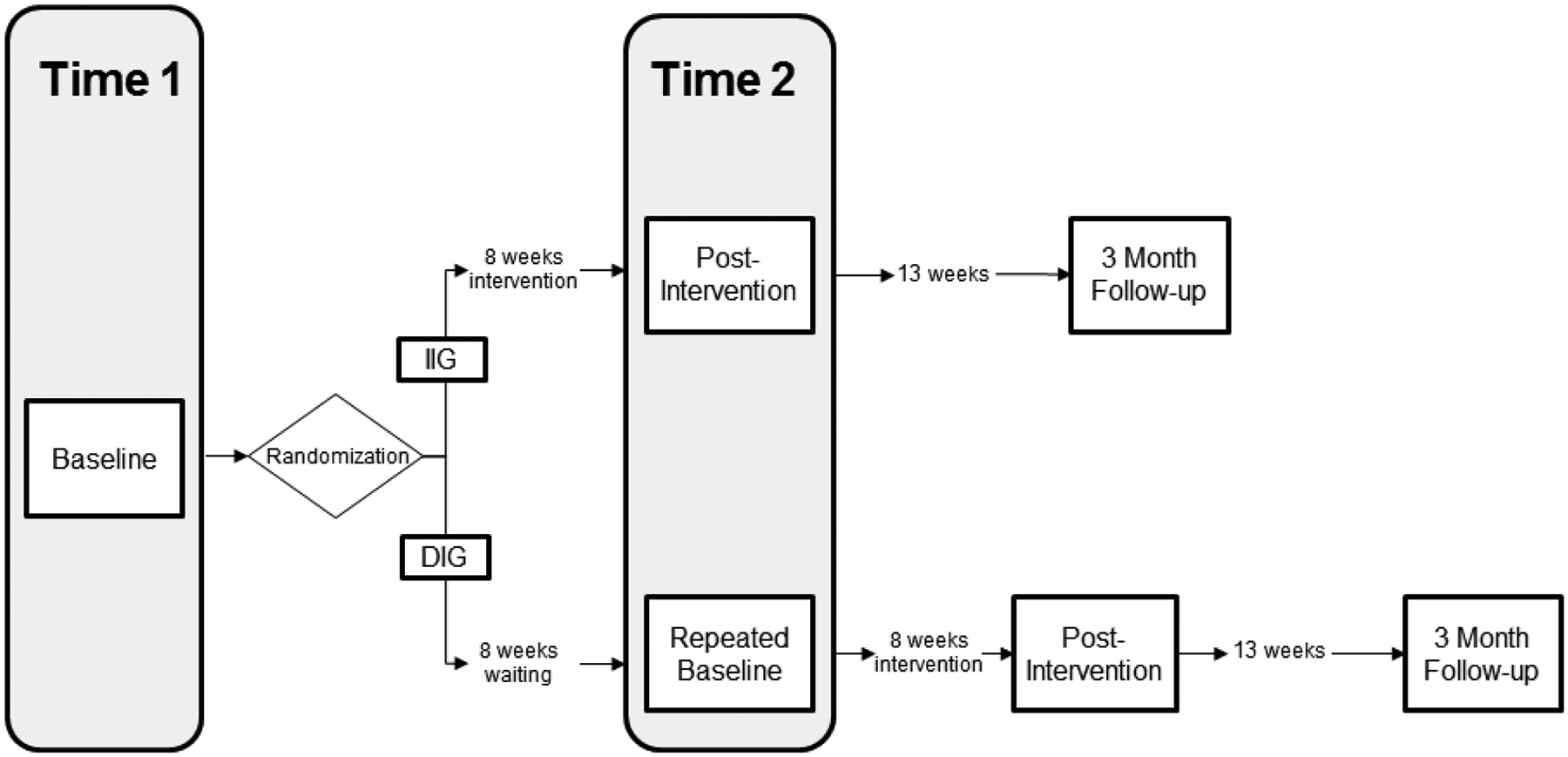
Assessment timeline
Note. IIG = Initial Intervention Group, DIG = Delayed Intervention Group, Time1 = initial baseline for both groups. Time2 = post-intervention assessment for IIG and repeated baseline for DIG.
Assessment Measures
The Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992) is a 10-item self-report measure of alcohol use and alcohol-related problems. Items are scored from 0 to 4, and summed to yield a composite score ranging from 0 to 40. The AUDIT cutoff scores yield a sensitivity of .71 and specificity of .85 based on a Veteran sample (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998). Across 18 studies, Reinert and Allen (2007) calculated a median reliability coefficient of .83.
The Quick Drink Screen (QDS; Sobell et al., 2003) is a four-item self-report measure of alcohol consumption focused on quantity and frequency of drinking in the last 30 days. The scale is considered a valid and expedient method for collecting data on alcohol use. The QDS and TimeLineFollowBack intraclass correlation coefficients over one year range from .65 to .82 (Sobell et al., 2003). All alcohol consumption variables in this study are derived from the QDS.
The Short Inventory of Problems (SIP-2R) is a 15-item self-report measure of alcohol-related problems (Miller et al., 1995). Participants indicate how often each of the consequences occurred during the past three months on a scale of 0–3. The overall problem severity score was used in analyses. The SIP demonstrates good internal consistency (Cronbach’s alpha = .95; Kenna et al., 2005) and test-retest reliability (r = .89; Miller, Tonigan & Longabaugh, 1995).
The Combat Experiences Scale of the Deployment Risk and Resilience Inventory (CES-DRRI; King, King, & Vogt, 2003) is a 15-item self-report scale that measures exposure to combat experiences in a yes/no format. The Kuder-Richardson 20 coefficient alpha for the scale was .85 in a study with troops representing Army, Navy, Air Force, Marines and Coast Guard branches of the military who had served in Gulf War I (Vogt, King, & King, 2004). The CES-DRRI has good internal consistency (alpha = .85; King, King, Vogt, Knight & Samper, 2006).
