Abstract
BACKGROUND:
Urinary tract infections (UTIs) are more common in females than males and predominantly based on their unhealthy practices in their day to day lives. This study is trying to assess the occurrence of UTI and strategies used by female student to prevent UTI.
MATERIALS AND METHODS:
A cross-sectional descriptive study carried out in a tertiary care teaching institute. A total of 338 conveniently selected B. Sc. Nursing and MBBS Medical students were surveyed. The data were collected by using a pretested, a self-structured questionnaire related to occurrence and practices to prevent UTI along with necessary demographic details. Descriptive (frequency, percentage, mean and standard deviation) and inferential (Chi-square test) statistics was used to compute the data.
RESULTS:
The result of this study shows that 10.05% female students reported of having UTI. The proportion was higher in nursing students (67.6%) than medical (32.4%) but did not show a significance difference (P = 0.61). Age, duration of hostel life, and marital status were significantly associated with the status of UTI (P = 0.001). To prevent UTI, students were using commercial product with Tea Tree Oil, soap, drinking 3–4 l water/day, increased frequency of peri-wash during menstruation period, and use of Citrus Fruits. The use of western toilet was also significantly associated with status of UTI (P = 0.04).
CONCLUSION:
The occurrence of UTI was more among nursing students. Most of the perineal hygienic practices by the female students were associated with occurrence of UTI; hence, it is necessary to emphasize on preventive practices to minimize re-occurrence.
Keywords: Female, hygiene, medical, menstruation, nursing, students, urinary tract infections
Introduction
Urinary tract infections (UTIs) are the second-most common infections, especially among females accounting approximately 8.3 million hospital visit every year leading to serious health issues.[1,2] Bacteria present in urine are the cause for UTIs, even though fungi and virus could also be involved. Among the women, who infected have been seen recurrent in a single year. Females are more susceptible for UTIs, although UTIs occur in both male and females.[3,4,5,6]
UTIs affect lower urinary tract most commonly; however, infection can spread to upper urinary tract. Cystitis is the term used to describe lower UTIs, characterized by dysuria, increased frequency of urination, urgency to urinate, and may have supra-pubic pain. Ascending infections may cause severe pyelonephritis, which is a concerned kidney infection.[7] Although even if the urine has significant bacteria without any symptoms, that would be termed as asymptomatic bacteriuria, on the other hand with symptoms it is symptomatic bacteriuria.[8,9]
Every year about 250 million people diagnosed with UTI.[10] In young girls, the estimated number of UTIs are 0.5 per person per year. Furthermore, repeated infections are common among 80% of infected persons; usually with in a period of 3 months of original infection. The incidence of UTIs increases as age advances and sexual activity starts.[11,12] The available scientific literatures suggest that various factors related to UTIs including education, socioeconomic status, marital status, menstrual status, diet, and past history of UTI.[13,14,15,16]
UTIs are most common in children and teenagers,[8] females are more likely to get UTI than males due to their shorter urethral length, facilitating bacteria and other microbes to ascend to the bladder easily, causing infection;[17] almost 60% of females experience a lower UTI at a some point in their lifetime.[18]
Among causative pathogens, Escherichia coli is the most common organism for UTIs, and it is common infection in women transmits through fecal flora easily.[15,19]
Female medical and nursing students are more vulnerable to develop UTI than the general population and require attention. Studies from India as well as other part of world have reported that 20%–65% of female medical and nursing students have experienced symptoms of UTIs.[20,21,22] The higher number of UTIs among medical and nursing students are attributable to various risk factors such as clinical posting, continue classes, toileting practices, and type of toilets.
Based on the evidence and incidence of UTIs among young hostellers, knowing the occurrence of UTIs will help for the early diagnosis, prompt treatment; eventually results in early prognosis and prevention from re-infection. In India, there is a limited evidence available regarding factors associating with UTI among female students. In India, there is a limited evidence available regarding the occurrence rate and practices to prevent UTI among female students. Therefore, the present work is carried out to find out the occurrence of UTI among female students residing in the hostels of Medical Teaching Institute in northern part of India.
Materials and Methods
Study design and setting
A cross-sectional descriptive study was conducted in a tertiary level medical teaching institute from north India. The study was conducted from July 2019 to September 2019.
Study participants and sampling
A total of 338 female students (Medical 241, nursing 97) were conveniently selected in the present study. The inclusion criteria were: (1) Female students of medical and nursing, (2) staying in the hostel for more than 1 year, (3) age between 18-30 years, (4) available at the time of data collection, and (5) willing to participate in this study were included. The exclusion criteria were: History of hospitalization or catheterization in the past 3 months.
