Abstract
Objectives
Medication administration errors (MAEs) are the most common and significant type of medication errors worldwide. This study aims to assess the prevalence, types, and severity of MAEs. Furthermore, this study attempts to determine the factors associated with the occurrence of MAEs.
Method
This cross-sectional study was conducted over a three-month interval in the internal medicine ward of a tertiary teaching hospital in Jordan. During the study period, 13 nurses were observed while they were preparing and administering medications using a direct disguised observation method. All the recorded observations about the preparation and administration were compared with the physician's orders in the medications' records to identify any possible MAEs.
Results
Having observed a total of 1,012 opportunities for errors, 910 MAEs were identified. Among these 910 errors, adherence errors were found to be the most frequent type (n = 364, 35.9%), followed by incorrect drug preparation (n = 247, 24.4%). None of the MAEs revealed any serious harm to patients or contributed to prolonged hospitalization. Antimicrobial drugs (n = 210, 23.0%) was the most common class associated with MAEs, followed by the class of cardiovascular (n = 157, 17.2%) medicines. Results have shown that the occurrence of MAEs was significantly higher in the non-intravenous medications in comparison to the intravenous medications (p-value < 0.001).
Conclusion
While this study revealed a high rate of MAEs, all the identified errors did not cause harm to the patients. Continuous awareness and education campaigns targeting the nurses about the importance of proper and safe drug administration are highly recommended.
Keywords: Direct observation, Internal medicine, Jordan, Medication administration errors, Tertiary hospital
الملخص
أهداف البحث
أخطاء إعطاء الدواء هي من بين أكثر أنواع الأخطاء الدوائية شيوعا وأهمية في جميع أنحاء العالم. هدفت هذه الدراسة إلى تقييم انتشار أخطاء إعطاء الدواء وأنواعها وشدتها، وتحديد العوامل المرتبطة بحدوث مثل هذه الأخطاء.
طرق البحث
أجريت هذه الدراسة المقطعية على مدى ثلاثة أشهر في جناح الطب الباطني في مستشفى تعليمي ثلاثي في الأردن. خلال فترة الدراسة، تمت ملاحظة ما مجموعه 13 ممرضة أثناء تحضير الأدوية وإعطائها باستخدام طريقة الملاحظة المقنعة المباشرة. تمت مقارنة جميع الملاحظات المسجلة المتعلقة بالتحضير والإدارة مع أوامر الطبيب في سجل الأدوية لتحديد أي أخطاء محتملة.
النتائج
لوحظ ما مجموعه 1012 فرصة للأخطاء، وتم تحديد 910 خطأ في إعطاء الأدوية. من بين هذه الأخطاء البالغ عددها 910، كانت أخطاء الالتزام هي النوع الأكثر شيوعا (العدد 364 ، 35.9٪)، يليها تحضير دواء غير صحيح (العدد 247، 24.4٪). لم يسفر أي من أخطاء إعطاء الأدوية عن ضرر جسيم للمرضى أو ساهم في البقاء في المستشفى لفترات طويلة. كانت الأدوية المضادة للميكروبات (العدد 210 ، 23.0٪) هي الفئة الأكثر شيوعا المرتبطة بـأخطاء إعطاء الأدوية، تليها أدوية أمراض القلب والأوعية الدموية (العدد 157 ، 17.2٪). أظهرت النتائج أن حدوث أخطاء إعطاء الأدوية كان أعلى بشكل ملحوظ في الأدوية غير الوريدية مقارنة بالأدوية الوريدية (القيمة الاحتمالية أقل من 0.001).
الاستنتاجات
كشفت هذه الدراسة عن وجود معدل مرتفع من أخطاء إعطاء الأدوية. على الرغم من أن جميع الأخطاء التي تم تحديدها لم تسبب أي ضرر للمرضى، إلا أن الأخطاء كانت موجودة دائما. يوصى بشدة بحملات التوعية والتثقيف المستمرة للممرضين والممرضات حول أهمية الإدارة السليمة والآمنة للأدوية.
