Abstract
Introduction
Registered respiratory therapists (RRTs) are heavily involved in the care of individuals infected with COVID-19. The experiences and challenges specific to the RRT profession during the pandemic have not been qualified and the aim of this study is to bridge that gap.
Methods
With institutional ethics approval, a cross-sectional survey was created through the survey software Redcap and made available online from 29 May to 6 July 2020. Any RRT working in Canada during the COVID-19 pandemic was eligible to participate. Responses to yes/no questions were calculated as frequencies and percentages, and free-text responses were summarized.
Results
In total, 345 RRTs working in 11/13 of the provinces and territories, with varying years of experience completed the survey. The results reflected impacts of the pandemic that affected RRTs in a variety of ways at work, from being reassigned (30.7%) to caring for COVID-19 positive patients (57.4%) and intubated COVID-19 positive patients (50.7%). RRTs experienced communication issues around guidelines (66.7%) and some departments had run out of personal protective equipment (PPE; 19%). RRTs were personally impacted, including feeling overwhelmed by new and frequently changing guidelines (89.6%) and feeling concerned for themselves or their family members becoming infected because of their proximity to COVID-19 positive patients (89%).
Discussion
RRTs reported being required to work more during the pandemic. The unpredictability and constantly changing schedules were sources of stress and anxiety. RRTs were faced with issues of overwhelming amounts of new information and had difficulty in disseminating it in a timely manner. Lack of guidance and lack of confidence in the current protocols added to the confusion, anxiety, and stress. RRTs were at the center of many high-risk moments for contracting the virus (intubation, extubation), and PPE shortages were a major challenge reported. RRTs working during the pandemic have been concerned for their own health and the health of their family members.
Conclusion
The COVID-19 pandemic adds another layer of stress for RRT professionals who are working in high-risk situations and feel anxious, overwhelmed, and concerned about their personal safety.
Keywords: disease outbreaks, public health, healthcare surveys, questionnaires
INTRODUCTION
COVID-19 is a highly infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is a newly discovered strain of coronavirus. On 30 January 2020, COVID-19 was declared an international public health emergency by the World Health Organization (WHO), and by March 11 it was characterized as a global pandemic [1]. COVID-19 is spread primarily through droplets when an individual coughs or sneezes, as well as through contaminated surfaces [2]. Infected individuals exhibit a range of symptoms, many of which involve respiratory complications such as cough, shortness of breath or difficulty breathing, and low oxygen levels in the body, sometimes resulting in pale or blue-coloured skin, lips, or nail beds (hypoxemia) [3–5]. Certain patient populations, including elderly individuals or those with significant comorbidities, are at risk of very serious illness and potentially life-threatening complications [6]. Individuals most severely affected by COVID-19 will often require hospitalization and may suffer respiratory failure requiring intubation and mechanical ventilation [7]. The Canadian Institute for Health Information (CIHI) reported that from January to November 2020 there were 85,400 emergency department (ED) visits related to COVID-19 (excluding Quebec), and 20% of patients that presented to the ED ended up being admitted to hospital [8]. In 23% of these cases, the patient’s hospital admission also involved an admission to the intensive care unit (ICU), and 60% of patients admitted to ICU required mechanical ventilation.
Registered respiratory therapists (RRTs) are trained in all aspects of respiratory health and care for individuals of all ages [9]. RRTs work in a variety of healthcare settings including acute, critical, and emergency care; outpatient clinics; community care; home care; education; management; and administration for example. Since COVID-19 presents predominantly as respiratory and cardiopulmonary symptoms [10], it is not surprising that RRTs are heavily involved in the care of infected individuals. From the mildest hospitalized patients to those in full respiratory failure requiring mechanical ventilation in the ICU, RRTs are involved in the care of nearly all COVID-19 patients. Out of hospital, RRTs are required to care for patients in long-term care facilities, in clinics, or at home. Since RRTs consistently work at the front lines of the fight against COVID-19, there is more focus on the profession than ever before.
Researchers have observed aspects of mental health, psychological burden, post-traumatic stress disorder (PTSD) and burnout in various professional groups working during COVID-19, including nurses, physicians, and paramedics [11–13]. Studies have also looked at the effects on all front-line care workers, including respiratory therapists [14, 15]. A Canadian effort by the Organization for Health Action (HEAL), surveyed members of over 40 national healthcare organizations about the challenges and concerns surrounding COVID-19 [16]. Although RRTs were included in this survey, they have not been the primary focus of any research about COVID-19.
This study aimed to isolate the perspective of RRTs working on the front lines or involved in the preparation and planning for the COVID-19 pandemic. We hypothesized that RRTs would experience their own individual challenges, concerns, and stresses unique to this profession during the pandemic. We expected that worry about access to personal protective equipment (PPE), exposure to the infection for themselves, and exposure for their families would be some of the most common concerns. We also expected to highlight difficulties facing RRTs who are treating COVID-19 patients and aimed to provide insight that may be useful to both front-line professionals and leadership.
