1. Introduction
With over half a billion cases of COVID-19 reported globally since December 2019, medical knowledge of COVID-19, its mode of transmission, clinical manifestations and possible long-term complications has increased significantly. Advice regarding investigation, management and return to exercise has also changed over this time in line with emerging evidence, vaccine distribution and the features of new variants. This editorial seeks to synthesize the current knowledge on return to exercise following COVID-19 infection, based on current scientific literature and real-world experience. The authors work in elite sport & exercise medicine and sports cardiology, in different settings in Australia. We provide recommendations which we believe are suitable for those wishing to return to exercise post-COVID-19 infection, from the elite level to community sport, in May 2022. We acknowledge that the prevailing wisdom has changed quickly through the pandemic and may change again in the future.
2. SARS-CoV-2 variants and previous recommendations of return to exercise
While successive SARS-COV-2 variants have demonstrated increased transmissibility, there is no evidence to date that the variants have become more virulent. There is evidence that the Omicron variant is less virulent than previous variants.1 The severity of the disease caused by SARS-CoV-2 in the Australian and New Zealand populations in May 2022 has likely been further attenuated by widespread prior infection and vaccination, and more recently with the emergence of effective antiviral medications. Initial advice regarding return to exercise, including high-performance sport, was influenced by early reports of cardiac and respiratory complications following COVID-19, including asymptomatic and mildly symptomatic infections.2 , 3 The changing clinical picture of COVID-19, as a result of widespread availability of vaccines and the emergence of new variants, necessitates an update to this original advice.
The evidence base for return to exercise post COVID-19 infection is sparse in relation to the Omicron variant. A recent surge in infections in Australia and New Zealand, in conjunction with the widespread use of home diagnostic tests for COVID-19 and the milder clinical picture, has led to a more “hands off” approach to medical management of COVID-19 in most cases. There has been a change from direct medical assessment to general advice and self-care as the mainstay of COVID-19 management. As a result, data regarding clinical symptomatology and return to exercise and sport is less comprehensive than it was early in the pandemic. However, with over 6 million cases recorded in Australia & NZ in the first 4 months of 2022, and few reports of serious adverse outcomes with exercise, the approach to return to exercise has become more pragmatic.
Return to exercise guidelines post-COVID-19 need to consider an individual's duration & severity of symptoms, the presence of co-existing medical conditions, pre-morbid fitness, and the intensity of intended post-infection exercise. Return to exercise should also aim to minimize the development of non-COVID-19 related complications (e.g. musculoskeletal injuries) that may be associated with sudden increases in training volume and intensity following a period of mandatory isolation & relative inactivity.
Initial return to sport guidelines following COVID-19 were necessarily cautious due to the limited knowledge of the disease and its complications, and the absence of an effective vaccine. Early reports suggested that even people who were asymptomatic or mildly symptomatic could have serious underlying pathology.2 , 3 Concern regarding the risk of cardiac complications, including sudden cardiac death as a result of COVID-related myocarditis, resulted in many of the early guidelines from medical and sporting associations recommending routine clinical evaluation by a physician and cardiac screening, including ECG, echocardiography and cardiac biomarkers, for those with symptomatic infection.4., 5., 6., 7., 8., 9., 10. Some also recommended cardiac MRI and exercise testing for high performance athletes returning to competition.11
The clinical course of severe COVID-19 prior to vaccination and the new variants often involved mild viral symptoms in the first week followed by a deterioration in the second week.12 To limit transmission at that time, isolation periods were 14 days in most parts of the world. This isolation period resulted in prolonged inactivity. Early recommendations to avoid exercise for a further 14 days after symptom resolution,13 in recognition of the potential for clinical deterioration after the first week, further delayed return to exercise.
3. Real-world return to exercise experiences following Omicron infection
The COVID-19 pandemic has moved so quickly that sophisticated analysis of COVID-19 trends by media outlets has often been more up to date than the scientific literature, where the peer review process can slow publication by a number of months. Even without vaccination, the risk of cardiac complications in young athletes following COVID-19 infection has been relatively low.4 , 6 , 14 In the rare cases where myocarditis does occur in young athletes, a cautious approach will almost always facilitate resumption of exercise without cardiac event. Large registries have proved reassuring with very low rates of clinically meaningful cardiac complications among athlete populations.15 , 16 Australia and New Zealand were in the fortunate position that very few athletes (other than those training or competing overseas) caught COVID-19 prior to vaccination. Once vaccination rates in both countries reached high levels, restrictions were lifted and COVID-19 infections soared through the Omicron waves (December 2021 and early 2022).