The PTSD Checklist (PCL-5; Weathers et al., 2010) is a 20-item self-report measure of PTSD symptoms. Items correspond to the newly approved PTSD symptom criteria in the Diagnostic and Statistical Manual of Mental Disorders-Fifth Version (DSM-5). Symptom categories in DSM-5 include re-experiencing, avoidance, negative alterations of cognitions and moods, and hyperarousal. Participants anchor responses to “stressful life experiences” on a scale of 0 to 4 (2 or greater is considered a positive symptom). The original PCL, a 17-item self-report measure corresponding to the DSM-IV criteria for PTSD (Weathers, Litz, Herman, Huska, & Keane, 1993) demonstrated excellent reliability and validity across trauma populations (Weathers & Ford, 1996). The psychometrics of the PCL-5 are currently being evaluated. Across two studies, both with Veterans from multiple conflicts, total PCL and PCL-5 scores were highly correlated (r = 0.88 and 0.97), and the PCL-5 demonstrated high levels of internal consistency (alphas = 0.97 and 0.95). In addition, evidence for good convergent validity (r = 0.75 with the Clinician Administered PTSD Scale-IV) was found (B. Marx, personal communication, March 21, 2013).
The AUDIT (eligibility) and CES (baseline) were administered once. The QDS was administered at screening (eligibility) and all other assessment time points. The PCL-5 was administered at baseline, end of the intervention, and three months post-intervention. The SIP was administered at baseline and three months post-intervention.
Intervention
VetChange is designed to motivate Veterans to make changes in drinking and to develop skills necessary to reduce drinking to a safer level (either moderation or abstinence). To achieve these goals, VetChange incorporates elements of evidence-based care for problem drinkers including motivational, cognitive-behavioral, and self-control training strategies (Miller & Munoz, 2005; Miller & Wilbourne, 2002; Sobell & Sobell, 1996). In Modules 1–3 participants receive personalized feedback on drinking and PTSD symptoms, evaluate the importance of and readiness to change, weigh pros and cons of change, set drinking goals, develop a change plan, and review moderation or abstinence strategies (depending on their goal). In Module 4 participants are introduced to external high risk situations for drinking (e.g., social situations, environmental reminders of combat) and develop adaptive coping plans to manage these situations.
In Modules 5–7 VetChange focuses on helping Veterans learn a combination of cognitive and behavioral strategies to manage a range of internal high risk situations for drinking. Topics include mood management, stress management, anger management, and sleep hygiene. In Modules 6 and 7 participants are encouraged to select topics most relevant to their personal situation. This approach is consistent with symptom management approaches for trauma survivors (e.g., Chemtob, Novaco, Hamada, & Gross, 1997; Zlotnick et al., 1997). Module 8 focuses on building a support system to assist with recovery efforts following completion of VetChange.
The Web intervention is designed to be used as a self-management program without the required involvement of a therapist. Participants were allowed eight weeks to complete all modules with access to one new module per week, except in Week 1 during which use of Modules 1 and 2 was recommended. The estimated module completion time was 20 minutes. Home exercises and self-monitoring are essential components of VetChange. Participants receive tailored feedback in each module related to progress in meeting drinking goals and developing effective coping plans, and can click on a Resources page at any time for information on face-to-face treatment (for more information on VetChange see Brief, Rubin, Enggasser, Roy, & Keane, 2011).
Analyses
All analyses were conducted with either the SPSS statistics package (Version 18) or SAS (Version 9.2). The significance level for all statistical tests was set at a two-tailed p = .05 level of significance unless otherwise specified. Preliminary data analyses included examination of dependent variables for skewness and kurtosis, with the natural log transformation used for Drinks per Drinking Day (DDD) and Average Weekly Drinks (AWD) and the square root transformation used for Percent Heavy Drinking Days (PHDD) across all time points. To determine whether there were baseline differences between IIG and DIG participants, we conducted one-way analyses of variance (ANOVA) or Gamma regression analyses (for skewed count variables) comparing all continuous demographic and outcome variables at baseline and chi-square or Fisher’s Exact tests to compare categorical measures. The same analyses were used to examine differences between participants who completed both Time1 and Time2 assessments and those who dropped out.
We took an intent-to-treat (ITT) approach to primary analyses comparing IIG to DIG between Time1 and Time2, and to the within-group analyses examining change over time. All randomized participants were included in primary analyses. The primary outcomes were analyzed using mixed effect models (“PROC MIXED” in SAS) testing specific hypotheses with linear contrasts. Both slope and intercept were treated as random factors, allowing each individual to have different time trajectories. First, we ran mixed effect models for the four outcome measures comparing treatment effects between IIG and DIG groups from Time1 to Time2. Time1 to Time2 represents the eight-week interval following randomization during which IIG participants had access to the intervention and DIG participants were waiting for access to VetChange (Figure 2). The interaction term between time and study group was used to quantify the treatment effect. We examined changes in SIP scores from Time1 to three month follow-up assessments only using mixed effect models.