الكلمات المفتاحية: المراقبة المباشرة, الأردن, الطب الباطني, أخطاء إدارة الدواء, مستشفى الرعاية المتقدمة
Introduction
Medication errors are regarded as a serious worldwide problem in clinical practice.1 They are among the top 10 causes of death worldwide.2 They are also considered as one of the most common causes of morbidity and mortality found in hospitals.3 Medication errors are defined by the National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) as ‘any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer’.4 The American Society of Health-System Pharmacists (ASHP) classifies medication errors into the following main categories: prescribing, transcribing, dispensing, administration, monitoring, and other medication errors.5
Medication administration errors (MAEs) are among the most common and significant types of medication errors.6,7 A systematic literature review showed MAEs to have the highest prevalence, ranging from 14.3% to 70%, in comparison to the other types of errors such as prescribing error (29.8–47.8%), dispensing error (3–33.6%), and transcribing errors (10–51.8%).8 MAEs are defined as ‘any deviation from a prescriber's valid prescription or the hospital's policy about drug administration, including failure to correctly record the administration of a medication’.9 They occur as a result of the failure in any of the six aspects of rightness related to patients (the right medication, the right dose, the right patient, the right route, the right time, and the right documentation).10
On the one hand, nurses are the healthcare providers who are responsible for administering drugs to patients in hospital settings. They are always trying to minimize the occurrence of MAEs by implementing the six aspects of rightness pertaining to the safe administration of medication.11 Nevertheless, the possibility of committing errors always exists. Unfortunately, when medication errors occur, nurses may avoid admitting the occurrence of errors because of the fear of consequences.12
On the other hand, pharmacists constitute the drug specialists who can perform effective clinical judgments pertaining to the performance of medication processes to reduce drug-related problems that can trigger harm. They have a positive effect on the early detection of MAEs.13 This early detection and prevention of MAEs could reduce patient harm and healthcare costs.13
The maintenance of a safe environment is a high priority in the healthcare system, within which the detection and reporting of medication errors constitute crucial elements when it comes to improving the quality of healthcare.1 In Jordan, there have been a few studies conducted to assess the incidence and severity of reported MAEs in Jordanian Hospitals.14,15 Results of these studies show that there have been a high incidence of medication errors in the hospital wards.14,15 Thus, the aim of this study is to assess the prevalence, types, and severity of MAEs found in the internal medicine ward of a tertiary teaching hospital in Jordan using a direct disguised observation method.
Materials and Methods
Study design and clinical setting
This cross-sectional study was conducted between October and December 2020 to evaluate the prevalence, types, and severity of MAEs found among the internal-medicine patients admitted to Jordan University Hospital (JUH), one of the largest tertiary teaching hospitals in Amman, Jordan. The internal-medicine ward of the hospital has 53 beds, which are distributed equally between the male and female sections. The ward has a medication preparation room, a pharmacy, and a nurse area.
When it comes to the drug distribution policy at JUH, the medication sheets are hand-written by physicians. They include information about the drug name, dose, frequency, and route of administration. In the morning shift of each day, nurses collect all the medication sheets and transfer them to the pharmacy located in the same ward. Within the pharmacy, the prescribed medications' details are entered by the pharmacist in the hospital system, and each medication is dispensed individually inside a see-through plastic bag and provided with a label that contains information about the date, patient name, drug name, drug dose, dosage form, and quantity dispensed. Following this, the nurse double-checks the dispensed medications for each patient. In this procedure, all the prescribed medications are prepared for the next 24 hours. Finally, at the time of drug administration, the nurses prepare, mix, compound, and administer the medications in accordance to the patients’ medication sheets.
Data collection process
The disguised researcher has a PharmD degree and holds a master's in pharmaceutical sciences. She is skilled enough to know or pick up on the errors using a criteria sheet meant for assessing errors.
