Abstract
Introduction
Lipomas are one of the most common benign tumors, but deep tissue and huge lipomas are rare.
Presentation of case
A 59-year-old middle-aged woman was admitted to hospital for right hip mass resection because of numbness and pain in her right lower limb for 6 months. Ultrasound and nuclear magnetic resonance imaging (MRI) showed irregular mass. On the assumption of malignancy, the patient underwent a right hip mass resection and returned to normal with no short-term or long-term response. HE (hematoxylin-eosin) staining of the tumor showed the characteristics of a benign tumor.
Discussion
The pathogenesis of myolipoma is not clear, and it may be related to brown adipose tissue. When lipoma is huge, it needs interventional treatment. Complete encapsulated myolipoma can usually be completely removed, with low recurrence possibility and good prognosis.
Conclusion
Giant intramuscular lipoma of hip and its clinical manifestations are relatively rare. And the results of ultrasound imaging are similar to those of the surrounding normal adipose tissue. No significant difference was observed by naked eye. In particular, postoperative pathological examination is needed to make a definite diagnosis and differential diagnosis. Clinically, surgical treatment is often used, and the prognosis is good, but recurrence is possible. The following report discusses the experience of one of our patients, with literature review.
Keywords: Gluteal giant intramuscular lipoma, Surgical treatment, Case report
Highlights
-
•
Compared with other lipomas on the body surface, our reported lipomas in the deep tissues are very rare.
-
•
Lipomas are a common benign tumor, but huge lipomas are rare and may be malignant.
-
•
After the operation, the lipoma was removed and the symptoms of nerve compression of the patient were obviously relieved.
1. Introduction
Lipoma is one of the most common soft tissue benign tumors in adults, and it is also one of the most common benign mesenchymal tumors in the body. Only 1% of soft tissue masses are malignant [1]. Lipomas can be found in almost all organs in the body and account for (5%) of soft tissue tumors, infiltrating lipomas (including inter- and intramuscular lipomas, with an estimated incidence of 1.8 and 0.3%, respectively [2]), which is why lipomas are also called ubiquitous tumors or generalized tumors [3], [4]. Lipoma is the most common soft tissue tumor in adults. The peak incidence is between 40 and 60 years old, and it rarely happens in children [5]. Benign lipoma is usually isolated, soft to touch, with some activity and no obvious pain. Usually, small lipomas are asymptomatic and easily overlooked. These tumors do not require special treatment. If it has symptoms or discomfort, you should have surgery to remove them in time [6], [7]. This small and superficial lipoma is easy and common to resect, but some huge and deep lipomas bring great difficulties for diagnosis and surgical treatment, especially those closely related to important tissues of the body. Sanchez et al. defined giant lipoma as a lesion that measures at least 10 cm in one dimension or weighs a minimum of 1000 g [8]. Other manifestations caused by lipomas usually depend on the location and size of the lesion and the squeezing of the surrounding local tissues [9].
In this article, we reported a rare giant lipoma. Our patient's condition was diagnosed, and the tumor was surgically removed, and pathological analysis of the excised specimen provided a basis for clinical treatment of similar diseases. This case report conforms to the SCARE guidelines and has been reported according to the SCARE checklist [10].