To address study attrition we conducted a non-parametric test examining assumption of missingness completely at random (MCAR; Diggle, Heagerty, Liang & Zeger, 2002). The test yielded possible violations of the MCAR assumption. We then conducted a sensitivity analysis using multiple imputations technique of primary outcomes to examine potential bias due to loss to follow-up (Rubin, 1976; 1987). For participants missing Time2 data, Time2 responses were imputed for DDD (on the natural log scale), AWD (on the natural log scale), PHDD (with a square root transformation), and PCL-5 total scores using a regression approach to imputation in ‘PROC MI’ in SAS. Imputed values were based on baseline (Time1) levels of drinking variables, age, gender, baseline AUDIT score, and an indicator for previous alcohol-related treatment. Data were imputed separately for DIG and IIG. Five imputed data sets were generated, and composite results across the imputed data sets were calculated using ‘PROC MIANALYZE’ SAS.
Results
Participant Characteristics
There were no significant differences between IIG and DIG participants on demographic measures or variables related to military service (branch of service, location of deployment, and number and length of deployments, see Table 1). The majority (61.8%) of participants reported involvement in treatment (inpatient, residential, or outpatient counseling, medication, and/or self-help group) during the three months prior to the study. The majority of those who reported treatment involvement indicated this was for mental health (59.6%) or problems with both mental health and substance use (32.6%). Nearly 80% of participants who reported treatment involvement indicated some focus on PTSD. There were no differences between groups in the number of participants who were in treatment during the three months prior to the intervention (Fisher’s exact test, p = .37).
Table 1.
Demographics by Group
| Variable | IIG (n = 404) % (n) |
DIG (n =196) % (n) |
χ 2 | p |
|---|---|---|---|---|
| Gender (% Male) | 86.1% (348) | 86.7% (170) | 0.04 | 0.842 |
| Race/Ethnicity | 3.503 | 0.744 | ||
| White | 79% (319) | 80.1% (157) | ||
| Hispanic/Latino | 10.1% (41) | 8.7% (17) | ||
| African American/Black | 4% (16) | 5.1% (10) | ||
| Asian American/Pacific Islander | 1% (4) | 1% (2) | ||
| American Indian/Native Alaskan | 1.7% (7) | 2% (4) | ||
| Branch | 2.861 | 0.721 | ||
| Army | 58.7% (237) | 56.6% (111) | ||
| Marines | 17.8% (72) | 15.8% (31) | ||
| Air Force | 5.7% (23) | 4.6% (9) | ||
| Navy | 6.2% (25) | 9.2% (18) | ||
| Theater | ||||
| Iraq | 82.7% (334) | 85.2% (167) | 0.614 | 0.433 |
| Afghanistan | 30.2% (122) | 30.1% (59) | 0.001 | 0.981 |
| Reported Treatment in Past 3 Months (% Yes) | 63.1% (255) | 59.2% (116) | 0.866 | 0.352 |
| M (SD) | M (SD) | χ 2 | p | |
| Total Tours | 2.2 (1.9) | 2.2 (1.6) | 0.009 | 0.926 |
| Total Months Deployed | 19.0 (14.3) | 20.0 (15.7) | 1.169 | 0.280 |
| M (SD) | M (SD) | F | p | |
| Age | 32 (7.8) | 32.1 (7.7) | 0.033 | 0.856 |
There were no significant differences between IIG and DIG participants on baseline drinking measures (Table 2). An average AUDIT score of 17.7 (SD = 4.7) for the sample indicates that participants were primarily engaging in “harmful or hazardous drinking” although those above 20 may have had symptoms of “alcohol dependence” based on AUDIT guidelines (Babor et al, 1992). Men were drinking an average of 7.43 (SD = 3.75) DDD and 29.1 (SD = 18.7) AWD, while women were drinking an average of 4.68 (SD = 2.47) DDD and 18.4 (SD = 14.2) AWD. Approximately one third of baseline drinking days were heavy drinking days. Alcohol consumption variables were highly skewed at baseline (Table 3); these variables were transformed for analyses to normalize their distributions at all time points. Study participants reported a moderate level of alcohol-related problems on the SIP at baseline (Miller, et al. 1995).
Table 2.
Time 1 (Baseline) Assessment Results by Group
| Variable | IIG (n=404) M(SD) |
DIG (n=196) M(SD) |
p |
|---|---|---|---|
| AUDIT | 17.7 (4.8) | 17.6 (4.7) | .845 |
| Log Average Drinks per Drinking Day | 1.99 (0.46) | 1.97 (0.45) | .365 |
| Log Average Drinks per Week | 3.14 (0.73)4 | 3.11 (0.75) | .212 |
| SQRT Percent Heavy Drinking Days | 0.54 (0.24) | 0.53 (0.24) | .108 |
| SIP | 17.6 (8.2) | 17.0 (8.0) | .427 |
| PCL-5 | 41.5 (19.5) | 39.4 (18.7) | .218 |
| DRRI-CES | 7.9 (4.2) | 8.3 (4.0) | .257 |
Note: IIG = Immediate Intervention Group, DIG = Delayed Intervention Group, AUDIT = Alcohol Use Disorders Identification Test, SIP=Short Inventory of Problems, PCL-5 = PTSD Checklist for DSM-5, DRRI-CES = Combat Experiences Scale of the DRRI.
Table 3.
