Abstract
Background
The acceptability of COVID-19 vaccine varies depending on the time, place, type of vaccine and information available at the time. Knowledge of attitudes and practices towards COVID-19 among the population at high risk of developing the disease would help to tailor the strategy to improve adherence to vaccination recommendations.
Aim
To analyze the willingness, knowledge and risk perception of patients and health care workers (HCW) to get the vaccines against SARS-CoV-2.
Methods
Cross-sectional survey in Araba/Álava province (Spain). Subjects who met the criteria for the influenza vaccination in 2019 and HCWS from the Basque Public Health Service were included. The participants answered a questionnaire on the knowledge, attitudes and practices towards COVID-19 before starting vaccination against SARS-CoV-2. The intention to vaccinate was compared using the chi-squared test.
Results
316 HCWs and 389 patients responded to the survey. Around 90% of the patients and 80% of HCW would accept vaccination in all scenarios according to the questionnaire (p < 0.001). Only 3–12% hesitated about the COVID-19 vaccines. Compared to 40–70% of patients, 60–80% of HCWs perceived a high risk of COVID-19 (p < 0.001). Statistically significant differences were found in 10 of the 17 questions regarding the mechanism of transmission and symptoms.
Conclusion
HCWs had a better knowledge and risk perception of COVID-19 than the surveyed patients. They had a higher proportion of hesitancy to get COVID-19 vaccine, probably related to doubts about the effectiveness of the new vaccines and the scientific evidence.
Keywords: COVID-19, Knowledge, Attitudes, Practices, Vaccine, Healthcare workers
Introduction
On the 31st of December 2019, a new coronavirus was identified as the etiological agent of pneumonia cases reported in Wuhan (China). The new virus was named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and caused the coronavirus disease 2019 (COVID-19). The World Health Organization (WHO) declared COVID-19 a Public Health Emergency of International Concern on the 30th of January 2020 and a pandemic on the 11th of March 2020. The COVID-19 has rapidly become a major global public health crisis, affecting 524 million people around the world and causing 6 million deaths [1]. A systematic review of 53,000 hospitalized patients indicated that 20.2% of COVID-19 cases developed severe disease with a mortality rate of 3.1% [2]. Older adults and those with underlying health conditions are at greatest risk for severe infection and death due to COVID-19 [3]. Health care workers (HCWs) are also extremely vulnerable to SARS-CoV-2 infection since they are frequently in contact with COVID-19 patients. According to a recent report, in some countries nearly 10–20% of HCWs are been infected with SARS-CoV-2 [4].
During the initial few pandemic waves several drugs were used to treat severe COVID-19 patients, but with very limited success. Social distancing strategies are effective for mitigating the COVID-19, but such measures are very costly due to their impact on the economic activity. Besides, the durability of the immunity against SARS-CoV-2 has not yet been fully established [5]. Therefore, increasing the proportion of immune individuals among HCWs and the general population by an efficacious vaccination program is essential to mitigate both, the disease and the resulting deaths.
However, vaccine availability does not guarantee sufficient vaccination coverage due to vaccine hesitancy [6]. The rise of vaccine hesitancy, including the delay or total refusal to immunization, poses a real threat to the fight against vaccine-preventable disease outbreaks, and is being increasingly recognized as a barrier to the success of immunization programs. Indeed, in 2019 the WHO listed vaccine hesitancy as one of the top ten threats to global health [7]. Vaccine hesitancy is complex and context-specific varying across time, place and type of vaccine. Factors such as complacency, convenience and confidence play an important role in vaccine hesitancy [8]. Furthermore, vaccine hesitancy can have effects for both, the individual and potentially the community.
On the 6th of January 2021, two COVID-19 vaccines with efficacy to reduce symptomatic infection risk greater than 90% were approved, and 16 candidate vaccines were in phase 3 trials. Vaccine acceptance-rates varies substantially across countries and is generally lower in the working-age population than in older people [9]. In HCWs, vaccination intention-rates range from 40% to 70% [9]. This is relevant because clinicians are a trustworthy and creditable source of vaccine-related information for patients and, therefore, can improve adherence to vaccination recommendations.
According to a systematic review of 126 surveys on COVID-19 published before November 2020, COVID-19 vaccine hesitancy was increasing worldwide [10]. COVID-19 vaccine hesitancy might represent an important hurdle to achieving herd immunity [11], [12].
People who are at increased risk of becoming severely ill from COVID-19 and HCWs are priority targets for vaccination and are, therefore, affected by vaccine hesitancy. Thus, we analyzed the acceptability of the vaccines against SARS-CoV-2 in the population targeted for both SARS-CoV-2 and influenza vaccination (people older than 65, pregnant women, HCWs, people with chronic diseases). Additionally, we assessed the knowledge and risk perception of COVID-19.
Methods
We performed a cross-sectional survey study in 81.423 subjects who met the criteria for influenza vaccination in 2019 (patients henceforth) in Araba/Alava (northern region of Spain). Before starting vaccination against SARS-CoV-2, a sample of patients was surveyed over the telephone and an electronic form was sent to the HCWs of Basque Public Health Service of the Alava province. All subjects signed an informed consent prior to their participation in the study. HCWs were surveyed between the 14th of December 2020 and the 11th of January of 2021. And patients between the 7th of January of 2021 and the 23th February of 2021.
Sample and procedure
Under the worst-case assumption that q = p = 0.5 and with a sampling error of ± 5%, we estimated that 385 subjects would need to be surveyed. Considering a refusal rate of 40%, the total number of subjects to be surveyed was 539 [13].
Patients were selected, amongst influenza vaccination target groups, by random cluster sampling according to gender, age (over/under 65 years), influenza vaccination, and COVID-19 infection. In December 2020, an invitation letter was sent to 517 subjects, the remaining 22 did not have a postal address (first round). At the end of January 2021 vaccination had not yet begun in the group of patients in the study (except for those in nursing homes), so we performed a second round to reach the estimated sample size and we invited 279 more subjects. In any case, participants were asked whether they had received the COVID-19 vaccine and if so, this was considered an exclusion criterion. Those subjects with a severe cognitive or hearing impairment, HCWs, children and deceased subjects who were not recorded by the system were also excluded from the study. Several calls were made to patients in different time slots until the subjects were contacted and the survey completed. The reason for non-inclusion in the study was also recorded.
