Significance
Although family planning services are crucial for global health and achievement of the Sustainable Development Goals, their funding remains controversial. We document the health consequences of the “Mexico City Policy” (MCP), which restricts US funding for abortion-related activities worldwide. Since its enactment in 1985, the MCP has been enforced only under Republican administrations and quickly rescinded when a Democrat wins the presidency. Our analysis shows that the MCP makes it harder for women to get information on and support for reproductive health and is associated with higher maternal and child mortality rates and HIV rates worldwide. We estimate that reinstating the MCP between 2017 and 2021 resulted in approximately 108,000 maternal and child deaths and 360,000 new HIV infections.
Keywords: Mexico City Policy, maternal health, children’s health, family planning
Abstract
This paper analyzes the link between foreign aid for family planning services and a broad set of health outcomes. More specifically, it documents the harmful effects of the so-called “Mexico City Policy” (MCP), which restricts US funding for nongovernmental organizations that provide abortion-related services abroad. First enacted in 1985, the MCP is implemented along partisan lines; it is enforced only when a Republican administration is in office and quickly rescinded when a Democrat wins the presidency. Although previous research has shown that MCP causes significant disruption to family planning programs worldwide, its consequences for health outcomes, such as mortality and HIV rates, remain underexplored. The independence of the MCP’s implementation from the situation in recipient countries allows us to systematically study its impact. Using country-level data from 134 countries between 1990 and 2015, we first show that the MCP is associated with higher maternal and child mortality and HIV incidence rates. These effects are magnified by dependence on US aid while mitigated by funds from non-US donors. Next, we complement these results using individual-level data from 30 low- and middle-income countries and show that, under the MCP, women have less access to modern contraception and are less exposed to information on family planning and AIDS via in-person channels. Moreover, pregnant women are more likely to report that their pregnancy is not desired. Our findings highlight the importance of mitigating the harmful effects of MCP by redesigning or counteracting this policy.
Family planning services bring immense benefits to societies by saving lives and promoting Sustainable Development Goals (SDGs). Family planning can lower maternal and child mortality, which continues to take millions of lives every year and remains among the most urgent global public health problems (1). Additionally, family planning services can help women invest in their careers and gain economic power (2, 3). For these reasons, family planning and reproductive health services directly contribute to the global development agenda and are crucial elements for the achievement of the SDGs, particularly SDG3 (“ensuring healthy lives”) and SDG5 (“achieving gender equality”). Despite these benefits, funding for family planning services can be controversial and subject to partisan politics in aid donor countries.
In this paper, we study the effects of the “Mexico City Policy” (MCP), a cornerstone of US foreign aid policy since its inception in 1985. The main goal of MCP is to prevent US taxpayer contributions from being used to fund abortions in other countries by restricting US federal disbursements for nongovernmental organizations (NGOs) that provide information on or access to abortion around the world. Importantly, MCP is enforced and rescinded along partisan lines. It is one of the first policies implemented (Reagan, Bush 43, and Trump) or continued (Bush 41) by every Republican president and lifted by every Democratic president (Clinton, Obama, and Biden), usually in the first week of a new administration (4). In other words, the MCP’s implementation is due to the outcome of US presidential elections and is exogenous to the situation in aid recipient countries. Over the years, the scope of the MCP has broadened; under Reagan and Bush 41, it applied only to funding given by the US Agency for International Development (USAID), while under Bush (43) and Trump, the aims of the policy were expanded to include funding given by the Department of State and by the vast majority of US bilateral global health assistance, respectively (5).
Since the United States has long been a leader in international population assistance, including family planning and reproductive health programs, the MCP causes a significant disruption in global health systems (6). Many NGOs affected by the MCP are important providers of family planning programs and modern contraceptive methods (7). While NGOs that reject the policy lose US funding and often have to terminate or scale down their programs, even NGOs that sign the policy may become unwilling to provide many sexual and reproductive health services for fear of breaching the policy (what is known as a “chilling effect”) (8, 9). As a result, the MCP is associated with reduced resources and health service provision in many countries.
What are the health consequences of the MCP and the resulting disruption in family planning services for populations around the world? Although researchers and activists predict that health system disruptions should be associated with worse health outcomes (10), we have very little systematic and cross-country analysis of the magnitude of the MCP’s effects and the contextual factors that amplify or mitigate them (6). Several important studies have analyzed abortion rates under the MCP and found that ironically, when the MCP is in place, the numbers of pregnancies and abortions increase (4, 11, 12). In our macrolevel analysis, we develop this literature further by looking at a broader set of global health issues and using multiple datasets.