METHODS
After securing institutional Research Ethics Board approval, a cross--sectional survey was created using REDCap [17, 18] survey software hosted at Nova Scotia Health. Any RRTs licensed to work in Canada, who had worked during any portion of the COVID-19 pandemic or preparation period were eligible to participate in the survey. The survey was distributed through emails by various provincial regulatory bodies (including Alberta, Saskatchewan, Ontario, Quebec, Nova Scotia, and New Brunswick) and professional societies (typically as an initial posting or email and a follow-up, reminder posting, or email) and advertised through social media platforms. French and English versions of the survey were available. The survey was available from 29 May 2020 to 6 July 2020. Data relating to clinical workload, access to resources and individual challenges, fears, and concerns facing RRTs were collected. For most questions, we provided only “yes” or “no” options from a dropdown (e.g., Are/were you ever responsible for caring for a confirmed COVID-19 positive patient?). Two questions about concerns offered four response options from “not at all concerned” to “very concerned” (e.g., Did you ever feel concerned about the possibility of being infected with COVID-19 in your workplace, as a direct result of working with COVID-19 positive patients?). Throughout the survey, we provided free-text boxes for participants to provide explanations or comments.
Survey data were extracted into an excel worksheet for analyses by the primary investigator. Incomplete survey responses (i.e., with demographic data only) were removed from the dataset; however, participants were allowed to leave individual questions blank if they preferred not to answer. Analyses were completed using descriptive statistics. Means and standard deviations were calculated for age of participants and number of COVID-19 patients. Responses to the yes/no questions were calculated as frequencies and percentages. For free-text responses, answers for each question were extracted into a separate text document and analyzed by the primary investigator. Answers were then grouped by key themes like “workload” and “communication” and were summarized. Responses were also analyzed by province, and results of selected questions were summarized into Table 1.
Table 1.
Provincial-level results of selected survey questions and COVID-19 case data at the time of the survey closing date.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | Quebec | NB, NS, PEI, NFLD, Yukon | |
|---|---|---|---|---|---|---|---|
| Positive COVID-19 Cases (to 6 July 2020) | 2,978 | 8,389 | 805 | 325 | 37,829 | 55,937 | 1,534 |
| COVID-related deaths (to 6 July 2020) | 183 | 155 | 14 | 7 | 2,743 | 5,665 | 69 |
| Survey questions | |||||||
| Work requirements: “Are/were you being required to work more, or different hours than your normal work assignment outside of the pandemic?” (n = positive responses) | 19% (n = 7) |
28% (n = 13) |
29% (n = 4) |
19% (n = 5) |
49% (n = 37) |
53% (n = 10) |
45% (n = 54) |
| Communication: “Have you experienced any issues with the communication of new information or receiving updates to practice recommendations within your department or practice?” (n = positive responses) | 62% (n = 23) |
55% (n = 26) |
64% (n = 9) |
93% (n = 25) |
74% (n = 56) |
84% (n = 16) |
62% (n = 74) |
| Psychological stress: “Have you ever experienced: feeling overwhelmed by new information or guidelines in your practice?” (n = positive responses) | 86% (n = 32) |
91% (n = 43) |
100% (n = 14) |
93% (n = 25) |
89% (n = 68) |
89% (n = 17) |
88% (n = 105) |
| Perceived risk: “Did you ever feel that you were at an increased risk of exposure to COVID-19 as a result of a decreased availability of hospital resources?” (PPE, staff, equipment, etc.) (n = positive response) | 19% (n = 7) |
32% (n = 15) |
50% (n = 7) |
52% (n = 14) |
51% (n = 39) |
26% (n = 5) |
24% (n = 29) |
| Perceived risk: “Did you ever feel concerned about the possibility of being infected with COVID-19 in your workplace, as a direct result of working with COVID positive patients?” (n = somewhat, quite or very concerned) | 95% (n = 35) |
83% (n = 39) |
100% (n = 14) |
81% (n = 22) |
92% (n = 70) |
95% (n = 18) |
88% (n = 105) |
Note: NB, New Brunswick; NS, Nova Scotia; PEI, Prince Edward Island, NFLD, Newfoundland and Labrador.
RESULTS
The survey was accessed 452 times. Of these, 92 entries had no data and were removed. A further 15 participants completed only the demographic data and were excluded. A total of 345 survey entries remained for analysis.