HCWs from the Basque Public Health Service of Araba/Alava (including medical doctors, nurses and administrative staff from hospital and primary care) were invited to participate by electronic mailing and the surveys were completed using an online form.
The study was approved by the Ethics Committee for Clinical Research of Araba/Alava (Expte. 2020-048) and the data management was approved by the Data Protection Officer in accordance with the General Data Protection Regulation of the Basque Public Health Service.
Measurement tool
Data were collected with a self-administered questionnaire, which was developed based on the COVID-19 Behaviour Insights- tool- from WHO Regional Office for Europe [14] and a survey used by Apiñaniz et al. [15]. Two new questions were added to the survey (Q10 and Q18) in the part 1 of questionnaire.
The questionnaire had 34 items divided into four parts: demographics (Q1-Q9), attitudes towards COVID-19 vaccines (Q10-Q18), questions on COVID-19-related knowledge (Q19-Q23) and questions related to risk perception and severity of the disease (Q24-Q34) (Anex I). Response categories included “yes,” “no,” and “don't know/no answer” (hesitant/undecided). The items related to the COVID-19 symptoms and SARS-CoV-2 virus transmission were multiple-choice questions.
The Electronic Health Record information register was used to collect patient information on comorbidities (diabetes mellitus, heart disease, COPD), previous SARS-CoV-2 infection, influenza vaccination in 2019, resident patient and MEDEA deprivation index [16].
Statistical analysis
The main characteristics of the sample were described. The primary endpoint was determined by calculating the absolute and relative frequencies of HCWs and remaining study subjects who intended to get a COVID-19 vaccine. Finally, the intention to get vaccinated in patients and HCWs was compared using the chi-squared test.
A statistical significance level of p = 0.05 was considered in the analysis. Statistical analysis was performed with IBP SPSS Statistics, version 23 for Windows.
Results
Study population
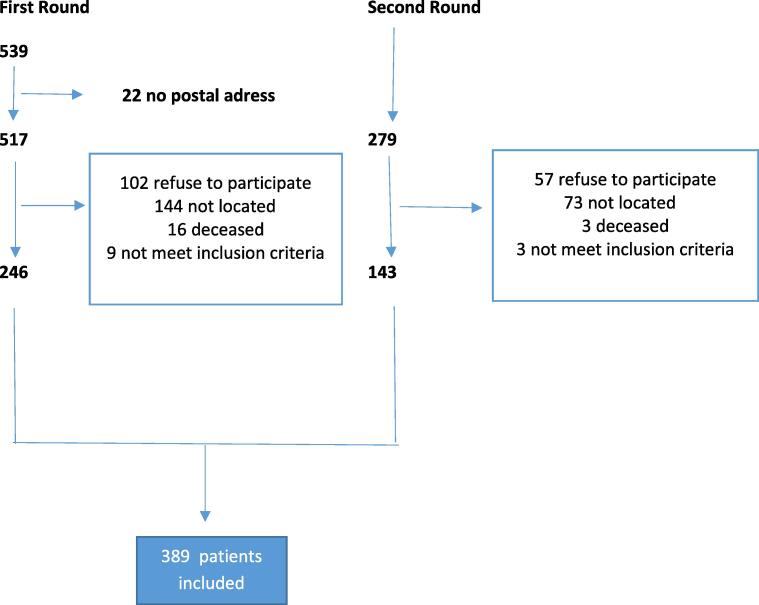
We contacted 796 participants by telephone and 389 of them (48.9%) completed the survey. Regarding the remaining 407, we could not reach 217 people (53.3%) (incorrect telephone number/did not pick up), 159 (38.8%) refused to answer, 12 (2.9%) did not meet the inclusion criteria and 19 were dead (Fig. 1). Additionally, 8.9% of the 3,558 HCWs of the Basque Public Health System of Araba/Alava answered the electronic survey (75 doctors, 124 nurses and 117 classified as other professionals).
Fig. 1.
Flow chart of subjects included in the study.
The study included 316 HCWs and 389 patients who responded to the survey. Most of them were female (80% and 50% respectively) and they had a mean age of 45 and 71 years, respectively. In the previous year, 45% of the HCWs and 63% of the patients were vaccinated against influenza and around 80% had been vaccinated on previous occasions in both groups. Twenty per cent of the HCWs and 2% of patients had been infected by SARS-CoV-2 (Table 1).
Table 1.
Characteristics of the study subjects.