The sample size calculation was performed by online Rao software. In the present study, setting the population size 570 female students, 99% confidence level, and 5% margin of error, with 10% attrition rate, it was estimated that the required sample size would be 338 participants for this study.[23]
Data collection tool and technique
A predesigned, self-administered, structured questionnaire was developed by extensive literature review from databases, i.e., Google Scholar, Medline, PubMed, and EMBASE. The data collection tool consisted of three sections: (1) Participants’ profile; (2) Practices to prevent UTI; and (3) Symptoms or Experiences of UTI.
Participants profile
It consisted of necessary demographic details, including the category of student, age in years, marital status, socioeconomic class by modified Kuppuswamy socioeconomic scale[24] and occurrence of UTI in the last 3 months.
Symptoms of urinary tract infection and experiences
The questions related to the clinical symptoms of UTI in the last 3 months were explored in this section. The questions were related to increased urination frequency, persistence urge, burning, painful micturition, off urination, and fever. Furthermore, questions regarding frequency, duration of UTI and treatment taken in the past for UTI were included.
Practices to prevent urinary tract infection
This section included 20 questions related to perineal hygiene, use of sanitary napkin pads, undergarments and their frequency of use, sexual activity, water intake, use of citric acid fruits in diet, history of infections, and type of toilet used.
The validity of questionnaire was done by giving it to experts in the field of medical and nursing, and reliability was computed by the test-retest method (r = 0.82).
Data were collected by the four female researchers during free classes. A list of all the female students residing in the hostel was collected from the administration office and contacted after classes. Among the 570 female students, 356 answered all the questions. Students were given 40 min to complete the questionnaire without discussion with each other under the supervision of researchers. However, 18 students were excluded because of the incompleteness of the questionnaires.
Ethical consideration
Students were explained about the objectives of the study and were free to withdraw at any stage of the study. A written consent was taken from all the students who were willing to participate in the study. The present study was approved by Institutional Ethical Committee (12/IEC/STS/2019).
Data analysis
All the data were entered into the Microsoft excel 2016 and Software Statistical Package (version 23) (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). Descriptive statistics were used to summarize the characteristics of study participants, symptoms of UTI and experiences, practices to prevent UTI. To find the association between participants’ characteristics, practices to prevent UTI, and female students with UTI Chi-square test was performed. A P < 0.05 was considered statistically significant.
Results
Demographic characteristic
A total of 338 students (MBBS 97; B. Sc. Nursing 241) were surveyed. Approximately 10% of the students had experienced symptoms of UTIs. The student category and presence of UTIs did not show any significant differences. Higher age, duration of hostel life, and marital status have shown significant differences with the presence of UTIs. More than half of the students were from upper, upper-middle socioeconomic class families, but that was not associated with the presence of UTIs among students [Table 1].
Table 1.
Demographic characteristic of the study population (n=338)
| Demographic characters | Status of UTIs, frequency (%) | Total (n=338), frequency (%) | Significance level (χ2, df, P) | |
|---|---|---|---|---|
|
| ||||
| Present (n=34) | Absent (n=304) | |||
| Students category | ||||
| B.Sc. nursing | 23 (67.6) | 218 (71.7) | 241 (71.3) | 0.24, 1, 0.61 |
| MBBS | 11 (32.4) | 86 (28.3) | 97 (28.7) | |
| Age (years) | ||||
| ≤20 | 7 (20.6) | 203 (66.8) | 210 (62.1) | 27.72, 1, <0.001 |
| >20 | 27 (79.4) | 101 (33.2) | 128 (37.9) | |
| Duration of hostel life (years) | ||||
| 2-3 | 27 (79.4) | 89 (29.3) | 116 (34.3) | 34.09, 1, <0.001 |
| ≥3-5 | 7 (20.6) | 215 (70.7) | 222 (65.7) | |
| Marital status | ||||
| Married | 9 (26.5) | 14 (4.6) | 23 (6.8) | 23.05, 1, <0.001 |
| Unmarried | 25 (73.5) | 290 (95.4) | 315 (93.2) | |
| Socioeconomic class of family | ||||
| Lower middle and lower | 15 (44.1) | 129 (42.4) | 144 (42.6) | 0.03, 1, 0.85 |
| Upper, upper-middle | 19 (55.9) | 175 (57.6) | 194 (57.4) | |
UTIs=Urinary tract infections
The relationship between preventive strategies practiced and urinary tract infections
The present study demonstrated the significant relationship between perineal hygiene practice, number of peri-wash during menstruation per day, tissue paper used in perineal cleaning, number of sanitary napkins used during mensturation, perineum being usually moist, change of undergarment frequency, sexual activity status, water intake, use of citrus fruits in diet, history of frequent UTIs, and type of toilet used on the occurrence of UTIs p>0.01 level of significance [Table 2].