We expect the MCP to be associated with higher maternal mortality, child mortality, and HIV incidence rates based on qualitative and single-country evidence showing that a reduction in family planning services means less information on and access to modern contraceptives, more unwanted pregnancies, lower quality of care for women and children, and fewer HIV clinics that provide testing and prevention services (a recent review is in ref. 6). More unwanted pregnancies and lower-quality care are likely to result in higher maternal and child mortality. Reduced access to modern contraceptives and fewer HIV clinics are likely to result in more HIV infections. Furthermore, we expect these associations to be stronger in countries more dependent on US aid for family planning services. The results of our analysis (based on a sample of 134 countries between 1990 and 2015) confirm that the MCP is associated with higher maternal and child mortality and higher HIV incidence rates. Consistent with theory, the effects are magnified by US aid and mitigated by aid from non-US donors whose support is unaffected by the MCP. For countries highly dependent on US funding, we estimate that the effects imply between 1 and 4% increases in maternal and child mortality and HIV incidence rates, making them comparable with the effect of an ongoing civil conflict in a country. In absolute numbers, our estimates imply that reinstating the MCP between 2017 and 2021 increased the number of maternal and child deaths by about 27,000 per year and a total of 108,000 over the 4-y term. In addition, we estimate that an additional 90,000 new HIV infections per year took place while the MCP was in effect.
We complement these cross-country regressions with individual-level analysis on how disruptions in family planning services directly affect program recipients. Our microlevel analysis is based on 30 low- and middle-income countries (LMICs) covering more than 30 y and five US presidents. One candidate explanation for the associations between the MCP and mortality is that the MCP causes more unwanted pregnancies, which may lead to more induced abortions (including under unsafe circumstances) or may cause women to carry unwanted pregnancies to term, which may lead to worse outcomes as well. This may happen because the MCP forces organizations to close clinics and scale down programs, which restrict people’s access to in-person family planning services and AIDS-related information. Such programs are usually implemented through two different channels: via mass media and through in-person services and community-based provision. Although mass media campaigns are cheaper than face-to-face interventions and can reach a large audience, their effectiveness is determined by the reach of the media and audience characteristics, such as its socioeconomic (SES) background (13). In contrast, face-to-face interventions are more expensive but also particularly effective in serving women in underresourced communities, as evidence from Bangladesh, Bolivia, Ethiopia, Guatemala, Madagascar, Peru, and Uganda consistently shows (14, 15). In short, we expect MCP-related disruptions to restrict people’s in-person access to family planning services and AIDS-related information, which are more effective than mass media campaigns. Consequently, we also expect the MCP to negatively impact modern contraception use and lower the quality of care for pregnant women and small children. Our microlevel results confirm these expectations. Indeed, the MCP is associated with women having significantly less direct access to in-person family planning programs and in-person AIDS-related information. Furthermore, when MCP is in place, women are less likely to declare to be using modern contraceptive methods and more likely to claim that they are using folkloristic or traditional practices. Unsurprisingly, under the MCP, pregnant women are more likely to report that their pregnancy is not desired. Lastly, we show that under the MCP, newborns are less likely to be tested for HIV as a part of the antenatal care, and their mothers are less likely to receive health support from professional health staff after delivery. We conclude that by restricting access to family planning programs, the MCP makes it harder for people (especially women) to get information on and support for sexual and reproductive health, which result in higher maternal and child mortality as well as HIV incidence around the globe.
Our paper is organized as follows. In Results, we present the results of our cross-country and individual-level analyses. In Discussion and Conclusion, we discuss the implications of our findings. In Materials and Methods, we provide the details of our empirical analysis.
Results
Global Macrolevel Associations.
In this section, we analyze the relationship between the MCP and a series of health indicators (child and maternal mortality and HIV incidence rate) at the global (cross-country) macrolevel.
Our theory suggests that countries that are more dependent on US funds for family planning services are more exposed to the MCP, whereas countries receiving more aid from other countries are less exposed to it. To account for this variation in exposure to US policy, we regress each health indicator on a dummy variable MCP, two variables measuring US and non-US funds for family planning services, the interactions of MCP with the two aid measures, and a set of controls. The two aid measures are calculated per capita, logged, and to avoid endogeneity, measured in the year before a US president’s term begins. Our control variables include several time-varying country characteristics, country fixed effects, and region × decade fixed effects. Details are in Materials and Methods.
We expect MCP and its interaction with US Aid Per Capita to be positive and MCP and its interaction with Non-US Aid Per Capita to be negative. Our key estimates are shown in Table 1, and the full regression table is in SI Appendix, Table S2.
Table 1.
Effects of the MCP conditional on a country’s dependence on foreign aid (United States and non–United States) for family planning services
| 1) Child mortality | 2) Maternal mortality | 3) HIV incidence | |
|---|---|---|---|
| MCP | 0.003 | 0.011** | 0.014** |
| (0.003) | (0.005) | (0.004) | |
| US Aid per capita | -0.002** | -0.002 | -0.001 |
| (0.001) | (0.001) | (0.001) | |
| Non-US Aid per capita | 0.001 | 0.003** | 0.004** |
| (0.001) | (0.001) | (0.001) | |
| MCP × US Aid pc | 0.001** | 0.001 | 0.004** |
| (0.001) | (0.001) | (0.001) | |
| MCP × Non-US Aid pc | -0.002* | -0.005** | -0.003 |
| (0.001) | (0.001) | (0.002) | |
| Time-varying controls | Yes | Yes | Yes |
| Region × decade FE | Yes | Yes | Yes |
| Country FE | Yes | Yes | Yes |
| Adjusted R2 | 0.983 | 0.971 | 0.976 |
| N | 3,168 | 3,001 | 2,732 |
The full set of estimates, including time-varying controls, is in SI Appendix, Table S2. The estimator is the ordinary least squares (OLS). Country-clustered robust SEs are in parentheses. FE, fixed effect. *P < 0.1; **P < 0.05.