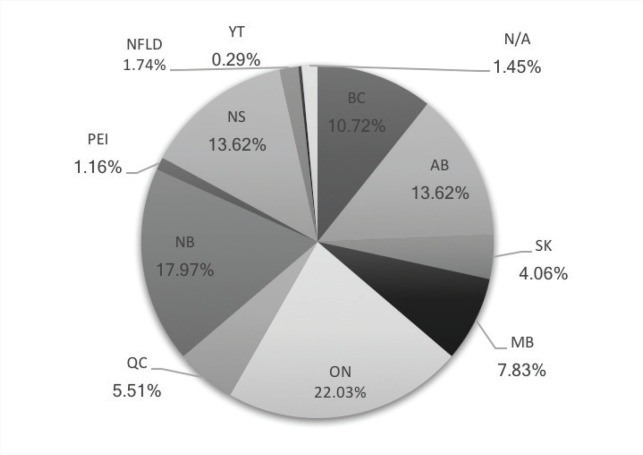
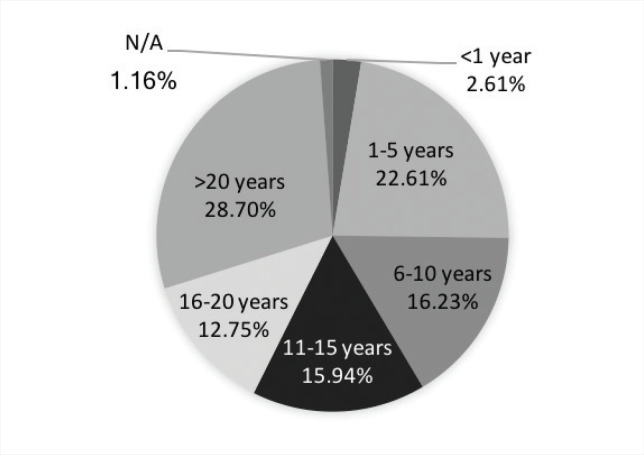
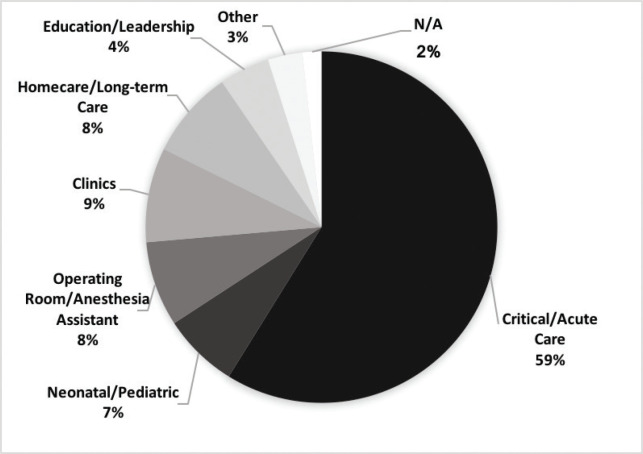
We received completed responses from RRTs working in 11/13 of the provinces and territories. The breakdown of responses by province or territory of employment is shown in Figure 1. There were responses from 276 individuals (80%) who identified as female and 69 individuals (20%) who identified as male. The average age of respondents was 39.15 years (min = 21, max = 70). The years of work experience and primary work environment of survey respondents are shown in Figures 2 and 3, respectively. Primary work environments included critical and acute care, neonatal and pediatric care, operating room (and anesthesia assistants), various clinics (including pulmonary function testing, sleep clinics, COPD and asthma clinics, and a variety of outpatient clinics), homecare and long-term care, education and leadership, or other settings not previously listed.
Figure 1.
Breakdown of survey respondents by province of employment.
Figure 2.
Breakdown of survey respondents by years of work experience.
Figure 3.
Breakdown of survey respondents by primary work environment prior to COVID-19.
Across the 10 free-text questions we provided throughout the survey for participants to elaborate on their responses, we received a total of 775 free-text responses. For the free-text question at the end of the survey, we asked about overall experiences and general comments relating to working during the pandemic. A total of 83 responses were received in response to this question.
Workload
There were 106 participants (30.72%) who were reassigned or experienced a change in their workplace assignment as a result of the COVID-19 pandemic, and 27.35% (n = 29) of these were moved into a critical care setting. A total of 36.23% (n = 125) of participants stated that they had been required to work more, or different hours, during the pandemic, and 17.97% (n = 62) said that RRTs in their department had been asked to return to work from a leave of absence.
In total, 57.39% (n = 198) of RRTs reported that they had been responsible for the care of a confirmed COVID-19 positive patient and cared for an average of 3.7 COVID-19 patients at one time (min = 1, max = 20). Similarly, 50.72% (n = 175) of RRTs were responsible for the care of an intubated COVID-19 patient, with an average of 3.1 intubated COVID-19 patients at one time (min = 1, max = 12). There were 169 respondents (48.99%) who assisted with the intubation of a COVID-19 patient, 54 individuals (15.65%) who were responsible for performing the intubation, and 111 (32.17%) individuals responsible for extubation. There were two free-text questions asked, with a total of 141 responses received, that related to workload. RRTs reported being relocated, or being required to cover additional roles due to layoffs, staff shortages, or covering new areas or hours of work. Most commonly, RRTs reported being required to work more during the pandemic. Often staff worked overtime, had vacation time denied, or worked full-time instead of part-time. Some RRTs in clinic positions stated that they were working to cover additional roles of individuals who had been laid off. One respondent stated, “All employees except for me got laid off at my office therefore I needed to fill the admins role and take over for the other RT while also implementing new processes for COVID.” Meanwhile, others were forced to work fewer hours with less pay or had been laid off themselves: “Lost my respiratory education jobs as clinics shut down,” and “Sleep labs sending very few referrals at this time, hence laid off.”
