Abstract
Background
This retrospective study investigated the incidence rate of accidental foreign body aspiration and ingestion according to patient sex, age, and dental department. This study aimed to verify whether the incidence rate is higher in geriatric than in younger patients and whether it is different among dental departments.
Methods
Accidental foreign body aspiration and ingestion cases were collected from electronic health records and the safety report system of Yonsei University Dental Hospital from January 2011 to December 2017. The collected data included patients’ age, sex, medical conditions, treatment procedures, and foreign objects that were accidentally aspirated or ingested. The incidence rate was calculated as the number of accidental foreign body aspirations and ingestions relative to the total number of patient visits. Differences depending on the patients’ sex, age, and dental department were statistically identified.
Results
There were 2 aspiration and 37 ingestion cases during the 7-year analysis period. The male to female incidence ratio was 2.8:1. The incidence rate increased with age and increased rapidly among those aged 80 years or older. Seven of the 37 patients with accidental foreign body ingestion had intellectual disability, Lou Gehrig’s disease, dystonia, or oral and maxillofacial cancer. The incidence rate was highest in the Predoctoral Student Clinic and the Department of Prosthodontics. The most frequently swallowed objects were fixed dental prostheses and dental implant components.
Conclusion
The incidence rate of accidental foreign body aspiration and ingestion differed according to patient sex, age, and dental department. Dental practitioners must identify high-risk patients and apply various methods to prevent accidental foreign body aspiration and ingestion in dental clinics. Inexperienced practitioners should be particularly careful.
Keywords: Aspiration, Dentistry, Emergencies, Foreign Bodies, Incidence, Ingestion
INTRODUCTION
Since the 1990s, there has been growing interest in patient safety, and an increasing number of articles have been published regarding the same. Based on this, we can establish and apply preventive strategies to ensure patient safety [1]. However, because dentistry is perceived to be relatively safe among the medical field, there is a lack of research and literature regarding patient safety in dentistry compared with other medical fields [2,3].
Patient safety incidence (PSI) in dentistry includes: 1) errors in diagnosis, treatment planning, documentation, and communication at the preoperative stage; 2) procedure errors, equipment failure, infection control, accidental foreign body aspiration and ingestion, etc. at intraoperative stage; and 3) drug prescription errors and lack of follow-ups at postoperative stage [3].
A systematic review lists accidental foreign body ingestion or aspiration as one of the five major PSIs, along with errors in diagnosis and examination, treatment planning, communication, and procedural errors [3]. Accidental foreign body aspiration and ingestion are reported to be rare, with an incidence of less than 1%-12% of PSIs. However, when it does occur, it can become an emergency situation and, in rare cases, life-threatening [4,5,6]. For patient safety, dental practitioners should do their best to prevent accidental foreign body aspiration and ingestion in the dental office. Identifying high-risk patients and knowing which objects are frequently swallowed will help in this regard. Many objects can potentially be aspirated or ingested, including endodontic instruments, orthodontic materials, and dental implant components [7,8,9]. Ingestion occurs more frequently than aspiration, and the frequency is influenced by patient age, medical conditions, and type of dental procedure [10,11,12].
This retrospective study analyzed accidental foreign body aspiration and ingestion cases that occurred at Yonsei University Dental Hospital over a 7-year period. The incidence rate of accidental foreign body aspiration and ingestion and the affecting factors such as the patients’ age, sex, medical conditions, and dental treatment involved were analyzed. Based on an analysis of the present cases, we identified the information that should be included in predoctoral and continuing education to prevent accidental foreign body aspiration and ingestion.
METHODS
We collected and analyzed data to determine the incidence of accidental foreign body aspiration and ingestion according to sex, age, and dental department. This retrospective chart review study involving human participants was conducted in accordance with the ethical standards of the institutional and national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of Yonsei University Dental Hospital (approval number: 2-2019-0074). Formal consent was not required due to the nature of the study.
1. Data collection and analysis
We searched electronic health records (EHRs) for patients who visited Yonsei University Dental Hospital between January 2011 and December 2017. The following patient inclusion criteria were satisfied:
1) Visited a medical department on the day of the dental visit or the following day.