In general, we observe a statistically and substantively significant increase in child mortality, maternal mortality, and new HIV infections when the MCP is in effect. As expected, greater dependence on US funds magnifies this relationship, while funds from non-US donors mitigate it. In every model, MCP and its interaction with US aid are positive, its interaction with non-US aid is negative, and most of these coefficients are significant at the 5% level.
To aid with the interpretation of the results, Fig. 1 plots the marginal effect of the MCP for different combinations of US and non-US aid.* In each graph, the z axis presents the marginal effect of MCP on the corresponding health outcome. The x and y axes represent Non-US Aid and US AID, respectively.† In every graph, we see that the greatest increase (i.e., worsening) in health indicators occurs in the upper far corner (painted red), where US aid is high and non-US aid is low. In contrast, the smallest increase in each indicator occurs in the lower near corner (painted blue), where US aid is low and non-US aid is high.‡ In other words, we find that US aid magnifies the positive effect of the MCP on mortality and HIV infections, while non-US aid mitigates it.
Fig. 1.
Marginal effect of the MCP on health outcomes for different levels of aid for family planning services from US and non-US sources. In each graph, the z axis presents the marginal effect of MCP. The x axis (Non-US Aid) and the y axis (US Aid) go from zero to their 99th percentile. A higher point on a graph indicates a greater increase (i.e., worsening) in the corresponding health outcome when the MCP is in effect. Estimates are based on Table 1. (A) Child mortality. (B) Maternal mortality. (C) HIV incidence.
How large are the effects? Imagine a country highly dependent on US funds (i.e., 90th percentile among US aid recipients and receiving little aid from other donors).§ Based on our estimates, we predict that this country will suffer ∼80 additional child deaths and 9 additional maternal deaths per 100,000 live births every year while the MCP is in effect. These numbers represent 1 and 3% increases over the baseline child and maternal death rates, respectively. For comparison, these effects are larger than the estimated effect of civil conflict (SI Appendix, Table S2).
We now turn to cross-country evidence concerning HIV incidence and the MCP. Restricting family planning services and closing HIV clinics can result in more unprotected sex and consequently, greater HIV transmission. We find that the MCP is positively associated with higher HIV incidence rates, especially in countries more dependent on US aid. Substantively, for a country highly dependent on US family planning aid, we predict that under the MCP, the HIV incidence rate will be higher by 1 (per 10,000 uninfected people) relative to non-MCP years. This number represents a 4% increase over the baseline HIV incidence rate.
What do our estimates imply about the global impact of the MCP? To answer this question, we focus on the countries most sensitive to changes in US aid policy. These are countries receiving high levels of aid for family planning services from the United States and significantly less from other donors. As of 2015, there were 38 countries in our sample that satisfy those criteria (i.e., they received more US aid than from other donors combined, and their per capita US aid was above the sample average).¶ The yearly total number of live births in these countries is about 30 million. Based on our estimates, reinstating the MCP in the future is likely to result in ∼24,000 additional child deaths and 2,700 additional maternal deaths every year. In addition, about 900 million people uninfected with HIV live in these countries. According to our estimates, 90,000 additional new HIV infections per year are likely to occur under the MCP. To summarize, we predict that reinstating the MCP is likely to have significant harmful consequences in the countries most dependent on US aid and over a 4-y US presidential term, result in ∼108,000 maternal and child deaths and 360,000 more HIV infections relative to periods when the MCP is not enacted. There are three reasons to believe that these figures underestimate the full burden of the MCP. First, they do not include the lingering effects of the policy after it is lifted. Our results regarding the Post-MCP dummy and its interactions with foreign aid (SI Appendix, Table S2) show that, in the 2 y following the MCP, we continue to observe substantively smaller but statistically significant effects on health outcomes, such as higher child and maternal mortality. Second, our aid variables are based on the year before a president takes office, which means they do not capture efforts by non-US donors to counteract the policy by increasing their contributions when the MCP is reinstated. Third, these numbers represent the MCP’s burden on only the countries most sensitive to US aid policy. In countries less dependent on US aid, there will be relatively milder but substantial increases in negative health outcomes.
