Abstract
Blindness is defined as presenting visual acuity worse than 3/60 in the better eye. Its highest proportion has been conforming to the developing countries such as Ethiopia. So, timely information is crucial to design strategies. However, the study on the magnitude of blindness in Ethiopia was outdated which means it was conducted in 2005–2006. Therefore, this study was proposed to estimate the pooled prevalence of blindness in Ethiopia.
Databases like PubMed, Cochrane library, Google Scholar and references of retrieved articles were used to search for articles. A standard data extraction approach was employed and presented using Preferred Reporting of Items for Systematic Reviews and Meta-Analyses. The Newcastle-Ottawa Scale quality assessment tool was used to evaluate the quality of studies. Analysis held using STATA V.11. The funnel plot and Egger’s regression test were applied to check for the potential sources of bias. Heterogeneity among the studies was tested using I² statistics that have been calculated and compared with the standard. Meta-regression and subgroup analysis were done to identify the potential sources of heterogeneity. Estimation of blindness was carried out using Duval and Twee die’s trim and fill analysis. The pooled prevalence of blindness in Ethiopia is found to be 1.18% (95% CI 0.650% to 1.706%). Blindness is among the main public health difficulties in Ethiopia. So, it demands up-to-date strategies and its implementation, preventive and curative eye care service with affordable and accessible interventions, and evidence-based advocacy. The trial Registration Number is CRD42021268448.
Keywords: anterior chamber, cornea, colour vision, epidemiology, eye (globe), glaucoma, low vision aid, macula
Introduction
Blindness refers to a lack of vision which may happen suddenly or over some time due to many reasons1 while WHO defined blindness as presenting visual acuity worse than 3/60 in the better eye.2 Its causes vary from region to region and from country to country.3 The causes of blindness have been either avoidable with prevention and treatment or unavoidable.4 Though the highest percentage of avoidable blindness has been corresponding to low-income and middle-income countries5 like Ethiopia. So, timely information is crucial to design strategies that address the life quality of sightless individuals.
The rationale of the current systematic review
The magnitude of blindness is increasing globally due to an increasing population and longer life expectancy.6 This statement may be true for our country Ethiopia. However, the study on the magnitude of blindness in Ethiopia was outdated (ie, done in 2005–2006).7 Thus, that is the reason that initiated authors to conduct this study while different studies have been conducted at the different segments of the country. Therefore, the authors are interested to estimate the pooled prevalence of blindness in Ethiopia to provide up-to-date comprehensive evidence on this theme.
Objective
To conduct a systematic review and meta-analysis on the prevalence of blindness in Ethiopia.
Review question
What is the pooled prevalence of blindness in Ethiopia?
Methods
Databases and searching strategy
We searched articles from the following databases which are directly related to the subject matter under review. So, PubMed, Cochrane library, Google Scholar and retrieving references from a list of eligible studies were employed. In addition to that, a supplemental search of databases had been applied through manual searching of the reference list of all included papers. We applied a Boolean operator that is “AND” and “OR”. Through consideration of Boolean operator we searched as follows (“Blindness” OR “Blindness” [Mesh Terms] OR “Blindness” [All Fields] “Vision loss”[Mesh Terms] OR “total blindness” [Mesh Terms] OR “avoidable blindness”[All Fields] OR “functional blindness” [All Fields] OR “treatable blindness” [All Fields] OR “preventable blindness” [All Fields] OR “needless blindness”[All Fields] OR “Visual impairment” [All Fields] AND “Ethiopia” [All Fields] by 13 October 2021.
Eligibility criteria
Inclusion criteria
The key features of the target population that the authors used to answer the research question were based on the mnemonic (Condition, Context and Population) approach. So, articles that meet the following criteria were included in this systematic review and meta-analysis.
Ethiopia inhabitants irrespective of their age, occupation, level of education and gender were considered.
Papers in which blindness was measured either based on best-corrected visual acuity or presenting visual acuity using any type of optotype (eg, LogMAR, Snellen E chart) were considered.
Original studies published only from 1990 to 2021, and that fulfil the other inclusion criteria were included.
This review included all cross-sectional and survey studies done using probability sampling techniques to keep the representativeness of the research finding (ie, including studies done using non-probability sampling may reduce the generalisability and accuracy of the estimation and its CI).
Studies only done in Ethiopia were included.
Exclusion criteria
Studies that did not fulfil the inclusion criteria were excluded.