In this study, the researcher used the direct disguised observation method to collect information about the actual drug preparation and administration. She pretended to be a pharmacy student who wanted to acquire some training about the drug administration techniques. This disguised method is considered to be the most efficient and effective way for detecting MAEs, which has been used in several prior studies.3,6,9,16 It has the advantage of allowing the researchers to detect the real and actual errors performed by nurses without any Hawthorne effect.17
During the observation, all the prescribed information was collected from medical records using a structured checklist. The following steps were observed and recorded for each drug using the predefined checklist, which includes information about the dose calculation, dosage formulation, route of administration, administration time, administration to the patient, documentation in medication record, and for intravenous (IV) drugs, the type and volume of diluent used, rate of administration, and normal saline flushing. To ensure the complete observation of the drug administration procedure, the researcher observed only one nurse in each of the observational rounds. The nurses were selected using convenience sample techniques.
Identification of administration errors
All the recorded observations were compared with the physician's orders in the medication record to identify any preparation and administration errors. As per the predefined criteria of medication errors, any deviation in the prepared/administered medication from the prescribed order was considered a MAE.
Medication administration errors were classified as follows18: 1) wrong medication - when administering a different drug from the one prescribed; 2) incorrect dose - when the dose is given beyond ±10% of the prescribed dose; 3) wrong patient - when the drug is administered to another patient; 4) incorrect time - when the dose is not given within the predefined interval (±30 minutes); 5) incorrect drug preparation - when the drug is incorrectly formulated or manipulated before dispensing; 6) incorrect administration technique - when the drug is administrated using different routes or at different rates; 7) omission error - defined as a dose that should be administered, but was not; 8) lack of documentation in the medication sheet; and 9) adherence errors - defined as the lack of verification when a drug was administered by the patient. Finally, the detected errors were classified based on their severity in accordance to the NCCMERP index of medication errors severity.4 The severity of the identified errors was categorized by two independent clinical pharmacists to ensure consistency in the classification process. Moreover, in this study, the observer intervenes to resolve MAEs only when those errors are severe.
Nurses related information
During the observational period, the nurses were not informed about the study's aim to overcome the Hawthorne effect. However, the researcher only recorded the names of the observed nurses. Then, by the end of the study period (post-observation), the observed nursing staff provided a full explanation about the real aim and method of the research, and why the concealment was necessary. Later, information about the age, gender, educational level, marital status, number of shifts per month, monthly income, and working experience were collected from each of the nurses. However, the nurses had the opportunity to not include their data in the analysis if they did not agree with the study.
Outcome measured
The main outcome measured in this study was the MAE rate. MAE rate is calculated by dividing the number of actual errors by the total number of opportunities of errors and multiplying that sum with 100. Total Opportunity for Errors includes any dose that is ordered within the medication sheet.
Statistical analysis
All the collected data were coded, entered, and analysed using the Statistical Package for Social Sciences (SPSS) version 22. The descriptive analysis was conducted using the mean and standard deviation (SD) of the continuous variables and the percentages of categorical variables. The checking for normality was carried out using the Shapiro–Wilk test, with a P-value > 0.05 indicating normally distributed continuous variables. Pearson Chi-square test was used to evaluate the factors associated with administration errors. For all the statistical analyses, all the tests were two-tailed and a P-value ≤ 0.05 was considered statistically significant.
Results
A total of 13 nurses were observed over an interval of three months (31 observational days). The nurses' average age was 36.5 years (SD = 3.9). Male nurses represented 76.9% (n = 10) of the total observed nurses. A majority of the nurses had a bachelor's degree (n = 11, 84.6%), and around three-quarters of the nurses were married (n = 10, 76.9%). Most of the nurses had 21-25 working shifts per month (n = 9, 69.2%). Further, around 61% of the nurses (n = 8, 61.5%) attained 501–750 JD per month. The nurses' work experience on an average was 13 years (SD = 5.1). In addition, the nurses were responsible for handling 9.0 patients (SD = 3.3) per round on an average. The Sociodemographic characteristics of the observed nurses are detailed in Table 1.