We conduct four additional analyses to check the robustness of our results. First, we replace our dependent variables with similar health indicators to show that our results are not sensitive to small changes in measurement. Specifically, we show that the results are similar if we replace child mortality and total HIV incidence rate with infant mortality and HIV incidence rate among young people, respectively (SI Appendix, Table S3). Second, we repeat our analysis with placebo outcomes (i.e., health indicators that should be unrelated to foreign aid for family planning services) and show that there is no empirical relationship between these placebo outcomes and the MCP. Specifically, we analyze the relationship between the MCP and three placebo outcomes: Anemia among Nonpregnant Women, Death in Traffic Accidents, and Percentage Using Safe Sanitation. We do not find any evidence of an association between MCP and these outcomes, which strengthens our confidence that our findings are due to changes in US aid policy and not some unobserved factor that affects health outcomes more broadly (SI Appendix, Table S4). Third, we change our model specification by using an index measure of a country’s dependence on US aid: Difference in US vs. Non-US Aid. We prefer the original specification because nonlogged aid measures are sensitive to outliers. Nevertheless, we show that our findings remain broadly similar when using this alternative measure (SI Appendix, Table S5). Fourth, we rerun our analysis, limiting the sample to only those countries that are in low- or middle-income categories (as defined by the World Bank). Our findings continue to hold (SI Appendix, Table S6).
Microlevel Associations from LMICs.
So far, we have presented cross-country evidence that the MCP is associated with higher mortality rates and HIV incidence. We have argued that the most likely explanation for these patterns is the disruptions caused by the MCP to programs offering in-person family planning services and AIDS-related information. In this section, we provide direct individual-level evidence of this explanation from 30 countries over 33 y.
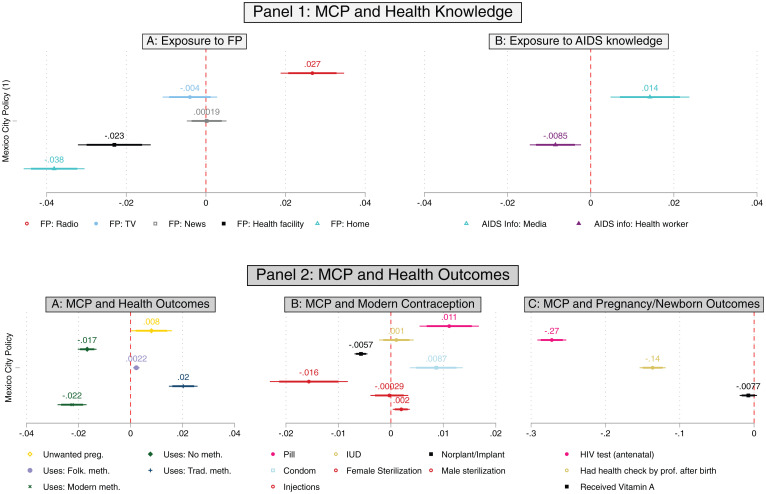
In the following econometric models, we regress indicators related to maternal and child health on a dummy variable assuming a value one when the MCP is in place and a set of controls. First, we study health-related knowledge using five binary variables that code whether the respondent received information on family planning in the past 12 mo from newspapers, radio, television, medical staff at health facilities, or in-person visits from a family planning worker at home and two binary variables that code whether the respondent received information on AIDS through media or through family planning or health workers. Second, we study maternal health–related outcomes using the information available on current contraceptive use. The Demographic Health Surveys Program (DHS) collects information on four types of contraceptive methods (traditional, folkloristic, modern, and no use). Among women using modern contraceptive methods, we also study the types of methods used. To this end, we use binary variables that take a value of one if the respondent reports currently using pills, an intrauterine device (IUD), a norplant/implant, condoms, female sterilization, male sterilization, or injections. Moreover, we restrict the sample to currently pregnant women, and we use the information available on whether the current pregnancy was desired or not. Third, we restrict the sample to women having a child under the age of 1 y at the time of the interview to study whether the baby received vitamin A in the first 2 mo from birth, whether the baby got tested for HIV as a part of antenatal care, and whether the mother had a health check by professionals after birth.
Fig. 2 summarizes the results. We start by looking at knowledge-related variables. Results from Fig. 2 A, Upper (also shown in SI Appendix, Tables S10 and S11) indicate that, as expected, women interviewed when the MCP is enacted have a lower probability of being exposed to in-person family planning either through social workers or through health facilities (consistent with evidence from Uganda reported in ref. 16) while having a higher probability of being exposed to family planning through radio. Estimated coefficients are sizable, as for most outcomes, the association with the MCP is at least as large as that of employment status. Results from Fig. 2 B, Upper (also depicted in SI Appendix, Tables S12 and S13) show that when the MCP is enacted, women are less likely to receive in-person AIDS-related information and more likely to receive it through the media. Turning to outcomes, Fig. 2 A, Lower shows that, overall, when the MCP is enacted, women are less likely to report that they are not using any method of contraception. When the MCP is enacted, those women who are using any form of contraception are less likely to report using modern contraceptives and more likely to declare that they are using traditional or folkloric methods. Digging deeper into the relationship between the MCP and modern methods of contraception, Fig. 2 B, Lower shows that among those using modern contraceptive methods, when the MCP is enacted, women prefer relatively cheaper and more accessible solutions (such as pills, condoms, and injections), which are, however, riskier if not used constantly. These relationships between the MCP, exposure to family planning programs, and current use of contraceptives could explain why all things being equal, when the MCP is in place, pregnant women are more likely to report that their pregnancy is not desired (the yellow coefficient in Fig. 2 A, Lower). When looking at the health outcomes of newborn babies and their mothers (Fig. 2 C, Lower and SI Appendix, Table S14), we note that, as expected, the MCP is negatively associated with the likelihood that babies received a test for HIV as a part of the antenatal care and that their mothers have had a health check by health professionals after birth. Once more, the magnitude of the associations is sizeable and comparable with—if not bigger than—that of belonging to the highest wealth quintile across models. Notice that, when also accounting for time trends (SI Appendix, Table S15), results are unchanged.