Sample size
In the current meta-analysis, a total of 96 101 participants were included to estimate the pooled prevalence of blindness in Ethiopia. The study’s sample size was ranged from the highest (n=25 650)7 to the lowest (n=93).8
Data extraction and management
Standard systematic searching was conducted from those databases. Studies conducted before 1990, conducted in countries other than Ethiopia and unrelated articles based on their title were excluded. Those potentially eligible studies were imported to Endnote V.7 and exact duplicates had been removed. Two independent reviewers did the abstract and full-text review and data abstraction. In case of disagreement between the reviewers, a discussion was made to reach on consensus. Lastly, studies were screened and selected for full-text reviews based on the inclusion criteria. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was used for reporting systematic review and meta-analysis to present the study inclusion, exclusion and reason for exclusion information in the diagram. The extraction included: author, publication status, region in the country where the study was conducted, study design, year of publication, the sample size and frequency of participants with blindness. Excel software was used for data storage.
Quality assessment
To evaluate the quality of the studies, the authors utilised the Newcastle-Ottawa Scale quality assessment tool.9 Using the tool as a protocol, the reviewers (MM, BK and HBT) used the blinded review approach to evaluate the quality of the original articles. Those studies with high-quality scores (≥6 out of 10 scales) were included for analysis while it should be noted that medium and low-quality studies have been excluded from the meta-analysis. Conflicting ratings were resolved by taking the mean score of the authors to reach on consensus among reviewers.
Statistical analysis
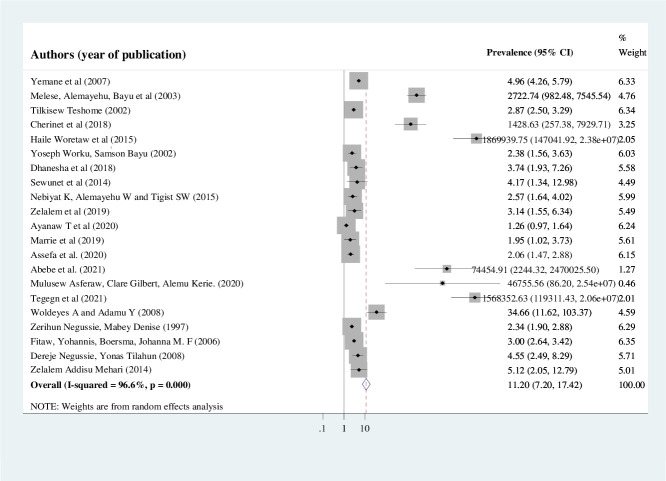
A structured and standardised approach in which the prevalence of blindness, methodology (ie, sample size, study design), Year of publication, and authors were extracted from the primary studies using Microsoft Excel V.2013 format. A meta-analysis that based on a proportions approach was performed to determine the pooled estimate of blindness by using STATA V.11 software. The primary articles were summarised by using the table (table 1) and forest plot (figure 2). The researchers calculated the SE of the prevalence of blindness for each original article using the formula √ (P (100 P)/N) (where, P is the prevalence of blindness for each original article, N is the sample size of that specific study, √=the square root). If any heterogeneity is observed, it is considered as high (≥75%), moderate (25%–75%) and low (25% or less).10 Due to the high (considerable) degree of heterogeneity between the results of primary studies (I²=96.6%, p=0.000), a random effect model was applied to estimate the pooled prevalence of blindness. Univariate meta-regression was undertaken by taking the year of publication and sample size to detect the possible source (s) of heterogeneity, and authors identified sample size (p=0.005) to be a statistically significant source of heterogeneity. Point and pooled estimates as well as their 95% confidence intervals were illustrated by forest plots. Potential publication bias was assessed subjectively by funnel plot and objectively using Egger’s weighted correlation and Begg’s regression intercept at 5% significance level.11 In Egger’s test (p=0.008) and Begg’s test (p=0.001), the p value found to be less than 0.05 indicates the presence of publication bias. Therefore, further estimation was carried out using Duval and Twee die’s trim-and-fill analysis.
Table 1.