2) The patient underwent neck, chest, or abdominal radiography; laryngoscopy; or endoscopy on that day.
3) The presence of a foreign body stated in the EHR.
4) The occurrence of accidental foreign body aspiration and ingestion confirmed in the EHR.
We also included accidental foreign body aspiration and ingestion cases reported in the safety report system of Yonsei University Dental Hospital from January 2011 to December 2017. In addition to the cases identified through the EHR search, 12 cases were added through the patient safety report.
The collected data included the patients’ age, sex, medical conditions, dental departments where accidental foreign body aspiration or ingestion occurred, dental treatment applied, aspirated or ingested foreign body medical examination, treatment, and progress.
During the same period, the total number of patient visits by sex, age, clinical department, and treatment procedure in which foreign body aspiration and ingestion were reviewed, and the incidence rate was calculated as the ratio of the number of cases of accidental foreign body aspiration and ingestion relative to the total number of patient visits. The incidence rates were calculated according to the patients’ age, sex, dental departments, and treatment procedures.
2. Statistical analysis
The incidence rates according to sex, age, and clinical department were compared using the chi-square test. Data analysis was performed using SPSS ver. 25.0 software (SPSS Inc., Chicago, IL, USA) with a significance criterion of P < 0.05.
RESULTS
1. Incidence
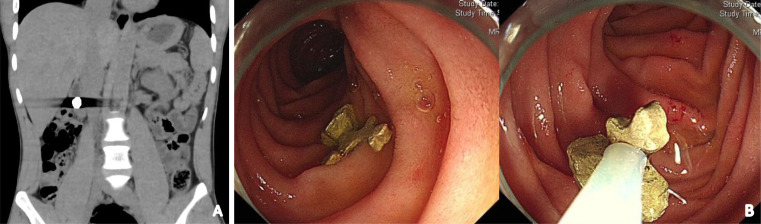
There were 39 cases of foreign body aspiration (n = 2) and ingestion (n = 37) identified during the 7-year study period. During the same period, the total number of patient visit was 2,672,250 and the incidence rate was 14.6/million. The 37 ingestion cases included seven patients with the following conditions that could affect swallowing or cognition: one with intellectual disability, one with Lou Gehrig’s disease, one with oromandibular dystonia, and four with a history of extensive resection due to oral or maxillofacial cancer (three with oral cancer and one with maxillary sinus cancer). Fig. 1 shows some cases of foreign body foreign body ingestion.
Fig. 1. A radiograph and endoscopic views of accidental foreign body and ingestion cases. (A) CT image showing a gold crown that was ingested during test placement. (B) Endoscopy images showing a gold inlay in the duodenum that was ingested during test placement. CT, computed tomography.
2. Medical progress
One of the two aspiration cases was that of an 83-year-old woman who aspirated the crown portion of a resected tooth during extraction. She exhibited no major symptoms such as shortness of breath. After a failed attempt to remove the object using bronchoscopy on the same day, it was removed using rigid bronchoscopy under general anesthesia the following day. The other patient was a 77-year-old man who aspirated a fixed dental prosthesis that had been removed for extraction. The aspirated object was removed by bronchoscopy under conscious sedation.
The 37 ingestion cases comprised 16 ingested foreign bodies removed by endoscopy and 21 cases that were followed-up. There were no medical complications such as abdominal pain or gastrointestinal bleeding, with only one case of a minor mucosal scratch that occurred while removing an ingested high-speed bur. All large instruments, such as a lip clip of an electronic apex locator and an implant drill, or sharp instruments, such as a high-speed diamond bur and a suture needle, were removed. The inlays, crowns, and low-speed burs were ingested multiple times, and among these cases, there were cases where the foreign bodies were removed, cases where removal was attempted but failed, and were followed up without attempting removal.