2. Presentation of case
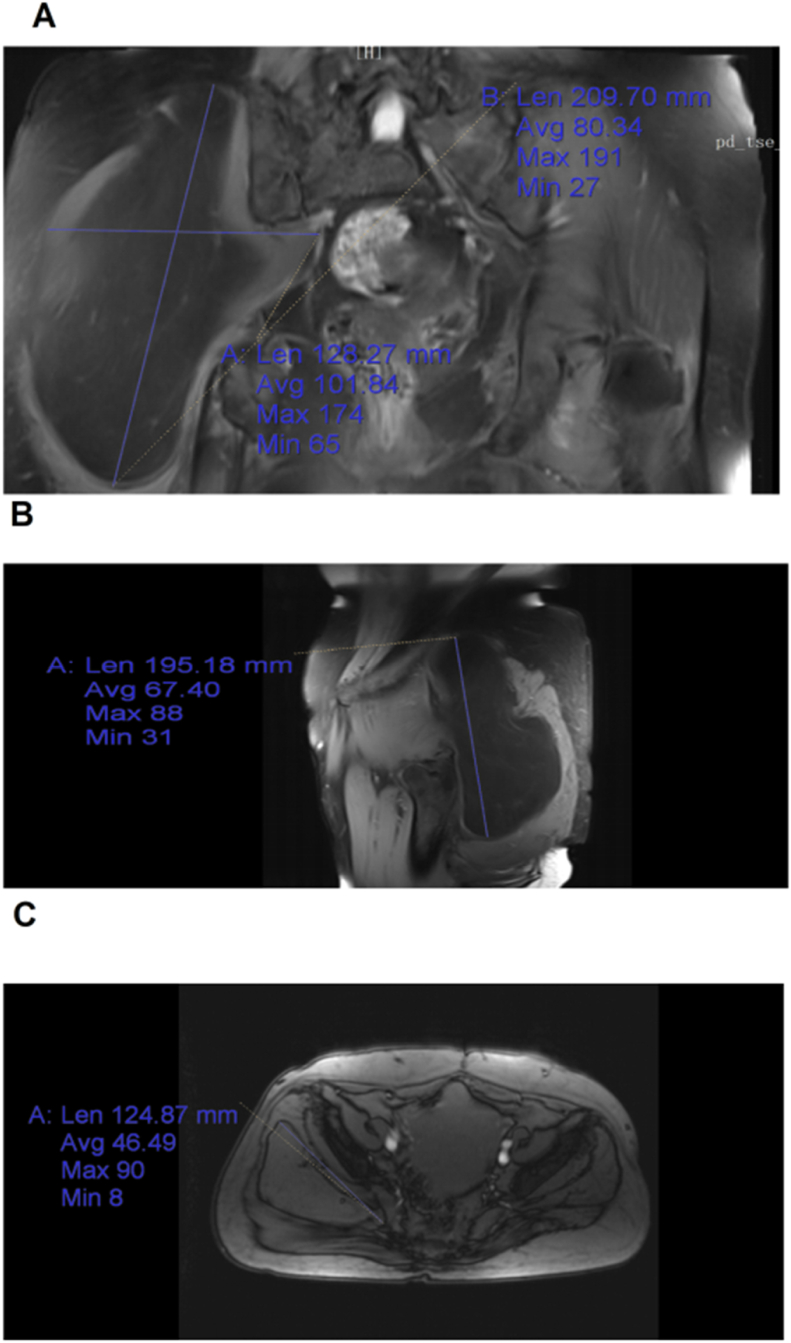
A 59-year-old Chinese woman, who was previously healthy, was admitted to the Department of Orthopaedics, Affiliated Hospital of Changchun University of Traditional Chinese Medicine, because of “right hip mass and right lower limb tingling for 6 months” and no obvious family or social history. Physical examination showed that the right buttock was swollen, the palpable size was 20 ∗ 13 cm, and the skin color and skin temperature were normal. The boundary is clear, there was no tenderness. The right lower limb of Lasegue sign is positive, the right lower limb was slightly numb and the blood supply was good. Auxiliary examination: MRI examination of sacrococcygeal bone revealed that a slightly shorter T2 signal of quasi-circular isometric T1 could be seen in the right gluteal muscle, and the boundary was clear, with the range of about 10.9 cm ∗ 9.6 cm ∗ 19 cm as shown in Fig. 1. Ultrasound of the right hip joint showed that the muscle layer of the right hip joint had a heterogeneous echoes of about 15.3 cm ∗ 5.8 cm ∗ 20 cm. CDFI showed that there was no obvious blood flow signal except lipoma. Preoperative examination ruled out the contraindications, and the operation time was determined according to preoperative discussion, ultrasound and MRI results.
Fig. 1.