Primary studies included in the study of the prevalence of blindness in Ethiopia, 2021 (n=21)
| Author (s) name | Year of publication | Publication status | Sample size | Prevalence (95% CI) | Response rate | Quality score (out of 10) |
| Berhane et al7 | 2007 | Published | 25 650 | 1.60 (1.45 to 1.76) | 85.40% | 7 |
| Melese et al62 | 2003 | Published | 2693 | 7.91 (6.89 to 8.93) | 90.8% | 8 |
| Tilkisew52 | 2002 | Published | 21 350 | 1.05 (0.92 to 1.19) | 92.8% | 7 |
| Cherinet et al67 | 2018 | Published | 881 | 7.26 (5.55 to 8.98) | 97.4% | 9 |
| Haile and Destaye53 | 2015 | Published | 734 | 14.44 (11.9 to 16.98) | 100% | 8 |
| Worku and Bayu63 | 2002 | Published | 1846 | 0.87 (0.44 to 1.29) | 100% | 7 |
| Dhanesha et al61 | 2018 | Published | 1137 | 1.32 (0.66 to 1.98) | 95.1% | 7 |
| Sewunet et al55 | 2014 | Published | 420 | 1.43 (0.29 to 2.56) | 97.2% | 8 |
| Nebiyat et al68 | 2015 | Published | 1800 | 0.94 (0.50 to 1.39) | 99.4% | 8 |
| Zelalem et al54 | 2019 | Published | 875 | 1.14 (0.44 to 1.85) | 100% | 8 |
| Ferede et al56 | 2020 | Published | 1289 | 0.23 (-0.03 to 0.50) | 100% | 6 |
| Marrie et al57 | 2019 | Published | 601 | 0.67 (0.02 to 1.32) | 95.2% | 8 |
| Assefa et al58 | 2020 | Published | 416 | 0.72 (0.38 to 1.06) | 98.6% | 7 |
| Abebe et al16 | 2021 | Published | 312 | 11.22 (7.72 to 14.72) | 96% | 8 |
| Asferaw et al8 | 2020 | Published | 93 | 10.75 (4.46 to 17.05) | NR | 6 |
| Tegegn et al59 | 2021 | Published | 708 | 14.27 (11.69 to 16.84) | 99.02% | 9 |
| Woldeyes and Adamu64 | 2008 | Published | 1100 | 3.55 (2.45 to 4.64) | 100% | 8 |
| Zerihun and Mabey51 | 1997 | Published | 7423 | 0.85 (0.64 to 1.06) | 90.4% | 6 |
| Fitaw and Boersma60 | 2006 | Published | 24 453 | 1.10 (0.97 to 1.23) | 100% | 7 |
| Negussie and Tilahun66 | 2008 | Published | 1585 | 1.51 (0.91 to 2.12) | 100% | 7 |
| Mehari65 | 2014 | Published | 735 | 1.63 (0.72 to 2.55) | NR | 6 |
NR, not reported.
Subgroup analysis
Subgroup analysis was conducted based on region, year of publication, sample size and based on meta-regression output.
Results
Searching results
The authors searched for pieces of literature for the theme under appraisal by 13 October 2021. A total of 319, 1040, 248 and 11 records have been identified through PubMed, Google Scholar, Cochrane Library and reference lists of retrieved articles, respectively.
A total of 1407 retrievals remained after the removal of duplicates. After evaluating the titles and abstracts, 1331 retrievals had been excluded because they were inappropriate for this meta-analysis regarding the outcome of interest. A total of 16 full-text studies and reviews come to be illegible because they were conducted outside Ethiopia.
Sixty-one full-text articles were assessed for eligibility based on the consideration criteria. Of those articles, 31 were found to be irrelevant for this review.12–42 Two articles that were done using non-probability sampling technique43 44 were excluded due to the concern that they may reduce the success of the study outcome. Two articles in which participants were self-selected45 46 were rejected with the caution to not bias representativeness of the result.
Four studies with an agreed quality score of less than six36 47–49 were disallowed to this meta-analysis to be confident that the reported results reflect the true nature of the data. One study done at refugee camps was banned from this meta-analysis, because it may include non-Ethiopian population.50
Finally, 21 studies were included in this qualitative and quantitative synthesis (online supplemental figure 1).
bmjophth-2021-000949supp001.pdf (464.2KB, pdf)
Description of original studies
In this study, 21 survey and cross-sectional studies were included (table 1). The studies were conducted from the year 1990–2021. The study’s sample size was ranged from the highest (n=25 650)7 to the lowest (n=93).8 In the current meta-analysis, a total of 96 101 participants were included to estimate the pooled prevalence of blindness in Ethiopia. The studies were conducted in the different parts of Ethiopia: Nationwide,7 36 Oromia Region,51 Amhara Region,16 48 49 52–60 Tigray Region,61 Southern Nation Nationalities Peoples Region (SNNPR),62–66 Gambella and Benishangul Gumuz Regions,50 Addis Ababa City Administration8 67 68 and unspecified (ie, area) school-based study.47 All of the studies were published. Independent evaluators’ (MM, BK and HBT) reassessed the articles and reached a consensus on articles on which disagreement was raised before the analysis. All studies with a quality score greater than or equal to 6 out of 10 were considered for synthesis.
Meta-analysis
Prevalence of blindness in Ethiopia
In this meta-analysis, a random effect model was used to estimate the overall pooled prevalence of blindness in Ethiopia (figure 1). But, considerable heterogeneity was seen among studies, objectively detected by I² statistic (I²=96.6%, p˂0.0001). Then, univariate Meta-regression was performed to explore the possible sources of heterogeneity. In meta-regression, sample size (p=0.005) and quality assessment score (p=0.047) were found to be potentially significant factors associated with the heterogeneity (table 2). So, the convention of the pooled prevalence of blindness in Ethiopia was attained using Duval and Twee die’s trim-and-fill analysis and found to be 1.18% (95% CI 0.650% to 1.706%).