1) Incidence rate by treatment procedure (Table 1)
Table 1. Incidence rate by treatment procedure.
| Treatment procedure | Patient visit | Foreign body ingestion/aspiration | Incidence rate per million |
|---|---|---|---|
| Implant removal | 586 | 1 | 1706.5 |
| Inlay try in | 2691 | 3 | 1114.8 |
| Crown try in | 13716 | 8 | 583.3 |
| Crown and bridge removal | 7114 | 4 | 562.3 |
| Implant impression | 10845 | 5 | 461.0 |
| Implant 1st surgery | 11170 | 4 | 358.1 |
| Implant fixed prosthesis placement | 10837 | 3 | 276.8 |
| Composite resin restoration polishing | 12114 | 3 | 247.6 |
| Temporary crown fabrication | 30351 | 2 | 65.9 |
| Extraction | 109028 | 4 | 36.7 |
| Root canal therapy | 91934 | 1 | 10.9 |
| Scaling | 99059 | 1 | 10.1 |
| Sum | 399445 | 39 | 97.6 |
The total number of patient visit for the treatment procedures in which foreign body aspiration and ingestion occurred was 399,445, and the incidence rate was 97.6/million. The incidence rate was high for implants, inlays, and fixed prostheses.
2) Incidence rate by sex
Overall, 39 cases occurred in 12 women (1 aspiration and 11 ingestion) and 27 men (1 aspiration and 26 ingestion). The incidence rate was 22.7/million in men and 8.1/million in women, with a significant sex difference (P = 0.002).
3) Incidence rate by age (Fig. 2)
Fig. 2. Incidence rate of accidental foreign body aspiration and ingestion by age group. The incidence rate differed significantly between the age groups (P < 0.001). The incidence tended to increase with age, with a particularly marked increase in patients aged 80 years or older.
The incidence rate ranged from 2.7 to 14.4/million among patients younger than 60 years and increased to 22.2 and 32.6/million among those aged 60–69 and 70–79 years, respectively, and markedly to 100.5/million for those aged 80 years or older. The incidence rate differed significantly between the age groups (P < 0.001).
4) Incidence rate by department (Fig. 3)
Fig. 3. Incidence rate of accidental foreign body aspiration and ingestion by department. The incidence rate differed significantly between departments (P < 0.001) and was highest in the Predoctoral Student Clinic, followed by the Department of Prosthodontics.
The incidence rate was highest in the Predoctoral Student Clinic, at 66.7/million, followed by (in decreasing order) the Department of Prosthodontics (44.6/million), Department of Advanced General Dentistry (20.4/million), Department of Conservative Dentistry (15.0/million), Department of Oral and Maxillofacial Surgery (14.8/million), Department of Pediatric Dentistry (5.9/million) and Department of Periodontics (5.5/million). No cases of accidental foreign body aspiration or ingestion were reported in the Department of Orthodontics and Oral Medicine. The incidence rate differed significantly between the departments (P < 0.001).
5) Aspirated and ingested objects
Crowns and bridges were the objects that were most frequently aspirated or ingested during try-in, cementation, or removal of prostheses for extraction. The second most common object was dental implant components. Three cases of swallowing low-speed contra-angle dental burs during composite polishing were reported in the Predoctoral Student Clinic. The other cases included the lip clip of an electronic apex locator during endodontic treatment, suture needle during suturing after extraction, and fractured fragment of an ultrasonic scaler tip during scaling. In the Department of Pediatric Dentistry there were two cases of foreign body swallowing, and in both cases, the teeth were swallowed during tooth extraction.
DISCUSSION
This study analyzed foreign body aspiration and ingestion cases that occurred in one institution over 7 years and showed that there were differences in the incidence rate according to patient sex and age, dental department.
The incidence rate relative to the total number of patient visits may have been underestimated because all visits with no possibility of foreign body aspiration and ingestion were included. In this study, we showed the incidence rate of procedures in which foreign body aspiration and ingestion occurred. The former was 14.6/million and the latter was 97.6/million, which is approximately six times higher. These values should alert dental practitioners.
An interesting finding of this study was that the incidence rate was more than twofold higher in men than in women. Another 7-year-long retrospective study analyzing cases of endoscopic removal of dental foreign bodies in a medical and dental hospital in Japan found a male-to-female ratio of 21:8 [13], which is similar to that in the present study. The anatomy of the larynx and pharynx is known to differ between men and women, with the oropharynx volume being larger in men [14]. In addition to anatomical differences, tongue strength and endurance might also affect the incidence rate, although sex-related differences in these parameters are controversial [15,16].
