Abstract
Background
This study aimed to investigate the prevalence and management of diabetes mellitus, risk-factor control, and comorbidities among Korean adults.
Methods
We conducted a cross-sectional analysis of data from the Korea National Health and Nutrition Examination Survey to assess the prevalence, treatment, risk factors, comorbidities, and self-management behaviors of diabetes mellitus from 2019 to 2020. We also analyzed data from the Korean National Health Insurance Service to evaluate the use of antidiabetic medications in people with diabetes mellitus from 2002 through 2018.
Results
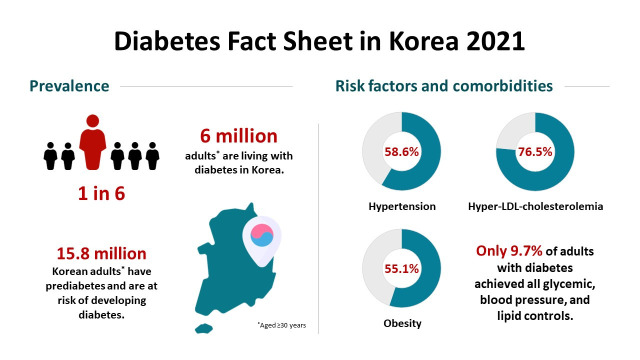
Among Korean adults aged 30 years or older, the estimated prevalence of diabetes mellitus was 16.7% in 2020. From 2019 through 2020, 65.8% of adults with diabetes mellitus were aware of the disease and treated with antidiabetic medications. The percentage of adults with diabetes mellitus who achieved glycosylated hemoglobin (HbA1c) <6.5% was 24.5% despite the increased use of new antidiabetic medications. We found that adults with diabetes mellitus who achieved all three goals of HbA1c <6.5%, blood pressure (BP) <140/85 mm Hg, and low-density lipoprotein cholesterol <100 mg/dL were 9.7%. The percentage of self-management behaviors was lower in men than women. Excess energy intake was observed in 16.7% of adults with diabetes mellitus.
Conclusion
The prevalence of diabetes mellitus among Korean adults remained high. Only 9.7% of adults with diabetes mellitus achieved all glycemic, BP, and lipid controls from 2019 to 2020. Continuous evaluation of national diabetes statistics and a national effort to increase awareness of diabetes mellitus and improve comprehensive diabetes care are needed.
Keywords: Comorbidity, Diabetes mellitus, Disease management, Health behavior, Prevalence, Republic of Korea, Risk factors
Graphical abstract
INTRODUCTION
Diabetes mellitus is a major public health problem, leading to morbidity, disability, and mortality globally, with rapidly growing incidence and prevalence [1]. According to the International Diabetes Federation Diabetes Atlas, 537 million adults aged 20 to 79 years had diabetes worldwide in 2021, and the number is estimated to rise to 783 million by 2045 [2]. The causes of the diabetes epidemic are complex, and overweight and obesity, unhealthy diets, and physical inactivity influence the development of diabetes mellitus, in conjunction with genetic and epigenetic predispositions [3]. Therefore, valid and reliable assessments of disease status, risk factors, and comorbidities are essential to reduce the burden of diabetes mellitus.
Coping with a rise in diabetes mellitus, the Korean Diabetes Association (KDA) has published the Diabetes Fact Sheet in Korea since 2012 to provide representative national statistics on diabetes mellitus. Previous reports showed that approximately one out of seven Korean adults aged 30 years or older and three out of 10 aged 65 years had diabetes mellitus and poor glycemic and risk-factor controls [4,5]. In the Korean National Burden of Disease study, diabetes mellitus ranked the highest cause of disability-adjusted life years [6], which further increased given diabetic complications [7]. These findings warrant immediate action to halt the diabetes epidemic in Korea. The importance of managing diabetes mellitus is further heightened during the coronavirus disease 2019 (COVID-19) pandemic because numerous studies showed that diabetes mellitus was associated with an increased risk of severe COVID-19 outcomes [8-11]. On the other hand, preclinical studies reported that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection might elicit impaired β-cell function [12] or insulin resistance [13]. In addition, the COVID-19 pandemic could have indirect effects on diabetes management by affecting the diagnoses and monitoring of diabetes mellitus [14]. Approval of new antidiabetic medications and changes in clinical practice guidelines based on recent clinical trials also impact diabetes care and support [15,16]. In this respect, understanding the current status of diabetes mellitus has important clinical and public health implications.
We aimed to investigate the prevalence and management of diabetes mellitus, risk-factor control, and comorbidities among Korean adults and update the Diabetes Fact Sheet in Korea 2020 [17]. In this study, we analyzed data from Korea National Health and Nutrition Examination Survey (KNHANES) and the Korean National Health Insurance Service (NHIS) to provide representative national estimates of diabetes mellitus.