|
Patients (n=389) |
Professionals (n=316) |
TOTAL (n=705) |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age | ||||||
| < 65 years old | 69 | 17.7 | 307 | 97.2 | 376 | 53.3 |
| ≥ 65 años | 315 | 81.0 | 2 | 0.6 | 317 | 45.0 |
| DK/DA | 5 | 1.3 | 7 | 2.2 | 12 | 1.7 |
| Sex | ||||||
| Man | 190 | 48.8 | 58 | 18.4 | 248 | 35.2 |
| Woman | 194 | 49.9 | 252 | 79.7 | 446 | 63.3 |
| DK/DA | 5 | 1.3 | 6 | 1.9 | 11 | 1.6 |
| Education | ||||||
| No education | 125 | 32.1 | ||||
| Basic/Middle | 196 | 50.4 | ||||
| University | 66 | 17.0 | ||||
| DK/DA | 2 | 0.3 | ||||
| Employment status | ||||||
| Worker | 44 | 11.3 | 316 | 100 | 360 | 51.1 |
| Not working (retired/unemployed) | 251 | 64.5 | - | - | 251 | 35.7 |
| DK/DA | 94 | 24.3 | - | - | 94 | 13.3 |
| Marital status | ||||||
| Single | 61 | 15.6 | 94 | 29.7 | 155 | 21.9 |
| Married/Couple | 267 | 68.6 | 201 | 63.6% | 468 | 66.4 |
| Widowed | 54 | 13.9 | 54 | 7.7 | ||
| DK/DA | 7 | 1.8% | 21 | 6.6% | 28 | 4 |
| Flu vaccinated 2019 | ‘ | |||||
| Yes | 245 | 63.0 | 144 | 45.6 | 389 | 55.2 |
| No | 144 | 37.0 | 170 | 53.8 | 314 | 44.5 |
| DK/DA | - | - | 2 | 0.6 | 2 | 0.3 |
| On some occasion | ||||||
| Yes | 335 | 86.1 | 241 | 76.3 | 576 | 81.7 |
| No | 54 | 13.9 | 72 | 22.8 | 126 | 17.9 |
| DK/DA | 3 | 0.9 | 3 | 0.4 | ||
| COVID-19 infection | ||||||
| Yes | 9 | 2.3 | 64 | 20.3 | 73 | 10.4 |
| No | 380 | 97.7 | 242 | 76.6 | 622 | 88.2 |
| DK/DA | 10 | 3.2 | 10 | 3.2 | ||
| Resident | 1 | 0.3 | ||||
| DK/DA | 5 | 1.3 | ||||
| Diabetes Mellitus | 86 | 22.1 | ||||
| DK/DA | 260 | 66.8 | ||||
| Heart disease | 24 | 6.2 | ||||
| DK/DA | 260 | 66.8 | ||||
| COPD | 26 | 6.7 | ||||
| DK/DA | 260 | 66.8 | ||||
| MEDEA deprivation index | 2.84 ± 1.35 | |||||
| Quintil 1 | 84 | 21.6 | ||||
| Quintil 2 | 68 | 17.5 | ||||
| Quintil 3 | 77 | 19.8 | ||||
| Quintil 4 | 87 | 22.4 | ||||
| Quintil 5 | 45 | 11.6 | ||||
| Missing | 27 | 7.0 | ||||
DK = Do not Know.
DA = Do not Answer.
COPD = Chronic Obstructive Pulmonary Disease.
Attitudes towards vaccines against SARS-CoV-2
When respondents were asked whether they would get a COVID-19 vaccine if it was offered for free (Q11) 93% (n = 363; 95% confidence interval 91–96%) of the patients and 81% (n = 256; 95% confidence interval 76–86%) of HCWs answered yes (Table 2). The response was similar if the price of the vaccine would be 10 euros (Q12), if the vaccine was recommended for them (Q10) or when they belonged to one of the risk groups (Q14). The differences between the two groups were statistically significant in all cases, reaching the lowest value in the latter case.
Table 2.
Acceptability of the SARS-Cov2 vaccine.
| Yes |
No |
pa | Uncertain |
pb | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Q10- Would you get vaccinated if were recommended for you? | ||||||||
| Patients | 355 | 91.3 | 17 | 4.4 | 0.213 | 17 | 4.4 | <0.00 |
| Professionals | 259 | 82.0 | 20 | 6.3 | 37 | 11.7 | 1 | |
| Q11- Would you get vaccinated if the vaccine was free? | ||||||||
| Patients | 363 | 93.3 | 14 | 3.6 | 0.006 | 12 | 3.1 | <0.00 |
| Professionals | 256 | 81.0 | 26 | 8.2 | 34 | 10.8 | 1 | |
| Q12- Would you get vaccinated if the vaccine cost €10? | ||||||||
| Patients | 330 | 84.8 | 32 | 8.2 | 0.054 | 27 | 6.9 | 0.011 |
| Professionals | 240 | 75.9 | 39 | 12.3 | 37 | 11.7 | ||
| Q14- Would you get vaccinated if you belonged to a risk group? | ||||||||
| Patients | 346 | 88.9 | 16 | 4.1 | 0.178 | 27 | 6.9 | 0.016 |
| Professionals | 257 | 81.3 | 20 | 6.3 | 39 | 12.3 | ||
| Q16- Do you think the vaccine to prevent COVID-19 is effective? | ||||||||
| Patients | 262 | 67.4 | 10 | 2.6 | 0.655 | 117 | 30.1 | 0.001 |
| Professionals | 171 | 54.1 | 9 | 2.9 | 136 | 43.0 | ||
| Q17- Do you think the vaccine to prevent COVID-19 has been sufficiently researched? | ||||||||
| Patients | 225 | 57.8 | 78 | 20.1 | <0.00 | 86 | 22.1 | <0.00 |
| Professionals | 127 | 40.2 | 96 | 30.4 | 1 | 93 | 29.4 | 1 |
| Q18- Would you get vaccinated later? | ||||||||
| Patients | 366 | 94.1 | 9 | 2.3 | 0.299 | 14 | 3.6 | 0.020 |
| Professionals | 279 | 88.3 | 12 | 3.8 | 25 | 7.9 | ||
Calculated without taking into account undecideds.
Adjusted for undecideds.
We found a 3–7% (n = 12–27) of vaccine hesitancy in all scenarios in the patient group, and 10–12% in the HCWs (n = 34–39). Only 4–8% of patients and 6–12% of HCWs would refuse to get a COVID-19 vaccine.
More than half of the respondents believed the vaccines were effective (Q16), 67% of patients (n = 263; 95% confidence interval 61–73%) and 54% of HCWs (n = 171; 95% confidence interval 47–62%). About 3% believed new COVID-19 vaccines were not effective in both groups and 30–40% were unclear. Furthermore, 58% (n = 226; 95% confidence interval 52–64%) of patients thought that the vaccines had been sufficiently investigated (Q17), compared to 40% (n = 127; 95% confidence interval 32–49%) of HCWs. Around 20–30% of respondents believed that there has not been sufficient research on the COVID-19 vaccines and 22–29% were undecided. In both groups of respondents, around 90% would prefer to get the COVID-19 vaccine later in time (Q18).