Fig. 2.
Coefficient estimates for the association between the MCP and health-related knowledge (A, Upper and B, Upper) and outcomes (A, Lower, B, Lower, and C, Lower). FP stands for family planning. Models are estimated on the IPUMS-DHS samples from 30 countries (1986 to 2018). Whiskers represent 90 and 95% CIs. Covariates used in the models are age, age squared, education, marital status, household size, household wealth index, urban/rural location, cluster-level share of highly educated women, birth order (only in C, Lower), and country fixed effects. SEs are clustered at the cluster level. Note that the coefficient for the variable unwanted pregnancy in A, Lower, the coefficients for the variables in B, Lower, and the coefficients for the variables in C, Lower are estimated from three smaller samples (i.e., the subset of currently pregnant women [for unwanted pregnancy], the subset of women who are currently using modern contraceptive methods [B, Lower], and the subset of mothers having the youngest child below one [C, Lower]).
SI Appendix, Tables S16–S18 use age, education, wealth, location of residence, and a measure of dependency on US funds (Difference in US vs. Non-US Aid) as moderators of the relationship between the MCP and the outcomes of interest. They show that the adverse consequences of the MCP are often greater for women from low-SES backgrounds, which indicates that long-term investment in gender equality and education can mitigate the negative effect of foreign aid cuts and ultimately, promote sustainable development (17). Finally, we focus on African countries, which have received in the last 20 y more than $100 billion in global health spending, of which roughly 75% went to addressing HIV/AIDS, malaria, maternal and child health, and nutrition.# When restricting the sample to African countries only (the “Only Africa” rows in SI Appendix, Tables S16–S18), our results are unchanged or even more clear cut.
Discussion and Conclusion
This study provides both global macrolevel and individual-level evidence of the harmful effects of the MCP on important health outcomes, such as maternal health, child health, and HIV incidence. Previous research (4) has shown that the MCP might have unintended consequences, such as raising the number of abortions, when it is in place. According to our findings, the unintended consequences of the MCP are broader than previously realized; the policy is not only counterproductive but is harmful in important ways.
At the macrolevel, our results show that the MCP is associated with higher maternal and child mortality rates and higher HIV incidence. The impact of the MCP is strongest in countries that rely more on US funding for family planning programs and weaker in countries that receive more aid from non-US donors. At the individual level, our results show that the MCP is associated with a reduction in a woman’s likelihood of being exposed to face-to-face family planning programs or using safer contraceptive methods and a higher probability of reporting that the current pregnancy was unwanted. Our results further show that children of women interviewed when the MCP is enacted are less likely to get an HIV test as part of the antenatal screening, while their mothers are less likely to be checked by health professionals after birth. Although our results are based on observational data and and cannot be interpreted as causal, the exogenous timing of the MCP and the robustness of our results to various checks strengthen our confidence in our findings.
Our analysis opens up multiple avenues for future research. First, the positive relationship between the MCP and HIV incidence suggests that sexually transmitted diseases other than HIV could spread more quickly under the MCP, an aspect worth exploring. Second, the MCP and its effects on the size and characteristics of new birth cohorts might be long lasting, an element that is still unexplored in the extant literature. Third, even more health outcomes, such as malnutrition or height and weight at birth, might be affected by the MCP, as suggested by evidence from Ghana (18). More textured case studies that examine variation in country-specific findings are also important to assess the exact consequences of the MCP in impacting the resources available and the provision of health service at the local level. Fourth, ensuring access to free essential health services is critical to mitigating the impact of any health crisis. This is especially true during or in the aftermath of global health crises, such as the COVID-19 pandemic. As noted in our paper, the MCP exacerbates global health divides and disrupts the delivery of essential sexual, reproductive, maternal, and child health services, ultimately putting a strain on already vulnerable groups. Had it not been removed, the MCP could have imposed much higher costs during the COVID-19 pandemic.
Our findings should be of interest to policy makers and activists in at least two ways. First, although observers have previously warned of the MCP’s potential impact on mortality and disease transmission, this paper provides systematic evidence of these effects. Our findings paint a fuller picture of the MCP’s unintended consequences and can help activists and policy makers who seek to redesign or counteract it. Second, our finding that non-US funding tends to mitigate the MCP’s effects highlights the importance of non-US actors stepping up when the MCP is reinstated. In particular, international aid donors should prepare a contingency fund to counteract the MCP’s effects, and it should prioritize countries that are most dependent on US aid and therefore, most sensitive to the effects of the MCP.