A: Morphology of coronary mass on MRI; B: morphology of sagittal mass on MRI; C: morphology of transverse position mass on MRI.
The patient was sent to the operating room. The operation was performed by two senior deputy chief orthopedic surgeons under the supervision of one chief orthopedic surgeon. After the general anesthesia takes effect, the patient took the prone position, the operating area is routinely disinfected and towel are laid. An oblique anterograde incision was made along the gluteal muscle in the posterolateral aspect of the right buttock. The incision was about 13 cm long, and cuts through the skin, subcutaneous tissue and deep fascia (Fig. 2A). The gluteal muscle fibers were separated to expose the mass. It can be seen by naked eyes that the substance is a fat mass (Fig. 2B) with thin envelope. Through exploration, the edge of the fat mass reached the lower edge of posterior superior iliac spine, reaches the sacroiliac joint by internal measurement, reaches the femoral trochanter by external measurement, and reaches 2 cm below the lesser trochanter by internal measurement. The lump was carefully separated from the surrounding soft tissues. The lump was completely removed (Fig. 2C), no residue was detected, the bleeding stopped completely, the incision was flushed, and the negative pressure drainage was kept. After the instruments and gauze were checked, the incision was sutured layer by layer (Fig. 2D) and the wound was wrapped with sterile dressing. The operation was completed, very smoothly, with a little bleeding during the operation. The infusion volume was 700 ml, and the urine volume is 200. After the operation, the patient woke up and returned to the ward. The resected mass is sent for pathological examination after being confirmed by the patient and his/her family members.
Fig. 2.
A: Incision of the skin, subcutaneous tissue and deep fascia; B: the mass is exposed and visible as a mass of fat with the naked eye; C: the mass is completely taken out; D: suture the incision.
It took 50 min for the operation. During the operation, it was found that the mass was huge, leaving a huge cavity after being taken out, which was easy to form hematoma and infection. The solution was to stop bleeding thoroughly, suture layer by layer, actively avoid the formation of hollow tissue, and drain the blood under negative pressure to avoid the formation of hematoma.
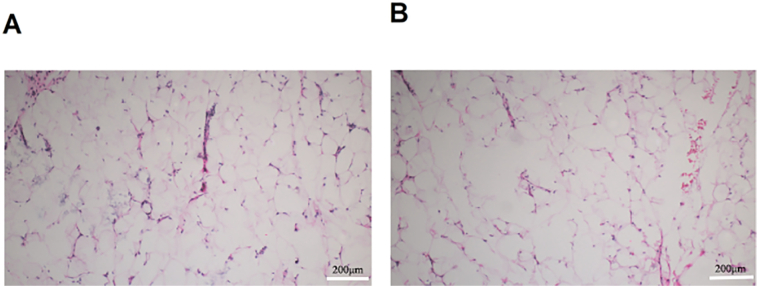
The examination of the resected specimen of the right hip joint tumors showed that: A yellow lump, 19 ∗ 18 ∗ 4.5 cm in size, complete capsule, solid section, yellowish color and soft texture. Microscopically, the tumor was composed of a large number of differentiated and mature adipocytes and a small number of fibroblasts (Fig. 3). Pathological diagnosis: Lipoma. Normal section staining showed differentiated and mature adipose tissue, and the pathological diagnosis was definite, so it was unnecessary to further detect diagnostic pathological markers such as immunohistochemistry.
Fig. 3.
Hematoxylin-eosin staining showed a large number of mature adipocytes and a small number of fibroblasts. Scale bar = 200 μm.
The incision healed well after operation, and there was no obvious infection and exudation. After the anesthesia completely disappeared, the patient was awake, the numbness of the right lower limb was relieved, and the patient's condition in the ward was stable. Subsequently, she was discharged from hospital on the seventh day, with normal blood and physical examinations, normal diet and defecation. During the follow-up, her clinical process remained calm, with no signs of recurrence. Half a month after the operation to determine whether the incision healing, monthly telephone follow-up for pain and discomfort, nerve compression symptoms, etc. Every six months to check the color ultrasound and MRI to see whether the recurrence, three years after the annual review of imaging examination.