METHODS
Study design and data collection
We analyzed data from the KNHANES (2019 and 2020) and the Korean NHIS (2002 through 2018). The KNHANES is a series of nationally representative, cross-sectional surveys designed to evaluate health behaviors, health status, and food and nutrient intake of the Korean population [18]. Data are collected from health interviews, health examinations, and nutrition surveys. The response rate for health interviews and health examinations was 71.0% and for nutritional surveys was 79.3% in 2019. We used the KNHANES data to evaluate the prevalence of diabetes mellitus among adults aged 19 years or older and risk-factor control, comorbidities, and self-management behaviors among adults aged 30 years or older. The Korean NHIS is a single, compulsory health insurance system managed by the Korean government, providing healthcare coverage to almost the entire Korean population [19]. The Korean NHIS database includes sociodemographic information, use of medical services, medical claims, and health examinations. We examined the use of antidiabetic medications among adults aged 30 years or older with diabetes mellitus using the Korean NHIS data. We defined diabetes mellitus as the tenth revision of the International Classification of Diseases codes E11–E14 and at least one prescription of antidiabetic medications. This study was approved by the Institutional Review Board of Korea University Anam Hospital (IRB No. 2022AN-0146). Informed consent was waived by the board.
Definition of diabetes mellitus and comorbidities
We defined diabetes mellitus as having fasting plasma glucose (FPG) ≥126 mg/dL or glycosylated hemoglobin (HbA1c) ≥6.5% or a previous diagnosis of diabetes mellitus or taking medications for diabetes mellitus [20]. Prediabetes was defined as an FPG of 100 to 125 mg/dL or an HbA1c of 5.7% to 6.4% [16]. We defined hypertension as systolic blood pressure (SBP) ≥140 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg or taking antihypertensive medications [20]. We defined hyper-low-density lipoprotein (LDL)-cholesterolemia as low-density lipoprotein cholesterol (LDL-C) ≥100 mg/dL or taking lipid-lowering medications [5]. Overweight and obesity were defined as a body mass index (BMI) of 23.0–24.9 and ≥25.0 kg/m2, respectively [16]. Abdominal obesity was defined as waist circumference ≥90 cm in men and ≥85 cm in women [21].
Risk factors and self-management behaviors
We defined awareness of diabetes mellitus as the percentage of people previously diagnosed with diabetes mellitus among people with diabetes mellitus [20]. We defined the treatment rate of diabetes mellitus as the percentage of people taking antidiabetic medications among people with diabetes mellitus [20]. The control rate of diabetes mellitus was defined as the percentage of people with HbA1c <6.5% among people with diabetes mellitus [16]. We defined blood pressure (BP) control as SBP <140 mm Hg and DBP <85 mm Hg [16]. We defined lipid control as LDL-C <100 mg/dL [16].
Current smoking was defined as having smoked five packs (or 100 cigarettes) in his or her lifetime and currently smoking cigarettes [20]. High-risk alcohol consumption was defined as more than seven drinks twice a week for men and more than five for women [20]. Regular walking was defined as a minimum of 30 minutes a day of walking five or more days per week [20]. Excess energy intake was defined as 125% or more of the estimated energy requirement recommended by the Dietary Reference Intakes for Koreans 2015 [22]. We calculated the percentages of energy intake from macronutrients (carbohydrates, protein, and fat) as previously reported [17].
Use of antidiabetic medications
We evaluated the management of diabetes mellitus as insulin, oral glucose-lowering medications, non-pharmacologic treatment, and no treatment using a health interview survey of the KNHANES. In addition, we analyzed claims data from the Korean NHIS to further assess changes in the prescription of antidiabetic medication classes (metformin, sodium-glucose cotransporter 2 [SGLT2] inhibitors, glucagon-like peptide-1 [GLP-1] receptor agonists, dipeptidyl peptidase-4 [DPP-4] inhibitors, thiazolidinediones, α-glucosidase inhibitors, sulfonylureas/glinides, and insulin) in people with diabetes mellitus from 2002 through 2018.
Statistical analysis
We examined descriptive statistics for diabetes mellitus among adult KNHANES and Korean NHIS participants. The estimated prevalence of diabetes mellitus was presented as mean and standard error. The proportions of comorbidities, risk-factor control, and self-management behaviors were presented as percentages. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Prevalence of diabetes mellitus
Among Korean adults aged 30 years or older, approximately 6.05 million people, or 16.7% (19.2% in men and 14.3% in women), had diabetes mellitus in 2020 (Table 1). When defined based on FPG alone, the estimated prevalence of diabetes mellitus was 14.5% (16.8% in men and 12.3% in women). The estimated prevalence of diabetes mellitus among adults aged 19 years or older and aged 65 years was 13.9% (15.8% in men and 12.1% in women) and 30.1% (29.8% in men and 30.2% in women), respectively. The prevalence of diabetes mellitus increased with increasing age. The prevalence of diabetes mellitus was higher in adults with lower equivalized household incomes. Among adults aged 30 years or older, approximately 15.83 million people, or 44.0% (46.9% in men and 41.2% in women), had prediabetes in 2020 (Supplementary Table 1). The estimated prevalence of impaired fasting glucose, defined as an FPG of 100 to 125 mg/dL, was 26.9% (33.1% in men and 20.8% in women). The estimated prevalence of prediabetes among adults aged 19 years or older and aged 65 years was 39.3% (42.3% in men and 36.3% in women) and 50.0% (51.0% in men and 49.1% in women), respectively.
