Summary:
Extremely atrophic mandibles are difficult to treat. Most patients choose to live with removable dentures. However, what if the atrophy is so extreme that spontaneous fractures occur? The objective of this report is to offer a single-stage augmentation method, which uses patient-specific crib-shaped implants (PSI) combined with autogenous free bone grafts. PSI were planned using three-dimensional (3D) segmentation and 3D virtual-planning software. Implants were designed according to the patient’s mandible with a mesh-like structure and included large holes for allowing blood supply recovery. During surgery, the PSI fitted perfectly. In cases exhibiting malposition of the mandibular fragments, repositioning was performed using 3D virtual planning. When repositioning mandibular segments, the PSI served as a guide for the correct positioning. Iliac-crest bone graft was harvested and fixed as an onlay over the residual mandibular basal bone. External approach was used to avoid contamination. Six months following surgery, fixation wires were removed, and dental implants were positioned in the newly formed bone. The PSI allowed for rigid fixation, thus leading to optimal incorporation of the iliac-crest bone graft. No further augmentation was required. Bony continuity for future stability and secession of the spontaneous fractures was achieved. Dental implants were placed effortlessly. Treating extremely atrophic mandibles is an entity of its own and is considered one of the most challenging in craniofacial reconstruction. It mostly requires multiple operations with high rates of failure. We offer a novel method of 3D mandibular reconstruction, both vertically and horizontally, showing promising results and achieving enough bone for further dental rehabilitation.
Takeaways
Question: How to reconstruct a severely atrophic lower jaw?
Findings: We present a novel method for reconstructing an atrophic lower jaw using a crib-shaped patient-specific titanium implant concomitantly with an iliac crest bone graft. 3D planning was used for reduction of malunion or nonunion lower jaws and creation of crib-shaped titanium implant fitting perfectly to the lower border of the lower jaw. Free bone graft was connected to the existing bone for 6 months. Following that period, dental implants were easily placed and reconstructed.
Meaning: A new treatment option for surgeons encountering severely atrophic lower jaws.
INTRODUCTION
As life expectancy increases, there is an increase in the prevalence of atrophic mandibles following tooth loss.1 The mechanical effect of teeth and dental implants on bone preservation was previously established. Missing teeth results in the lack of bone stimulation, which facilitates resorption.2 The rate of resorption is influenced by various factors and is variable among different individuals.3 Rate of resorption usually increases during the first year following tooth loss and then decreases.4 In some individuals, bone resorption continues until extreme atrophy is observed. These patients are prone to spontaneous fractures.5 Luhr et al6 classified atrophic mandibles into three categories: class I, moderate atrophy in which the height of the mandible is between 16 and 20 mm; class II, significant atrophy with a height of 11–15 mm; and class III, extreme atrophy with a height of 10 mm or less.
Treatment of fractured atrophic mandibles is complex. The remaining bone should be supported by a reconstruction plate.7 Decreased blood supply, lower mandibular height, and poor healing capacity increase the rates of complications.8,9 In the era of dental implants, the standard of care includes a full fixed rehabilitation, a demand difficult to achieve in patients with extreme atrophy of the mandible. There are two major reasons for this often-unequivocal request. The first is the embarrassment and discomfort, which accompanies the need to remove dentures at night. The second is the difficulty in achieving a stable removable full mandibular denture. During function, such as talking and eating, the intrinsic muscles of the tongue and the floor of the mouth cause instability and displacement of the denture. One of the challenges in rehabilitating an atrophic mandible is the superior position of the inferior alveolar nerve. This nerve supplies sensation to the chin and lower lip. Its superior position is a major limitation for placing future dental implants.
In cases of moderate resorption, several options for rehabilitation exist10: onlay and interpositional bone graft, distraction-osteogenesis, guided bone regeneration, and inferior alveolar nerve lateralization. The above-mentioned techniques except for the latter require minimal bone above the inferior alveolar nerve or are limited in the possible vertical gain achieved and thus are contraindicated in severe cases of Luhr class III mandibles.10 Nerve lateralization is a one-stage technique, including dental implant placement, yet no vertical augmentation is performed, thus resulting in unfavorable crown-implant ratio. In addition, in this technique, high rates of inferior alveolar nerve dysesthesia are observed, and there is a concern for a fracture during or following implant placement.