Median and Interquartile Range for untransformed outcome variables at each time point for IIG and DIG
| IIG | DIG | ||||||
|---|---|---|---|---|---|---|---|
| T1 (n=404) Md(IQR) |
T2 (n=195) Md(IQR) |
3-Month (n=183) Md(IQR) |
T1 (n=196) Md(IQR) |
T2 (n=120) Md(IQR) |
Post (n=79) Md(IQR) |
3-Month (n=78) Md(IQR) |
|
| DDD | 6 (4, 10) | 4 (2, 6) | 3 (2, 5) | 6 (4, 9) | 5 (4, 8) | 4 (3, 6) | 3 (2, 4) |
| AWD | 24 (15, 36) | 10 (6, 20) | 6 (2, 15) | 24 (12, 36) | 15 (10, 28) | 12 (5, 21) | 6 (2, 15) |
| PHDD | .267 (.1, .5) | 0.1 (0.033, .2) | .03 (0, .133) | .267 (.13, .5) | 0.167 (.067, .333) | 0.13 (0.03, .267) | 0.03 (0, .167) |
| PCL | 41 (26, 56) | 33 (18, 50) | 32 (18, 48) | 40 (24, 53) | 37 (21.5, 54.8) | 33 (14, 53) | 27 (11, 43.5) |
Note. IIG = Immediate Intervention Group, DIG = Delayed Intervention Group, DDD = drinks per drinking day, AWD = average drinks per week, PHDD = percent heavy drinking days, PCL-5 = PTSD Checklist for DSM-5.
There were no differences between groups in combat exposure or baseline total PCL-5 scores. Both male and female Veterans were exposed to combat although men were exposed to a greater diversity of events (M = 8.5, SD = 4.1) than women (M = 4.8, SD = 3.3). There was a wide range of PTSD symptom severity in the sample at baseline, with total PCL-5 scores ranging from 0 to 80 and normally distributed with a median of 40. The average total PCL-5 score at baseline for the sample was 40.8 (SD = 19.3). Average total PCL-5 scores at baseline were similar for men (M = 41.0, SD = 19.3) and women (M = 39.6, SD = 19.0).
Cutoff scores for probable PTSD diagnoses are not yet available for the PCL-5. However, based on the symptom cluster method (i.e., participants met criteria for at least one re-experiencing and one avoidance symptom, and at least two symptoms of negative alterations of cognitions or moods and hyperarousal), approximately 62% of IIG and 59% of DIG participants met DSM-5 criteria for PTSD at baseline. The average total PCL-5 score for those who met criteria was 52.7 (SD = 13.4) while the average score for those who did not meet criteria based on this method was 22.4 (SD = 10.7).
Attrition
Forty-eight percent (n = 195) of IIG and 61% (n = 120) of DIG participants completed Time2 assessment. Participants with higher AUDIT scores (p < .01), higher average DDD (p < .05), higher AWD (p < .01), and higher PHDD (p < .01) at baseline were less likely to complete the Time2 assessment. Approximately 40% of participants randomized to IIG (n=161) and DIG (n=78) returned for all assessments including the three month follow-up.
Primary Outcomes Comparing IIG and DIG Changes from Time1 to Time2
Table 3 provides medians and interquartile ranges for outcome variables across all time points and Table 4 shows the results of mixed effects model analysis for the primary outcomes. Participants in IIG demonstrated a significantly greater reduction in DDD (B = −.387, SE=.063, p < .0001), AWD (B = −.597, SE = .105, p< .0001), PHDD (B = −.122, SE = .027, p < .0001), and PTSD symptoms (B = −5.577, SE = 1.67, p = .009) during the intervention compared to DIG participants during their waiting period. A similar analysis with treatment involvement as a covariate provided virtually identical findings for between group analyses from Time1 to Time 2 for DDD (B = −.387, SE=.063, p < .0001), AWD (B = −.601, SE = .105, p <, .0001), PHDD (B = −.124, SE = .027, p < .0001), and PTSD symptoms (B = −4.469, SE = 1.74, p = .0076).
Table 4.
Results of random effects mixed models comparing changes in the Initial Intervention Group to the Delayed Intervention Group across the first two time points
| Ln(DDD)a | Ln(AWD)a | Sqrt(PHDD)b | PCL-5 | |
|---|---|---|---|---|
| Estimate(SE) | Estimate(SE) | Estimate(SE) | Estimate(SE) | |
| Time | −0.306(0.032)* | −0.523(0.052)* | −0.137(0.014)* | −5.519(0.834)* |
| Group | 0.024(0.040) | 0.030(0.064) | 0.007(0.021) | 2.069(1.677) |
| Group × Time | −0.387(0.063)** | −0.597(0.105)** | −0.122(0.027)** | −5.577(1.668)*** |
Note: DDD = drinks per drinking day, AWD = average drinks per week, PHDD = percent heavy drinking days, PCL-5 = PTSD checklist for DSM-5.
variables transformed on natural log scale,
variable transformed on square root scale
p < .001,
p < .0001,
p = .009
The multiple imputation analyses yielded results similar to those provided by the mixed effects model based on all available data ITT findings. IIG participants demonstrated a significantly greater reduction in DDD (B = −.45, SE =.11, p < .001)), AWD (B = −.56, SE = .10, p < .001), PHDD (B = −.08, SE =.02, p < .001), and PTSD symptoms (B = −5.19, SE = 1.52, p = .00) compared to DIG participants between Time1 and Time2.
Within Group Changes Across All Time Points for the Initial Intervention Group
IIG participants showed a significant decrease in DDD (B = −.504, SE = 0.042, p < .001), AWD (B = −.831, SE = 0.067, p <.001), PHDD (B = −.199, SE = 0.017, p < .001), and PTSD symptoms (B = −8.182, SE = 1.041, p <.001) from Time1 to Time2. Between end-of-intervention and three month follow-up, all alcohol consumption variables (DDD [B = −.157, SE = 0.047, p < .01], AWD [B = −.452, SE = 0.076, p < .001], PHDD [B = −.096, SE = 0.019, p < .001]) continued to show a significant decrease. There were no further changes in PTSD symptom scores for IIG participants during this time period (B = −1.199, SE = 1.144, p = .29).