Table 1.
Sociodemographic characteristics of the observed nurses (n = 13).
| Parameter | Mean (SD) | n (%) |
|---|---|---|
| Age (years) | 36.5 (3.9) | |
| Gender | ||
|
3 (23.1%) | |
|
10 (76.9%) | |
| Educational level | ||
|
11 (84.6%) | |
|
2 (15.4%) | |
| Marital status | ||
|
10 (76.9%) | |
|
2 (15.4%) | |
|
1 (7.7%) | |
| Number of shifts per month | ||
|
1 (7.7%) | |
|
1 (7.7%) | |
|
9 (69.2%) | |
|
2 (15.4%) | |
| Monthly income in Jordanian Dinar (JD) | ||
|
1 (7.7%) | |
|
8 (61.5%) | |
|
4 (30.8%) | |
| Working experience (years) | 13.0 (5.1) | |
JD = 0.72 US$.
During the study period, a total of 1,012 opportunities of errors were observed. During the observation, 910 MAEs were identified. Of the 1012 opportunities of errors, 558 (55.1%) of the administration processes had one MAE, 130 (12.8%) of the administration processes had two MAEs, 24 (2.4%) of the administration processes had three MAEs, and five administration processes (0.5%) had four identified MAEs (Figure 1).
Figure 1.
Distributions of the opportunity of errors based on the number of medication administration errors (n = 1012).
The total MAE rate was 89.9%. The adherence errors were the most frequent type (n = 364, 35.97%), which were followed by incorrect drug preparation (n = 247, 24.4%). The percentage and example of each of the types of MAEs are presented in Table 2.
Table 2.
Frequency and examples of the different types of medication administration errors per opportunity of errors (n = 1012).
| Error type | Description of example | Frequency | Error rate (%) |
|---|---|---|---|
| Wrong Dose | Levofloxacin 750 mg, nurse roughly threw half of drug solution bag (500mg/100 ml) into the sink. | 18 | 1.78 |
| Wrong Time | Allopurinol 300 mg was administered at 3–4 PM instead of 8 AM. | 84 | 8.3 |
| Wrong Route | Heparin was given (subcutaneous) SQ instead of IV. | 1 | 0.01 |
| The drug is not given | A lactulose enema was not given to the patient to treat constipation associated with morphine use. | 7 | 0.7 |
| Incorrect drug preparation | 247 | 24.4 | |
|
Bisoprolol 5 mg, nurse broke the tablet by his nails. | 148 | 14.6 |
|
Vancomycin diluted with NS instead of SWFI. | 30 | 2.96 |
|
Micafungin 100 mg reconstituted in 10 ml NS then diluted it in 100 ml NS. | 69 | 6.8 |
| The incorrect technique of administration | 188 | 18.6 | |
|
The prefilled syringe of Enoxaparin was administered to the patient while the injection site was not swabbed with alcohol. | 84 | 8.3 |
|
Vancomycin 1250 mg constituted with 10 ml NS (instead of 20 ml SWFI) and then diluted in 100 ml NS instead of 200 ml, rate of administration = 30 min instead of 60 min | 114 | 11.3 |
| No documentation | Pethidine given but not documented | 1 | 0.01 |
| Adherence error | Ticagrelor tablet was left on the patient's bedside while he was sleeping, and the nurse did not verify whether the medication was taken or not. | 364 | 35.97 |
| Total | 910 | 89.9 |
SWFI: sterile water for injection.
The medication administration errors were classified in accordance to the NCCMERP severity index (Table 3). None of the MAEs revealed serious harm to the patients or contributed to prolonged hospitalization or death. Of the total MAEs, 137 (15%) of the errors were categorized as category D, which required monitoring to ensure that they resulted in no harm.
Table 3.