Table 1.
Estimated prevalence of diabetes mellitus among adult KNHANES participants, 2020
| Variable | Number | Percentage±SE | Estimated population |
|---|---|---|---|
| Age group, yr | |||
| ≥19 | |||
| FPG or HbA1ca | 5,612 | 13.9±0.6 | 6,101,158 |
| FPG | 5,613 | 12.2±0.5 | 5,327,384 |
| ≥30 | |||
| FPG or HbA1ca | 4,848 | 16.7±0.7 | 6,047,618 |
| FPG | 4,849 | 14.5±0.6 | 5,273,844 |
| ≥65 | |||
| FPG or HbA1ca | 1,545 | 30.1±1.3 | 2,450,207 |
| FPG | 1,546 | 27.0±1.2 | 2,202,928 |
| 19–29a | 764 | 0.7±0.3 | 53,540 |
| 30–39a | 734 | 4.4±0.8 | 314,033 |
| 40–49a | 936 | 9.0±1.1 | 740,264 |
| 50–59a | 1,025 | 19.1±1.4 | 1,636,363 |
| 60–69a | 1,068 | 25.1±1.6 | 1,626,599 |
| ≥70a | 1,085 | 31.5±1.6 | 1,730,360 |
| Sexa | |||
| Men | |||
| Age ≥19 yr | 2,516 | 15.8±0.9 | 3,417,978 |
| Age ≥30 yr | 2,135 | 19.2±1.0 | 3,393,466 |
| Age ≥65 yr | 671 | 29.8±2.1 | 1,109,812 |
| Women | |||
| Age ≥19 yr | 3,096 | 12.1±0.7 | 3,212,364 |
| Age ≥30 yr | 2,713 | 14.3±0.8 | 3,187,148 |
| Age ≥65 yr | 874 | 30.2±1.5 | 1,459,697 |
| Equivalized household incomea,b | |||
| Quintile 1 (lowest) | 752 | 30.8±2.0 | - |
| Quintile 2 | 911 | 22.1±1.7 | - |
| Quintile 3 | 981 | 14.3±1.3 | - |
| Quintile 4 | 1,084 | 12.9±1.1 | - |
| Quintile 5 (highest) | 1,104 | 12.3±1.1 | - |
KNHANES, Korea National Health and Nutrition Examination Survey; SE, standard error; FPG, fasting plasma glucose; HbA1c, glycosylated hemoglobin.
Diabetes mellitus was defined by FPG or HbA1c criteria,
Data were analyzed among adults aged 30 years or older.
Diabetes management
From 2019 through 2020, awareness of diabetes mellitus in adults was 65.8%, and 61.4% of adults with diabetes mellitus were receiving oral glucose-lowering medications or insulin (Table 2). The proportion of adults with diabetes mellitus who achieved an HbA1c target of <6.5% was 24.5%. We found that 86.0% of adults with previously diagnosed diabetes mellitus were taking oral glucose-lowering medications without insulin, and 7.5% were treated with insulin. However, 6.3% of them were not receiving any treatment for diabetes mellitus (Fig. 1).
Table 2.
Proportions of adult KNHANES participants who had a diagnosis of diabetes mellitus, who were taking medications, and who achieved glycosylated hemoglobin <6.5%, 2019–2020
| Variable | Total diabetes mellitus |
Diagnosed diabetes mellitus |
||
|---|---|---|---|---|
| Number | Percentage±SE | Number | Percentage±SE | |
| Awareness or detectiona | ||||
| Age, yr | ||||
| ≥30 | 1,770 | 65.8±1.4 | - | - |
| ≥65 | 914 | 76.4±1.5 | - | - |
| Sex | ||||
| Men | 1,225 | 62.6±1.9 | - | - |
| Women | 1,168 | 69.7±1.8 | - | - |
| Treatment rateb | ||||
| Age, yr | ||||
| ≥30 | 1,770 | 61.4±1.5 | 1,202 | 93.4±1.0 |
| ≥65 | 914 | 73.3±1.6 | 694 | 95.9±0.8 |
| Sex | ||||
| Men | 899 | 57.1±2.1 | 589 | 91.2±1.7 |
| Women | 871 | 66.8±1.8 | 613 | 95.8±0.8 |
| Control ratec | ||||
| Age, yr | ||||
| ≥30 | 1,770 | 24.5±1.2 | 1,202 | 26.8±1.4 |
| ≥65 | 914 | 28.3±1.7 | 694 | 31.3±2.0 |
| Sex | ||||
| Men | 899 | 24.4±1.6 | 589 | 25.3±2.0 |
| Women | 871 | 24.5±1.7 | 613 | 28.5±2.0 |
KNHANES, Korea National Health and Nutrition Examination Survey; SE, standard error.