In cases with Luhr class III, the mandible is prone to spontaneous fractures, and augmentation is required for bone continuity and not only for rehabilitation. We describe a novel method for using patient-specific implants (PSI) in combination with an onlay bone graft for augmentation and rehabilitation of extreme atrophic mandibles prone to spontaneous fractures.
TECHNIQUE
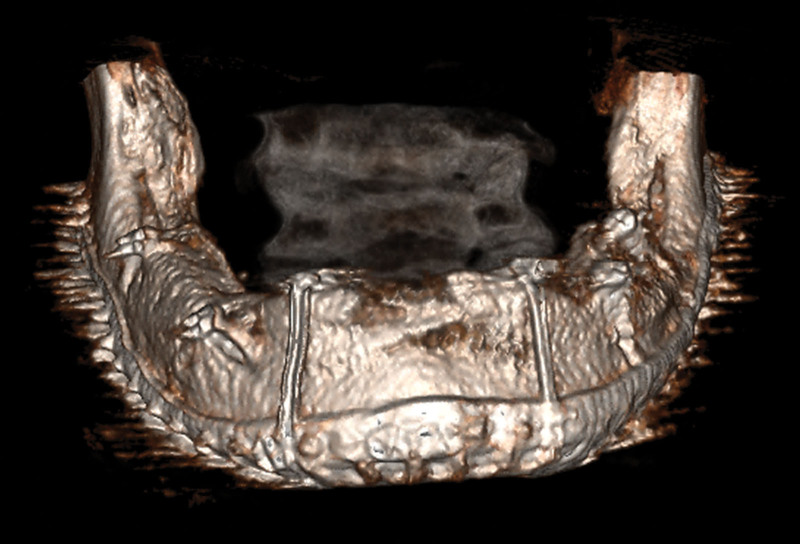
Two cases of Luhr III mandibles6 were treated using a novel crib-shaped PSI with simultaneous iliac-crest free bone graft. Computed tomography imaging was performed and exported (Fig. 1). Planning of the cases included two computer-assisted design software: one for segmentation (D2P; 3D systems, Ore.) and the other for designing the PSI (Geomagic-Freeform; 3D systems). The process included segmenting the mandible and creating a stereolithography file using the D2P software. In case there was a fracture in need of repositioning, the mandible was segmented into two segments. The stereolithography file was then exported into the Geomagic-Freeform software for further manipulation, and the segments were repositioned in the correct form. A crib-shaped mesh-like PSI was created, fitting perfectly to the patient’s mandible (Fig. 2). The process of 3D planning is detailed in a previous report (See Video [online], which displays a step by step video presenting the 3D virtual planning of the patient-specific implant).11 The PSI was sent for 3D printing in selective laser sintering technology (3D Systems, S.C.), and a model of the mandible was printed in-house using a fused deposition modeling printer for confirming the passive fitting of the PSI. The operation included an extra oral approach to avoid contamination of the bone graft and to achieve proper visualization. Repositioning of the segments was performed if malposition existed. The mandible was augmented using an iliac-crest free bone graft fixed to the PSI. The PSI was fixed to the remaining mandible using screws and to the bone graft using wires. The inferior alveolar nerve, if located on the crest, was repositioned lingually.
Fig. 1.
Radiographic evaluation. Anterior aspect of a 3D reconstruction from a CT demonstrating the severe mandibular atrophy. A previous fracture showing fibrous healing can be observed in the right mandibular body.
Fig. 2.
3D manipulation and designing the PSI. Following segmentation of the mandible, the left segment was repositioned to create an aligned mandible. A crib-shaped mesh-like PSI was designed according to the final location of the segments.
Video 1. This video reviews the step by step video presenting the 3D virtual planning of the patient specific implant.
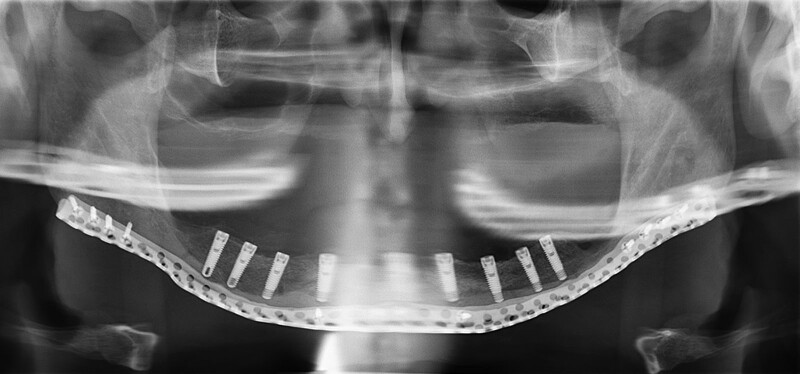
Superimposition of the pre- and postoperative computed tomography images (Figs. 1 and 3) was performed to evaluate the bone gain. Fixation wires were removed 6.5 months postoperative under local anesthesia during dental implant placement. Dental implant placement was directed using an in-house 3D-printed guide created based on a 3D reconstruction of the dentition (Fig. 4).