Table 2.
Association between preventive strategies practiced and presence of urinary tract infections among female students
| Practices | UTIs | Chi-square test | P | |
|---|---|---|---|---|
|
| ||||
| Present (n=34) | Absent (n=304) | |||
| Perineal wash by | ||||
| Use of soap and water | 12 (35.3) | 212 (69.7) | 75.46 | <0.001 |
| Use of commercial product with tea tree oil | 8 (23.5) | 84 (27.6) | ||
| Plain water | 14 (41.2) | 8 (2.6) | ||
| Frequency of peri-wash during menstruation | ||||
| 3-6 times/day | 23 (67.6) | 54 (17.8) | 15.99 | <0.001 |
| 7-10 times/day | 11 (32.4) | 250 (82.2) | ||
| Direction of perineal wash | ||||
| Front to back | 8 (23.5) | 57 (18.8) | 4.01 | 0.13 |
| Back to front | 25 (73.5) | 200 (65.8) | ||
| Both | 1 (2.9) | 47 (15.5) | ||
| Tissue paper use in perineal cleaning: Yes | 16 (47.1) | 198 (65.1) | 4.30 | 0.038 |
| Use of sanitary napkins pads: Yes | 34 (100) | 304 (100) | NA | NA |
| Number of sanitary napkins used during menstruation | ||||
| 3-5 every day | 32 (94.1) | 65 (21.4) | 79.06 | <0.001 |
| 6-8 every day | 2 (5.9) | 239 (78.6) | ||
| Is your perineum being usually moist: Yes | 23 (67.6) | 280 (92.1) | 19.70 | <0.001 |
| Fabric of undergarment used | ||||
| Pure cotton | 13 (38.2) | 83 (27.3) | 1.79 | 0.18 |
| Mixed cotton | 21 (61.8) | 221 (72.7) | ||
| Change of undergarments | ||||
| Once a day | 22 (64.7) | 182 (59.9) | 5.9 | 0.05 |
| Twice a day | 4 (11.8) | 75 (24.7) | ||
| After soiling | 1 (2.9) | 54 (17.8) | ||
| Drying of undergarments under sunlight: Yes | 12 (35.3) | 81 (26.6) | 1.14 | 0.28 |
| Sexual activity status | ||||
| Active | 2 (5.9) | 87 (28.6) | 8.14 | 0.004 |
| Inactive | 32 (94.1) | 217 (71.4) | ||
| Habitual delayed in urination: Yes | 26 (76.5) | 64 (21.1) | 48.07 | <0.001 |
| Frequency of urination per day | ||||
| 3-5 | 14 (41.2) | 140 (46.1) | 0.29 | 0.58 |
| 6-8 | 20 (58.8) | 164 (53.9) | ||
| Water intake (liters/day) | ||||
| 1-2 | 22 (64.7) | 103 (33.9) | 12.46 | <0.001 |
| 3-4 | 12 (35.3) | 201 (66.1) | ||
| Intake of citrus fruits (oranges/lemons/grapefruits/cranberry): Yes | 25 (73.5) | 264 (86.8) | 4.37 | 0.036 |
| History of frequent infection of UTI: Yes | 9 (26.5) | 23 (7.6) | 12.75 | <0.001 |
| Type of toilet used | ||||
| Indian | 3 (8.8) | 80 (26.3) | 4.15# | 0.04# |
| Western | 31 (91.2) | 224 (73.7) | ||
#The Chi-square statistic with Yates correction. NA=Not Applicable, UTIs=Urinary tract infections
Pattern and signs and symptoms experienced during urinary tract infections by students
The frequency distribution of UTIs and symptoms are presented in Table 3 and Figure 1. Among the female students, approximately 79% had a one-time UTI in the last 1 year period, 47% suffered for 8–14 days. The most symptom was burning micturition, and the least was white foul-smelling discharge reported by female students [Figure 1].
Table 3.
Frequency of urinary tract infection experienced by participants (n=34)
| Characteristic of UTI occurrence | Frequency (%) |
|---|---|
| Frequency of UTIs in last 1 year | |
| One time | 27 (79.4) |
| Two times | 5 (14.7) |
| Three times | 1 (02.9) |
| Seldon | 1 (02.9) |
| Duration of suffering (days) | |
| 2-7 | 9 (26.5) |
| 8-14 | 16 (47.1) |
| 15-21 | 5 (14.7) |
| 22-30 | 4 (11.8) |
| Treatment taken for UTIs | |
| Yes | 21 (61.8) |
| No | 13 (38.2) |
UTIs=Urinary tract infections
Figure 1.