Figure 1.
Forest plot representing the pooled prevalence of blindness in Ethiopia, 2021.
Table 2.
Factors related to the prevalence of blindness in Ethiopia, 2021 (based on univariate meta-regression)
| Variables | Coefficient | P value |
| Year of publication | −0.94564 | 0.174 |
| Sample size | −0.00088 | 0.005 |
Begg’s and Egger’s tests revealed the presence of statistically significant publication bias (p=0.001) and (p=0.008), respectively. The funnel plot also showed that the dots, representing the studies, were asymmetrically indicated the presence of publication bias (figure 2). Therefore, the trim-and-fill method was applied, and with this method, the pooled prevalence of blindness in Ethiopia was found to be 1.18% (95% CI 0.650% to 1.706%).
Figure 2.
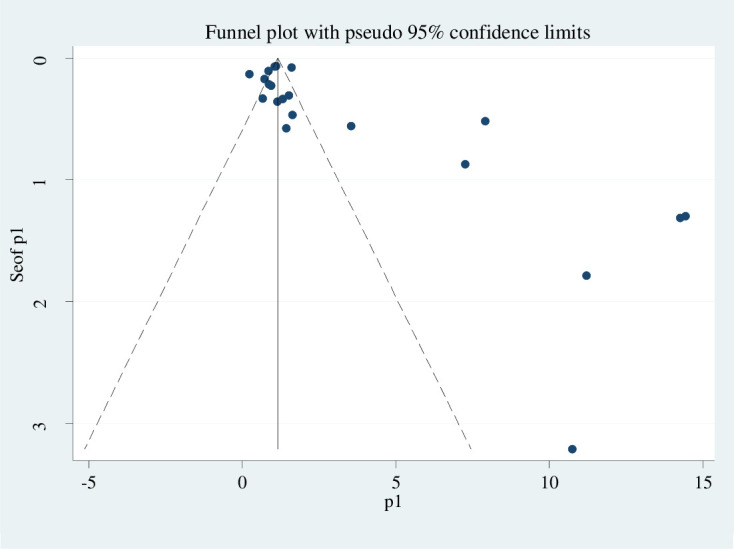
The funnel plot of meta-analysis in the pooled prevalence of blindness in Ethiopia including 21 studies, 2021
Subgroup analysis
Also, we performed subgroup analysis to explore sources of heterogeneity based on the region where the studies conducted, sample size and year of publication (table 3).
Table 3.
Subgroup analysis of the prevalence of blindness in Ethiopia, 2021 (n=21)
| Variables | Characteristics | Number of studies | Prevalence with 95% CI |
| Region | Amhara | 10 | 1.00 (0.92 to 1.08) |
| Addis Ababa | 3 | 1.39 (0.96 to 1.82) | |
| SNNPR | 5 | 1.90 (1.60 to 2.20) | |
| Other* | 3 | 1.34 (1.22 to 1.46) | |
| Sample size | Greater than 1000 | 11 | 1.14 (1.07 to 1.21) |
| Less than 1000 | 10 | 1.34 (1.09 to 1.59) | |
| Year of publication | Before 2010 | 8 | 1.21 (1.14 to 1.29) |
| After 2010 | 13 | 0.86 (0.70 to 1.02) |
*Tigray region, nationwide.
SNNPR, Southern Nation Nationalities Peoples Region.
Accordingly, the highest prevalence was reported in the SNNP region with a prevalence of 1.90% (95% CI 1.60% to 2.20%) (table 3). Concerning sample size, the prevalence of blindness is found to be nearly comparable in studies that had been included less than 1000 participants (1.14%; 95% CI 1.07% to 1.21%) and greater than 1000 participants (1.34%, 95% CI 1.09% to 1.59%) (table 3). Regarding the year of publication of studies, the prevalence of blindness was higher in studies that had been conducted before 2010 (1.21%; 95% CI 1.14% to 1.29%) as compared with those studies carried out after 2010 (0.86%; 95% CI 0.70% to 1.02%) (table 3).