Fig. 3.
Evaluating the results. CT evaluation 6 months after surgery was performed, exhibiting abundant bone augmentation in all aspects of the mandible.
Fig. 4.
Results and dentition reconstruction. Panoramic x-ray 6.5 months after surgery, following fixation wire removal and dental implant placement. Notice the extent of bone augmentation achieved and the positioning of the dental implants.
DISCUSSION
Treating extremely atrophic mandibles is an entity of its own and is considered one of the most challenging in craniofacial reconstruction. It mostly requires multiple operations with high rates of failure. Different methods offer immediate solutions such as reconstruction plates for stabilization and sporadic dental implants in the anterior aspect of the mandible.12 These solutions have several disadvantages. First, this focuses the forces of mastication on the reconstruction plate rather than sharing the load with the bone, thus increasing the chance of failure due to loss of bony anchorage around the screws or plate fracture. Second, the forces of mastication are concentrated on dental implants placed on the anterior segment, potentially leading to their failure. Finally, this method only allows for the placement of removable dentures and does not allow for a fixed solution.
Our solution includes a PSI for stabilization combined with an autogenous bone graft for continuity and rehabilitation. It allows for anterior as well as posterior dental implant placement for a fixed dental rehabilitation. The disadvantages include an external submandibular scar and a two-stage approach. We offer a novel method of bony reconstruction showing promising results, allowing for full reconstruction of the mandible in both the vertical and horizontal aspects. Bony continuity for future stability and secession of the spontaneous fractures was achieved, and abundant bone for further dental rehabilitation was observed.
Footnotes
Published online 6 June 2022.
Drs. Shilo and Capucha contributed equally to this work.
Disclosure: The authors have no financial interests to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Atwood DA. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971;26:266–279. [DOI] [PubMed] [Google Scholar]
- 2.Frost HM. Bone’s mechanostat: a 2003 update. Anat Rec A Discov Mol Cell Evol Biol. 2003;275:1081–1101. [DOI] [PubMed] [Google Scholar]
- 3.Bras J. Mandibular atrophy and metabolic bone loss. Int Dent J. 1990;40:298–302. [PubMed] [Google Scholar]
- 4.Denissen HW, Kalk W, Veldhuis HA, et al. Anatomic considerations for preventive implantation. Int J Oral Maxillofac Implants. 1993;8:191–196. [PubMed] [Google Scholar]
- 5.Cope MR. Spontaneous fracture of an atrophic endentulous mandible treated without fixation. Br J Oral Surg. 1982;20:22–30. [DOI] [PubMed] [Google Scholar]
- 6.Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:250–254. [DOI] [PubMed] [Google Scholar]
- 7.Ellis E, III, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008;66:421–435. [DOI] [PubMed] [Google Scholar]
- 8.Bruce RA, Ellis E. III. The second Chalmers J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993;51:904–911. [DOI] [PubMed] [Google Scholar]
- 9.Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232–236. [DOI] [PubMed] [Google Scholar]
- 10.Rachmiel A, Emodi O, Rachmiel D, et al. Sandwich osteotomy for the reconstruction of deficient alveolar bone. Int J Oral Maxillofac Surg. 2018;47:1350–1357. [DOI] [PubMed] [Google Scholar]
- 11.Capucha T, Shilo D, Blanc O, et al. 3D planning and printing of patient specific implants for reconstruction of bony defects. J Vis Exp. 2020;162:e60929. [DOI] [PubMed] [Google Scholar]
- 12.Lopes N, Oliveira DM, Vajgel A, et al. A new approach for reconstruction of a severely atrophic mandible. J Oral Maxillofac Surg. 2009;67:2455–2459. [DOI] [PubMed] [Google Scholar]