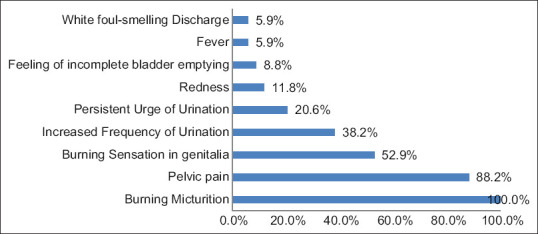
Distribution of Signs and symptoms during urinary tract infection among students
Discussion
The present study reported a lower frequency (10.06%) of UTI whereas other studies reported a higher range (19%–31%) of UTIs among female nursing, dental and medical students in India,[21,25,26] Ethiopia,[27] Nigeria, Washington.[28] This could be due to better facilities in the central government institution. The student categories, medical and nursing, were not associated with UTIs.
Although there was no significant association between nursing and medical students, a higher proportion of nursing students reported the presence of UTI. Nurses being a vulnerable group of health care team leading to develop more infections as compared to others as they spend more time with patients comparatively.[20,21]
The study revealed that UTI was less prevalent in younger than 20 years of age, which was similar to the findings of Zalina et al. from Malaysia, who reported approximately 76% of medical and nursing female students between the age of 21–29 years with UTIs.[29] Whereas a study from India found younger nursing female students (17–20 years) with a higher frequency of UTIs.[21]
Most of the student experiences hostel life during the college period, and this is the beginning where female students attempt to accommodate hostel life with sharing of living areas as well as lavatory. The present findings found that the shorter duration of hostel life was significantly associated with UTI among female students.
In this study, the rate of UTI was higher among unmarried female students. This is difficult to explain and is not consistent with other studies[30,31] that reported a lower proportion of UTI in unmarried females.
Almost an equal number of female students were from lower-middle and lower and upper, upper-middle socioeconomic class, which has also been found in a study from the central part of India.[26] However, in other studies, higher economic status was less likely to be experienced lower rate of UTI; also, income is significantly associated with better health quality.[32,33]
Our results, noting that UTI among female students was significantly high among those who were cleaning perineal area with plain water and lowest among who used commercial product with Tea Tree Oil. It has been reported by various literature that Tea tree oil is an essential oil containing various components with microbicidal and fungicidal as well as anti-inflammatory properties.[34,35,36]
It is well-known facts that the accumulated residue from sweating, urine or feces, causes irritation, and promotes bacterial growth. Adequate practice of perineal hygiene after urination and during menstruation can minimize not only UTI but also infection related to genital area infections. The current study demonstrated a higher frequency of peri-wash after urination and during menstruation had shown a lower number of UTI, which was similar to a study by Das et al.[37] The correct technique/method of cleaning perineal area also plays a significant role in preventing UTI.
The direction of cleaning of perineum area from front to back is a correct method that reduces the risk of UTI among females.[38,39] Almost three-fourths of female students were followed wrong techniques of perineal wash in the present study, which was incongruent with other studies.[22,26]
It is important to wash and dry the genitourinary areas to prevent UTI, which was found in the present study findings where more than half of the students were not drying the perineal area after washing, and reported a higher number of UTI. Similar results were reported by a study by Vyas et al.[26] A study from Brazil reported that most (66.4%) of the gynecologists use toilet paper after urination to clean the area, and 78.5% use toilet paper for hygiene after evacuation.[39]
In the present study, all the students with UTI reported using sanitary pads, whereas a study from Zambia reported that due to the inability to buy, girls were not using sanitary pads.[40] A study from India found that a large proportion of girls with UTI reported using sanitary pads, while only a few girls who were using homemade sanitary pads reported having UTI.[26] In a recent survey from Maharashtra, Chhattisgarh, Tamil Nadu reported that 2564 (70.9%) menstruating girls, only 45% of female students were using disposable sanitary pads, while 28% used clothes.[41] Along with use, it is also important how frequently the soiled sanitary pad was changed. In the present study, students who changed their soiled sanitary pad during the menstruation period more frequently had significantly lower rates of UTI.