Discussion
Globally, blindness is recognised as one of the major public health problems, especially in low-income and middle-income countries where 90% of blind live.69 Ethiopia is one of the countries in which blindness was a public health issue according to Berhane et al.7
It is not always feasible to do a constant nationwide survey to have up-to-date information for health policy-makers, planners and advocators due to financial and qualified eye care insufficiency in developing countries. So, systematic review and meta-analysis of the existing small-scale studies in different parts of the country may play a significant role to address such kinds of concerns. In this meta-analysis, the estimated prevalence of blindness in Ethiopia is found to be 1.18% (ie, approximately 120 individuals are blind per 10 000 population) using 21 relevant studies. This finding is higher than the ‘vision 2020: the right to sight’ plan, to reduce blindness to less than 0.5% in all countries of the world, especially avoidable blindness.70 In Ethiopia, more than 80% of blindness has been preventable or treatable.7
The prevalence of blindness in this meta-analysis (1.18%, ie, 13.9 million of the current estimate of 118 million population) is lower than that of nationwide survey (1.6%, ie, 1.2 million of 75 million estimated population).7 The prevalence of blindness in Ethiopia was found to be reduced compared with the 2005–2006 study.7 However, the actual number of people with blindness has probably substantially increased, owing to population increase71 and ageing.72 This is all consistent with the Vision Loss Expert Group global blindness findings.6 Another possible explanation could be that health education and health promotion on primary eye care specifically on eye care may not be adequate. Our finding implies that the problem requires much more striving to reduce the prevalence of blindness in Ethiopia.
It was also the author’s concern to provide more information on the age distribution of blindness prevalence and numbers affected, however, the authors did not report that due to disagreement on data clarity regarding this specific issue and that is what hindered us from doing subgroup analysis based on age category.
The subgroup analysis of this study also showed that the prevalence of blindness varies across regions of Ethiopia. The highest prevalence of blindness was seen in people living in SNNPR (1.90%) as compared with other regions of the country. This pinpoints that despite the ‘vision 2020’ strategy implementation throughout the country, the condition (ie, blindness) is still in need of action while the SNNP region is yet another part of Ethiopia where incredible intervention to be viably implemented. This highest prevalence in the SNNP region may be comparatively due to obsolete studies (ie, most of the studies done in SNNPR and included in this meta-analysis were not performed recently).62–64 66 Appreciating this finding as evidence, we regret its representativeness of the recent outcome of that region of Ethiopia.
In this review, the prevalence of blindness was not relatively dependent on sample size (ie, 1.14% and 1.34% with comparable (overlapping) CIs for studies with a sample size of greater than 1000 and less than 1000, respectively). This cut point was not formally tested, but it is a subjective decision by authors to see any effect of sample size difference on the prevalence of blindness. At the same time, readers should recognise that there was no minimum sample size for studies to be included in this review. We hypothesise that this relative similarity may be due to the similar socioeconomic status of the study participants involved in studies that have been incorporated in this meta-analysis. Concerning study year, the prevalence of blindness was significantly lower in those studies conducted since 2010 as compared with those studied before 2010. This is probably due to the recently increasing number of outreach campaigns in different parts of the country. Another possible explanation could be that nearly all studies that were conducted in Ethiopia since 2010 may be fairly quality controlled.
This met-analysis is satisfactory in that it denotes the overall prevalence of blindness in Ethiopia, was stuck to the guidelines, ensuring the reliability in reporting and the full systematic review, and it offers the prevalence of blindness in regions of Ethiopia while it is limited in that it didn’t provide age and gender-specific prevalence of blindness.
Conclusion
According to this meta-analysis, blindness in Ethiopia is among the main public health difficulties of the country. So, it can cause a huge economic and social impact for the affected persons and to the community, and the country at large. Thus, to address this backlog of blindness, it demands up-to-date strategies and its implementation, preventive and curative eye care service with affordable and accessible interventions, and evidence-based advocacy to awaken all concerned bodies who are working to discourse avoidable blindness.