Knowledge about the COVID-19 and risk perception
We found statistically significant differences in the responses given by patients and HCWs in eight of the 11 questions on mechanisms of disease transmission (Q19-Q21) and in two of the six questions on symptoms (Q22) (Table 3a,b).
Table 3a.
Knowledge about COVID-19 (multiple choice questions).
|
Yes |
No |
p |
|||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Q19- Indicate the most common ways in which COVID-19 is transmitted | |||||
| Drops produced when coughing or talking | |||||
| Patients | 343 | 88.2 | 46 | 11.9 | <0.001 |
| Professionals | 316 | 100 | 0 | 0 | |
| Touching contaminated surfaces | |||||
| Patients | 303 | 77.9 | 86 | 22.1 | 0.196 |
| Professionals | 232 | 73.4 | 84 | 26.6 | |
| Physical contact with someone infected | |||||
| Patients | 326 | 83.8 | 63 | 16.2 | 0.383 |
| Professionals | 256 | 81.0 | 60 | 19.0 | |
| Through the air | |||||
| Patients | 278 | 71.5 | 111 | 28.5 | 0.019 |
| Professionals | 251 | 79.4 | 65 | 20.6 | |
| By blood transfusion | |||||
| Patients | 124 | 31.9 | 265 | 68.1 | <0.001 |
| Professionals | 13 | 4.1 | 303 | 95.9 | |
| Through the pets | |||||
| Patients | 71 | 18.3 | 318 | 81.7 | <0.001 |
| Professionals | 7 | 2.2 | 309 | 97.8 | |
| Through an insect bite | |||||
| Patients | 102 | 26.2 | 287 | 73.8 | <0.001 |
| Professionals | 1 | 0.32 | 315 | 99.7 | |
| Q20- How do you think you could become infected? | |||||
| When you go shopping | |||||
| Patients | 262 | 67.4 | 127 | 32.6 | 0.663 |
| Professionals | 207 | 65.5 | 109 | 34.5 | |
| When using public transport | |||||
| Patients | 296 | 76.1 | 93 | 23.9 | <0.001 |
| Professionals | 275 | 87.0 | 41 | 13.0 | |
| At work | |||||
| Patients | 181 | 46.5 | 208 | 53.5 | <0.001 |
| Professionals | 299 | 94.6 | 17 | 5.4 | |
| Q22 – What are the most common symptoms of COVID-19? | |||||
| Fever | |||||
| Patients | 366 | 94.1 | 23 | 5.9 | 0.001 |
| Professionals | 313 | 99.0 | 3 | 1.0 | |
| Cough | |||||
| Patients | 326 | 83.8 | 63 | 16.2 | <0.001 |
| Professionals | 294 | 93.0 | 22 | 7.0 | |
| Lack of air | |||||
| Patients | 331 | 85.1 | 58 | 14.9 | 0.365 |
| Professionals | 260 | 82.3 | 56 | 17.7 | |
| Fatigue | |||||
| Patients | 309 | 79.4 | 80 | 20.6 | 0.522 |
| Professionals | 258 | 81.6 | 58 | 18.4 | |
| Pain | |||||
| Patients | 291 | 74.8 | 98 | 25.2 | 0.147 |
| Professionals | 220 | 69.6 | 96 | 30.4 | |
| Diarrhoea | |||||
| Patients | 224 | 57.6 | 165 | 42.4 | 0.397 |
| Professionals | 171 | 54.1 | 145 | 45.9 | |
| Q23- How did you mainly find out about COVID-19? | |||||
| Ministry of Health or health care professionals | |||||
| Patients | 117 | 30.1 | 272 | 69.9 | <0.001 |
| Professionals | 267 | 84.5 | 49 | 15.5 | |
| The media | |||||
| Patients | 352 | 90.5 | 37 | 9.5 | <0.001 |
| Professionals | 211 | 66.8 | 105 | 33.2 | |
| Social media | |||||
| Patients | 62 | 15.9 | 327 | 84.1 | 0.001 |
| Professionals | 82 | 25.9 | 234 | 74.1 | |
| Other media | |||||
| Patients | 65 | 16.7 | 324 | 83.3 | <0.001 |
| Professionals | 95 | 30.1 | 221 | 69.9 | |
| I am not looking for information | |||||
| Patients | 4 | 1.0 | 385 | 99.0 | 0.047 |
| Professionals | 11 | 3.5 | 305 | 96.5 | |
The most frequent transmission mechanisms selected by both patients and HCWs were: drops produced when coughing or talking, physical contact (reported by 80–100%), contaminated surfaces, air and public transport (reported by 70%). A higher proportion of HCWs believed they could be contagious at work (95% versus 47%, p < 0.001) and that people without fever could be contagious (98% versus 75%, p < 0,001), as compared to patients.
Regarding knowledge of COVID-19 risk groups (Q13), 96% of HCWs reported they had knowledge of such risk groups, compared to 70% of patients (p < 0.001). Fever, cough, shortness of breath and tiredness were the most frequent symptoms reported by 80–100% of patients and HCWs (Q22).
The Ministry of Health and the media were the main sources of information for HCWs, with percentages of 85% and 67%, respectively (Q23). While 90% of patients reported getting the information through the media.
We found a higher proportion of HCWs perceiving a high-risk of COVID-19 as compared to patients (60–80% versus 40–70%, p < 0.001) (Table 4a,b) (Q29-Q31). In both groups, the perception of high-risk of COVID-19 in the general population was higher than the perception of high-risk among members of the family or for the person questioned. Over 50% believed the COVID-19 caused much more harm, many more infected persons and many more deaths than seasonal influenza (Q32-Q34).
Table 4a.