Within Group Changes Across All Time Points for the Delayed Intervention Group
DIG participants showed a significant decrease in DDD (B = −.125, SE = 0.05, p <.05), AWD (B = −.245, SE = 0.083, p < .01), PHDD (B = .075, SE = 0.019, p < .001), and total PCL-5 scores (B = −2.73, SE = 1.123, p < .05) between Time1 and Time2, although changes were significantly greater for IIG participants. Once provided access to the intervention, DIG participants demonstrated a significant reduction in DDD (B = −.188, SE = .062, p < .01), AWD (B = −.346, SE = .103, p < .01) and PTSD symptoms (B = −4.076, SE = 1.339, p < .01). Between end-of-intervention and three month follow up, DIG showed significant decreases in DDD (B = −0.355, SE = 0.067, p < .001), AWD (B = −0.519, SE = 0.111, p < .001), PHDD (B = −0.130, SE = 0.025, p < .001) and PTSD symptoms (B = −3.062, SE = 1.442, p < .05).
Changes in alcohol-related problems (SIP) from baseline to 3 month follow-up within groups
There was a significant reduction in the average SIP score from Time1 to the three month follow-up for IIG (B = −10.391, SE = .632, p < .001) and in the average SIP score from repeated baseline to three month follow up (B = −10.334, SE = .909, p < .001) for DIG participants.
Module Completion - VetChange
Approximately 90% of IIG and 88% of DIG participants (who completed the repeated baseline assessment) completed Module 1, 54% of IIG and 58% of DIG participants completed four modules, and 34% of IIG and 39% of DIG participants completed eight modules.
Discussion
The results of this RCT provide empirical support for the efficacy of a newly developed Web intervention, VetChange, to reduce drinking and PTSD symptoms in returning Veterans. Participants in our Immediate Intervention Group (IIG) demonstrated a significantly greater reduction in alcohol consumption and PTSD symptoms than participants in our Delayed Intervention Group (DIG). Further, once the delayed group had access to VetChange they demonstrated the same pattern of reductions in drinking seen in IIG participants. By demonstrating changes in two important outcomes by end-of-intervention, this study makes an important contribution to our understanding of the potential effectiveness of Web interventions for this population. Three month outcomes also suggest that VetChange may provide Veterans with the skills necessary to maintain lasting changes in behavior.
The efficacy of VetChange in reducing both alcohol consumption and PTSD suggests that the intervention can be helpful to returning Veterans with co-occurring problems. Although our data did not allow us to determine the mechanism of change for VetChange we believe that the use of a combination of motivational and cognitive-behavioral strategies (similar to other effective Web interventions for problem drinkers [e.g., Hester et al., 2009]) and PTSD [e.g., Litz et al., 2007]) may have increased the self-efficacy of participants to cope with a range of problems, a factor that is important for individuals recovering from both alcohol problems and PTSD.
One of the strengths of the current study was our success in reaching a large population of returning Veterans with problem drinking. Facebook advertising alone attracted approximately 11,000 individuals to the Website. Further, with Web based screening, we achieved our recruitment goal of 600 participants in 46 days. We recruited participants through Facebook in order to minimize potential for fraudulent enrollment (Kramer et al., in press). This approach appeared to provide us with a study sample that is reasonably representative of the current population of active duty personnel (including an accurate proportion of women), with only small differences (i.e., participants were slightly older and minority enrollment was lower than expected [DOD, 2012; National Center for Veterans Analysis and Statistics, 2010]).
Our study design also allowed us to evaluate the efficacy of VetChange with a diverse population of OEF and OIF Veterans with problem drinking. Although we felt it was important to establish an upper limit for drinking to minimize potential safety risks for the most severe drinkers, there were few other restrictions on study entry. As more severe drinkers were more likely to drop out, it may be that a self-management approach is not sufficient for these Veterans. However, we were able to demonstrate the efficacy of VetChange with participants regardless of demographic characteristics, variables related to military service, or levels of recent treatment involvement. These data suggest that the results may be generalizable to a larger returning Veteran population of problem drinkers.
The current study offers methodological improvements over many Web-based studies (Kiluk et al., 2011) by randomly assigning participants, demonstrating baseline comparability of groups, obtaining comparable levels of outcome data from both groups, ensuring an adequate sample size to test hypotheses, deriving the Web intervention from empirically-based therapies, reporting rates of intervention completion, and including follow-up assessments.
Nonetheless, there were limitations in the study. We encountered high rates of attrition from the intervention (34% of IIG and 39% of DIG completed all eight modules). Although many Web studies for problem drinkers fail to report completion rates, available data indicate that completion rates vary widely (e.g., 6% for a six-week Web intervention [Linke, Brown, & Wallace, 2004] compared to 73% to 91% for two three-module Web interventions [Pemberton et al., 2011]). Rates of intervention completion in the current study are similar to those reported for many face-to-face interventions for alcohol problems (approximately 30%), including brief interventions in primary care (Edwards & Rollnick, 1997), intensive interventions for alcohol abuse or dependence (Dale, Coulton, Godfrey et al., 2011), and integrated therapies for alcohol dependence and PTSD (Coffey, Stasiewicz, Hughes, & Brimo, 2006).
In evaluating the value of Web interventions it is important to consider attrition in the context of the potential reach and cost-effectiveness of these interventions. Although attrition rates for the full intervention were noteworthy in this study, approximately one third of the participants completed all eight modules of the intervention. Thus, from a public health perspective (Bennet & Glasgow, 2009), a Web intervention such as VetChange, which can be widely accessed by the target population and delivered in a cost-effective manner, can have a substantial impact on population health even with high rates of individual attrition.