Among female students, majority (83.43%) were using mixed cotton underwear; among them, 61.8% had UTI. The studies have reported a significant association between the UTI and material of undergarments reported by the females; cotton clothes had a lower rate of UTI than mixed and synthetic material.[26,42] The frequency of changing undergarments also considered as a part of hygiene practices, as continue wearing same moistened cloth favors the growth of bacteria and increase the risk of infection. In the present study, a large proportion of participants were changing their undergarments once in a day, which was reported by Vyas et al.[26]
Exposure of clothes under sunlight act as disinfecting action is a well-known fact among medical and nursing students. Even then, 72.5% of students were not drying their undergarments under the sunlight, of which 64.7% reported having UTI. This finding was consistent with the results of other studies.[25,26,42,43,44] Inactive in the sex was significantly associated with higher number of students with UTI, which was in contrast with the findings from another study.[45]
Habitual delaying in urination is unhealthy toileting behaviors which were reported significantly higher among female students with UTI. These results are similar to other studies.[14,45] Increased water intake helps in flushing out the bacteria and dead epithelial cells, reducing nutrients for bacterial growth.[46,47,48]
In the present study, higher water intake of was significantly associated with lower rates of UTI, which was reported in a recent meta-analysis that if a person is not in the harm, can be advised to increase the water intake to minimize the recurrence of the UTI.[49] Citrus fruits such as oranges, lemons, grapefruits, and cranberries are reported as antibacterial, antifungal, anticancer, antiviral, and antidiabetic properties.[50] The students who reported consuming citrus fruits in their routine diet had significantly lower frequency (6.5%) of UTI.
In addition, a study has reported that berry juice and other dietary factors were associated with a lowered risk of UTI.[50] An another exploratory study In another interventional[15] and review[51] has reported that citrus fruits were found effective in the management of bacteriuria and recurrence of UTI.
Our study findings indicated that a history of recurrence of UTIs was significantly associated with UTI. Similar results reported[14] that frequent UTI was a risk factor for presence of UTI, as infection decreases sphincter pressure by contracting detrusor muscles.[52]
The type of toilet has a significant role in good health; in Indian toilets, individuals have to use a squatting posture, which can prevent various disorders such as UTI and hemorrhoids/piles.[53] A vast number (91.2%) of female students with UTI was using a western type of toilets, a similar pattern reported in a study from Malaysia.[54]
Limitation and recommendation
Although in the present study, many aspects were covered regarding practices to prevent UTI among medical and nursing students, there are few limitations of this study. First, we did not observe the practices which students were practicing in their daily life. Second, the occurrence of UTIs was not confirmed by urinalysis or urine culture as a confirmatory test to diagnose the condition. All the data were self-reported by the study participants, which could be subjected to information bias regarding the accuracy of the reported information. In this study, we recommend that there should be health education activities on prevention and management of UTIs at the school level as well as at the time of admission in the hostel among female students. In addition, female students should be encouraged to visit a physician at an early stage if they have any signs and symptoms of genitourinary tract-related problem.
Conclusion
In the study, it was concluded that a higher number of female nursing students had UTI than medical. Even though medical and nursing students know the basics of sciences and preventive practices, many were not practicing in the UTI group. Perineal hygiene, use of sanitary pads during menstruation, sexual activities, water intake, use of citrus fruits in the diet, history of UTI, and type of toilets used were significantly associated with the presence of UTI among female students. Emphasizing preventive measures for UTIs is important to minimize the rate of UTI and their re-occurrences.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We, the authors of this study, would like to thanks the participants to participate in this study and give their valuable time to complete the questionnaire.