Perception of risk and severity (yes or no questions).
| Yes |
No |
pa | Uncertain |
pb | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Q29- Do you think you are at high risk for COVID-19 infection? | ||||||||
| Patients | 159 | 40.9 | 201 | 51.7 | <0.001 | 29 | 7.5 | <0.001 |
| Professionals | 193 | 61.1 | 89 | 28.2 | 34 | 10.8 | ||
| Q30- Do you think there is a high risk for COVID-19 infection in your family? | ||||||||
| Patients | 194 | 49.9 | 168 | 43.1 | <0.001 | 27 | 6.9 | <0.001 |
| Professionals | 220 | 69.6 | 59 | 18.7 | 37 | 11.7 | ||
| Q31- Do you think there is a high risk for COVID-19 infection in the general population? | ||||||||
| Patients | 266 | 68.4 | 81 | 20.8 | <0.001 | 42 | 10.8 | 0.001 |
| Professionals | 254 | 80.4 | 35 | 11.1 | 27 | 8.5 | ||
| Q25- Do you believe that COVID-19 can cause serious and irreversible effects in the general population? | ||||||||
| Patients | 331 | 85.1 | 26 | 6.7 | 0.462 | 32 | 8.2 | 0.662 |
| Professionals | 273 | 86.4 | 16 | 5.1 | 27 | 8.5 | ||
| Q27- Do you think there are sick people who have been infected with COVID-19 and have not realized it? | ||||||||
| Patients | 26 | 6.7 | 363 | 93.3 | <0.001 | 0 | 0 | <0.001 |
| Professionals | 1 | 0.3 | 306 | 96.8 | 9 | 2.8 | ||
| Q28- Do you think it is a disease that concerns the majority of the population in Vitoria-Gasteiz? | ||||||||
| Patients | 177 | 45.5 | 171 | 44.0 | 0.007 | 41 | 10.5 | 0.006 |
| Professionals | 107 | 33.9 | 163 | 51.6 | 46 | 14.6 | ||
Calculated without taking into account undecideds.
Adjusted for undecideds.
Table 4b.
Perception of risk and severity (more than two options questions).
| Patients |
Professionals |
pa | pb | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Q24- What mortality rate do you think COVID-19 has in the general population? | ||||||
| <1% | 43 | 11.1 | 66 | 21.0 | <0.001 | <0.001 |
| 1-5% | 140 | 36.0 | 169 | 53.8 | ||
| >5% | 106 | 27.2 | 28 | 8.9 | ||
| Uncertain | 100 | 25.7 | 51 | 16.2 | ||
| Q26- How many deaths do you think Covid-19 will cause in Vitoria-Gasteiz in 2021? | ||||||
| None | 3 | 0.8 | 0 | 0.0 | <0.001 | <0.001 |
| 1-10 | 21 | 5.4 | 2 | 0.6 | ||
| 11-50 | 53 | 13.6 | 27 | 8.6 | ||
| >50 | 233 | 59.9 | 214 | 68.2 | ||
| Uncertain | 79 | 20.3 | 71 | 22.6 | ||
| Q32- How many deaths do you think COVID-19 causes in relation to influenza? | ||||||
| Many less | 6 | 1.5 | 19 | 6.0 | <0.001 | 0.001 |
| A few less | 18 | 4.6 | 22 | 7.0 | ||
| The same | 38 | 9.8 | 13 | 4.1 | ||
| A few more | 81 | 20.8 | 56 | 17.7 | ||
| Many more | 203 | 52.2 | 174 | 55.1 | ||
| Uncertain | 43 | 11.1 | 32 | 10.1 | ||
| Q33- How many people do you think get sick from COVID-19 compared to seasonal flu? | ||||||
| Many less | 3 | 0.8 | 24 | 7.6 | <0.001 | <0.001 |
| A few less | 24 | 6.2 | 19 | 6.0 | ||
| The same | 36 | 9.3 | 18 | 5.7 | ||
| A few more | 77 | 19.8 | 68 | 21.5 | ||
| Many more | 206 | 53.0 | 153 | 48.4 | ||
| Uncertain | 43 | 11.1 | 34 | 10.8 | ||
| Q34- How much harm do you think Covid-19 can do to you regarding seasonal flu? | ||||||
| Many less | 2 | 0.5 | 1 | 0.3 | 0.566 | 0.549 |
| A few less | 8 | 2.1 | 4 | 1.3 | ||
| The same | 19 | 4.9 | 20 | 6.3 | ||
| A few more | 74 | 19.0 | 50 | 15.8 | ||
| Many more | 248 | 63.8 | 217 | 68.7 | ||
| Uncertain | 38 | 9.8 | 24 | 7.6 | ||
Calculated without taking into account undecideds.
Adjusted for undecideds.
Table 3b.
Knowledge about COVID-19 (yes or no questions).
| Yes |
No |
pa | Uncertain |
pb | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Q21- Do you think that people without fever can be contagious? | ||||||||
| Patients | 291 | 74.8 | 26 | 6.7 | <0.001 | 72 | 18.5 | <0.001 |
| Professionals | 308 | 97.5 | 1 | 0.3 | 7 | 2.2 | ||
| Q13- Do you know the risk groups for SARS-Cov-2 infection? | ||||||||
| Patients | 273 | 70.2 | 97 | 24.9 | <0.001 | 19 | 4.9 | <0.001 |
| Professionals | 304 | 96.2 | 5 | 1.6 | 7 | 2.2 | ||
| a Calculated without taking into account undecideds | ||||||||
| b Adjusted for undecideds | ||||||||
Calculated without taking into account undecideds.
Adjusted for undecideds.
Around 85% of patients and HCWs considered that COVID-19 could cause serious and irreversible effects (Q25). Sixty percent of both, HCWs and patients thought that by 2021 there would be more than 50 deaths from COVID-19 in their city of residence (Vitoria-Gasteiz, administrative capital of the Basque Country) (Q26). However, 50% of the enquired HCWs believed that mortality due to COVID-19 in the general population is 1–5% compared to 36% of patients (Q24).