Awareness of diabetes mellitus was defined as the percentage of people previously diagnosed with diabetes mellitus among people with diabetes mellitus,
Treatment rate of diabetes mellitus was defined as the percentage of people taking antidiabetic medications among people with diabetes mellitus,
Control rate of diabetes mellitus was defined as the percentage of people with glycosylated hemoglobin <6.5% among people with diabetes mellitus.
Fig. 1.
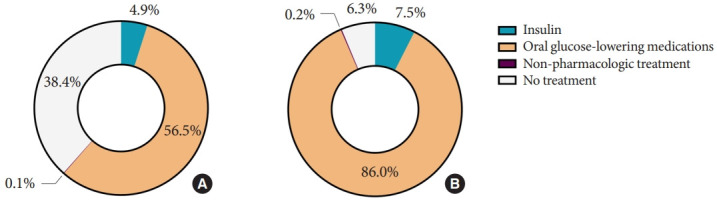
Diabetes treatment among adult Korea National Health and Nutrition Examination Survey (KNHANES) participants with (A) diabetes mellitus and (B) previously diagnosed diabetes mellitus, 2019 to 2020.
Among adults with diabetes mellitus, the use of metformin steadily increased from 2002 to 2016 and then leveled off (Fig. 2, Supplementary Table 2). Since 2008, the use of new antidiabetic medications, including DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors, had increased. In 2018, 62.0% of adults receiving antidiabetic medications used DPP-4 inhibitors. There was a steady decrease in the use of sulfonylureas/glinides and α-glucosidase inhibitors. The use of insulin and thiazolidinediones remained stable from 2002 to 2018.
Fig. 2.
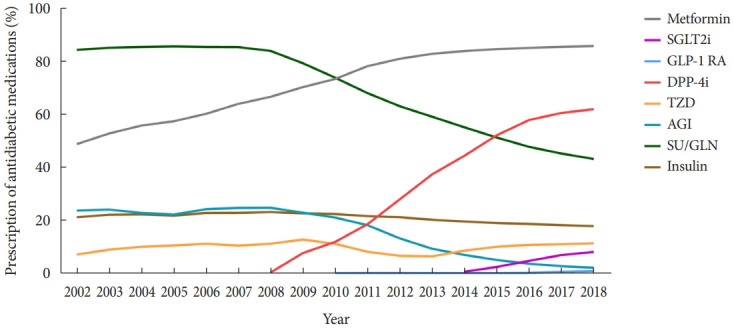
Trends in the use of antidiabetic medications in adults with diabetes mellitus from the Korean National Health Insurance Service (NHIS) data, 2002 to 2018. SGLT2i, sodium-glucose cotransporter 2 inhibitor; GLP-1 RA, glucagon-like peptide-1 receptor agonist; DPP-4i, dipeptidyl pepdiase-4 inhibitor; TZD, thiazolidinedione; AGI, α-glucosidase inhibitor; SU, sulfonylurea; GLN, glinide.
Risk-factor control and comorbidities
The percentages of adults with diabetes mellitus who achieved an HbA1c level of <6.5%, <7.0%, and <8.0% were 24.5%, 55.6%, and 80.5%, respectively (Table 3, Supplementary Fig. 1). The prevalence of hypertension among adults with diabetes mellitus was 58.6% (57.9% in men and 59.5% in women), and 55.5% of adults with diabetes mellitus achieved BP control (<140/85 mm Hg). The prevalence of hyper-LDL-cholesterolemia among adults with diabetes mellitus was 76.5% (73.3% in men and 80.5% in women). The percentage of adults with diabetes mellitus who achieved lipid control (LDL-C <100 mg/dL) was 38.3%. Only 9.7% of adults with diabetes mellitus achieved all three goals of HbA1c <6.5%, BP <140/85 mm Hg, and LDL-C <100 mg/dL for diabetes care in patients without cardiovascular disease (CVD) based on the 2021 KDA Clinical Practice Guideline [16].
Table 3.
Prevalence of risk-factor control and comorbidities among adult KNHANES participants with diabetes mellitus, 2019–2020
| Variable | Total | Men | Women |
|---|---|---|---|
| HbA1c | |||
| <6.5% | 24.5 | 24.4 | 24.5 |
| <7.0% | 55.6 | 55.0 | 56.3 |
| <8.0% | 80.5 | 79.5 | 81.7 |
| <9.0% | 89.9 | 89.3 | 90.5 |
| Hypertensiona | 58.6 | 57.9 | 59.5 |
| BP <140/85 mm Hg | 55.5 | 51.7 | 60.2 |
| Hyper-LDL-cholesterolemiab | 76.5 | 73.3 | 80.5 |
| LDL-C <100 mg/dL | 38.3 | 36.1 | 40.9 |
| Hypertensiona and hyper-LDL- cholesterolemiab | 43.9 | 41.9 | 46.4 |
| HbA1c <6.5% +BP <140/85 mm Hg + LDL-C <100 mg/dL | 9.7 | 11.0 | 8.1 |
| Weight status (BMI, kg/m2) | |||
| Underweight (<18.5) | 1.2 | 1.1 | 1.3 |
| Normal weight (18.5–22.9) | 20.7 | 18.2 | 23.8 |
| Overweight (23.0–24.9) | 23.1 | 23.7 | 22.4 |
| Class I obesity (25.0–29.9) | 41.3 | 43.5 | 38.5 |
| Class II obesity (30.0–34.9) | 11.2 | 11.0 | 11.4 |
| Class III obesity (≥35.0) | 2.6 | 2.5 | 2.6 |
| Abdominal obesity (WC, cm) | |||
| No (<90 in men, <85 in women) | 36.7 | 37.8 | 35.4 |
| Yes (≥90 in men, ≥85 in women) | 63.3 | 62.2 | 64.6 |
| Current smokingc | 22.3 | 36.0 | 5.0 |
| High-risk alcohol consumptiond | 22.8 | 31.1 | 4.2 |
| Regular walkinge | 38.1 | 37.2 | 39.4 |
Values are presented as percentages.