Footnotes
Contributors: MM: conception of research protocol, study design, literature review, data extraction, data analysis, quality assessment, interpretation and drafting the manuscript. BK and HBT: Data extraction, quality assessment and reviewing the manuscript. All the authors have read and approved the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Medical Encyclopedia . Blindness and vision loss, 2021. [Google Scholar]
- 2.World Health Organization . Fact sheets detail in blindness and visual impairment, 2021. [Google Scholar]
- 3.Kv V, Vijayalakshmi P. Understanding definitions of visual impairment and functional vision. Community Eye Health 2020;33:S16–17. [PMC free article] [PubMed] [Google Scholar]
- 4.Dunning H. Leading causes of 'avoidable blindness' identified as cases set to increase. The Lancet Glob Health 2017. [Google Scholar]
- 5.Resnikoff S, Pascolini D, Etya'ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004;82:844–51. doi:/S0042-96862004001100009 [PMC free article] [PubMed] [Google Scholar]
- 6.Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health 2017;5:e1221–34. 10.1016/S2214-109X(17)30393-5 [DOI] [PubMed] [Google Scholar]
- 7.Berhane Y, Worku A, Bejiga A. Prevalence and causes of blindness and low vision in Ethiopia. Ethiop J Health Dev 2007;21:204–10. [Google Scholar]
- 8.Asferaw M, Gilbert C, Kerie A. Retinopathy of prematurity -an emerging cause of childhood blindness in Ethiopia. Ethiop Med J 2020;58:167–72. [Google Scholar]
- 9.Newcastle-Ottawa . Scale customized for cross-sectional studies. [Google Scholar]
- 10.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 11.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001;54:1046–55. 10.1016/s0895-4356(01)00377-8 [DOI] [PubMed] [Google Scholar]
- 12.Alemayehu W, Tekle-Haimanot R, Forsgren L. Causes of visual impairment in central Ethiopia. Ethiop Med J 1995;33:163–74. [PubMed] [Google Scholar]
- 13.Alemayehu Woldeyes YA. Prevalence of cataract blindness in rural Ethiopia. Ethiop J Health Dev 2011;25:156–60. [Google Scholar]
- 14.Assefa NL, Tegegn MT, Wolde SY. Knowledge and attitude of refractive error among public high school students in Gondar City. Clin Optom 2021;13:201–8. 10.2147/OPTO.S322438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Assem AS, Tegegne MM, Fekadu SA. Prevalence and associated factors of myopia among school children in Bahir Dar City, Northwest Ethiopia, 2019. PLoS One 2021;16:e0248936. 10.1371/journal.pone.0248936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abebe H, Wagnew F, Zeleke H, et al. Magnitude of visual impairment and associated factors among patients attending ophthalmic clinics of Debre Markos referral Hospital, North West Ethiopia. BMC Ophthalmol 2021;21:96. 10.1186/s12886-021-01863-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bayu S, Alemayehu W. Pattern of neuro-ophthalmic disorders in a tertiary eye care centre in Addis Ababa. Ethiop Med J 1997;35:43–51. [PubMed] [Google Scholar]
- 18.Belete G, Anbesse D, Tsegaye A, et al. Prevalence and associated factors of myopia among high school students in Gondar town, Northwest Ethiopia, 2016. Clin. Optom 2017;9:11–18. 10.2147/OPTO.S120485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bezabih L, Abebe TW, Fite RO. Prevalence and factors associated with childhood visual impairment in Ethiopia. Clin Ophthalmol 2017;11:1941–8. 10.2147/OPTH.S135011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biza M, Mossie A, Woldemichael K. Visual impairment and road traffic accidents among drivers in Jimma town, Southwest Ethiopia. Ethiop Med J 2013;51:123–32. [PubMed] [Google Scholar]
- 21.Chala MB, Mekonnen S, Andargie G, et al. Prevalence of disability and associated factors in Dabat health and demographic surveillance system site, Northwest Ethiopia. BMC Public Health 2017;17:762. 10.1186/s12889-017-4763-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clarke EL, Evans JR, Smeeth L. Community screening for visual impairment in older people. Cochrane Database Syst Rev 2018;2:CD001054. 10.1002/14651858.CD001054.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Courtright P, Klungsøyr P, Lewallen S. The epidemiology of blindness and visual loss in Hamar tribesmen of Ethiopia. The role of gender. Trop Geogr Med 1993;45:168–70. [PubMed] [Google Scholar]
- 24.Darge HF, Shibru G, Mulugeta A, et al. The prevalence of visual acuity impairment among school children at Arada Subcity primary schools in Addis Ababa, Ethiopia. J Ophthalmol 2017;2017:1–7. 10.1155/2017/9326108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demissie BS, Solomon AW. Magnitude and causes of childhood blindness and severe visual impairment in Sekoru district, Southwest Ethiopia: a survey using the key informant method. Trans R Soc Trop Med Hyg 2011;105:507–11. 10.1016/j.trstmh.2011.04.007 [DOI] [PubMed] [Google Scholar]
- 26.Thomas BJ, Sanders DS, Oliva MS, et al. Blindness, cataract surgery and mortality in Ethiopia. Br J Ophthalmol 2016;100:1157–62. 10.1136/bjophthalmol-2015-308328 [DOI] [PubMed] [Google Scholar]