Discussion
Before the beginning of the SARS-CoV-2 vaccination campaign in the province of Araba/Alava, the majority of the at-risk population was willing to receive a COVID-19 vaccine. Specifically, 90% of patients and 80% of HCWs would agree to get vaccinated. These results were confirmed by current vaccination data [17]. Vaccination-rates against COVID-19 in our country are among the highest in the world. However, the intention of the population to get a COVID-19 vaccine changes depending on the time of the survey, among other factors. Thus, according to the results of cross-sectional internet surveys conducted in April and May 2020, 58 to 69% of adults intended to get a vaccine against COVID-19 [18], [19]. From June to December 2020 other studies that surveyed more than 13,000 people in 19 countries found that 70% of the population was willing to receive COVID-19 vaccine [11], [12], [20]. Inter-country variability ranged from 90% (Vietnam, India, China, Denmark and South Korea) to 40% (Serbia, Croatia and France). Nevertheless, Szilagyi et al. [21] tracked the same subjects over time and reported that the willingness to get the COVID-19 vaccine decreased from 74% to 56% between April and December 2020.
Regarding HCWs, previous reports suggest that willingness to get a COVID-19 vaccine laid between 40% and 75% during the first infection wave [22], [23] (43% February 2020 in Greece and 74% March-July 2020 in France), as well as during the second and third waves [24], [25], [26] (October-November 36% in Mexico and Texas and 70% in France, Italy and 60% November-December in Philadelphia and New York). In contrast to our study, other studies observed that self-reported willingness to receive vaccination against COVID-19 differs according to hospital roles [23], [25], with physicians and research scientists showing the highest acceptance.
We found hesitancy vaccination-rates of 3–12%, with significantly lower percentages among patients than among HCWs. Such rates ranged between 20 and 30% in other studies and were similar to those reported by other authors for health professionals [22], [23], [24], [25], [26] and the general population [27], [28].
Hesitancy against vaccination was mostly influenced by the characteristics of the new vaccines, the clinical evidence on the efficacy and the potential side effects, as well as the national vaccination strategy, among various other factors [24], [25], [27]. Safety (69–85%), effectiveness (69%) and speed of development/approval (74%) were noted as the most common concerns regarding the COVID-19 vaccines in HCWs [25], [29]. While the general population was more concerned about the effectiveness (81%) and the potential side effects of the vaccines (58%) [19]. In addition, trust towards scientific research and the attitude towards vaccines’ efficacy decreased in the second wave compared to the first [30].
Focusing on the enquired high-risk population of developing COVID-19 severe disease in Araba/Alava, 30–40% hesitated about the effectiveness of the vaccine or did not answer and 3% believed it was not effective. Twenty to 30% thought there had not been sufficient research and 20–30% did not know or did not answer. Around 90% of both, patients and HCWs would have delayed vaccination compared to 66.5% of the health care workers participating in the survey conducted by Gadoth et al.[31].
Besides attitude and behavior, knowledge and risk perception of the people play an important role on the course of the SARS-CoV-2 pandemic, for both the infection management and the acceptability of vaccines. Our results showed that HCWs and patients responded significantly differently to 10 of the 17 questions on symptoms and routes of SARS-CoV-2 transmission. As reported in other studies [22], [32], [33], [34], fever, cough, shortness of breath and tiredness were the most frequent symptoms reported by 80–100% of the subjects. The most frequent mechanisms of transmission are coughing, talking and physical contact. Furthermore, 97% of the HCWs in our study and 85% in the study carried out by Bashir at al. [35] believe that people without fever can be contagious. Among patients, this percentage was 75%.
Among the HCWs, 85% reported to use official sources for information about COVID-19, whereas 90% “patients used the media. Moreover, a systematic review by Sarria-Guzman et al. [32] in the general population and several studies in HCWs [22], [29], [35] reported the same findings.
Around 85% of patients and HCWs believed that COVID-19 can cause serious and irreversible effects and 60% thought that by 2021 there would be more than 50 deaths from COVID-19 in their place of residence. Moreover, over 50% of patients and HCWs believed that COVID-19 causes much more harm, many more cases of infection and many more deaths than seasonal influenza. However, a higher proportion of HCWs perceived a high risk of COVID-19 as compared to patients (60–80% versus 40–70%) and believed that mortality in the general population was around 1–5% (50% versus 36%). Our findings are consistent with those found in other studies [19], [25], [28], [33], [35].
Thus, according to the results of our survey, HCWs have more knowledge and risk perception of the COVID-19 than patients and tend to consult more reliable/official sources of information but are less willing to get a COVID-19 vaccine than patients and have a higher proportion of hesitancy.
The high acceptance of the COVID-19 vaccines in patients surveyed in the present study may be due to the high perception of risk of SARS-CoV-2 infection, as well as to the fact that this is a more vulnerable population to COVID-19 than the ones included in other studies. We have only found three other studies that focus on populations similar to ours but they only assessed knowledge and risk perception of COVID-19. However, the figure of 9.5% of patients with a high perception of risk found by Wolf et al. [34] is surprisingly low compared to the 85% found for our study population. The authors concluded that personal risk perception might be limited for people living below the poverty level (29%) or for those with low health literacy (50%). In this regard, it should be taken into account that 70% of the population of Araba/Alava is below the third quintile of the MEDEA deprivation index.
On the other hand, in the province of Araba/Alava SARS-CoV-2 infections began among HCWs and 20% of them became infected. Therefore, the surveyed HCWs could have a higher perception of protection against the new coronavirus and thus, might decide not to get the COVID-19 vaccine or have doubts about it. In addition, more HCWs than patients hesitated about the effectiveness of the newly developed vaccines and believed that the clinical research conducted so far was insufficient.
The above-mentioned reasons may explain the differences in vaccine acceptance between patients and HCWs.
Despite this, hesitancy rates were lower than those found in other studies (3–12% versus 20–30%). This could be due to the proximity of the start of the vaccination campaign in our study. However, the percentage of subjects unwilling to get a vaccine is similar to other studies (8–12%).
Finally, it is important to note that 45–60% of the subjects in our survey had received an influenza vaccine during the previous year indicating a generally favorable perception towards vaccination.