3. Discussion
Lipomas is a benign tumor, originated from germ cell layer of the mesoderm, and is mainly composed of mature adipose tissues. They are mainly found in superficial parts of the body, but lipoma in deep tissues is rare. According to the WHO Classification of Soft Tissue and Bone (fourth edition, 2013) [11], lipomas can be divided into superficial lipoma, deep lipoma, intramuscular or intramuscular lipoma and osteolipoma. Myolipoma is caused by infiltration of undifferentiated fully mature fat cells between the muscle bundles and the muscle cells. The tumor grows slowly and is limited. The tumor growth is slow and limited. In the early stage, the tumor is small, and there may be no symptoms. However, with the gradual enlargement of the tumor, it can oppress the important nerves, blood vessels and lymph around it, resulting in abnormal sensation, swelling and even limited movement, especially when the limbs move more or stand for too long. Myolipoma is a common clinical disease, which mostly occurs in the larger muscle of the limbs, especially the lower limb muscles. More common in the middle-aged and elderly people, and more common in males. There are also similar literature reports on myolipoma in China. The pathogenesis is still unclear, and it may be related to brown adipose tissue [12]. In addition, the relationship between lipoma and heredity has been confirmed, and some studies have shown that lipoma shows genetic abnormalities, in which the HMGA 2 gene (located at 12 q 14.3) is involved in the pathogenesis of tumor [13].
Proper imaging studies is very important for definite diagnosis and treatment. Ultrasound has become the preferred imaging modality for lipoma due to its advantages of low cost, non-invasiveness and convenience [14]. Its basic performance is regular, mostly oval, with uniform echo and clear boundary, and there was usually no blood flow or a small amount of blood flow could be detected inside. The echo of intramuscular lipoma is determined by the homogeneity of the mixture of adipose tissue and other tissues within the mass, and homogeneity determines the number and size of the interfaces. Color Doppler ultrasound of myolipoma is characterized by insufficient blood flow [15]. Ultrasonic examination can provide the characteristic basis for the diagnosis of myolipoma, which is of great significance for the rational selection of surgical methods [16]. CT and MRI can be used to assist in the diagnosis of complex or difficult lipomas. The main CT findings are typical fat density. The density in the mass was relatively uniform, with clear boundaries and capsules. The scan showed no enhancement. MRI can easily determine the nature of the mass according to different signal intensities, and the signals are characteristic, usually short T1 long T2 signals with clear boundaries [17].
Interventional therapy can be omitted if the lipoma has no symptoms of compression due to excessive volume or special anatomical position. Interventional treatment is needed for huge lipomas that compresses adjacent important organs, tissues, blood vessels and nerves, especially for lipoma with pain during compression. Lower limb numbness is mainly due to ischemia or neurological problems, such as sciatic nerve compression. In this case, due to the huge size of lipoma, it compresses the sciatic nerve, resulting in numbness and pain in the right lower limb. After the operation, the lipoma is removed to relieve the symptoms of nerve compression and numbness pain. The treatment methods include injecting sodium deoxycholate into the lesion [18], injecting steroids and isoproterenol together into the lesion [19], liposuction [20] and surgical resection, of which surgical resection is still the most effective treatment. At present, the main treatment of myolipoma is surgical resection. Complete encapsulated myolipoma can usually be completely removed, with low recurrence possibility and good prognosis. During the operation, the scope of resection should be appropriately expanded to minimize the injury of muscle attachments. The local recurrence rate is about 19% [21]. This is because the disease can't be completely resected, so it is easy to recur. Like the primary tumor, the recurrent tumor tissue is well differentiated and can be treated by surgery again. Multiple recurrences requiring multiple surgical resection. Radiation treatment can also be used for local recurrence.