Classification of medication administration errors by severity according to NCCMERP index (n = 910).
| Category | Degree of error | Definition | Frequency | % |
|---|---|---|---|---|
| A | No error | Circumstances or events that have the capacity to cause error | 627 | 68.9 |
| B | Error but no harm | An error occurred but the error did not reach the patient | 23 | 2.5 |
| C | Error but no harm | An error occurred that reached the patient but did not cause patient harm | 123 | 13.5 |
| D | Error but no harm | An error occurred that reached the patient and required monitoring to confirm that it resulted in no harm to the patient and/or required intervention to preclude harm | 137 | 15.0 |
| E | Error, harm | An error occurred that may have contributed to or resulted in temporary harm to the patient and required intervention | 0 | 0 |
| F | Error, harm | An error occurred that may have contributed to or resulted in temporary harm to the patient and required initial or prolonged intervention | 0 | 0 |
| G | Error, harm | An error occurred that may have contributed to or resulted in permanent harm to the patient | 0 | 0 |
| H | Error, harm | An error occurred that required intervention necessary to sustain life | 0 | 0 |
| I | Error, death | An error occurred that may have contributed to or resulted in the patient's death. | 0 | 0 |
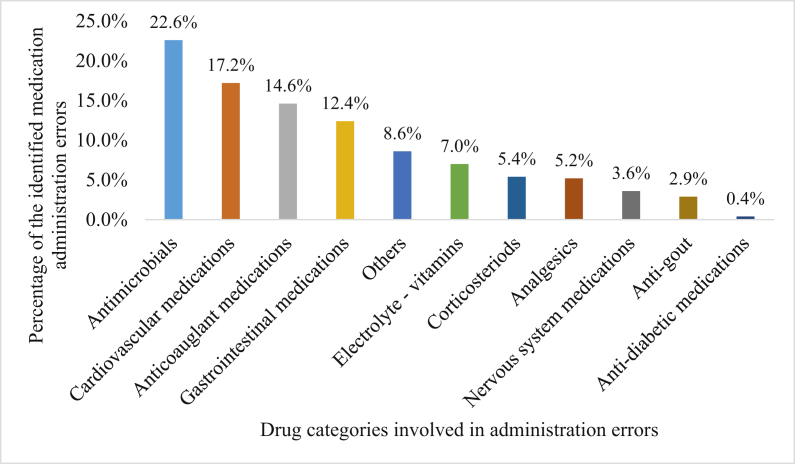
With regard to the classes of medications involved in MAEs (Figure 2), antimicrobials (n = 210, 23.0%) recorded the most frequent MAEs, followed by the cardiovascular (n = 157, 17.2%) and anticoagulant medications (n = 133, 14.6%).
Figure 2.
Percentage of drug classes associated with the medication administration errors (n = 910).
Finally, the Pearson chi-square test was conducted to assess the factors associated with MAEs (Table 4). Results have shown that the occurrence of MAEs was significantly higher in non-intravenous medications in comparison to intravenous medications (P-value < 0.001), while no significant differences were found with regard to the work shift, day of administration, and nurses’ gender (P-value > 0.05).
Table 4.
Factors associated with medication administration errors (n = 910).
| Factors | Occurrence of errors |
P valuea | |
|---|---|---|---|
| Yes n (%) | No n (%) | ||
| Working shift | |||
|
185 (25.8) | 70 (23.7) | 0.490 |
|
532 (74.2) | 225 (76.3) | |
| Days of administration | |||
|
512 (71.4) | 205 (69.5) | 0.542 |
|
205 (28.6) | 90 (30.5) | |
| Route of administration | |||
|
251 (35.0) | 164 (55.6) | <0.001b |
|
466 (65.0) | 131 (44.4) | |
| Nurses' gender | |||
|
328 (45.7) | 135 (45.8) | 0.996 |
|
389 (54.3) | 160 (54.2) | |
Pearson Chi square test, Significant at 0.05 significance level.
Significance at 0.05 significance level.