Understanding reasons for attrition is critical for interpreting the potential impact on outcomes. Postel et al. (2010) report that some participants discontinue Web treatments because they believe they have achieved sufficient benefit. In our study, most participants completed Module 1, which is similar to effective single-session Web interventions for problem drinking (Walters, Hester, Chiauzzi, & Miller, 2005). Also, a majority completed half of VetChange and received a “dose” of the intervention that is similar to the length and format of effective in-person treatments for problem drinkers (Sobell & Sobell, 1996). Future research is needed to determine how much of the intervention is needed to achieve positive outcomes.
High rates of attrition at assessment points is also a limitation. Other investigators have observed similar high rates of attrition in studies with returning Veterans. Adler, Bliese, McGurk, Hoge & Castro (2009) reported nearly 54% attrition in an evaluation of three early-intervention models of care with returning Veterans. To prevent bias in interpretation of data, our analyses took missing data into account by using regression-based multiple imputation and mixed effect models. Both analyses yielded similar outcomes and demonstrated strong effects of the intervention.
While we implemented safeguards to prevent attrition from our assessments (i.e., providing incentives for completing assessments [Khadjesari et al., 2011]), the use of additional strategies such as tailored e-mail messages, adding a social networking component (Bennett & Glasgow, 2009), or translating VetChange into a mobile phone application should be considered. Although adding therapist interactions to a Web intervention may also help to reduce attrition (Kiluk et al., 2011) this would likely have compromised our ability to reach as many returning Veterans and reduced the overall impact on the population that we hoped to reach.
There are other potential limitations related to study design. First, in order to be fully automated the study assessments needed to rely on self-report data. Requiring face-to-face assessment would have precluded us from reaching Veterans from around the United States and overseas locations. Second, with studies designed to assess self-management Web interventions there is limited availability of suitable comparison conditions. Testing the efficacy of VetChange by adding it to treatment as usual (e.g., Carroll et al., 2008) would have interfered with promotion of a confidential and convenient intervention. By using a delayed intervention design we were able to provide an active intervention to two-thirds of the sample immediately, to offer the active intervention to all participants within eight weeks, and to rapidly replicate the findings of those in IIG. Finally, we did not use block randomization, which could have been a limitation; however, our overall group assignment matched the 2:1 target ratio and we did not find evidence of disproportionate assignment to treatment condition during any period of the randomization.
In summary, this study makes an important contribution by demonstrating the efficacy of VetChange to change two of the central conditions associated with warzone deployment: problem drinking and PTSD. With these changes, VetChange has the potential to mitigate the major impact of warzone stress exposure and reduce morbidity, disability, and mortality associated with problem drinking in a new generation of combat-deployed Veterans. The high level of interest demonstrated in the intervention and the positive outcomes associated with its use suggest that it would be valuable to provide ready access to VetChange and other similar Web interventions for Veterans. Goals for future research with VetChange include evaluating its efficacy with other Veteran samples, as an integrated component of face-to-face treatment, or as one component in a stepped care approach to treating alcohol problems and PTSD (e.g., Zatzick et al., 2004). In addition, more long-term follow up is needed to fully assess the lasting impact of the intervention.
Acknowledgments
This research was supported by Grant RC1AA019248 (PI: Keane) from the National Institute on Alcohol Abuse and Alcoholism and by the National Center for Posttraumatic Stress Disorder (Behavioral Sciences Division).
Footnotes
On June 19, 2011, after 15 days of recruiting, we detected an attempt to register 120 fraudulent accounts over the course of approximately 12 hours. These registrations coincided with unusual enrollment-related Website traffic originating from a single province in China, as determined by anonymous Web analytics data. We temporarily suspended new enrollments while keeping the VetChange intervention fully open for enrolled participants. Procedural and technical improvements were added to the protocol, approved by the Institutional Review Boards (Boston University and VA Boston Healthcare System), and enrollment began again. These 120 fraudulent accounts were excluded, and were not included in any of the reporting in this paper. Please see (Kramer et al., in press) for a full discussion of these events.
We’d like to thank Timothy Heeren, Robert Lew, Errol Baker and David Gagnon for their statistical expertise and consultation.
Contributor Information
Eric Helmuth, Boston University School of Public Health.
John Hermos, Boston University School of Medicine.
Mark Lachowicz, VA Boston Healthcare System and Boston University School of Medicine.
Denis Rybin, Boston University School of Public Health.
David Rosenbloom, Boston University School of Public Health.