- 27.Gessesse SA, Teshome AW. Prevalence of myopia among secondary school students in Welkite town: south-western Ethiopia. BMC Ophthalmol 2020;20:176. 10.1186/s12886-020-01457-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abayo G, Gessesse GW, Asaminew T. Prevalence and pattern of ocular morbidity among school children in southern Ethiopia. Ethiop J Health Sci 2021;31:831–6. 10.4314/ejhs.v31i4.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Getnet M, Akalu Y, Dagnew B, et al. Visual impairment and its associated factors among medical and health sciences students at the University of Gondar, Northwest Ethiopia. PLoS One 2021;16:e0255369. 10.1371/journal.pone.0255369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hailu Y, Hiko D, Shaweno T. Prevalence of visual impairment and associated factors among primary schoolchildren in Addis Ababa, central Ethiopia. Clin Ophthalmol 2020;14:767–74. 10.2147/OPTH.S245675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehari ZA, Yimer AW. Prevalence of refractive errors among schoolchildren in rural central Ethiopia. Clin Exp Optom 2013;96:65–9. 10.1111/j.1444-0938.2012.00762.x [DOI] [PubMed] [Google Scholar]
- 32.Shaffi M, Bejiga A. Common eye diseases in children of rural community in Goro district, central Ethiopia. Ethiop JHealth Dev 2005;19:148–52. 10.4314/ejhd.v19i2.9984 [DOI] [Google Scholar]
- 33.Shiferaw Alemu D, Desalegn Gudeta A, Tsega Ferede A, et al. Prevalence and degrees of myopia and hyperopia at Gondar university hospital tertiary eye care and training center, Northwest Ethiopia. Clin Optom 2016;8:85–91. 10.2147/OPTO.S116535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tegegn MT, Belete GT, Ferede AT, et al. Proportion and associated factors of low vision among adult patients attending at University of Gondar tertiary eye care and training center, Gondar town, Ethiopia. J Ophthalmol 2020;2020:1–7. 10.1155/2020/7042905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tesfaye A, Bejiga A. Ocular injuries in a rural Ethiopian community. East Afr Med J 2008;85:593–6. [PubMed] [Google Scholar]
- 36.Kello AB, Gilbert C. Causes of severe visual impairment and blindness in children in schools for the blind in Ethiopia. Br J Ophthalmol 2003;87:526–30. 10.1136/bjo.87.5.526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woldeamanuel GG, Biru MD, Geta TG, et al. Visual impairment and associated factors among primary school children in Gurage zone, southern Ethiopia. Afr Health Sci 2020;20:533–42. 10.4314/ahs.v20i1.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.WoldeKidan E, Daka D, Legesse D, et al. Prevalence of active trachoma and associated factors among children aged 1 to 9 years in rural communities of Lemo district, southern Ethiopia: community based cross sectional study. BMC Infect Dis 2019;19:886. 10.1186/s12879-019-4495-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yared AW, Belaynew WT, Destaye S, et al. Prevalence of refractive errors among school children in gondar town, Northwest Ethiopia. Middle East Afr J Ophthalmol 2012;19:372–6. 10.4103/0974-9233.102742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kedir J, Girma A. Prevalence of refractive error and visual impairment among rural school-age children of Goro district, Gurage zone, Ethiopia. Ethiop J Health Sci 2014;24:353–8. 10.4314/ejhs.v24i4.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abebe H, Abebe Y, Loha E, et al. Consumption of vitamin A rich foods and dark adaptation threshold of pregnant women at Damot sore district, Wolayita, southern Ethiopia. Ethiop J Health Sci 2014;24:219–26. 10.4314/ejhs.v24i3.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yibekal BT, Alemu DS, Anbesse DH, et al. Vision-Related quality of life among adult patients with visual impairment at University of Gondar, Northwest Ethiopia. J Ophthalmol 2020;2020:1–7. 10.1155/2020/9056097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Basha GK, van Heerden HJ. Profile and opinion of people with disability with respect to adapted physical activity participation in Ethiopia. Afr J Disabil 2020;9:a657. 10.4102/ajod.v9i0.657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Demissie BS, Demissie ES. Patterns of eye diseases in children visiting a tertiary teaching hospital: south-western Ethiopia. Ethiop J Health Sci 2014;24:69–74. 10.4314/ejhs.v24i1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aga A. Avoidable visual impairment among elderly people in a slum of Addis Ababa. Ethiop J Health Dev 2001;15:139–44. 10.4314/ejhd.v15i2.9888 [DOI] [Google Scholar]
- 46.Mehari ZA. A study of ocular morbidity of patients attending ophthalmic outreach services in rural Ethiopia. Int J Med Sci 2013;3:450–4. [Google Scholar]
- 47.Wolde-Gebriel Z, Gebru H, West CE. Causes of blindness in children in the blind schools of Ethiopia. Trop Geogr Med 1992;44:135–41. [PubMed] [Google Scholar]