KNHANES, Korea National Health and Nutrition Examination Survey; HbA1c, glycosylated hemoglobin; BP, blood pressure; LDL-C, low-density lipoprotein cholesterol; BMI, body mass index; WC, waist circumference.
Hypertension was defined as systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg or taking antihypertensive medications,
Hyper-LDL-cholesterolemia was defined as LDL-C ≥100 mg/dL or taking lipid-lowering medications,
Current smoking was defined as having smoked five packs (or 100 cigarettes) in his or her lifetime and currently smoking cigarettes,
High-risk alcohol consumption was defined as more than seven drinks twice a week for men and more than five for women,
Regular walking was defined as a minimum of 30 minutes a day of walking five or more days per week.
The prevalence of obesity among adults with diabetes mellitus was 55.1% (57.0% in men and 52.5% in women), of which class I obesity accounted for 41.3% (Table 3). The prevalence of overweight among adults with diabetes mellitus was 23.1%. The prevalence of abdominal obesity among adults with diabetes mellitus was 63.3%, showing slightly higher percentages in women (64.6%) than men (62.2%).
Self-management behaviors
Current smoking and high-risk alcohol consumption were observed in 22.3% (36.0% in men and 5.0% in women) and 22.8% (31.1% in men and 4.2% in women) of adults with diabetes mellitus, respectively. Those with regular walking accounted for 38.1% (37.2% in men and 39.4% in women) (Table 3). Total energy intake was higher in adults without diabetes mellitus than those with diabetes mellitus or previously diagnosed diabetes mellitus (Table 4). The percentage of energy intake from carbohydrates was higher in adults with diabetes mellitus, whereas those from protein and fat were higher in those without diabetes mellitus.
Table 4.
Total energy intake, excess energy intake, and percentages of energy intake from macronutrients among adults KNHANES participants with diabetes mellitus, 2019–2020
| Variable | Total diabetes mellitus | Diagnosed diabetes mellitus | Non- diabetes mellitus | P valuea |
|---|---|---|---|---|
| Total energy intake, kcal | 1,825 | 1,785 | 1,911 | 0.009 |
| Men | 2,127 | 2,111 | 2,251 | 0.013 |
| Women | 1,439 | 1,402 | 1,596 | <0.001 |
| Excess energy intake, %b | 16.7 | 15.8 | 16.9 | 0.914 |
| Men | 19.5 | 18.9 | 20.5 | 0.637 |
| Women | 13.2 | 12.2 | 13.5 | 0.827 |
| Percentages of energy intake from macronutrients | ||||
| Carbohydrates, % | 66.3 | 66.8 | 62.4 | <0.001 |
| Men | 64.5 | 64.7 | 61.5 | <0.001 |
| Women | 68.6 | 69.2 | 63.3 | <0.001 |
| Protein, % | 15.0 | 14.8 | 15.6 | <0.001 |
| Men | 15.5 | 15.5 | 16.0 | 0.008 |
| Women | 14.3 | 14.0 | 15.1 | <0.001 |
| Fat, % | 18.7 | 18.4 | 22.0 | <0.001 |
| Men | 20.0 | 19.8 | 22.4 | <0.001 |
| Women | 17.1 | 16.9 | 21.6 | <0.001 |
KNHANES, Korea National Health and Nutrition Examination Survey.
P values are for comparing total diabetes mellitus and non-diabetes mellitus,
Excess energy intake was defined as 125% or more of the estimated energy requirement recommended by the Dietary Reference Intakes for Koreans 2015 [22].
DISCUSSION
The estimated prevalence of Korean adults aged 30 years or older with diabetes mellitus was 16.7% in 2020. The proportion of adults being aware of and treated for diabetes mellitus did not increase in 2019–2020 compared with 2016–2018 [17]. The percentage of adults with diabetes mellitus who achieved HbA1c <6.5% and LDL-C <100 mg/dL were lower than those who achieved BP <140/85 mm Hg. Only 9.7% of adults with diabetes mellitus achieved all glycemic, BP, and lipid controls. The prevalence of self-management behaviors for diabetes mellitus was lower in men than women.