Communication
For 308 (89.28%) survey participants, new practice guidelines were implemented specifically for COVID-19 patients. A total of 70.14% (n = 242) of RRTs reported feeling that they were provided with updates to best practice guidelines for treating COVID-19 patients, and 309 (89.56%) RRTs said they felt overwhelmed by the influx of new information. As well, 66.67% (n = 230) said they had experienced issues with communication around new information or guidelines, and 88.12% (n = 304) had received conflicting information from different care areas (intensive care unit, emergency department, or patient floors, for example). There were two free-text questions asked, with a total of 365 responses received that related to communication. Respondents commented on the massive volume of new information being introduced and the continuously changing guidelines, which varied from one day to the next and sometimes even changed multiple times within the same day. Communication felt slow within and between professions, and staff reported feeling that their practices were lagging behind the current recommendations and research. Respondents in managerial positions also reported having difficulties communicating the overwhelming amounts of new information to staff. Many reported that meeting with staff in-person was key, but with RRTs frequently working different hours, this was not always possible. When new guidelines were eventually introduced, it did not happen uniformly across care areas. Sometimes the written guidelines also varied significantly from what was being encouraged in practice. Many RRTs reported inconsistencies between the expectations from different care areas, professions, and even between different practitioners. They frequently felt as though they were forced into conflicts between professionals with different preferred practices. As well, they knew that many other professions had received different, or limited, information and looked to them as leaders. However, they felt confused themselves and were unsure how to help educate others. RRTs felt that they were not included in many of the important conversations and decisions within their institutions, despite being at the center of treating COVID-19 patients.
Health and safety and psychosocial risks
Of all respondents, 42 (12.17%) RRTs did not feel adequately trained in the use of PPE in preparation for the pandemic, 21 (6.09%) reported that they did not receive formal N95 mask fit testing, and 74 (21.45%) had not received any additional training on the use of PPE in the context of COVID-19 patients.
In 84.06% (n = 290) of responses, RRTs reported their department had implemented equipment-sparing measures to preserve PPE supplies. This included restricting the use of certain PPE (n = 100/290), using the same PPE for multiple patients or the whole shift (189/290), re-using or re-sterilizing PPE (171/290), or by other means (45/290). In 19.42% (n = 67) of responses, RRTs reported their department had run out of PPE. Three respondents (0.87%) reported having to restrict ventilator access in their hospitals due to equipment shortages, and 24 (7.00%) respondents reported having to withhold care for COVID-19 patients for other reasons (such as cancelling some services, withholding certain treatments, or refusal to intubate).
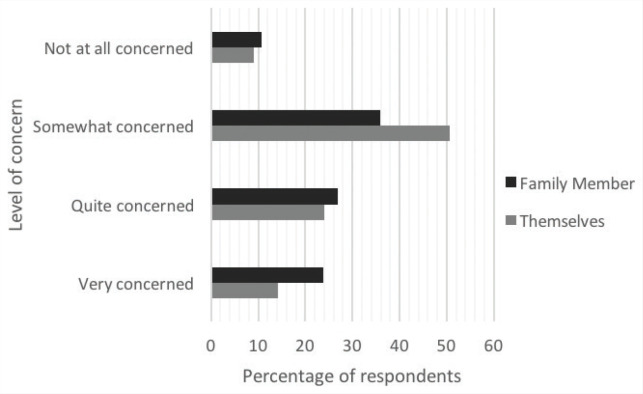
The survey showed that 32.17% (n = 111) of RRTs felt they were at an increased risk of contracting COVID-19 themselves, due to shortages or lack of PPE, and 40.87% (n = 141) felt at an increased risk due to overall decreases in hospital resources (staff, equipment, training). In total, 88.98% (n = 307) of RRTs felt some level of concern about being infected with COVID-19 themselves, and 86.67% (n = 299) felt concerned about someone in their immediate family becoming infected as a direct result of them working with positive patients (Figure 4).
Figure 4.
Respondents’ reported level of concern for themselves or their family members contracting COVID-19 as a result of their professional responsibilities.
Results showed that 19.7% (n = 68) of respondents had been tested for COVID-19, 10.4% (n = 36) had someone in their department who had contracted the virus, 1.74% (n = 6) had contracted COVID-19 themselves, and 19.42% (n = 67) had missed work due to isolation or illness. There were five free-text questions asked, with a total of 186 responses received, that related to health and safety or psychosocial risks. RRTs commented on a lack of training and education and again felt that there were issues with communication, conflicting information and instructions, and frequently changing guidelines. With PPE shortages, proper equipment was often difficult to access and couldn’t be used for learning and training. Some RRTs even felt obligated to purchase their own PPE for their safety. RRTs frequently felt that they were unnecessarily exposed due to equipment-sparing measures, especially near the beginning of the pandemic: “Some staff became positive after sparing measures early on,” and “Initially, procedure masks were not given to staff due to supply levels. Several staff members became Covid + from fellow staff and some from patients in ER where access to N95s was restricted.” Poor screening of patients, PPE that was difficult to access or used for multiple patients over extended periods of time, or even use of alternative PPE that didn’t fit as well, all led to potential exposures for RRTs. Many departments did not accommodate social distancing or allow for clean changing and eating areas away from work areas, often leaving RRTs to become unnecessarily infected by other staff within their own and other professions. RRTs reported feeling that their safety or the safety of patients was not always the highest priority. Conservation of PPE, financial implications, and even other professions felt like they were being prioritized over RRT staff safety: “We were asked to do the job of other professions so they did not have to be exposed (draw blood for the lab, perform ECG’s). We did not necessarily have to see these [patients] therefore we were being exposed more often and to [patients] that would not have been ours to treat.” PPE was reportedly available for some people, or some situations, which again led to perceived disorganization and confusion. Patients were still being brought in to appointments in some clinics, which may have led to unnecessary exposures for RRTs working there. Respondents frequently reported feeling that the overall quality of care they were able to provide was lower, and they were forced to withhold care on patients in certain circumstances. Many aerosol-generating medical procedures (AGMP) were initially being withheld on all patients, and they were often given alternative treatments that were viewed as less effective. In the most severe cases, ventilator access was restricted. Patients who refused intubation may not have been offered the usual comfort therapies, such as Hi flow oxygen or Bilevel Positive Airway Pressure therapy, as these were considered AGMPs.