To sum up, giant myolipoma is relatively rare, and it is difficult to find it because of its deep location and younger age. It is only easy to find out the corresponding clinical symptoms when it is large or because of the compression of important surrounding tissues. At the same time, surgery is needed. The final diagnosis of lipoma relies on the pathological diagnosis. Although the diagnosis cannot be confirmed through imaging examinations such as ultrasound and MRI, it also has good reference value in the preoperative diagnosis.
4. Conclusion
A key point of this case debate is that giant lipomas in deep tissues is relatively rare, so the diagnosis, treatment and prognosis of this case are very important. The diagnosis of lipoma needs the support of ultrasonic imaging and diagnosis. Giant lipomas is usually treated by surgery, and the nature of the lump is determined by pathological analysis after operation.
In this case, the ultrasonographic and imaging findings are similar to those of surrounding normal adipose tissue. There was no obvious difference by naked eye. Therefore, after the diagnosis and differential diagnosis were confirmed by postoperative pathological examination, surgical treatment was adopted. The prognosis of this case is good, but recurrence is not excluded.
Provenance and peer review
We're not commissioned; the paper was externally peer reviewed.
Data availability statement
Raw data were generated at Affiliated Hospital of Changchun University of Chinese Medicine, Jilin China. Derived data supporting the findings of this study are available from the corresponding author on request.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
All procedures were performed in accordance with the guidelines of the Medical Ethics Committee of Affiliated Hospital of Changchun University of Chinese Medicine (No. CCZYFYLL2020,016-01).
Funding
This work was supported by the Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (No: ZYYCXTD-D-202001), the TCM Clinical Research Center for Bone diseases of Jilin Province (No. 20180623048TC), the Evidence-based capacity-building project for traditional Chinese medicine (No. 2019XZZX-GK005).
Guarantor
Dr. Xiangyang Leng.
Research registration number
N/A.
CRediT authorship contribution statement
Dr. Yuyan Jia: writing original draft, editing,
Dr. Jianyu Wang: Patient care, data collection and writing of original draft.
Dr. Wei Deng: Patient care, Perform the operation.
Dr. Sharol Ngwenya: Perform the operation.
Professor Xiangyang Leng: Getting ethics approval and patient consent. Approval of the final manuscript.
Professor Haisi Dong: Review, editing and approval of the final manuscript.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
Contributor Information
Haisi Dong, Email: adonghaisi@163.com.
Xiangyang Leng, Email: lengxiangy@163.com.
References
- 1.Johnson C.N., Ha A.S., Chen E., Davidson D. Lipomatous soft-tissue tumors. J.Am.Acad.Orthop.Surg. 2018;26(22):779–788. doi: 10.5435/JAAOS-D-17-00045. [DOI] [PubMed] [Google Scholar]
- 2.Liu D.R., Li C., Chen L. Management of giant intermuscular lipoma of hips: a case report and review of literature. Mol.Clin.Oncol. 2013;1(2):369–372. doi: 10.3892/mco.2013.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis C., Jr., Gruhn J.G., Jr. Giant lipoma of the thigh. Arch. Surg. (Chicago, Ill.: 1960) 1967;95(1):151–156. doi: 10.1001/archsurg.1967.01330130153030. [DOI] [PubMed] [Google Scholar]
- 4.Singh M., Saxena A., Kumar L., Karande S.K., Kolhe Y. Giant lipoma of posterior cervical region. Case Rep.Surg. 2014;2014 doi: 10.1155/2014/289383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jo V.Y., Fletcher C.D. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46(2):95–104. doi: 10.1097/PAT.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 6.Reddy O.J., Gafoor J.A., Suresh B., Prasad P.O. Lipoma in liver: a rare presentation. J.Dr. NTR Univ.Health Sci. 2015;4(3):185. https://www.jdrntruhs.org/text.asp?2015/4/3/185/165398 https://www.jdrntruhs.org/text.asp?2015/4/3/185/165398. [Google Scholar]