This study updated previous findings of the Diabetes Fact Sheet in Korea 2020 [17] using the 2019 and 2020 data from the KNHANES. The most notable change was an increase in the prevalence of diabetes mellitus among adults aged 30 years or older in 2020 (16.7%). The prevalence of diabetes mellitus among Korean adults remained stable, ranging from 11.4% to 14.4% between 2012 and 2018 [5], despite increasing BMI and waist circumference [23], decreasing mortality in diabetes mellitus [24], and increasing young adults with diabetes mellitus [25,26]. Growing evidence suggests that COVID-19 could increase the risk of diabetes mellitus [27]. A recent cohort study in the United States provided further evidence that COVID-19 was significantly associated with an increased risk of incident diabetes mellitus beyond the first 30 days of infection [28]. In Korea, 60,726 confirmed COVID-19 cases were reported from January 2020 to December 2020 [29]. Although the actual effect is difficult to evaluate, the infection and preventive measures, such as social distancing and working from home, may in part have contributed to the increased prevalence of diabetes mellitus during the COVID-19 pandemic. Further investigation on data in 2021 or later will give a clear picture of changes in the prevalence of diabetes mellitus in Korea.
Risk-factor control among adults with diabetes mellitus worsened in 2019–2020 compared with 2016–2018 [17]. We examined the use of antidiabetic medications from the Korean NHIS data to complement the KNHANES data on the management of diabetes mellitus. The improvement in glycemic control stalled in this period despite the increased use of new antidiabetic medications with additional benefits of weight loss, a low risk of hypoglycemia, and cardiorenal protection. Similar to another study [30], individualized glycemic targets based on patient characteristics and risks and benefits of therapy might affect glycemic control in Korean adults with diabetes mellitus [16]. The prevalence of hypertension and BP control among adults with diabetes mellitus were similar between 2016–2018 [17] and 2019–2020. On the other hand, lipid control significantly worsened in 2019–2020 (38.3%) compared with 2016–2018 (53.3%), with a higher prevalence of hyper-LDL-cholesterolemia (72.0% in 2016–2018 and 76.5% in 2019–2020) [17]. Although additional information is required to elucidate these changes, a substantial increase in abdominal obesity among adults with diabetes mellitus (53.2% in 2016–2018 [17] and 63.3% in 2019–2020) may have influenced the prevalence of hyper-LDL-cholesterolemia and lipid control. In line with these findings, only a small proportion of adults with diabetes mellitus achieved goals of all three risk factors in 2019 to 2020, which was lower than 11.5% in 2016 to 2018 [17]. The decline in risk-factor control in people with diabetes mellitus has public health implications. Compared with nondiabetic individuals, people with type 2 diabetes mellitus had higher cardiovascular morbidity and mortality [31]. However, people with type 2 diabetes mellitus who had risk factors within the target ranges had marginally higher risks of mortality and CVD than the general population [32]. Given the increased prevalence of diabetes mellitus in our study, urgent interventions are needed to improve risk-factor control in Korean adults with diabetes mellitus.
The prevalence of obesity and abdominal obesity among adults with diabetes mellitus steadily increased from 2013–2018 [4,5] to 2019–2020. Excessive adiposity is intertwined with the incidence and progression of type 2 diabetes mellitus [33]. Asian populations tended to develop type 2 diabetes mellitus at a lower BMI than Western populations, indicating that impaired β-cell function for progressive decline in insulin sensitivity was crucial in the pathophysiology [34]. However, along with a recent rise in obesity in Asia, insulin resistance also largely contributes to developing type 2 diabetes mellitus in the Asian population [35]. In addition, weight loss is beneficial to glycemic and risk-factor controls regardless of heterogeneity of diabetes mellitus [33]. Therefore, lifestyle and pharmacologic interventions should be offered to people with diabetes mellitus considering their effects on weight management.
With regard to self-management behaviors, current smoking among adults with diabetes mellitus continues to decrease from 2013–2018 to 2019–2020, whereas high-risk alcohol consumption continues to increase [4,5]. Current smoking and high-risk alcohol consumption were approximately seven times more prevalent in men than women. The proportion of patients with regular walking increased in 2019–2020 compared with 2013–2018 [4,5]. Excess energy intake in Korean adults with diabetes mellitus decreased from 18.1% in 2016–2018 [17] to 16.7% in 2019–2020. A total of 66.3% of energy intake came from carbohydrates. A previous study using the KDA-Korean Ministry of Health and Welfare index showed that overall adherence to dietary guidelines was low in Korean adults with diabetes mellitus, particularly non-elderly patients [36]. Maintaining healthy behaviors is fundamental to achieving treatment goals in people with diabetes mellitus [37]. This includes diabetes self-management education and support, medical nutrition therapy, physical activity, smoking cessation, and addressing social determinants of health [38,39]. Person-centered comprehensive care is needed to improve health outcomes in diabetes mellitus.