Materials and Methods
Our empirical analysis includes a global macrolevel (cross-country) analysis and a microlevel (individual-level) analysis. This section presents an in-depth description of the data and methods used in the empirical analysis.
Global Macrolevel (Cross-Country) Analysis.
Data.
Data for health outcomes come from the World Development Indicators (WDIs).‖ Our samples cover the years 1990 to 2015 and up to 134 countries for which we have the necessary data. Data on foreign aid come from the Development Assistance for Health Database (DAHD) (collected from ref. 19) and have two main advantages. 1) The DAHD includes not only aid given bilaterally but also, aid through multilateral agencies and NGOs. 2) The DAHD disaggregates funds in terms of their purpose and separates funds for reproductive and maternal health (the category of data we use in our analyses) from other categories (e.g., funds for malaria). In short, the detailed and comprehensive nature of the database allows us to produce good measures of countries’ dependence on foreign funds for family planning services. Data on the Gross Domestic Product (GDP) and population come from WDIs. Data on civil conflict come from the Uppsala Armed Conflict database (20), and data on political regime type come from the V-Dem project (21).
Methods.
In the global macrolevel portion, we conduct a series of time series cross-national regressions in which our dependent variables are child and maternal mortality rates and HIV incidence rates. We log the dependent variables to reduce the influence of outliers. Theoretically, countries that are more dependent on US funds for family planning services will be more sensitive to changes in US policy, while those receiving more aid from non-US donors will be less sensitive (4). For this reason, we regress each dependent variable on the following explanatory variables: a dummy variable (MCP), two indicators of aid for family planning services from US and non-US donors, interactions of MCP with US and non-US funds, and a set of controls and fixed effects. Both aid variables (US Aid pc and Non-US Aid pc) are calculated per capita and logged. As mentioned above, to measure a country’s exposure to the MCP, our aid measures only include funds for reproductive and maternal health. To avoid endogeneity, we measure the aid variables in the last year before a US president’s term begins (e.g., 1992 for Clinton).
Our controls include two dummy variables (Pre-MCP and Post-MCP) that indicate the 2 y before and after the MCP’s implementation and their interactions with US and non-US foreign aid. These variables take into account the possibility of pre-MCP trends or post-MCP lingering effects of the policy. We also include country fixed effects and five time-varying country characteristics (logged GDP per capita and Population, GDP Growth, a Civil Conflict dummy, and a Liberal Democracy Index) to control for country-level factors correlated with health outcomes. The time-varying country characteristics are lagged. Lastly, we include region × decade dummies to account for global and regional shocks, such as medical innovation. We use the the ordinary least squares (OLS) estimator and report robust SEs clustered at the country level.
Formally, for our macroanalysis, we estimate the following model:
| [1] |
where is a health outcome for country c in year t. The key explanatory variables are MCPt, , and . Consequently, we use the coefficients γ1, γ4, and γ5 to understand the impact of the MCP on . represents the time-varying country-level controls (GDP per capita, Population, GDP Growth, Civil Conflict, and Liberal Democracy Index). represents country fixed effects. represent the set of region × decade dummies.
To strengthen our claim about the effects of the MCP, we follow a four-pronged strategy. The first two analyses rerun the main model using different health outcomes. First, we repeat our analysis using other health outcomes that are conceptually similar to our main dependent variables and show that our findings remain similar. Specifically, we repeat our analysis using Infant Mortality (instead of Child Mortality) and HIV Incidence among Young Adults (instead of Total HIV Incidence). Second, we conduct placebo tests. If changes in foreign aid are the key factor behind the MCP’s effects, then our results should disappear when we study health outcomes that are theoretically unrelated to family planning. Indeed, repeating our analysis with three placebo dependent variables (Anemia among Nonpregnant Women, Death in Traffic Accidents, and Percentage Using Safe Sanitation), we do not find an effect for the MCP and US aid.**
Our third check is to use an alternative measure of a country’s dependence on US funds. This measure (Difference in US vs. Non-US Aid) is defined as US Aid per capita minus Non-US Aid per capita and is higher for countries that are more dependent on US aid.†† When we repeat our analysis using this measure, we again find that the MCP is positively correlated with mortality and HIV incidence, especially in countries that are more dependent on US funds. Our fourth check is to limit our analysis to LMICs (according to World Bank categorization) because these countries should be more sensitive to fluctuations in foreign aid than high-income countries. Our findings are robust to this check.
Microlevel (Individual-Level) Analysis.
Data.
As for the individual-level part, we employ the IPUMS-DHS dataset.‡‡ We rely on this dataset, which contains thousands of consistently coded variables on the health and well-being of women and children from the DHS data. The DHS collects information on a wide range of topics related to women and their offspring across LMICs, such as contraceptive use, maternal health, and child health and nutrition. Respondents are women aged 15 to 49 whose husbands/partners are either permanent members of the surveyed household or visited the household the night before the interview. To be included in the dataset, the countries should report the interview date and information both before and after the MCP. We, therefore, conduct our main analysis on individual-level data from 141 nationally representative household surveys across 30 countries from 33 y (from 1986 to 2018). SI Appendix, Table S8 depicts the combination of countries/years included in the analysis.