References
- 1.Kant S, Lohiya A, Kapil A, Gupta SK. Urinary tract infection among pregnant women at a secondary level hospital in Northern India. Indian J Public Health. 2017;61:118–23. doi: 10.4103/ijph.IJPH_293_15. [DOI] [PubMed] [Google Scholar]
- 2.Ojo OO, Anibijuwon II. Urinary tract infection among female students residing in the campus of the University of Ado Ekiti, Nigeria. Afr J Microbiol Res. 2010;4:1195–8. [Google Scholar]
- 3.Raheela M, Mutahir SK. Recurrent urinary tract infections in females. [Last accessed on 2020 Oct 26];Natl Libr Med. 2010 60:55–9. Available from: https://pubmed.ncbi.nlm.nih.gov/20055283/ [Google Scholar]
- 4.Matthews SJ, Lancaster JW. Urinary tract infections in the elderly population. [Last accessed on 2020 Oct 26];Am J Geriatr Pharmacother. 2011 9:286–309. doi: 10.1016/j.amjopharm.2011.07.002. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21840265 . [DOI] [PubMed] [Google Scholar]
- 5.Afoakwa P, Domfeh SA, Afranie BO, Owusu DO, Donkor S, Sakyi KK, et al. Asymptomatic bacteriuria and anti-microbial susceptibility patterns among women of reproductive age. A cross-sectional study in primary care, Ghana. Med Sci (Basel) 2018;6:E118. doi: 10.3390/medsci6040118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rejali M, Ahmadi SS, Hassanzadeh A, Yazdani R, Ahmadi SN. The relationship between weight gain during pregnancy and urinary tract infections in pregnant women of Shahrekord, by using the “Nested case-control study”, in 2013. J Educ Health Promot. 2015;4:84. doi: 10.4103/2277-9531.171797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers J. Understanding the most commonly billed diagnoses in primary care. [Last accessed on 2020 Oct 28];Nurse Pract. 2020 45:35–40. doi: 10.1097/01.NPR.0000718516.64801.27. Available from: https://journals.lww.com/10.1097/01.NPR.0000718516.64801.27 . [DOI] [PubMed] [Google Scholar]
- 8.Lane DR, Takhar SS. Diagnosis and management of urinary tract infection and pyelonephritis. [Last accessed on 2020 Oct 26];Emerg Med Clin North Am. 2011 29:539–52. doi: 10.1016/j.emc.2011.04.001. Available from: http://www.emed.theclinics.com/article/S0733862711000356/fulltext . [DOI] [PubMed] [Google Scholar]
- 9.Givler DN, Givler A. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2021. Jul 25, [Last accessed on 2020 Oct 28]. Asymptomatic Bacteriuria. 2021 Jan–. PMID: 28722878. Available from: https://pubmed.ncbi.nlm.nih.gov/28722878/ [Google Scholar]
- 10.Mackenzie D. UTIs could soon be life-threatening without new antibiotics. New Sci. 2017. p. 3115. https://www.newscientist.com/article/2122891-utis-could-soon-be-life-threatening-withoutnew-antibiotics/
- 11.Al-Badr A, Al-Shaikh G. UTI in CKD. Sultan Qaboos Univ Med J A. 2013;13:359–67. doi: 10.12816/0003256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aslam S, Albo M, Brubaker L. Recurrent urinary tract infections in adult women. JAMA. 2020;323:658–9. doi: 10.1001/jama.2019.21377. [DOI] [PubMed] [Google Scholar]
- 13.Sharma R, Negi S, Kunj D, Sharma V, Vardha Promoting menstrual hygiene among adolescent girls. Indian J Community Health. 2015;27:376–80. [Google Scholar]
- 14.Wan X, Wu C, Xu D, Huang L, Wang K. Toileting behaviours and lower urinary tract symptoms among female nurses: A cross-sectional questionnaire survey. Int J Nurs Stud. 2017;65:1–7. doi: 10.1016/j.ijnurstu.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Kontiokari T, Laitinen J, Järvi L, Pokka T, Sundqvist K, Uhari M. Dietary factors protecting women from urinary tract infection. Am J Clin Nutr. 2003;77:600–4. doi: 10.1093/ajcn/77.3.600. [DOI] [PubMed] [Google Scholar]
- 16.Singh A, Gupta V, Agrawal D, Goyal P, Singh M, Lukhmana S. A Cross-sectional study to investigate the impact of focused group discussion on menstrual hygiene among rural school girls of Southern Haryana, India. J Educ Health Promot. 2020;9:260. doi: 10.4103/jehp.jehp_475_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta M, Bhardwaj S, Sharma J. Screening of urinary isolates for the prevalence and antimicrobial susceptibility of enterobacteria other than Escherichia coli. Int J Life Sci Pharm Res. 2013;3:100–4. [Google Scholar]
- 18.Foxman B. Urinary tract infection syndromes occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin N Am. 2014;28:1–13. doi: 10.1016/j.idc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Gupta S, Malakar M, Kalita P, Pandey FK. Bacterial profile and antibiograms in urinary tract infection. Al Ameen J Med Sci. 2019;12:192–6. [Google Scholar]
- 20.Liao YM, Yang CY, Kao CC, Dougherty MC, Lai YH, Chang Y, et al. Prevalence and impact on quality of life of lower urinary tract symptoms among a sample of employed women in Taipei: A questionnaire survey. Int J Nurs Stud. 2009;46:633–44. doi: 10.1016/j.ijnurstu.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Vyas S, Varshney D, Sharma P, Juyal R, Nautiyal V, Shrotriya V. An overview of the predictors of symptomatic urinary tract infection among nursing students. Ann Med Health Sci Res. 2015;5:54–8. doi: 10.4103/2141-9248.149790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vati S, Prabhakaran N. Prevalence of symptoms of urinary tract infection and its risk factors among unmarried female medical and dental students in a tertiary care hospital, Kannur. [Last accessed on 2020 Dec 17];IOSR J Dent Med Sci. 2020 19:30–6. Available from: https://www.iosrjournals.org . [Google Scholar]
- 23.Sample Size Calculator by Raosoft, Inc. 2004. [Last accessed on 2020 Jul 23]. Available from: http://www.raosoft.com/samplesize.html .