This study has several limitations. First, since this study analyzed cross-sectional data, we could not assess causality and may not reflect changes in variables. Second, misclassification of diabetes mellitus is possible because self-reported information was used for medical history. Third, we evaluated the use of antidiabetic medications using the Korean NHIS data, which may have made a difference from other analyses in study participants. Fourth, we did not examine risk-factor control according to cardiovascular risk or established CVD.
In conclusion, the prevalence of diabetes mellitus among Korean adults remained high. Only 9.7% of adults with diabetes mellitus achieved all glycemic, BP, and lipid controls from 2019 to 2020. Continuous evaluation of national diabetes statistics is important to support and advocate public health policy in reducing the burden of diabetes mellitus and its complication. A national effort to increase awareness of diabetes mellitus and improve comprehensive diabetes care, including preventive practices, is needed to tackle the diabetes epidemic in Korea.
Acknowledgments
We acknowledge the Korean Diabetes Association for supporting this study.
Footnotes
CONFLICTS OF INTEREST
Seung-Hyun Ko has been executive editor of the Diabetes & Metabolism Journal since 2022. Kyung Mook Choi has been editor-in-chief of the Diabetes & Metabolism Journal since 2022. Kyu Chang Won has been the publisher of the Diabetes & Metabolism Journal since 2022. They were not involved in the review process of this article. Otherwise, there was no conflict of interest.
AUTHOR CONTRIBUTIONS
Conception or design: J.H.B., K.D.H., S.H.K., H.S.K.
Acquisition, analysis, or interpretation of data: J.H.B., K.D.H., S.H.K., H.S.K.
Drafting the work or revising: J.H.B., K.D.H., S.H.K., H.S.K.
Final approval of the manuscript: J.H.B., K.D.H., S.H.K., Y.S.Y., J.H.C., K.M.C., H.S.K., K.C.W.
FUNDING
None
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2022.0106.
Estimated prevalence of prediabetes among adult KNHANES participants, 2020
Proportions of prescription of antidiabetic medications in adults with diabetes mellitus from the Korean NHIS data, 2002–2018
Distribution of glycosylated hemoglobin levels among adults Korea National Health and Nutrition Examination Survey (KNHANES) participants with total diabetes mellitus and diagnosed diabetes mellitus, 2019 to 2020.
REFERENCES
- 1.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation . IDF diabetes atlas. 10th ed. Brussels: IDF; 2021. [Google Scholar]
- 3.Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14:88–98. doi: 10.1038/nrendo.2017.151. [DOI] [PubMed] [Google Scholar]
- 4.Korean Diabetes Association . Seoul: Korean Diabetes Association; 2018. Diabetes fact sheet in Korea, 2018. [Google Scholar]
- 5.Korean Diabetes Association . Seoul: Korean Diabetes Association; 2020. Diabetes fact sheet in Korea, 2020. [Google Scholar]
- 6.Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019;34(Suppl 1):e75. doi: 10.3346/jkms.2019.34.e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim J, Yoon SJ, Jo MW. Estimating the disease burden of Korean type 2 diabetes mellitus patients considering its complications. PLoS One. 2021;16:e0246635. doi: 10.1371/journal.pone.0246635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17:11–30. doi: 10.1038/s41574-020-00435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–6. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barron E, Bakhai C, Kar P, Weaver A, Bradley D, Ismail H, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8:813–22. doi: 10.1016/S2213-8587(20)30272-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moon SJ, Rhee EJ, Jung JH, Han KD, Kim SR, Lee WY, et al. Independent impact of diabetes on the severity of coronavirus disease 2019 in 5,307 patients in South Korea: a nationwide cohort study. Diabetes Metab J. 2020;44:737–46. doi: 10.4093/dmj.2020.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muller JA, Gross R, Conzelmann C, Kruger J, Merle U, Steinhart J, et al. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat Metab. 2021;3:149–65. doi: 10.1038/s42255-021-00347-1. [DOI] [PubMed] [Google Scholar]
- 13.Reiterer M, Rajan M, Gomez-Banoy N, Lau JD, Gomez-Escobar LG, Ma L, et al. Hyperglycemia in acute COVID-19 is characterized by insulin resistance and adipose tissue infectivity by SARS-CoV-2. Cell Metab. 2021;33:2174–88. doi: 10.1016/j.cmet.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carr MJ, Wright AK, Leelarathna L, Thabit H, Milne N, Kanumilli N, et al. Impact of COVID-19 on diagnoses, monitoring, and mortality in people with type 2 diabetes in the UK. Lancet Diabetes Endocrinol. 2021;9:413–5. doi: 10.1016/S2213-8587(21)00116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Diabetes Association Professional Practice Committee. Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, et al. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S125–43. doi: 10.2337/dc22-S009. [DOI] [PubMed] [Google Scholar]
