Dear Editor:
Previous viral infections have traditionally been considered to be the cause of a cross-immunity phenomenon in the aetiopathogenesis of granulomatous thyroiditis. The numerous cases described after SARS-CoV-2 infection serve as an example. However, they have hardly been reported following the administration of vaccines. Two cases of De Quervain's thyroiditis following vaccination against COVID-19 are reported below.
Case 1: 32-year-old woman, with no previous history, who 3 days after administration of the second dose of Comirnaty© presented with anterior cervical pain and pain on palpation, as well as general symptoms such as asthenia, malaise, weakness and hyperthermia. She was assessed by her primary care physician, who prescribed naproxen and requested a general blood test, which showed suppressed TSH values (<0.008 mIU/L) (0, 350–4,940 mIU/L), free T4 of 1.93 ng/dL (0.7–1.48 ng/dL) and free T3 of 6.33 pg/mL (1.59–3.91 pg/mL). The patient responded favourably to naproxen, reducing pain and general symptoms. In view of these laboratory results, the patient was referred to endocrinology Fig. 1 .
Figure 1.
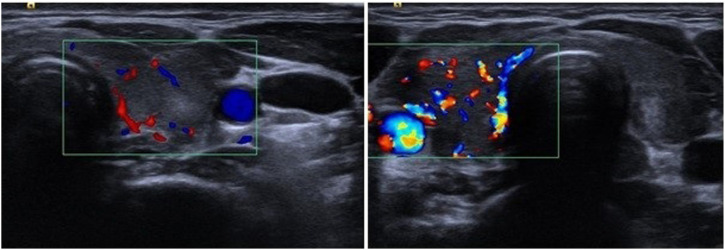
Figure no. 1: Thyroid ultrasound of the cases described in the article:
Left: Ultrasound image of case number 1.
Right: Ultrasound image of case number 2.
At the time of being evaluated by endocrinology, the patient was asymptomatic, without the need for analgesia and without significant findings on physical examination. Ultrasound examination showed a thyroid gland with heterogeneous structure and moderately increased vascularisation. A diagnosis of granulomatous thyroiditis was considered; therefore, the patient was left untreated, and an appointment was made at one month for follow-up, with TSH values of 0.168 mIU/L, free T4 of 0.57 ng/dL and free T3 of 2.03 pg/mL. Finally, after another 4 weeks, the thyroid profile returned to normal (TSH 2.253 mIU/L, free T4 0.79 ng/dL).
Case 2: 33-year-old woman, with no previous history, who on the day after the administration of the first dose of Vaxzevria© started with odynophagia and left earache. Within 2 weeks of the initial clinical presentation, new symptoms developed, such as hyperthermia, asthenia, tachycardia, diarrhoea and weight loss. Physical examination revealed a grade II goitre with significant discomfort on palpation. The patient was admitted to internal medicine due to the lack of resolution of the clinical symptoms.
At admission, she had suppressed TSH (<0.008 mIU/L), free T4 of 3.62 ng/dL and free T3 of 10.47 pg/mL. Other notable findings included elevated CRP (55.4 mg/L) (0–5 mg/L) and ESR (43 ml/h) (<25). Given the suspicion of subacute thyroiditis, the patient was discharged on symptomatic treatment with ibuprofen and propranolol and was referred to the outpatient endocrinology department for follow-up.
The patient was found to be asymptomatic and without any discomfort on cervical palpation after 2 months. A new blood test showed TSH values of 10.615 mIU/L and free T4 of 0.58 ng/dL. On thyroid ultrasound, the thyroid was found to be slightly enlarged, predominantly hypoechoic and with intensely increased vascularisation. In the absence of symptoms of hypothyroidism, replacement therapy was not prescribed, and the patient was seen again one month later; partial recovery was observed, with TSH values of 8.617 mIU/L and free T4 0.78 ng/dL. To date, the patient is pending further evaluation.
Discussion: since the outbreak of SARS-CoV-2,1 numerous cases of granulomatous thyroiditis have been reported following SARS-CoV-22 infection. Some cases of subacute thyroiditis following vaccination have also been reported, e.g., the cases described following influenza vaccination.3 However, few cases of subacute thyroiditis have been detected after vaccination against COVID-19.
The mechanism by which these phenomena occur is unknown, although it is speculated that certain vaccine adjuvants4 may trigger these developments. It is also believed that there could be a cross-immunity component between the viral spike proteins produced by the vaccine and certain antigens expressed on the surface of healthy thyroid follicular cells.5
Given the wide population coverage of vaccination against COVID-19, it is important to keep in mind the diagnosis of subacute thyroiditis, to be considered in patients experiencing anterior neck pain and general symptoms in the context of recent vaccination against SARS-CoV-2. In addition to the aforementioned symptoms, this diagnosis is based on a thyroid profile characterised by a triphasic course and a compatible ultrasound examination.
Footnotes
Please cite this article as: González López J, Martín Niñno I, Arana Molina C, Tiroiditis subaguda tras vacunación contra el SARS-CoV-2: a propósito de dos casos, Med Clin (Barc). 2022;158:e13–e14.
References
- 1.Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med. 2020;382(8):692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 2.Khatri A., Charlap E., Kim A. Subacute thyroiditis from COVID-19 infection: a case report and review of literature. Eur Thyroid J. 2021;9(6):324–328. doi: 10.1159/000511872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altay F.A., Güz G., Altay M. Subacute thyroiditis following seasonal influenza vaccination. Hum Vaccin Immunother. 2016;12(4):1033–1034. doi: 10.1080/21645515.2015.1117716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watad A., David P., Brown S., Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvants and thyroid autoimmunity. Front Endocrinol (Lausanne). 2017;7:150. doi: 10.3389/fendo.2016.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vojdani A., Kharrazian D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin Immunol. 2020;217 doi: 10.1016/j.clim.2020.108480. [DOI] [PMC free article] [PubMed] [Google Scholar]