The results of our study provide baseline data about Knowledge, Attitudes and Practices (KAP) towards SARS-CoV-2 pandemic, which will help devise effective preventive strategies. However, the study has certain limitations. Patients were selected by random sampling but HCWs were enrolled using a non-probability convenience sampling technique. The survey was also voluntary, raising the possibility of selection bias among respondents opting to participate. Furthermore, the response-rate among HCWs in our study is very low and may be unrepresentative. However, similar results were found in other studies with higher participation-rates.
Data were collected using a self-reported questionnaire, which can be a potential cause of reporting bias. Prior research on SARS-CoV-2 and H1N1 virus outbreaks guided our selection and creation of survey items, but we were unable to validate all questions. On the other hand, it is not possible to directly compare the results of all existing surveys due to differences in the countries included, as well as in the different questionnaires and methodologies used.
The present cross-sectional survey was conducted in a single public healthcare service and among a high-risk population of developing severe COVID-19 disease. Thus, generalizability to other regions of Spain and other countries may be limited. Nevertheless, we believe that there are likely lessons learned that can be more broadly applied. Moreover, conducting the same survey on both, HCWs and patients within the same health system minimizes the information bias that may be caused by contextual factors.
Finally, the survey was conducted at a single point in time amid a dynamic pandemic, where information, options and perceptions are rapidly changing and individualś willingness to get a COVID-19 vaccine may change over time, as vaccination decisions are multifactorial. However, we think that the time selected for the study was a particularly important one, since it was conducted almost immediately after the population perceived vaccine availability. Furthermore, the population selected for the study was also of great interest, since people at high-risk of developing severe COVID-19 were expected to be among the priority groups for vaccination.
The results of the study are useful for the design and planning of the vaccination strategy for the prevention and mitigation of the COVID-19. Although the study presented hereby is descriptive, the determinants of COVID-19 vaccine acceptance will be assessed in a subsequent study.
Declaration of Competing Interest
The authors reports financial support was provided by Caja Vital Foundation (BAFV20-008).
Acknowledgments
Acknowledgements
Funding for the study was provided by the Caja Vital Foundation.
We thank the participants; Carmen Gabarain and David Vallinas for their assistance in the preparation of the questionnaire; Angelica Ibañez and Maria Dolores Siles for coordinating letter delivery to patients; Jesús María Mongelos for providing the data for the study and the managers of the Data Protection Office and Alavás Basque Health System.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jvacx.2022.100176.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Home - Johns Hopkins Coronavirus Resource Center [Internet]. [cited 2022 May 18]. Available from: https://coronavirus.jhu.edu/.
- 2.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E., Villamizar-Peña R., Holguin-Rivera Y., Escalera-Antezana J.P., et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis [Internet] 2020;34:101623. doi: 10.1016/j.tmaid.2020.101623. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1477893920300910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang J., Zheng Y.a., Gou X.i., Pu K.e., Chen Z., Guo Q., et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis [Internet] 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1201971220301363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrison D., Muradali K., El Sahly H., Bozkurt B., Jneid H. Impact of the SARS-CoV-2 pandemic on health-care workers. Hosp Pract [Internet] 2020 Aug 7;48(4):161–164. doi: 10.1080/21548331.2020.1771010. https://www.tandfonline.com/doi/full/10.1080/21548331.2020.1771010 Available from. [DOI] [PubMed] [Google Scholar]
- 5.Cromer D., Juno J.A., Khoury D., Reynaldi A., Wheatley A.K., Kent S.J., et al. Prospects for durable immune control of SARS-CoV-2 and prevention of reinfection. Nat Rev Immunol [Internet] 2021 Jun 29;21(6):395–404. doi: 10.1038/s41577-021-00550-x. http://www.nature.com/articles/s41577-021-00550-x Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine [Internet] 2016 Dec;34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. https://linkinghub.elsevier.com/retrieve/pii/S0264410X1630977X Available from. [DOI] [PubMed] [Google Scholar]
- 7.Ten threats to global health in 2019 [Internet]. [cited 2021 Jun 10]. Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 8.MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine [Internet] 2015 Aug;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. https://linkinghub.elsevier.com/retrieve/pii/S0264410X15005009 Available from. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen K.H., Srivastav A., Razzaghi H., Williams W., Lindley M.C., Jorgensen C., et al. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinating Among Groups Prioritized for Early Vaccination — United States, September and December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):217–222. doi: 10.15585/mmwr.mm7006e3. Available from: http://www.cdc.gov/mmwr/volumes/70/wr/mm7006e3.htm?s_cid=mm7006e3_w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin C., Tu P., Beitsch L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines [Internet] 2020;9(1):16. doi: 10.3390/vaccines9010016. https://www.mdpi.com/2076-393X/9/1/16 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med [Internet] 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. Available from: http://www.nature.com/articles/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wouters O.J., Shadlen K.C., Salcher-Konrad M., Pollard A.J., Larson H.J., Teerawattananon Y., et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397(10278):1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mateu E., Casal J. Tamaño de la muestra de la encuesta. Rev Epidem Med Prev [Internet] 2003;1:8–14. https://investmkt.files.wordpress.com/2013/03/21_06_58_2tamanomuestra3.pdf Available from. [Google Scholar]
- 14.Survey tool and guidance: behavioural insights on COVID-19, 29 July 2020 (produced by the WHO European Region). 2020 Nov 30 [cited 2021 Jun 10]; Available from: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/risk-communication-and-community-engagement/who-tool-for-behavioural-insights-on-covid-19/survey-tool-and-guidance-behavioural-insights-on-covid-19-produced-by-the-who-european-region.