To limit exposure, RRTs also reported performing fewer ventilator checks. RRTs working in clinics reported that many of their clinic and outpatient services were cancelled or restricted, leaving their patients without access to those services.
Provincial-level results
Respondents’ results were examined at a provincial level as well. The results and breakdown by province for some of the survey questions can be seen in Table 1. Some of the most impactful questions were included, and some provinces with similar COVID-19 case numbers were grouped to preserve anonymity in provinces with low response rates. COVID-19 case numbers and COVID-19-related deaths are also reported up to the survey closing date (6 July 2020). The results showed that the experiences were similar across the country when it came to communication challenges, stress or perceived risk, regardless of the number of positive COVID-19 cases.
DISCUSSION
The results of this study shed light on the experiences, challenges, and difficulties faced by RRTs working on the front lines of the COVID-19 pandemic in Canada. There were 345 completed survey responses from RRTs in 11/13 provinces and territories (Figure 1). According to the CIHI, there were 11,976 active RRTs in Canada in 2018 [19] giving a nearly 3% response rate for this survey. There were also 80% (n = 276) of respondents who self-identified as female and 20% (n = 69) who identified as male, which is consistent with the CIHI data showing that an average of 74.9% of RRTs in Canada in 2018 were females. The results highlight some of the concerns of the RRTs working during a pandemic, in an already stressful profession.
Workload
RRTs work in a variety of settings, both in and out of hospital, and may work varying schedules including shift work and on-call coverage. In anticipation of increased hospitalizations during COVID-19, many hospitals redeployed staff to help on the front lines and created space to accommodate the potential influx of infected individuals [20]. Most commonly, RRTs reported being required to work more (including mandated overtime shifts and being denied vacation time) during the pandemic. Some worked longer shifts or more hours each day; covered more on-call, nights, evenings, and weekends; or had fewer days off. Working with critically ill patients is physically demanding too, and this increase in workload was evidently felt within the profession. This level of physical demand without adequate rest and recovery has been linked to burnout, physical exhaustion, work-related injuries, and self-sacrifice [21]. In some cases, hospital departments increased their staffing to help with the increased workload, which meant more support for RRTs on each shift, but still meant an increase in staffing requirements. The unpredictability and constantly changing schedules were sources of stress and anxiety for many. Notably, the increase in work requirements was reported more dramatically in the mid- and eastern provinces than the western provinces (Table 1). While this may reflect the staffing models being used, and the ability to accommodate an influx of patients at baseline staffing levels, further research should be conducted to explain this difference.
The challenges highlighted here are important for both the physical and emotional health of RRTs, and should be considered by leadership and management for improved resource planning through future waves of COVID-19.
Communication
Though COVID-19 is similar to other known coronaviruses, such as Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome, COVID-19 is the first of these to cause a global pandemic [1]. In the age of social media and technology, new research, information, and best-practice guidelines can be disseminated more quickly than ever before, as can misinformation about the pandemic. As a result, the COVID-19 pandemic has also been accompanied by an infodemic, which caused significant confusion and anxiety [22]. This is particularly problematic for front-line workers who need timely access to the most current, consistent, and accurate information. RRTs in Canada were also faced with these issues of overwhelming amounts of information, difficulty in disseminating this new data in a timely manner, and conflicting information. Survey respondents overwhelmingly named this as one of the biggest challenges. Though only 2/9 free-text survey questions asked directly about communication, over half of the free-text responses received related to communication challenges. This is an indication to leadership about how significant the communication issues were for RRTs and reveals an area where more focus and emphasis should be placed on making improvements for the profession moving forward. As this was arguably the most significant challenge, and the one that was discussed most by survey respondents, it needs to be prioritized for improvement in relation to COVID-19 and in general within the profession.
The vast majority of RRTs reported that their department had implemented new treatment guidelines, specifically related to COVID-19 patients, often with regards to AGMPs such as intubation or extubation, mechanically ventilated patients, suctioning, and cardiac arrest procedures. Similarly, nearly all RRTs reported feeling overwhelmed by the new information and guidelines being introduced, and two-thirds had experienced issues with the communication of this new information. Staff felt confused, as information seemed contradictory or unclear, at times. For RRTs doing shift work, coming back to work after several days off caused significant anxiety, knowing that all of the practice guidelines would likely be different.