Discussion
This study is the first study in Jordan to have focused on the identification of MAEs in the internal medicine ward using the direct disguised observation method. There were 910 identified MAEs, which were considered relatively high in comparison to the previous similar studies that found the error rates to range from 9.8 to 49%.6,19, 20, 21, 22 The reason behind the high error rate in our study is the massive workload on nurses during the COVID-19 period due to the shortages in the working staff. This claim is supported in the literature, which correlated high nurses’ workload with the high frequency of MAEs.20
The most common type of MAEs found in this study was adherence errors (n = 354, 35.9%), wherein, most of the nurses left the medications at patients' bedside without ensuring that they took them. Unfortunately, this could be related to the nurses’ heavy workload and lack of standardized procedures in medication administration. This was inconsistent with the findings of other studies, where wrong time was the most common type of MAEs.6,23 It is worth noting that this is the case for all medications except opioids; the nurses in the ward made sure that every patient took his/her opioid medication. Opioids are considered narcotics, requiring two nurses to sign on the medication sheet at the time of administration. Also, the narcotics regulations in Jordan are very strict and firm. Violation of these rules may lead to legal actions or even several years in prison.
The most common class of medication associated with MAEs was antimicrobials (23.0%), followed by cardiovascular medications (17.2%) and anticoagulants (14.6%). To compare our study with the study of Berdot et al., they found cardiovascular drugs (28.3%) to be the most common medication class associated with MAEs.16
All the observed MAEs were classified in accordance to the NCCMERP index for medication error severity, and all of them did not cause any patient harm or prolonged hospitalization. This finding is similar to a previous study that found none of the MAEs to be considered potentially harmful or to prolong patients’ hospitalization.24 In our study, a majority of the errors were classified in category A, as in the cases of adherence errors and lack of aseptic techniques, in which they can be recognized as the circumstances that cause errors. Additionally, 137 errors (15%) were categorized as belonging to the D class, as in the case of the administration of some of the antibiotics. The fast rate of IV administration could result in anaphylactic body reaction or seizures. Results from the literature varied when it comes to the severity of MAEs, while Kumar et al. (2011) reported a majority of MAEs as belonging to category C,25 Sacks et al. reported 91% of MAEs as being non-harmful (belonging to the Categories A, B, C, and D).26
In general, incorrect drug preparation included errors in preparations, wrong intravenous mixture, and volume. Errors in preparations included cases where neither the hands were washed, nor the gloves were worn. In addition, the ampoules of IV drugs were not swapped with alcohol before breaking. These findings were similar to the errors reported by Ong et al.27 While the errors during IV preparation occurred mainly because of the drugs being reconstituted and diluted with normal saline, there was a documented shortage in SWFI availability in the ward, in addition to the lack of aseptic techniques. These findings were in alignment with the findings of Al Khawaldeh and Wazaify, which reported the lack of the use of aseptic technique during medication preparation.14 The administration process with wrong dose errors was primarily because of the doses of medications not being measured accurately. The omission errors were identified with suppositories, enemas, or drug suspensions.
An analysis of the potential factors affecting the occurrence of MAEs revealed that time differences (weekends, weekdays, morning, evenings) did not significantly contribute to MAEs. This was inconsistent with the results reported by other studies that stated time difference to be significantly associated with MAEs.27,28 Non-IV medications were significantly associated with higher error occurrence in comparison to IV medications throughout the study. This was in agreement with the findings of Chau et al. as the route of administration was significantly associated with MAEs.28 As a result of this study, we started preparing a guideline on the correct administration technique to be used in a hospital ward, which includes the correct way to administer oral, IV, SQ, intramuscular (I.M), and rectal drugs, as well as the proper constitution and dilution of the most commonly administered drugs in the ward.
One of the main limitations of this study is that it was only conducted in one ward, and thus, it may not be representative of all the departments of the hospital. The disadvantages of the direct observational method are that it is very exhausting, time-consuming, and costly, requiring the full-time observation of the drug administration rounds.
Conclusion
This study found there to be a high rate of MAEs identified through the direct and disguised observation methods. Adherence errors were the most common type of MAEs, followed by incorrect drug preparation and incorrect administration technique. The occurrence of these errors may be related to heavy workload and lack of standardized procedures for medication administration.