- 24.Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care. 2019;8:1846–9. doi: 10.4103/jfmpc.jfmpc_288_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vati S, Prabhakaran N, Madhusoodanan KV, Sneha S, Devika MR. Prevalence of symptoms of urinary tract infection and its risk factors among unmarried female Medical and dental students in a tertiary care hospital, Kannur. IOSR J Dent Med Sci. 2020;19:30–6. [Google Scholar]
- 26.Vyas S, Sharma P, Srivastava K, Nautiyal V, Shrotriya VP. Role of behavioural risk factors in symptoms related to UTI among nursing students. J Clin Diagnostic Res. 2015;9:LC15–8. doi: 10.7860/JCDR/2015/10995.6547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gebremariam G, Legese H, Woldu Y, Araya T, Hagos K, GebreyesusWasihun A. Bacteriological profile, risk factors and antimicrobial susceptibility patterns of symptomatic urinary tract infection among students of Mekelle University, Northern Ethiopia. BMC Infect Dis. 2019;19:950. doi: 10.1186/s12879-019-4610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scholes D, Hooton TM, Roberts PL, Stapleton AE, Gupta K, Stamm WE. Risk factors for recurrent urinary tract infection in young women. J Infect Dis. 2000;182:1177–82. doi: 10.1086/315827. [DOI] [PubMed] [Google Scholar]
- 29.Zalina N, Aruku N, Azura N, Shahida N, Akhmarina N, Dian F. Prevalence of lower urinary tract symptoms (LUTS) among young age medical population. IIUM Med J Malaysia. 2011;10(1):7–15. [Google Scholar]
- 30.Almukhtar SH. Urinary tract infection among women aged (18-40) years old in Kirkuk city, Iraq. Open Nurs J. 2019;12:248–54. [Google Scholar]
- 31.Muthulakshmi M, Gopalakrishnan S. Study on urinary tract infection among females of reproductive age group in a rural area of Kancheepuram district, Tamil Nadu. Int J Community Med Public Health. 2017 Sep 22;4(10):3915–21. [Google Scholar]
- 32.Choi EP, Lam CL, Chin WY. The health-related quality of life of Chinese patients with lower urinary tract symptoms in primary care. Qual Life Res. 2014;23:2723–33. doi: 10.1007/s11136-014-0725-5. [DOI] [PubMed] [Google Scholar]
- 33.Koh JS, Cho KJ, Kim HS, Kim JC. Twelve-month medication persistence in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Int J Clin Pract. 2014;68:197–202. doi: 10.1111/ijcp.12241. [DOI] [PubMed] [Google Scholar]
- 34.Loose M, Pilger E, Wagenlehner F. Anti-bacterial effects of essential oils against uropathogenic bacteria. Antibiot (Basel, Switzerland) 2020;9:358. doi: 10.3390/antibiotics9060358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Swamy MK, Akhtar MS, Sinniah UR. Antimicrobial Properties of Plant Essential Oils against Human Pathogens and Their Mode of Action: An Updated Review. Evid Based Complement Alternat Med. 2016. 2016. Available from: https://pubmed.ncbi.nlm.nih.gov/28090211 . [DOI] [PMC free article] [PubMed]
- 36.Khalil NS, Ibrahim A, Abdelazeem RM. Effect of Body Wash with Tea Tree Oil on the Prevention of Methicillin-Resistant Staphylococcus aureus in Critically Ill Patients at a university hospital in Egypt. Iris J Nurs Care. 2019;1(4):1–5. [Google Scholar]
- 37.Das P, Baker KK, Dutta A, Swain T, Sahoo S, Das BS, et al. Menstrual hygiene practices, wash access and the risk of urogenital infection in women from Odisha, India. PLoS One. 2015;10:e0130777. doi: 10.1371/journal.pone.0130777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moustafa MF, Makhlouf EM. Association between the hygiene practices for genital organs and sexual activity on urinary tract infection in pregnant women at women's health center, at Assiut University Hospital. J Am Sci. 2012;8:512–22. [Google Scholar]
- 39.Ruiz C, Giraldo PC, Sanches JM, Reis V, Beghini J, Laguna C, et al. Daily genital cares of female gynecologists: A descriptive study. Rev Assoc Med Bras. 2019;65:171–6. doi: 10.1590/1806-9282.65.2.171. [DOI] [PubMed] [Google Scholar]