Although new guidelines were rapidly being introduced, RRTs reported that implementation felt very slow. While many respondents felt confident that they were being provided with the current best--practice guidelines for treating COVID-19 patients through their workplaces, implementation of these changes was slow to become formalized, and sometimes the recommendations had already changed again by that time. These challenges surrounding communication of crucial information, combined with delays in formalizing and implementing this information in practice led to confusion and inconsistency. These results highlight an opportunity for management and senior leadership to make improvements to the way that information is communicated. These continuously changing guidelines and protocols and lack of clear or consistent communication and leadership had a major impact and was a source of significant stress for the profession. In the hospital, RRTs work in so many different areas and are unique in that they are expected to know and work under the different protocols and guidelines in each of these areas. With most respondents reporting that they had received conflicting information in different care areas (intensive care unit versus emergency department, or different floors or patient wards, for example), this was a significant issue faced by RRTs. “Different areas of the hospital had their own protocols, which made it difficult because we had to know all of them,” and “…different interpretation and implementation of policy across the hospital” were two comments provided from respondents. One respondent also noted that different areas “…had different policies in place which made it difficult to know what respiratory care could be provided to each patient. Updates were made at different times and it was difficult and stressful to follow along.” While communication issues were not specific to the RRT profession [23], the experience of having to work in so many different care areas and be expected to know the nuances between the policies, guidelines, and expectations in each is unique to the RRT experience.
The confusion and inconsistencies were compounded by a perceived lack of leadership and guidance. At times, new policies were created by non-clinical team members and felt impractical. This lack of guidance and lack of confidence in the current protocols added to the confusion, anxiety and stress felt by many RRTs.
Health and safety risks
RRTs are put in many high-risk professional situations and are at a higher risk for respiratory infections and illnesses than other health professionals [24, 25]. RRTs are involved in most, or all AGMPs in the hospital. In the context of COVID-19, which is primarily spread through airborne droplets, this puts RRTs at the center of many high-risk moments for contracting the virus.
Over half of respondents had cared for a confirmed COVID-19 positive patient, and half had cared for an intubated COVID-19 patient. Endotracheal intubation and extubation are considered especially hazardous AGMPs [26]. Of all respondents, half reported being present for the intubation of a COVID-19 patient, with some being personally responsible for the intubation, and nearly one-third were responsible for the extubation of a COVID-19 patient.
An integral part of ensuring the personal safety of healthcare workers treating COVID-19 patients is the proper use of appropriate PPE. Droplet and contact precautions have been recommended for routine care of COVID-19 patients, and airborne precautions have been recommended for any AGMPs performed on confirmed or suspected positive patients [27]. Improper donning and doffing of PPE can lead to potential virus contamination, highlighting the importance of proper education, training and individual fit-testing of PPE [28]. The majority of respondents felt that they received adequate education and training around the use of PPE in the context of COVID-19 patients. They had undergone simulation training sessions, education sessions, and some hospitals had assigned “safety officers” to be available to observe and help, when required. However, some still reported feeling unprepared or confused about proper procedures and techniques. Less than one--quarter of respondents had not received additional PPE training to prepare for the pandemic, and a small number had still not been fit-tested for N95 masks.
PPE shortages were a major challenge reported by RRTs. The majority of respondents reported that their department had implemented equipment-sparing measures to save PPE, though few reported that their hospital had actually run out of PPE at the time of the survey. The impacts of these shortages were felt by RRTs across the country, nearly half of respondents reportedly feeling that they were at an increased risk of exposure to the virus as a direct result of resource shortages such as PPE, staff, or equipment. At the time the survey was completed, there were RRT respondents that had required COVID-19 testing, had someone in their department who had contracted the virus, or had tested positive themselves. At a time when RRTs were already being spread very thin, many RRTs also reported having missed work due to isolation or illness. This was very challenging for RRTs, who were forced to work short-staffed and left feeling like their safety was not a top priority, having frequently been unnecessarily exposed to COVID-19.
Psychosocial risks
The psychological toll on front line RRTs in the pandemic has been enormous. Stress, burnout, and compassion fatigue are all well-documented challenges facing critical care workers and RRTs caring for critically ill patients [29–31]. Burnout in front-line workers has been linked to a decrease in quality of care, patient satisfaction, productivity, and team morale, and an increase in medical errors and rates of turnover [21]. On a personal level, the emotional toll to healthcare professionals is significant as well, with burnout being tied to higher rates of substance abuse, depression, PTSD, and suicide [21]. As well as the health and well-being of their patients, RRTs working during the pandemic have been concerned for their own health and the health of their family members. The majority of RRTs were concerned about being infected because of their work with COVID-19 patients and the risk that this may pose to their family members (Figure 4).
There has been a significant emotional toll on RRTs in the pandemic. Respondents frequently reported feeling that the overall quality of care they were able to provide was lower, and they were forced to withhold care on patients in certain circumstances. Though RRTs are familiar with critical illness and death in their work, repeated exposures to these situations can cause significant emotional distress, anxiety, and stress [32]. Aside from COVID-19 patients, RRTs commented that they felt the overall quality of care for all patients was affected. For example, AGMP procedures were often temporarily being withheld which “…prevented some patients from receiving the optimal therapy (high flow nasal prongs, non-invasive ventilation, aerosol therapy,” and “necessary therapies had to be withheld from patients due to isolation or PPE concerns until COVID swab samples were received.” Care for non-COVID-19 patients was negatively impacted: “It was difficult treating emergency room and floor patients with COPD exacerbations that had symptoms of their pathology which were also symptoms of COVID,” and “In the midst of people being scared of getting COVID, I felt that the overall quality of care was less, instead of treating the obvious issues, care was delayed due to COVID concerns.” This feeling of also being unable to properly provide care for non-COVID-19 patients added to the emotional toll and stress of trying to make the best decisions for all patients in the face of so many new challenges.