Recommendations
A continuous education program about the correct and safe drug administration is highly recommended to effectively reduce the incidence of MAEs. In addition, pharmacists should take their responsibilities to ensure safe medication use within the hospital via appropriate selection, dispensing, preparation, and administration of medications. Future studies should focus on the effect of increasing nurses’ awareness in reducing MAEs as well as the contribution of clinical pharmacists in preventing such errors.
Source of funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The guidance of the World Medical Association Declaration of Helsinki was followed in this study.29 The direct observation was performed after obtaining the approval of the IRB committee at the Jordan University Hospital on 6th October, 2020 (Approval No. 247/2020). The information obtained about the participants and their medications were stored in the personal computer of the principle investigator using password-protected files.
Authors contributions
All the authors designed and conceptualised the study. AMY and RKA were responsible for the collection of data. AMY and RKA carried out the data analysis and interpretation of results. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.WHO . World Health Organization; 2017. Medication without harm: the third WHO global patient safety challenge. [Google Scholar]
- 2.Anderson J.G., Abrahamson K., editors. Your health care may kill you: medical errors. ITCH; 2017. [PubMed] [Google Scholar]
- 3.Salameh L., Farha R.A., Basheti I. Identification of medication discrepancies during hospital admission in Jordan: prevalence and risk factors. Saudi Pharmaceut J. 2018;26(1):125–132. doi: 10.1016/j.jsps.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MERP N . 2015. National coordinating Council for medication error reporting and prevention: about medication errors: what is a medication error. [Google Scholar]
- 5.Billstein-Leber M., Carrillo C.J.D., Cassano A.T., Moline K., Robertson J. ASHP guidelines on preventing medication errors in hospitals. Am J Health Syst Pharm. 2018;75(19):1493–1517. doi: 10.2146/ajhp170811. [DOI] [PubMed] [Google Scholar]
- 6.Sulaiman Z.H., Hamadi S.A., Obeidat N.M., Basheti I.A. Evaluating medication errors for hospitalized patients: the Jordanian experience. Jordan J Pharmaceut Sci. 2017;403(5438):1–15. [Google Scholar]
- 7.Dos Santos L., Winkler N., Dos Santos M.A., Martinbiancho J.K. Description of medication errors detected at a drug information centre in Southern Brazil. Pharm Pract. 2015;13(1):524. doi: 10.18549/pharmpract.2015.01.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmadizar F., Soleymani F., Abdollahi M. Study of drug-drug interactions in prescriptions of general practitioners and specialists in Iran 2007-2009. Iranian journal of pharmaceutical research. Iran J Pharm Res (IJPR) 2011;10(4):921–931. [PMC free article] [PubMed] [Google Scholar]
- 9.Flynn E.A., Barker K.N., Pepper G.A., Bates D.W., Mikeal R.L. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm. 2002;59(5):436–446. doi: 10.1093/ajhp/59.5.436. [DOI] [PubMed] [Google Scholar]
- 10.Potter P.A., Perry A.G., Kerr J.C., Wood M. Mosby/Elsevier Canada; 2009. Canadian fundamentals of nursing. [Google Scholar]
- 11.Kartika I.R., Melani V. Application of “six rights” on medication administration by nurse and patient satisfaction. Indones Nurs J Educ Clin. 2018;2(2):178–183. [Google Scholar]
- 12.Schelbred A.B., Nord R. Nurses' experiences of drug administration errors. J Adv Nurs. 2007;60(3):317–324. doi: 10.1111/j.1365-2648.2007.04437.x. [DOI] [PubMed] [Google Scholar]