- 16.Hur KY, Moon MK, Park JS, Kim SK, Lee SH, Yun JS, et al. 2021 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J. 2021;45:461–81. doi: 10.4093/dmj.2021.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021;45:1–10. doi: 10.4093/dmj.2020.0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oh K, Kim Y, Kweon S, Kim S, Yun S, Park S, et al. Korea National Health and Nutrition Examination Survey, 20th anniversary: accomplishments and future directions. Epidemiol Health. 2021;43:e2021025. doi: 10.4178/epih.e2021025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi EK. Cardiovascular research using the Korean National Health Information Database. Korean Circ J. 2020;50:754–72. doi: 10.4070/kcj.2020.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ministry of Health and Welfare. Korea Disease Control and Prevention Agency . Seoul: KDCA; 2022. Korea Health Statistics 2020: Korea National Health and Nutrition Examination Survey (KNHANES VIII-2) [Google Scholar]
- 21.Kim BY, Kang SM, Kang JH, Kang SY, Kim KK, Kim KB, et al. 2020 Korean Society for the Study of Obesity guidelines for the management of obesity in Korea. J Obes Metab Syndr. 2021;30:81–92. doi: 10.7570/jomes21022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health and Welfare. The Korean Nutritional Society . Seoul: KNS; 2015. Dietary Reference Intakes for Koreans 2015. [Google Scholar]
- 23.Korean Society for the Study of Obesity . Seoul: KSSO; 2021. 2021 Obesity fact sheet. [Google Scholar]
- 24.Park JH, Ha KH, Kim BY, Lee JH, Kim DJ. Trends in cardiovascular complications and mortality among patients with diabetes in South Korea. Diabetes Metab J. 2021;45:120–4. doi: 10.4093/dmj.2020.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi HH, Choi G, Yoon H, Ha KH, Kim DJ. Rising incidence of diabetes in young adults in South Korea: a national cohort study. Diabetes Metab J. 2022 Jan 11; doi: 10.4093/dmj.2021.0236. [Epub]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang YS, Han K, Sohn TS, Kim NH. Young-onset type 2 diabetes in South Korea: a review of the current status and unmet need. Korean J Intern Med. 2021;36:1049–58. doi: 10.3904/kjim.2021.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Montefusco L, Ben Nasr M, D’Addio F, Loretelli C, Rossi A, Pastore I, et al. Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection. Nat Metab. 2021;3:774–85. doi: 10.1038/s42255-021-00407-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022;10:311–21. doi: 10.1016/S2213-8587(22)00044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ministry of Health and Welfare: Coronavirus (COVID-19), Republic of Korea. Available from: http://ncov.mohw.go.kr/en/ (cited 2022 Apr 28)
- 30.Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med. 2021;384:2219–28. doi: 10.1056/NEJMsa2032271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wright AK, Suarez-Ortegon MF, Read SH, Kontopantelis E, Buchan I, Emsley R, et al. Risk factor control and cardiovascular event risk in people with type 2 diabetes in primary and secondary prevention settings. Circulation. 2020;142:1925–36. doi: 10.1161/CIRCULATIONAHA.120.046783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rawshani A, Rawshani A, Franzen S, Sattar N, Eliasson B, Svensson AM, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379:633–44. doi: 10.1056/NEJMoa1800256. [DOI] [PubMed] [Google Scholar]
- 33.Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399:394–405. doi: 10.1016/S0140-6736(21)01919-X. [DOI] [PubMed] [Google Scholar]
- 34.Yabe D, Seino Y. Type 2 diabetes via β-cell dysfunction in east Asian people. Lancet Diabetes Endocrinol. 2016;4:2–3. doi: 10.1016/S2213-8587(15)00389-7. [DOI] [PubMed] [Google Scholar]
- 35.Yoshinari M, Hirakawa Y, Hata J, Higashioka M, Honda T, Yoshida D, et al. Comparison of the contributions of impaired beta cell function and insulin resistance to the development of type 2 diabetes in a Japanese community: the Hisayama Study. Diabetologia. 2021;64:1775–84. doi: 10.1007/s00125-021-05459-7. [DOI] [PubMed] [Google Scholar]
- 36.Jang H, Im J, Park K. Adherence to dietary guidelines among diabetes patients: comparison between elderly and non-elderly groups. Clin Nutr Res. 2021;10:14–23. doi: 10.7762/cnr.2021.10.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020;43:1636–49. doi: 10.2337/dci20-0023. [DOI] [PubMed] [Google Scholar]
- 38.American Diabetes Association Professional Practice Committee. American Diabetes Association Professional Practice Committee. Aroda VR, Bakris G, Benson G, et al. 5. Facilitating behavior change and well-being to improve health outcomes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S60–82. doi: 10.2337/dc22-S005. [DOI] [PubMed] [Google Scholar]
- 39.Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2020;44:258–79. doi: 10.2337/dci20-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Estimated prevalence of prediabetes among adult KNHANES participants, 2020
Proportions of prescription of antidiabetic medications in adults with diabetes mellitus from the Korean NHIS data, 2002–2018
Distribution of glycosylated hemoglobin levels among adults Korea National Health and Nutrition Examination Survey (KNHANES) participants with total diabetes mellitus and diagnosed diabetes mellitus, 2019 to 2020.