Several strategies have been recommended to help build resilience and combat challenges like burnout, stress, and anxiety often facing front-line healthcare professionals. These interventions can be at an organizational level (improving staffing levels, education and infrastructure), at a team level (team-building and communication training, regular debriefing sessions, prioritizing just culture, and increased engagement from leadership and management), and an individual level (identifying the need for and availability of support, mental health wellness days, and follow-up on long-term ICU patients) [21]. Many or all these strategies would be beneficial to RRTs in the months and years to come and should be supported by their respective institutions and leadership teams.
Provincial-level results
The provinces were disproportionately affected by the initial waves of COVID-19. The number of positive COVID-19 cases and COVID-19-related deaths (Table 1) were much higher in some provinces than others. To observe the effect that this may have had on frontline RRTs and their experiences dealing with the pandemic, the results of survey questions relating to some of the most impactful issues were examined at a provincial level. Despite having lower overall numbers of positive COVID-19 cases, the Atlantic provinces reported some of the highest rates of increases or changes to working hours, along with Ontario and Quebec. British Columbia, Alberta, Saskatchewan, and Manitoba reported lower rates of increased work requirements.
When it came to encountering challenges with communication, feeling overwhelmed by new information and guidelines, and a perceived risk of potentially being exposed and infected with COVID-19, RRTs unquestionably reported having experienced these issues across the country, regardless of infection rates. The fear and concern about potentially being infected as a direct result of being a frontline RRT was reported conclusively in all provinces, in spite of the highly variable infection rates. Some respondents in provinces with lower COVID-19 rates commented that “…seeing what was transpiring in other provinces and the anticipation and preparation for the worst case scenario was very anxiety inducing in itself.” Overall, the differences among provinces were minimal in terms of the psychosocial toll of being a frontline RRT.
Limitations
One limitation of our study is a low response rate. Though response rates for surveys can vary considerably [33], online surveys typically have a response rate of 20%–30% [34]. With such a low response rate, there is potential for nonresponse bias and poor representation. Considering the themes that emerged from the survey results, including the increase in workload and stress for RRTs, it is not surprising that the response rate was low. RRTs are already so fatigued from working in the pandemic, the added responsibility of completing the survey would be challenging for many. We felt that the responses that we did receive were very valuable and provided rich insight into the lives of RRTs working during the pandemic. Future data collection of this type could be coordinated by the regulating bodies or professional associations, which might help to improve the response rates and mitigate some of the issues with poor representation and generalisability.
Another possible limitation is that our survey provides a picture of one small portion of the COVID-19 pandemic. As future “waves” continue to occur, RRTs will continue to be at the front lines. Some of the experiences may change, and new challenges may arise. As well, though we tried to make most of the survey questions applicable to RRTs working in all settings, many were specific to RRTs working in the hospital setting. We appreciate that RRTs are working in a large variety of settings throughout the pandemic, and this survey may not have been able to look at each of these specialty practices in detail.
Surveys are also susceptible to bias as a result of the subjective experiences of each individual respondent. Self-reporting is thought to rarely be an accurate account of events [35]. These subjective responses could potentially influence the overall results and impact the applicability of proposed findings. Though every attempt was made to ensure that the survey questions remained neutral, there is also a potential that biases from the research team could influence the wording of questions which could influence the way in which they were answered.
CONCLUSION
The results of our survey highlight the RRT experience during the COVID-19 pandemic. Though RRTs across the country may have experienced different approaches to preparing for the pandemic, the challenges, emotions, fears and triumphs were similar for everyone. RRTs are heavily involved in the care of infected individuals and the profession has many unique challenges. While challenges with communication and increased workload were not specific to this profession, the respiratory aspect of this virus and the massive reach of the RRT profession within the healthcare sector uniquely positions these professionals to be impacted by many of these issues in a very significant way. Further research is needed to quantify the extent of the differences between RRTs and other professions. The COVID-19 pandemic adds another layer of stress for RRT professionals, who are working in high-risk situations and feel anxious, overwhelmed, and concerned about their personal safety. Responses were collected near the beginning of the pandemic’s appearance in Canada and may help RRTs and respiratory departments prepare for the future of combating COVID-19. The results of this survey will also be useful to management and senior leadership and administration looking to understand some of the issues that RRTs encountered and how to address these in the future and moving forward through the pandemic.
Acknowledgments
Thank you to the CSRT and the provincial regulatory bodies that helped to distribute our survey to RRTs.
AUTHOR DISCLOSURES
Contributors
All authors contributed to the conception or design of the work, the acquisition, analysis, or interpretation of the data. All authors were involved in drafting and commenting on the paper and have approved the final version.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare no conflict of interest.
Ethical approval
This study was approved by our institutional research ethical board.