- 13.Mangino P.D. Role of the pharmacist in reducing medication errors. J Surg Oncol. 2004;88(3):189–194. doi: 10.1002/jso.20127. [DOI] [PubMed] [Google Scholar]
- 14.Al Khawaldeh T.A., Wazaify M. Intravenous cancer chemotherapy administration errors: an observational study at referral hospital in Jordan. Eur J Cancer Care. 2018;27(4):e12863. doi: 10.1111/ecc.12863. [DOI] [PubMed] [Google Scholar]
- 15.Hammour K.A., Jalil M.H.A. Medication errors in voluntary reported incidents at a Jordanian hospital. Med J. 2016;50(2):87–96. [Google Scholar]
- 16.Berdot S., Sabatier B., Gillaizeau F., Caruba T., Prognon P., Durieux P. Evaluation of drug administration errors in a teaching hospital. BMC Health Serv Res. 2012;12(1):1–8. doi: 10.1186/1472-6963-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allan E.A., Barker K.N. Fundamentals of medication error research. Am J Hosp Pharm. 1990;47(3):555–571. [PubMed] [Google Scholar]
- 18.Otero López M.J., Castaño Rodríguez B., Pérez Encinas M., Codina Jané C., Tamés Alonso M.J., Sánchez Muñoz T. Updated classification for medication errors by the Ruiz-Jarabo 2000 Group. Farmac Hosp: organo oficial de expresion cientifica de la Sociedad Espanola de Farmacia Hospitalaria. 2008;32(1):38–52. doi: 10.1016/s1130-6343(08)72808-3. [DOI] [PubMed] [Google Scholar]
- 19.Tabatabaee S.S., Kalhor R., Nejatzadegan Z., Kohpeima Jahromi V., Sharifi T. Barriers to medication error reporting from nurses' perspective: a private hospital survey. Int J Hosp Res. 2014;3(2):97–102. [Google Scholar]
- 20.Tang F.I., Sheu S.J., Yu S., Wei I.L., Chen C.H. Nurses relate the contributing factors involved in medication errors. J Clin Nurs. 2007;16(3):447–457. doi: 10.1111/j.1365-2702.2005.01540.x. [DOI] [PubMed] [Google Scholar]
- 21.Vazin A., Delfani S. Medication errors in an internal intensive care unit of a large teaching hospital: a direct observation study. Acta Med Iran. 2012:425–432. [PubMed] [Google Scholar]
- 22.Taxis K., Barber N. Ethnographic study of incidence and severity of intravenous drug errors. Br Med J. 2003;326(7391):684. doi: 10.1136/bmj.326.7391.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chua S.S., Chua H.M., Omar A. Drug administration errors in paediatric wards: a direct observation approach. Eur J Pediatr. 2010;169(5):603–611. doi: 10.1007/s00431-009-1084-z. [DOI] [PubMed] [Google Scholar]
- 24.Lyons I., Furniss D., Blandford A., Chumbley G., Iacovides I., Wei L., et al. Errors and discrepancies in the administration of intravenous infusions: a mixed methods multihospital observational study. BMJ Qual Saf. 2018;27(11):892–901. doi: 10.1136/bmjqs-2017-007476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arun Kumar K., Venkateswarlu K., Ramesh A. A study of medication administration errors in a tertiary care hospital. Ind J Pharm Pract. 2011;4(2):37. [Google Scholar]
- 26.Sacks G.S., Rough S., Kudsk K.A. Frequency and severity of harm of medication errors related to the parenteral nutrition process in a large university teaching hospital. Pharmacotherapy. 2009;29(8):966–974. doi: 10.1592/phco.29.8.966. [DOI] [PubMed] [Google Scholar]
- 27.Ong W., Subasyini S. Medication errors in intravenous drug preparation and administration. Med J Malaysia. 2013;68(1):52–57. [PubMed] [Google Scholar]
- 28.Chua S., Tea M., Rahman M. An observational study of drug administration errors in a Malaysian hospital (study of drug administration errors) J Clin Pharm Therapeut. 2009;34(2):215–223. doi: 10.1111/j.1365-2710.2008.00997.x. [DOI] [PubMed] [Google Scholar]
- 29.World Medical A World medical association declaration of helsinki: ethical principles for medical research involving human subjects. J Am Med Assoc. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]