References
- Adler AB, Bliese PD, McGurk D, Hoge CW, & Castro CA (2009). Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: Randomization by platoon. Journal of Consulting and Clinical Psychology, 77, 928–940. doi: 10.1037/a0016877 [DOI] [PubMed] [Google Scholar]
- Amstadter AA, Broman-Fulks J, Zinzow H, Ruggiero KJ & Cercone J (2009). Internet-based interventions for traumatic stress-related mental health problems: A review and suggestion for future research. Clinical Psychology Review, 29, 410–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, & Grant M (1992). AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care Health. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Bennett GG & Glasgow RE (2009). The Delivery of Public Health Interventions via the Internet: Actualizing Their Potential. Annual Review of Public Health, 30, 273–292. [DOI] [PubMed] [Google Scholar]
- Blankers M, Koeter MWJ, & Schippers GM (2011). Internet therapy versus internet self-help versus no treatment for problematic alcohol use: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79, 330–341. doi: 10.1037/a0023498 [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL,…Kivlahan DR (2003). Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Archives of Internal Medicine, 163, 821–829. doi: 10.1001/archinte.163.7.821163/7/821 [DOI] [PubMed] [Google Scholar]
- Brief DJ, Rubin A, Enggasser JL, Roy M, & Keane TM (2011). Web-based intervention for returning Veterans with symptoms of posttraumatic stress disorder and risky alcohol use. Journal of Contemporary Psychotherapy, 41, 237–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C) are an effective brief screening test for problem drinking. Archives of Internal Medicine, 158, 1789–1795. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Elter JR, Jones ER, Kudler H & Straits-Troster K (2008). Hazardous alcohol use and receipt of risk-reduction counseling among U.S. Veterans of the Wars in Iraq and Afghanistan. Journal of Clinical Psychiatry, 69, 1686–1693. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, … Rounsaville BJ (2008). Computer-assisted delivery of cognitive-behavioral therapy for addiction: A randomized trial of CBT4CBT. American Journal of Psychiatry, 165, 881–888. doi: 10.1176/appi.ajp.2008.07111835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob CM, Novaco RW, Hamada RS, & Gross DM (1997). Cognitive-behavioral treatment for severe anger in posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 65(1), 184–189. [DOI] [PubMed] [Google Scholar]
- Cucciare MA, Weingardt KR, & Humphreys K (2009). How Internet Technology Can Improve the Quality of Care for Substance Use Disorders. Current Drug Abuse Reviews, 2, 256–262. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, & Li TK (2005). Quantifying the risks associated with exceeding recommended drinking limits. Alcoholism:Clinical & Experimental Research, 29, 902–908. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Heagerty P, Liang K, Zeger SL (2002) Analysis of longitudinal data, Oxford: Oxford University Press, USA. [Google Scholar]
- Edwards AG, & Rollnick S (1997). Outcome studies of brief alcohol intervention in general practice: the problem of lost subjects. Addiction, 92, 1699–1704. [PubMed] [Google Scholar]
- Eysenbach G (2005). The law of attrition. Journal of Medical Internet Research, 7(1), e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney JW, Wilbourne PL, & Moos RH (2007). Psychosocial treatments for substance use disorders. In Nathan PE & Gorman JM (Eds.), A Guide to Treatments that Work (3rd ed.). (pp. 179–202). New York, NY US: Oxford University Press. [Google Scholar]
- Hawkins EJ, Lapham GT, Kivlahan DR, & Bradley KA (2010). Recognition and management of alcohol misuse in OEF/OIF and other veterans in the VA: A cross-sectional study. Drug and Alcohol Dependence, 109, 147–153. doi: S0376–8716(10)00027-X [pii] 10.1016/j.drugalcdep.2009.12.025 [DOI] [PubMed] [Google Scholar]
- Hester RK, Delaney HD, Campbell W, & Handmaker N (2009). A web application for moderation training: initial results of a randomized clinical trial. Journal of Substance Abuse Treatment, 37, 266–276. doi: S0740–5472(09)00029–4 [pii] 10.1016/j.jsat.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22. doi: 10.1056/NEJMoa040603351/1/13 [pii] [DOI] [PubMed] [Google Scholar]
- Jacobson IG, Ryan MK, Hooper TJ, Smith TC, Amoroso PJ, Boyko EJ, Bell NS (2008). Alcohol use and alcohol-related problems before and after military combat deployment. Journal of the American Medical Association, 300, 663–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, & Kaloupek DG (1997). Comorbid psychiatric disorders in PTSD: Implications for research. In Yehuda R & McFarlane A (Eds.), Psychobiology of Posttraumatic Stress Disorder (pp. 24–34). New York, NY: Annals of the NY Academy of Sciences. [DOI] [PubMed] [Google Scholar]
- Kenna GA, Longabaugh R, Gogineni A, Woolard RH, Nirenberg TD, Becker B, …Karolczuk K (2005). Can the Short Index of Problems (SIP) be improved? Validity and reliability of the three-month SIP in an emergency department sample. Journal of Studies on Alcohol, 66, 433–437. [DOI] [PubMed] [Google Scholar]
- Khadjesari Z, Murray E, Kalaitzaki E, White IR, McCambridge J, Thompson SG, …Godfrey C (2011). Impact and Costs of Incentives to Reduce Attrition in Online Trials: Two Randomized Controlled Trials. Journal of Medical Internet Research, 13, e26. doi: 10.2196/jmir.1523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiluk BD, Sugarman DE, Nich C, Gibbons CJ, Martino S, Rounsaville BJ, & Carroll KM (2011). A methodological analysis of randomized clinical trials of computer-assisted therapies for psychiatric disorders: toward improved standards for an emerging field. American Journal of Psychiatry, 168, 790–799. doi: 10.1176/appi.ajp.2011.10101443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DW, King LA, & Vogt DS (2003). Manual for the Deployment Risk and Resilience Inventory (DRRI): A collection of measures for studying deployment-related experiences in military veterans. Boston (MA): National Center for PTSD. [Google Scholar]
- King L, King D, Vogt DS, Knight J, & Samper RE (2006). Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology, 18, 89–120. [Google Scholar]
- Kramer J, Rubin A, Coster W, Helmuth E, Hermos J, Rosenbloom D…. Keane TM (in press). Strategies to address the challenges of participant misrepresentation in Web-based research. International Journal of Methods in Psychiatric Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linke S, Brown A, & Wallace P (2004). Down your drink: a web-based intervention for people with excessive alcohol consumption. Alcohol and Alcoholism, 39(1), 29–32. [DOI] [PubMed] [Google Scholar]