- 15.Apiñaniz A., López-Picado A., Miranda-Serrano E., Latorre A., Cobos R., Parraza-Díez N., et al. Estudio transversal basado en la población sobre la aceptabilidad de la vacuna y la percepción de la gravedad de la gripe A/H1N1: Opinión de la población general y de los profesionales sanitarios. Gac Sanit. 2010;24(4):314–320. doi: 10.1016/j.gaceta.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 16.Felícitas Domínguez-Berjón M., Borrell C., Cano-Serral G., Esnaola S., Nolasco A., Isabel Pasarín M., et al. Construcción de un índice de privación a partir de datos censales en grandes ciudades españolas (Proyecto MEDEA) Gac Sanit [Internet] 2008;22(3):179–187. doi: 10.1157/13123961. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0213911108712329. [DOI] [PubMed] [Google Scholar]
- 17.Ministerio de Sanidad. Ministerio de Sanidad, Consumo y Bienestar Social - Profesionales - Estrategia de vacunación COVID-19 en España [Internet]. 2021 [cited 2021 Jun 10]. Available from: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Informe_GIV_comunicacion_20210607.pdf.
- 18.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine. Ann Intern Med [Internet] 2020;173(12):964–973. doi: 10.7326/M20-3569. https://www.acpjournals.org/doi/10.7326/M20-3569 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine [Internet] 2020 Sep;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. https://linkinghub.elsevier.com/retrieve/pii/S0264410X20310847 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang W, Wu Q, Yang J, Dong K, Chen X, Bai X, et al. Global, regional, and national estimates of target population sizes for covid-19 vaccination: descriptive study. BMJ [Internet]. 2020 Dec 15;371:m4704. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.m4704. [DOI] [PMC free article] [PubMed]
- 21.Szilagyi P.G., Thomas K., Shah M.D., Vizueta N., Cui Y., Vangala S., et al. National Trends in the US Public’s Likelihood of Getting a COVID-19 Vaccine—April 1 to December 8, 2020. JAMA. 2021;325(4):396. doi: 10.1001/jama.2020.26419. Available from: https://jamanetwork.com/journals/jama/fullarticle/2774711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papagiannis D, Malli F, Raptis DG, Papathanasiou I V, Fradelos EC, Daniil Z, et al. Assessment of Knowledge, Attitudes, and Practices towards New Coronavirus (SARS-CoV-2) of Health Care Professionals in Greece before the Outbreak Period. Int J Environ Res Public Health [Internet]. 2020 Jul 8;17(14):4925. Available from: https://www.mdpi.com/1660-4601/17/14/4925. [DOI] [PMC free article] [PubMed]
- 23.Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect [Internet] 2021 Feb;108:168–173. doi: 10.1016/j.jhin.2020.11.020. https://linkinghub.elsevier.com/retrieve/pii/S0195670120305442 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verger P., Scronias D., Dauby N., Adedzi K.A., Gobert C., Bergeat M., et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada. Eurosurveillance [Internet] 2021;26(3) doi: 10.2807/1560-7917.ES.2021.26.3.2002047. Available from: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shekhar R., Sheikh A.B., Upadhyay S., Singh M., Kottewar S., Mir H., et al. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines [Internet] 2021;9(2):119. doi: 10.3390/vaccines9020119. Available from: https://www.mdpi.com/2076-393X/9/2/119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuter B.J., Browne S., Momplaisir F.M., Feemster K.A., Shen A.K., Green-McKenzie J., et al. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia. Vaccine [Internet] 2021;39(12):1693–1700. doi: 10.1016/j.vaccine.2021.02.029. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X21001857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peretti-Watel P., Seror V., Cortaredona S., Launay O., Raude J., Verger P., et al. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis [Internet] 2020;20(7):769–770. doi: 10.1016/S1473-3099(20)30426-6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1473309920304266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal [Internet] 2021 Apr;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. https://linkinghub.elsevier.com/retrieve/pii/S2468266721000128 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Gennaro F., Murri R., Segala F.V., Cerruti L., Abdulle A., Saracino A., et al. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses [Internet] 2021;13(3):371. doi: 10.3390/v13030371. Available from: https://www.mdpi.com/1999-4915/13/3/371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol [Internet] 2020 Aug 17;35(8):785–788. doi: 10.1007/s10654-020-00675-8. http://link.springer.com/10.1007/s10654-020-00675-8 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gadoth A., Halbrook M., Martin-Blais R., Gray A., Tobin N.H., Ferbas K.G., et al. Cross-sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles. Ann Intern Med [Internet] 2021;174(6):882–885. doi: 10.7326/M20-7580. Available from: https://www.acpjournals.org/doi/10.7326/M20-7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarria-Guzmán Y., Fusaro C., Bernal J.E., Mosso-González C., González-Jiménez F.E., Serrano-Silva N. Knowledge, Attitude and Practices (KAP) towards COVID-19 pandemic in America: A preliminary systematic review. J Infect Dev Ctries [Internet] 2021 Jan 31;15(01):9–21. doi: 10.3855/jidc.14388. https://www.jidc.org/index.php/journal/article/view/14388 Available from. [DOI] [PubMed] [Google Scholar]
- 33.O’Conor R., Opsasnick L., Benavente J.Y., Russell A.M., Wismer G., Eifler M., et al. Knowledge and Behaviors of Adults with Underlying Health Conditions During the Onset of the COVID-19 U.S. Outbreak: The Chicago COVID-19 Comorbidities Survey. J Community Health [Internet] 2020;45(6):1149–1157. doi: 10.1007/s10900-020-00906-9. Available from: http://link.springer.com/10.1007/s10900-020-00906-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolf M.S., Serper M., Opsasnick L., O'Conor R.M., Curtis L., Benavente J.Y., et al. Awareness, Attitudes, and Actions Related to COVID-19 Among Adults With Chronic Conditions at the Onset of the U.S. Outbreak. Ann Intern Med [Internet] 2020;173(2):100–109. doi: 10.7326/M20-1239. Available from: https://www.acpjournals.org/doi/10.7326/M20-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bashir S., Alsultan F., Iqbal M., Alabdulkarim N., Alammari K., Almousa A., et al. Healthcare workers’ knowledge and attitudes towards COVID-19 in Saudi Arabia. Eur Rev Med Pharmacol Sci. 2021;25(3):1060–1069. doi: 10.26355/eurrev_202101_24676. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.