- 48.Asemu MT, Ahunie MA. The impact of diabetes on visual acuity in Ethiopia, 2021. PLoS One 2021;16:e0256145. 10.1371/journal.pone.0256145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Asferaw M, Woodruff G, Gilbert C. Causes of severe visual impairment and blindness in students in schools for the blind in Northwest Ethiopia. BMJ Glob Health 2017;2:e000264. 10.1136/bmjgh-2016-000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gelaw Y, Abateneh A. Ocular morbidity among refugees in Southwest Ethiopia. Ethiop J Health Sci 2014;24:227–34. 10.4314/ejhs.v24i3.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zerihun N, Mabey D. Blindness and low vision in Jimma zone, Ethopia: results of a population-based survey. Ophthalmic Epidemiol 1997;4:19–26. 10.3109/09286589709058057 [DOI] [PubMed] [Google Scholar]
- 52.Teshome T. Prevalence and causes of blindness in Merhabete, North Shoa, Ethiopia. Ethiop J Health Dev 2002;16:71–6. 10.4314/ejhd.v16i1.9828 [DOI] [Google Scholar]
- 53.Haile W, Destaye S. Prevalence and associated factors of visual impairment and blindness at University of Gondar teaching Hospital, Godar, Northwest Ethiopia. Int. j. pharm. health care res 2015;03:48–54. [Google Scholar]
- 54.Zelalem M, Abebe Y, Adamu Y, et al. Prevalence of visual impairment among school children in three primary schools of Sekela Woreda, Amhara regional state, north-west Ethiopia. SAGE Open Med 2019;7:205031211984976. 10.1177/2050312119849769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sewunet SA, Aredo KK, Gedefew M. Uncorrected refractive error and associated factors among primary school children in Debre Markos district, Northwest Ethiopia. BMC Ophthalmol 2014;14:95. 10.1186/1471-2415-14-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ferede AT, Alemu DS, Gudeta AD, et al. Visual impairment among primary school children in Gondar town, Northwest Ethiopia. J Ophthalmol 2020;2020:1–6. 10.1155/2020/6934013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Merrie YA, Tegegne MM, Munaw MB, et al. Prevalence and associated factors of visual impairment among school-age children in Bahir Dar City, Northwest Ethiopia. Clin Optom 2019;11:135–43. 10.2147/OPTO.S213047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Assefa NL, Admas AW, Adimasu NF. Prevalence and associated factors of visual impairment among adults at Debre Berhan town, North Shewa, Ethiopia. BMC Ophthalmol 2020;20:316. 10.1186/s12886-020-01586-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tegegn MT, Assaye AK, Mersha GA. Proportion, causes and associated factors of blindness among adult patients attending tertiary eye care and training center in Ethiopia. Clin Optom 2021;13:82–91. 10.2147/OPTO.S295626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fitaw Y, Boersma JMF. Prevalence and impact of disability in north-western Ethiopia. Disabil Rehabil 2006;28:949–53. 10.1080/09638280500404552 [DOI] [PubMed] [Google Scholar]
- 61.Dhanesha U, Polack S, Bastawrous A, et al. Prevalence and causes of visual impairment among schoolchildren in Mekelle, Ethiopia. Cogent Med 2018;5:1554832. 10.1080/2331205X.2018.1554832 [DOI] [Google Scholar]
- 62.Melese M, Alemayehu W, Bayu S, et al. Low vision and blindness in adults in Gurage zone, central Ethiopia. Br J Ophthalmol 2003;87:677–80. 10.1136/bjo.87.6.677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Worku Y, Bayu S. Screening for ocular abnormalities and subnormal vision in school children of Butajira town, southern Ethiopia. Ethiop J Health Dev 2002;16:165–71. 10.4314/ejhd.v16i2.9807 [DOI] [Google Scholar]
- 64.Woldeyes A, Adamu Y. Gender differences in adult blindness and low vision, central Ethiopia. Ethiop Med J 2008;46:211–8. [PubMed] [Google Scholar]
- 65.Mehari ZA. Pattern of childhood ocular morbidity in rural eye Hospital, central Ethiopia. BMC Ophthalmol 2014;14:1–6. 10.1186/1471-2415-14-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Negussie D, Tilahun Y. Pattern of corneal blindness in Goro district, Gurage zone, southern Ethiopia. Ethiop. J.Health Dev 2008;22:298–301. [Google Scholar]
- 67.Cherinet FM, Tekalign SY, Anbesse DH, et al. Prevalence and associated factors of low vision and blindness among patients attending St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. BMC Ophthalmol 2018;18:1–6. 10.1186/s12886-018-0899-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nebiyat K, Alemayehu W, Tigist S. Refractive errors among school children in Addis Ababa, Ethiopia. J Ophthalmol East Cent S Afr 2015:57–62. [Google Scholar]
- 69.Thylefors B, Négrel AD, Pararajasegaram R, et al. Global data on blindness. Bull World Health Organ 1995;73:115–21. [PMC free article] [PubMed] [Google Scholar]
- 70.WHO . Prevention of blindness and deafness. global initiative for the elimination of avoidable blindness WHO document WHO/PBL/97.61 Rev 2. Geneva: WHO, 2000. [Google Scholar]
- 71.Macrotrends . Ethiopia population 2021, 2021. [Google Scholar]
- 72.Macrotrends . Ethiopia life expectancy 1950-2021, 2021. Available: https://www.macrotrends.net
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjophth-2021-000949supp001.pdf (464.2KB, pdf)