Methods.
Our estimation framework proceeds in parallel with the macroanalysis; we implement a series of individual-level analyses in which we regress indicators related to maternal and child health on a dummy variable (MCP) and a set of controls. The main model of the microanalysis is
| [2] |
where MCPi is the key explanatory variable. Consequently, δ1 is the estimate of the impact of the MCP on Outcomei. and are matrices that contain individual-level controls and cluster-level covariates, respectively (SI Appendix).
The main explanatory variable (MCPi in Eq. 2, MCP) equals one when the policy is in place. Our dependent variables (Outcomei in Eq. 2) include five binary variables that code whether the respondent received information on family planning in the past 12 mo from newspapers, radio, television, medical staff at health facilities, and family planning workers visiting the house; two binary variables that code whether the respondent received information on AIDS through media or through family planning or health workers; current contraceptive use (traditional, folkloristic, modern, and no use); current type of modern contraceptive use (variables that take a value of one if the respondent reports currently using pills, IUD, norplant/implant, condoms, female sterilization, male sterilization, and injections); whether the current pregnancy was desired or not; whether the baby received vitamin A in the first 2 mo from birth; whether he/she got tested for HIV as a part of the antenatal care; and whether the mother had a health check by health professionals after birth. In analyses involving the variables related to exposure to knowledge (i.e., the five binary variables that code whether the respondent received information on family planning in the past 12 mo and the two binary variables that code whether the respondent received information on AIDS), we set the cutoff point for the MCP 1 y after its (re-)implementation [MCP (1)] because the knowledge variables are retrospective. As a robustness check, we restricted the sample to only those surveys that were on the field exactly in between the implementation (or withdrawal) of the MCP by taking advantage of the fact that some interviews were done after the official closure of the field work. In our sample, those countries are Burkina Faso (1993), Uganda (2001), Senegal (1992), Mali (2001), Madagascar (2008), Kenya (2008), India (1992), and Burundi (2016). Recall that our explanatory variable is created using the date of the interview. As a result, using a restricted time frame (1 y before or after the introduction/withdrawal of the policy) and limiting the analysis to those countries that were on the field during the implementation (withdrawal) of the MCP would greatly reduce the probability that our estimation strategy is biased due to omitted secular time trends. Furthermore, we also conducted a placebo analysis on the same sample of countries by setting an arbitrary cutoff point. The results (reported in SI Appendix, Table S19) are virtually unchanged when using a limited time frame and are, reassuringly, insignificant when using a placebo test. The analyses of variables related to newborn children and pregnant women are conducted on the restricted samples of women having children younger than 1 y and being pregnant at the time of interview, respectively. Our control variables (Xi in Eq. 2) include the respondent’s current age and its square, the respondent’s years of education, dummies for current employment and marital status, household size, household-level wealth index, urban/rural location of residence, and two measures at the cluster level that represent the share of women who are highly educated and who are using a modern method of contraception. In models regarding children’s health outcomes, we also control for birth order. Notice that, as a robustness check in SI Appendix, Table S15, we also account for time trends. SI Appendix, Tables S16–S18 use age, education, wealth, location of residence, and a measure of dependency on US funds (Difference in US vs. Non-US Aid) as moderators (i.e., an interaction model) of the relationship between the MCP and the outcomes of interest. The dependency variable is defined more precisely in the previous subsection.
Our main empirical strategy is to estimate an OLS regression for each outcome (or a linear probability model when the dependent variable is binary). When we estimate a multilevel model or a probit model, the results are qualitatively unchanged. All analyses are pooled, with country fixed effects included. Analyses are weighted using DHS sampling weights.§§ SEs are clustered at the cluster level.
Summary statistics for our macrolevel and microlevel analyses are in SI Appendix (SI Appendix, Tables S1 and S9).
Supplementary Material
Acknowledgments
V.R. thanks the Leverhulme Trust within the Leverhulme Center for Demographic Science for support. K.C.K. and V.R. acknowledge funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation program (Grant 694262), project DisCont– Discontinuities in Household and Family Formation (PI: F. C. Billari).
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
See online for related content such as Commentaries.
*Fig. 1 is based on models 1 to 3 in Table 1. SI Appendix, Figs. S1–S3 present these graphs in two-dimensional format with 95% CIs.
†Each axis varies the corresponding variable between zero and its 99th percentile.
‡For example, according to Fig. 1A, when Non-US Aid is near its maximum and US Aid is near zero, the marginal effect of the MCP on child mortality is essentially zero (dark blue region). In contrast, when Non-US Aid is near zero and US Aid is near its sample maximum, then we predict (logged) child mortality to be about 0.01 higher under the MCP relative to non-MCP periods (dark red region).
§Specifically, we assume that US aid is 90 USD per capita, while non-US aid is zero.
¶SI Appendix, Table S7 lists these 38 countries.