The higher incidence of accidental foreign body aspiration and ingestion in older people is consistent with the findings of previous studies, which may be explained by the effects of a decreased gag reflex and increased prevalence of various medical conditions [10]. Foreign body aspiration and ingestion have been reported to occur frequently in children and rarely in adults [17,18], which contrasts with the present study that found a low incidence in the Department of Pediatric Dentistry. This might be due to various methods for preventing accidental foreign body aspiration and ingestion being applied more actively in children. In the Department of Pediatric Dentistry of Yonsei University Dental Hospital, rubber dams are strictly used during all possible treatments. There were two cases of foreign body ingestion in the Department of Pediatric Dentistry, both of which occurred during tooth extraction where rubber dam installation was impossible.
It is noteworthy that seven of the 39 patients in this study had impaired cognition or conditions that may have affected swallowing. Patients who undergo excisional surgery for oral and maxillofacial cancer and those with oral and maxillofacial deformities may be at a higher risk of accidental foreign body aspiration and ingestion because their throat is open during dental treatment. Several case reports have described accidental foreign body aspiration and ingestion in patients with Parkinson’s disease, stroke, and psychiatric problems [19,20]. The present retrospective study confirmed that these patients were at high risk. Another article describing the predisposing factors for foreign body ingestion and aspiration also reported that it was more likely to occur in the elderly, patients with mental retardation, psychotic patients, people with severe vomiting reflex, and patients with anxiety [21].
The high incidence rate found in the Predoctoral Student Clinic in this study is consistent with other studies finding that accidental foreign body ingestion occurs more frequently when procedures are performed by unskilled practitioners [22,23]. This may be because unskilled practitioners are more likely to make various mistakes compared to skilled operators. Patient safety events in the Predoctoral Student Clinic were monitored through a quality assurance program, and student education was provided frequently to prevent recurrence. In case of treatment with a high possibility of foreign body ingestion and aspiration, such as inlay placement, clinical instructors instructed students to apply the method for preventing foreign body aspiration.
If object loss is identified in the oral cavity and the object is not found in the treatment field, the presence of the foreign body within the respiratory or digestive tract can be confirmed using radiography, laryngoscopy, or bronchoscopy because there might be no symptoms even if the foreign body is aspirated [24]. Urgent endoscopic intervention may be required, depending on the type and location of the foreign body in cases of ingestion. Sharp ingested foreign bodies are much more likely to cause complications; therefore, they must be removed [18]. A case report found that a dental implant screwdriver which was swallowed had remained in the intestine for more than 7 days; therefore, colonoscopy under general anesthesia was needed to remove it [25]. Ingested foreign bodies for which the decision is made not to remove them must be followed up until they are excreted.
It is crucial to apply interventions aimed at preventing aspiration and ingestion of foreign bodies. First, dental practitioners should identify high-risk patients. Patients aged ≥ 80 years are considered to be at very high risk. Patients with conditions that cause muscle weakness, decreased reflexes, and cognitive impairment, which can affect swallowing, are also at high risk. All possible preventive measures should be actively implemented in high-risk patients.
A rubber dam is the most obvious preventive measure, and a dam that completely covers the oral cavity should be used whenever possible. Alternatives may be used in situations where a rubber dam is unsuitable. It is advisable to wear tight gloves and not to recline the chair too much (i.e., only in the semi-supine position) when handling small objects within the oral cavity or when extracting deciduous teeth. It might be prudent to use floss to secure objects, such as rubber dam clamps, bridge restorations, dental implant screwdrivers, and endodontic files. Placing a gauze screen in front of the throat is also recommended. However, because such gauze can be swallowed, the use of 4 × 4 gauze with a radiopaque thread that can be seen in the case of swallowing is recommended over a 2 × 2 size.