The Omicron variant, compared to previous COVID-19 variants, has had slightly lower mortality rates for those admitted to hospital17 but has had greater transmissibility.18 The individual case fatality ratio for the Omicron variant has – at population level – has been far lower than for previous variants. This has largely been the result of the highly vaccinated status of the Australian and New Zealand populations, at the time of Omicron spread.19 Death rates from Omicron have been higher in countries where vaccination coverage, especially in the elderly, has been lower.20
In May 2022, both Australia and New Zealand have maintained a minimum of seven day self-isolation for anyone who tests positive for COVID-19, which includes athletes. Because it is not logistically feasible for most individuals to train during isolation, isolation ensures that the absolute earliest return to exercise post-infection for most people has been 7 days. Some athletes who have had access to exercise facilities during isolation, and who have been asymptomatic or minimally symptomatic, have continued to train during isolation. The important question is; when is it safe for most individuals to return to exercise? The question needs to be framed in two parts: (1) safety for the individual (in terms of risks of developing complications) and (2) safety for other individuals that the recuperating individual comes in contact with on return (in terms of potential to infect others).
Individual response to viral infection is variable, with many individuals minimally symptomatic (and historically able to exercise) when suffering from viral infections. Pre-COVID-19 there was a culture that a ‘tough athlete’ was one who was able to train and compete despite suffering viral illness.21 The pandemic provides an opportunity to reset the culture of training and competing when sick. Post-viral fatigue syndrome in athletes has been recognized for many years.22 Early return prior to full recovery has been proposed as a risk factor, but the culture of needing to “push through” for the sake of the team or one's own performance was ingrained.
The experience of the authors is that many athletes with confirmed COVID-19 on PCR testing, are minimally symptomatic or asymptomatic. Asymptomatic infections, detected as a result of contact tracing, have been found in athletes who are training at full capacity, while infected, without any deleterious effects.
Being asymptomatic and with two days of negative supervised Rapid Antigen Tests (RATs) starting at the earliest of Day 6/Day 7 indicate low infectiousness from a public health perspective. This has been described as a “Test to Release” protocol.23 Return to outdoor exercise at Day 7 or later after two negative RATs is very low risk of infecting others. Indoor sessions, especially dining or long meetings or shared travel, might still have a small transmission risk at this stage which could further be reduced by other measures. Sensible other measures would be mask wearing indoors (for the convalescent individual especially) until Day 11 and either separated dining or a move to outdoor dining.24
In terms of safety for individuals themselves, we are fortunate to be in an era where elite athletes have baseline data of training efficiency such as defined heart rate zones in relation to intensity of exercise and subjective scoring for training sessions. Immediately achieving at or close to pre-morbid fitness values post-COVID represents evidence of uncomplicated recovery. Our experience in Australia during the Omicron wave is that this has been achieved by Days 7–14 in most vaccinated elite athletes. Advice to the recreationally active individual, where there is less pressure to return to maximum fitness levels quickly, is to do so in a more conservative fashion. There is strong evidence that moderate physical activity (e.g. doing 7000 steps per day) is associated with reduced all-cause mortality.25 Therefore, we should encourage a quick return to moderate exercise with a more cautious return to higher intensity exercise.
4. Recommendation for a graduated return to exercise approach
Routine medical investigation, including cardiac screening, is not recommended in those returning to exercise following COVID-19. Symptom burden and duration should remain the key indicator guiding return to exercise. Cardiac investigation should only be considered where clinically indicated.
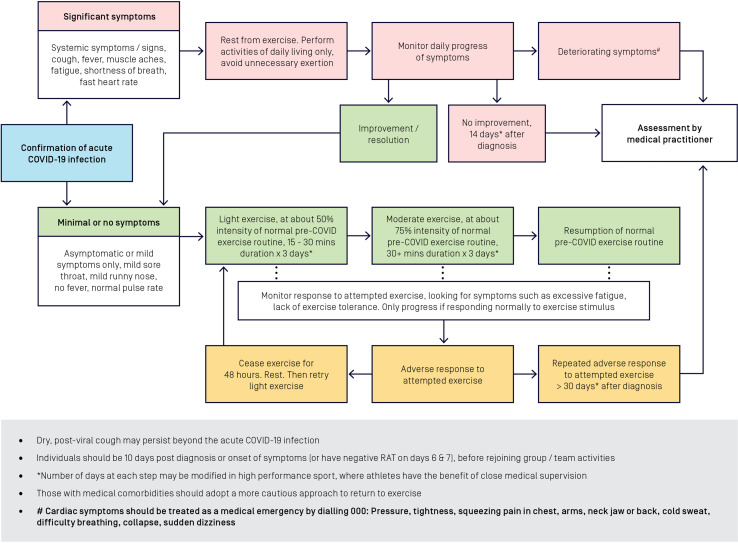
The following protocol for return to exercise is applicable for recreational and elite athletes (refer to Fig. 1 ). Those with pre-existing medical comorbidities should adopt a more cautious approach to return to exercise. It is acknowledged that timeframes for return to exercise for elite athletes may be modified on the basis that those individuals have the benefit of access to close medical monitoring. Return to exercise after COVID-19 infection should happen in a graduated fashion where individuals with no symptoms or minimal symptoms aim to return to their pre-infection exercise habits in approximately 7–14 days.