- Litz BT, Engel CC, Bryant RA, Papa A (2007). A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. American Journal of Psychiatry. 164:1676–1683. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG (2010). PTSD symptoms, hazardous drinking, and health functioning among U.S. OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress, 23(1), 108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Steenkamp M, Levy H, & Litz B (2009). Technology-assisted interventions for PTSD. In Cucciare MA & Weingardt KR (Eds.). The Use of Technology to Support Evidence-Based Behavioral health Practices: A Clinician’s Guide (pp. 45–68). New York: Taylor and Francis. [Google Scholar]
- Miller WR, Tonigan JS, & Longabaugh R. (1995). The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse. Washington, DC: U.S. Gov’t Printing Office. [Google Scholar]
- Miller WR, & Munoz RF (2005). Controlling your drinking: Tools to Make Moderation Work for You. New York, NY: Guilford Press. [Google Scholar]
- Miller WR, & Wilbourne PL (2002). Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction, 97, 265–277. [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, & Hoge CW (2007). Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Journal of the American Medical Association, 298, 2141–2148. [DOI] [PubMed] [Google Scholar]
- Najavits L, Ryngala D, Back S, Bolton E, Mueser K, Brady K (2009). Treatment of PTSD and Comorbid Disorders. In Foa E, Keane TM, Friedman M & Cohen JA (Editors). Effective Treatments for PTSD. pp. 508–538. [Google Scholar]
- National Center for Veterans Analysis and Statistics (December 2010). Veteran Population Projections: FY2000 to FY2036 [data file]. Department of Veterans Affairs, Office of the Actuary, Veteran Population Projections Model (VetPop), 2007, Table 10L. Retrieved from http://www.va.gov/VETDATA/Demographics/Demographics.asp [Google Scholar]
- Office of the Deputy Under Secretary of Defense (2010). Demographics 2010: Profile of the military community: Department of Defense. Retrived from http://www.militaryonesource.mil/footer?content_id=267470
- Pemberton MR, Williams J, Herman-Stahl M, Calvin SL, Bradshaw MR, Bray RM, … Mitchell GM (2011). Evaluation of two web-based alcohol interventions in the U.S. military. Journal of Studies on Alcohol and Drugs, 72, 480–489. [DOI] [PubMed] [Google Scholar]
- Postel MG, de Haan HA, ter Huurne ED, Becker ES, & de Jong CA (2010). Effectiveness of a web-based intervention for problem drinkers and reasons for dropout: randomized controlled trial. Journal of Medical Internet Research, 12, e68. doi: 10.2196/jmir.1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinert DF & Allen JP (2007). The Alcohol Use Disorders Identification Test: An update of research findings. Alcoholism: Clinical and Experimental Research, 31, 185–199. [DOI] [PubMed] [Google Scholar]
- Riper H, Kramer J, Smit F, Conijn B, Schippers G, & Cuijpers P (2007). Web-based self-help for problem drinkers: A pragmatic randomized trial. Addiction, 103, 218–227. [DOI] [PubMed] [Google Scholar]
- Riper H, Spek V, Boon B, Conijn B, Kramer K, Martin-Abello K, & Smit F (2011). Effectiveness of e-self-help interventions for curbing adult problem drinking: A meta-analysis. Journal of Medical Internet Research, 12, e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB (1976). Inference and missing data. Biometrika, 63, 581–590. [Google Scholar]
- Rubin DB (1987). Multiple Imputation for Nonresponse in Surveys, New York: John Wiley & Sons, Inc. [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, & Marmar CR (2009). Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. American Journal of Public Health, 99, 1651–1658. doi: AJPH.2008.150284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell MB, & Sobell LC (1996). Problem drinkers: Guided Self Change Treatment. New York: Guilford Press. [Google Scholar]
- Sobell LC, Agrawal S, Sobell MB, Leo GI, Young LJ, Cunningham JA, & Simco ER (2003). Comparison of a Quick Drinking Screen with the Timeline Followback for individuals with alcohol problems. Journal of Studies on Alcohol, 64, 858–861. [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA & Hoge CW (2010). Prevalence of mental health problems and functional impairment among active component and National Guard Soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67, 614–623. [DOI] [PubMed] [Google Scholar]
- USDHHS & USDA. (2010). Dietary Guidelines for Americans (7th ed.), pp. 30–31. Washington D.C.: U. S. Government Printing Office. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt DS, King DW, & King LA (2004). Focus groups in psychological assessment: Enhancing content validity by consulting members of the target population. Psychological Assessment, 16, 231–243. [DOI] [PubMed] [Google Scholar]
- Walters ST, Hester RK, Chiauzzi E, Miller E (2005). Demon rum: High-Tech solutions to an age-old problem. Alcoholism: Clinical and Experimental Research, 29, 270–277. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane TM (1993, October). The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Weathers FW, & Ford J (1996). Psychometric properties of the PTSD checklist (PCL-C, PCL-S, PCL-M, PCL-PR). In Stamm BH (Ed.), Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press. [Google Scholar]
- Weathers FW, Keane TM, & Foa EB (2009). Assessment and diagnosis of adults. In Foa EB, Keane TM, Friedman MJ & Cohen JA (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.). (pp. 23–61). New York, NY: Guilford Press. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2010). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
- World Medical Association (2008). Declaration of Helsinki: Recommendations Guiding Doctors in Clinical Research: World Medical Assoc. [Google Scholar]
- Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, … Katon W (2004). A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives of General Psychiatry, 61, 498–506. doi: 10.1001/archpsyc.61.5.498. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Shea TM, Rosen K, Simpson E, Mulrenin K, Begin A, & Pearlstein T (1997). An affect-management group for women with posttraumatic stress disorder and histories of childhood sexual abuse. Journal of Traumatic Stress, 10, 425–436. [DOI] [PubMed] [Google Scholar]
- Zwarenstein M, Treweek S, Gagnier J, Altman D, Tunis Se., Haynes B, …Moher D (2008). Improving the reporting of pragmatic trials: an extension of the CONSORT statement. British Medical Journal, 337,, a2390, doi: 10.1136/bmja2390. [DOI] [PMC free article] [PubMed] [Google Scholar]