Checking if dental burs are properly installed is useful for preventing them from dropping into the oral cavity. When a dental bur is mounted on a handpiece, it should be pushed all the way in and then pulled back to ensure that it does not come out. Activating a handpiece before using it in oral cavity will confirm whether the bur is installed properly and does not detach from the handpiece. Most dental burs are sharp and dangerous and can puncture the digestive tract, if ingested.
The case of a fractured scaler tip fragment being swallowed indicates that dental practitioners should be aware that instruments with thin tips may fracture. Care should therefore be taken to ensure that the instrument does not fracture within the oral cavity by ensuring the use of correct instrumentation and avoiding excessive force. Dentists should check the connections of the instruments with detachable parts, such as dental mirrors. The use of a swaged needle is recommended to prevent needle ingestion.
In conclusion, the incidence rate of accidental foreign body aspiration and ingestion was significantly higher in patients aged 80 years or older and in the Predoctoral Student Clinic and the Department of Prosthodontics. Dental practitioners should identify high-risk patients and apply various methods to prevent foreign body aspiration and ingestion. Inexperienced practitioners should understand actual cases and be more careful.
Footnotes
- Jisun Huh: Conceptualization, Data curation, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing.
- Namkwon Lee: Formal analysis, Investigation, Validation, Writing – review & editing.
- Ki-Yeol Kim: Formal analysis, Writing – review & editing.
- Seoyeon Jung: Data curation, Writing – review & editing.
- Jungyul Cha: Conceptualization, Writing – review & editing.
- Kee-Deog Kim: Conceptualization, Writing – review & editing.
- Wonse Park: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing.
CONFLICT OF INTERESTS: The authors declare that they have no conflict of interests.
FUNDING: This work was not supported by any grant.
References
- 1.Yamalik N, Pérez BP. Patient safety and dentistry: what do we need to know? Fundamentals of patient safety, the safety culture and implementation of patient safety measures in dental practice. Int Dent J. 2012;62:189–196. doi: 10.1111/j.1875-595X.2012.00119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thusu S, Panesar S, Bedi R. Patient safety in dentistry–state of play as revealed by a national database of errors. Br Dent J. 2012;213:E3. doi: 10.1038/sj.bdj.2012.669. [DOI] [PubMed] [Google Scholar]
- 3.Ensaldo-Carrasco E, Suarez-Ortegon MF, Carson-Stevens A, Cresswell K, Bedi R, Sheikh A. Patient safety incidents and adverse events in ambulatory dental care: a systematic scoping review. J Patient Saf. 2021;17:381–391. doi: 10.1097/PTS.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 4.Walji MF, Yansane A, Hebballi NB, Ibarra-Noriega AM, Kookal KK, Tungare S, et al. Finding dental harm to patients through electronic health record-based triggers. JDR Clin Trans Res. 2020;5:271–277. doi: 10.1177/2380084419892550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill EE, Rubel B. A practical review of prevention and management of ingested/aspirated dental items. Gen Dent. 2008;56:691–694. [PubMed] [Google Scholar]
- 6.Kim E, Noh W, Panchal N. Mortality from an aspiration of dental crown during extraction. Gerodontology. 2017;34:498–500. doi: 10.1111/ger.12288. [DOI] [PubMed] [Google Scholar]
- 7.Abusamaan M, Giannobile WV, Jhawar P, Gunaratnam NT. Swallowed and aspirated dental prostheses and instruments in clinical dental practice: a report of five cases and a proposed management algorithm. J Am Dent Assoc. 2014;145:459–463. doi: 10.14219/jada.2013.55. [DOI] [PubMed] [Google Scholar]