Fig. 1.
Graduated return to exercise after COVID-19 infection.
Symptom burden is the key. Cases that are asymptomatic at time of testing positive, may develop symptoms over subsequent days. Where individuals have significant symptoms, they should rest and avoid exercise. Those who remain asymptomatic or whose symptoms have resolved or diminished, can commence a graded return to pre-infection activity levels. Resumption of exercise is based on the exercise habits of the individual, prior to infection. As a starting point, individuals should attempt 15 to 30 min of exercise at about 50 % of the intensity that they were used to, prior to infection. If this is well-tolerated, the same should be repeated for the subsequent two days (Days 2 & 3). All going well, exercise intensity can then be increased to about 75 % of the intensity that the individual was used to, prior to infection, from Day 4. The duration can also be increased to 30 or more minutes. If well-tolerated, this again should be repeated on the two subsequent days (Days 5 & 6). If there has been absolutely no adverse response to attempted exercise, the individual could consider resumption of normal pre-COVID-19 exercise habits from Day 7 (see Fig. 1). In elite sport, where athletes have the benefit of close medical supervision, the number of days that each step may be modified. Any unusual exercise intolerance should trigger a pause for 24–48 h, before resuming a graded increase in activity. Persistent exercise intolerance warrants a medical review.
If by 30 days post-infection, an individual is having persistent difficulty with attempted return to pre-infection exercise levels, then review by a medical practitioner for a possible cardiac assessment is recommended, including consideration of ECG, cardiac biomarkers and echocardiography. However, it is possible to have a reduced exercise capacity as part of “Long COVID” even in the presence of a completely normal cardiac workup.26
While myocarditis and other cardiac conditions related to COVID-19 are rare, any cardiac symptoms such as pressure, tightness, squeezing pain in chest, arms, neck jaw or back, cold sweat, difficulty breathing, collapse or sudden dizziness, whether occurring during exercise or at rest, should be treated as a medical emergency.
5. Conclusion
The COVID-19 pandemic has evolved with Omicron and its sub-variants having a lower case-fatality rate than previous variants. In Australia and New Zealand, the virus began to spread widely, only after a majority of the population were vaccinated. As a result of the ready availability of Rapid Antigen Tests, most individuals are now being diagnosed, undertaking isolation, and returning to pre-infection activities, without any direct involvement of a medical practitioner. Early concern over myocarditis occurring in young healthy individuals has eased as large studies of young athletes have revealed very low rates of myocarditis. Most individuals can return to pre-infection activity levels within 7–14 days of the infection. The presence or otherwise of medical comorbidities, symptoms occurring during the infection and symptoms in response to resumption of exercise, should guide the timelines in individual cases. This guidance provides a safe pathway for individuals to return to exercise following COVID-19 infection, based on contemporary evidence regarding COVID-19 and its effects, and the real-world experience of the authors.