- 7.Özer M., Ulusoy S., Parlak Ö. A rare location: a giant mesenteric lipoma. Med.J.Islam.World Acad.Sci. 2016;24(1):24–26. [Google Scholar]
- 8.Sanchez M.R., Golomb F.M., Moy J.A., Potozkin J.R. Giant lipoma: case report and review of the literature. J. Am. Acad. Dermatol. 1993;28(2 Pt 1):266–268. doi: 10.1016/s0190-9622(08)81151-6. [DOI] [PubMed] [Google Scholar]
- 9.Hussain A., Mahmood H. Ulcerated giant lipoma of the right thigh. Internet J.Surg. 2007;11(1) [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. (London, England) 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg A.E. WHO classification of soft tissue and bone, fourth edition: summary and commentary. Curr. Opin. Oncol. 2013;25(5):571–573. doi: 10.1097/01.cco.0000432522.16734.2d. [DOI] [PubMed] [Google Scholar]
- 12.Enzi G., Busetto L., Sergi G., Coin A., Inelmen E.M., Vindigni V., Bassetto F., Cinti S. Multiple symmetric lipomatosis: a rare disease and its possible links to brown adipose tissue. Nutr. Metab. Cardiovasc. Dis. 2015;25(4):347–353. doi: 10.1016/j.numecd.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Lacaria M., El Demellawy D., McGowan-Jordan J. A rare case of pediatric lipoma with t(9;12) (p22;q14) and evidence of HMGA2-NFIB gene fusion. Cancer Genet. 2017;216–217:100–104. doi: 10.1016/j.cancergen.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 14.Onesti M.G., Maruccia M., Malpassini F., Olive M., Medevedeyeva E., Guerrisi I., Di Segni M., Maldur V., Dessy L.A. A case of subfascial lipoma in the lateral space of neck: US and CT findings. J.Ultrasound. 2009;12(4):160–162. doi: 10.1016/j.jus.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiping Yan, Zhiping Wang, Xin Sun. Two-dimensional and color Doppler ultrasonography of intramuscular lipoma. Chin. J. Med. Clin. Med. 2004;4(12):950–951. [Google Scholar]
- 16.Nishida J., Morita T., Ogose A., Okada K., Kakizaki H., Tajino T., Hatori M., Orui H., Ehara S., Satoh T., Shimamura T. Imaging characteristics of deep-seated lipomatous tumors: intramuscular lipoma, intermuscular lipoma, and lipoma-like liposarcoma. J.Orthop.Sci. 2007;12(6):533–541. doi: 10.1007/s00776-007-1177-3. [DOI] [PubMed] [Google Scholar]
- 17.Yumin Li, Yan Li, Xianghua Liu, et al. <sb:contribution><sb:title>Chin. J. Integr. Tradit. West. Med.</sb:title> </sb:contribution><sb:host><sb:issue><sb:series><sb:title>Imaging</sb:title></sb:series></sb:issue></sb:host>. 2016;14(6):695–697. [Google Scholar]
- 18.Rotunda A.M., Ablon G., Kolodney M.S. Lipomas treated with subcutaneous deoxycholate injections. J. Am. Acad. Dermatol. 2005;53(6):973–978. doi: 10.1016/j.jaad.2005.07.068. [DOI] [PubMed] [Google Scholar]
- 19.Redman L.M., Moro C., Dobak J., Yu Y., Guillot T.S., Greenway F.L. Association of β-2 adrenergic agonist and corticosteroid injection in the treatment of lipomas. Diabetes Obes. Metab. 2011;13(6):517–522. doi: 10.1111/j.1463-1326.2011.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bassetto F., Scarpa C., De Stefano F., Busetto L. Surgical treatment of multiple symmetric lipomatosis with ultrasound-assisted liposuction. Ann. Plast. Surg. 2014;73(5):559–562. doi: 10.1097/SAP.0b013e31827f5295. [DOI] [PubMed] [Google Scholar]
- 21.Guotai Xu. Invasive lipoma. Chin.J.Gen.Surg. 1998;7(4):213–215. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data were generated at Affiliated Hospital of Changchun University of Chinese Medicine, Jilin China. Derived data supporting the findings of this study are available from the corresponding author on request.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.