REFERENCES
- 1.Timeline of WHO’s response to COVID-19. World Health Organization (WHO); 2020. Available at: https://www.who.int/news-room/detail/29-06-2020-covidtimeline (Accessed August 25, 2020). [Google Scholar]
- 2.Coronavirus disease (COVID-19): Prevention and risks. Government of Canada; 2020. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks.html (Accessed August 24, 2020). [Google Scholar]
- 3.Coronavirus disease (COVID-19): Symptoms and treatment. Government of Canada; 2020. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/symptoms.html (Accessed August 27, 2020). [Google Scholar]
- 4.Coronavirus disease 2019 (COVID-19). Mayo Clinic; 2020. Available at: https://www.mayoclinic.org/diseases-conditions/coronavirus/symptoms-causes/syc-20479963 (Accessed August 27, 2020). [Google Scholar]
- 5.Symptoms of COVID-19. Centers for Disease Control and Prevention (CDC); 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (Accessed August 27, 2020). [Google Scholar]
- 6.Coronavirus Overview. World Health Organization (WHO); 2020. Available at: https://www.who.int/health-topics/coronavirus#tab=tab_1 (Accessed August 24, 2020). [Google Scholar]
- 7.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment of Coronavirus (COVID-19). StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 8.Covid-19’s Impact on Emergency Departments. CIHI; 2021. Available at: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/emergency-departments (Accessed January 15, 2022). [Google Scholar]
- 9.The RT Profession. Canadian Society of Respiratory Therapists (CSRT). Available at: http://www.csrt.com/rt-profession/ (Accessed August 30, 2020). [Google Scholar]
- 10.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020;17(5):259–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Z, Han B, Jiang R, et al. Mental health status of doctors and nurses during COVID-19 epidemic in China. 2020. [Google Scholar]
- 12.Nursing professionals pulse survey: 2020 pandemic. NurseGrid; 2020. Available at: https://nursegrid.com/help-nurses-now/survey-results/ (Accessed August 31, 2020). [Google Scholar]
- 13.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open 2020;3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu PE, Styra R, Gold WL. Mitigating the psychological effects of COVID-19 on health care workers. CMAJ 2020;192(17):E459–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grimm CA. Hospital experiences responding to the COVID-19 pandemic: Results of a National Pulse Survey March 23–27, 2020. In US Department of health and human services OoIG. pp. 1–41. 2020. [Google Scholar]
- 16.Summary of survey results: Current impact of COVID-19 on national healthcare organizations and their members. HEAL: Organizations for Health Action. Available at: https://static1.squarespace.com/static/5cd45467fb22a5107d310b81/t/5e8e788c971c052db420cfcb/1586395277826/HEAL+COVID+survey+results+March+2020_forGov_v3.pdf (Accessed August 31, 2020). [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software partners. J Biomed Inform 2019. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canadian Institute for Health Information. Canada’s health care providers, 2014 to 2018 — Data tables. Ottawa, ON: CIHI; 2020. [Google Scholar]
- 20.Zangrillo A, Beretta L, Silvani P, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit Care Resusc 2020;22(2):91–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hancock J, Witter T, Comber S, et al. Understanding burnout and moral distress to build resilience: a qualitative study of an interprofessional intensive care unit team. Can J Anesth 2020;67(11):1541–8. [DOI] [PubMed] [Google Scholar]
- 22.Zhu Z, Lian X, Su X, et al. From SARS and MERS to COVID-19: a brief summary and comparison of severe acute respiratory infections caused by three highly pathogenic human coronaviruses. Respir Res 2020;21(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shinners J, Cosme S. COVID-19: perspectives from nurses across the country. J Cont Educ Nurs 2020;51(7):304–8. [DOI] [PubMed] [Google Scholar]
- 24.Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care 2015;60(10):1409–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaur R, Weiss TT, Perez A, et al. Practical strategies to reduce nosocomial transmission to healthcare professionals providing respiratory care to patients with COVID-19. Crit Care 2020;24(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weissman DN, De Perio MA, Radonovich LJ. COVID-19 and risks posed to personnel during endotracheal intubation. JAMA 2020;323(20):2027–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.IPAC recommendations for use of personal protective equipment for care of individuals with suspect or confirmed COVID-19. Public Health Ontario. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/updated-ipac-measures-covid-19.pdf?la=en (Accessed October 30, 2020). [Google Scholar]
- 28.Muñoz-Leyva F, Niazi AU. Common breaches in biosafety during donning and doffing of protective personal equipment used in the care of COVID-19 patients. Can J Anaesth 2020;67(7):900–1. doi: 10.1007/s12630-020-01648-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saravanabavan L, Sivakumar MN, Hisham M. Stress and burnout among intensive care unit healthcare professionals in an Indian Tertiary Care Hospital. Indian J Crit Care Med 2019;23(10):462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fumis RRL, Amarante GAJ, De Fátima Nascimento A, Junior JMV. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann Intensive Care 2017;7(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholar 2016;48(5):456–65. [DOI] [PubMed] [Google Scholar]
- 32.Mahan K. Death and dying: tools to help respiratory therapists handle frequent exposure to end of life care. J Allied Health 2019;48(1):72–5. [PubMed] [Google Scholar]
- 33.Abbo L, Lo K, Sinkowitz-Cochran R, et al. Antimicrobial stewardship programs in Florida’s acute care facilities. Infect Contr Hosp Epidemiol 2013;34(6):634–7. [DOI] [PubMed] [Google Scholar]
- 34.Safdar N, Abbo LM, Knobloch MJ, Seo SK. Research methods in healthcare epidemiology: survey and qualitative research. Infect Contr Hosp Epidemiol 2016;37(11):1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tempelaar D, Rienties B, Nguyen Q. Subjective data, objective data and the role of bias in predictive modelling: lessons from a dispositional learning analytics application. PLoS One 2020;15(6):e0233977. [DOI] [PMC free article] [PubMed] [Google Scholar]