- 8.Milton TM, Hearing SD, Ireland AJ. Ingested foreign bodies associated with orthodontic treatment: report of three cases and review of ingestion/aspiration incident management. Br Dent J. 2001;190:592–596. doi: 10.1038/sj.bdj.4801046. [DOI] [PubMed] [Google Scholar]
- 9.Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40:585–589. doi: 10.1111/j.1365-2591.2007.01249.x. [DOI] [PubMed] [Google Scholar]
- 10.Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: a review. J Am Dent Assoc. 1996;127:1224–1229. doi: 10.14219/jada.archive.1996.0415. [DOI] [PubMed] [Google Scholar]
- 11.Cossellu G, Farronato G, Carrassi A, Angiero F. Accidental aspiration of foreign bodies in dental practice: clinical management and prevention. Gerodontology. 2015;32:229–233. doi: 10.1111/ger.12068. [DOI] [PubMed] [Google Scholar]
- 12.Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: a 10-year institutional review. J Am Dent Assoc. 2004;135:1287–1291. doi: 10.14219/jada.archive.2004.0404. [DOI] [PubMed] [Google Scholar]
- 13.Mizuno KI, Takahashi K, Tominaga K, Nishigaki Y, Sato H, Ikarashi S, et al. Endoscopic removal of ingested dentures and dental instruments: a retrospective analysis. Gastroenterol Res Pract. 2016;2016:1–5. doi: 10.1155/2016/3537147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inamoto Y, Saitoh E, Okada S, Kagaya H, Shibata S, Baba M, et al. Anatomy of the larynx and pharynx: effects of age, gender and height revealed by multidetector computed tomography. J Oral Rehabil. 2015;42:670–677. doi: 10.1111/joor.12298. [DOI] [PubMed] [Google Scholar]
- 15.Vanderwegen J, Guns C, Van Nuffelen G, Elen R, De Bodt M. The influence of age, sex, bulb position, visual feedback, and the order of testing on maximum anterior and posterior tongue strength and endurance in healthy Belgian adults. Dysphagia. 2013;28:159–166. doi: 10.1007/s00455-012-9425-x. [DOI] [PubMed] [Google Scholar]
- 16.Youmans SR, Youmans GL, Stierwalt JA. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24:57–65. doi: 10.1007/s00455-008-9171-2. [DOI] [PubMed] [Google Scholar]
- 17.Boyd M, Chatterjee A, Chiles C, Chin R., Jr Tracheobronchial foreign body aspiration in adults. South Med J. 2009;102:171–174. doi: 10.1097/SMJ.0b013e318193c9c8. [DOI] [PubMed] [Google Scholar]
- 18.Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802–806. doi: 10.1016/s0016-5107(02)70407-0. [DOI] [PubMed] [Google Scholar]
- 19.Deliberador TM, Marengo G, Scaratti R, Giovanini AF, Zielak JC, Baratto Filho F. Accidental aspiration in a patient with Parkinson's disease during implant-supported prosthesis construction: a case report. Spec Care Dentist. 2011;31:156–161. doi: 10.1111/j.1754-4505.2011.00202.x. [DOI] [PubMed] [Google Scholar]
- 20.Worthington P. Ingested foreign body associated with oral implant treatment: report of a case. Int J Oral Maxillofac Implants. 1996;11:679–681. [PubMed] [Google Scholar]
- 21.Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:657–660. doi: 10.1016/s1079-2104(99)70004-1. [DOI] [PubMed] [Google Scholar]
- 22.Hisanaga R, Hagita K, Nojima K, Katakura A, Morinaga K, Ichinohe T, et al. Survey of accidental ingestion and aspiration at Tokyo Dental College Chiba Hospital. Bull Tokyo Dent Coll. 2010;51:95–101. doi: 10.2209/tdcpublication.51.95. [DOI] [PubMed] [Google Scholar]
- 23.Obinata K, Satoh T, Towfik AM, Nakamura M. An investigation of accidental ingestion during dental procedures. J Oral Sci. 2011;53:495–500. doi: 10.2334/josnusd.53.495. [DOI] [PubMed] [Google Scholar]
- 24.Foltran F, Ballali S, Passali FM, Kern E, Morra B, Passali GC, et al. Foreign bodies in the airways: a meta-analysis of published papers. Int J Pediatr Otorhinolaryngol. 2012;76:S12–S19. doi: 10.1016/j.ijporl.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Santos Tde S, Antunes AA, Vajgel A, Cavalcanti TB, Nogueira LR, Laureano Filho JR. Foreign body ingestion during dental implant procedures. J Craniofac Surg. 2012;23:e119–e123. doi: 10.1097/SCS.0b013e31824cda32. [DOI] [PubMed] [Google Scholar]