- 40.Lahme AM, Stern R, Cooper D. Factors impacting on menstrual hygiene and their implications for health promotion. Glob Health Promot. 2018;25:54–62. doi: 10.1177/1757975916648301. [DOI] [PubMed] [Google Scholar]
- 41.Sivakami M, Maria van Eijk A, Thakur H, Kakade N, Patil C, Shinde S, et al. Effect of menstruation on girls and their schooling, and facilitators of menstrual hygiene management in schools: Surveys in government schools in three states in India, 2015. J Glob Health. 2019;9:010408. doi: 10.7189/jogh.09.010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sevil S, Kevser O, Aleattin U, Dilek A, Tijen N. An evaluation of the relationship between genital hygiene practices, genital infection. Gynecol Obs. 2013;3:1–5. [Google Scholar]
- 43.Yaliwal RG, Biradar AM, Kori SS, Mudanur SR, Pujeri SU, Shannawaz M. Menstrual morbidities, menstrual hygiene, cultural practices during menstruation, and wash practices at schools in adolescent girls of north Karnataka, India: A crosssectional prospective study. Obstet Gynecol Int. 2020. 2020. Available from: https://pubmed.ncbi.nlm.nih.gov/33133193 . [DOI] [PMC free article] [PubMed]
- 44.Moradpour S, Shahnazi H, Hassanzadeh A. Predictability of constructs of theory of planned behavior in adopting urinary tract infection prevention behaviors among pregnant women. J Educ Health Promot. 2021;10(1):233. doi: 10.4103/jehp.jehp_1501_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moore EE, Hawes SE, Scholes D, Boyko EJ, Hughes JP, Fihn SD. Sexual intercourse and risk of symptomatic urinary tract infection in post-menopausal women. J Gen Intern Med. 2008;23:595–9. doi: 10.1007/s11606-008-0535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tian Y, Cai X, Wazir R, Wang K, Li H. Water consumption and urinary tract infections: An in vitro study. Int Urol Nephrol. 2016;48:949–54. doi: 10.1007/s11255-016-1262-7. [DOI] [PubMed] [Google Scholar]
- 47.Khalil NS, Dead AI, Abdelazeem RM. Effect of body wash with tea tree oil on the prevention of methicillin-resistant staphylococcus aureus in critically Ill patients at a university hospital in Egypt. Iris J Nurs Care. 2019;1:1–5. [Google Scholar]
- 48.Hooton TM, Vecchio M, Iroz A, Tack I, Dornic Q, Seksek I, et al. Effect of increased daily water intake in premenopausal women with recurrent urinary tract infections: A randomized clinical trial. JAMA Intern Med. 2018;178:1509–15. doi: 10.1001/jamainternmed.2018.4204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scott AM, Clark J, Del Mar C, Glasziou P. Increased fluid intake to prevent urinary tract infections: Systematic review and meta-analysis. Br J Gen Pract. 2020;70:E200–7. doi: 10.3399/bjgp20X708125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ali J, Das B, Saikia T. Antimicrobial activity of lemon peel (citrus limon) extract. [Last accessed on 2021 Jan 08];Int J Curr Pharm Res. 2017 9:82. Available from: http://creativecommons.org/licenses/by/4.0/ [Google Scholar]
- 51.Das S. Natural therapeutics for urinary tract infections-a review. Futur J Pharm Sci. 2020;6:64. doi: 10.1186/s43094-020-00086-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Basak T, Kok G, Guvenc G. Prevalence, risk factors and quality of life in Turkish women with urinary incontinence: A synthesis of the literature. Int Nurs Rev. 2013;60:448–60. doi: 10.1111/inr.12048. [DOI] [PubMed] [Google Scholar]
- 53.Dimmer C, Martin B, Reeves N, Sullivan F. Squatting for the Prevention of Haemorrhoids? Townsend Lett Dr Patients. 1996;159:66–70. Available from: https://documents.uow.edu.au/~bmartin/pubs/96tldp.html . [Google Scholar]
- 54.Parasuraman S, Wen L, Sam A, Christapher P, Kumar K. Analysis of correlation between defecation posture and risk of urinary tract infections among adolescent populations. [Last accessed on 2021 Jan 07];Environ Dis. 2016 1:82. Available from: http://www.environmentmed.org/text.asp?2016/1/2/77/185305 . [Google Scholar]