References
- 1.Sheikh A., Kerr S., Woolhouse M., et al. Severity of omicron variant of concern and effectiveness of vaccine boosters against symptomatic disease in Scotland (EAVE II): a national cohort study with nested test-negative design. Lancet Infect Dis. 2022 doi: 10.1016/S1473-3099(22)00141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shi H., Han X., Jiang N., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puntmann V.O., Carerj M.L., Wieters I., et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(11):1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baggish A., Drezner J.A., Kim J., et al. Resurgence of sport in the wake of COVID-19: cardiac considerations in competitive athletes. Br J Sports Med. 2020;54(19):1130–1131. doi: 10.1136/bjsports-2020-102516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes D., Saw R., Perera N.K.P., et al. The Australian Institute of Sport framework for rebooting sport in a COVID-19 environment. J Sci Med Sport. 2020;23(7):639–663. doi: 10.1016/j.jsams.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson M.G., Hull J.H., Rogers J., et al. Cardiorespiratory considerations for return-to-play in elite athletes after COVID-19 infection: a practical guide for sport and exercise medicine physicians. Br J Sports Med. 2020;54(19):1157–1161. doi: 10.1136/bjsports-2020-102710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schellhorn P., Klingel K., Burgstahler C. Return to sports after COVID-19 infection. Eur Heart J. 2020;41(46):4382–4384. doi: 10.1093/eurheartj/ehaa448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Löllgen H., Bachl N., Papadopoulou T., et al. Recommendations for return to sport during the SARS-CoV-2 pandemic. BMJ Open Sport Exerc Med. 2020;6(1) doi: 10.1136/bmjsem-2020-000858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verwoert G.C., de Vries S.T., Bijsterveld N., et al. Return to sports after COVID-19: a position paper from the Dutch Sports Cardiology Section of the Netherlands Society of Cardiology. Neth Heart J. 2020;28(7–8):391–395. doi: 10.1007/s12471-020-01469-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phelan D., Kim J.H., Chung E.H. A game plan for the resumption of sport and exercise after coronavirus disease 2019 (COVID-19) infection. JAMA Cardiol. 2020;5(10):1085–1086. doi: 10.1001/jamacardio.2020.2136. [DOI] [PubMed] [Google Scholar]
- 11.Rajpal S., Tong M.S., Borchers J., et al. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2021;6(1):116–118. doi: 10.1001/jamacardio.2020.4916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baggish A.L., Levine B.D. Icarus and sports after COVID 19: too close to the sun? Circulation. 2020;142(7):615–617. doi: 10.1161/CIRCULATIONAHA.120.048335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costello B.T., Climie R.E., Wright L., et al. Athletes with mild COVID-19 illness demonstrate subtle imaging abnormalities without exercise impairment or arrhythmias. Eur J Prev Cardiol. 2022;29(6):e220–e223. doi: 10.1093/eurjpc/zwab166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez M.W., Tucker A.M., Bloom O.J., et al. Prevalence of inflammatory heart disease among professional athletes with prior COVID-19 infection who received systematic return-to-play cardiac screening. JAMA Cardiol. 2021;6(7):745–752. doi: 10.1001/jamacardio.2021.0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moulson N., Petek B.J., Drezner J.A., et al. SARS-CoV-2 cardiac involvement in young competitive athletes. Circulation. 2021;144(4):256–266. doi: 10.1161/CIRCULATIONAHA.121.054824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauring A.S., Tenforde M.W., Chappell J.D., et al. Clinical severity of, and effectiveness of mRNA vaccines against, covid-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: prospective observational study. BMJ. 2022;376 doi: 10.1136/bmj-2021-069761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Araf Y., Akter F., Tang Y.D., et al. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. 2022;94(5):1825–1832. doi: 10.1002/jmv.27588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.luliano A.D., Brunkard J.M., Boehmer T.K., et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods - United States, December 2020-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(4):146–152. doi: 10.15585/mmwr.mm7104e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.HQ WHO . 2021. Enhancing Readiness for Omicron (B.1.1.529): Technical Brief and Priority Actions for Member States. (Online) [Google Scholar]
- 21.Orchard J.W., Orchard J.J., Puranik R. ‘Stay home when sick’ advice: implications for sport and exercise. BMJ Open Sport Exerc Med. 2021;7(4) doi: 10.1136/bmjsem-2021-001227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maffulli N., Testa V., Capasso G. Post-viral fatigue syndrome. A longitudinal assessment in varsity athletes. J Sports Med Phys Fitness. 1993;33(4):392–399. [PubMed] [Google Scholar]
- 23.Mack C.D., Wasserman E.B., Killerby M.E., et al. Results from a test-to-release from isolation strategy among fully vaccinated National Football League players and staff members with COVID-19 - United States, December 14–19, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(8):299–305. doi: 10.15585/mmwr.mm7108a4. [DOI] [PubMed] [Google Scholar]
- 24.Bouton T.C., Atarere J., Turcinovic J., et al. Viral dynamics of Omicron and Delta SARS-CoV-2 variants with implications for timing of release from isolation: a longitudinal cohort study. medRxiv. 2022 doi: 10.1093/cid/ciac510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ekelund U., Tarp J., Steene-Johannessen J., et al. Dose–response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evers G., Schulze A.B., Osiaevi I., et al. Sustained impairment in cardiopulmonary exercise capacity testing in patients after COVID-19: a single center experience. Can Respir J. 2022;2022 doi: 10.1155/2022/2466789. [DOI] [PMC free article] [PubMed] [Google Scholar]