#Information is available at https://sgp.fas.org/crs/row/R46368.pdf.
‖Information is available at https://databank.worldbank.org/source/world-development-indicators.
**Anemia is measured as a percentage. Deaths in traffic accidents are per 100,000 people. Data come from WDI.
††We also considered using “percentage of aid coming from the United States,” but it is a coarse measure that does not capture the scale of foreign aid coming to a country. Two countries can receive the same percentage of their aid from the United States, but if the amount of aid per capita is much higher in one country, then it will be more sensitive to US aid policy. For example, in 2015, Bolivia and Sudan both received about 65% of their (family planning–related) aid from the United States; however, Bolivia received 120 US dollars (USD) per capita, while for Sudan, this number was only 5 USD.
‡‡Information is available at https://www.idhsdata.org/idhs/.
§§The DHS sampling design is based on the last available population census for each country.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2123177119/-/DCSupplemental.
Data Availability
Code data have been deposited in Open Science Framework (https://osf.io/tec6a/).
References
- 1.Casterline J. B., “Determinants and consequences of high fertility: A synopsis of the evidence.” Washington, DC: The World Bank; 2010. http://documents.worldbank.org/curated/en/389381468147851589/pdf/630690WP0P10870nants0pub08023010web.pdf. Accessed 6 April 2022.
- 2.Goldin C., Katz L. F., The power of the pill: Oral contraceptives and women’s career and marriage decisions. J. Polit. Econ. 110, 730–770 (2002). [Google Scholar]
- 3.Miller G., Contraception as development? New evidence from family planning in Colombia. Econ. J. (Lond.) 120, 709–736 (2010). [Google Scholar]
- 4.Brooks N., Bendavid E., Miller G., USA aid policy and induced abortion in sub-Saharan Africa: An analysis of the Mexico City Policy. Lancet Glob. Health 7, e1046–e1053 (2019). [DOI] [PubMed] [Google Scholar]
- 5.Schaaf M., Maistrellis E., Thomas H., Cooper B.; GGR Research Working Group, ‘Protecting life in global health assistance’? Towards a framework for assessing the health systems impact of the expanded global gag rule. BMJ Glob. Health 4, e001786 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mavodza C., Goldman R., Cooper B., The impacts of the global gag rule on global health: A scoping review. Glob. Heal. Res. Policy 4, 26 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zulu J. M., Haaland M. E. S., Situating the Mexico City Policy: What shapes contraceptive access and abortion? Lancet Glob. Health 7, e984–e985 (2019). [DOI] [PubMed] [Google Scholar]
- 8.Barot S., Cohen S. A., The global gag rule and fights over funding UNFPA: The issues that won’t go away. Guttmacher Policy Rev. 18, 27–33 (2015). [Google Scholar]
- 9.Bingenheimer J. B., Skuster P., The foreseeable harms of Trump’s global gag rule. Stud. Fam. Plann. 48, 279–290 (2017). [DOI] [PubMed] [Google Scholar]
- 10.Ushie B. A., et al., Foreign assistance or attack? Impact of the expanded global gag rule on sexual and reproductive health and rights in Kenya. Sex. Reprod. Health Matters 28, 1794412 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bendavid E., Avila P., Miller G., United States aid policy and induced abortion in sub-Saharan Africa. Bull. World Health Organ. 89, 873–880C (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Meulen Rodgers Y., The Global Gag Rule and Women’s Reproductive Health: Rhetoric Versus Reality (Oxford University Press, 2018). [Google Scholar]
- 13.Della Vigna S., La Ferrara E., “Economic and social impacts of the media” in Handbook of Media Economics, Anderson S., Waldfogel J., Stromberg D., Eds. (North Holland, 2015), pp. 723–768. [Google Scholar]
- 14.Huber D., Saeedi N., Samadi A. K., Achieving success with family planning in rural Afghanistan. Bull. World Health Organ. 88, 227–231 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malarcher S., et al., Provision of DMPA by community health workers: What the evidence shows. Contraception 83, 495–503 (2011). [DOI] [PubMed] [Google Scholar]
- 16.Giorgio M., et al., Investigating the early impact of the Trump administration’s global gag rule on sexual and reproductive health service delivery in Uganda. PLoS One 15, e0231960 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lutz W., et al., Education rather than age structure brings demographic dividend. Proc. Natl. Acad. Sci. U.S.A. 116, 12798–12803 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke M., Gong E., Jones K., Income shocks and HIV in Africa. Econ. J. (Lond.) 125, 1157–1189 (2015). [Google Scholar]
- 19.IHME, Development assistance for health database 1990-2019 (2020). Accessed 4 July 2020.
- 20.Harbom L., Melander E., Wallensteen P., Dyadic dimensions of armed conflict, 1946–2007. J. Peace Res. 45, 697–710 (2008). [Google Scholar]
- 21.Coppedge M., et al., V-Dem [Country-Year/Country-Date] Dataset v10 (2020). Accessed 18 April 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Code data have been deposited in Open Science Framework (https://osf.io/tec6a/).